Abstract
A 77-year-old woman developed dyspnea over three years which occurred during sitting, standing or walking. Her physical examination, chest X-ray, ECG and cardiac catheterization results were all normal. A marked fall in arterial oxygen saturation was observed on sitting or standing. Transesophageal echocardiography showed an increase of right to left shunt flow on sitting. The patient was diagnosed with platypnea-orthodeoxia syndrome and underwent the surgical closure of an atrial septal defect of 19 mm in diameter. After the surgery, the patient's POS symptoms were completely resolved. She was discharged and followed at the outpatient clinic. Her post-treatment course was uneventful.
Keywords: dyspnea, atrial septal defect, right-to-left shunt, elongated aorta
Introduction
Platypnea-orthodeoxia (POS) is a disease that is characterized by dyspnea and hypoxemia, which appear during sitting or standing (1,2). Mechanistically, an intra-pulmonary atrial-venous shunt or right-to-left atrial shunt is thought to increase during standing or sitting, thus resulting in hypoxemia (3-5). A small number of cases of POS in patients with an occult atrial septal defect (ASD) have been reported and successfully treated in Japan (6-9).
We encountered a 77-year-old woman with POS who had an ASD and an elongated aorta. The POS symptoms were induced upon sitting or standing. Increased right to left atrial shunt flow was confirmed by transesophageal echocardiography. The surgical closure of the ASD was effective for resolving the symptoms of POS.
Case Report
A 77-year-old woman visited our hospital due to dyspnea. Her symptoms developed over three years and occurred during sitting, standing or walking. She was a mother of two children and had no heart or lung disease. She developed a vertebral compression fracture at 73 years of age and was hospitalized for a brain abscess at 74 years of age. She had no relevant family history.
The examination upon admission
The patient was 153 cm tall and weighed 59 kg, her body temperature was 36.7°C, her blood pressure was 140/80 mmHg (systolic and diastolic), and her heart rate was 95 beats per minute. The physical examination indicated no abnormalities. We did not observe neck vein dilatation or peripheral edema.
A chest X-ray revealed no lung abnormalities and a normal cardiac silhouette (Fig. 1A). Her electrocardiography (ECG) showed a normal sinus rhythm with normal atrio-ventricular conduction and a normal QTc interval. Counterclockwise rotation was observed in the precordial leads (Fig. 1B). Echocardiography showed that the patient's cardiac function and cardiac structure were normal; no shunt flow was noted.
Figure 1.
The chest X-ray upon admission. A: The chest X ray film showed normal lungs and a normal cardiac silhouette. B: ECG showed a normal sinus rhythm with normal atrio-ventricular conduction, a normal QRS width and a normal QT interval: 200 ms, 80 ms and 436 ms1/2, respectively. Counterclockwise rotation is visible.
Her blood chemistry and serology results were normal, as were her total blood counts. Her peripheral oxygen saturation was 92-93%, and her N-terminal pro-brain natriuretic peptide (NT-proBNP) was slightly elevated to 168 pg/mL.
The patient's course during hospitalization
Cardiac catheterization was performed soon after the patient's admission, but it showed normal pressure tracings. The cardiac wall motion and anatomy were also normal. Angiography of the coronary artery and left ventricle revealed normal findings. The patient's oxygen saturation was within the normal range in each chamber (Table 1).
Table 1.
Catheterization Data.
| Sampling site | Pressure (mean) (mmHg) |
O2 saturation (%) |
|---|---|---|
| Superior vena cava | 12/7 (8) | 73.5 |
| Inferior vena cava | 10/8 (9) | 73.4 |
| Right atrium | 10/6 (8) | 71.4 |
| Right ventricle | 28/0 (10) | 68.1 |
| Pulmonary artery | 28/10 (18) | 71.0 |
| Left ventricle | 142/0 (10) | 96.4 |
| Aorta | 140/80 (90) | 96.4 |
Because POS was suspected on the basis of her history, the patient's oxygen saturation was re-measured in different postures. The oxygen saturation was observed to markedly decrease when the patient changed from the supine position to a sitting or standing position (Fig. 2). Lung perfusion scintigraphy indicated a >20% right-to-left shunt.
Figure 2.
A marked decrease in the oxygen saturation was observed when the patient changed to a sitting position from a supine position (red line). After the surgical closure of the ASD, her symptoms were cleared and the oxygen saturation no longer decreased (blue line).
To demonstrate the right to left shunt, normal saline shaken with air was rapidly intravenously injected under transthoracic echocardiography. Bubbles appeared in the left atrium within 3 heart beats after reaching the right atrium when the patient was in a sitting position; however, this process was not observed when the patient was in the supine position. It was difficult to obtain the usual four-chamber view with transesophageal echocardiography but the procedure showed a small ASD with a slight right to left shunt flow, even when the patient was in the supine position. The shunt flow increased when the patient changed to a sitting position, flowing from the inferior vena cava directly to the ASD (Fig. 3). Computed tomography (CT) showed the elongation of the aorta, which was compressing the right atrium and the right ventricle and distorting the heart position (Fig. 4).
Figure 3.
Transesophageal echocardiography. A typical four-chamber view was difficult to obtain, but a shunting flow was observed through the atrial septum when the patient was in the supine position. The flow increased upon the assumption of a sitting position. The blood appeared to be flowing directly from the inferior vena cava to the ASD.
Figure 4.
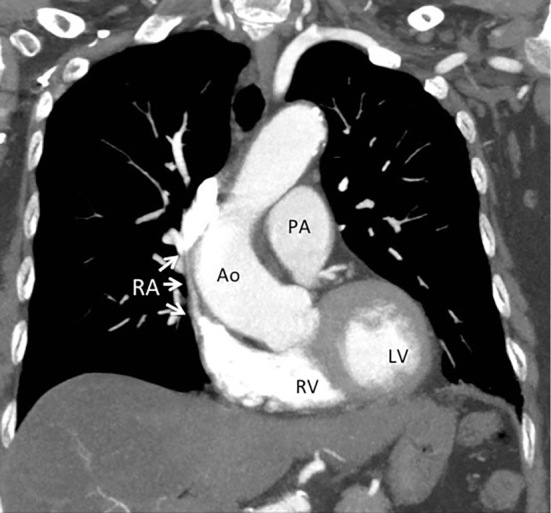
Chest computed tomography (CT). Chest CT showed the elongation of the aorta, which caused the compression of the right atrium and ventricle. A trans-section view of the left ventricular cavity was obtained in the coronary view and revealed the abnormal position of the left ventricle due to the elongated aorta.
Re-catheterization was performed to close the ASD. The pressure tracings were normal in the atria and ventricles and the pressure of the right atrium never exceeded the left atrial pressure. The ASD was estimated to be 8-9 mm in diameter. Because of the crooked atrial septum, trans-catheter closure was abandoned. The surgical closure of the ASD was performed, but the elongated aorta was not corrected. At the time of surgery, the maximal diameter of the ASD was 19 mm.
After surgery, the patient's POS symptoms were completely resolved, and her oxygen saturation no longer decreased during sitting or standing (Fig. 2). The patient was discharged and was followed up at the outpatient clinic, but there were no further events.
Discussion
A 77-year-old woman developed typical symptoms of POS (dyspnea during standing or exertion). Catheterization, when the patient was in the supine position, revealed no sign of congestion or shunting. An increase in the right to left shunt through the ASD, when the patient was in a sitting position, was confirmed by transesophageal echocardiography, and a decrease in the arterial O2 saturation was observed. The CT showed elongation of the aorta that compressed the right side of the heart and displaced the entire heart. The ASD was surgically closed without the correction of the elongated aorta, and the patient showed a full improvement.
POS can occur due to intracardiac shunts, pulmonary areteriovenous shunts or ventilation/perfusion mismatch in the lung (1,2). Rodrigues et al. (10) collected 188 patients with POS caused by interatrial right to left shunts. Among them, patent foramen ovale (PFO) was the main cause of interatrial shunts (88.3%), and ASDs and atrial septal aneurysms were observed in 19.5% and 14.3% of the patients, respectively. Table 2 shows a summary of the POS cases with ASD that have been reported in Japan (6-9). The number of cases is limited either due to the rarity of POS cases with ASD or because many cases have not been reported.
Table 2.
POS Cases Due to ASD Reported in Japan.
| Reference No. | Age (years) |
Gender | Diagnosis | Treatment | Outcome |
|---|---|---|---|---|---|
| 6 | 75 | M | ASD, elongated Ao. | Surgery | Improved |
| 7 | 79 | F | ASD | Catheter | Improved |
| 8 | 79 | F | ASD | Catheter | Improved |
| 9 | 76 | M | ASD, Pneumonitis | Observation | No change |
| Present case | 77 | F | ASD, elongated Ao. | Surgery | Improved |
*: Written in Japanese. M: male, F: female, ASD: atrial septal defect, Ao: aorta
All of the cases displayed characteristic POS symptoms that occurred during sitting or standing and which were aggravated during exercise. Patients with POS may visit cardiologists; however, a physical examination usually reveals normal results and catheterization may reveal apparently normal findings, including normal pressure tracings and normal coronary arteries with no sign of congestive heart failure.
Attention to a patient's history would provide important clues for the diagnosis of POS. Dyspnea and a decrease in the arterial oxygen saturation upon the assumption of a sitting or standing position is a characteristic of POS (Fig. 2). A transesophageal echocardiography is crucial for confirming an increase in the right to left shunt through the ASD (Fig. 3). The patient had a history of a brain abscess, which might have occurred due to the paradoxical shunt through the ASD, but no further examinations were performed at that time.
Since interatrial right-to-left shunts due to PFO or ASD occur without the elevation of the right atrial pressure, additional factors are considered to be involved. Among the 188 patients, Rodrigues et al. observed aortic dilatation, aneurysm or distortion in 23.4% (10). Eicher et al. (11) observed aortic dilatation in 16 of the 19 POS patients (63%). Excessive elongation of the aorta, aortic root dilatation or aortic aneurysm was considered to induce changes in the conformation, size and mobility of the atrial septum, and to potentiate the right-to-left shunts (12-15). In the present case, the elongated aorta was compressing the atrium and the right ventricle and altering the heart position, which resulted in counterclockwise rotation and lifted the heart apex (Fig. 4). During sitting or standing, the ASD is considered to face directly toward the inferior vena cava, resulting in an increased right-to-left atrial shunt (Fig. 3). The mechanism of aortic elongation remains unknown. However, the present patient had a compression fracture of the vertebrae, which might have resulted in the relative elongation of the aorta and a distortion of the heart geometry and position.
Most POS patients with interatrial shunts have been successfully treated by percutaneous closure of the PFO or ASD (7,8,10-12); catheterization is the first-line approach. However, we abandoned the trans-catheter technique due to the deformation of the atrial septum, and treated the patient surgically.
The concomitant correction of the elongated aorta has been reported in cases of POS with PFO (16,17); however, the closure of the ASD alone resulted in the complete resolution of the POS symptoms of the patient in the present case.
The patient's dyspnea during standing or exertion led to the diagnosis of POS. A careful assessment of the patient's history and the demonstration of a decrease in the arterial O2 saturation and an increase in the right to left shunt through the ASD by transesophageal echocardiography were essential for the diagnosis. Closure of the ASD improved her symptoms.
The authors state that they have no Conflict of Interest (COI).
References
- 1. Burchell HB, Helmholz HF Jr, Wood EH. Reflex orthostatic dyspnea associated with pulmonary hypotension. Am J Physiol 159: 563-564, 1949. [Google Scholar]
- 2. Cheng TO. Platypnea-orthodeoxia syndrome: Etiology, differential diagnosis, and management. Cathet Cardiovasc Interv 47: 64-66, 1999. [DOI] [PubMed] [Google Scholar]
- 3. Zanchetta M. A mystery featuring right-to-left shunting despite normal intracardiac pressure. Chest 128: 998-1002, 2005. [DOI] [PubMed] [Google Scholar]
- 4. Laybourn KA, Martin ET, Cooper RA, Holman WL. Platypnea and orthodeoxia: shunting associated with an aortic aneurysm. J Thorac Cardiovasc Surg 113: 955-956, 1997. [DOI] [PubMed] [Google Scholar]
- 5. Levin AR, Spach MS, Boineau JP, Canent RV Jr, Capp MP, Jewett PH. Atrial pressure flow dynamics and atrial septal defects (secundum type). Circulation 37: 476-488, 1968. [DOI] [PubMed] [Google Scholar]
- 6. Hirai N, Fukunaga T, Kawano H, et al. Platypnea-orthodeoxia syndrome with atrial septal defect. Circulation J 67: 172-175, 2003. [DOI] [PubMed] [Google Scholar]
- 7. Ohfuji T, Obase Y, Ikeda M, et al. A case of platypnea orthodeoxia syndrome; A presistent history taking was the key to the diagnosis. Intern Med 51: 1701-1704, 2012. [DOI] [PubMed] [Google Scholar]
- 8. Takiguchi H, Niimi K, Aoki T, et al. Platypnea-orthodeoxia syndrome caused by a latent atrial septal defect. Intern Med 52: 1809-1811, 2013. [DOI] [PubMed] [Google Scholar]
- 9. Ishiguro T, Takayanagi N, Yamamoto M, et al. A case of platypnea-orthodeoxia syndrome due to atrial septal defect. J Jpn Respirat 3: 287-292, 2014. (in Japanese, Abstract in English). [Google Scholar]
- 10. Rodrigues P, Palma P, Sousa-Pereira L. Platypnea-othodeoxia syndrome in review: defining a new disease? Cardiology 123: 15-23, 2012. [DOI] [PubMed] [Google Scholar]
- 11. Eicher JC, Bonniaud P, Baudouin N, et al. Hypoxaemia associated with an enlarged aortic root: a new syndrome? Heart 91: 1030-1035, 2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Townsend Rda S, Costa MAL, Gib MC, Neto FLD. Platypnea-orthodeoxia syndrome in patients presenting enlarged aortic root: case report and literature review. Rev Bras Ter Intensiva 26: 313-316, 2014. (in English, Portuguese, Abstract in English). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Bertaux G, Eicher JC, Petit A, Dobsak P, Wolf JE. Anatomic interaction between the aortic root and the atrial septum: a prospective echocardiographic study. J Am Soc Echocardiogr 20: 409-414, 2007. [DOI] [PubMed] [Google Scholar]
- 14. Laybourn KA, Martin ET, Cooper RA, Holman WL. Platypnea and orthodeoxia: Shunting associated with an aortic aneurysm. J Thorac Cardiovasc Surg 113: 955-956, 1997. [DOI] [PubMed] [Google Scholar]
- 15. Popp G, Melek H, Garnett AR Jr. Platypnea-orthodeoxia related to aortic elongation. Chest 112: 1682-1684, 1997. [DOI] [PubMed] [Google Scholar]
- 16. Takashima N, Suzuki T, Asai T, Hosoda S. Successful surgical repair of platypnea-orhtodeozia syndrome in a patient with cerebral infarction. Interact Cardiovasc Thorac Surg 15: 178-180, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hojo H, Ogiwara M, Kyo S. A case of platypnea-orthodeoxia syndrome caused by patent foramen ovale. J Jpn Cardiovasc Sur 36: 68-71, 2007. (in Japanese, Abstract in English). [Google Scholar]





