Abstract
Ischemic priapism (IP) is a urological emergency that requires early intervention in order to prevent irreversible structural and functional changes. The purpose of penile shunt surgery is to passage out ischemic blood in the corpus cavernosum (CC), restoring the normal circulation within these structures. Here, we present our first experience using modification of Al-Ghorab shunt procedure to treat severe and prolonged IP. The Al-Ghorab shunt procedure was modified by the retrograde insertion of a 7/8 Hegar dilator into the opening of the distal cavernous tissue via the original Al-Ghorab incision. Priapism was successfully relieved, and no recurrent IP was reported.
Keyword: Al-Ghorab shunt, Intracorporeal dilatation, Ischemic priapism, Winter procedure
Introduction
Ischemic priapism (IP) is a urological emergency which requires early intervention in order to prevent irreversible structural and functional changes. Nowadays, the management of IP principally occurs in a step-wise fashion aimed to achieve detumescence as quickly as possible. The first-line treatment to manage IP is aspiration of corpus cavernosum (CC). Patients who failed this first-line therapy require surgical intervention in the form of penile shunt surgery.1 Adequate shunt for the treatment of prolonged IP is hard to achieve.2 Here, we report the use of a modified Al-Ghorab shunt procedure, using intracorporeal dilatation to facilitate evacuation of clotted blood from the CC in a patient with severe and prolonged IP, for which we report good results.
Case presentation
A 35-year-old man arrived at the emergency room with a painful penile erection that had lasted for 5 days. The erection was not associated with sexual stimuli, administration of intracavernous drugs, or genital or perineal trauma. The patient had been diagnosed with chronic myelogenous leukemia one month earlier, and his medications included hydroxyurea, folic acid, sodium bicarbonate and allopurinol. From the physical examination, the penis was fully erect, with an erection hardness score (EHS) of 4 and pain visual analog score (VAS) of 9. The CC showed full tumescence, and the glans was flaccid. Laboratory examination revealed that the patient had anemia (8.9 g/dL) and hyperleukocytosis (305,800 cells/μL). Aspiration using 18G needle and cavernosal irrigation with 0.9% saline solution was performed. Gas analysis was performed on blood collected from CC puncture, which was consistent with an IP pattern (pH 7.15, pCO2 62 mmHg, and pO2 25 mmHg). Penile detumescence was not observed so we underwent Winter procedure using large bore biopsy needle. Large bore biopsy needle was inserted via the glans. Penile detumescence was observed following this procedure, with a penile hardness score of 0 and VAS of 1. However, the patient had recurrent painful priapism (EHS 4) 24-hours after the Winter procedure. The patient underwent another Winter procedure, which did not achieved detumescence because no adequate blood drown form the CC. The patient then underwent surgery for Al-Ghorab shunt plus intracorporal tunneling.
Surgical technique
The patient was placed in the supine position, and received general anesthesia. A tourniquet was temporarily placed at the proximal end of the penile shaft to control bleeding. A 2-cm transversal incision was made on the penile glans, 1 cm distal of the coronal sulcus. The cavernous tissue at the penile glans was retracted, fixed with 2-0 sutures. We excised two 5-mm circular cone segments of the tunica albuginea to create a corporoglandular shunt (Al-Ghorab shunt). Dark-colored blood was noticed during the creation of the shunt, which difficult to drains spontaneously from the engorged corporal tissue. We performed a modified Al-Ghorab shunt procedure, which included retrograde insertion of a 7/8 Hegar dilator into the opening of the distal cavernous tissue via the original Al-Ghorab incision (Fig. 1). After removal of the dilator, manual digital compression of the penis (proximal to distal) was performed to facilitate blood clot removal. Insertion of the dilator and manual compression was performed three times until complete detumescence was observed, after which closure of the glans penis skins was performed with 4-0 chromic sutures (Fig. 2). A urethral catheter was placed and secured to the patient's thigh.
Figure 1.
A) Schematic diagram of Al-Ghorab corporoglandular shunt; B) modification of Al-Ghorab with intracorporal dilatation using Hegar Dilator.
Picture illustration by Andika Afriansyah.
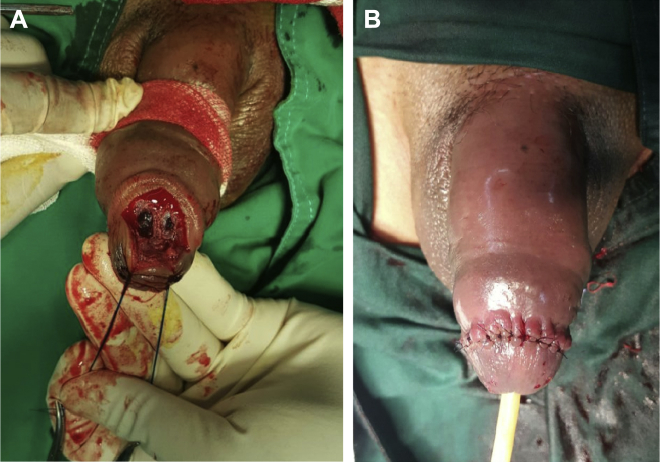
Figure 2.
A) Al-Ghorab corporoglandular shunt. B) Closure of the glans penis skin.
Discussion
The first-line management of IP is aspiration and intracavernous injection of alpha-adrenergic agonists. The use of an intracorporeal alpha-adrenergic agonist together with irrigation has a resolution rate up to 80%. If conservative management is unsuccessful, a surgical approach can be initiated. The principle surgical management for IP is the creation of a fistula between engorged CC and the corpus spongiosum, glans or saphenous veins. A shunt between the CC and corpus spongiosum can be formed regardless of whether a distal or proximal approach is used.1 The decision for which surgical technique to use is based on five factors: (1) the duration of IP, (2) previous intervention, (3) success rate of the proposed surgical technique, (4) possible complications, and (5) familiarity of surgeon with the technique.
We created a corporoglandular shunt using the Al-Ghorab technique by opening the tunica albuginea at the glans. The Al-Ghorab shunt procedure was modified by the retrograde insertion of a 7/8 Hegar dilator into the opening of the distal cavernous tissue via the original Al-Ghorab incision. We decided to apply this maneuver based on the observation that the clogged blood in the CC did not adequately drain after an opening of the tunica albuginea was created. The use of a Hegar dilator to remove the blood clot is similar to the method used by plumbers to unclog debris in a water pipe using a “snake” device.3 Brant et al described a similar technique to achieve corporal tunneling for adequate drainage of blood clots using urethral sounds.4 Shiraishi et al created drainage using Pean forceps. After removing the CC, the Pean was opened as wide as possible to create an adequate drainage route.5
At follow up, the patient had not experienced recurrent IP, but had severe erectile dysfunction. We believe that prolonged IP causes erectile dysfunction, rather than this being a consequence of the procedure. The long ischemic time causes irreversible damage to the CC tissue, such as necrosis and fibrosis, resulting in erectile dysfunction and decreased quality of life. We think that cannulation process to drain the blood clot does not cause significant tissue damage. The cavernous arteries are vigorous and uninjured by dilatation as the arteries run in same longitudinal direction as the inserted dilator.
Conclusion
In the current report we have described our first experience using Al-Ghorab corporoglandular shunt plus intracorporal tunneling for the treatment of prolonged IP. The use of this procedure adequately resolved the recurrent IP that failed treatment with conservative management and the Winter method. The use of a Hegar dilator facilitated adequate blood clot drainage in this case of prolonged IP. Priapism was successfully relieved, and no recurrent IP was reported.
Conflict of interest
The authors declare that there is no conflict of interest regarding the publication of this article.
References
- 1.Salonia A., Eardley I., Giuliano F. European Association of Urology guidelines on priapism. Eur Urol. 2014;65(2):480–489. doi: 10.1016/j.eururo.2013.11.008. [DOI] [PubMed] [Google Scholar]
- 2.Nixon R.G., O'Connor J.L., Milam D.F. Efficacy of shunt surgery for refractory low flow priapism: a report on the incidence of failed detumescence and erectile dysfunction. J Urol. 2003;170(3):883–886. doi: 10.1097/01.ju.0000081291.37860.a5. [DOI] [PubMed] [Google Scholar]
- 3.Burnett A.L., Pierorazio P.M. Corporal “snake” maneuver: corporoglanular shunt surgical modification for ischemic priapism. J Sex Med. 2009;6(4):1171–1176. doi: 10.1111/j.1743-6109.2008.01176.x. [DOI] [PubMed] [Google Scholar]
- 4.Brant W.O., Garcia M.M., Bella A.J. T-shaped shunt and intracavernous tunneling for prolonged ischemic priapism. J Urol. 2009;181(4):1699–1705. doi: 10.1016/j.juro.2008.12.021. [DOI] [PubMed] [Google Scholar]
- 5.Shiraishi K., Matsuyama H. Salvage management of prolonged ischemic priapism: Al-Ghorab shunt plus cavernous tunneling with blunt cavernosotomy. J Sex Med. 2013;10(2):599–602. doi: 10.1111/j.1743-6109.2012.02973.x. [DOI] [PubMed] [Google Scholar]