Abstract
Study Objectives:
Mandibular protrusion during sleep monitoring has been proposed as a method to predict oral appliance treatment outcome.
A commercial remotely controlled mandibular protrusion (RCMP) device has become available for this purpose with predictive accuracy demonstrated in an initial study. Our aim was to validate this RCMP method for oral appliance treatment outcome prediction in a clinical sleep laboratory setting.
Methods:
Forty-two obstructive sleep apnea (OSA) patients (apnea-hypopnea index [AHI] > 10 events/h) were recruited to undergo a RCMP sleep study before commencing oral appliance treatment. The RCMP study was used to make a prediction of treatment “Success” or “Failure” based on a rule of ≤ 1 respiratory event per 5 min supine rapid eye movement sleep. Oral appliance treatment response was verified by polysomonography and defined as treatment AHI < 10 events/h with 50% reduction.
Results:
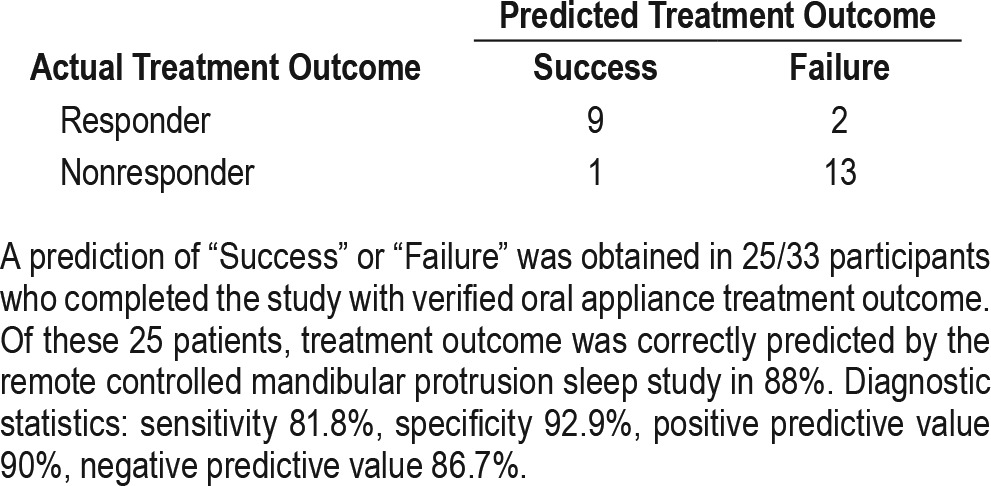
Participants were on average middle-aged (57.1 ± 11.6 y) and overweight (29.6 ± 4.5 kg/m2) with baseline AHI 31.5 ± 20.5 events/h, 39% severe OSA (AHI > 30 events/h). Two participants (5%) were not able to tolerate the RCMP study. Oral appliance treatment outcome was verified in 33 participants (RCMP results: “Success” n = 10, “Failure” n = 15, “Inconclusive” n = 8). In those with a treatment outcome prediction (n = 25) the diagnostic characteristics of the RCMP test were sensitivity 81.8%, specificity 92.9%, positive predictive value 90%, and negative predictive value 86.7% (n = 3 misclassified).
Conclusions:
The RCMP device was well tolerated by patients and successfully used to perform mandibular protrusion sleep studies in our sleep laboratory. The RCMP sleep study showed good accuracy as a prediction technique for oral appliance treatment outcome, although there was a high rate of inconclusive tests.
Citation:
Sutherland K, Ngiam J, Cistulli PA. Performance of remotely controlled mandibular protrusion sleep studies for prediction of oral appliance treatment response. J Clin Sleep Med. 2017;13(3):411–417.
Keywords: obstructive sleep apnea, oral appliance, polysomnography, remotely controlled mandibular protrusion, treatment outcome prediction
INTRODUCTION
Obstructive sleep apnea (OSA) is a common sleep disorder associated with significant health consequences including excess daytime sleepiness, reduced quality of life, motor vehicle and occupational accidents, hypertension, and cardiovascular disease.1–7 Adequately treating this chronic condition to circumvent downstream consequences can be challenging. The mainstays of treatment are devices to prevent pharyngeal collapse during sleep; this is most effectively achieved using nasal continuous positive airway pressure (CPAP), which is highly efficacious when worn. However, many patients reportedly use CPAP at either suboptimal levels for health benefit or abandon it altogether after only months of use.8 An alternative approach is an oral appliance, specifically a mandibular advancement splint, which holds the mandible in a protruded position to enlarge and stabilize the pharyngeal airway.9,10 These intraoral devices are less obtrusive than the CPAP mask and machine complex and are often preferred by patients who experience both therapies and with better reported adherence.11 Oral appliances have demonstrated efficacy in reducing OSA; however, unlike CPAP, which will be efficacious in all who can tolerate adequate pressure, individual treatment response is highly variable. More than one-third of patients will achieve a complete response to oral appliance therapy (apnea-hypopnea index [AHI] < 5 events/h) and two-thirds will experience a significant improvement (> 50% reduction in AHI).12 However this leaves one-third of OSA patients with minimal clinical benefit from oral appliance therapy. How to select appropriate patients for oral appliance therapy has been an ongoing clinical challenge. Various patient characteristics have been associated with higher rates of treatment success, such as, younger age, less obesity, female sex, and less severe OSA.13 However, these are not always consistent between studies and predictive accuracy based on these patient factors alone is not adequate. Therefore, other approaches to predict oral appliance treatment response are needed, although prospectively validated reliable methods have remained elusive.
BRIEF SUMMARY
Current Knowledge/Study Rationale: Oral appliance treatment response varies between individuals and development of methods to pre-identify treatment responders has been an ongoing challenge. A commercially available RCMP device has become available for use during sleep studies for this purpose; we wished to assess this methodology in our own laboratory setting for accuracy in prediction of oral appliance treatment outcome.
Study Impact: This study presents predictive accuracy of the RCMP methodology in an independent site to the original validation study. This study provides further information about the performance of this technique in another center and supports the application of this methodology in the clinical setting.
One promising strategy is the use of remotely controlled mandibular protrusion (RCMP) applied during monitored sleep in response to obstructive breathing events. The level of protrusion is incrementally increased until either obstructive events are adequately controlled (therapeutic protrusion level) or maximum protrusion is reached. The concept is analogous to increasing CPAP pressure in response to apnea to determine optimal fixed pressure. RCMP as a tool for oral appliance treatment outcome prediction was originally explored using prototype devices with promising results.14–16 A commercially available device to provide RCMP has subsequently become available (MATRx, Zephyr Sleep Technologies Inc., Calgary, Canada) and was tested as a prediction tool for oral appliance treatment response in 67 patients in Canada.6 In this study, OSA patients underwent an in-laboratory attended sleep study with the RCMP device in which the sleep technician remotely advanced the protrusive position in increments in response to the appearance of sleep-disordered breathing. A prediction rule to classify patients as “success” or “failure” was developed based on a cutoff of one event per 5 min of supine rapid eye movement (REM) sleep.
Although this initial study showed this RCMP device to be a useful clinical prediction tool for oral appliance response, it is important to replicate these findings in other centers. Our aim was to assess the MATRx RCMP device as a prediction tool for oral appliance treatment response in our clinical sleep laboratory using full-night polysomnography.
METHODS
Participants
Adults with OSA (AHI > 10 events/h on in-laboratory polysomnography within the past 12 mo) who were willing to try oral appliance treatment were recruited from sleep clinics. OSA patients needed to be eligible for oral appliance treatment with the requirement to have enough teeth in the upper and lower dental arches to anchor the device for adequate retention (generally considered a minimum of 10 teeth per arch) and to be free of significant periodontal disease. There were no restrictions placed on AHI or body mass index (BMI) for entry into the study. The study was approved by the human research ethics committee of the Sydney Local Health District (Protocol No. X11-0134 & HREC/11/RPAH/192).
Remotely Controlled Mandibular Protrusion Sleep Study
The commercially available RCMP device, MATRx (Zephyr Sleep Technologies Inc., Calgary, Canada) was used for the treatment outcome prediction studies. The RCMP studies were performed between June 2014 and May 2015 and were undertaken by each participant before the commencement of oral appliance treatment. Patients attended an initial dental visit to fit the upper and lower disposable dental impression trays that attach to the RCMP positioner. The dentist recorded measurements from the millimeter scale on the upper bracket of the dental trays which correspond to the “rest” position (habitual bite position), maximum retrusion, and maximum protrusion (RCMP maximal protrusive limit), as voluntarily performed during wakefulness. These measurements were used to set the individual's mandibular range of motion for the RCMP study. Standard overnight polysomnography (Compumedics Ltd, Victoria, Australia) in the clinical sleep laboratory was performed with the addition of RCMP operated through the device software (OATRx TS, Zephyr Sleep Technologies Inc., Calgary, Canada). The studies were performed in accordance with the instructions for use of the device (MATRx Clinical Applications Guide version 2). Before study commencement, the sleep technologist calibrated the RCMP system and entered the values of the individual's range of mandibular motion and rest position. The RCMP was set at 1 mm short of rest position to commence the study. The RCMP studies were conducted by a single experienced sleep technologist. The sleep technologist was instructed to follow the flow chart for mandibular titration from the manual. Specifically, this involved observation for obstructive apneas and hypopneas with the response to advance the mandibular position by RCMP (3 × 0.2 mm increments). The technologist waited for 2 min following the mandibular protrusion for equilibration. Mandibular titration continued according to the recommended algorithm for manual CPAP titration.17 Mandibular protrusion was again applied (3 × 0.2 mm) if in a 5-min interval there were two or more obstructive apneas, three or more hypopneas, or five or more respiratory effort-related arousals. This process was continued until satisfactory control of obstructive events or the RCMP maximal protrusive limit was reached. The protrusive level reached was maintained for the remainder of the sleep study.
Treatment Outcome Prediction
RCMP studies were scored by an experienced technologist using the 2012 American Academy of Sleep Medicine scoring rules (1A recommended criteria for hypopneas). The studies were scored blinded to any information about the participant or treatment response. The prediction was based on the number of events from the total supine REM sleep at maximal protrusion (either continuous or fragmented intervals of REM). The prediction algorithm from the original RCMP study6 was used to classify the studies with a prediction of “Success” or “Failure.” The prediction algorithm is based on the occurrence of respiratory events in supine REM sleep. If fewer than one event (apnea or hypopnea) is detected per 5 min of supine REM sleep, than the study is labeled “Success.” If more than one event is observed, even at the RCMP maximal protrusive limit than the study is labeled “Failure.” An “inconclusive” study occurs if respiratory events remained but the RCMP maximal protrusive limit was not reached or if insufficient supine REM sleep (< 5 min) was present. Lateral REM sleep could substitute for supine REM sleep if the diagnostic sleep study indicated lateral sleep position predominated.
Oral Appliance Treatment
All participants were treated with a customized two-piece mandibular advancement splint (SomnoDent Fusion, SomnoMed Ltd, Australia). The appliance is initially set at 70% of maximum mandibular protrusion, being an empiric level of advancement for comfortable initiation of treatment. Upon receiving the appliance, patients underwent an acclimatization period (approximately 6 to 12 w) in which they self-titrated the level of mandibular protrusion to their maximum comfortable limit (oral appliance treatment level). This individual maximum protrusive level, or oral appliance treatment limit, was confirmed by the treating dentist. The maximum advancement provided by the appliance is measured by as a percentage of the distance from the most retrusive to protrusive position. Full-night polysomnography with the treatment oral appliance in situ was performed to determine actual treatment response. Treatment response was defined as an AHI < 10 events/h accompanied by a 50% reduction in AHI from baseline levels, in keeping with the original MATRx study.6
Statistical Analysis
Participant characteristics were summarized using descripting statistics. Differences between groups (responders/nonresponders, completers/noncompleters) were assessed using independent t-tests. Statistical significance was accepted at the level of p < 0.05. Two-by-two frequency tables were used to examine association between predicted and actual treatment outcome with diagnostic statistics of sensitivity, specificity, and positive and negative predictive values calculated.
RESULTS
A total of 42 participants were recruited to undergo RCMP sleep studies. Two participants (5%) were unable to complete the RCMP study. One patient was unable to sleep with the dental trays and attached RCMP, the other was unable to commence the RCMP study because excess salivation prevented retention of the dental trays. Of 40 participants who completed the RCMP study, a prediction of success or failure was obtained in 78%, with 9 studies returning an “Inconclusive” result (Insufficient REM sleep n = 6, RCMP maximal protrusive limit not reached during study n = 3). A full night polysomnography with oral appliance in situ to assess treatment outcome was completed in 33 participants (n = 10 predicted “Success,” n = 15 predicted “Fail,” n = 8 “Inconclusive”). A flow chart outlining the study is provided in Figure 1.
Figure 1. Study flow.
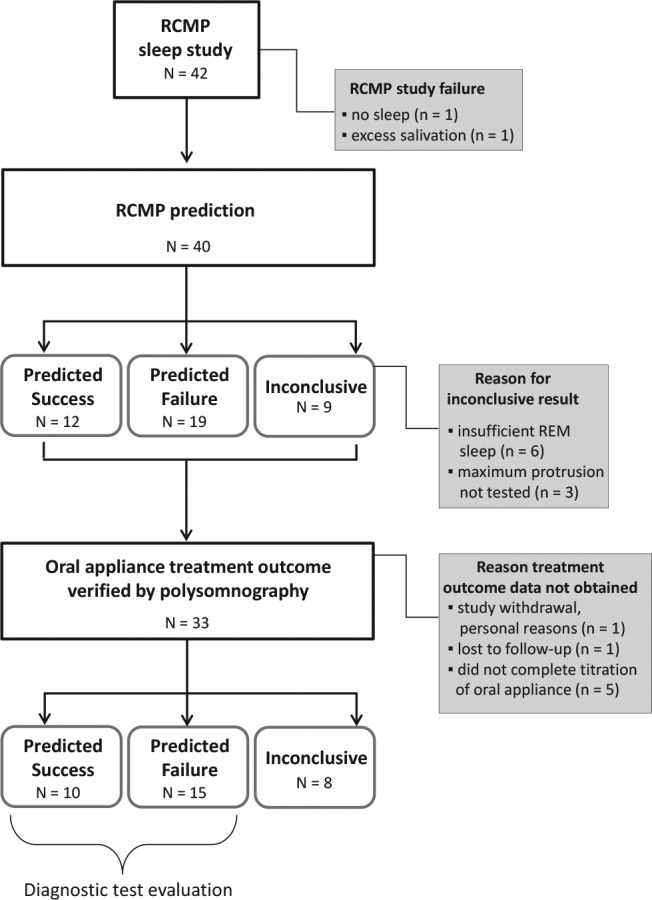
Predictive accuracy of remote controlled mandibular protrusion (RCMP) sleep studies for oral appliance treatment outcome was performed in study completers with a “Success” or “Failure” outcome from the RCMP night (n = 25). REM = rapid eye movement.
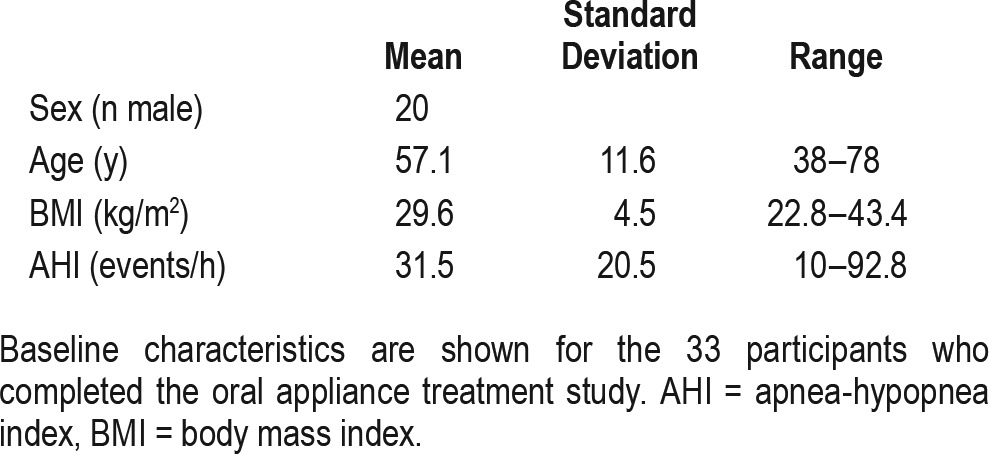
Patient Characteristics
Patient characteristics for the 33 study completers are given in Table 1. Participants were typical of the general OSA clinical population, being on average overweight and middle-aged, with a higher proportion of males (60%). On average, participants had OSA severity in the severe range (18% mild OSA, 42% moderate OSA, 39% severe OSA). There was no difference between the 33 RCMP study participants who completed the polysomnography study with the oral appliance and the 7 who did not complete the study in terms of age, BMI, AHI, or sex.
Table 1.
Patient characteristics.
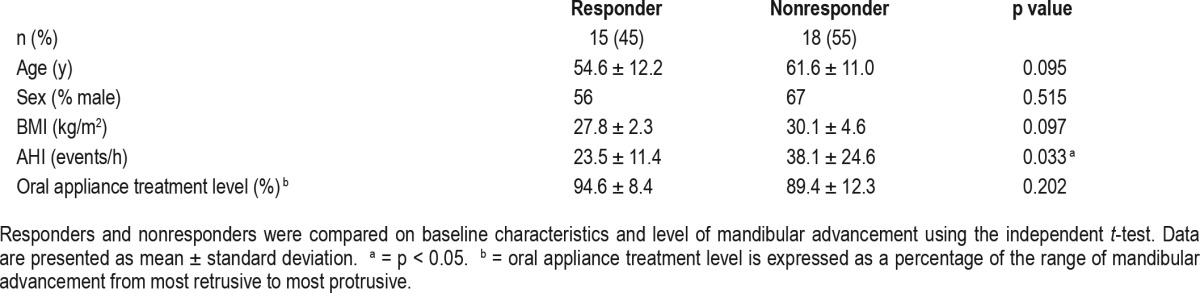
Fifteen of the study completers were oral appliance treatment responders (45%). A comparison of treatment responders and nonresponders in terms of baseline characteristics are shown in Table 2. There was no difference between responders and nonresponders in age, BMI, or sex. Nonresponders had a higher baseline AHI compared to the responders. Participants were treated with a high level of mandibular advancement (92 ± 11%, range 52.9–109.1%) and there was no difference between responders and nonresponders in the level of mandibular advancement.
Table 2.
Comparison of oral appliance treatment responders and nonresponders.
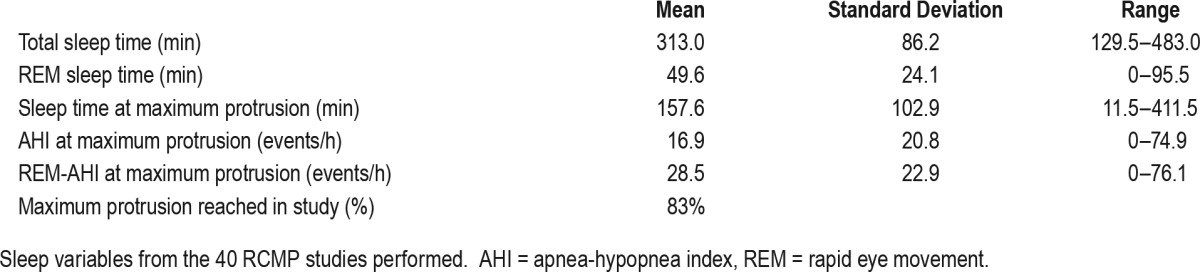
RCMP Studies
The RCMP studies were highly feasible, with 40 of 42 participants able to tolerate the dental trays and complete the sleep study. Sleep-related variables from the RCMP study night are shown in Table 3. Participants were able to sleep adequately during the night, with an average total sleep time of 5.2 h. At the final RCMP study protrusive level, the average AHI was in the moderate range (16.9 ± 20.8 events/h), with 15 of 40 participants (37.5%) showing an AHI < 5 events/h while at the final protrusion level.
Table 3.
Remote controlled mandibular protrusion (RCMP) sleep study variables.
Predictive Accuracy
The 25 participants with a prediction (“Success” or “Failure”) from the RCMP study and available oral appliance treatment outcome were used to assess predictive accuracy of the RCMP test (Table 4). Overall, 88% of patients were correctly classified as responders or nonresponders using the prediction rules for success or failure; two participants had false-negative results and one had a false-positive result (n = 3 misclassified). This equates to sensitivity of 81.8%, specificity 92.9%, positive predictive value 90%, and negative predictive value of 86.7%.
Table 4.
Diagnostic accuracy of oral appliance treatment outcome prediction using remote controlled mandibular protrusion sleep study.
In terms of the three misclassified patients, the false-positive result occurred in a male (age 43 y, BMI 32.8 kg/m2) who went from an AHI of 10 events/h to 7.8 events/h with oral appliance therapy. His AHI during REM sleep at RCMP maximal protrusive limit during the study was 2.4 events/h. The two patients with false-negative results were female. One patient (age 69 y, BMI 30.9 kg/m2) had severe OSA (38.2 events/h), which was reduced to 9.5 events/h using the oral appliance; however, she had an AHI of 32.8 events/h in supine REM sleep at RCMP maximal protrusive limit during the study. The other patient (age 60 y, BMI 24.7 kg/m2) had moderate OSA (AHI 17.5 events/h) and a complete response to treatment (AHI 1.9 events/h), although her AHI at the RCMP maximal protrusive limit in supine REM sleep on the RCMP study night was 19.4 events/h.
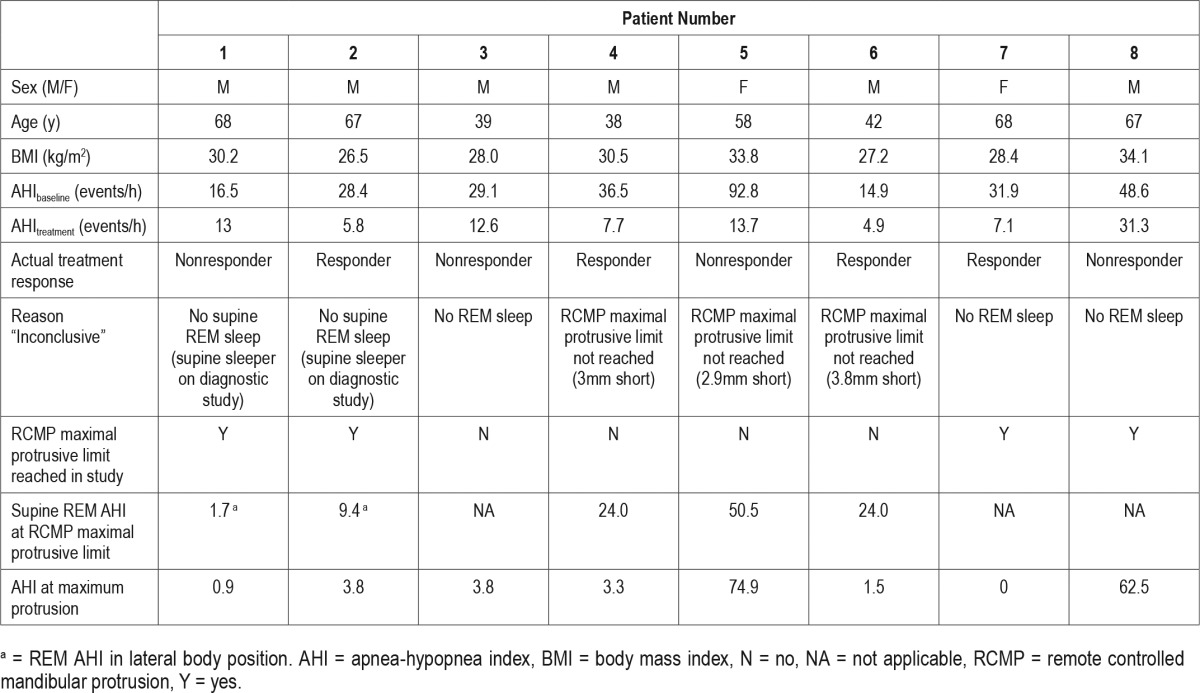
There were eight participants in whom a prediction from RCMP study result was not able to be obtained (“inconclusive”) due to insufficient REM sleep to use the prediction rules or insufficient time to test the RCMP maximal protrusive limit. Characteristics of these participants and their RCMP study are given in Table 5. There is no consistent alternative rule with which to correctly classify these patients as responders or nonresponders from the RCMP study data. For example, patients 5 and 8 are both nonresponders and both have high AHI in the severe range at the RCMP maximal protrusive limit during the study which could be considered to reflect actual response. However, other patients (1 and 3) have very low AHI (< 5 events/h) at RCMP maximal protrusive limit but are nonresponders to actual oral appliance treatment. Therefore, alternate prediction rules in the 24% of RCMP studies labeled “inconclusive” were not helpful in this small sample and 24% of RCMP studies were not able to be used for prediction in our hands in this initial run of tests.
Table 5.
Characteristics of participants (study completers) and remote controlled mandibular protrusion studies with “Inconclusive” result for prediction of oral appliance treatment outcome (n = 8).
We additionally assessed a prediction rule of AHI < 5 events/h during total sleep time at maximum protrusion (without requirement for supine REM sleep) in all 33 study completers. This prediction rule did not result in as robust prediction with 9 correctly predicted responders, 15 correctly predicted nonresponders, 3 false-positive results, and 6 false-negative results (sensitivity 60%, specificity 83%, PPV 75%, NPV 71.4%).
Effective Target Protrusion
An additional outcome from the original MATRx RCMP prediction study was the effective target protrusive position for oral appliance treatment outcome determined from the RCMP final protrusion level reached during the study. Our treatment outcome studies were all performed at maximum comfortable protrusion (oral appliance treatment level) after self-titration over titration period of approximately 2 mo, so we were not able to assess the effective target protrusive position for use in treatment. Of the correctly predicted responders (n = 9), only two of them did not reach RCMP maximal protrusive limit during the study (one by 0.8 mm and the other 2.5 mm). Therefore, most patients were required to proceed to the predetermined RCMP maximal protrusive limit to stop obstructive respiratory events based on the titration rules used in these RCMP sleep studies.
DISCUSSION
The purpose of this study was to assess a commercially available RCMP device for accuracy in prediction of oral appliance treatment outcome in a clinical sleep laboratory setting. Prospectively validated methods for oral appliance treatment outcome prediction that are sufficiently reliable for use in clinical practice have remained elusive.18 A sleep test that directly assesses the effect of mandibular protrusion is likely to provide a good indication of actual oral appliance treatment response; however, until recently this could only be achieved using prototype devices or by waking the patient to manually adjust a device to provide more advancement.19 The advent of a commercial RCMP device now provides a means for sleep laboratories to routinely perform such assessments in a consistent manner, in a method that is conceptually analogous to CPAP titration. This device showed good predictive utility in the original study. However, validation in other centers is important before widely adopting this method in routine clinical care. Also, this is the first study to compare the RCMP prediction results against treatment outcome verified during full night polysomnography. The original study of this RCMP device used a level 3 sleep monitoring device, and our results are the first to use in-laboratory polysomnography for diagnostic and treatment studies.
Our study confirmed that RCMP sleep studies are well tolerated by OSA patients, with only two of our recruited participants (5%) unable to tolerate the device to complete sleep recordings. In the RCMP studies where a prediction of “success” or “failure” was obtained, we found correct classification of actual treatment response in 88% of patients. Compared to the original study using the RCMP device,6 we had very similar sensitivity (81.8% versus 86%), specificity (92.9 % versus 92%), positive predictive value (90% versus 94%), and negative predictive value (86.7% versus 83%). The positive and negative predictive values obtained in the current study are also high for oral appliance treatment prediction methods18 and our results demonstrate that the technique is relatively easily adapted into other clinical sleep laboratories. We believe the findings of this study to be generalizable to our general clinic population, with minimal inclusion criteria imposed on the study apart from an AHI of approximately 10 events/h and no contraindications to oral appliance wear.
In this study we attempted to conduct the RCMP studies in a manner equivalent to that outlined in the original publication.6 However, there are some differences between methodologies between the studies. Particularly the original study used a 4% oxygen desaturation index from a portable monitoring device to classify treatment response, whereas the current study used the AHI from in-laboratory polysomnography. Despite this, the predictive accuracy of successful tests were very similar. We found that the original prediction rule (based on supine REM sleep) worked best in terms of predictive accuracy, with prediction based on a total AHI at RCMP maximal protrusive limit not returning as favorable diagnostic statistics. Therefore, the original conservative prediction rule based on supine REM sleep provides the most consistent predictive accuracy for actual oral appliance treatment response. Although our predictive accuracy was relatively similar to that of the previous study, we did find a much higher rate of “inconclusive” RCMP study results (> 20% of tests performed compared to 9% in the previous study). In most cases this was because of a lack of REM sleep during the RCMP study. Three of the inconclusive studies (33%) were designated such because RCMP maximal protrusive limit was not tested in the study, whereas supine REM events remained present. Of the three participants who did not reach RCMP maximal protrusive limit, the two who were oral appliance treatment responders had an AHI < 5 events/h at the RCMP final protrusive level during the study. The nonresponder had an AHI > 70 events/h in the RCMP final protrusive level. Therefore, potentially other variables from the RCMP study could be used to make a treatment decision in these cases and would have been appropriate in these cases. However, prediction of actual response did not occur robustly when using a total AHI in the whole sample. In the inconclusive tests with insufficient REM sleep (< 5 min), there was less of an indicative pattern based on the AHI at RCMP maximal protrusive limit, with two of the nonresponders achieving AHI < 5 events/h at RCMP maximal protrusive limit. The inconclusive RCMP studies were spread throughout the study period and hence it is unclear whether it can be attributed to the extent of experience with the technique. Whether this is an acceptable test fail rate would depend on the context and requires further investigation.
In this study, oral appliance treatment was initiated at 70% of maximal mandibular protrusion and treatment outcome was assessed using maximum comfortable protrusive position (oral appliance treatment level) after incremental titration over an acclimatization period. In this study, the oral appliance treatment level was on average 92% of maximal mandibular protrusion. Therefore, we did not directly test the accuracy of the RCMP for obtaining an “effective target protrusive position” for oral appliance treatment. Most of the RCMP studies reached the RCMP maximal protrusive limit during the test, and hence it is unlikely that we “overtreated” patients by titrating the actual appliance to the maximum comfortable protrusive position. Of the correctly predicted “success” cases, only two of these stopped short of their predetermined RCMP maximal protrusive limit during the RCMP study. Potentially the titration of advancement on the actual device could be ceased at the RCMP final protrusion level, although our study treatment protocol did not allow this to be tested. In our study the results of the RCMP study suggest that the oral appliance treatment limit should be as close to maximum as possible, because below this level obstructive events were still present in most cases. Ultimately, the level of mandibular protrusion must always be considered in relation to side effects in individual patients.
The predictive accuracy of the RCMP sleep test using this commercial device in multiple and distinct sleep centers is encouraging. Accurate prediction of oral appliance treatment response has long been a goal of the field because the inability to ascertain the success of the therapy before implementation is a clinical barrier. Although simple indicators such as OSA severity, obesity, and increasing age are associated with poor treatment response, these factors alone do not reliably indicate treatment success or failure on an individual basis.12 Many different prediction tests, both during wakefulness or sleep/sedation, have been investigated with varying degrees of success. Some methods to indicate oral appliance treatment response, such as detection of the site of pharyngeal collapse using multisensor catheters,20 have been shown to be accurate but are not practical for the clinical situation. Other procedures, such as nasopharyngoscopy to visualize pharyngeal size and stability during mandibular protrusion, have also been shown to have predictive utility but this also depends on specialist skills and potentially analysis time.21–23 The RCMP method has a great advantage now that a commercial device is available. The test itself is one that aligns with current sleep laboratory testing procedures and therefore it could be envisioned that incorporation into current practice would be relatively straightforward. However, practical issues such as dental time requirements and billing may be a barrier in some regions.
In conclusion, the RCMP device tested in our clinical sleep center was easily adapted into the setup and adequately performed by staff. The test itself was well tolerated by patients and predictive accuracy was good, although there were a high proportion of test results not applicable to the prediction algorithm. The assessment of this device in a sleep center separate from that where the original study was performed is a step toward further validation of a method for prediction of oral appliance treatment outcome.
DISCLOSURE STATEMENT
The MATRx device and disposable trays were provided at no cost by Zephyr Sleep Technologies, Inc. The company did not have any role in the design, conduct, analysis or interpretation of the study. Oral appliances were provided at no cost by SomnoMed. Dr. Cistulli holds an endowed Academic Chair position at the University of Sydney, funded by ResMed, Inc. He has received research support from ResMed, SomnoMed, Zephyr Sleep Technologies, and Exploramed, Inc. He is a consultant to Zephyr Sleep Technologies, NovoNordisk and Fisher & Paykel Healthcare. He has a pecuniary interest in SomnoMed, resulting from previous involvement in research and development. He is on the speakers bureau for SomnoMed, and receives royalties from Quintessence and UpToDate. The other authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
The authors thank the staff of the Sleep Investigation Laboratory, Centre for Sleep Health and Research, Royal North Shore Hospital, and particularly Fung Yau and Mohammad Ahmadi.
ABBREVIATIONS
- AHI
apnea-hypopnea index
- BMI
body mass index
- CPAP
continuous positive airway pressure
- NPV
negative predictive value
- OSA
obstructive sleep apnea
- PPV
positive predictive value
- RCMP
remotely controlled mandibular protrusion
- REM
rapid eye movement
REFERENCES
- 1.Baldwin CM, Griffith KA, Nieto FJ, O'Connor GT, Walsleben JA, Redline S. The association of sleep-disordered breathing and sleep symptoms with quality of life in the Sleep Heart Health Study. Sleep. 2001;24(1):96–105. doi: 10.1093/sleep/24.1.96. [DOI] [PubMed] [Google Scholar]
- 2.Marin JM, Carrizo SJ, Vicente E, Agusti AG. Long-term cardiovascular outcomes in men with obstructive sleep apnoea-hypopnoea with or without treatment with continuous positive airway pressure: an observational study. Lancet. 2005;365(9464):1046–1053. doi: 10.1016/S0140-6736(05)71141-7. [DOI] [PubMed] [Google Scholar]
- 3.Pack AI, Gislason T. Obstructive sleep apnea and cardiovascular disease: a perspective and future directions. Prog Cardiovasc Dis. 2009;51(5):434–451. doi: 10.1016/j.pcad.2009.01.002. [DOI] [PubMed] [Google Scholar]
- 4.Peppard PE, Young T, Palta M, Skatrud J. Prospective study of the association between sleep-disordered breathing and hypertension. N Engl J Med. 2000;342(19):1378–1384. doi: 10.1056/NEJM200005113421901. [DOI] [PubMed] [Google Scholar]
- 5.Rakel RE. Clinical and societal consequences of obstructive sleep apnea and excessive daytime sleepiness. Postgrad Med. 2009;121(1):86–95. doi: 10.3810/pgm.2009.01.1957. [DOI] [PubMed] [Google Scholar]
- 6.Remmers J, Charkhandeh S, Grosse J, et al. Remotely controlled mandibular protrusion during sleep predicts therapeutic success with oral appliances in patients with obstructive sleep apnea. Sleep. 2013;36(10):1517–1525. doi: 10.5665/sleep.3048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sassani A, Findley LJ, Kryger M, Goldlust E, George C, Davidson TM. Reducing motor-vehicle collisions, costs, and fatalities by treating obstructive sleep apnea syndrome. Sleep. 2004;27(3):453–458. doi: 10.1093/sleep/27.3.453. [DOI] [PubMed] [Google Scholar]
- 8.Bartlett D, Wong K, Richards D, et al. Increasing adherence to obstructive sleep apnea treatment with a group social cognitive therapy treatment intervention: a randomized trial. Sleep. 2013;36(11):1647–1654. doi: 10.5665/sleep.3118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chan AS, Sutherland K, Schwab RJ, et al. The effect of mandibular advancement on upper airway structure in obstructive sleep apnoea. Thorax. 2010;65(8):726–732. doi: 10.1136/thx.2009.131094. [DOI] [PubMed] [Google Scholar]
- 10.Ng AT, Gotsopoulos H, Qian J, Cistulli PA. Effect of oral appliance therapy on upper airway collapsibility in obstructive sleep apnea. Am J Respir Crit Care Med. 2003;168(2):238–241. doi: 10.1164/rccm.200211-1275OC. [DOI] [PubMed] [Google Scholar]
- 11.Phillips CL, Grunstein RR, Darendeliler MA, et al. Health outcomes of continuous positive airway pressure versus oral appliance treatment for obstructive sleep apnea: a randomized controlled trial. Am J Respir Crit Care Med. 2013;187(8):879–887. doi: 10.1164/rccm.201212-2223OC. [DOI] [PubMed] [Google Scholar]
- 12.Sutherland K, Takaya H, Qian J, Petocz P, Ng AT, Cistulli PA. Oral appliance treatment response and polysomnographic phenotypes of obstructive sleep apnea. J Clin Sleep Med. 2015;11(8):861–868. doi: 10.5664/jcsm.4934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sutherland K, Vanderveken OM, Tsuda H, et al. Oral appliance treatment for obstructive sleep apnea: an update. J Clin Sleep Med. 2014;10(2):215–227. doi: 10.5664/jcsm.3460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dort LC, Hadjuk E, Remmers JE. Mandibular advancement and obstructive sleep apnoea: a method for determining effective mandibular protrusion. Eur Respir J. 2006;27(5):1003–1009. doi: 10.1183/09031936.06.00077804. [DOI] [PubMed] [Google Scholar]
- 15.Petelle B, Vincent G, Gagnadoux F, Rakotonanahary D, Meyer B, Fleury B. One-night mandibular advancement titration for obstructive sleep apnea syndrome: a pilot study. Am J Respir Crit Care Med. 2002;165(8):1150–1153. doi: 10.1164/ajrccm.165.8.2108056. [DOI] [PubMed] [Google Scholar]
- 16.Tsai WH, Vazquez JC, Oshima T, et al. Remotely controlled mandibular positioner predicts efficacy of oral appliances in sleep apnea. Am J Respir Crit Care Med. 2004;170(4):366–370. doi: 10.1164/rccm.200310-1446OC. [DOI] [PubMed] [Google Scholar]
- 17.Kushida CA, Chediak A, Berry RB, et al. Clinical guidelines for the manual titration of positive airway pressure in patients with obstructive sleep apnea. J Clin Sleep Med. 2008;4(2):157–171. [PMC free article] [PubMed] [Google Scholar]
- 18.Okuno K, Pliska BT, Hamoda M, Lowe AA, Almeida FR. Prediction of oral appliance treatment outcomes in obstructive sleep apnea: a systematic review. Sleep Med Rev. 2015;30:25–33. doi: 10.1016/j.smrv.2015.11.007. [DOI] [PubMed] [Google Scholar]
- 19.Kuna ST, Giarraputo PC, Stanton DC, Levin LM, Frantz D. Evaluation of an oral mandibular advancement titration appliance. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101(5):593–603. doi: 10.1016/j.tripleo.2005.08.033. [DOI] [PubMed] [Google Scholar]
- 20.Ng AT, Qian J, Cistulli PA. Oropharyngeal collapse predicts treatment response with oral appliance therapy in obstructive sleep apnea. Sleep. 2006;29(5):666–671. [PubMed] [Google Scholar]
- 21.Chan AS, Lee RW, Srinivasan VK, Darendeliler MA, Grunstein RR, Cistulli PA. Nasopharyngoscopic evaluation of oral appliance therapy for obstructive sleep apnoea. Eur Respir J. 2010;35(4):836–842. doi: 10.1183/09031936.00077409. [DOI] [PubMed] [Google Scholar]
- 22.Okuno K, Sasao Y, Nohara K, et al. Endoscopy evaluation to predict oral appliance outcomes in obstructive sleep apnoea. Eur Respir J. 2016;47(5):1410–1419. doi: 10.1183/13993003.01088-2015. [DOI] [PubMed] [Google Scholar]
- 23.Vroegop AV, Vanderveken OM, Dieltjens M, et al. Sleep endoscopy with simulation bite for prediction of oral appliance treatment outcome. J Sleep Res. 2013;22(3):348–355. doi: 10.1111/jsr.12008. [DOI] [PubMed] [Google Scholar]


