Abstract
Heart failure (HF) is a clinical syndrome, which is becoming a major public health problem in recent decades, due to its increasing prevalence, especially in the developed countries, mostly due to prolonged lifespan of the general population as well as the increased of HF patients. The HF treatment, particularly, new pharmacological and non-pharmacological agents, has markedly improved clinical outcomes of patients with HF including increased life expectancy and improved quality of life. However, despite the facts that mortality in HF patients has decreased, it still remains unacceptably high. This review of summarizes the evidence to date about the mortality of HF patients. Despite the impressive achievements in the pharmacological and non-pharmacological treatment of HF patients which has undeniably improved the survival of these patients, the mortality still remains high particularly among elderly, male and African-American patients. Patients with HF and reduced ejection fraction have higher mortality rates, most commonly due to cardiovascular causes, compared with patients HF and preserved ejection fraction.
Keywords: heart failure, mortality, race, elderly, gender
Introduction
Heart failure (HF) is a clinical syndrome, which is becoming a major public health problem in recent decades, due to its increasing prevalence, especially in the developed countries (1, 2). The increased prevalence is mostly due to prolonged lifespan of the general population in these countries (2, 3) as well as the increased life expectancy of HF patients. The life expectancy is prolonged in HF patients, mainly due to the improved pharmacological and non-pharmacological treatment (4). The etiology of HF is different in different countries and different populations, but nowadays arterial hypertension and coronary artery disease (CAD) are predominant etiologic factors (5). In the past, HF with reduced left ventricular ejection fraction (HFrEF) was the most commonly diagnosed clinical entity in HF patients. However, with the improvement of diagnostic tools, especially with the introduction of new echocardiography modalities, recent clinical and epidemiologic studies have shown that nearly half of HF patients have preserved EF, and this clinical entity of HF with preserved left ventricular EF (HFpEF) was introduced as (6, 7). HF is one of the most frequent causes of hospitalizations and multiple hospitalizations (8), as well as of high costs (9). Recent studies have shown that the HF treatment, particularly, new pharmacological agents, implantation of intra-cardiac defibrillators (ICD), cardiac resynchronization therapy (CRT) and other surgical procedures, has markedly improved clinical outcomes of patients with HF including increased life expectancy and improved quality of life (4, 10). However, despite the facts that mortality in HF patients has decreased, it still remains unacceptably high (3).
Trends of mortality in patients with heart failure
Many studies have addressed trends in the mortality and survival patients with HF comparing different time periods in different countries (Table 1). Based on the Framingham Heart Study, the mortality rate after diagnosis of HF in the USA was around 10% at 30 days, 20-30% at 1 year and 45-60% over 5 years of follow-up (11). Conversely, the Rotterdam study, which included HF patients in Europe, showed a lower mortality, with 11% and 41% mortality rates at 1 year and 5 years of follow-up, respectively (12).
Table 1.
The mortality rate in heart failure patients in different period of time
| Author | Study | Number of patients | Period of time | Mortality | P |
| Levy et al. (11) | Framingham Heart Study, USA | 1075 | 1950 - 1959 | 1 year, M: 30%, F: 28% 5 years, M: 70%, F: 57% |
0.01, for M 0.02, for F |
| (Population Based cohort) | 1990 - 1999 | 1 year, M: 28%, F: 24% 5 years, M: 57%, F: 45% |
|||
| Roger et al. (17) | Olmsted Country MN, USA | 4537 | 1979 -1984 | 1 year, M: 30%, F: 20% 5 years, M: 65%, F: 51% |
<0.001, for M <0.001, for F |
| (Population Based cohort) | 1996-2000 | 1 year, M: 21%, F: 17% 5 years, M: 50%, F: 46% |
|||
| Loh et al. (4) | Ahmanson-University of California | 2507 | 1993 - 1998 | 1 year, 20.6% 3 years, 36.4 % |
0.04, for 1 y 0.02, for 3 y |
| Los Angeles Cardio-myopathy Centre | 2005 - 2010 | 1 year, 17.8% 3 years, 31.5% |
|||
| Mehta et al. (14) | Hillingdon-Hasting study, England | 948 | 1995 - 1997 2004 - 2005 |
6 months, 22% 6 months, 16% |
<0.001 |
| (Population Based cohort) | |||||
| Laribi et al. (15) | Seven European Countries | 1987 2008 |
54.2/100 000 32.6/100 000 |
<0.001 | |
| (Population Based cohort) | |||||
| Gomez-Soto et al. (13) | Framingham criteria HUPR, Spain | 4793 | 2000 2007 |
1 year, M: 34.8/100 F: 27.0/100 |
<0.05, for M <0.05, for F |
| 1 year, M: 33.4/100 F: 23.7/100 |
F - female; M: male; MN - Minnesota; Seven European Countries - Germany, Greece, England and Wales, Spain, France, Finland and Sweden; HUPR - The University Hospital of Puerto Real; y - year
Most epidemiological studies demonstrated a trend toward a decrease in mortality rates in HF patients in the last decades (3, 4, 13). From the 1959-1969 to 1990-1999 time periods, mortality in HF patients is decreased from 70% to 59% in man, and from 57 to 45% in women (3). Hillingdon-Hasting Study demonstrated that 6-month mortality after diagnosis of HF decreased significantly (p<0.001) from 26% in 1995-1997 to 14% in 2004-2005 (14). Similarly, the Framingham heart study documented that 30-day, 1-year and 5-year mortality among men with HF declined (p=0.01) from 12%, 30% and 70% in the period 1959-1969, to 11%, 28% and 59% in the period 1990-1999. The mortality rate among women was also decreased (p=0.02) from 18%, 28% and 57% in the period 1959-1969 to 10%, 24% and 45% in the period 1990-1999 (3, 11). Along the same lines, the study by Loh et al. (4) showed a significant decrease of 3 years mortality among patients with HF with reduced EF from 36% in the time period between 1993 and 1998 to 31% in the time period between 2005 and 2010 (p=0.02). Moreover, a recent study by Laribi et al. (15) found that mortality decreased in seven European countries (Germany, Greece, England and Wales, Spain, France, Finland and Sweden) from 52 per 100 000 inhabitants in 1987, to 33 per 100 000 inhabitants in 2008.
In summary, the overall survival and lifespan of HF patients increased in last decades, particularly after 1998 (4, 16). From 1989-1991 to 1999-2001, the survival of patients with HF at 30 days, 1 year and 5 years, improved by 5%, 10% and 9%, respectively (16). Data from the Framingham study showed comparable improvement in the long-term survival in both man and women (12% per decade) after HF onset (11). Likewise the Olmsted Country study underscored the improvement of 5-year survival, from 43% during the period of time 1979-1984 to 52%, during the period of 1996-2000 (p<0.001). This survival improvement was better in women than men (17). The study by Barker et al. (18) showed an improvement of survival in elderly (≥65 years) patients after the HF diagnosis, by 33% in men and 24% in women from mid-1970s to mid-1990s.
In-hospital mortality in patients with heart failure
Epidemiological studies have shown that despite increased total number of HF hospitalizations and readmissions rates in last decades (19), the mean length of hospital stay as well as the in-hospital mortality were significantly decreased (Table 2) (8, 20). Data from the National Hospital Discharge Survey showed that the total number of hospitalizations for HF in USA was tripled from 1979 to 2004 (21). Likewise, Blecker et al. (22) showed that hospitalizations for HF in USA increased from 2.75 million in 2001 to 3.15 million in 2009.
Table 2.
Trends of mortality in heart failure related hospitalization, in different period of time
| Author | Setting | Number of hospitalizations | Period of time | Mean length of stay | In-hospital mortality |
|---|---|---|---|---|---|
| Kosiborod et al. (25) | CMS, USA | 3 957 520 | 1992 | 7.3 days | 30 days: 11.0% 1 year: 32.5% |
| 1999 | 5.5 days | 30 days:10.3% 1 year: 31.7% |
|||
| Bueno et al. (22) | MEDPAR, CMS USA |
498 500 412 614 |
1993 2003 |
8.8 days 6.3 days |
8.50% 4.20% |
| Schaufelberger et al. (24) | National Hospital Discharge Register Sweden | 156 919 | 1988 | 1 year age 45-54, M: 23%, F: 31% age 75-84, M: 48%, F: 41% |
|
| 2000 | 1 year age 45-54, M: 9%, F: 8% age 75-84, M: 36%, F: 29% |
||||
| Blackledge et al. (23) | Office of National Statistics England | 498 500 413 614 |
1993-1994 2000-2001 |
9 days 9 days |
22 months, 24.8% 22 months, 20.5% |
| Shahar et al. (26) | Hospitals of Minneapolis-St. | 2257 | 1995 | 6 months, M: 27%, F: 21% 1 year, M: 36%, F: 27% |
|
| USA | 1825 | 2000 | 6 months, M: 21%, F: 18% 1 year, M: 27%, F: 27% |
CMS - Centers for Medicare and Medicaid Services; F - female; M - male; MEDPAR - Medicare Provider Analysis and Review
The Based on Centers for Medicare and Medicaid Services (CMS) data, showed that in-hospital mortality rate in HF patients during the 16 years study period, declined by 4.3%, from 1993 to 2008 (8.5% to 4.2%, p<0.001) (23). The mean length of hospital stay also decreased (p<0.001) from 6 days in 1987-1991 to 4 days in 2002-2007 (8). Moreover, Blackledge et al. (24) showed that, similarly to other countries, the hospital mortality rate decreased in England from 25% during the 1993-1994 to 20% during 2000-2001 years. In Sweden, Schaufelberger et al. (25), also reported trends toward decreasing hospital mortality due to HF, from 1988 to 2000, but the decrease rate was more evident among patients of younger age. In this study, between 1988 and 2000, 1-year mortality declined from 9% in men and 10% in women 45-54 years of age and 4% and 5%, respectively among men and women among 75-84 years of age. Contrary to this study, Kosiborod et al. (26) found no substantial improvement in mortality, during the 1990s particularly among elderly patients hospitalized with HF. In this study, 30-day mortality (11.0% to 10.3%) and 1-year (32.5% to 31.7%) inhospital mortality did not change significantly during the study period between 1992 and 1999.
Mortality in HF patients in relation to age, gender and race
There are differences in mortality of patients with HF in groups according age, gender and race (Fig. 1) (2). The earlier studies have shown that mortality rate in HF patients is age-dependent and it increases progressively with the advancing age (27-30). As the life of expectancy lengthened in recent years in Western Countries, the mean age of patients at the time of death increased in last decade: from 70±9 years, before 1980, to 81±9 years after1980 (27). Saczynski et al. (28) found that in-hospital death rates increased from 3% in patients younger than 65 years to 8.2% in those older than 75 years. In addition, the study of Wong et al. (29), also demonstrated that mortality rate increased by increasing patients’ age. In this study, 3-year mortality of HF patients increased parallel to the age of patients at the time of their admission for symptomatic HF: 12% (for the age group 20-39 years), 13% (for the age group 40-49 years), 13% (for the age group 50-59 years), 19% (for the age group 60-69 years) and 31% (for the age group ≥70 years). In contrast, Rodriguez etal. (30), using data from the 2007-2008 Healthcare Cost and Utilization Project, found an U-shaped pattern of mortality across the ages for men with mortality rates for age groups <25, 25-64, and >64 years being 2.9%, 1.4%, and 3.8%, respectively.
Figure 1.
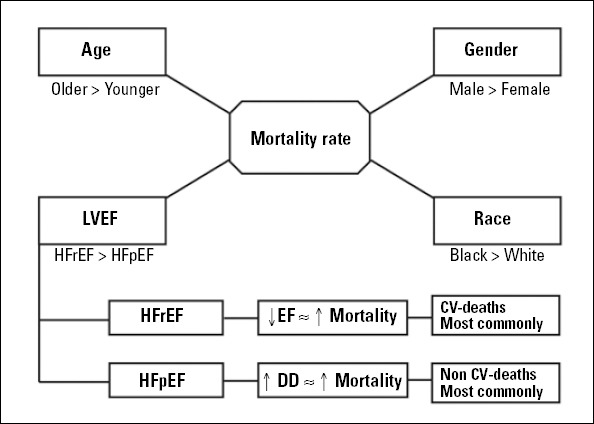
CV - cardiovascular; DD - diastolic dysfunction; EF - ejection fraction; HFpEF - heart failure with preserved ejection fraction; HFrEF - heart failure with reduced ejection fraction; LVEF - left ventricular ejection fraction
Moreover, several studies showed that mortality was different in male vs. female patients with HF (Table 3), (17, 31-34). In the study by Rathore et al. (32), the mortality rate was lower in female patients than in male US patients with HF during time period between 1998 and 1999. In this study, the 30-day mortality was 9.2%, in female patients versus 11.4% in male patients (p<0.001). Similarly, 1-year mortality was 36.2% in females versus 43.0% in males (p<0.001). The cohort study by Vaartjes et al. (33), which was based on the National Cause of Death Registry, showed that mortality risk for HF is higher among men than women. One-year mortality risk was 17% in men and 14% in women younger than 55 years, and 58% in men and 49% in women older than 85 years. However, the 5-year mortality risk in these patients did not differ between genders. Few epidemiological data have also shown that the mortality rate in patients with HF did not differ according to gender (34, 35).
Table 3.
The mortality rate in patients with heart failure male vs. female
| Author | Study | Period of time | Follow up | Number of patients | Mortality in males | Mortality in females | p |
|---|---|---|---|---|---|---|---|
| Rathore et al. (31) | NHF Project, USA | 1998-1999 | 30 996 | 30 day: 11.4% | 30 day: 9.2% | <0.001 | |
| (Population Based cohort) | 1 year: 43.0% | 1 year: 36.2% | <0.001 | ||||
| Parashar et al. (32) | CHS Forsyth Country, North Carolina | 1989-1993 | 3 years | 1264 | White: 35.5/100 American-African: 33.6/100 | White: 44.4/100 American-African: 40.5/100 | |
| Roger et al. (17) | Olmsted Country, MN (Population based cohort) | 1996-2000 | 4.2 years (mean) | 1 year: 21% 5 years: 50% |
1 year: 17% 5 years: 46% |
<0.001 <0.001 |
|
| Sakata et al. (35) | CHART-2 Study Japan Prospective study | 2006-2010 | 3.1 years (mean) | 4736 | 47.3/1000 | 52.4/1000 | 0.22 |
CHART-2 Study - Chronic Heart Failure Analysis and Registry in the Tohoku District; CHS - Cardiovascular Health Study; NHF Project - National Heart Failure Project
Racial or ethnic differences in the mortality among patients with HF have been reported. It has been reported that mortality in African American patients was higher than in white patients (2). From the Atherosclerosis Risk in Communities (ARIC) study, the 2-year mortality rates were similar for white and African- American patients, but 5-year mortality rate was higher among African-American male (52% vs. 41%, p=0.02) and female (46% vs. 36%, p=0.03) patients compared with white patients with HF (36).
Mortality rate in HFrEF compared HFpEF
In general, the mortality rate of patients with HFpEF varied substantially across the studies (7). Many cohort studies reported lower mortality in HFpEF patients compared with HFrEF patients (Table 4) (8, 37). Smith et al. (38) found that patients with HFrEF had a higher death rate during six months of follow-up compared with HFpEF patients (21% vs. 13%; p=0.02). Along the same lines, the Veterans Administration Heart Failure Trial (V-HeFT) showed that the annual mortality was higher in HFrEF compared with HFpEF patients (19% vs. 8%, p=0.0001) (39). Similarly, the study by Tribouilloy et al. (40), showed that patients with reduced EF had higher in-hospital mortality rate than those with preserved (8.2% vs. 2.7%, p=0.002). Similarly, a meta-analysis of 17 studies of HF patients with a total of 24501 patients, by Somaratne et al. (41) also showed that there is difference in mortality between these two groups of patients. In this study, after 47 months of follow-up period (starting in 2006), the mortality rate among patients with HFrEF was 40.6% compared with 32.1% among HFpEF patients. In regard to age, Kerzner et al. (42) found that mortality rate in elderly HFrEF patients was higher compared with HFpEF (53.9% vs. 35.8%, p=0.03), whereas in patients older than 75 years, the difference in mortality rates between groups was not significant (38.5% vs. 29.6%, p=0.22).
Table 4.
The mortality in patients with HFrEF vs. HFpEF
| Author | Study | Period of time | Follow up | Number of patients | Mortality in HFrEF | Mortality in HFpEF | P | |
|---|---|---|---|---|---|---|---|---|
| Gottdiener et al. (41) | CHS, USA | 1989-1993 | 6.4 years | 300 | 6 year: 54% | 6 year: 43% | <0.001 | |
| Smith et al. (37) | Yale-New Haven Hospital Center | 1996-1998 | 6 months | 413 | 6 months: 21% | 6 months: 13% | 0.02 | |
| Kerzner et al. (42) | SSA Death Registry Washington, USA | 1999-2001 | 25 months (mean) | 373 | Age<75y: 38.5% Age≥75 y: 53.9% |
Age<75y: 29.6% Age≥75 y:35.8% |
0.22 0.03 |
|
| Tribouilloy et al. (39) | Framingham Criteria, France | 2000 | 1 year | 799 | 8.20% | 2.70% | 0.002 | |
| Bhatia et al. (44) | EFFECT study Ontario, Canada | 1999-2001 | 1 year | 2802 | 30 days: 7.0% 1 year: 26% |
30 days: 5.0% 1 year: 22% |
0.08 0.07 |
|
| Quiroz et al. (45) | BMC, USA GWTG registry | 2006-2008 | 22 months | 1097 | 30 days: 3.0% 1 year: 18.2% |
30 days: 2.7% 17.10% |
0.74 0.34 |
BMC - Boston Medical Centre; CHS - Cardiovascular Health Study; EFECT - Enhanced Feedback for Effective Cardiac Treatment; GWTG - Get With The Guidelines registry;
HFpEF - Heart Failure with preserved ejection fraction; HFrEF - failure with reduced ejection fraction; SSA Death registry - Social Security Administration Death Registry
On the other hand, several epidemiological cohort studies reported similar mortality rates in patients with HFpEF and HFrEF (43-45). Bhatia et al. (44) based on the data from 103 hospitals in the province of Ontario, Canada during the 1999-2001 period, demonstrated that mortality rate in these two types of HF was similar: 1 year mortality in HFrEF was 26% compared to 22% in HFpEF (p=0.07). More recently, Quiroz et al. (45) noted that 30-day and 1-year mortality rates were not different between HFrEF and HFpEF groups (3.0% versus EF versus 2.7%, p=0.74 for 30-day mortality and 18.2% versus 17.1%, p=0.34 for 1-year mortality, respectively).
Several studies have shown that the mortality rate among patients with HFrEF correlates closely with the level of reduced left ventricular EF (46, 47). Curtis et al. (47) based on the Digitalis Investigation Group (DIG) trial showed that the mortality rate increased proportionally with the decrease in the left ventricular EF. In this study, the mortality rates among patients group with left ventricular EF <15%, 16-25%, 26-35% and 36-45% were 51%, 41.7%, 31.4% and 25.6%, respectively. The mortality rates, however, were comparable among patients with HFpEF (23.3% among patients with left ventricular EF 46-55% versus 23.5% among patients with left ventricular >55%; p=0.25). Redfield et al. (48) described a relationship between the degree of diastolic dysfunction and mortality in HFpEF. Mortality rate in HFpEF increased as the degree of diastolic dysfunction increased. Compared to normal, mild diastolic dysfunction increased the risk of death by 8.3 fold (p<0.001) and moderate to severe diastolic dysfunction increased the risk of mortality by 10.2 fold (p<0.001).
The mode of death is also different between the two groups of patients. Among patients with reduced EF, death was due to cardiovascular causes in 64% of deaths (43% coronary heart disease and 21% other cardiovascular causes) and to non-cardiovascular causes in 36%. In contrast, deaths among patients with preserved EF were most commonly due to non-cardiovascular causes (49% of all deaths) followed by coronary artery disease (29%) and other cardiovascular (22%) causes (49). Similarly, Hamaguchi et al. (50) also showed that mortality from non-cardiovascular causes was significantly higher among HFpEF than among patients with HFrEF (28% vs. 18%, p=0.02). In particular, cardiovascular causes including sudden death, were more frequent among patients with reduced EF compared with patients with preserved EF (68% vs. 58%, p=0.02).
Conclusion
Despite the impressive achievements in the pharmacological and non-pharmacological treatment of HF patients which has undeniably improved the survival of these patients, the mortality still remains high particularly among elderly, male and African American patients. HFrEF patients have higher mortality rates, most commonly due to cardiovascular causes, compared with patients with HFpEF.
Footnotes
Conflict of interest: None declared.
References
- 1.Roger VL. Epidemiology of heart failure. Circ Res. 2013;113:646–59. doi: 10.1161/CIRCRESAHA.113.300268. [CrossRef] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bui AL, Horwich TB, Fonarow GC. Epidemiology and risk profile of heart failure. Nat Rev Cardiol. 2011;8:30–41. doi: 10.1038/nrcardio.2010.165. [CrossRef] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mosterd A, Hoes AW. Clinical epidemiology of heart failure. Heart. 2007;93:1137–46. doi: 10.1136/hrt.2003.025270. [CrossRef] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Loh JC, Creaser J, Rourke DA, Livingston N, Harrison TK, Vandenbogaart E, et al. Temporal trends in treatment and outcomes for advanced heart failure with reduced ejection fraction from 1993-2010: findings from a university referral center. Circ Heart Fail. 2013;6:411–9. doi: 10.1161/CIRCHEARTFAILURE.112.000178. [CrossRef] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lee DS, Gona P, Vasan RS, Larson MG, Benjamin EJ, Wang TJ, et al. Relation of disease etiology and risk factors to heart failure with preserved or reduced ejection fraction. Circulation. 2009;119:3070–7. doi: 10.1161/CIRCULATIONAHA.108.815944. [CrossRef] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Owan TE, Redfield MM. Epidemiology of diastolic heart failure. Prog Cardiovasc Dis. 2005;47:320–32. doi: 10.1016/j.pcad.2005.02.010. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 7.Lam CS, Donal E, Kraigher-Krainer E, Vasan RS. Epidemiology and clinical course of heart failure with preserved ejection fraction. Eur J Heart Fail. 2011;13:18–28. doi: 10.1093/eurjhf/hfq121. [CrossRef] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dunlay SM, Redfield MM, Weston SA, Therneau TM, Hall Long K, Shah ND, et al. Hospitalizations after heart failure diagnosis a com-munity perspective. J Am Coll Cardiol. 2009;54:1695–702. doi: 10.1016/j.jacc.2009.08.019. [CrossRef] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rohde LE, Bertoldi EG, Goldraich L, Polanczyk CA. Cost-effectiveness of heart failure therapies. Nat Rev Cardiol. 2013;10:338–54. doi: 10.1038/nrcardio.2013.60. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 10.Friedrich EB, Böhm M. Management of end-stage heart failure. Heart. 2007;93:626–31. doi: 10.1136/hrt.2006.098814. [CrossRef] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Levy D, Kenchaiah S, Larson MG, Benjamin EJ, Kupka MJ, Ho KK, et al. Long-term trends in the incidence of and survival with heart failure. N Engl J Med. 2002;347:1397–402. doi: 10.1056/NEJMoa020265. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 12.Mosterd A, Cost B, Hoes AW, de Bruijne MC, Deckers JW, Hofman A, et al. The prognosis of heart failure in the general population: The Rotterdam Study. Eur Heart J. 2001;22:1318–27. doi: 10.1053/euhj.2000.2533. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 13.Gomez-Soto FM, Andrey JL, Garcia-Egido AA, Escobar MA, Romero SP, Garcia-Arjona R, et al. Incidence and mortality of heart failure: a commu-nity-based study. Int J Cardiol. 2011;151:40–5. doi: 10.1016/j.ijcard.2010.04.055. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 14.Mehta PA, Dubrey SW, McIntyre HF, Walker DM, Hardman SM, Sutton GC, et al. Improving survival in the 6 months after diagnosis of heart fail-ure in the past decade: population-based data from the UK. Heart. 2009;95:1851–6. doi: 10.1136/hrt.2008.156034. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 15.Laribi S, Aouba A, Nikolaou M, Lassus J, Cohen-Solal A, Plaisance P, et al. Trends in death attributed to heart failure over the past two decades in Europe. Eur J Heart Fail. 2012;14:234–9. doi: 10.1093/eurjhf/hfr182. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 16.Feinglass J, Martin GJ, Lin E, Johnson MR, Gheorghiade M. Is heart fail-ure survival improving? Evidence from 2323 elderly patients hospitalized between 1989-2000. Am Heart J. 2003;146:111–4. doi: 10.1016/S0002-8703(03)00116-9. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 17.Roger VL, Weston SA, Redfield MM, Hellermann-Homan JP, Killian J, Yawn BP, et al. Trends in heart failure incidence and survival in a commu-nity-based population. JAMA. 2004;292:344–50. doi: 10.1001/jama.292.3.344. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 18.Barker WH, Mullooly JP, Getchell W. Changing incidence and survival for heart failure in a well-defined older population 1970-1974 and 1990-1994. Circulation. 2006;113:799–805. doi: 10.1161/CIRCULATIONAHA.104.492033. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 19.Reitsma JB, Mosterd A, de Craen AJ, Koster RW, van Capelle FJ, Grobbee DE, et al. Increase in hospital admission rates for heart failure in The Netherlands 1980-1993. Heart. 1996;76:388–92. doi: 10.1136/hrt.76.5.388. [CrossRef] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shahar E, Lee S. Historical trends in survival of hospitalized heart failure patients 2000 versus 1995. BMC Cardiovasc Disord. 2007;7:2. doi: 10.1186/1471-2261-7-2. [CrossRef] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fang J, Mensah GA, Croft JB, Keenan NL. Heart failure-related hospitalization in the U.S. 1979 to 2004. J Am Coll Cardiol. 2008;52:428–34. doi: 10.1016/j.jacc.2008.03.061. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 22.Blecker S, Paul M, Taksler G, Ogedegbe G, Katz S. Heart failure–associ-ated hospitalizations in the United States. J Am Coll Cardiol. 2013;61:1259–67. doi: 10.1016/j.jacc.2012.12.038. [CrossRef] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bueno H, Ross JS, Wang Y, Chen J, Vidán MT, Normand SL, et al. Trends in length of stay and short-term outcomes among medicare patients hospital-ized for heart failure: 1993-2008. JAMA. 2010;303:2141–7. doi: 10.1001/jama.2010.748. [CrossRef] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Blackledge HM, Tomlinson J, Squire IB. Prognosis for patients newly admitted to hospital with heart failure: survival trends in 12 220 index admissions in Leicestershire 1993-2001. Heart. 2003;89:615–20. doi: 10.1136/heart.89.6.615. [CrossRef] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schaufelberger M, Swedberg K, Köster M, Rosén M, Rosengren A. Decreasing one-year mortality and hospitalization rates for heart failure in Sweden;Data from the Swedish Hospital Discharge Registry 1988 to 2000. Eur Heart J. 2004;25:300–7. doi: 10.1016/j.ehj.2003.12.012. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 26.Kosiborod M, Lichtman JH, Heidenreich PA, Normand SL, Wang Y, Brass LM, et al. National trends in outcomes among elderly patients with heart failure. Am J Med. 2006;119:616–7. doi: 10.1016/j.amjmed.2005.11.019. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 27.Lee DS, Gona P, Albano I, Larson MG, Benjamin EJ, Levy D, et al. A systematic assessment of causes of death after heart failure onset in the community: impact of age at death, time period, and left ventricular systolic dysfunction. Circ Heart Fail. 2011;4:36–43. doi: 10.1161/CIRCHEARTFAILURE.110.957480. [CrossRef] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Saczynski JS, Darling CE, Spencer FA, Lessard D, Gore JM, Goldberg RJ. Clinical features, treatment practices, and hospital and long-term outcomes of older patients hospitalized with decompensated heart failure: The Worcester Heart Failure Study. J Am Geriatr Soc. 2009;57:1587–94. doi: 10.1111/j.1532-5415.2009.02407.x. [CrossRef] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wong CM, Hawkins NM, Jhund PS, MacDonald MR, Solomon SD, Granger CB, et al. Clinical characteristics and outcomes of young and very young adults with heart failure: The CHARM programme (Candesartan in Heart Failure Assessment of Reduction in Mortality and Morbidity) J Am Coll Cardiol. 2013;62:1845–54. doi: 10.1016/j.jacc.2013.05.072. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 30.Rodriguez F, Wang Y, Johnson CE, Foody JM. National patterns of heart failure hospitalizations and mortality by sex and age. J Card Fail. 2013;19:542–9. doi: 10.1016/j.cardfail.2013.05.016. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 31.Parashar S, Katz R, Smith NL, Arnold AM, Vaccarino V, Wenger NK, et al. Race, gender, and mortality in adults >or =65 years of age with incident heart failure (from the Cardiovascular Health Study) Am J Cardiol. 2009;103:1120–7. doi: 10.1016/j.amjcard.2008.12.043. [CrossRef] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rathore SS, Foody JM, Wang Y, Herrin J, Masoudi FA, Havranek EP, et al. Sex, quality of care, and outcomes of elderly patients hospitalized with heart failure: findings from the National Heart Failure Project. Am Heart J. 2005;149:121–8. doi: 10.1016/j.ahj.2004.06.008. [CrossRef] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Vaartjes I, Hoes AW, Reitsma JB, de Bruin A, Grobbee DE, Mosterd A, et al. Age- and gender-specific risk of death after first hospitalization for heart failure. BMC Public Health. 2010;10:637. doi: 10.1186/1471-2458-10-637. [CrossRef] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jiménez-Navarro MF, Ramirez-Marrero MA, Anguita-Sánchez M, Castillo JC. Influence of gender on long-term prognosis of patients with chronic heart failure seen in heart failure clinics. Clin Cardiol. 2010;33:13–8. doi: 10.1002/clc.20476. [CrossRef] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sakata Y, Miyata S, Nochioka K, Miura M, Takada T, Tadaki S, et al. Gender differences in clinical characteristics, treatment and long-term outcome in patients with stage C/D heart failure in Japan. Report from the CHART-2 study. Circ J. 2014;78:428–35. doi: 10.1253/circj.cj-13-1009. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 36.Loehr LR, Rosamond WD, Chang PP, Folsom AR, Chambless LE. Heart failure incidence and survival (from the Atherosclerosis Risk in Communities study) Am J Cardiol. 2008;101:1016–22. doi: 10.1016/j.amjcard.2007.11.061. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 37.Gottdiener JS, McClelland RL, Marshall R, Shemanski L, Furberg CD, Kitzman DW, et al. Outcome of congestive heart failure in elderly persons: influence of left ventricular systolic function. The Cardiovascular Health Study. Ann Intern Med. 2002;137:631–9. doi: 10.7326/0003-4819-137-8-200210150-00006. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 38.Smith GL, Masoudi FA, Vaccarino V, Radford MJ, Krumholz HM. Outcomes in heart failure patients with preserved ejection fraction: mortality, readmission, and functional decline. J Am Coll Cardiol. 2003;41:1510–8. doi: 10.1016/s0735-1097(03)00185-2. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 39.Cohn JN, Johnson G. Heart failure with normal ejection fraction. The V-HeFT Study. Veterans Administration Cooperative Study Group. Circulation. 1990;81:48–53. [PubMed] [Google Scholar]
- 40.Tribouilloy C, Rusinaru D, Leborgne L, Mahjoub H, Szymanski C, Houpe D, et al. In-hospital mortality and prognostic factors in patients admitted for new-onset heart failure with preserved or reduced ejection fraction: a prospec-tive observational study. Arch Cardiovasc Dis. 2008;101:226–34. doi: 10.1016/s1875-2136(08)73697-0. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 41.Somaratne JB, Berry C, McMurray JJ, Poppe KK, Doughty RN, Whalley GA. The prognostic significance of heart failure with preserved left ven-tricular ejection fraction: a literature-based meta-analysis. Eur J Heart Fail. 2009;11:855–62. doi: 10.1093/eurjhf/hfp103. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 42.Kerzner R, Gage BF, Freedland KE, Rich MW. Predictors of mortality in younger and older patients with heart failure and preserved or reduced left ventricular ejection fraction. Am Heart J. 2003;146:286–90. doi: 10.1016/S0002-8703(03)00151-0. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 43.Bursi F, Weston SA, Redfield MM, Jacobsen SJ, Pakhomov S, Nkomo VT, et al. Systolic and diastolic heart failure in the community. JAMA. 2006;296:2209–16. doi: 10.1001/jama.296.18.2209. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 44.Bhatia RS, Tu JV, Lee DS, Austin PC, Fang J, Haouzi A, et al. Outcome of heart failure with preserved ejection fraction in a population-based study. N Engl J Med. 2006;355:260–9. doi: 10.1056/NEJMoa051530. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 45.Quiroz R, Doros G, Shaw P, Liang CS, Gauthier DF, Sam F. Comparison of characteristics and outcomes of patients with heart failure preserved ejection fraction versus reduced left ventricular ejection fraction in an urban cohort. Am J Cardiol. 2014;113:691–6. doi: 10.1016/j.amjcard.2013.11.014. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 46.Tarantini L, Faggiano P, Senni M, Lucci D, Bertoli D, Porcu M, et al. Clinical features and prognosis associated with a preserved left ventricular systolic function in a large cohort of congestive heart failure outpatients managed by cardiologists. Data from the Italian Network on Congestive Heart Failure. Ital Heart J. 2002;3:656–64. [PubMed] [Google Scholar]
- 47.Curtis JP, Sokol SI, Wang Y, Rathore SS, Ko DT, Jadbabaie F, et al. The association of left ventricular ejection fraction, mortality, and cause of death in stable outpatients with heart failure. J Am Coll Cardiol. 2003;42:736–42. doi: 10.1016/s0735-1097(03)00789-7. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 48.Redfield MM, Jacobsen SJ, Burnett JC, Jr, Mahoney DW, Bailey KR, Rodeheffer RJ. Burden of systolic and diastolic ventricular dysfunction in the community: appreciating the scope of the heart failure epidemic. JAMA. 2003;289:194–202. doi: 10.1001/jama.289.2.194. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 49.Henkel DM, Redfield MM, Weston SA, Gerber Y, Roger VL. Death in heart failure: a community perspective. Circ Heart Fail. 2008;1:91–7. doi: 10.1161/CIRCHEARTFAILURE.107.743146. [CrossRef] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hamaguchi S, Kinugawa S, Sobirin MA, Goto D, Tsuchihashi-Makaya M, Yamada S, et al. Mode of death in patients with heart failure and reduced vs. preserved ejection fraction: report from the registry of hospitalized heart failure patients. Circ J. 2012;76:1662–9. doi: 10.1253/circj.cj-11-1355. [CrossRef] [DOI] [PubMed] [Google Scholar]


