Abstract
Objective:
The prognostic value of the Global Registry of Acute Coronary Events (GRACE) risk score (GRS) and the Thrombolysis In Myocardial Infarction (TIMI) risk index (TRI) has been reported in coronary artery disease (CAD) patients. We aimed to evaluate the relationship between the GRS, TRI, and severity of CAD evaluated by SYNTAX score (SS) in patients with acute coronary syndrome (ACS).
Methods:
Patients with ACS who were admitted to the coronary care unit of our institution were retrospectively evaluated in this study. A total of 287 patients with ACS [154 non-ST elevated ACS (NSTE-ACS), 133 ST elevated myocardial infarction (STEMI)] were included in the study. The GRS and TRI were calculated on admission using specified variables. The severity of CAD was evaluated using the SS. The patients were divided into low (GRS<109)-, intermediate (GRS 109-140)-, and high (GRS>140)-risk groups and group 1 (TRI<17), group 2 (TRI 17-26), and group 3 (TRI>26) according to GRS and TRI scores. A Pearson correlation analysis was used for the relation between GRS, TRI, and SS.
Results:
Patients with a history of coronary artery bypass surgery, those who had missing data for calculating the GRS and TRI, and those whose systolic blood pressure (SBP) was more than 180 mm Hg or whose diastolic blood pressure (DBP) was more than 110 mm Hg were excluded from the study. Were excluded from the study. There were significant differences in mean age (p<0.001), heart rate (p<0.001), SS (p<0.001), TRI (p<0.001), rate of NSTE-ACS (p<0.001), and STEMI (p<0.001) in all patients between the risk groups. There was a positive significant correlation between the GRS and the SS (r=0.427, p<0.001), but there were no significant correlation between the TRI and SS (r=0.121, p=0.135). The area under the ROC curve value for GRS was 0.65 (95% CI: 0.56-0.74, p=0.001) in the prediction of severity of CAD.
Conclusion:
The GRS is more associated with SS than TRI in predicting the severity of CAD in patients with ACS.
Keywords: acute coronary syndrome, GRACE risk score, SYNTAX score, TIMI risk index
Introduction
Acute coronary syndrome (ACS) is a significant cause of morbidity and mortality in patients with coronary heart disease in developed countries (1). ACS includes non-ST elevated ACS (NSTE-ACS) and ST elevated myocardial infarction (STEMI). Recently, one of the major issues cardiologists have addressed is risk stratification in patients with ACS, in order to identify the severity and complexity of coronary artery disease (CAD). For this purpose, a large number of scoring systems and laboratory parameters have been used in clinical practice. The SYNTAX score (SS) is one of the scoring systems for determining the extent and severity of CAD (2). Although these scoring systems have many advantages, they require an invasive method, such as coronary angiography, to perform the scoring. Therefore, those interested in cardiovascular medicine still need an easily accessible, cost-effective, and noninvasive method to carry out risk stratification by determining the extent and severity of CAD in ACS patients.
In order to identify high-risk patients with ACS, various risk classification systems and scoring systems are quite frequently used (3-8). The prediction of early and late mortality with the GRACE risk score and TIMI risk score has been used for testing populations of hundreds of thousands of patients. Recently, the TIMI risk index (TRI) has been improved and is able to predict mortality, is easier to assess, and can perform scoring with fewer parameters (age, blood pressure, and heart rate, etc.) in patients with NSTE-ACS and patients with STEMI. This index has been shown in many studies to be useful and helpful (9, 10). However, although a number of studies have investigated the relationship between GRS, TRI, and CAD (11, 12), none has addressed the association between GRS, TRI, and the severity of CAD assessed by SS in patients with ACS. Thus, the aim of the current study was to investigate whether high GRS and TRI are associated with the extent and severity of CAD in patients with ACS.
Methods
Study design
Patients with ACS who were admitted to the coronary care unit of our Çanakkale Onsekiz Mart University Faculty of Medicine between April 2012 and August 2013 were retrospectively evaluated in this study.
Study population
Patients with ACS, defined as NSTE-ACS and STEMI. Patients with a history of coronary artery bypass surgery, those who had missing data for calculating the GRS and TRI, and those whose systolic blood pressure (SBP) was more than 180 mm Hg or whose diastolic blood pressure (DBP) was more than 110 mm Hg were excluded from the study. Therefore, a total of 287 patients diagnosed with ACS (154 NSTE-ACS and 133 STEMI) were included in the analysis. The study protocol was approved by the local Ethics Committee of Çanakkale Onsekiz Mart University Faculty of Medicine hospital.
Study protocol
First, the patients were divided into low (GRS <109, n=90)-, intermediate (GRS 109-140, n=104)-, and high (GRS >140, n=93)- risk groups based on the GRS. Second, the study population was divided into tertiles based on TRI values. High [Group 1 (TRI >26, n=94)], moderate [Group 2 (TRI 17-26, n=97)], and low [Group 3 (TRI <17, n=96)] groups were defined as patients having values in the third, second, and first tertiles. The GRS and TRI were calculated on admission using specified variables.
Study variables
The diagnosis of ACS was based on the criteria of the Joint European Society of Cardiology/American College of Cardiology Foundation/American Heart Association/Word Heart Federation Task definition (13). NSTE-ACS was diagnosed according to the following criteria: typical chest pain and/or electrocardiographic changes without new ST elevation indicating myocardial ischemia with negative or elevated cardiac enzymes. Typical chest pain was evaluated as follows: more than 20 minutes in duration, new-onset angina, and an increase in its frequency and duration or severity. The diagnosis of STEMI was based on typical chest pain and new ST-segment elevation at the J point in ≥2 contiguous leads (≥0.2 mV in V1 through V3 and ≥ 0.1 mV in other leads). (According to the new definition; the J point is used to determine the magnitude of the ST-segment shift. New, or presumed new, J point elevation 0.1mV is required in all leads other than V2 and V3.) Demographic information, cardiovascular history, and risk factors [i.e., smoking, hypertension (HT), and diabetes mellitus (DM)] were obtained from the patients’ medical records. Patients who had been treated with antihypertensive drugs or those whose baseline blood pressure exceeded 140/90 mm Hg were diagnosed with HT (14). Patients with DM were defined as being prediagnosed and/or being antidiabetic medications or newly diagnosed if fasting plasma glucose was ≥126 mg/dL or blood glucose was ≥200 mg/dL at any time (15).
Calculation of the GRACE risk score and the TIMI risk index
For each patient, GRS (for death in hospital GRS) was calculated by using specific variables (age, heart rate, SBP, creatinine, Killip class, cardiac arrest at admission, elevated cardiac markers, and ST-segment deviation) collected at admission. The TRI of patients was calculated by the formula “heart rate X (age÷10)2÷SBP”
Analysis of blood samples and echocardiography
CBCs and biochemical values were retrospectively evaluated from blood samples obtained by antecubital vein puncture upon admission to the emergency department. The hemogram parameters and other biochemical measurements were determined using standard biochemical techniques with the Beckman Coulter LH 780 (Beckman Coulter Ireland Inc. Mervue, Galway, Ireland) device in the hematology laboratory of our institution. Simpson’s method was used to assess left ventricular ejection fraction (LVEF), as recommended by the American Society of Echocardiography (16), by using a machine (Vivid 7®, GE Vingmed Ultrasound A/S, Horten, Norway) with a 3.5-MHz transducer for all patients.
Coronary angiography and SYNTAX score
All patients underwent a coronary angiography by using a machine (GE Healthcare Innova 2100, New Jersey, USA) by the femoral approach using the standard Judkins technique. Iopromide as a contrast agent (Ultravist-370, Bayer Schering Pharma, Germany) and a 6 F diagnostic catheter were used in all subjects. The extent and severity of CAD were assessed by the SS (17). All angiographic variables pertinent to the SS calculation were computed by 2 of 3 experienced cardiologists who were blinded to the current study on the angiograms. In the case of disagreement, an opinion was obtained from the third cardiologist, and the final decision was made by consensus. Occluded infarct-related arteries in patients with AMI were scored as occlusions of less than 3 months in duration. Each coronary lesion with a diameter stenosis of at least 50%, in vessels of at least 1.5 mm, had to be scored. The latest online updated version was used for the calculation of the SYNTAX score (http://www.SYNTAXscore.com).
Statistical analysis
All statistical studies were carried out with the SPSS program (version 17.0, SPSS, Chicago, IL, USA). Quantitative variables were expressed as the mean value±standard deviation, and qualitative variables were expressed as percentages (%). The Kolmogorov-Smirnov test was used for normal distribution. A comparison of parametric values between the groups was performed using one-way ANOVA and Tukey test for post hoc analysis for normal distribution. Categorical variables were compared by the likelihood ratio chi-square test. Pearson correlation analysis was used for determining the association between GRS, TRI, and SS. A p value <0.05 was considered statistically significant. The receiver operating characteristics (ROC) curve was used to test the predictive accuracy of risk scores regarding the severity of CAD. A significant prediction occurred when the area under the ROC curve was statistically different from 0.5.
Results
A total of 287 patients [215 females (74.9%), mean age 61.9±12.7 years] were enrolled in this study. There were 154 NSTE-ACS and 133 STEMI patients in our study. Table 1 shows the characteristics of all patients.
Table 1.
The characteristics of all patients
| Parameters | All patients n=287 |
|---|---|
| Age, years | 61.9±12.7 |
| Heart rate, bpm | 75±15 |
| Creatinine, mg/dL | 0.84±0.21 |
| Blood urea nitrogen, mg/dL | 11.9±3.6 |
| Systolic blood pressure, mm Hg | 138±26 |
| Diastolic blood pressure, mm Hg | 87±16 |
| Body mass index, kg/m2 | 25.4±5.4 |
| Ejection fraction, % | 48±9 |
| Female, % (n) | 74.9 (215) |
| Smoking, % (n) | 31.7 (91) |
| GRS | 124.3±35.2 |
| TRI | 22.5±10.4 |
| SYNTAX score | 13.4±7.9 |
| Diabetes mellitus, % (n) | 40.1 (115) |
| Hypertension, % (n) | 45.3 (130) |
| Type of ACS, % (n) | |
| Non-ST elevated ACS | 53.7 (154) |
| ST elevated ACS | 46.3 (133) |
| Culprit lesion, % (n) | |
| Left anterior descending | 45.3 (130) |
| Circumflex | 24.4 (70) |
| Right coronary artery | 30.3 (87) |
| Glucose, mg/dL | 157±78 |
| Low-density lipoprotein, mg/dL | 123±36 |
| High-density lipoprotein, mg/dL | 42.5±14.2 |
| Triglyceride, mg/dL | 140±59 |
| Hemoglobin, g/dL | 13.3±1.9 |
| Neutrophil, 103/mm3 | 8.4±3.9 |
| Lymphocyte, 103/mm3 | 3.9±3.3 |
| Neutrophil-lymphocyte ratio | 3.2±2.3 |
| High-sensitivity troponin-T, ng/L | 592±1086 |
ACS - acute coronary syndrome; bpm - beat per minute; GRS - Grace risk score; TRI - TIMI risk index
There were significant differences regarding mean age (p<0.001), heart rate (p<0.001), SS (p<0.001), TRI (p<0.001), rate of NSTE-ACS (p<0.001), and STEMI (p<0.001) in all patients between the low-, intermediate-, and high-risk groups (Table 2). The rates of females (p=0.021) and admission level of glucose (p=0.044) were significantly higher and the level of hemoglobin (p=0.028) and the rate of circumflex lesion (p=0.001) were significantly lower in the high-risk patients compared to the low-risk patients. The neutrophil-to-lymphocyte ratio (NLR) (p=0.016) was significantly higher in the high-risk patients compared to the intermediate-risk patients (Table 2).
Table 2.
The baseline characteristics and laboratory findings of patients with low, intermediate, and high GRS
| Variable | Low GRS (n=90) | Intermediate GRS (n=104) | High GRS (n=93) | P |
|---|---|---|---|---|
| Age, years | 52±10a,b | 63± 10b,c | 70±10a,c | <0.001 |
| Heart rate, bpm | 70±13a,b | 76±14b | 80±16a | <0.001 |
| Creatinine, mg/dL | 0.8±0.2 | 0.9±0.2 | 0.8±0.2 | 0.166 |
| BUN, mg/dL | 12±3.7 | 11.8±3.7 | 11.8±3.4 | 0.928 |
| Systolic BP, mm Hg | 141±26 | 137±26 | 135±25 | 0.358 |
| Diastolic BP, mm Hg | 90±16 | 87±16 | 86±16 | 0.248 |
| Body mass index, kg/m2 | 25.5±5.5 | 25.3±5.4 | 25.4±5.3 | 0.968 |
| Left ventricle EF, % | 46.7±8.9 | 47.5±10.5 | 49.6±9.6 | 0.127 |
| Female, % (n) | 15.6 (14)a | 26 (27) | 33.3 (31)a | 0.021 |
| Smoking, % (n) | 27.8 (25) | 32.7 (34) | 34.4 (32) | 0.606 |
| GRS | 84.4±19.8a,b | 124.3±8.8b,c | 162.8±18.5a,c | <0.001 |
| TRI | 14.1±5.9a,b | 22.8±8.1b,c | 30.3±10.1a,c | <0.001 |
| SYNTAX score | 9.9±8.3a,b | 12.6±6.9b,c | 17.9±6.7a,c | <0.001 |
| Diabetes mellitus, % (n) | 31.1 (28) | 40.4 (42) | 48.4 (45) | 0.058 |
| Hypertension, % (n) | 52.2 (47) | 44.2 (46) | 39.8 (37) | 0.231 |
| Type of ACS, % (n) | 0.001 | |||
| NSTE-ACS | 80 (72)a,c | 52.9 (55)b,c | 29 (27)a,c | |
| STE-ACS | 20 (18)a,c | 47.1 (49)b,c | 71 (66)a,c | |
| Culprit lesion, % (n) | ||||
| LAD | 37.8 (34) | 49 (51) | 48.4 (45) | 0.223 |
| Cx | 40 (36)a | 23.1 (24) | 17.2 (16)a | 0.001 |
| RCA | 25.6 (23) | 30.8 (32) | 34.4 (32) | 0.425 |
| Glucose, mg/dL | 145±77a | 153±73 | 172±81a | 0.044 |
| LDL, mg/dL | 128.1±33.3 | 123.1±37.7 | 118.4±36.4 | 0.190 |
| HDL, mg/dL | 40.3±12.1 | 43±12.4 | 44±17.5 | 0.199 |
| Triglyceride, mg/dL | 151.4±70.4 | 135.6±54.2 | 133.8±52.1 | 0.086 |
| Hemoglobin, g/dL | 13.7±1.8a | 13.4±2.1 | 12.9±1.8a | 0.028 |
| Neutrophil, 103/mm3 | 8.3±3.9 | 8.2±3.6 | 8.8±4.3 | 0.507 |
| Lymphocyte, 103/mm3 | 4.1±3.6 | 4±3.2 | 3.6±3.2 | 0.557 |
| NLR | 3±2.4 | 2.8±1.8° | 3.7±2.7c | 0.016 |
| hs-TnT, ng/L | 625±1099 | 488±893 | 676±1259 | 0.451 |
P<0.05 between the low and high GRS groups,
P<0.05 between the low and intermediate GRS groups,
P<0.05 between the intermediate and high GRS groups, ACS - acute coronary syndrome; BP - blood pressure; bpm - beats per minute; BUN - blood urea nitrogen; Cx - circumflex; EF - ejection fraction; GRS - Grace risk score; HDL - high-density lipoprotein; Hs-TnT - high-sensitivity troponin-T; LAD - left anterior descending; LDL - low-density lipoprotein; NLR - neutrophil-lymphocyte ratio; NSTE-ACS - non-ST elevated acute coronary syndrome; RCA - right coronary artery; STEMI - ST elevation myocardial infarction; TRI - TIMI risk index
one-way ANOVA and chi-square test
There were significant differences regarding mean age (p<0.001), heart rate (p<0.001), rate of females (p<0.001), and GRS (p<0.001) in all patients between groups according to TRI (Table 3). SBP and DBP were significantly higher in patient group 1 compared to patient groups 2 and 3 (p<0.001), and triglycerides were significantly higher in patient group 1 compared to patient group 3 (p=0.039). There were no statistically significant differences between the SS and TRI in the study groups (p=0.686) (Table 3).
Table 3.
The baseline characteristics and laboratory findings of patient groups according to TRI
| Variable | Group 1 (n=96) | Group 2 (n=97) | Group 3 (n=94) | P |
|---|---|---|---|---|
| Age, years | 50±9a,b | 63±8b,c | 73±10a,c | <0.001 |
| Heart rate, bpm | 68±12a,b | 74±12b,c | 85±16a,c | <0.001 |
| Creatinine, mg/dL | 0.8±0.2 | 0.8±0.2 | 0.9±0.2 | 0.189 |
| BUN, mg/dL | 11.5±3.7 | 12.2±3.8 | 11.8±3.2 | 0.367 |
| Systolic BP, mm Hg | 145±25a | 138±26 | 130±24a | <0.001 |
| Diastolic BP, mm Hg | 93±15a,b | 87±16b | 83±15a | <0.001 |
| Body mass index, kg/m2 | 25.6±5.5 | 24.9±5.3 | 25.8±5.3 | 0.451 |
| Left ventricle EF, % | 47.3±9.9 | 47.7±9 | 48.9±10.3 | 0.508 |
| Female, % (n) | 12.5 (12)a,b | 25.8 (25)b,c | 37.2 (35)a,c | <0.001 |
| Smoking, % (n) | 30.2 (29) | 34 (33) | 30.9 (29) | 0.831 |
| GRS | 98.6±34.5a,b | 123.4±22.1b,c | 151.3±26a,c | <0.001 |
| TRI | 11.8±3.2a,b | 21.3±2.7b,c | 34.7±6.9a,c | <0.001 |
| SYNTAX score | 13.1±9 | 13.2±7.3 | 14±7.5a,c | 0.686 |
| Diabetes mellitus, % (n) | 32.3 (31) | 41.2 (40) | 46.8 (44) | 0.119 |
| Hypertension, % (n) | 54.2 (52)a | 49.5 (48)c | 31.9 (30)a,c | 0.005 |
| Type of ACS, % (n) | 0.804 | |||
| NSTE-ACS | 51 (49) | 55.7 (54) | 54.3 (51) | |
| STE-ACS | 49 (47) | 44.3 (43) | 45.7 (43) | |
| Culprit lesion, % (n) | ||||
| LAD | 41.7 (40) | 46.4 (45) | 47.9 (45) | 0.667 |
| Cx | 32.3 (31) | 22.7 (22) | 24.5 (23) | 0.275 |
| RCA | 27.1 (26) | 35.1 (34) | 28.7 (27) | 0.445 |
| Glucose, mg/dL | 145±70 | 159±77 | 166±85 | 0.171 |
| LDL, mg/dL | 126.9±35.1 | 124.9±39.2 | 117.5±33.2 | 0.170 |
| HDL, mg/dL | 40±9.8 | 43.5±15.7 | 43.9±16.1 | 0.120 |
| Triglyceride, mg/dL | 148.6±66.7a | 143.4±61.3 | 127.5±47a | 0.039 |
| Hemoglobin, g/dL | 13.9±1.7a | 13.5±1.9c | 12.6±1.9a,c | <0.001 |
| Neutrophil, 103/mm3 | 9.2±4.3 | 8.1±3.7 | 7.9±3.7 | 0.05 |
| Lymphocyte, 103/mm3 | 4±3.2 | 4.2±3.8 | 3.5±3 | 0.315 |
| NLR | 3.2±2.3 | 2.8±2 | 3.5±2.6 | 0.194 |
| hs-TnT, ng/L | 759±1231 | 543±983 | 471±1017 | 0.163 |
P<0.05 between groups 1 and 3,
P<0.05 between groups 1 and 2,
P<0.05 between groups 2 and 3, ACS - acute coronary syndrome; BP - blood pressure; bpm - beats per minute; BUN - blood urea nitrogen; Cx - circumflex; EF - ejection fraction; GRS - Grace risk score; HDL - high-density lipoprotein; hs-TnT - high-sensitivity troponin-T; LAD - left anterior descending; LDL - low-density lipoprotein; NLR - neutrophil-lymphocyte ratio; NSTE-ACS - non-ST elevated acute coronary syndrome; RCA - right coronary artery; STEMI - ST elevation myocardial infarction; TRI - TIMI risk index one-way ANOVA and chi-square test
In the correlation analysis, there were significant positive correlations between GRS and SS (r=0.423, p<0.001) and between GRS and TRI (r=0.756, p<0.001), but there were no significant correlations between TRI and SS (r=0.121, p=0.135). The relationship between GRS and SS in patients with ACS is shown in Figure 1. The area under the ROC curves for GRS was 0.65 (95% CI: 0.56-0.74, p=0.001) in the prediction of the severity of CAD (SS >22) in patients with ACS (Fig. 2).
Figure 1.
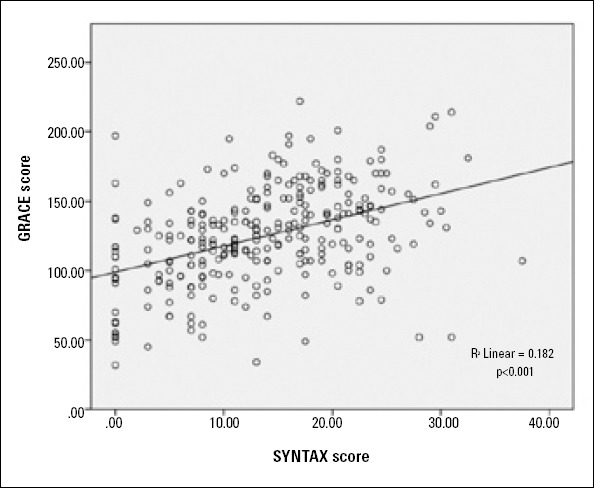
The relationship between GRACE risk score and SYNTAX score in patients with acute coronary
Pearson correlation analysis
Figure 2.
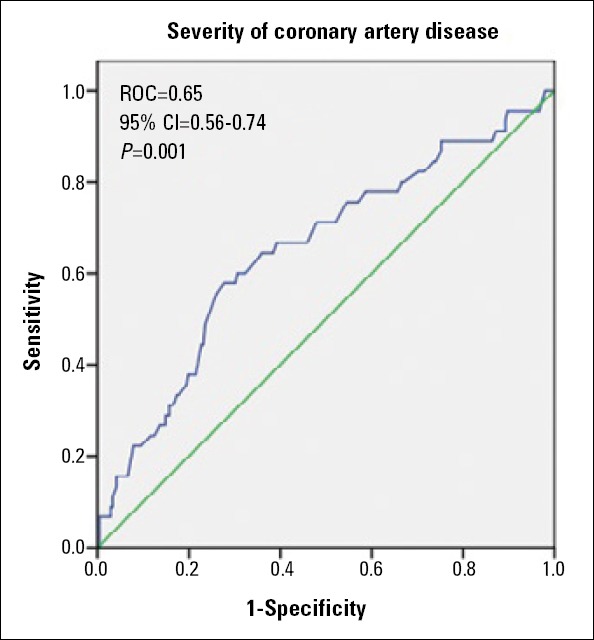
Receiver operating characteristic (ROC) curves for GRACE risk score in the prediction of CAD severity (SYNTAX score >22) in patients with acute coronary syndrome
Discussion
In our study, two important results were obtained. Firstly, in patients with ACS, there was a significant positive correlation between GRS and SS, one of the quantitative indicators of the extent and severity of CAD. Secondly, TRI was not correlated with SS. Because the parameters in TRI are in GRS and because TRI is not correlated with SS, we think that parameters other than age, heart rate, and SBP predict the extent and severity of CAD. In addition, in our study, significant differences in admission glucose levels and NLR between the GRACE risk groups were confirmed by the results of recently conducted studies (18, 19) in large patient groups.
Because GRACE score has been shown to be a predictor of major adverse cardiac events in patients with ACS (20), it is frequently used in clinical practice. GRS includes a variety of clinical, laboratory, and electrocardiographic parameters. Because angiographic findings are not included in these parameters, scoring systems that predict the prognosis and also the prevalence and severity of CAD, such as SS, have begun to be used in the clinic to contribute to risk stratification (2).
Undoubtedly, one of the important scoring systems used in risk stratification in patients with ACS is the TIMI risk score, since it has been shown to be useful and helpful in many studies with large patient populations. Also, the relationship between the TIMI risk score and the severity of CAD has been shown in several studies. For example, the TIMI score was compared with the results of coronary angiography in 683 patients with NSTE-ACS. In each increased risk category, 3-vessel disease or left main coronary disease was shown to be more frequent (12). In another study, the PRISM-PLUS study, in 1491 patients with ACS, it was shown that there were more severe coronary lesions and left main coronary lesions in patients with high TIMI risk scores compared to those with low TIMI risk scores (21). These results were confirmed in the retrospective study of Ben Salem et al. (22). Also, in another study, the relationship between GRS, TIMI risk score, and Gensini score was investigated in patients with NSTE-ACS, and a positive significant correlation was observed between GRS and Gensini score, but it has been shown that this significance was not sufficient for GRS to predict obstructive CAD (23).
As a result of these studies conducted with the GRACE and TIMI risk score, SBP, heart rate, and age were found to be three major important parameters predicting mortality. Therefore, Morrow et al. (24) showed that TRI, an index consisting of these three parameters, can be used in the risk assessment of patients with ACS. In another study, Truong et al. (25) showed that TRI predicts long-term mortality and heart failure in patients with STEMI. Ilkhanoff et al. (26) and Bradshaw et al. (10) showed that TRI predicts short- and long-term mortality in patients with ACS (NSTE-ACS and STEMI).
Our study is important, because it is the first study in the literature in which GRS and TRI and their relationship with SS were evaluated in the same patient population. In this study, we think that with the help of the calculated GRS of patients who are admitted to the emergency department with ACS, information about the short-and long-term mortality of patients and information about the severity and extent of CAD may be obtained.
Study limitations
Our study has some limitations. Firstly, this was a retrospective study based on a relatively small number of patients, and the study population was from a single center. Secondly, the method of measuring SBP, which is one of the GRS and TRI parameters, was by arterial blood pressure. This method is non-invasive, and the evaluation of interobserver variability is important for accurate and clear results. However, this evaluation could not be done in our study, since our study was retrospective. Third, because there was a predominance of female patients in our study, the results may not be applicable to a group with a male predominance. Fourth, 109 and 140 values were used for the risk classification of GRS in all patients (STE-ACS and NSTE-ACS). This condition might not be applicable for STEMI patients.
Conclusion
The GRS is associated more with SS than TRI in predicting the extent and severity of the CAD in patients with ACS. The GRS is using simple and inexpensive methods for evaluating patients with ACS. In addition, high GRS may be helpful in identifying high-risk patients and determining appropriate treatment strategies.
Footnotes
Conflict of interest: None declared.
Peer-review: Externally peer-reviewed.
Authorship contributions: Concept - A.B., B.A., E.G.; Design - A.B., B.A., E.G.; Supervision - A.B., A.T., A.Barutçu.; Resource - A.T., A. Barutçu.; Materials - M.T.A.Ö., S.Ö.; Data collection &/or processing - S.Ö., B.K.; Analysis &/or interpretation - M.T.A.Ö., B.K.; Literature search - Ö.G., S.G.; Writing - A.B., E.G.; Critical review - Ö.G., S.G.
References
- 1.European Heart Network. European cardiovascular disease statistics. 2008 edition. 2008. [accessed 21 August 2012]. Available at: http:/www.ehnheart.org/cvd-statistics.html .
- 2.Sianos G, Morel MA, Kappetein AP, Morice MC, Colombo A, Dawkins K, et al. The SYNTAX Score: an angiographic tool grading the complexity of coronary artery disease. Euro Intervention. 2005;1:219–27. [PubMed] [Google Scholar]
- 3.Braunwald E, Antman EM, Beasley JW, Califf RM, Cheitlin MD, Hochman JS, et al. ACC/AHA 2002 guideline update for the management of patients with unstable angina and non-ST-segment elevation myocardial infarction-summary article: a report of the American College of Cardiology/American Heart Association task force on practice guidelines (Committee on the Management of Patients With Unstable Angina) J Am Coll Cardiol. 2002;40:1366–74. doi: 10.1016/s0735-1097(02)02336-7. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 4.Sabatine MS, Antman EM. The thrombolysis in myocardial infarction risk score in unstable angina pectoris/non-ST-segment elevation myocardial infarction. J Am Coll Cardiol. 2003;41:89S–95S. doi: 10.1016/s0735-1097(02)03019-x. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 5.Simoons ML GUSTO IV-ACS Investigators. Effect of glycoprotein 2b/3a receptor blocker abciximab on outcome in patients with acute coronary syndromes without early coronary revascularization: The GUSTO 4-ACS randomised trial. Lancet. 2001;357:1915–24. doi: 10.1016/s0140-6736(00)05060-1. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 6.Boersma E, Pieper KS, Steyerberg EW, Wilcox RG, Chang WC, Lee KL, et al. Predictors of outcome in patients with acute coronary syndromes without persistent ST-segment elevation. Results from an international trial of 9461 patients. The PURSUITS Investigators. Circulation. 2000;101:2557–67. doi: 10.1161/01.cir.101.22.2557. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 7.de Araújo Gonçalves P, Ferreira J, Aguiar C, Seabra-Gomes R. TIMI, PURSUIT and GRACE risk scores: sustained prognostic value and interaction with revascularization in NSTE-ACS. Eur Heart J. 2005;26:865–72. doi: 10.1093/eurheartj/ehi187. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 8.Granger CB, Goldberg RJ, Dabbous O, Pieper KS, Eagle KA, Cannon CİP, et al. Predictors of hospital mortality in the global registry of acute coronary events. Arch Intern Med. 2003;163:2345–53. doi: 10.1001/archinte.163.19.2345. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 9.Wiviott SD, Morrow DA, Frederick PD, Giugliano RF, Gibson CM, Mc Cabe CH, et al. Performance of the thrombolysis in myocardial infarction risk index in the National Registry of Myocardial Infarction-3 and -4: a simple index that predicts mortality in ST-segment elevation myocardial infarction. J Am Coll Cardiol. 2004;44:783–9. doi: 10.1016/j.jacc.2004.05.045. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 10.Bradshaw PJ, Ko DT, Newman AM, Donovan LR, Tu JV. Validation of the Thrombolysis In Myocardial Infarction (TIMI) risk index for predicting early mortality in a population-based cohort of STEMI and non-STEMI patients. Can J Cardiol. 2007;23:51–6. doi: 10.1016/s0828-282x(07)70213-1. [CrossRef] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Santos ES, Aguiar Filho Lde F, Fonseca DM, Londero HJ, Xavier RM, Pereira MP, et al. Correlation of risk scores with coronary anatomy in non-ST-elevation acute coronary syndrome. Arq Bras Cardiol. 2013;100:511–7. doi: 10.5935/abc.20130088. [DOI] [PubMed] [Google Scholar]
- 12.Garcia S, Canoniero M, Peter A, de Marchena E, Ferreira A. Correlation of TIMI risk score with angiographic severity and extent of coronary artery disease in patients with non-ST-elevation acute coronary syndromes. Am J Cardiol. 2004;93:813–6. doi: 10.1016/j.amjcard.2003.12.015. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 13.Thygesen K, Alpert J S, White HD, Jaffe AS, Apple FS, Galvani M on behalf of the Joint ESC/ACCF/AHA/WHF Task Force for the redefinition of myocardial infarction. Universal definition of myocardial infarction. Circulation. 2007;116:2634–53. doi: 10.1161/CIRCULATIONAHA.107.187397. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 14.James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8) JAMA. 2014;311:507–20. doi: 10.1001/jama.2013.284427. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 15.American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2011;34:62–9. [CrossRef] [Google Scholar]
- 16.Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, et al. Recommendations for chamber quantification. Eur J Echocardiogr. 2006;7:79–108. doi: 10.1016/j.euje.2005.12.014. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 17.SYNTAX Working Group. SYNTAX score calculator. [Accessed 15 January 2011]. Available at: http://www.SYNTAXscore.com .
- 18.Timóteo AT, Papoila AL, Rio P, Miranda F, Ferreira ML, Ferreira RC. Prognostic impact of admission blood glucose for all-cause mortality in patients with acute coronary syndromes: added value on top of GRACE risk score. Eur Heart J Acute Cardiovasc Care. 2014;3:257–63. doi: 10.1177/2048872614528858. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 19.Acet H, Ertaş F, Akıl MA, Özyurtlu F, Polat N, Bilik MZ, et al. Relationship between hematologic indices and Global Registry of Acute Coronary Events Risk Score in Patients With ST-Segment Elevation Myocardial Infarction. Clin Appl Thromb Hemost. 2014 May 8; doi: 10.1177/1076029614533145. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 20.Tang EW, Wong CK, Herbison R. Global Registry of Acute Coronary Events (GRACE) hospital discharge risk score accurately predicts long-term mortality post acute coronary syndrome. Am Heart J. 2007;153:29–35. doi: 10.1016/j.ahj.2006.10.004. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 21.Mega JL, Morrow DA, Sabatine MS, Zhao XQ, Snapinn SM, DiBattiste PM, et al. Correlation between the TIMI risk score and high-risk angiographic findings in non-ST-elevation acute coronary syndromes: observations from the Platelet Receptor Inhibition in Ischemic Syndrome Management in Patients Limited by Unstable Signs and Symptoms (PRISM-PLUS) trial. Am Heart J. 2005;149:846–50. doi: 10.1016/j.ahj.2004.08.042. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 22.Ben Salem H, Ouali S, Hammas S, Bougmiza I, Gribaa R, Ghannem K, et al. Correlation of TIMI risk score with angiographic extent and severity of coronary artery disease in non-ST-elevation acute coronary syndromes. Ann Cardiol Angeiol (Paris) 2011;60:87–91. doi: 10.1016/j.ancard.2010.12.014. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 23.Barbosa CE, Viana M, Brito M, Sabino M, Garcia G, Maraux M, et al. Accuracy of the GRACE and TIMI scores in predicting the angiographic severity of acute coronary syndrome. Arq Bras Cardiol. 2012;99:818–24. doi: 10.1590/s0066-782x2012005000080. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 24.Morrow DA, Antman EM, Giugliano RR, Cairns R, Charlesworth A, Murphy SA, et al. A simple risk index for rapid initial triage of patients with ST-elevation myocardial infarction: an InTIME II sub-study. Lancet. 2001;358:1571–5. doi: 10.1016/S0140-6736(01)06649-1. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 25.Truong QA, Cannon CR, Zakai NA, Rogers IS, Giugliano RR, Wiviott SD, et al. Thrombolysis in Myocardial Infarction (TIMI) Risk Index predicts long-term mortality and heart failure in patients with ST-elevation myocardial infarction in the TIMI 2 clinical trial. Am Heart J. 2009;157:673–9. doi: 10.1016/j.ahj.2008.12.010. [CrossRef] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ilkhanoff L, O’Donnell CJ, Camargo CA, O’Halloran TD, Giugliano RR, Lloyd-Jones DM. Usefulness of the TIMI risk index in predicting short- and long-term mortality in patients with acute coronary syndromes. Am J Cardiol. 2005;96:773–7. doi: 10.1016/j.amjcard.2005.04.059. [CrossRef] [DOI] [PubMed] [Google Scholar]


