Abstract
Objective:
The aim of this study was to evaluate the relationship between atrial electromechanical delay (EMD) measured with tissue Doppler imaging (TDI) and left atrial (LA) mechanical functions in patients with ischemic stroke and compare them with healthy controls.
Methods:
Thirty patients with ischemic stroke were enrolled into this cross-sectional, observational study. The control group consisted of 35 age- and gender-matched apparently healthy individuals patients. Acute cerebral infarcts of probable embolic origin were diagnosed via imaging and were confirmed by a neurologist. Echocardiographically, time intervals from the beginning of P wave to beginning of A wave from the lateral and septal mitral and right ventricular tricuspid annuli in TDI were recorded. The differences between these intervals gave the mechanical delays (inter- and intra-atrial). Left atrial (LA) volumes were measured using the biplane area-length method, and LA mechanical function parameters were calculated. Statistical analysis was performed using student’s t-test, chi-squared test, and Pearson’s test.
Results:
The laboratory and clinical characteristics were similar in the two groups. Increased left atrial EMD (21.36±10.38 ms versus 11.74±6.06 ms, p<0.001), right atrial EMD (13.66±8.62 ms versus 9.66±6.81 ms, p=0.040), and interatrial EMD (35.03±9.95 ms versus 21.40±8.47 ms, p<0.001) were observed in stroke patients as compared to controls. Active LA emptying volume and fraction and passive LA emptying volumes and fraction were similar between controls and stroke patients. Total LA emptying volumes were significantly increased in stroke patients as compared to healthy controls (33.19±11.99 mL/m2 versus 27.48±7.08 mL/m2, p=0.021).
Conclusion:
According to the results of our study, interatrial electromechanical delay may be a new predictor for ischemic stroke.
Keywords: atrial electromechanical delay, stroke, left atrial functions
Introduction
Electrophysiological studies are typically employed to evaluate abnormalities of atrial conduction, but the invasiveness of this procedure limits its use. An alternative to electrophysiological studies is measuring the electromechanical delay (EMD), which is the temporal delay between the onset of detectable electrical activity and the initiation of myocardial contraction. Tissue Doppler imaging (TDI) is another simple and noninvasive alternative that provides real-time atrial and ventricular contraction analysis (1). Atrial EMD is measured from the onset of the P wave on the electrocardiogram (ECG) to the beginning of the atrial contraction as determined by TDI (2, 3). Atrial EMD has been associated with paroxysmal atrial fibrillation (AF), which increases the risk of thromboembolic events and may transform into permanent AF (4). Atrial fibrillation is one of the leading causes of embolic stroke, and so, it is imperative to diagnose this arrhythmia promptly to avoid fatal complications. Previous studies have evaluated the association between interatrial delay and embolic stroke via ECG. The aim of this study was to evaluate the relationship between atrial EMD, measured with tissue Doppler imaging (TDI), and left atrial mechanical functions in patients with ischemic stroke and compare them with the healthy controls.
Methods
Study design
This study was a cross-sectional observational study.
Study population
A total of 30 patients with ischemic stroke with an average age of 50±17 years were enrolled in the study. Thirty-five healthy subjects matching with the patients in terms of age and gender formed the control group. Diagnosis of acute cerebral ischemic infarcts of probable embolic origin was established via cranial magnetic resonance imaging (MRI) after neurologist evaluation, consistent with American Heart Association (AHA) guidelines and the Lausanne Stroke Registry and modified Oxfordshire Community Stroke Project criteria (5). Embolism was preliminarily cited as a probable cause in each patient, based on the clinical history and presentation, as well as newly evidenced lesion size, numbers, and anatomical cerebrovascular location in the absence of other etiologies prior to further investigation, such as Doppler ultrasonographic evaluations. Also, patients with evident thrombus/mass image in the left heart chambers and a patent foramen ovale detected on transesophageal echocardiography were excluded from the study. Patients with the following heart conditions were excluded from the study: heart failure (left ventricular ejection fraction less than 50% or any degree of diastolic dysfunction), heart valve disease, known coronary artery disease (more than 50% luminal stenosis in coronary arteries), atrial fibrillation, right or left bundle branch block on ECG, and mitral annular calcification. Certain medical conditions also precluded patients from study participation, such as diabetes mellitus, hypertension, evidence or history of thyroid dysfunction, symptomatic pulmonary disease, a serum creatinine level greater than 1.5 mg/dL, and severe anemia (hemoglobin less than 8 g/dL). Lastly, patients that required a permanent pacemaker, had poor echocardiographic studies, and were on medications that affected atrial conduction were excluded from the study, as well.
Informed consent was obtained from all patients. The study was approved by our local ethical committee.
Standard echocardiography
Echocardiographic examination (Vivid system 5, GE, Horten, Norway) was performed with a 2-4 MHz phased array transducer by a blinded cardiologist on the days 2-7 (median, day 4) of stroke. Single-lead ECG was conducted and recorded simultaneously with the echocardiographic examination. M-mode measurements and conventional Doppler echocardiography were attained according to the American Society of Echocardiography guidelines (6). M-mode measurements in the parasternal long-axis view consisted of dimensions for left atrial volume, end-systolic and end-diastolic left ventricular (LV) volumes, diastolic ventricular septum thickness, and diastolic LV posterior wall thickness. All measurements were recorded over an average of three cardiac cycles.
Left atrial mechanical function
Left atrial (LA) volumes were obtained via echocardiogram with apical four-chamber views that were obtained by the biplane area-length method (7, 8). Intra-observer coefficient of variation for LA volume was 4.1%. Left atrial maximum volume (Vmax) was measured at the end-systolic phase and was defined as the volume at the onset of mitral valve opening. LA minimum volume (Vmin) was determined at the end-diastolic phase when the mitral valve began to close. LA volume before atrial systole (Vp) was measured at the beginning of atrial systole during the onset of the P wave on the ECG and calculated according to body surface area. LA functional parameters were calculated with the following equations (8, 9):
Passive emptying volume = Vmax-Vp
Passive emptying fraction = [(Vmax-Vp)/Vmax] × 100%
Active emptying volume = Vp-Vmin
Active emptying fraction = [(Vp-Vmin)/Vp] × 100%
Total emptying volume = Vmax-Vmin
Atrial electromechanical delay
Tissue Doppler echocardiography was performed with a transducer set at a frequency of 3.5 to 4.0 MHz. The spectral pulsed Doppler signal filters were adjusting to obtain a Nyquist limit of 15 to 20 cm/sec with the minimum optimal gain setting. The monitor sweep speed was set at 50 to 100 mm/sec to optimize the spectral display of myocardial velocities. The lateral mitral annulus, septal mitral annulus, and tricuspid lateral annulus were all evaluated by TDI. Myocardial velocity curves were constructed from digitized images from apical 4-chamber views to assess atrial EMD. Atrial EMD, defined as the time interval from P wave onset on the ECG to the beginning of the late diastolic wave (Am wave), was calculated from the lateral (PA lateral) and septal (PA septum) mitral annuli, as well as the lateral tricuspid annulus (PA tricuspid) (Fig. 1). Values for atrial EMD were averaged over three consecutive beats. The difference between PA lateral and PA tricuspid (PA lateral-PA tricuspid) was called the interatrial EMD. The difference between PA septum and PA tricuspid (PA septum-PA tricuspid) was defined as the right atrial EMD. Lastly, the difference between PA lateral and PA septum (PA lateral-PA septum) was the left atrial EMD (8). Intra-observer coefficient of variation for intra- and interatrial EMD were 2.9% and 3.8%, respectively.
Figure 1.
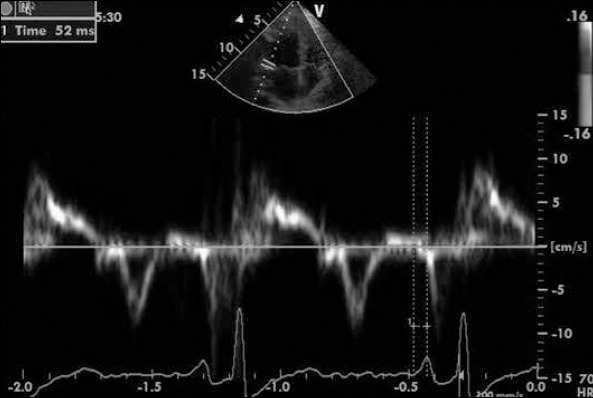
Measurement of the time between P wave onset and the beginning of the Am wave
Statistical analysis
Statistical analyses were performed with SPSS software, version 16.0 (SPSS, Chicago, IL, USA). Data variables were analyzed via visual methods, including histograms and probability plots, whereas the Kolmogorov-Smirnov and Shapiro-Wilks tests were utilized to determine whether the data conformed to a normal distribution. Descriptive data were expressed as the mean and standard deviation for normally distributed variables. Categorical variables were presented as quantities and percentages. For numerical data that were not normally distributed, a logarithmic transformation was utilized so that the data would then conform to a normal distribution. Numerical variables were compared using the student’s t-test. Categorical data were compared via the chi-squared test, and Pearson’s test was used for correlation analysis. Receiver operating characteristic (ROC) curve analysis was used to determine the optimum cut-off level of interatrial EMD to predict ischemic stroke. Multivariate logistic regression analysis was performed to assess the independent predictors of stroke. All variables that were significant in the univariate analysis were included in the model of logistic regression model, and the results are shown as an odds ratio (OR) with 95% confidence intervals (CIs). Statistical significance was defined as a p value less than 0.05.
Results
Study participant demographics and echocardiographic findings are demonstrated in Table 1. There were no significant differences regarding age, gender, systolic and diastolic blood pressures, and body mass index between patient and control groups (p>0.05). Left ventricular end-diastolic volume, LV ejection fraction, LA diameter, and LV deceleration time were similar between stroke patients and controls. Doppler and tissue Doppler echocardiography revealed that the LV E/A ratio was similar between patients and controls, but heart rate was higher in stroke patients (p=0.001), and LV isovolumetric relaxation time was greater in patients with stroke (88.73±17.98 ms versus 72.88±14.66 ms, p<0.001) (Table 1).
Table 1.
Baseline characteristics of stroke patients and controls
| Ischemic stroke group (n=30) | Control group (n=35) | P | |
|---|---|---|---|
| Age, years | 50.23±17.04 | 48.89±11.83 | 0.709 |
| Male, n (%) | 16.00 (53.3) | 18.00 (51.4) | 0.878 |
| Female, n (%) | 14.00 (46.7) | 17.00 (48.6) | 0.878 |
| Body mass index, kg/m2 | 24.80±4.50 | 25.07±4.31 | 0.811 |
| Systolic blood pressure, mm Hg | 118.65±10.44 | 116.51±8.83 | 0.845 |
| Diastolic blood pressure, mm Hg | 79.67±8.71 | 78.84±7.56 | 0.967 |
| Heart rate, beat/min | 81.37±9.56 | 74.97±6.20 | 0.001 |
| LV end-diastolic diameter, cm | 4.46±0.32 | 4.48±0.44 | 0.837 |
| LV end-systolic diameter, cm | 3.14±0.56 | 3.05±0.46 | 0.853 |
| Ejection fraction, % | 63.37±3.76 | 64.14±5.49 | 0.516 |
| Left atrial diameter, cm | 3.62±0.52 | 3.62±0.29 | 0.999 |
| Mitral E wave/A wave | 1.23±0.47 | 1.37±0.34 | 0.178 |
| E deceleration time, ms | 225.50±26.56 | 213.89±28.43 | 0.096 |
| Isovolumetric relaxation time, ms | 88.73±17.98 | 72.88±14.66 | <0.001 |
LV - left ventricular
Atrial EMD findings, as measured by TDI, are shown in Table 2. PA lateral (65.90±2.25 ms versus 51.34±10.15 ms, p<0.001) was significantly higher in patients with stroke as compared to controls. However, PA septum (44.53±11.52 ms versus 39.60±10.60 ms, p=0.077) and PA tricuspid were similar between both groups (30.86±7.72 ms versus 29.94±9.63 ms, p=0.675). Increased left atrial EMD (21.36±10.38 ms versus 11.74±6.06 ms, p<0.001), right atrial EMD (13.66±8.62 ms versus 9.66±6.81 ms, p=0.040), and interatrial EMD (35.03 ms±9.95 ms versus 21.40±8.47 ms, p<0.001) were observed in stroke patients as compared to controls. Left atrial volume indices are shown in Table 3. Vmax, Vp, and Vmin were similar between both groups (p>0.05). Active LA emptying volumes, active LA emptying fraction, and passive LA emptying fraction were similar between stroke patients and controls (p>0.05). Passive LA emptying volumes (18.85±9.19 mL/m2 versus 14.28±6.78 mL/m2, p=0.025) and total LA emptying volumes (33.19±11.99 mL/m2 versus 27.72±7.38 mL/m2, p=0.021) were significantly increased in stroke patients as compared to healthy controls. There was a positive correlation between interatrial EMD and left atrial EMD, right atrial EMD, and PA lateral. No significant correlations were found between interatrial EMD and age, body mass index, PA septal isovolumetric LV relaxation time, LV deceleration time, mitral E/A, passive LA emptying volume, and active LA emptying volume (Table 4).
Table 2.
Intra-and interatrial electromechanical delays for controls and stroke patients
| Ischemic stroke group (n=30) | Control group (n=35) | P | |
|---|---|---|---|
| PA lateral, ms | 65.90±12.25 | 51.34±10.15 | <0.001 |
| PA septal, ms | 44.53±11.52 | 39.60±10.60 | 0.077 |
| PA tricuspid, ms | 30.86±7.72 | 29.94±9.63 | 0.675 |
| Left atrial electromechanical delay, ms | 21.36±10.38 | 11.74±6.06 | <0.001 |
| Right atrial electromechanical delay, ms | 13.66±8.62 | 9.66±6.81 | 0.040 |
| Interatrial electromechanical delay, ms | 35.03±9.95 | 21.40±8.47 | <0.001 |
PA - time interval from the onset of the P wave to the beginning of the Am wave
Table 3.
Left atrial volume measurements of the stroke patient group
| Ischemic stroke group (n=30) | Control group (n=35) | P | |
|---|---|---|---|
| Vmax, mL/m2 | 55.45±22.00 | 47.32±12.22 | 0.079 |
| Vp, mL/m2 | 36.60±15.47 | 33.05±9.19 | 0.276 |
| Vmin, mL/m2 | 22.26±12.71 | 19.87±7.44 | 0.368 |
| Passive emptying volume, mL/m2 | 18.85±9.19 | 14.28±6.78 | 0.025 |
| Passive emptying fraction, % | 33.80±10.82 | 30.02±11.37 | 0.185 |
| Active emptying volume, mL/m2 | 14.34±8.00 | 13.20±5.35 | 0.240 |
| Active emptying fraction, % | 43.95±16.43 | 40.00±12.69 | 0.279 |
| Total emptying volume, mL/m2 | 33.19±11.99 | 27.48±7.08 | 0.021 |
Vmax - left atrial maximum volume; Vmin - minimal left atrial volume; Vp - left atrial volume at the beginning of atrial systole
Table 4.
The association between interatrial electromechanical delay and echocardiographic findings*
| r value | P | |
|---|---|---|
| Age, years | 0.006 | 0.975 |
| Body mass index, kg/m2 | -0.015 | 0.936 |
| Mitral E wave/A wave | 0.125 | 0.509 |
| Isovolumetric relaxation time, ms | -0.194 | 0.304 |
| E deceleration time, ms | -0.110 | 0.562 |
| Total emptying volume, mL/m2 | -0.061 | 0.750 |
| Passive emptying volume, mL/m2 | -0.078 | 0.683 |
| Active emptying volume, mL/m2 | -0.091 | 0.632 |
| PA lateral, ms | 0.777 | <0.001 |
| PA septal, ms | 0.248 | 0.187 |
| Left atrial electromechanical delay, ms | 0.642 | <0.001 |
| Right atrial electromechanical delay, ms | 0.381 | 0.038 |
PA - time interval from the onset of the P wave to the beginning of the Am wave
Pearson’s test was used for correlation analysis
Using a cut-off level of 25 ms, interatrial EMD predicted stroke with a sensitivity of 83% and specificity of 75% (ROC area under the curve: 0.860, 95% CI: 0.773-0.948, p<0.001; Fig. 2).
Figure 2.
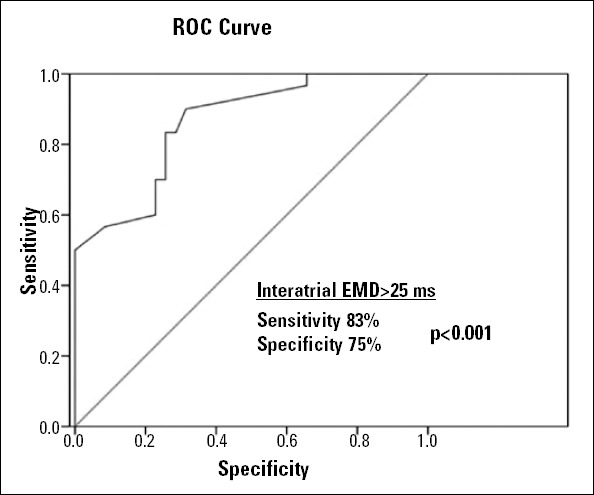
Receiver operating characteristics (ROC) curve analysis of interatrial electromechanical delay (EMD) for predicting the presence of ischemic stroke
After multivariate analysis, a high level of interatrial EMD was found to be an independent predictor of stroke (OR: 1.115, 95% CI: 1.045-1.265, p=0.004), together with isovolumetric relaxation time (OR: 1.091, 95% CI: 1.018-1.169, p=0.013; Table 5).
Table 5.
Multivariate logistic regression analysis to assess predictors of ischemic stroke
| Odds ratio (95% CI) | P | |
|---|---|---|
| Total emptying volume, mL/m2 | 0.967 (0.842-1.111) | 0.635 |
| Interatrial electromechanical delay, ms | 1.115 (1.045-1.265) | 0.004 |
| Heart rate, beat/min | 1.135 (0.980-1.315) | 0.091 |
| Isovolumetric relaxation time, ms | 1.091 (1.018-1.169) | 0.013 |
| Passive emptying volume, mL/m2 | 1.101 (0.947-1.281) | 0.211 |
CI - confidence interval
Discussion
In the present study, we demonstrated an independent association between interatrial EMD and stroke. Also, passive LA emptying volumes and total LA emptying volumes were significantly increased in patients with stroke. Moreover, our study showed that an interatrial EMD >25 ms predicted stroke with a sensitivity of 83% and specificity of 75%. To our knowledge, this is the first study to report on the relationship between tissue Doppler EMD and stroke patients.
An embolism to the brain can be either arterial or cardiac in origin, with atrial fibrillation (AF) being the most common cause of cardioembolic stroke (10). Ischemic strokes without a well-defined etiology are labeled cryptogenic and account for 30%- 40% of all ischemic strokes (11). It has been suggested that cardiac embolism constitutes a major causative mechanism of cryptogenic stroke (12). A recent multicenter study demonstrated that almost 20% of patients with cryptogenic cerebral ischemia had occult paroxysmal atrial fibrillation (PAF) detected on outpatient cardiac telemetry over a 21-day period (13). There are several predictors of PAF, such as hypertension, heart failure, valvular heart disease, and hyperthyroidism (14, 15). In our previous multicenter study, the Atrial Fibrillation Registry in Turkey (AFTER), we found that hypertension was the most common comorbid condition in patients with AF (16, 17). In fact, an increased P wave duration on standard 12-lead ECG indicates the presence of an atrial conduction disorder (18). However, for patients without documented arrhythmias and suspected AF, 24-hour Holter monitoring has low sensitivity and specificity for detecting arrhythmias. P wave dispersion appears to correlate with increased P wave duration and may be a useful predictive indicator of AF (19). In a study by Doğan et al. (20), P wave dispersion on a single 12-lead ECG detected within 24 hours of an acute ischemic stroke was helpful in predicting PAF and may be utilized as a risk indicator for recurrent strokes. Also, several clinical studies have demonstrated a causal relationship between increased LA size and the development of paroxysmal and persistent AF (21, 22). However, in our study, there was no significant difference between stroke patients and controls in terms of LA size.
Several studies have demonstrated associations between interatrial or intra-atrial conduction block and PAF (23, 24). Kumagai et al. (25) reported that prolonged intra-atrial and interatrial conduction were observed in AF patients following electrocardioversion. Patients with a history of PAF, even those with a history of isolated AF, have abnormal atrial refractoriness and conduction as compared to patients without AF. Specifically, greater atrial mass shortens the refractory period and delays conduction, which may increase the quantity of daughter wavelets. Deniz et al. (26) suggested that TDI may be used to measure inter- and intra-atrial mechanical delays and that TDI may indicate an increase in left atrial electromechanical delay in PAF patients. Also, Ariyarajah et al. (27) proposed that an interatrial block on ECG may be a novel predictor of embolic stroke. Consistent with these studies, we demonstrated that left and right intra- and interatrial conduction delays were significantly prolonged in stroke patients as compared to healthy controls.
Atrial enlargement is associated with increased mortality in the general population. Increased left atrial diameter is correlated with cardiovascular disease and is a risk factor of AF (28). As such, atrial volumes may be utilized as indicators of atrial health and function. Direct and indirect atrial tissue damage arising from atrial overload impacts atrial mechanical function. In fact, LA function is an important determinant of ventricular diastolic filling (29). It has been demonstrated that in diabetic patients, decreased passive LA emptying volume is associated with higher end-diastolic LV pressures. In addition, increased active LA emptying volume is associated with greater LA contraction compensatory mechanisms (30). In our study, among LA mechanical functions, LV isovolumetric relaxation time and passive and total emptying volume were significantly increased in stroke patients.
There have been studies that have investigated whether echocardiographic examinations of LA predict the development of AF (31). Previous studies showed that a reduced A’, which is a parameter of LA contractile function, might predict future AF episodes (32). Moreover, an association between LA dilatation and interatrial EMD has been demonstrated in previous studies (3). Our study revealed that PA lateral and septal, in addition to right and left intra-atrial EMDs, are correlated with interatrial electromechanical delay. These data suggest that left and right atrial EMDs, as well as interatrial EMD, are all significantly associated with stroke. Moreover, total LA emptying volumes were significantly increased in stroke patients, and left atrial electromechanical function was associated with intra-atrial EMD.
Study limitations
The main limitation of our study was its small sample size. Another limitation was the lack of 24-hour rhythm Holter monitoring of patients and controls.
Conclusion
Interatrial delay and intra-atrial delay, which are predisposing factors for AF, may contribute to identify individuals at risk for ischemic stroke. Prospective, large-scale, multicenter investigations are needed to clarify the predictor role of inter-and intra- atrial delay for future ischemic stroke.
Footnotes
Conflict of interest: None declared.
Peer-review: Externally peer-reviewed.
Authorship contributions: Concept - M.A.A., E.A.; Design - M.A.A., E.A.; Supervision - M.A.A., H.A., M.O.; Resource - E.A., A.A., F.E.; Materials - M.O., E.A.; Data collection and/or processing - E.A., A.A., F.E.; Analysis and/or Interpretation - H.A., M.Z.B., A.Y.; Literature search - M.O., M.Z.B., A.Y.; Writing - M.A.A., H. A., A.Y., N.T.; Critical review - F.E., N.T.; Other - N.T.
This study was accepted at the Joint Congress of European Neurology, 31 May-3 June 2014; İstanbul, Turkey
References
- 1.Rein AJ, O’Donnell CP, Colan SD, Marx GR. Tissue velocity Doppler assessment of atrial and ventricular electromechanical coupling and atrioventricular time intervals in normal subjects. Am J Cardiol. 2003;92:1347–50. doi: 10.1016/j.amjcard.2003.08.026. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 2.Ermiş N, Açıkgöz N, Yaşar E, Taşolar H, Yağmur J, Cansel M, et al. Evaluation of atrial conduction time by P wave dispersion and tissue Doppler echocardiography in prehypertensive patients. Turk Kardiyol Dern Ars. 2010;38:525–30. [PubMed] [Google Scholar]
- 3.Özer N, Yavuz B, Can I, Atalar E, Aksöyek S, Övünç K, et al. Doppler tissue evaluation of intraatrial and interatrial electromechanical delay and comparison with P-wave dispersion in patients with mitral stenosis. J Am Soc Echocardiogr. 2005;18:945–8. doi: 10.1016/j.echo.2005.01.015. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 4.Bennett D. Atrial fibrillation. Eur Heart J. 1984;5(Suppl):A89–93. doi: 10.1093/eurheartj/5.suppl_a.89. [DOI] [PubMed] [Google Scholar]
- 5.Rojo-Martinez E, Sandin-Fuentes M, Calleja-Sanz AI, Cortijo-Garcia E, Garcia-Bermejo IP, Ruiz-Pinero M, et al. High performance of an implantable Holter monitor in the detection of concealed paroxysmal atrial fibrillation in patients with cryptogenic stroke and a suspected embolic mechanism. Rev Neurol. 2013;57:251–7. [PubMed] [Google Scholar]
- 6.Quinones MA, Otto CM, Stoddard M, Waggoner A, Zoghbi WA. Recommendations for quantification of Doppler echocardiography: a report from the Doppler Quantification Task Force of the Nomenclature and Standards Committee of the American Society of Echocardiography. J Am Soc Echocardiogr. 2002;15:167–84. doi: 10.1067/mje.2002.120202. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 7.Haffajee JA, Lee Y, Alsheikh-Ali AA, Kuvin JT, Pandian NG, Patel AR. Pre-operative left atrial mechanical function predicts risk of atrial fibrillation following cardiac surgery. JACC Cardiovasc Imaging. 2011;4:833–40. doi: 10.1016/j.jcmg.2011.03.019. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 8.Acar G, Akçay A, Sökmen A, Özkaya M, Güler E, Sökmen G, et al. Assessment of atrial electromechanical delay, diastolic functions, and left atrial mechanical functions in patients with type 1 diabetes mellitus. J Am Soc Echocardiogr. 2009;22:732–8. doi: 10.1016/j.echo.2009.03.028. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 9.Dilaveris PE, Gialafos EJ, Sideris SK, Theopistou AM, Andrikopoulos GK, Kyriakidis M, et al. Simple electrocardiographic markers for the prediction of paroxysmal idiopathic atrial fibrillation. Am Heart J. 1998;135:733–8. doi: 10.1016/s0002-8703(98)70030-4. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 10.Ferro JM. Cardioembolic stroke: an update. Lancet Neurol. 2003;2:177–88. doi: 10.1016/s1474-4422(03)00324-7. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 11.Bang OY, Lee PH, Joo SY, Lee JS, Joo IS, Huh K. Frequency and mechanisms of stroke recurrence after cryptogenic stroke. Ann Neurol. 2003;54:227–34. doi: 10.1002/ana.10644. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 12.Jickling GC, Stamova B, Ander BP, Zhan X, Liu D, Sison SM, et al. Prediction of cardioembolic, arterial, and lacunar causes of cryptogenic stroke by gene expression and infarct location. Stroke. 2012;43:2036–41. doi: 10.1161/STROKEAHA.111.648725. [CrossRef] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Miller DJ, Khan MA, Schultz LR, Simpson JR, Katramados AM, Russman AN, et al. Outpatient cardiac telemetry detects a high rate of atrial fibrillation in cryptogenic stroke. J Neurol Sci. 2013;324:57–61. doi: 10.1016/j.jns.2012.10.001. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 14.Wijffels MC, Kirchhof CJ, Dorland R, Allessie MA. Atrial fibrillation begets atrial fibrillation. A study in awake chronically instrumented goats. Circulation. 1995;92:1954–68. doi: 10.1161/01.cir.92.7.1954. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 15.Nattel S, Li D, Yue L. Basic mechanisms of atrial fibrillation-very new insights into very old ideas. Annu Rev Physiol. 2000;62:51–77. doi: 10.1146/annurev.physiol.62.1.51. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 16.Ertaş F, Kaya H, Yüksel M, Soydinç MS, Alan S, Ülgen MS. Atrial Fibrillation in Turkey: Epidemiologic Registry (AFTER) study design. Anadolu Kardiyol Derg. 2013;13:339–43. doi: 10.5152/akd.2013.073. [DOI] [PubMed] [Google Scholar]
- 17.Ertaş F, Kaya H, Kaya Z, Bulur S, Köse N, Gül M, et al. Epidemiology of atrial fibrillation in Turkey: preliminary results of the multicenter AFTER study. Turk Kardiyol Dern Ars. 2013;41:99–104. doi: 10.5543/tkda.2013.18488. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 18.Daubert JC, Pavin D, Jauvert G, Mabo P. Intra- and interatrial conduction delay: implications for cardiac pacing. Pacing Clin Electrophysiol. 2004;27:507–25. doi: 10.1111/j.1540-8159.2004.00473.x. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 19.Aytemir K, Özer N, Atalar E, Sade E, Aksöyek S, Övünç K, et al. P wave dispersion on 12-lead electrocardiography in patients with paroxysmal atrial fibrillation. Pacing Clin Electrophysiol. 2000;23:1109–12. doi: 10.1111/j.1540-8159.2000.tb00910.x. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 20.Doğan U, Doğan EA, Tekinalp M, Tokgöz OS, Arıbaş A, Akıllı H, et al. P-wave dispersion for predicting paroxysmal atrial fibrillation in acute ischemic stroke. Int J Med Sci. 2012;9:108–14. doi: 10.7150/ijms.9.108. [CrossRef] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Henry WL, Morganroth J, Pearlman AS, Clark CE, Redwood DR, Itscoitz SB, et al. Relation between echocardiographically determined left atrial size and atrial fibrillation. Circulation. 1976;53:273–9. doi: 10.1161/01.cir.53.2.273. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 22.Asinger RW. Role of transthoracic echocardiography in atrial fibrillation. Echocardiography. 2000;17:357–64. doi: 10.1111/j.1540-8175.2000.tb01151.x. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 23.Simpson RJ, Jr, Amara I, Foster JR, Woelfel A, Gettes LS. Thresholds, refractory periods, and conduction times of the normal and diseased human atrium. Am Heart J. 1988;116:1080–90. doi: 10.1016/0002-8703(88)90163-9. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 24.Platonov PG, Yuan S, Hertervig E, Kongstad O, Roijer A, Vygovsky AB, et al. Further evidence of localized posterior interatrial conduction delay in lone paroxysmal atrial fibrillation. Europace. 2001;3:100–7. doi: 10.1053/eupc.2001.0150. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 25.Kumagai K, Akimitsu S, Kawahira K, Kawanami F, Yamanouchi Y, Hiroki T, et al. Electrophysiological properties in chronic lone atrial fibrillation. Circulation. 1991;84:1662–8. doi: 10.1161/01.cir.84.4.1662. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 26.Deniz A, Yavuz B, Aytemir K, Hayran M, Köse S, Okutucu S, et al. Intra-left atrial mechanical delay detected by tissue Doppler echo-cardiography can be a useful marker for paroxysmal atrial fibrillation. Echocardiography. 2009;26:779–84. doi: 10.1111/j.1540-8175.2008.00881.x. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 27.Ariyarajah V, Puri P, Apiyasawat S, Spodick DH. Interatrial block: a novel risk factor for embolic stroke? Ann Noninvasive Electrocardiol. 2007;12:15–20. doi: 10.1111/j.1542-474X.2007.00133.x. [CrossRef] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Benjamin EJ, D’Agostino RB, Belanger AJ, Wolf PA, Levy D. Left atrial size and the risk of stroke and death. The Framingham Heart Study. Circulation. 1995;92:835–41. doi: 10.1161/01.cir.92.4.835. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 29.Rossi A, Zardini P, Marino P. Modulation of left atrial function by ventricular filling impairment. Heart Fail Rev. 2000;5:325–31. doi: 10.1023/a:1026507128973. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 30.Aydın M, Özeren A, Bilge M, Dursun A, Cam F, Elbey MA. Effects of dipper and non-dipper status of essential hypertension on left atrial mechanical functions. Int J Cardiol. 2004;96:419–24. doi: 10.1016/j.ijcard.2003.08.017. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 31.Spodick DH. Effect of interatrial block on left atrial function. J Cardiol. 2001;38:169–71. [PubMed] [Google Scholar]
- 32.Choi JO, Han H, Cho SJ, Yang JH, Song BG, Lee SY, et al. Reduced peak atrial systolic mitral annular velocity predicts the development of nonvalvular atrial fibrillation. Echocardiography. 2009;26:645–50. doi: 10.1111/j.1540-8175.2008.00858.x. [CrossRef] [DOI] [PubMed] [Google Scholar]


