Introduction
Cannabis/cannabinoid and bonsai, which is a synthetic derivative of cannabis, are ever increasing public health problems, particularly in adolescents and young adults. Cannabis and its synthetic derivatives have cardiovascular side effects, including myocardial infarction (1, 2). We hereby reported a case of sudden cardiac arrest due to ST elevation myocardial infarction (MI) developing after 45 minutes of bonsai use that was treated with primary percutaneous coronary intervention after successful cardiopulmonary resuscitation (CPR).
Case Report
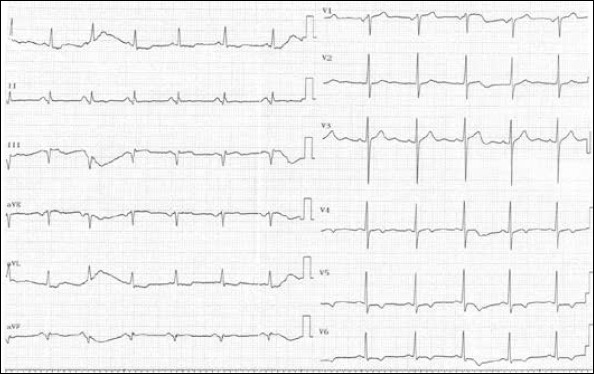
A 31-year-old male patient without any known atherosclerotic risk factor was taken to our emergency department (ED) owing to sudden cardiac arrest that developed during assessment by a 112 doctor who was called due to syncope after 45 minutes of bonsai use. The patient was intubated, and there was no spontaneous respiration, with a blood pressure of 100/70 mm Hg, when the patient was brought to ED. The electrocardiogram (ECG) denoted sinus rhythm and ST elevation in the inferior leads (Fig. 1). The patient’s history, taken from his family, revealed bonsai use merely 2 to 3 times a week. The patient was taken to the angiography laboratory after administration of 300 mg of acetylsalicylic acid and 600 mg of clopidogrel via nasogastric catheter while being intubated. The patient was defibrillated twice by virtue of ventricular fibrillation just before a diagnostic coronary angiography. The left anterior descending artery and circumflex artery were completely normal (Fig. 2), while the right coronary angiography demonstrated a 90% thrombosed lesion in the middle segment (Fig. 3). Bare metal stents of 3.0 x 18 mm and 3.0 x 9 mm were implanted into the right coronary artery (Fig. 4). Unfractionated heparin of 7000 units was administered, and tirofiban loading and infusion were applied on account of thrombus burden. ST-segment resolution was seen on the ECG after coronary intervention (Fig. 5). Fibrinogen and homocysteine levels and antithrombin activity were all in the normal range. No factor V Leiden or prothrombin 20210 gene mutation was ascertained. The patient was extubated on the third day of hospitalization. The patient was evaluated by neurology and psychiatry clinics and assigned to the neurology department due to organic mental disorder secondary to hypoxia that developed during cardiac arrest.
Figure 1.
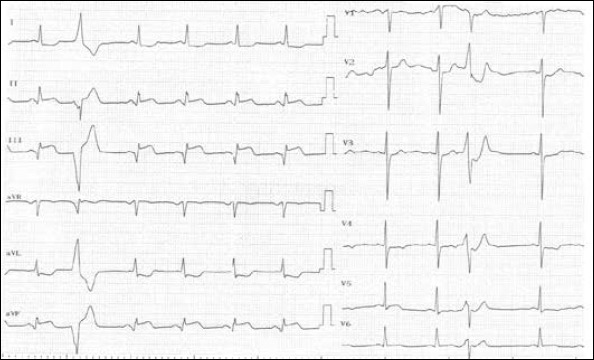
ST elevation in inferior leads on 12-derivation ECG obtained in the emergency department
Figure 2.
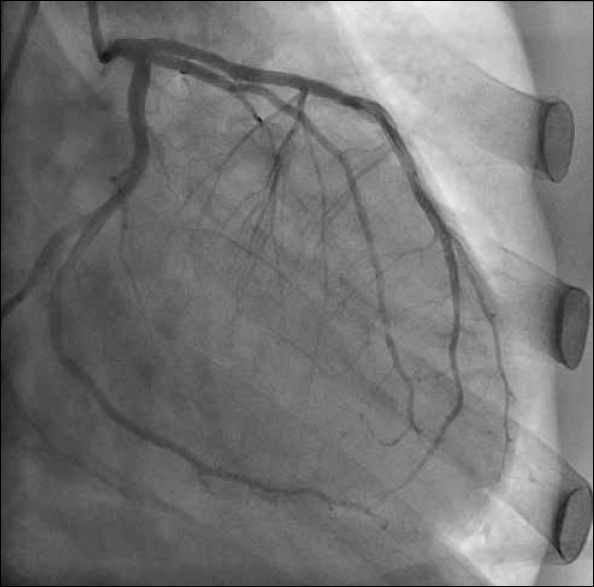
Angiographies demonstrating LMCA, LAD, and Cx in the right anterior oblique position
Figure 3.
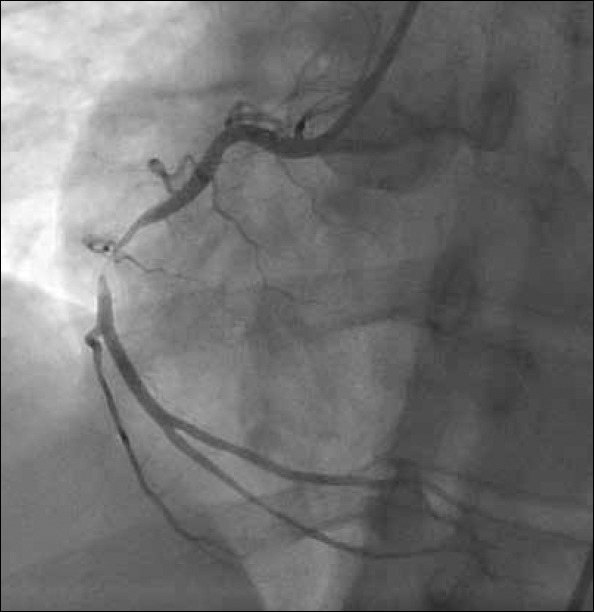
Thrombotic stenosis in mid-RCA in the left anterior oblique position
Figure 4.
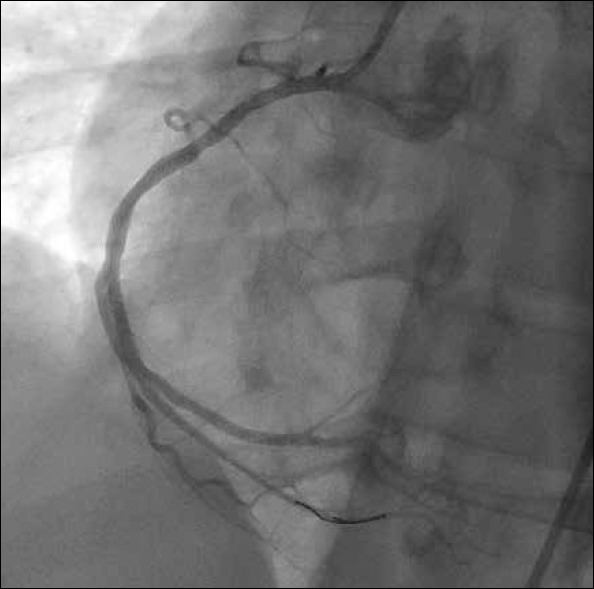
RCA angiography after primary percutaneous coronary intervention in the left anterior oblique position
Figure 5.
ST-segment resolution after primary percutaneous coronary intervention
Discussion
Cannabinoid, the active ingredient of which is tetrahydrocannabinol, is used all over the world for exhilaration. Bonsai, a synthetic derivative of cannabis, is used by young adults and even adolescents increasingly on account of the fact that it is cheaper and easily accessible. Moreover, some addicts consider that it is a natural herb, and they are not conscious of its deleterious impacts and its addictiveness, which again enhances its usage.
Cannabinoids have significant adverse effects on the cardiovascular system. The acute effect of cannabis is sympathetic hyperactivation, leading to heart rate increase and hypertension (3-5) in the supine position and postural hypotension, albeit bradycardia and hypotension might be seen on long-term use (6). Furthermore, cannabinoids may diminish the capacity of erythrocytes to carry oxygen by means of an increase in carboxyhemoglobin levels. A decrease in effort capacity and chest pain may develop when these effects are combined with an increase in heart rate and cardiac output. However, sedation after cannabis use might mask the symptoms, particularly chest pain, regarding acute coronary syndrome (ACS). Mittleman et al. (7) stated that there is a 5-fold greater increase in MI risk after 1 hour of cannabis use. Our case had symptoms within 1 hour of bonsai use, and bonsai was the supposed agent to cause ACS by virtue of the absence of cardiovascular risk factors.
Cannabinoids exert their effect via cannabinoid receptors 1 and 2. The affinity of synthetic cannabinoids to cannabinoid receptors, clinical impacts, addictiveness, and adverse effects are more prevalent than non-synthetic cannabinoids (8).
Conclusion
Bonsai, a synthetic derivative of cannabis, might cause acute myocardial infarction. Illegal drug abuse should be queried in patients without cardiovascular risk factors who present with MI or cardiac arrest.
The exact mechanism of MI owing to cannabis is not well known. Enhanced platelet aggregation and increased factor VII levels due to cannabis were reported in various articles (8). Moreover, cannabis may result in vasospasm and slow flow in the coronary arteries, particularly in atherosclerotic segments (3). However, atherosclerotic lesions were not ascertained in most patients with ACS and cannabis use (9). This finding may demonstrate that vasoconstriction and endothelial dysfunction might contribute to the pathophysiology of cannabis-induced MI.
References
- 1.Canga Y, Osmonov D, Karataş MB, Durmuş G, İlhan E, Kırbaş V. Cannabis: a rare trigger of premature myocardial infarction. Anadolu Kardiyol Derg. 2011;11:272–4. doi: 10.5152/akd.2011.066. [DOI] [PubMed] [Google Scholar]
- 2.Casier I, Vanduynhoven P, Haine S, Vrints C, Jorens PG. Is recent cannabis use associated with acute coronary syndromes?An illustrative case series. Acta Cardiol. 2014;69:131–6. doi: 10.1080/ac.69.2.3017293. [DOI] [PubMed] [Google Scholar]
- 3.Jouanjus E, Lapeyre-Mestre M, Micallef J. Cannabis use: signal of increasing risk of serious cardiovascular disorders. J Am Heart Assoc. 2014;3:e000638. doi: 10.1161/JAHA.113.000638. [CrossRef] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Thomas G, Kloner RA, Rezkalla S. Adverse cardiovascular, cerebrovascular and peripheral vascular effect of marijuana inhalation: what cardiologists need to know?Am J Cardiol. 2014;113:187–90. doi: 10.1016/j.amjcard.2013.09.042. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 5.Menahem S. Cardiac asystole following cannabis (marijuana) usage-additional mechanism for sudden death?Forensic Sci Int. 2013;233:3–5. doi: 10.1016/j.forsciint.2013.10.007. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 6.Hartung B, Kauferstein S, Ritz-Timme S, Daldrup T. Sudden unexpected death under acute influence of cannabis. Forensic Sci Int. 2014;237:11–3. doi: 10.1016/j.forsciint.2014.02.001. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 7.Mittleman MA, Lewis RA, Maclure M, Sherwood JB, Muller JE. Triggering myocardial infarction by marijuana. Circulation. 2001;103:2805–9. doi: 10.1161/01.cir.103.23.2805. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 8.Mach F, Montecucco F, Steffens S. Cannabinoid receptors in acute and chronic complications of atherosclerosis. Br J Pharmacol. 2008;153:290–8. doi: 10.1038/sj.bjp.0707517. [CrossRef] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hodcroft CJ, Rossiter MC, Buch AN. Cannabis associated myocardial infarction in a young man with normal coronary arteries. J Emerg Med. 2014;47:277–81. doi: 10.1016/j.jemermed.2013.11.077. [CrossRef] [DOI] [PubMed] [Google Scholar]


