Abstract
Background and Objectives
The general population and most physicians have implicit racial bias against black adults. Pediatricians also have implicit bias against black adults, albeit less than other specialties. There is no published research on the implicit racial attitudes of pediatricians or other physicians towards children. Our objectives were to compare implicit racial bias towards adults versus children among resident physicians working in a pediatric emergency department (ED), and to assess whether bias varied by specialty (pediatrics, emergency medicine, or other), gender, race, age, and year of training.
Methods
We measured implicit racial bias of residents before a pediatric ED shift using the Adult and Child Race Implicit Association Tests (IATs). Generalized linear models compared Adult and Child IAT scores and determined the association of participant demographics with Adult and Child IAT scores.
Results
Among 91 residents, we found moderate pro-white/anti-black bias on both the Adult (M=0.49, SD=0.34) and Child Race IAT (M=0.55, SD=0.37). There was no significant difference between Adult and Child Race IAT scores (difference=0.06, p=0.15). Implicit bias was not associated with resident demographic characteristics, including specialty.
Conclusions
This is the first study demonstrating that resident physicians have implicit racial bias against black children, similar to levels of bias against black adults. Bias in our study did not vary by resident demographic characteristics, including specialty, suggesting that pediatric residents are as susceptible as other physicians to implicit bias. Future studies are needed to explore how physicians’ implicit attitudes towards parents and children may impact inequities in pediatric healthcare.
Keywords: physician implicit attitudes, racial disparities, racial bias, implicit bias, pediatric healthcare disparities
INTRODUCTION
Achieving health equity is a universal principle of the American Academy of Pediatrics. Yet a large body of research has documented that racial/ethnic disparities in pediatric healthcare are “quite extensive, pervasive, and persistent.”1 Investigating attitudes that physicians have towards black children, including implicitly activated attitudes, is important to advance our understanding of factors that contribute to inequities in the care and outcomes of children.
Implicit biases are unconscious attitudes and beliefs that may influence behaviors such as nonverbal communication, physician perceptions and clinical assessments about patients, and decisions about patient management.2 The Implicit Association Test (IAT) is a validated and reliable tool that has been used to measure implicit racial bias in hundreds of studies across a range of participants.3-5 Research in the general population shows that most Americans have an implicit pro-white/anti-black bias.5,6 Research conducted on over 4,000 healthcare students, trainees, and attending physicians using the Adult Race IAT demonstrates that most healthcare providers also have pro-white/anti-black implicit racial bias, similar to the general population.7-18 While studies show that pediatricians are among those who have implicit bias against black adults,8,19 one study found lower levels of bias among pediatricians compared to other physicians or the general population.8
One limitation of previous research investigating racial bias among pediatricians and other healthcare providers who care for children is that it has largely been limited to the use of adult specific IATs, which does not allow assessment of racial bias towards children. The implicit racial attitudes that physicians, including pediatricians, have towards black children have not been established. The Child Race IAT uses images of black and white children and can therefore assess implicitly activated racial attitudes that individuals have towards children.20
The primary objective of this study was to compare differences in implicit racial attitudes towards adults versus children among residents caring for children in a pediatric emergency department (ED). The secondary objective was to examine whether levels of bias towards adults or children vary by resident demographic characteristics, including race, age, specialty, gender, and training year. We hypothesized that residents would have lower levels of bias on the Child Race IAT compared to the Adult Race IAT. Based on previous research, we further hypothesized that Adult and Child Race IAT scores would be lower among pediatric residents (versus residents of other specialties) and female residents (versus male).8,9
METHODS
Setting, Participants, and Data Collection
We used computer-based instruments to investigate the implicit racial bias of resident physicians working in a pediatric ED. We chose to focus our investigation on the ED because it is a setting characterized by high patient acuity, time pressure, workflow interruptions, patient handoffs, high patient load, and a lack of established doctor-patient relationships. These characteristics may make providers working in the ED more prone to the use of cognitive heuristics, such as implicit racial bias. This was a planned secondary analysis of data from an original study examining the impact of cognitive stressors during an ED shift on levels of physician implicit bias.19 We collected data for the original study from 91 of 106 residents rotating in the ED between April and June 2013. The study was conducted in an urban academic pediatric ED with over 70,000 annual visits, of which 61.5% involve patients who are non-Hispanic white, 33.5% non-Hispanic black, 0.9% Asian, and 0.6% Hispanic. The study site trains over 200 pediatric, emergency medicine, family practice, anesthesia, and transitional year residents from eight different training programs.
Residents completed electronic instruments assessing demographic characteristics (race/ethnicity, age, gender, specialty, training year) and implicit racial bias using both the Adult and Child Race IAT. To meet the objectives of the original study, residents working in the ED completed both pre- and post-shift instruments, and were randomized to complete their first assessment either before (pre-shift) or after (post-shift) a scheduled shift. The pre-shift IAT scores were the first assessment for 47 residents (52%), and second assessment for 44 (48%) residents. Analysis for the current manuscript is limited to pre-shift Adult and Child IAT scores for all 91 residents. This study was approved by the University's Institutional Review Board.
Study Measures
Demographic Characteristics
Residents self-reported their race (response options included American Indian/Alaska Native, Asian, Native Hawaiian or other Pacific Islander, black, white, more than one race - black/white, more than one race - other, and other race), ethnicity (Hispanic or Latino, not Hispanic or Latino, or unknown), age, gender (male or female), specialty, and training year.
Implicit Racial Bias
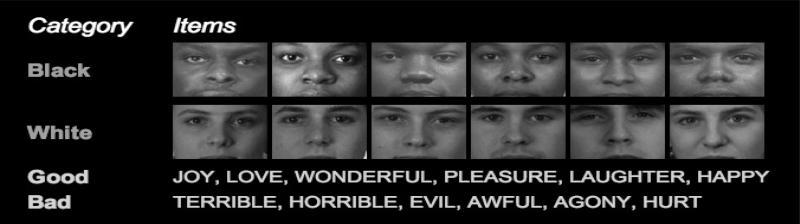
We used the Adult and Child Race IATs to assess implicit bias.3,5,6,21-23 Details about the general IAT procedures, scoring, and psychometric properties have been published.5,6,21,23 Briefly, the IAT requires participants to complete randomized blocks of trials in which they categorize pictures of black and white faces (Figures 1 and 2) while simultaneously categorizing good and bad words. The IAT measures the strength of association between the category of faces (black, white) and the category of words (good, bad) using response latency time and frequency of errors. Participants who categorize white faces (adult or child) more quickly and with fewer errors when they are paired with good (vs. bad) words have an implicit pro-white bias/anti-black. The IAT is a continuous measure ranging from −2 to +2. IATs are scored using the D algorithm, with values ranging from -0.15-0.15 indicating no racial bias; 0.16-0.35, slight pro-white bias; 0.36-0.65, moderate pro-white bias; and >0.65, strong pro-white bias.24 Negative scores indicate pro-black bias of similar magnitudes. IAT demonstrations can be found at https://implicit.harvard.edu/implicit/.
Fig 1.
For the Adult Race Implicit Association Test (IAT) participants categorize pictures of black and white adult faces while simultaneously categorizing good and bad words. The IAT measures the strength of association between the category of faces (black, white) and the category of words (good, bad) using response latency time and frequency of errors.
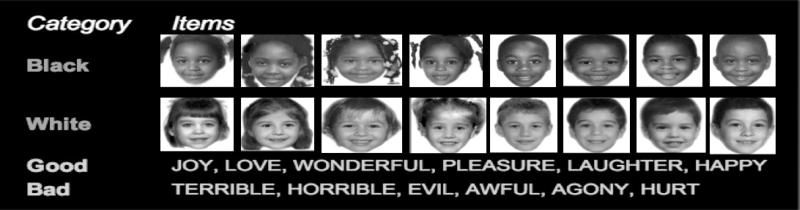
Fig 2.
For the Child Race Implicit Association Test (IAT) participants categorize pictures of black and white child faces while simultaneously categorizing good and bad words. The IAT measures the strength of association between the category of faces (black, white) and the category of words (good, bad) using response latency time and frequency of errors.
The IAT is a well-validated and reliable tool that has been used in hundreds of studies across a range of disciplines,3-5 including healthcare.7-18 For the Child Race IAT, adult facial images (Figure 1) are replaced with images of black and white children (Figure 2), but otherwise uses standard IAT procedures.5,20,25 Although there has been limited published research using the Child Race IAT, between 2001-2004 it was taken by 28,826 visitors to publically available websites featuring 17 different IATs.5 Data on the Child Race IAT reveals strong and robust associations consistent with findings on the Adult Race IAT.5
Statistical Analyses
Descriptive statistics were used to summarize resident demographic characteristics. IATs were scored and categorized using published guidelines.24 Linear models were used to analyze Adult Race, Child Race, and Difference (calculated by subtracting Adult from Child) IAT scores. To take into account potential IAT practice effects based on the repeated measures design of the original study,19 linear models were adjusted for whether residents completed their pre-shift assessments first (N=47) or second (N=44). We also examined the association of resident demographic characteristics (race/ethnicity, age, gender, specialty, and training year) with Adult, Child, and Difference IAT scores using separate linear models, each adjusted for practice effect. Due to small group sizes, physician race was analyzed as a three-category variable consisting of White non-Hispanic; Asian; and other, which included Black Non-Hispanic, Hispanic, and those who identified themselves as more than one race or another race. All analyses were carried out in IBM SPSS 22 (IBM Corp., Armonk, NY). Two-sided p-values < 0.05 were considered to be statistically significant.
RESULTS
Participant demographic characteristics
Of the 91 participants in our sample (Table 1), pediatric residents accounted for the greatest proportion (45%), with the remainder from emergency medicine residency (35%) or other training programs such as family medicine and anesthesiology (19%). Roughly half were females (52%), and most were of non-Hispanic white race (74%), followed by Asian (13%), Hispanic (4%), and non-Hispanic black (1%). Five (6%) residents were from other racial/ethnic groups, including four who reported being more than one race, and two (2%) did not report their race/ethnicity.
Table 1.
| Demographic Characteristics | |
|---|---|
| Race, N (%) | |
| Non-Hispanic White | 67 (74) |
| Non-Hispanic Black | 1 (1) |
| Hispanic | 4 (4) |
| Asian | 12 (13) |
| Other | 5 (6) |
| Unknown c | 2 (2) |
| Age, y, mean (SD) | 28.8 (±2.2) |
| Female gender, N (%) | 47 (52) |
| Specialty, N (%) | |
| Pediatrics | 41 (45) |
| Emergency Medicine | 32 (35) |
| Other d | 17 (19) |
| Unknown | 1(1) |
| Training year, N (%) | |
| 1 | 32 (35) |
| 2 | 34 (37) |
| 3 | 23 (25) |
| 4 | 1 (1) |
| Unknown | 1 (1) |
Abbreviations: y, years; SD, standard deviation
Data are based on surveys of 91 of the 106 residents working in a Pediatric Emergency Department between April to June 2013.
Because of rounding, percentages may not total 100.
Participant did not answer the question.
Other specialties included family medicine and anesthesiology
Implicit racial attitudes towards adults and children
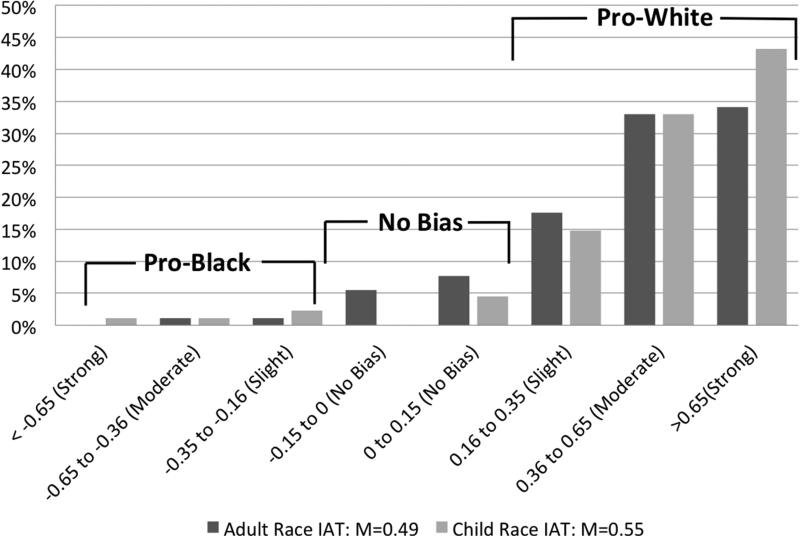
According to standard interpretations of IAT scores,24 we found moderate pro-white/anti-black bias on both the Adult Race (M=0.49, SD=0.34) and Child Race IAT (M=0.55, SD=0.37). There was no significant difference between Adult and Child Race IAT scores (difference=0.06, p=0.15). As shown in Figure 3, most residents had IAT scores consistent with pro-white/anti-black racial bias on both the Adult Race IAT (85%) and Child Race IAT (91%). In linear models adjusting for practice effect, none of the resident characteristics (i.e., specialty, gender, race, age, and training year) were associated with Adult or Child Race IAT scores (Table 2).
Fig 3.
Findings are from assessments of 91 of 106 residents working in a Pediatric Emergency Department between April and June 2013. Figure shows the percentage of residents with each category of IAT score (no, slight, moderate, and strong bias favoring black or white) on the Adult Race and Child Race IAT.
Table 2.
Associations Between Participant Demographic Characteristics with Adult and Child Race Implicit Association Test (IAT) Scores a
| Adult IAT | Child IAT | |||||
|---|---|---|---|---|---|---|
| Resident characteristics | Coefficient | 95% CI | P value | Coefficient | 95% CI | P value |
| Specialty | 0.68 | 0.56 | ||||
| Pediatrics | Ref | Ref | ||||
| Emergency medicine | −0.03 | −0.18, 0.12 | −0.05 | −0.22, 0.12 | ||
| Other | −0.08 | −0.26, 0.10 | −0.11 | −0.32, 0.10 | ||
| Male gender | 0.03 | −0.10, 0.17 | 0.61 | −0.08 | −0.23, 0.08 | 0.33 |
| Race | 0.87 | 0.82 | ||||
| Non-Hispanic White | Ref | Ref | ||||
| Asian | 0.04 | −0.16, 0.24 | 0.07 | −0.15, 0.30 | ||
| Other b | 0.04 | −0.17, 0.25 | 0.01 | −0.23, 0.25 | ||
| Age | 0.01 | −0.02, 0.04 | 0.44 | 0.01 | −0.03, 0.04 | 0.90 |
| Training year | 0.03 | −0.06, 0.11 | 0.54 | −0.02 | −0.11, 0.08 | 0.71 |
Abbreviations: CI, Confidence Interval
Data are based on separate linear models, each adjusted for practice effect of group assignment, to determine if each participant demographic characteristic is associated with Adult Race or Child Race IAT scores.
Includes Non-Hispanic Black (n=1), Hispanic (n=4), and those who identified themselves as another race (n=5).
DISCUSSION
To our knowledge, this is the first study to examine implicit racial attitudes that physicians, including pediatric trainees, have towards black children using the Child Race IAT. Two important findings are evident based on this sample of 91 resident physicians working in a large urban pediatric ED. First, we demonstrate for the first time that physician trainees have implicit racial bias against black children, similar to levels of bias against black adults. These findings suggest that, similar to adult patients, children are potentially vulnerable to implicit racial bias from their healthcare providers. Second, neither Adult Race nor Child Race IAT scores varied by resident demographic characteristics in our study, including specialty. These findings suggest that pediatric residents are equally as susceptible as residents from other specialties to having implicit racial bias towards both adults and children.
We expand prior knowledge about physician implicit bias that used the Adult Race IAT by using the Child Race IAT. Our findings that physicians in training, including pediatric residents, have implicit racial bias towards both adults and children have important implications as physician racial bias has been cited as a factor contributing to healthcare disparities.26 While beyond the scope of this study, other studies have linked higher pro-white/anti-black bias on the Adult Race IAT with poor physician communication during visits12 and poor ratings of care among black patients.12,27 Higher pro-white implicit racial bias is also associated with racial differences in treatment recommendations for chest pain7 and prescribing narcotic analgesics for children with postoperative pain8 in vignette-based studies. Physician implicit bias is also associated with poorer psychosocial health outcomes for patients with spinal cord injury.15 With growing evidence demonstrating racial/ethnic disparities in pediatric healthcare,1 future studies are needed to explore how physicians’ implicit attitudes towards both parents and their children may impact inequities in care.
We limited our investigation to resident physicians given the need to understand racial attitudes of front-line ordering providers. Research has identified factors that impact changes in implicit bias between the first and fourth years of medical school, such as bias training and diversity climate.28 Changes in implicit bias (increased or decreased) over the course of residency training and as attending physicians amass more clinical experience is unknown and warrants further research.
Although we are unaware of any prior studies that have examined the implicit racial bias that physicians have towards children, our findings of pro-white/anti-black bias are similar to studies using the Child Race IAT in other settings.5,20,25 Among people who accessed the Child Race IAT on a publically available IAT demonstration website, there was moderate implicit pro-white/anti-black bias towards children (N=28,816, M=0.33), similar to levels of bias found on the Adult Race IAT (N=732,881, M=0.37).5 Other research using the Child Race IAT among white subjects in child and adult age groups also found implicit bias favoring white children over black children.20,25
Our findings of implicit pro-white/anti-black racial bias using the Child Race IAT are consistent with research indirectly investigating physician bias towards children. During recorded interviews of pediatric acute care office visits, physicians were less likely to ask black children to answer questions during a visit than white children, independent of the child's age and socioeconomic status.29 The authors hypothesized that these disparate interactions were due to physicians attributing less competence to black children than to white children.
Our finding that physicians have implicit pro-white/anti-black racial bias on the Child Race IAT is also consistent with research investigating bias against children in other settings, such as the criminal justice system. For example, in a vignette study among psychology students, black and Hispanic child sexual abuse victims were perceived to be more responsible for their abuse than white victims.30 In another series of studies examining perceptions about the innocence of children, black children were rated as less innocent than white children of similar ages.31 That research also used a Dehumanization IAT to measure the implicit associations between stereotypically black names and names of animals in the great ape category (e.g., gorilla) in a sample of police officers, finding that officers with stronger implicit black-ape associations had a history of using greater force against black children compared to children of other races.31 Our findings thus add to a growing body of research showing that black children are vulnerable to implicit racial bias in multiple settings.
Despite known inequities, bias, and discrimination that black children experience in America, we hypothesized that pediatric residents would have less implicit racial bias, particularly on the Child Race IAT. However, IAT scores in our study did not vary by resident demographic characteristics, including specialty, gender, race, age, or training year. One other group who has published research on implicit racial bias among pediatricians found weak pro-white bias among 43 pediatric residents, fellows, and attending physicians who completed the Adult Race IAT (M=0.18, SD=0.44), which is lower than in other groups of physicians and the general population.8 With respect to gender, although one study found lower IAT scores for female physicians (n=955, M=0.30) compared to male physicians (n=1566, M=0.45),9 gender differences have not been found in other research studies, including ours.7,10-12,16 With regard to physician race, studies using Adult Race IAT scores have shown that black physicians and healthcare students have either no implicit racial bias7,9-12 or slight pro-white bias towards adults.16 Physician race was also not associated with Adult or Child Race IAT scores in our sample. This may be due to few minorities who are underrepresented in medicine, with only 1 non-Hispanic black and 4 Hispanic residents.
With a growing body of evidence documenting the presence of implicit racial bias in the United States and its impact on behaviors, there has been a call for strategies aimed at reducing bias. In a recently published randomized control trial, psychology students were given training on strategies for reducing implicit racial bias, concrete examples of how these strategies could be applied to everyday situations, and asked to generate situations in which they could use such strategies, resulting in long-term reduction of implicit racial bias.32 While this intervention has not yet been tested in the healthcare setting, other interventions have been proposed to mitigate the effects of implicit provider racial bias on healthcare disparities.33-39 Examples include using positive image priming to counter automatic stereotyping.33-35
LIMITATIONS
An important limitation to consider is that this study was conducted at a single institution, which may limit the generalizability of our results. However, our findings of pro-white bias on both the Adult and Child Race IATs are consistent with research in other populations, including health professionals.5,7-18,20,25 Also, although we had a high response rate, with enrollment of 91 of 106 of residents working in the ED during the study period, we acknowledge the relatively small sample size. Our sample also included few underrepresented minority physicians (1 black, 4 Hispanic); however, this reflects the lack of racial/ethnic diversity in the US physician workforce. We limited our investigation to resident physicians, which limits the generalizability of our results to more experienced physicians.
We chose to limit our investigation of racial attitudes to white and black races because 95% of the patients served by the study site are white or black. However, disparities in care have been described for other minority populations. Future studies should investigate if physicians have similar implicit bias against children of other races or ethnicities. Based on our study design, we were not able to determine how implicit racial bias towards children impacts physician behaviors, and this represents an important area of future research.
Despite the stated limitations, strengths of our study include a high response rate of 86%, and use of well-validated instruments that measure implicit bias. Also, unlike other research on implicit bias of physicians, we investigated racial attitudes towards both adults (parents) and children (pediatric patients), which is important to further our understanding of pediatric healthcare disparities.
CONCLUSION
We provide new evidence that resident physicians in our sample, including pediatric trainees, have similar levels of bias towards children and adults. Racial attitudes towards children and their parents should be taken into consideration in future studies that seek to understand how bias impacts the care of pediatric patients. Researchers have argued that individuals must first become aware of their biases in order to eliminate them.32,40,41 Therefore, physicians caring for children should be made aware of implicit racial biases they may have against black patients and parents.
What's New?
Physicians have similar levels of implicit racial bias towards children and adults. With growing evidence of pediatric healthcare disparities, it is important to explore physicians’ implicit attitudes towards both parents and their children, which may impact healthcare equity.
ACKNOWLEDGMENTS
Thank you to Dennis Durbin, MD, MSCE from the Children's Hospital of Philadelphia for his critical review of the manuscript.
Funding/Support: This research was supported by grants from the Agency for Healthcare Research and Quality (T32 HS 017587), the National Heart Lung and Blood Institute (K12 HL109009), the Robert Wood Johnson Foundation Harold Amos Medical Faculty Development Program (RWJF AMFDP 72430), and The National Institutes of Health (UL1-TR-000005). The sponsoring agencies had no role in the design and conduct of the study; in the collection, management, analysis, and interpretation of the data; or in the preparation, review, or approval of the manuscript. The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the sponsoring agency.
Abbreviations
- CI
Confidence Interval
- ED
emergency department
- IAT
Implicit Association Tests
- M
mean
- SD
standard deviation
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The authors have no conflicts of interest relevant to this article to disclose.
References
- 1.Flores G. Technical report--racial and ethnic disparities in the health and health care of children. Pediatrics. 2010 Apr;125(4):e979–e1020. doi: 10.1542/peds.2010-0188. [DOI] [PubMed] [Google Scholar]
- 2.Greenwald A, Banaji MR. Implicit social cognition: attitudes, self-esteem, and stereotypes. Psychological Review. 1995;102(1):4–27. doi: 10.1037/0033-295x.102.1.4. [DOI] [PubMed] [Google Scholar]
- 3.Greenwald AG, Poehlman TA, Uhlmann EL, Banaji MR. Understanding and using the Implicit Association Test: III. Meta-analysis of predictive validity. J Pers Soc Psychol. 2009 Jul;97(1):17–41. doi: 10.1037/a0015575. [DOI] [PubMed] [Google Scholar]
- 4.Wittenbrink B, Schwarz N. Implicit measures of attitudes. Guilford Press; New York: 2007. [Google Scholar]
- 5.Lane KA, Banaji MR, Nosek BA, Greenwald AG. Understanding and using the implicit association test: IV What we know (so far) about the Method. In: Wittenbrink B, Schwarz N, editors. Implicit measures of attitudes. The Guilford Press; 2007. [Google Scholar]
- 6.Nosek BA, Greenwald AG, Banaji MR. The Implicit Association Test at age 7: A methodological and conceptual review. Psychology Press; 2007. pp. 265–292. [Google Scholar]
- 7.Green AR, Carney DR, Pallin DJ, et al. Implicit bias among physicians and its prediction of thrombolysis decisions for black and white patients. J Gen Intern Med. 2007 Sep;22(9):1231–1238. doi: 10.1007/s11606-007-0258-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sabin JA, Rivara FP, Greenwald AG. Physician implicit attitudes and stereotypes about race and quality of medical care. Med Care. 2008 Jul;46(7):678–685. doi: 10.1097/MLR.0b013e3181653d58. [DOI] [PubMed] [Google Scholar]
- 9.Sabin J, Nosek BA, Greenwald A, Rivara FP. Physicians' implicit and explicit attitudes about race by MD race, ethnicity, and gender. J Health Care Poor Underserved. 2009 Aug;20(3):896–913. doi: 10.1353/hpu.0.0185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.White-Means S, Zhiyong D, Hufstader M, Brown LT. Cultural competency, race, and skin tone bias among pharmacy, nursing, and medical students: implications for addressing health disparities. Med Care Res Rev. 2009 Aug;66(4):436–455. doi: 10.1177/1077558709333995. [DOI] [PubMed] [Google Scholar]
- 11.Haider AH, Sexton J, Sriram N, et al. Association of unconscious race and social class bias with vignette-based clinical assessments by medical students. Jama. 2011 Sep 7;306(9):942–951. doi: 10.1001/jama.2011.1248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cooper LA, Roter DL, Carson KA, et al. The associations of clinicians' implicit attitudes about race with medical visit communication and patient ratings of interpersonal care. Am J Public Health. 2012 May;102(5):979–987. doi: 10.2105/AJPH.2011.300558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Blair IV, Havranek EP, Price DW, et al. Assessment of biases against Latinos and African Americans among primary care providers and community members. Am J Public Health. 2013 Jan;103(1):92–98. doi: 10.2105/AJPH.2012.300812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Oliver MN, Wells KM, Joy-Gaba JA, Hawkins CB, Nosek BA. Do physicians' implicit views of African Americans affect clinical decision making? J Am Board Fam Med. 2014 Mar-Apr;27(2):177–188. doi: 10.3122/jabfm.2014.02.120314. [DOI] [PubMed] [Google Scholar]
- 15.Hausmann LR, Myaskovsky L, Niyonkuru C, et al. Examining implicit bias of physicians who care for individuals with spinal cord injury: A pilot study and future directions. J Spinal Cord Med. 2015;38(1):102–110. doi: 10.1179/2045772313Y.0000000184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Haider AH, Schneider EB, Sriram N, et al. Unconscious race and class bias: its association with decision making by trauma and acute care surgeons. J Trauma Acute Care Surg. 2014 Sep;77(3):409–416. doi: 10.1097/TA.0000000000000392. [DOI] [PubMed] [Google Scholar]
- 17.Penner LA, Dovidio JF, West TV, et al. Aversive Racism and Medical Interactions with Black Patients: A Field Study. J Exp Soc Psychol. 2010 Mar 1;46(2):436–440. doi: 10.1016/j.jesp.2009.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sabin JA, Greenwald AG. The influence of implicit bias on treatment recommendations for 4 common pediatric conditions: pain, urinary tract infection, attention deficit hyperactivity disorder, and asthma. Am J Public Health. 2012 May;102(5):988–995. doi: 10.2105/AJPH.2011.300621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Johnson TJ, Hickey RW, Switzer GE, et al. The Impact of Cognitive Stressors in the Emeregency Department on Physician Implicit Racial Bias. Acad Emerg Med. 2016 doi: 10.1111/acem.12901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Baron AS, Banaji MR. The development of implicit attitudes. Evidence of race evaluations from ages 6 and 10 and adulthood. Psychol Sci. 2006 Jan;17(1):53–58. doi: 10.1111/j.1467-9280.2005.01664.x. [DOI] [PubMed] [Google Scholar]
- 21.Greenwald AG, McGhee DE, Schwartz JL. Measuring individual differences in implicit cognition: the implicit association test. J Pers Soc Psychol. 1998 Jun;74(6):1464–1480. doi: 10.1037//0022-3514.74.6.1464. [DOI] [PubMed] [Google Scholar]
- 22.Nosek BA, Smyth FL. A multitrait-multimethod validation of the Implicit Association Test: implicit and explicit attitudes are related but distinct constructs. Exp Psychol. 2007;54(1):14–29. doi: 10.1027/1618-3169.54.1.14. [DOI] [PubMed] [Google Scholar]
- 23.Nosek BA, Greenwald AG, Banaji MR. Understanding and using the Implicit Association Test: II. Method variables and construct validity. Pers Soc Psychol Bull. 2005 Feb;31(2):166–180. doi: 10.1177/0146167204271418. [DOI] [PubMed] [Google Scholar]
- 24.Greenwald AG, Nosek BA, Banaji MR. Understanding and using the implicit association test: I. An improved scoring algorithm. J Pers Soc Psychol. 2003 Aug;85(2):197–216. doi: 10.1037/0022-3514.85.2.197. [DOI] [PubMed] [Google Scholar]
- 25.Newheiser AK, Olson KR. White and Black American Children's Implicit Intergroup Bias. J Exp Soc Psychol. 2012 Jan;48(1):264–270. doi: 10.1016/j.jesp.2011.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Smedley BD SA, Nelson A. Unequal Treatment: confronting Racial and Ethnic Disparities in Health Care. National Academies Press; Washington, DC: 2002. [PubMed] [Google Scholar]
- 27.Blair IV, Steiner JF, Fairclough DL, et al. Clinicians' implicit ethnic/racial bias and perceptions of care among black and latino patients. Ann Fam Med. 2013 Jan-Feb;11(1):43–52. doi: 10.1370/afm.1442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.van Ryn M, Hardeman R, Phelan SM, et al. Medical School Experiences Associated with Change in Implicit Racial Bias Among 3547 Students: A Medical Student CHANGES Study Report. J Gen Intern Med. 2015 Dec;30(12):1748–1756. doi: 10.1007/s11606-015-3447-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Stivers T, Majid A. Questioning children: interactional evidence of implicit bias in medical interviews. Social Psychology Quarterly. 2007;70(4):424–441. [Google Scholar]
- 30.Bottoms BL, Davis SL, Epstein MA. Effects of Victim and Defender Race on Jurors' Decisions in Child Sexual Abuse Cases. Journal of Applied Social Psychology. 2004;34(1):1–33. [Google Scholar]
- 31.Goff PA, Jackson MC, Di Leone BA, Culotta CM, DiTomasso NA. The essence of innocence: consequences of dehumanizing Black children. J Pers Soc Psychol. 2014 Apr;106(4):526–545. doi: 10.1037/a0035663. [DOI] [PubMed] [Google Scholar]
- 32.Devine PG, Forscher PS, Austin AJ, Cox WT. Long-term reduction in implicit race bias: A prejudice habit-breaking intervention. J Exp Soc Psychol. 2012 Nov;48(6):1267–1278. doi: 10.1016/j.jesp.2012.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Blair IV, Steiner JF, Havranek EP. Unconscious (implicit) bias and health disparities: where do we go from here? Perm J. Spring. 2011;15(2):71–78. doi: 10.7812/tpp/11.979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Blair IV, Ma JE, Lenton AP. Imagining stereotypes away: the moderation of implicit stereotypes through mental imagery. J Pers Soc Psychol. 2001 Nov;81(5):828–841. doi: 10.1037//0022-3514.81.5.828. [DOI] [PubMed] [Google Scholar]
- 35.Dasgupta N, Greenwald AG. On the malleability of automatic attitudes: combating automatic prejudice with images of admired and disliked individuals. J Pers Soc Psychol. 2001 Nov;81(5):800–814. doi: 10.1037//0022-3514.81.5.800. [DOI] [PubMed] [Google Scholar]
- 36.Burgess DJ, Warren J, Phelan S, Dovidio J, van Ryn M. Stereotype threat and health disparities: what medical educators and future physicians need to know. J Gen Intern Med. 2010 May;25(Suppl 2):S169–177. doi: 10.1007/s11606-009-1221-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cohen GL, Garcia J, Apfel N, Master A. Reducing the racial achievement gap: a social-psychological intervention. Science. 2006 Sep 1;313(5791):1307–1310. doi: 10.1126/science.1128317. [DOI] [PubMed] [Google Scholar]
- 38.Cohen GL, Garcia J, Purdie-Vaughns V, Apfel N, Brzustoski P. Recursive processes in self-affirmation: intervening to close the minority achievement gap. Science. 2009 Apr 17;324(5925):400–403. doi: 10.1126/science.1170769. [DOI] [PubMed] [Google Scholar]
- 39.Miyake A, Kost-Smith LE, Finkelstein ND, Pollock SJ, Cohen GL, Ito TA. Reducing the gender achievement gap in college science: a classroom study of values affirmation. Science. 2010 Nov 26;330(6008):1234–1237. doi: 10.1126/science.1195996. [DOI] [PubMed] [Google Scholar]
- 40.Plant EA, Devine PG. The active control of prejudice: unpacking the intentions guiding control efforts. J Pers Soc Psychol. 2009 Mar;96(3):640–652. doi: 10.1037/a0012960. [DOI] [PubMed] [Google Scholar]
- 41.Chapman EN, Kaatz A, Carnes M. Physicians and implicit bias: how doctors may unwittingly perpetuate health care disparities. J Gen Intern Med. 2013 Nov;28(11):1504–1510. doi: 10.1007/s11606-013-2441-1. [DOI] [PMC free article] [PubMed] [Google Scholar]