Abstract
Objective:
The ambulatory arterial stiffness index has been proposed as an indicator of arterial stiffness. The aim of this study was to test the hypothesis that increased ambulatory arterial stiffness index might be related with impaired left atrial function in hypertensive diabetic patients with no previous history of cardiovascular disease.
Methods:
Inclusion criteria included office systolic BP> 130 mm Hg or diastolic BP> 80 mm Hg and absence of secondary causes of HT, whereas exclusion criteria LV ejection fraction <50%, history of significant coronary artery disease, chronic renal failure, atrial fibrillation/flutter, second or third-degree atrioventricular block, moderate to severe valvular heart disease, history of cerebrovascular disease, non-dipper hypertensive pattern and sleep apnea. The study was composed of 121 hypertensive diabetic patients. Twenty-four-hour ambulatory blood pressure monitoring and echocardiography were performed in each patient. The relationship between ambulatory arterial stiffness index and left atrial functions was analyzed. AASI was calculated as 1 minus the regression slope of diastolic BP plotted against systolic BP obtained through individual 24-h ABPM.
Results:
The univariate analysis showed that ambulatory arterial stiffness index was positively correlated with age (r=:0.287, p=:0.001), hypertension duration (r=:0.388, p<0.001), fasting plasma glucose (r=:0.224, p=:0.014), HbA1c (r=:0.206, p=:0.023), LDL cholesterol (r=:0.254, p=:0.005), and also overall pulse pressure (r=:0.195, p=:0.002), office-pulse pressure (r=:0.188, p=:0.039), carotid intima-media thickness (r=:0.198, p=:0.029), E/E’ (r=:0.248, p=:0.006), and left atrial volume index (r=:0.237, p=:0.009). Moreover, ambulatory arterial stiffness index was negatively correlated with eGFR (r=:(-) 0.242, p=:0.008), peak left atrial strain during ventricular systole [S-LAs (r=:(-) 0.654, p<0.001)], peak left atrial strain at early diastole [S-LAe (r=:(-)0.215, p=:0.018)], and peak left atrial strain rate during ventricular systole [SR-LAs (r=:(-) 0.607, p<0.001)]. The multiple linear regression analysis showed that ambulatory arterial stiffness index was independently associated with peak left atrial strain rate during ventricular systole (SR-LAs) (p<0.001).
Conclusion:
In hypertensive diabetic patients, increased ambulatory arterial stiffness index is associated with impaired left atrial functions, independent of left ventricular diastolic dysfunction.
Keywords: ambulatory arterial stiffness index, left atrium
Introduction
Recently, the ambulatory arterial stiffness index (AASI) has been proposed as a novel indicator of arterial stiffness (1). It is defined as 1 minus the regression slope of diastolic on systolic blood pressure (BP) values obtained from a 24-h ambulatory blood pressure monitoring (ABPM) recordings (2). So, AASI shows the dynamic relationship between systolic and diastolic BP (3). It is determined by established predictors of arterial stiffness but also by ventriculo-arterial coupling factors (3). Although a strong correlation has been demonstrated between AASI and classic measures of arterial stiffness, such as pulse wave velocity (PWV) and augmentation index (1), AASI has been shown to be a better estimator of central arterial stiffness compared to other classical indicators, such as pulse pressure (PP) (4). Furthermore, it could predict stroke better than PWV (5). Recent studies demonstrated that AASI predicts cardiovascular (CV) mortality and morbidity and stroke, independent of other known risk factors (1).
Arterial stiffness increases in patients with diabetes mellitus (DM) and hypertension (HT), and it has been recognized as a key mediator of CV events (6, 7) and stroke (8). Increased arterial stiffness has an effect on left ventricular (LV) geometry and diastolic dysfunction (8). On the other hand, left atrial (LA) size has been used as a biomarker of chronic LV diastolic dysfunction (9). In addition, studies have shown that the association between arterial stiffness and LA size or function is independent of LV diastolic dysfunction grade-that is, LA-arterial coupling but not LA-LV-arterial coupling (6)-although there are limited data in the current literature.
Although LA functions can be analyzed using conventional echocardiographic methods, recently introduced two-dimensional speckle-tracking echocardiography (2D-STE) allows direct and angle-independent analysis of myocardial deformation and provides a better evaluation of LA functions (10-12). Global LA longitudinal strain has been found as a strong and independent predictor of CV events (including stroke) (13).
LA deformation mechanics are impaired in patients with HT and DM with normal LA size, and the coexistence of both conditions further impairs LA performance in an additive fashion (10). In this study, we investigated the association between AASI and LA functions in hypertensive diabetic patients with no evidence of CV disease with the use of 2D-STE. To our knowledge, this is the first study evaluating this specific topic in the literature.
Methods
Study population
From August 2012 to July 2013, we conducted a single-Ahi Evren Chest and Cardiovascular Surgery Education and Research Hospital, Department of Cardiology, Trabzon, Turkey cross-sectional study including 141 consecutive patients with HT and type-2 DM. All patients were receiving anti-hypertensive and anti-diabetic treatment for at least 1 year. Inclusion criteria included office systolic BP >130 mm Hg or diastolic BP >80 mm Hg and the absence of secondary causes of HT, whereas the exclusion criteria were echocardiographic evidence of either regional or global wall motion abnormalities, LV ejection fraction (LVEF) <50%, history of significant coronary artery disease, angina pectoris, positive treadmill test or nuclear perfusion stress test, ischemic electrocardiographic findings, chronic renal failure, atrial fibrillation/flutter, second- or third-degree atrioventricular block, moderate to severe valvular heart disease, history of cerebrovascular disease, non-dipper hypertensive pattern, and sleep apnea. Twenty patients who were found to be noncompliant with the ABPM measurements and/or had a poor echocardiographic window were also excluded from the study. The remaining 121 patients constituted the study population.
Informed consent was obtained from the patients, and the study was approved by the local Ethics Board. Baseline clinical and demographic information was obtained from all patients. Fasting blood glucose, HbA1c, lipid parameters, and creatinine values were measured. Estimated glomerular filtration rate (eGFR) was calculated by the Modification of Diet in Renal Disease (MDRD) study equation (14). Body mass index (BMI) was calculated as weight (kg)/height (m2). The body surface area was calculated according to the DuBois formula [(weight0.425x height0.725) x 0.007184], and 24-hour ABPM and echocardiography were carried out in all patients.
24-hour ABPM
First, 24-hour ABPM was performed using an Agilis-CD-ABPM (ELA Medical, France, 2002) device (15), a non-invasive ambulatory BP monitoring instrument. BP readings were obtained at 15-min intervals during the day and at 30-min intervals during the night. Of the total readings, ≥80% was considered valid. Furthermore, for the records valuable, at least 14 measurements during the daytime period or at least 7 measurements during the night or rest period were required (4). Individual correction was made for the awake and sleeping hours reported by the patient.
Ambulatory arterial stiffness index (AASI)
AASI was calculated as 1 minus the regression slope of diastolic BP plotted against systolic BP obtained through individual 24-h ABPM. The stiffer the arterial tree, the closer the regression slope and AASI are to 0 and 1, respectively (16).
Assessment of carotid intima-media thickness (CIMT)
Carotid arteries were investigated in the longitudinal and transverse projections with B-mode sonography (Mindray M7 DC7, 2012 Germany) using a 7 MHz linear probe. The intima-media thickness of both carotid arteries was always measured on the common carotid artery after the examination of a 10-mm longitudinal section at a distance of 1 cm from the bifurcation, outside the plaque, if any was present. Measurement of the right and left carotid arteries was calculated by taking the average of 3 readings (1). Mean IMT was considered abnormal if it exceeded 0.9 mm or if there were atherosclerotic plaques with a diameter of over 1.5 mm or a focal increase of 0.5 mm or 50% of the adjacent IMT (17).
Conventional echocardiography
The echocardiographic studies, including two-dimensional, M-mode, pulsed Doppler, and pulsed tissue Doppler imaging (TDI) examinations, were performed with the use of an echocardiography machine (VIVID S-5 General Electric Medical System Vingmed Ultrasound AS, Horten, Norway) equipped with a 3.6MHz transducer and TDI. Measurements were performed according to the American Society of Echocardiography guidelines (18) by a cardiologist who was unaware of the results of the AASI values. LV dimensions (end-diastolic and end-systolic) and wall thickness (septum and posterior wall) were obtained from the parasternal long axis. The LV end-diastolic volume (EDV) and end-systolic volume (ESV) were calculated from the apical two- and four-chamber views using a modified Simpson’s method. The LV-EF was calculated as LV-EF= (EDV-ESV)/EDV X 100 (18). LV mass was calculated according to the Devereux formula =0.8[1.04[[(LV-end diastolic dimension+ interventricular septum dimension + posterior wall dimension)3 - [LV-end diastolic dimension3)]] + 0.6 (19) and was indexed to the body surface area. The relative wall thickness (RWT) was calculated as the ratio [2x posterior wall thickness (PWT)/LV internal dimension at end-diastole (LVIDd)].
Mitral inflow velocities were evaluated by pulse wave Doppler with the sample volume placed at the tip of the mitral leaflets from the apical 4-chamber view. Using the average of three beats, we measured diastolic peak early (E), peak late transmitral flow velocity (A), E/A, and deceleration time of peak E velocity (EDT). Mitral annulus velocity was acquired from the septal and lateral sides of the annulus by TDI using the pulse wave Doppler mode. Systolic tissue velocity (S”) and early diastolic tissue velocity (E) were measured from averaging values. To evaluate LV filling pressures, the ratio of E/E’ was calculated.
Left atrial volume was measured by using the area-length (L) method using the apical 4-chamber view (A1) and apical 2-chamber view (A2) at ventricular end-systole. The information was put into the formula 0.85 (A1 x A2) divided by L for the atrial volume and indexed to body surface area (BSA), giving us the left atrial volume index (LAVI) (20).
Two-dimensional speckle tracking analysis
Two-dimensional grayscale images of the LA were acquired in the 2- and 4-chamber views at end-expiratory apnea during 5 cardiac cycles. Transthoracic images were processed for assessing left atrial deformation through speckle tracking imaging using 2D strain software (EchoPAC 108.1.12, General Electric Medical Systems, Horten, Norway, featuring software for speckle-tracking of the left ventricle) by two cardiologists who were blinded to the AASI results.
The left atrium endocardial surface was manually traced using a point-and-click approach, which allowed the automatic definition of a region of interest. The region of interest was divided into 6 segments by the software, and the resulting tracking quality for each segment was scored as either acceptable or non-acceptable. Segments classified as “non-acceptable” were rejected by the software and excluded from the analysis. In subjects with adequate image quality, global LA strain and strain rate parameters were assessed as the average of 6 segmental values. The values of LA function parameters, including peak LA strain and strain rate during ventricular systole (S-LAs and SR-LAs, respectively), peak early diastolic LA strain and strain rate (S-LAe and SR-LAe, respectively), and peak LA strain and strain rate during atrial systole (S-LAa and SR-LAa, respectively), were obtained by averaging values obtained in the apical 4- and 2-chamber views.
Statistical analysis
SPSS 17.0 statistical software (SPSS Inc., Chicago, IL, USA) was used for the statistical analysis. Continuous variables were expressed as mean±standard deviation (SD) or median and interquartile range, as appropriate. Categorical variables were expressed as percentage. The Kolmogorov-Smirnov test was used to test the normality of distribution of continuous variables. Pearson and Spearman correlation analysis was used for assessing the correlates of AASI. Logarithmic transformation was performed for non-normally distributed variables (LDL, S-LAe, carotid intima-media thickness, HT duration, fasting plasma glucose). Variables that correlated with AASI in the correlation analysis were entered into a multiple linear regression analysis that evaluated the independent predictors of AASI. A two-tailed p<0.05 was considered statistically significant.
Results
The clinical and demographic characteristics of the study population are presented in Table 1. The study consisted of 121 patients (70 females). The mean age of the patients was 58.49±8.04 years. The office systolic BP and diastolic BP was 149.31±12.09 (mm Hg) and 89.44±9.64 (mm Hg), respectively. The overall systolic BP and diastolic BP was 139.98±15.59 (mm Hg) and 78.28±9.28 (mm Hg), respectively. The mean AASI was 0.51±0.13.
Table 1.
General clinical and demographic characteristics of the study population (n: 121)
| Variables | Values |
|---|---|
| Age, years | 58.49±8.04 |
| Male, n, % | 51 (42.1%) |
| BMI, kg/m2 | 32.26±4.89 |
| Hypertension-duration, years | 7 (range: 0.5-20), [5-10] |
| Diabetes mellitus-duration, years | 6 (range: 0.5-12), [3-9] |
| Smokers, % | 14 (11.6%) |
| ACE inhibitors, ARB % | 103 (85.1%) |
| Beta-blockers % | 48 (39.7%) |
| Calcium channel blockers % | 38 (31.4%) |
| MDRD eGFR, mL/min | 86.97±18.27 |
| Fasting plasma glucose, mg/dL | 134 (range: 63-392), [115.5-172.5] |
| Triglycerides, mg/dL | 190.51±163.44 |
| Total cholesterol, mg/dL | 193.84±42.29 |
| LDL cholesterol, mg/dL | 127 (range: 65-251), [107.5-145] |
| HDL cholesterol, mg/dL | 44.78±9.24 |
| HbA1c, % | 8.04±1.57 |
| Overall systolic BP, mm Hg | 139.98±15.59 |
| Overall diastolic BP, mm Hg | 78.28±9.28 |
| Overall pulse pressure, mm Hg | 61.69±11.04 |
| Overall heart rate | 70.69±8.64 |
| Office systolic BP, mm Hg | 149.31±12.09 |
| Office diastolic BP, mm Hg | 89.44±9.64 |
| Office pulse pressure, mm Hg | 59.88±8.88 |
| Office heart rate | 73.17±12.91 |
| Carotid intima-media thickness, mm | 0.7 (range: 0.4-1.5), [0.6-0.9] |
| AASI | 0.51±0.13 |
Data are expressed in numbers (percentages), mean±1 SD or median and [range, (25% percentile-75% percentile)]. Percentages are rounded.
AASI - ambulatory artery stiffness index; ACE - angiotensin-converting enzyme;
ARB - angiotensin receptor blocker; BMI - body mass index; BP - blood pressure; eGFR - estimated glomerular filtration fraction; HDL - high-density lipoprotein; LDL - low-density lipoprotein; MDRD - modification of diet in renal disease
Conventional echocardiographic and 2D-STE parameters of the patients are presented in Table 2. The main findings were shown.
Table 2.
Conventional and 2D-STE parameters of the study population (n: 121)
| Variables | Values |
|---|---|
| LV end-diastolic dimension, mm | 48.82±5.18 |
| LV end-systolic dimension, mm | 29.38±4.03 |
| LV ejection fraction, % | 60.32±5.66 |
| Septal wall thickness, mm | 11.37±2.00 |
| Posterior wall thickness, mm | 10.81±1.90 |
| LV mass index, g/m2 | 110.09±34.08 |
| Relative wall thickness | 0.45±0.08 |
| E wave, m/s | 0.79±0.18 |
| A wave, m/s | 0.91±0.24 |
| E/A | 0.95±0.30 |
| Deceleration time, ms | 182.64±34.40 |
| S’ (systolic tissue velocity), m/s | 0.09±0.02 |
| E’ (early diastolic tissue velocity), m/s | 0.11±0.03 |
| E (early diastolic mitral inflow velocity)/E’ | 8.01±2.60 |
| LAVI, mL/m2 | 28.65±5.19 |
| S-LAs, % | 32.46±9.64 |
| S-LAe, % | 16.63 (8.51) |
| S-LAa, % | 17.88±4.19 |
| SR-LAs, s-1 | 1.45±0.39 |
| SR-LAe, s-1 | -1.46±0.48 |
| SR-LAa, s-1 | -2.37±0.60 |
Data are expressed mean±SD. Percentages are rounded.
LV - left ventricle; LAVI - left atrial volume index; S-LAs -peak left atrial strain during ventricular systole; S-LAe-peak left atrial strain at early diastole; S-LAa - peak left atrial strain at atrial systole; SR-LAs - peak left atrial strain rate during ventricular systole; SR-LAe - peak left atrial strain rate at early diastole; SR-LAa - peak left atrial strain rate at atrial systole
The univariate analysis showed that AASI was positively correlated with age (r=÷0.287, p=÷0.001), HT duration (year) (r=÷0.388, p=÷<0.001), fasting plasma glucose (mg/dL) (r=÷0.224, p=t0.014), HbA1c (%) (r=÷0.206, p=÷0.023), LDL cholesterol (mg/dL) (r=÷0.254, p=÷0.005), and also overall PP (mm Hg) (r=÷0.195, p=÷0.002), office PP (mm Hg) (r=÷0.188, p=÷0.039), CIMT (mm) (r=÷0.198, p=÷0.029), E/E’ (r=÷0.248, p=÷0.006), and LAVI (mL/m2) (r=÷0.237, p=÷0.009). Moreover, AASI was negatively correlated with GFR (mL/min) (r=÷(-) 0.242, p=÷0.008), S-LAs (%) (r=÷(-) 0.654, p<0.001), S-LAe (%) (r=÷(-) 0.215, p=÷0.018), and SR-LAs (s-1) (r=÷(-) 0.607, p<0.001) (Table 3).
Table 3.
The correlates of ambulatory arterial stiffness index (AASI)
| Variables | R | P |
|---|---|---|
| Age, years | 0.287 | 0.001 |
| BMI, kg/m2 | 0.238 | 0.109 |
| Hypertension duration, years | 0.388 | <0.001 |
| Diabetes mellitus duration, years | 0.169 | 0.063 |
| MDRD eGFR, mL/min | -0.242 | 0.008 |
| Fasting plasma glucose, mg/dL | 0.224 | 0.014 |
| Triglycerides, mg/dL | -0.086 | 0.350 |
| Total cholesterol, mg/dL | -0.251 | 0.005 |
| LDL cholesterol, mg/dL | 0.254 | 0.005 |
| HDL cholesterol, mg/dL | -0.031 | 0.735 |
| HbA1c, % | 0.206 | 0.023 |
| Overall systolic BP, mm Hg | 0.087 | 0.341 |
| Overall diastolic BP, mm Hg | -0.086 | 0.349 |
| Overall pulse pressure, mm Hg | 0.195 | 0.002 |
| Office systolic BP, mm Hg | 0.155 | 0.090 |
| Office diastolic BP, mm Hg | 0.021 | 0.815 |
| Office pulse pressure, mm Hg | 0.188 | 0.039 |
| Carotid intima-media thickness, mm | 0.198 | 0.029 |
| LV ejection fraction, % | 0.107 | 0.244 |
| LV mass index, g/m2 | 0.119 | 0.194 |
| Relative wall thickness | 0.052 | 0.559 |
| S’ (systolic tissue velocity), m/s | -0.038 | 0.676 |
| E (early diastolic mitral inflow velocity)/E’ | 0.248 | 0.006 |
| LAVI, mL/m2 | 0.237 | 0.009 |
| S-LAs, % | -0.654 | <0.001 |
| S-LAe, % | -0.215 | 0.018 |
| S-LAa, % | -0.093 | 0.311 |
| SR-LAs, s-1 | -0.607 | <0.001 |
| SR-LAe, s-1 | -0.072 | 0.431 |
| SR-LAa, s-1 | -0.052 | 0.571 |
BMI - body mass index; BP - blood pressure; eGFR - estimated glomerular filtration fraction; HDL - high-density lipoprotein; LDL - low-density lipoprotein; LV - left ventricle; LAVI - left atrial volume index; MDRD - modification of diet in renal disease; S-LAs - peak left atrial strain during ventricular systole; S-LAe - peak left atrial strain at early diastole; S-LAa - peak left atrial strain at atrial systole; SR-LAs - peak left atrial strain rate during ventricular systole; SR-LAe - peak left atrial strain rate at early diastole; SR-LAa - peak left atrial strain rate at atrial systole. Pearson and Spearman correlation analysis was used for assessing the correlates of AASI
A multiple linear regression model was built to find the independent determinants of AASI. Significant correlates of AASI, including age, overall PIP HT duration, fasting plasma glucose, eGFR, LDL cholesterol, E/E, LAVI, SR-LAs, S-LAe, and CIMT, were included in the model. The multiple linear regression analysis showed that AASI was independently associated with SR-LAs (β=÷-0.175, p<0.001) (Table 4). The correlation between AASI and SR-LAs is shown in Figure 1.
Table 4.
Independent predictors of AASI (ambulatory artery stiffness index)
| Variables | B | P | CI 95% |
|---|---|---|---|
| Age, years | 0.001 | 0.390 | -0.001-0.004 |
| Overall pulse pressure, mm Hg | 0.001 | 0.268 | -0.001-0.003 |
| LOG10 Hypertension duration, years | 0.045 | 0.149 | -0.016-0.107 |
| LOG10 Fasting plasma glucose, mg/dL | 0.054 | 0.342 | -0.058-0.165 |
| MDRD eGFR, mL/min | -0.001 | 0.109 | -0.002-0.000 |
| LOG10 LDL cholesterol, mg/dL | 0.154 | 0.074 | -0.323-0.015 |
| E (early diastolic mitral inflow velocity)/E’ | 0.006 | 0.115 | -0.001-0.013 |
| LAVI, mL/m2 | 0.003 | 0.151 | 0.001-0.006 |
| SR-LAs, s-1 | -0.175 | <0.001 | -0.225- -0.126 |
| LOG10 S-LAe, % | -0.011 | 0.861 | -0.138-0.116 |
| LOG10 Carotid intima-media thickness, mm | -0.011 | 0.882 | -0.151-0.130 |
E’ - early diastolic tissue velocity; eGFR - estimated glomerular filtration fraction; LAVI - left atrial volume index; LDL - low-density lipoprotein; MDRD - modification of diet in renal disease; SR-LAs - peak left atrial strain rate during ventricular systole; S-LAe - peak left atrial strain at early diastole
The independent predictors of AASI were evaluated with multiple linear regression analysis
Figure 1.
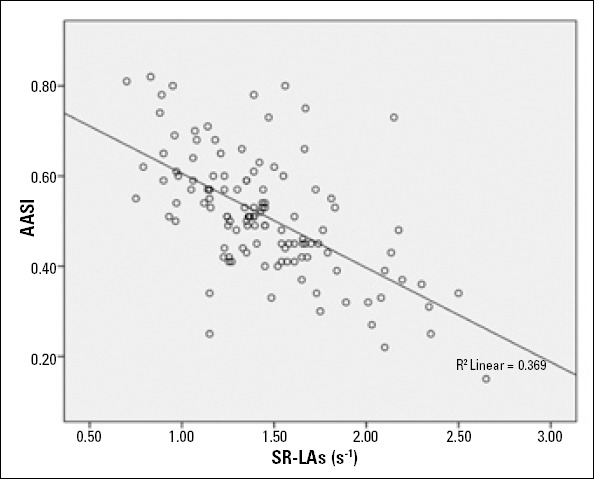
The correlation between AASI and SR-LAs
Multiple linear regression analysis showed that AASI was independently associated with SR-LAs.
A partial correlation analysis was performed to determine the partial correlation between LA strain parameters and AASI, adjusted for fasting plasma glucose, LDL cholesterol, HDL cholesterol, triglyceride, age, and LV mass index. We found that AASI was negatively correlated with SR-LAs (p<0.001, r=-0. 584) and S-LAs (p<0.001, r=-0.642) but not with S-LAe (p=0.177, r=-0.127).
Discussion
The results of the present study demonstrated that increased AASI is associated with impaired LA functions, independent of LV diastolic dysfunction, in hypertensive diabetic patients who are under medical treatment and have no history of CV disease.
Patients with type 2 DM are at high risk of developing CV disease (21). In addition, the clinical and morphologic features of CV disease are more severe in hypertensive diabetic patients compared to lone hypertensive or diabetic patients (22). Therapies during the early stages of CV structural changes in these patients can potentially delay or impede the progression of more permanent stages (22, 23). Clinical markers may be helpful in the early stages in the identification of patients who are at high CV risk.
Several authors suggested that AASI can be considered not as a marker of arterial stiffness but rather as a composite index reflecting cardiovascular properties (3). The Dublin study, which enrolled 11.291 hypertensive patients with a median follow-up of 5.3 years, showed that AASI could predict CV mortality beyond classical risk factors (24).
Vascular and structural changes increase during normal aging (6). Furthermore, the presence of HT and DM accelerates these changes, and it is increasingly being recognized that arterial stiffness is one of the most significant hemodynamic factors contributing to the development of CV complications (2, 25). It was considered that functional changes occur before structural changes. The arterial wave reflection returns during early diastole in compliant arteries, whereas it returns during late systole in individuals with stiffer arteries (6). The increase in late systolic load prolongs the systolic interval, resulting in delayed onset of LV relaxation (26). On the other hand, decreased disten-sibility of the arterial wall increases systolic BP and decreases diastolic BP, leading to increased LV afterload and impairment of myocardial blood flow because of decreased coronary perfusion pressure. These abnormalities cause a predominant decrease of blood supply in the subendocardial myocardium, resulting in a closer relationship between LV relaxation and arterial stiffness (6).
An increase in LA afterload through the development of LV-impaired relaxation and elevated filling pressure has previously been considered the main underlying mechanism of LA dysfunction. However, several studies showed that LA stiffness is already increased, even when LV filling pressure in not elevated (10, 12). Mondillo et al. (10) found in their study that hypertensive diabetic patients with normal values of LAVI had impaired LA deformation mechanics compared to a healthy control group, independent of LV diastolic dysfunction. Although our study did not include healthy controls, the study subjects had normal LAVI values, and we found that AASI is associated with impaired left atrial mechanical functions, independent of LV filling pressure. Moreover, after the adjustments for potential confounders (fasting plasma glucose, LDL cholesterol, HDL cholesterol, triglyceride, age, and LV mass index) were maintained, AASI remained significantly associated with LA mechanical functions. Miyoshi et al. (6) suggested that in preclinical patients (E/A>1), carotid arterial stiffness correlates with LAVI and LA strain variables, but only SR-LAs was an independent predictor related to carotid arterial stiffness. Our results are also in concordance with this study, but we evaluated arterial stiffness by AASI, which was found to be associated with CIMT. Oishi et al. (12) examined preclinical patients with CV risk factors and no elevation in LV filling pressure using 2D-STE, and in consistent with the findings of our study, they demonstrated that abdominal aortic stiffness is associated with LA stiffness during systole and LV relaxation in the longitudinal direction. Kuppahally et al. (27) found an inverse relationship between LA strain and percentage of fibrosis in the LA wall by delayed enhancement magnetic resonance imaging. Therefore, it is speculated that elevated LV filling pressure may not fully explain LA dysfunction and that LA myocardial fibrosis may play a key role in LA systolic and diastolic dysfunction (12). The development of a stiffer LA secondary to an LA subendocardial fibrotic process, in parallel with fibrotic alterations of the LV subendocardial layer (28) and medial degeneration, which leads to progressive stiffening of the large elastic arteries (29), could also occur in the earlier setting as a result of comorbid conditions, such as HT and DM (12). These findings could explain the normal or intermediate E/E” ratios in our study population, suggesting that LA functions are decreased, even when LV filling pressure is not elevated. We found that E/E’ and LAVI were positively correlated with AASI, but the multiple analysis showed that only SR-LAs was an independent predictor of AASI. The decreased systolic LA strain and strain rate and increased AASI in our study may indicate an early form of abnormal LA-arterial coupling in hypertensive diabetic patients.
Recently, LA deformation analyses using 2D-STE have been proven to be superior to conventional echocardiography in detecting subtle changes in LA function (28). Several studies suggested that SR-LAs correlated inversely with age and LA diameter in healthy individuals, SR-LAs decreased before the development of LA enlargement and LV hypertrophy in hypertensive patients, and LA wall fibrosis was inversely related with SR-LAs and S-LAs (30). So, we preferred to perform 2D-STE for the assessment of LA functions.
It has been shown that AASI predicts stroke independently of other known risk factors and is superior to PWV (2). Stroke risk is highly dependent on BP but also on arterial stiffness. Aortic stiffness and the subsequent increase in central PP are associated with CIMT, atheroma formation, and plaque rupture, providing a pathophysiological link between vascular mechanisms and cerebrovascular events (8). Gómez-Marcos et al. (16) examined the relationship between CIMT and arterial stiffness with PWV and AASI in diabetic and non-diabetic patients. They suggested that CIMT showed a positive correlation with PWV and AASI. However, when adjusting for age, gender, and heart rate, the association to PWV was lost in diabetic patients; so, this evidence may explain the superiority of AASI to PWV in predicting stroke. In this study, we showed that 24-h PP and CIMT were correlated with AASI. But, only SR-LAs was found to be an independent predictor of AASI. Decreased LA strain was found to be related with atrial fibrillation in previous studies (6). Therefore, we can speculate that the mechanism between AASI and stroke might be related with PP, CIMT, and also increased atrial fibrillation risk in these patients. In patients with type-2 DM and obesity, the fibrotic processes of the LV have been mainly related to perivascular fibrosis and increased collagen deposition in the LV, which was evaluated with E/E’ in our study. Also, the relationship between AASI and BMI is controversial (2) in studies and we did not found any correlation.
Study limitations
The sample size of subjects is relatively small to generalize our findings. Because dedicated software for LA strain has not yet been released, we used the current software for LV analysis to study LA strain. Another limitation was the lack of hemodynamic data about LV filling pressures. Nonetheless, several studies have demonstrated the high sensitivity, specificity, and accuracy of mitral E/E’ ratio in determining LV filling pressures.
Conclusion
In hypertensive diabetic patients, increased AASI is associated with impaired LA functions, independent of LV diastolic dysfunction. This can be an early sign of LV diastolic dysfunction. AASI could be used as a useful parameter for CV risk assessment.
Footnotes
Conflict of interest: None declared.
Peer-review: Externally peer-reviewed.
Authorship contributions: Concept - E.K., T.G., A.Ç.A., Ş.Ç.; Design - E.K., T.G., Ş.Ç.; Supervision - E.K., T.G., A.Ç.A., Ş.Ç.; Data collection &/or processing - A.Ç.A., G.Ç., E.H., M.Ç.; Analysis &/or interpretation - O.M.G., M.Ç., E.H.; Literature search - M.Ç., G.Ç., O.M.G.; Writing -M.G., Ş.Ç.; Critical review - Ş.Ç.
References
- 1.Leoncini G, Ratto E, Viazzi F, Vaccaro V, Parodi A, Falqui V, et al. Increased ambulatory arterial stiffness index is associated with target organ damage in primary hypertension. Hypertension. 2006;48:397–403. doi: 10.1161/01.HYP.0000236599.91051.1e. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 2.Kollias A, Stergiou GS, Dolan E, O’Brien E. Ambulatory arterial stiffness index: a systematic review and meta-analysis. Atherosclerosis. 2012;224:291–301. doi: 10.1016/j.atherosclerosis.2012.03.039. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 3.Li Y, Wang JG, Dolan E, Gao PJ, Guo HF, Nawrot T, et al. Ambulatory arterial stiffness index derived from 24-hour ambulatory blood pressure monitoring. Hypertension. 2006;47:359–64. doi: 10.1161/01.HYP.0000200695.34024.4c. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 4.García-García A, Gómez-Marcos MA, Recio-Rodriguez JI, González-Elena LJ, Parra-Sanchez J, Fe Munoz-Moreno M, et al. Relationship between ambulatory arterial stiffness index and sub-clinical target organ damage in hypertensive patients. Hypertens Res. 2011;34:180–6. doi: 10.1038/hr.2010.195. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 5.Hansen TW, Li Y, Staessen JA, Jeppesen J, Rasmussen S, Wang JG, et al. Independent prognostic value of the ambulatory arterial stiffness index and aortic pulse wave velocity in a general population. J Hum Hypertens. 2008;22:214–6. doi: 10.1038/sj.jhh.1002295. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 6.Miyoshi H, Mizuguchi Y, Oishi Y, Iuchi A, Nagase N, Ara N, et al. Early detection of abnormal left atrial-left ventricular-arterial coupling in preclinical patients with cardiovascular risk factors: evaluation by two-dimensional speckle-tracking echocardiography. Eur J Echocardiogr. 2011;12:431–9. doi: 10.1093/ejechocard/jer052. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 7.Kalay N, Elcik D, Doğan A, Saka T, Doğdu O, Koç F, et al. The effects of significant coronary stenosis and percutaneous coronary intervention on aortic stiffness. Turk Kardiyol Dern Ars. 2012;40:143–7. doi: 10.5543/tkda.2012.01714. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 8.Lantelme P, Laurent S, Besnard C, Bricca G, Vincent M, Legedz L, et al. Arterial stiffness is associated with left atrial size in hypertensive patients. Arch Cardiovasc Dis. 2008;101:35–40. doi: 10.1016/s1875-2136(08)70253-5. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 9.Douglas PS. The left atrium: a biomarker of chronic diastolic dysfunction and cardiovascular disease risk. J Am Coll Cardiol. 2003;42:1206–7. doi: 10.1016/s0735-1097(03)00956-2. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 10.Mondillo S, Cameli M, Caputo ML, Lisi M, Palmerini E, Padeletti M, et al. Early detection of left atrial strain abnormalities by speckle-tracking in hypertensive and diabetic patients with normal left atrial size. J Am Soc Echocardiogr. 2011;24:898–908. doi: 10.1016/j.echo.2011.04.014. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 11.Vianna-Pinton R, Moreno CA, Baxter CM, Lee KS, Tsang TS, Appleton CR. Two-dimensional speckle-tracking echocardiography of the left atrium: feasibility and regional contraction and relaxation differences in normal subjects. J Am Soc Echocardiogr. 2009;22:299–305. doi: 10.1016/j.echo.2008.12.017. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 12.Oishi Y, Miyoshi H, Iuchi A, Nagase N, Ara N, Oki T. Negative impact of cardiovascular risk factors on left atrial and left ventricular function related to aortic stiffness-new application of 2-dimensional speckle-tracking echocardiography. Circ J. 2013;77:1490–8. doi: 10.1253/circj.cj-12-1260. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 13.Cameli M, Lisi M, Focardi M, Reccia R, Natali BM, Sparla S, et al. Left atrial deformation analysis by speckle tracking echocardiography for prediction of cardiovascular outcomes. Am J Cardiol. 2012;110:264–9. doi: 10.1016/j.amjcard.2012.03.022. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 14.Imai E, Horio M, Nitta K, Yamagata K, Iseki K, Tsukamoto Y, et al. Modification of the Modification of Diet in Renal Disease (MDRD) Study equation for Japan. Am J Kidney Dis. 2007;50:927–37. doi: 10.1053/j.ajkd.2007.09.004. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 15.Mallion J-M, Pierre H, Neuder Y, Ormezzano O, Baguet JR. Validation of the AGILIS ambulatory blood pressure monitor according to the European Society of Hypertension International Protocol for validation of blood pressure measuring devices in adults. Blood Press Monit. 2005;10:97–101. doi: 10.1097/00126097-200504000-00008. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 16.Gómez-Marcos MA, Recio-Rodríguez JI, Patino-Alonso MC, Agudo-Conde C, Gómez-Sánchez L, Rodríguez-Sánchez E, et al. Relationship between intima-media thickness of the common carotid artery and arterial stiffness in subjects with and without type 2 diabetes: a case-series report. Cardiovasc Diabetol. 2011;10:3. doi: 10.1186/1475-2840-10-3. [CrossRef] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mancia G, De Backer G, Dominiczak A, Cifkova R, Fagard R, Germano G, et al. 2007 ESH-ESC Practice Guidelines for the Management of Arterial Hypertension: ESH-ESC Task Force on the Management of Arterial Hypertension. J Hypertens. 2007;25:1751–62. doi: 10.1097/HJH.0b013e3282f0580f. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 18.Gottdiener JS, Bednarz J, Devereux R, Gardin J, Klein A, Manning WJ, et al. American Society of Echocardiography recommendations for use of echocardiography in clinical trials. J Am Soc Echocardiogr. 2004;17:1086–119. doi: 10.1016/j.echo.2004.07.013. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 19.Jafary FH. Devereux formula for left ventricular mass-be careful to use the right units of measurement. J Am Soc Echocardiogr. 2007;20:783. doi: 10.1016/j.echo.2007.02.034. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 20.Shaikh Q, Ahmed B, Ahmed M, Mahar JH, Ahmad M, Ahmed A, et al. Left atrial volumes and associated stroke subtypes. BMC Neurol. 2013;13:149. doi: 10.1186/1471-2377-13-149. [CrossRef] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Alpaydın MS, Aksakal E, Erol MK, Simşek Z, Açıkel M, Arslan S, et al. Assessment of regional left ventricular functions by strain and strain rate echocardiography in type II diabetes mellitus patients without microvascular complications. Turk Kardiyol Dern Ars. 2011;39:378–84. doi: 10.5543/tkda.2011.01490. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 22.Fang ZY, Prins JB, Marwick TH. Diabetic cardiomyopathy: evidence, mechanisms, and therapeutic implications. Endocr Rev. 2004;25:543–67. doi: 10.1210/er.2003-0012. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 23.Fang ZY, Yuda S, Anderson V, Short L, Case C, Marwick TH. Echocardiographic detection of early diabetic myocardial disease. J Am Coll Cardiol. 2003;41:611–7. doi: 10.1016/s0735-1097(02)02869-3. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 24.Dolan E, Thijs L, Li Y, Atkins N, McCormack R, McClory S, et al. Ambulatory arterial stiffness index as a predictor of cardiovascular mortality in the Dublin Outcome Study. Hypertension. 2006;47:365–70. doi: 10.1161/01.HYP.0000200699.74641.c5. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 25.Kalaycıoğlu E, Gökdeniz T, Aykan AÇ, Gül I, Dursun I, Kiriş G, et al. The relationship between dipper/nondipper pattern and cardio-ankle vascular index in hypertensive diabetic patients. Blood Press Monit. 2013;18:188–94. doi: 10.1097/MBP.0b013e328362df70. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 26.Fukuta H, Ohte N, Wakami K, Asada K, Goto T, Mukai S, et al. Impact of arterial load on left ventricular diastolic function in patients undergoing cardiac catheterization for coronary artery disease. Circ J. 2010;74:1900–5. doi: 10.1253/circj.cj-10-0283. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 27.Kuppahally SS, Akoum N, Burgon NS, Badger TJ, Kholmovski EG, Vijayakumar S, et al. Left atrial strain and strain rate in patients with paroxysmal and persistent atrial fibrillation: relationship to left atrial structural remodeling detected by delayed-enhancement MRI. Circ Cardiovasc Imaging. 2010;3:231–9. doi: 10.1161/CIRCIMAGING.109.865683. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 28.Morris DA, Gailani M, Vaz Pérez A, Blaschke F, Dietz R, Haverkamp W, et al. Left atrial systolic and diastolic dysfunction in heart failure with normal left ventricular ejection fraction. J Am Soc Echocardiogr. 2011;24:651–62. doi: 10.1016/j.echo.2011.02.004. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 29.Jacob MR. Extracellular matrix remodeling and matrix metallopro-teinases in the vascular wall during aging and in pathological conditions. Biomed Pharmacother. 2003;57:195–202. doi: 10.1016/s0753-3322(03)00065-9. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 30.Kokubu N, Yuda S, Tsuchihashi K, Hashimoto A, Nakata T, Miura T, et al. Noninvasive assessment of left atrial function by strain rate imaging in patients with hypertension: a possible beneficial effect of renin-angiotensin system inhibition on left atrial function. Hypertens Res. 2007;30:13–21. doi: 10.1291/hypres.30.13. [CrossRef] [DOI] [PubMed] [Google Scholar]


