Abstract
Background
Determination and reporting of disease severity in emergency general surgery (EGS) lacks standardization. Recently, the American Association for the Surgery of Trauma (AAST) proposed an anatomic severity grading system. We aimed to validate this system in patients with appendicitis, and determine if cross sectional imaging correlates with disease severity at operation.
Methods
Patients 18 years or older undergoing treatment for acute appendicitis between 2013 and 2015 were identified. Baseline demographics, procedure types were recorded, and AAST grades were assigned based on intraoperative and radiologic findings. Outcomes including length of stay, 30 day mortality, and complications based on Clavien-Dindo categories and National Surgical Quality Improvement Program variables. Summary statistical univariate, nominal logistic and standard least squares analyses were performed comparing AAST grade with key outcomes. Bland-Altman analysis compared operative findings to preoperative cross sectional imaging to compare assigning grades.
Results
334 patients with mean (±SD) age of 39.3 years (±16.5) were included (53% male) and all patients had cross sectional imaging. 299 underwent appendectomy, and 85% completed laparoscopic. 30 day mortality rate was 0.9%, complication rate 21%. Increased median [IQR] AAST grade was recorded in patients with complications 2 [1-4] compared to those without 1 [1-1], p=0.001. For operative management, a median [IQR] AAST grades were significantly associated with procedure type: laparoscopic 1 [1-1], open 4 [2-5] conversion to open 3 [1-4], p=0.001. Increased median [IQR] AAST grades were significantly associated in non-operative management: patients having a complication had a higher median AAST grade of 4 [3-5], compared to those without 3 [2-3], p=0.001. Bland Altman analysis comparing AAST grade and cross sectional imaging demonstrated no difference; −0.02 ±0.02 p = 0.2 coefficient of repeatability 0.9.
Conclusions
The AAST grading system is valid in our population. Increased AAST grade is associated with open procedures, complications, and length of stay. AAST EGS grade determined by preoperative imaging strongly correlated to operative findings.
Keywords: Emergency General Surgery, Patient outcomes, Quality of care, Staging, Scoring Grading
Introduction
Acute care surgeons manage a broad spectrum of diseases with variable severity. As the disease severity and complexity increases, the ability to prognosticate and counsel patients on risk and of poor outcomes with their specific disease process is limited due to lack of stratification (1). Despite advances in operative technique and imaging for appendicitis, complications (10%) and mortality (1-5%) continue (2). Relying on anatomic information through imaging techniques such as CT and ultrasound (US) is common with high specificity and sensitivity for accuracy in diagnosis (3). Additionally, various scoring systems utilizing (CT) and clinical findings have been proposed to predict complicated appendicitis and, therefore, subsequent treatment (4–7). The pre-operative determination of anatomic severity, and subsequent surgical difficulty, however, remains unclassified (8).
In an effort to standardize emergency general surgery (EGS) disease processes, the American Association for the Surgery of Trauma (AAST) developed a grading system for the uniform assignment of anatomic severity to a variety of EGS diseases (8). This score ranks anatomic criteria on a scale of Grade I (mild) to Grade V (severe) (8). The score was modeled on the Organ Injury Scale (OIS), a commonly utilized system for the classification of anatomic injury severity, which has consistently been shown to correlate well with patient outcomes (9). These detailed categories of anatomic severity were created based on clinical, imaging, endoscopic, operative, and pathologic criteria (8). The AAST suggests that these scoring systems must be validated and their applicability defined for each of the EGS pathologies (8,10,11). Due to the criteria being strongly based on intra-operative findings, these systems cannot be used to determine the need for operative management. If strong correlation of imaging techniques can be demonstrated, then the AAST score can be calculated pre-operatively, potentially allowing surgeons to use the grading system to influence treatment. Validation of the score may also facilitate the standardization of research across institutions, allocation of resource spending, comparison of institution and operator outcomes, and assessment of expected healthcare quality outcomes. Therefore, we had two aims, 1) to determine if preoperative CT findings accurately correlate to intra-operative categorization of the AAST appendicitis grade, and 2) to determine if the AAST EGS grade predicts the type of operative intervention, mortality, duration of stay, and complications. We hypothesize that the correlation coefficient of the imaging-based AAST appendicitis grade (I-AAST) to the intra-operative AAST Appendicitis grade will be greater than 0.80 (Bland-Altman).
Methods
This is a retrospective single institution cohort study undertaken by the authors. Institutional Review Board approval was obtained prior to conducting the study.
Patient inclusion and data collection
Patients aged 18 years or older who presented with acute appendicitis from January 2013 - January 2015 were included. Exclusion criteria included pregnancy and active malignancy, < 18 years of age. Baseline demographic information including patient age, sex, pre-existing conditions based on Charlson comorbidity score (12), complication management based on Clavien-Dindo categorization (13) (Appendix), stress physiology according to sepsis and organ failure guidelines (SOFA score) (14), appendectomy procedure types, and non-operative management types. Outcomes including duration of stay, complication type and rates based on National Surgical Quality Improvement Program variables (15) subsequent interventions (such as reoperation, or image guided intervention), and 30 day mortality were recorded.
I-AAST Grade Assignment
Preoperative cross sectional imaging was reviewed and patients were assigned an I-AAST grade using criteria outlined in Table 1. The I-AAST grades were created to mirror the AAST operative grades. For patients who did not undergo appendectomy, only an I-AAST was calculated. One reviewer (MH) assigned I-AAST grades based on board certified radiologist interpretation of each patient. Patients who underwent non-operative management, and therefore no AAST score was calculable, had their I-AAST compared with duration of stay, presence of complication, and Clavien-Dindo complication grade.
Table 1.
American Association for the Surgery on Trauma Grading System for Anatomic Severity of Disease (8)
| Grade | Image AAST (I-AAST) Description of organ | Operative AAST Description of Appendicitis | N |
|---|---|---|---|
| Normal | Normal appearance, Appendix not visualized without any other abnormality | Normal appendix | 1 (0.002%) |
| Grade I | Appendiceal thickening >6 mm with mild periappendiceal edema | Acutely Inflamed Appendix, Intact | 230 (68.8%) |
| Grade II | Appendiceal thickening >6 mm with severe periappendiceal edema, | Gangrenous Appendix, Intact | 31 (9.3%) |
| Grade III | Appendiceal thickening >6mm, severe periappendiceal thickening with free intra-peritoneal fluid in the right lower quadrant/pelvis | Perforated Appendix with Local Contamination | 30 (9%) |
| Grade IV | Appendiceal thickening >6 mm or non-visualized appendix with abscess or phlegmon | Perforated Appendix with Periappendiceal Phlegmon or Abscess | 36 (10.8%) |
| Grade V | Appendiceal thickening >6 mm or non-visualized appendix with free intra-peritoneal fluid > 1 quadrant | Perforated Appendix with Generalized Peritonitis | 6 (1.8%) |
AAST Appendicitis Grade Assignment
The AAST grade of acute appendicitis was assigned, from grade I (mild) to grade V (severe) (Table 1), for all patients who underwent appendectomy (8). Grade category was used to analyze the relationship between patients undergoing operative intervention to determine if a correlation existed with duration of stay, presence and type of postoperative complication, conversion to open procedure, and Clavien-Dindo complication grade. Two reviewers (MH and AC) independently assigned grades to each patient, during data collection there were no discrepancies. Electronic medical records were reviewed to determine AAST grade based upon operative and pathology report. For any negative appendectomy, a score of zero was assigned.
Summary Statistical Analysis
Summary statistical univariate, nominal logistic, standard least squares and Bland Altman analyses were performed. Kappa coefficient comparing imaging and operative findings to assign AAST grade was performed. All continuous variables were described using means with standard deviations (SD) if normally distributed and medians with inter-quartile ranges if gross skewness was present. Categorical variables were summarized as proportions. All data analyses were performed using JMP (SAS Institute, Inc. Cary NC). Calculated AAST grade based on operative findings was compared with calculated AAST grade (I-AAST) for findings on cross sectional imaging via Bland Altman plot for patients who underwent operative treatment. We utilized GraphPad Prism (GraphPad Software, Inc. La Jolla CA) for all visual graphics.
Results
Overall demographics
A total of 334 patients were identified. All patients had preoperative cross sectional imaging. The population had mean (±SD) age of 39.3 years (±16.5) and 53% were male. 89.5% (299) of patients underwent appendectomy of which 85% were completed laparoscopically (Table 2). The 30-day mortality rate was 0.9% and overall 70 of 334 (21%) patients experienced a complication (Table 2). A single negative laparoscopic appendectomy was performed and graded as a zero. There was 100% concordance between reviewers for assignment of AAST grades.
Table 2.
Distribution of AAST grades, Management Types, and Patient Risk Factors with Appendicitis
| I-AAST grade | Laparoscopic Appendectomy |
Conversion to Open Appendectomy |
Open Appendectomy |
Non- Operative Percutaneous Drainage |
Non- Operative Antibiotic Therapy |
|---|---|---|---|---|---|
| n=284; 85% | n=5; 1.5% | n=10; 3% | n=19; 5.7% | n=16; 4.8% | |
| 0 | 1 | 0 | 0 | 0 | 0 |
| I | 220 | 1 | 3 | 0 | 3 |
| II | 25 | 0 | 0 | 0 | 2 |
| III | 30 | 1 | 2 | 0 | 5 |
| IV | 6 | 1 | 4 | 18 | 6 |
| V | 2 | 2 | 1 | 1 | 0 |
| Age (mean ± SD) | 37.3 ± 15.1 | 53.6 ± 16.5 | 43.7 ± 18.5 | 54.4 ± 22.3 | 50.2 ± 17.7 |
| % Male (53.3%) | 44.9 | 0.6 | 1.5 | 3.6 | 2.7 |
| ASA class | |||||
| 1 | 56 | 1 | 1 | 6 | 5 |
| 2 | 222 | 4 | 9 | 10 | 6 |
| 3 | 6 | 0 | 0 | 3 | 5 |
| 4 | ~ | ~ | ~ | ~ | ~ |
Imaging AAST grade and key outcomes for both operative and non-operative management
Complication type rate, management type and rate, duration of stay, and Clavien-Dindo grade for each AAST grade are reported in Table 2 and 3. A majority of patients had an AAST grade 0, I or II score (78.4%). For the combination of AAST grades (0-II), 11.8% developed a complication. For the combination of AAST grades (III-V) there was a complication rate of 54.2%. Increased median [IQR] AAST grade was recorded in patients with complications 2 [1-4] compared to those without 1 [1-1], p=0.001. Increased median [IQR] AAST grades were significantly associated in non-operative management: patients having a complication had a higher median AAST grade of 4 [3-5], compared to those without 3 [2-3], p=0.001. For the negative appendectomy, the AAST grade was reported as a grade I, however, operative and pathologic findings suggested a normal appendix.
Table 3.
Complication rates by NSQIP classification, duration of stay, and Clavien-Dindo grades for each AAST grade
| AAST Grade | ||||||
|---|---|---|---|---|---|---|
| Outcomes | 0 | I | II | III | IV | V |
| Morbidity n=x;% | n=1; 1.4 | n=29; 41.4 | n=6; 8.6 | n=7; 10 | n=22; 31.5 | n=5; 7.1 |
| Mortality n=x;% | 0 | 0 | 0 | 0 | 0.6 | 0.3 |
| Wound Type (CDC classification) (18) (median [IQR]) | 2 [2-2] | 2 [2-3] | 3 [2-4] | 3 [3-4] | 4 [2-4] | 4 [3-4] |
| Clavien-Dindo Grade (median [IQR]) | 3 [0-3] | 1 [0-1] | 1 [0-1] | 3 [0-3] | 3 [0-4] | 3 [3-4] |
| Duration of Stay in days (median [IQR]) | 0 [0-0] | 1 [0-1] | 1 [0-2] | 2 [1-5] | 4 [2-8] | 8 [5-13] |
| Operative Duration in minutes (median [IQR]) | ~ | 45 [36-56] | 47 [37-60] | 51 [30-77] | 54 [40-116] | 73 [30-117] |
| Charlson Comorbidity Score (median [IQR]) | ~ | 0 [0-1] | 0 [0-1] | 1 [0-2] | 1 [0-2] | 2 [0-5] |
| SOFA Score (median [IQR]) | ~ | 1 [0-1] | 1 [0-1] | 2 [1-3] | 2 [1-3] | 3 [2-5] |
| Morbidity Incidence (NSQIP) | ||||||
| Superficial SSI (n) | ~ | 14 | 3 | 2 | 1 | 1 |
| Deep Incisional SSI (n) | ~ | ~ | ~ | 2 | 1 | 1 |
| Organ Space SSI (n) | ~ | 2 | 1 | 2 | 13 | ~ |
| Wound Disruption (n) | ~ | ~ | ~ | ~ | ~ | 1 |
| Pneumonia (n) | ~ | ~ | ~ | ~ | 2 | 1 |
| Sepsis (n) | ~ | ~ | ~ | ~ | ~ | 1 |
| Pulmonary Embolus (n) | ~ | ~ | 1 | ~ | ~ | ~ |
| UTI (n) | ~ | 2 | ~ | 1 | ~ | ~ |
| Post Operative Hemorrhage (n) | ~ | 4 | ~ | ~ | 3 | ~ |
| Readmission for Pain (n) | ~ | 3 | 1 | ~ | ~ | ~ |
| Antibiotic related infection (C difficile infection) (n) | ~ | 2 | ~ | ~ | 2 | ~ |
| Superficial Hematoma (n) | ~ | 2 | ~ | ~ | ~ | ~ |
AAST Grades in operative management
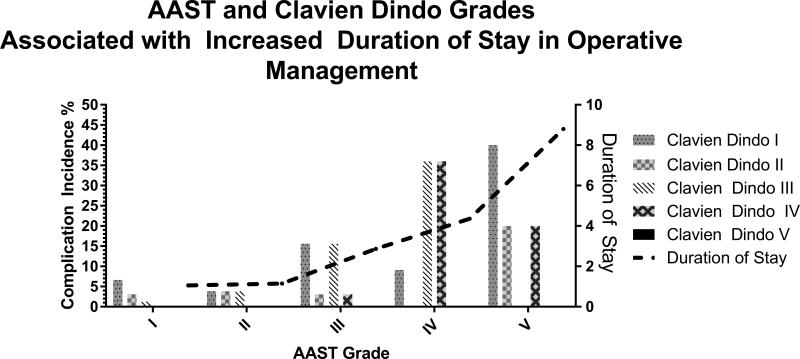
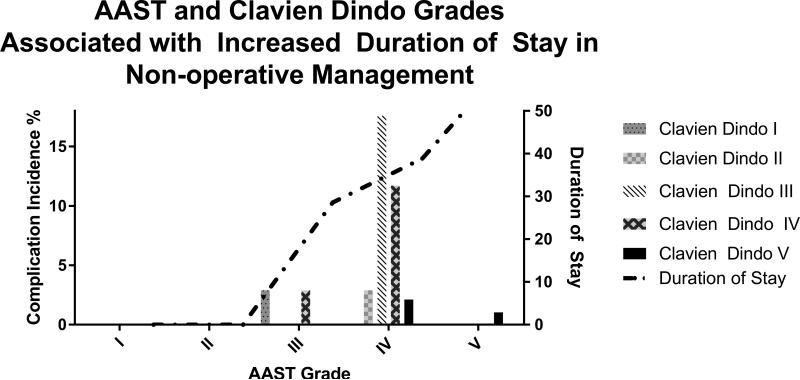
For patients undergoing operative management, increased median [IQR] AAST grades were significantly associated with procedure type: laparoscopic 1 [1-1], open 4 [2-5] conversion to open 3 [1-4], p=0.001. Overall, patients who had a complication had a significantly increased median [IQR] duration of stay compared to those without, 3 [1-7] versus 1 [0-1] days. Figures 2 and 3 demonstrate the increasing incidence of Clavien-Dindo complications based on subsequent therapy and durations of stay with increasing AAST grade.
Figure 2.
AAST and Clavien-Dindo Grades Associated with Increased LOS, who underwent appendectomy.
Figure 3.
AAST and Clavien-Dindo Grades Associated with Increased LOS, who underwent non operative management
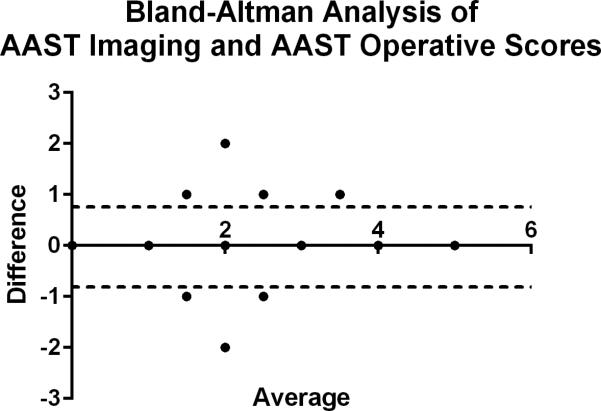
I-AAST versus AAST
The median [IQR] AAST score was 1 [1-1] while the median [IQR] I-AAST score was 1 [1-2]. AAST score strongly correlated with I-AAST grade; Bland Altman analysis comparing the mean differences between I-AAST and AAST grade were −0.02 ±0.02 (p = 0.2) with a coefficient of repeatability of 0.90 (Figure 1). Sensitivity analysis comparing I-AAST grade and operative AAST grade to was performed using an ordinal kappa coefficient. The kappa coefficient was 0.73(95 % CI, 0.64 – 0.81). Furthermore, there was no systematic difference in the assignment of imaging or operative grades as the P value for test of symmetry was 0.98.
Figure 1.
Bland-Altman Analysis Comparing Calculated AAST Operative and Imaging Scores
Discussion
This is the first report validating the AAST EGS grade system for appendicitis. The finding that a high degree of correlation exists between operative AAST grade and I-AAST has significant clinical utility. Currently, the AAST score relies on a variety of operative findings to assign a grade. Knowing that there is strong correlation of the AAST grade at operation compared to the preoperative cross sectional imaging grade allows for the pre-operative use of the scoring system to guide therapy. Additionally, after controlling for age, gender, comorbidities, a worse physiologic status, a greater mean AAST grade in appendicitis is on multivariate nominal logistic regression independently associated with critical outcomes.
As acute care surgeons treat patients with increasingly complex comorbidities concomitant with surgical disease, assigning an individual patient's severity score will become of even more importance for comparison of outcomes. Before this validation of the AAST grading system, there was a lack of standard validated measurements to describe and assess anatomic disease severity. While most surgeons accept that anatomic difficulty is an inherent part of EGS, the lack of standard language in which to communicate this between clinicians and surgeon-scientists has been limiting (8).
Traditionally, differentiating uncomplicated versus complicated appendicitis was performed utilizing history, clinical findings, laboratory data, and cross sectional imaging primarily via the Alvarado and Appendicitis Inflammatory Response (AIR) scores. The Alvarado and AIR scoring systems, however, do not allow for preoperative identification of variable disease states, severity at the time of exploration, and increased likelihood of complications. The AAST for appendicitis grade relies on operative findings. The AAST grade, compared to preoperative diagnostic indices, focuses on integrating multiple findings, most importantly operative, to describe severity. Assigning severity based on anatomic injury is a more logical method to guide therapy particularly if radiologic imaging is supportive. Furthermore, while the AAST EGS grading system incorporates various data, our data suggests that cross sectional imaging at admission can reliably diagnose and be a surrogate for assigning severity via AAST EGS grade. Recent work concluded that utilization of clinical findings or laboratory markers were unreliable to distinguish between complicated and uncomplicated acute appendicitis when compared to use of CT scan (16). Their results underscore the important role of cross sectional imaging for diagnosis and assessment of disease severity in acute appendicitis (16). Similar results were found the APPAC study where no predictive factors were able to account for failure of antibiotic treatment in uncomplicated appendicitis during initial hospitalization (17). Grading the severity of acute appendicitis without imaging appears to be difficult. Our work corroborates findings that complicated appendicitis has high degree of correlation of the AAST grade to I-AAST grade suggests that cross sectional imaging alone may allow for clinical guidance of treatment. For instance, patients with AAST grade IV appendicitis may suggest percutaneous management with antibiotics rather than operative intervention.
Not only do these findings validate the AAST EGS grade for appendicitis and affirm its use for pre-operative management guidance, it raises several important issues. The AAST grade needs to be validated for various EGS diseases. In particular, pathologies with far greater odds of death than appendicitis, such as small bowel obstruction and peptic ulcer disease, may provide sufficient power to validate the AAST grade for an end-point of mortality. Not only is the score a potential benchmark measuring associations between disease grades and subsequent outcomes, it may be utilized as a method of comparing quality of care delivery between operators, hospitals, and healthcare systems. Validated grading systems will provide the edifice for further research and comparability between facilities and institutions. We suggest with further validation of the grading system in the differing EGS pathologies, the feature of the score should be incorporated into an EGS national databank for future research.
Limitations
This paper has several limitations. It is a retrospective review of a single institution's experience. Despite our large catchment area, there is an inherent limitation in the generalizability and subsequent findings presented. We realize this is cohort's size is limited to generate findings necessary for complete validation of the AAST grading system in appendicitis, and our future work with AAST grading will rely on larger multi-institutional data to address this important limitation. All of the patients had cross sectional imaging, which does not occur for many patients in general practice that will often undergo ultrasound imaging or no imaging, in particular younger, male patients. It is possible that a single reviewer interpretation of the radiographic report by the radiologist may introduce possible bias. A great majority of the patients in this cohort had low grade appendicitis as scored by the AAST system confirming that appendicitis is often uncomplicated and that assigning five levels to the disease may not reflect severity wholly as compared to a more discrete scoring system. Additionally, our data set did not have wide variability in patient comorbidity, mortality or physiologic stress, and generalizing this system to a more diverse population may not be possible. A larger, multi-center patient sample size is necessary to determine if the differences and associations seen in anatomic severity in this study truly exist. The formation of an emergency general surgery databank could also aid in developing a more robust method of assessing outcomes in EGS diseases.
Increasing anatomic severity based on the proposed AAST grading system is significantly associated with open procedures, complications, and length of stay. Operative AAST grade has a strong correlation with preoperative imaging AAST grade, which may be predict severity of disease. This data externally validates AAST anatomic grading retrospectively. Further study aimed at validating AAST anatomic grading prospectively and through a multi-institutional study is needed to confirm our results.
Acknowledgments
Patrick Wilson: statistical review
Funding: This publication was made possible by CTSA grant KL2 TR000136 (Zielinski) from the National Center for Advancing Translational Sciences (NCATS), a component of the National Institutes of Health (NIH).
Grant from the National Heart, Lung, and Blood Institute T32 HL105355 (Aho), a component of the National Institutes of Health (NIH). This publication was made possible by CTSA Grant Number UL1 TR000135.
Footnotes
Meetings: This study was presented at the 75th annual meeting of the American Association for the Surgery of Trauma, September 14-17, 2016, in Waikoloa, Hawaii.
Conflicts: No conflicts of interest in the design and reporting of the manuscript.
Author contribution: MCH: study design, data collection, data analysis, interpretation, manuscript writing, and generation of figures. JMA: study design, data analysis, interpretation and manuscript writing and revisions. AC: data collection and manuscript editing. DM: study design and manuscript editing. MZ: study design and manuscript critical revisions. EBH: manuscript revisions
Level of evidence: Level V – Retrospective Study
References
- 1.Neary WD, Prytherch D, Foy C, Hearter BP, Earnshaw JJ. Comparison of different methods of risk stratification in urgent and emergency surgery. Br J Surg. 2007;94:1300–1305. doi: 10.1002/bjs.5809. [DOI] [PubMed] [Google Scholar]
- 2.Masoomi H, Nguyen NT, Dolich MO, Mills S, Carmichael JC, Stamos MJ. Laparoscopic appendectomy trends and outcomes in the United States: Data from the Nationwide Inpatient Sample (NIS), 2004-2011. Am Surg. 2014;80:1074–1077. [PubMed] [Google Scholar]
- 3.Alvarado A. A practical score for the early diagnosis of appendicitis. Ann Emerg. 1985;15(5):557–564. doi: 10.1016/s0196-0644(86)80993-3. [DOI] [PubMed] [Google Scholar]
- 4.Doria AS, Moineddin R, Kellenberger CJ, Epelman M, Beyene J, Schuh S, Babyn PS, Dick PT. US or CT for Diagnosis of Appendicitis in Children and Adults? A Meta-Analysis. Radiology. 2006;241:83–94. doi: 10.1148/radiol.2411050913. [DOI] [PubMed] [Google Scholar]
- 5.Kim TH, Cho BS, Jung JH, Lee MS, Jang JH, Kim CN. Predictive factors to distinguish between patients with noncomplicated appendicitis and those with complicated appendicitis. Ann. Coloproctol. 2015;31:192–197. doi: 10.3393/ac.2015.31.5.192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Atema JJ, van Rossem CC, Leeuwenburgh MM, Stoker J, Boermeester MA. Scoring system to distinguish uncomplicated from complicated acute appendicitis. Br J Surg. 2015:979–990. doi: 10.1002/bjs.9835. [DOI] [PubMed] [Google Scholar]
- 7.Gomes CA, Sartelli M, Di Saverio S, Ansaloni L, Catena F, Coccolini F, Inaba K, Demetriades D, Gomes FC, Gomes CC. Acute appendicitis: proposal of a new comprehensive grading system based on clinical, imaging and laparoscopic findings. World J Emerg Surg. 2015;10:60. doi: 10.1186/s13017-015-0053-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shafi S, Aboutanos M, Brown CV-R, Ciesla D, Cohen MJ, Crandall ML, Inaba K, Miller PR, Mowery NT. Measuring anatomic severity of disease in emergency general surgery. J. Trauma Acute Care Surg. 2014;76:884–7. doi: 10.1097/TA.0b013e3182aafdba. [DOI] [PubMed] [Google Scholar]
- 9.Moore EE, Cogbill TH, Malangoni MA, Jurkovich GJ, Champion HR, Gennarelli TA, McAninch JW, Pachter HL, Shackford SR, Trafton PG. Organ injury scaling, II: Pancreas, duodenum, small bowel, colon, and rectum. J Trauma. 1990;30:1427–9. [PubMed] [Google Scholar]
- 10.Savage SA, Klekar CS, Priest EL, Crandall ML, Rodriguez BC, Shafi S. Validating a new grading scale for emergency general surgery diseases. J Surg Res. 2015;196:264–269. doi: 10.1016/j.jss.2015.03.036. [DOI] [PubMed] [Google Scholar]
- 11.Shafi S, Priest EL, Crandall ML, Klekar CS, Nazim A, Aboutanos M, Agarwal S, Bhattacharya B, Byrge N, Rozycki G. Multicenter validation of American association for the surgery of trauma grading system for acute colonic diverticulitis and its use for emergency general surgery quality improvement program. J Trauma Acute Care Surg. 2015;80:405–411. doi: 10.1097/TA.0000000000000943. [DOI] [PubMed] [Google Scholar]
- 12.Charlton ME, Pompei P, Ales KL, MacKenzi Cr. A new method of classifying prognositc comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 13.Clavien P a, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, de Santibanes E, Pekolj J, Slankamenac K, Makuuchi M. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009;250:187–196. doi: 10.1097/SLA.0b013e3181b13ca2. [DOI] [PubMed] [Google Scholar]
- 14.Bone RC, Balk RA, Cerra FB, Dellinger RP, Fein AM, Knaus WA, Schein RM, Sibbald WJ. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Chest. 1992;101(6):1644–1655. doi: 10.1378/chest.101.6.1644. [DOI] [PubMed] [Google Scholar]
- 15.Khuri SF, Daley J, Henderson W, Hur K, Demakis J, Aust JB, Chong V, Fabri PJ, Gibbs JO, Stremple JF. The Department of Veterans Affairs’ NSQIP: the first national, validated, outcome-based, risk-adjusted, and peer-controlled program for the measurement and enhancement of the quality of surgical care. National VA Surgical Quality Improvement Program. Ann Surg. 1998;228:491–507. doi: 10.1097/00000658-199810000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lietzén E, Mällinen J, Grönroos JM, Rautio T, Paajanen H, Nordstrom P, Aarnio M, Rantanen T, Sand J, Salminen P. Is preoperative distinction between complicated and uncomplicated acute appendicitis feasible without imaging? Surgery. 2016 doi: 10.1016/j.surg.2016.04.021. [DOI] [PubMed] [Google Scholar]
- 17.Salminen P, Paajanen H, Rautio T, Nordstrom P, Aarnio M, Rantanen T, Touminen R, Hurme S, Gronroos JM. Antibiotic Therapy vs Appendectomy for Treatment of Uncomplicated Acute Appendicitis. Jama. 2015;313:2340. doi: 10.1001/jama.2015.6154. [DOI] [PubMed] [Google Scholar]