Abstract
Study Objectives:
Many adults sleep with a significant other; thus, sleep disorder symptoms and treatments of one partner are likely to impact the other partner's health. A literature review was conducted to examine the impact of obstructive sleep apnea (OSA) and OSA treatments on partner-assessed sleep and daytime functioning and partner involvement in OSA treatment.
Methods:
MEDLINE, EMBASE, and CINAHL searches yielded 38 pertinent quantitative and qualitative studies that described sleep and/or daytime functioning assessed in partners of patients with untreated OSA, sleep and/or daytime functioning assessed in partners who were referred for OSA treatment, including continuous positive airway pressure (CPAP) therapy, oral appliance (OA), or surgery, and/or associations between partner involvement and OSA treatment use.
Results:
The majority of studies found untreated OSA to have a negative impact on partners' objective and subjective sleep and daytime functioning, in particular mood, quality of life, and relationship quality. Improvements in partner-assessed sleep quality were reported for CPAP, OA, and surgery. Conflicting results were reported for partners' mood, quality of life, daytime sleepiness, and relationship quality. Perceived partner support was associated with greater CPAP use.
Conclusions:
Symptoms associated with OSA can negatively impact partners' sleep and daytime functioning. Treatment of OSA with CPAP, OA, or surgery can have health benefits for not only patients but also partners. Collaborative partner involvement may be a useful strategy for interventions promoting CPAP adherence.
Citation:
Luyster FS. Impact of obstructive sleep apnea and its treatments on partners: a literature review. J Clin Sleep Med. 2017;13(3):467–477.
Keywords: continuous positive airway pressure, obstructive sleep apnea, oral appliance, partner, spouse
INTRODUCTION
Obstructive sleep apnea (OSA) is an exceedingly common sleep disorder characterized by snoring, repetitive apneas, sleep disruption due to frequent arousals, and, for some, daytime sleepiness. Untreated OSA is associated with adverse health outcomes, including decreased quality of life, psychological symptoms, insulin resistance, and increased risk for cardiovascular disease and mortality.1–4 Continuous positive airway pressure (CPAP) therapy is the first-line treatment for OSA, and mounting evidence suggests that CPAP can reduce breathing disturbances and daytime sleepiness and improve sleep quality, quality of life, and blood pressure.5,6 Alternative treatment options, including oral appliances (OA) and upper airway surgery, are available to patients for whom CPAP therapy is not well tolerated, who are unresponsive to CPAP, or who are not appropriate candidates for CPAP. Adherence to treatment is critical for achieving optimal therapeutic benefit, yet adherence is problematic particularly for individuals undergoing CPAP.7
Sleep is often a shared experience for many adults.8 Because the hallmark symptoms of OSA (i.e., snoring, apneas) occur during the night, spouses and partners are likely to experience sleep disturbance that may contribute to daytime impairments and relationship problems. OSA treatment may also benefit partners as patients experience reductions in snoring, apneas, and daytime sleepiness. The nature of partner interaction during OSA treatment initiation may vary and is likely to have important implications for patients' continued use of treatment. The purpose of this review is to summarize the existing research on (1) the impact of OSA on partner-assessed sleep and daytime functioning, (2) the impact of OSA treatments on partner-assessed sleep and daytime functioning, and (3) partner involvement in OSA treatment.
METHODS
A literature search was conducted using MEDLINE, EMBASE, and CINAHL to identify English-language studies examining the effect of OSA and OSA treatments on partners' assessed sleep and daytime functioning and partner involvement in OSA treatments. Additionally, reference lists of all identified relevant articles were searched. The keywords used to search for articles included sleep apnea, sleep-disordered breathing, spouse, partner, wives, positive airway pressure, oral appliance, and surgery. Different combinations of these search terms yielded between 1 (wives and oral appliance) and 143 (partner and sleep apnea) articles that were considered for review. Studies were included in the review if (1) they reported data from an original study (i.e., no review articles or case reports), (2) patients had objective documentation of OSA such as laboratory or in-home polysomnography (PSG) and/ or were receiving OSA treatment, and (3) described (a) sleep and/or daytime functioning (e.g., mood, daytime sleepiness, cognitive function, quality of life, work performance, relationship quality) assessed in spouses or partners of patients with untreated OSA; (b) sleep and/or daytime functioning (e.g., mood, daytime sleepiness, cognitive function, quality of life, work performance, relationship quality) assessed in spouses or partners of OSA patients who were referred for OSA treatment, including CPAP, OA, or surgery; and/or (c) associations between spouses or partners and use of OSA treatments. Both quantitative and qualitative research studies were included in this review as hearing patients' and partners' perspectives about their experiences and concerns regarding OSA and its treatment can provide a richer understanding of these phenomenon which are unlikely to be fully captured by questionnaires. Articles were excluded if, for inclusion criterion a or b, partner outcomes were reported by the patient. In total, 38 studies were included in the current review.
REVIEW OF FINDINGS
Effects of Untreated OSA on Partners' Sleep and Daytime Functioning
Most research examining the impact of untreated OSA on partners have found negative daytime and nighttime consequences (Table 1). As compared to spouses from the general population, spouses of patients with heavy snoring and OSA are three times more likely to report insomnia symptoms, including difficulty initiating and maintaining sleep and unrefreshing sleep, and twice as likely to report fatigue and daytime sleepiness even after controlling for age, body mass index (BMI), number of children younger than 18 y, work time, own snoring, and use of sleep medications.9 Symptoms associated with OSA are major causes of sleep disturbance among partners. Among 37 partners of patients suspected of having OSA, 55% reported that patients' snoring disturbed their sleep every night or almost every night.10 Baseline assessments from 46 partners of patients with OSA in a crossover trial of CPAP versus placebo found significant numbers who reported moderate to severe sleep disturbance because of snoring (69%), apneas (54%), and restlessness (55%), and 66% who were “poor” sleepers (i.e., Pittsburgh Sleep Quality Index score > 5).11 Qualitative data reveal that partners are distressed by witnessing patients' apneas and feel a need to monitor the patient's breathing during the night to ensure he/she continues to breathe.12,13
Table 1.
Effect of obstructive sleep apnea on partner-assessed outcomes.
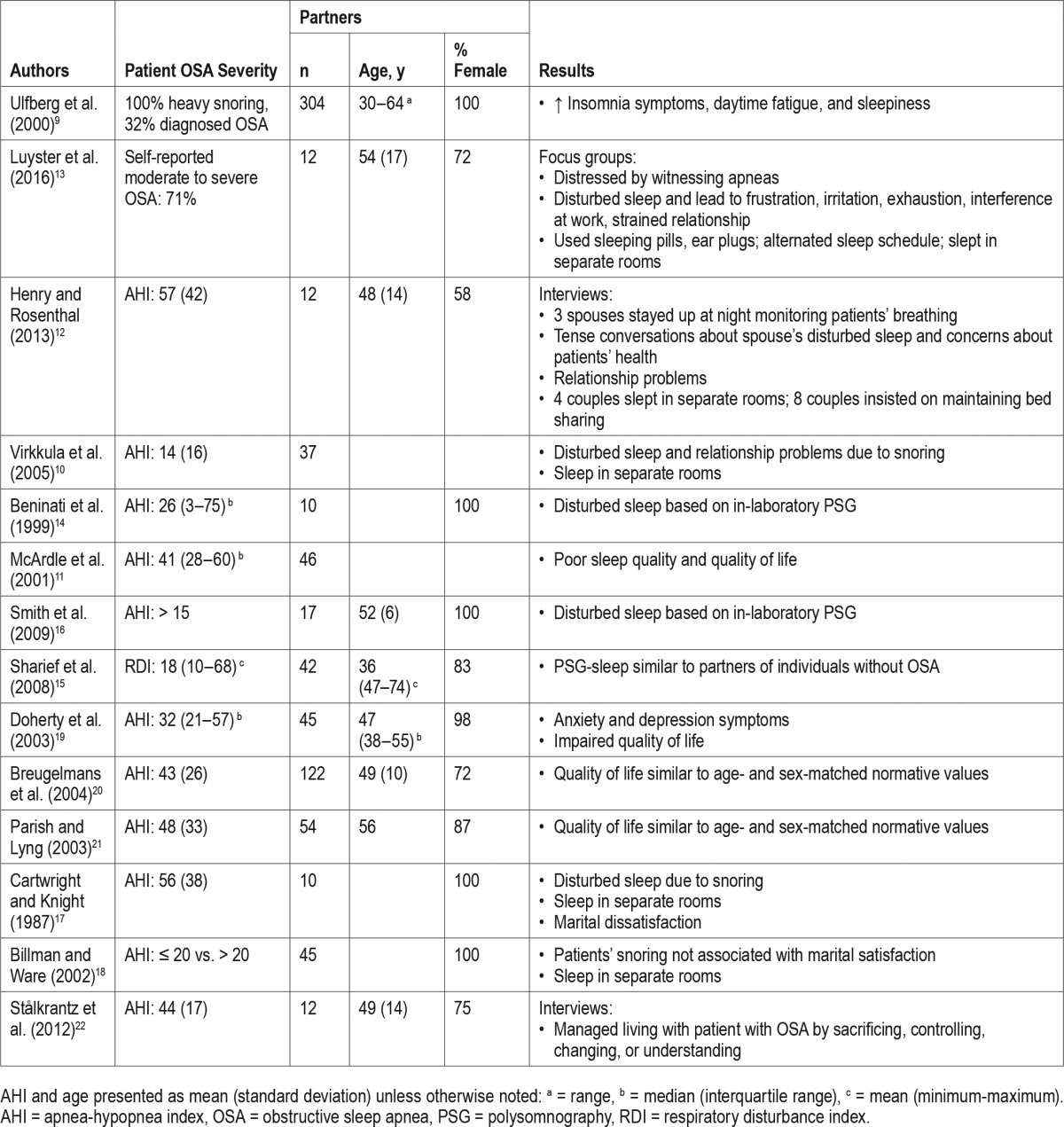
Studies utilizing PSG to assess sleep among partners of patients with untreated OSA also have found significant sleep disturbances.14–16 In an early study, 10 wives of husbands undergoing PSG for suspected OSA underwent concurrent PSG in the same bed as their husbands.14 Wives had a median PSG-assessed sleep efficiency of 74% and an arousal index of 21, with up to 32% having an arousal within 1 to 3 sec of a snore by the patient. A case-control study of 17 wives who regularly shared a bed with a spouse with untreated OSA found more wake after sleep onset, a higher percentage of stage 1 sleep, and alpha power during slow wave sleep during in-laboratory PSG without a shared bed compared to wives of healthy sleepers even after adjustment for age and menopausal status.16 In a cross-sectional study examining sleep of bed partners of individuals with OSA, 110 couples underwent in-home PSG and were classified according to OSA status into 1 of 3 groups: neither partner had OSA, one of the partners had OSA, or both had OSA.15 Comparison of sleep architecture and PSG-assessed sleep onset latency, total sleep time, and sleep efficiency between partners without OSA sleeping with OSA partners and partners sleeping with non-OSA partners showed no differences, suggesting that having a bed partner with OSA is not associated with worse sleep quality. In contrast to the previous studies that included clinic populations, this study included a community-based sample in which patients were not seeking treatment and had on average mild to moderate OSA severity.
In order to mitigate the disturbed sleep caused by the patients' OSA symptoms, partners report using ear plugs and/ or sleeping medication and alternating their sleep schedule with the patient.10,13 For some couples, patients' snoring and its interference with partners' sleep lead to sleeping in separate rooms.12,13,17 Others may insist on maintaining bed sharing despite disturbed sleep in order to avoid social stigma and to maintain the feeling of a “healthy” relationship.12 Partners' sleep loss often resulted in frustration, exhaustion, interference with work, and a strained relationship.13 In an early study, marital dissatisfaction, in particular conflict over childrearing, was reported by wives of OSA patients.17 Virkkula et al. found 35% of partners of men with suspected OSA (n = 37) reported relationship problems due to snoring.10 Although husbands' snoring was not associated with marital satisfaction among 45 wives of men with untreated OSA, they were 2.9 times more likely to sleep apart as compared to wives of men who did not snore frequently.18
Untreated OSA can negatively affect partners' quality of life.11,19 General health-related quality of life (mean 36-item Short Form Health Survey (SF-36) physical component summary score = 40.5 ± 14.2; mean SF-36 mental component summary score = 45.5 ± 11.3) was significantly worse among partners of patients with untreated OSA compared to the general population.11 Similarly, Doherty et al. found lower SF-36 scores among 55 partners of patients with OSA prior to initiation of CPAP therapy as compared to age- and sex-matched normative values, indicating impaired quality of life.19 More than 50% of partners reported anxiety symptoms and 18% reported depressive symptoms before CPAP treatment initiation. Conversely, a study of 122 partners of patients with untreated OSA found quality of life on the SF-36 to be similar to age- and sex-adjusted normative values.20 Parish and Lyng also found no significant difference in pretreatment quality of life between bed partners and national norms except for in the SF-36 domain of bodily pain.21 It is important to note that the aforementioned studies only included patients and partners who regularly shared a bed. Partners of patients who do not share a bed have been found to have worse quality of life and depression and anxiety symptoms than partners who share a bed with a patient with untreated OSA.19
Interviews with 12 spouses were conducted to learn about how they managed living with a patient with untreated OSA.22 Spouses expressed sacrificing their social activities and interactions in order to take on more of the household workload due to patients' tiredness. This often led to relationship problems and feeling like more of a caregiver than a spouse. Taking control was another way of managing the everyday life for the partner. Spouses thought it was their responsibility to help the patient by sharing the bedroom despite disturbed sleep to ensure the patient was breathing and making sure the patient received help and treatment for his or her symptoms, which lead to feeling like more of a parent than a spouse. Making changes to diet and lifestyle was also a means to dealing with their life situation. Spouses reported providing support to the patient and also engaging in these changes. Finally, spouses dealt with their life situation by feeling empathic toward the patient and consequently adapting daytime activities to the patient's tiredness and making the best of the situation.
Effect of OSA Treatments on Partners' Sleep and Daytime Functioning
CPAP Treatment
The majority of studies have found CPAP treatment in patients with OSA to have positive effects on their partners' physical and mental health, with improvements noted immediately and sustained up to 1 y (Table 2). Immediate increases in PSG-assessed sleep efficiency and percentage of rapid eye movement (REM) sleep and decreases in number of arousals and percentage of non-rapid eye movement sleep were noted in spouses when patients were treated with CPAP during an overnight diagnostic PSG study.14 No change in PSG-assessed total sleep time was found. In a cross-over study of CPAP versus placebo pill in 22 patients with OSA, partners of patients treated with CPAP had better sleep quality and less sleep disturbance at 1 mo compared to partners of patients treated with placebo.11 However, six partners reported moderate to severe sleep disturbance related to CPAP use, mainly from noise or cold air. No differences in daytime sleepiness, self-reported health, or marital satisfaction were found between partners of patients in the two treatment groups. Conversely, partners of male patients with moderate-severe OSA randomized to CPAP (n = 51) reported greater improvements in sleep quality, daytime alertness, mood, quality of life, and personal relationship with the patient (assessed by the Dublin Bed Partner's Assessment) at 4-w follow-up as compared to partners of patients randomized to sham CPAP (n = 51).23 These improvements have been found to be maintained up to 12 mo.24 Partners of 45 patients with OSA treated with CPAP for 6 w had less daytime sleepiness, anxiety symptoms, and better quality of life in the SF-36 domains of role-physical, role-emotion, social functioning, mental health, and vitality compared to before CPAP treatment.19 No changes in depressive symptoms nor the SF-36 domains of physical functioning, pain, and general health perception were found. Quality of life measured by the SF-36 and Sleep Apnea Quality of Life Index (SAQLI) were assessed in 54 partners of patients with OSA before and after 6 w of CPAP treatment.21 Significant improvements were found for daytime sleepiness, the SAQLI, and the role-physical, vitality, social functioning, and mental health domains of the SF-36, but the SF-36 domains of physical functioning, bodily pain, and role-emotional did not change from baseline. Following 12 w of CPAP treatment in 21 men with OSA, their female partners reported significant improvements in depression symptoms and overall sexual functioning assessed by the Female Sexual Function Index (FSFI) and within all 6 domains of the Female Sexual Function Index, including lubrication, orgasmic function, sexual desire, intercourse satisfaction, arousal, and pain.25 During focus groups conducted with spouses of patients with OSA managed with CPAP, partners described the experience of not hearing their partner snore during the first few nights with CPAP as alarming; however, after adjusting to this new occurrence, partners noted being able to fall asleep faster, having more energy, being happier, and resuming bed sharing.13
Table 2.
Effects of obstructive sleep apnea treatment on partner-assessed outcomes.
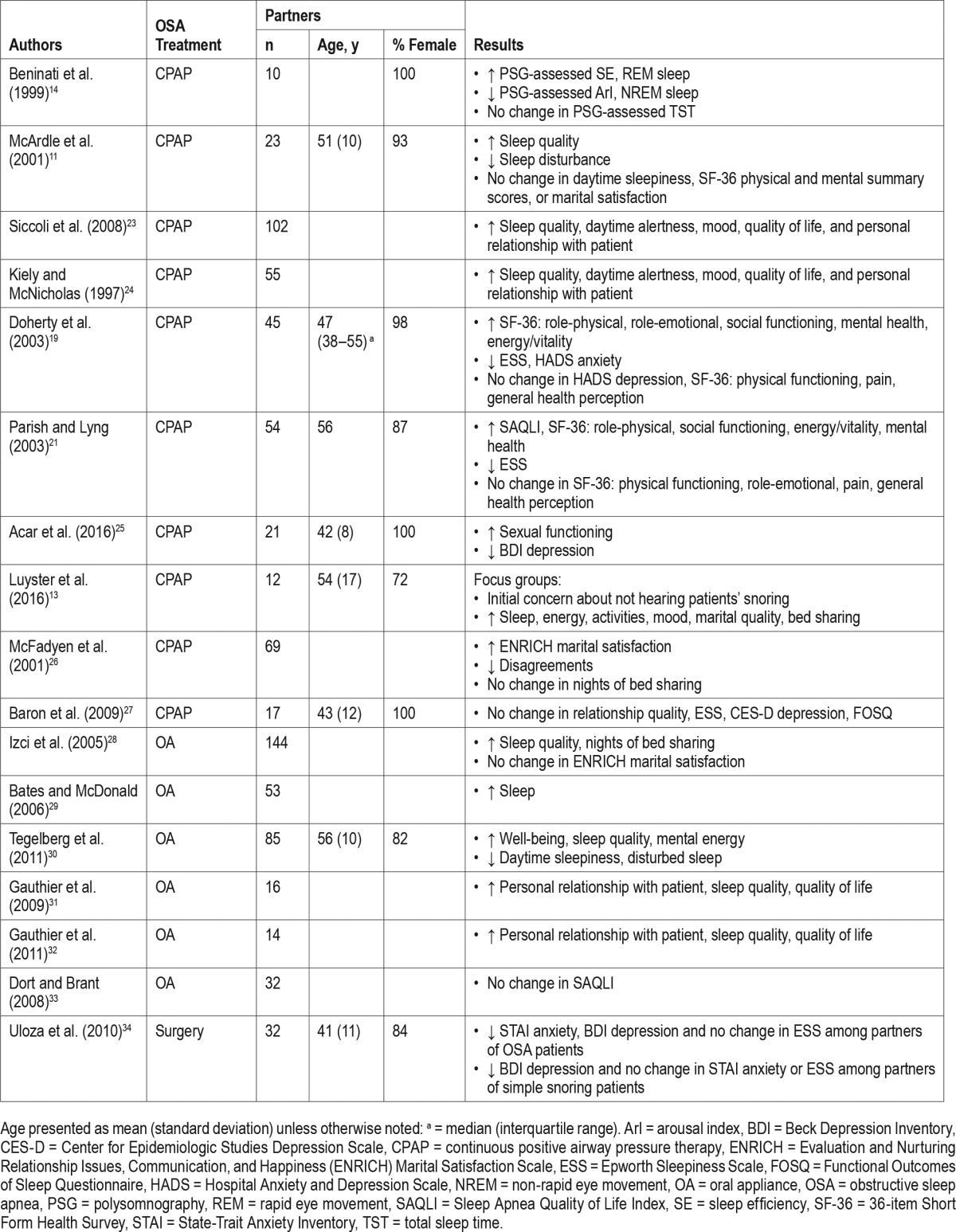
Studies examining the effect of CPAP treatment on marital satisfaction based on partners' report yield conflicting results. In a prospective trial of CPAP treatment versus conservative treatment (i.e., weight loss, sleeping posture, and avoidance of alcohol in the evening), 44 partners completed questionnaires about marital satisfaction before and 3 mo after treatment initiation.26 Partners of patients treated with CPAP had significantly greater improvements in marital satisfaction and less disagreements in the past week as compared to partners of patients treated conservatively. However, no difference in number of times per week of bed sharing were found between the groups. In contrast, Baron et al. did not find significant improvements in partners' reports of relationship quality, daytime sleepiness, depression, or functional impairment with 3 mo of CPAP treatment among their bed partners with OSA.27 It was noted that daytime sleepiness, depression, and functional impairment were at normal levels at baseline; thus, a floor effect could have contributed to the nonsignificant results.
Oral Appliances
In a study of 144 patients with OSA treated with an OA, partners of patients who reported continued use of their OA at a median 7 mo after fitting had greater improvement in sleep quality as compared to partners of patients who had discontinued OA use.28 Increased bed sharing was reported by partners of OA users, but no change in marital satisfaction was reported. Partners of non-OA users did not report changes in bed sharing frequency nor marital satisfaction. Another study of OA treatment among 121 patients with OSA found 64% of partners to report improvement in their sleep after 3 mo of treatment.29
Among 62 partners who share a bedroom with patients with OSA treated with an OA, more than half reported improvements in their general well-being, mental energy, and sleep quality and less daytime sleepiness and disturbed sleep after 1 y of treatment.30 In a comparative study of two OAs, 94% of partners (n = 16) reported improved sleep quality, quality of life, and personal relationship with the patient at 3-mo follow-up and these improvements were maintained at 2.5- to 4.5-y follow-up (n = 14).31,32
No improvements in quality of life assessed by the SAQLI were reported among 32 partners of patients with mild to moderate OSA participating in a randomized controlled crossover study of OA treatment versus a control device.33 The short study time period of 1-w acclimatization followed by a 1-w washout could account for these results.
Surgery
Changes in anxiety, depression, and daytime sleepiness were assessed in 36 partners of snoring and/or patients with OSA before and after patients received two sessions of radiofrequency tissue ablation treatment (RFTA).34 Significant reductions in anxiety and depression symptoms were found among partners of patients with OSA treated with RFTA, whereas no reduction in anxiety was found among partners of simple snoring patients treated with RFTA. No change in daytime sleepiness was detected for either group of partners.
Partner Involvement in OSA Treatment Adherence
Presence of Spouse or Live-In Partner
Limited data suggest that having a spouse or live-in partner can influence patients' acceptance and adherence to OSA treatment and that frequency of bed sharing may also have important implications for adherence (Table 3). Living with a partner was associated with CPAP acceptance among patients with OSA with average or high income, but was not a predictor of CPAP acceptance for low-income patients.35 Patients with a new diagnosis of OSA who reported living alone had significantly less CPAP use over the first month of treatment as compared to those living with a partner (3.6 h versus 5.0 h, respectively).36 Gagnadoux and colleagues found those who were married or living with a partner had a 1.5-fold increased likelihood of being adherent to CPAP (i.e., mean nightly hours of use ≥ 4 h) an average of 504 days after CPAP initiation among 1,141 patients with OSA.37 Conversely, a retrospective chart review of 33 older male patients with OSA found no significant difference in percentage of patients who had a spouse or live-in partner between those adherent (i.e., mean nightly hours of use ≥ 5 h) and not adherent to CPAP during a 6-mo period.38 In multivariate analysis controlling for age, BMI, daytime sleepiness, and apnea-hypopnea index (AHI), having a partner who sleeps in a separate room quadrupled the odds (odds ratio = 4.3, 95% confidence interval = 4.1–13.3) of purchasing a CPAP machine.39 Cartwright examined the association between bed sharing and CPAP adherence during the first 2 w of treatment.40 A greater number of nights the couple slept together based on wives' sleep log was significantly associated with higher average hours of CPAP use during the initial 2-w treatment period. Partners' reports of increased bed sharing since initiation of OA was associated with self-reported use of OA at a median 7 mo after fitting.28 Additionally, lower marital satisfaction before starting OA as reported by the partner was associated with continued OA use.
Table 3.
Partner involvement in obstructive sleep apnea treatment.
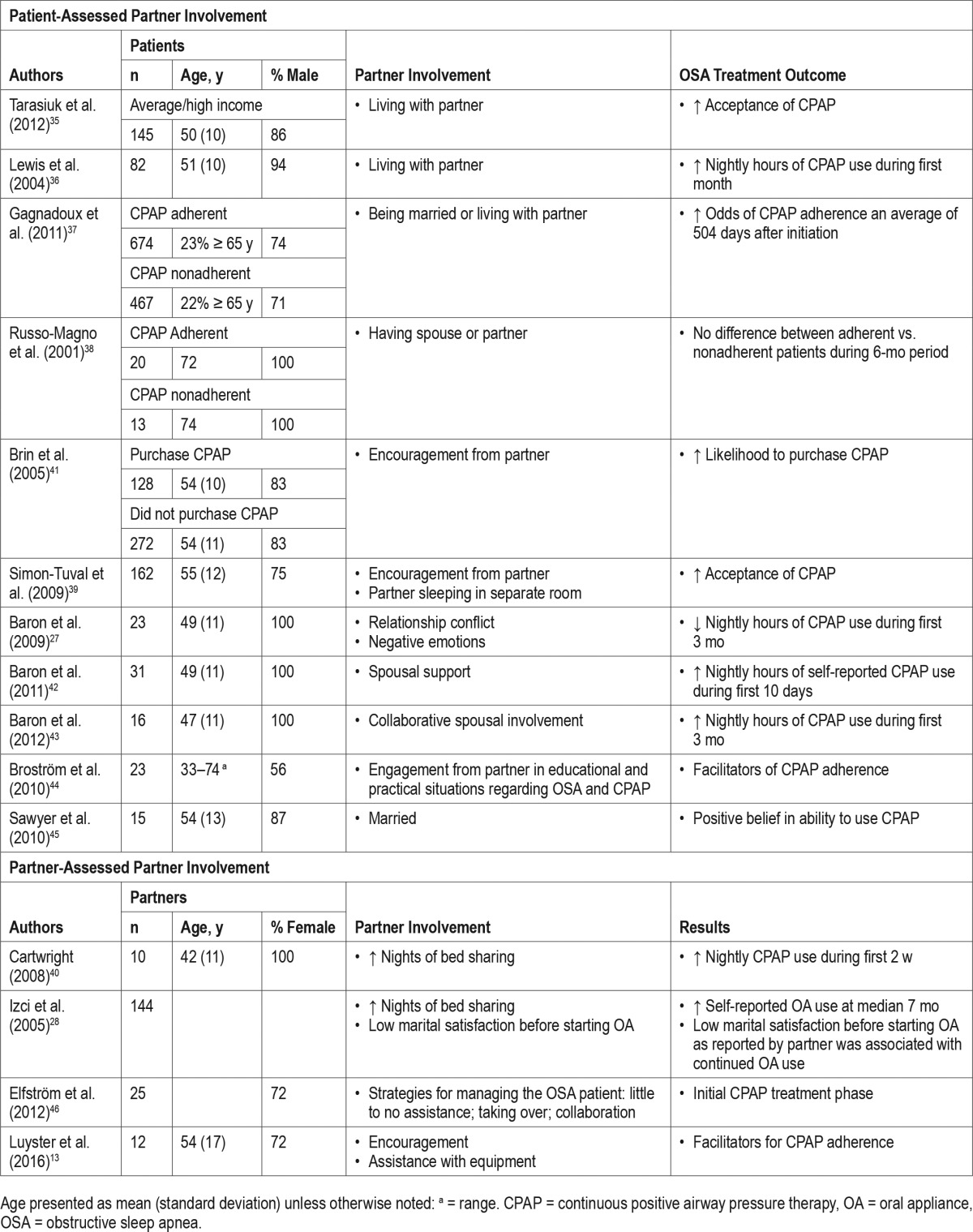
Partner Involvement
To date, studies assessing partner involvement in patients' use of his or her OSA treatment has focused solely on CPAP therapy. The majority of quantitative studies investigating the role of partners in patients' CPAP initiation and adherence have not obtained the partners' perspective but rather relied on patient assessment. Among patients with OSA who were recommended for CPAP therapy, 38% to 53% of patients who purchased CPAP reported receiving encouragement from their partner.39,41 In a prospective study of 23 married, male patients with OSA, marital conflict, in particular negative emotions such as anger, upset feelings, and criticism, reported by the patient was associated with lower CPAP adherence over the first 3 mo of treatment.27 Marital support reported by the patient was not associated with CPAP adherence.
To assess spousal involvement (i.e., pressure, collaboration, support) in CPAP therapy during the initial treatment phase, 31 male patients completed a daily questionnaire for a 10-day period starting within 1 w of receiving the CPAP machine in their home.42 The majority of patients (94%) expressed feeling supported by their spouse to use CPAP at least 1 day during the 10-day assessment period, whereas 13% did not report any spousal involvement. Perceptions of spouses' support predicted increased next-day self-reported CPAP use among patients with higher AHI. Following nights with decreased adherence, patients reported increased collaboration (e.g., helped with the machine) from their spouses the next day. Patients reporting low marital conflict reported greater increases in next-day collaboration following nights with CPAP problems (e.g., mask leaks, stuffy nose). Perceived pressure from spouses to use CPAP did not predict next-day adherence. A closer assessment of spousal involvement (i.e., collaborative, one-sided, positive, and negative) during the first 3 mo of CPAP treatment in 23 male patients with OSA revealed both positive (e.g., changed something at work or home to get me to use CPAP) and negative (e.g., tried to make me scared of the consequences of not using CPAP) involvement of wives approximately one to two times during the first week of treatment.43 Frequency of perceived spousal involvement remained the same at 3-mo follow-up except for negative involvement, which had decreased. Perceived collaborative spousal involvement was associated with greater CPAP adherence at 3 mo. One-sided, positive, and negative spousal involvement were not associated with 3-mo adherence.
Qualitative studies have captured both patients' and partners' perspectives of partners' involvement in the patients' use of CPAP. Semistructured interviews conducted with 23 CPAP-treated patients with OSA identified engagement of partners in education provided during diagnostic procedures and treatment initiation and in providing practical support (e.g., mask adjustments during the night) as facilitators for CPAP adherence.44 However, insufficient emotional and practical support from their partner was identified as a barrier for CPAP adherence. Similarly, partners identified providing emotional support (e.g., encouragement) and instrumental support (e.g., verbal reminders, help with putting on mask) as motivators for the patient to use CPAP during focus group discussions.13 During semistructured interviews with patients with OSA, unmarried patients described an absence of support, less belief in their ability to use CPAP, and fewer positive experiences with CPAP after the first week of treatment compared to married patients.45 Elfström et al. conducted semistructured interviews with 25 partners of patients with CPAP-treated OSA to learn about situations influencing partners' support to patients and strategies for managing these situations during the initial phase of CPAP treatment.46 Partners mentioned sounds from the mask or device that disturbed their sleep along with patients experiencing physical problems (e.g., mask leakage) or practical problems (e.g., traveling, limited sleeping positions) with the CPAP equipment as factors negatively affecting their willingness to support the patients' use of CPAP. Additionally, patients' shame, interference with closeness, and partners' limited presence were identified as situations negatively influencing support. Partners described an understanding of the consequences of OSA, positive treatment effects, patients' positive attitude about CPAP, and receiving support from family, friends, and healthcare professionals as motivators for providing support. Three management strategies used by the partners were identified: letting the patient handle the treatment themselves with little to no assistance from the partner; handling the treatment together with emotional and practical support provided by the partner; and taking over the treatment by supervising and controlling all practical aspects of the treatment, including giving out directives and ultimatums. From the patient perspective as expressed in the study by Broström et al.,44 a lack of emotional and practical support from a partner can deter adherence to CPAP therapy, thus a “hands-off” approach may not be the most effective strategy for partners during the CPAP initiation period.
CONCLUSIONS AND DIRECTIONS FOR FUTURE RESEARCH
Many adults sleep with a significant other, thus in the context of a sleep disorder such as OSA, its symptoms and treatments are likely to have profound effects on the well partners' sleep and daytime functioning. A growing body of literature suggests that OSA is a shared problem not only affecting patients but also partners, and that OSA treatments may also have beneficial effects for partners. Additionally, partners can positively and negatively influence patients' adoption and use of OSA treatments. This reviews highlights the importance of taking a dyadic (pairing of two individuals) perspective to the diagnosis and management of OSA.
Recent investigations have identified associations between patients' chronic illness symptoms (e.g., pain, physical limitations) and impairments in spouses' sleep and well-being.47–49 In the context of OSA, snoring contributes to partners' objective and subjective sleep disturbance. Qualitative studies suggest that partners' sleep may also be disturbed by monitoring the patients' breathing throughout the night due to witnessing apneas. It could be hypothesized that long-term exposure to untreated OSA could increase the risk of insomnia in bed-sharing partners, thus leading to both individuals having a sleep disorder. More detailed longitudinal studies are necessary to explore this possibility.
In a large population-based study of couples, both spouses' sleep problems (insomnia symptoms) and the partners' own sleep problems were associated with partners' poorer physical and mental health, well-being, social involvement, and marital quality.50 This finding suggests that the relationship problems, daytime sleepiness, anxiety and depression symptoms, and impaired quality of life reported by partners of patients with OSA could not only be the result of their own disturbed sleep but also the disturbed sleep of their OSA partner. Partners also reported frequently eliminating bed sharing. Sex differences in couples' sleep when co-sleeping and the interaction between sleep and relationship functioning have been identified in studies of healthy couples.51–54 Womens' objective and subjective sleep has been found to be disturbed by the presence of their male partner, whereas mens' subjective sleep improved with a woman's presence.54 An early study by Monroe found women to have significantly increased stage 4 sleep, greater total sleep time, and fewer awakenings than males when sleeping alone.52 Despite objective sleep disturbances experienced more frequently by women, they prefer to sleep with their partner.52,53 Among healthy co-sleeping couples, lower sleep efficiency predicted more negative perceptions of partner interactions the following day among males, whereas more negative perceptions of partner interactions predicted lower sleep efficiency that night for females.51 These findings suggest that sex of the partner is an important variable that needs to be considered in future studies examining the effects of OSA and its treatments on partners' sleep and daytime functioning. Sex differences were not examined in the studies included in this review. Although some of the studies did not report the demographics (e.g., sex) of the partners, those that did included a majority of women, which could have precluded the examination of sex differences.
OSA treatments, including CPAP, OA, and surgery, consistently were associated with improvements in partners' sleep. Discrepant results were reported for daytime sleepiness, quality of life, mood, and marital quality. Variation in assessments between studies and normal baseline levels of these variables could have accounted for the inconsistencies. Generally, patients' improvements in sleep and daytime functioning tracked with partners' improvements, although patients tended to have greater improvements than partners possibly because they were more impaired prior to treatment. Future research needs to examine cross-partner effects of OSA treatments on outcomes as improvements in patients' OSA symptoms, sleep, and well-being are likely to be associated with improvements in partners' sleep and well-being and vice versa. Adherence to OSA treatment also needs to be taken into consideration in future studies as improvements in patients' symptoms is dependent on consistent use, and thus partners' outcomes may be influenced by whether the patient is using his or her treatment. Interestingly, only one study of surgical treatment for OSA was identified that assessed partner outcomes.34 Most surgical trials obtained partners' assessment of patients' snoring without evaluation of how the partner was affected by the treatment. The scarcity of partner-assessed outcomes in OSA treatment studies, particularly surgical OSA treatment trials, raises the question of whether partner outcomes should be considered a standard outcome assessment in trials of OSA treatments.
An expansive body of literature demonstrates that partners can influence patients' health behaviors, with positive partner involvement (encouragement, collaborative approach) leading to greater patient engagement in the desired behavior, whereas negative partner involvement (criticizing, nagging) may back-fire and have opposite effects.55–62 Partners can positively and negatively affect all phases of CPAP therapy, from purchase to initiation and early and later use. Patients are frequently prompted by their partners to seek treatment in the first place, which can have potentially adverse consequences for CPAP adherence over time,63 particularly if participation is viewed by the patient as coercive. Partners can approach patients' initiation of CPAP differently, from being uninvolved to taking over all aspects to working together. These approaches can have a profound effect on patients' motivation to use CPAP. Limited studies suggest partner involvement that is collaborative and supportive is an important facilitator of CPAP use.42–44 Other than two qualitative studies,13,46 assessment of partner involvement has primarily been from the patients' perspective. Future research needs to take into consideration the dyadic nature of partner involvement and measure spousal involvement independently in both patients and partners as actual and perceived involvement may be incongruent. Other potentially important factors such as relationship quality, sex of the couple, and partners' knowledge and attitude toward OSA and CPAP should be considered when examining the association between partner involvement and CPAP adherence.64
A meta-analyses of couple-oriented interventions for chronic illnesses including cardiovascular disease, cancer, osteoarthritis, chronic pain, rheumatoid arthritis, human immunodeficiency virus, and type 2 diabetes found small but significant improvements in patient depressive symptoms, marital functioning, and pain.65 Additionally, couple-oriented interventions led to improvements in partners' psychological and marital functioning. It has been suggested that targeting partners' concerns and well-being and addressing communication and actions by the partner that can influence patients' health behaviors may strengthen the effects of couple-oriented interventions on patients' and partners' outcomes.65 A couple-oriented intervention aimed at improving CPAP adherence has not been developed. Two previous CPAP adherence intervention studies did mention the presence of partners during the intervention sessions, although these interventions were not couple-based.63,66 Focus group data from both OSA patients and their partners suggest that inclusion of partners in a new CPAP user program would be a key component.13 Partners expressed interest in participating in this type of program in order to obtain education about consequences of OSA and benefits of CPAP. Inclusion of partners throughout the diagnosis and treatment phases of OSA could help partners to feel more empowered to support the patient as he or she undertakes a challenging new treatment. Adoption of a collaborative approach to improving CPAP adherence may be a beneficial strategy for interventions promoting CPAP adherence.42,43
This review reveals the many opportunities for developing future studies to better understand the impact of OSA and OSA treatments on partners and partners' role in OSA treatment adherence. Longitudinal studies with assessments from both patients and partners will enable evaluation of interactive effects of health outcomes associated with OSA and its treatments. Greater insight into partners' perspectives of their involvement in CPAP treatment adherence and factors that affect their involvement could help guide the development of CPAP adherence interventions that are couple-based. Emphasis should be placed on clinician engagement of partners in discussions of negative health effects of OSA and benefits of OSA treatments for both patients and partners.
DISCLOSURE STATEMENT
This was not an industry supported study. Support for Dr. Luyster was provided by the National Heart, Lung, and Blood Institute (NHLBI) K23 HL105887. Dr. Luyster has indicated no financial conflicts of interest.
ABBREVIATIONS
- AHI
apnea-hypopnea index
- BMI
body mass index
- CPAP
continuous positive airway pressure
- FSFI
Female Sexual Function Index
- OA
oral appliance
- OSA
obstructive sleep apnea
- PSG
polysomnography
- REM
rapid eye movement
- RFTA
radio-frequency tissue ablation
- SAQLI
Sleep Apnea Quality of Life Index
- SF-36
36-item Short Form Health Survey
REFERENCES
- 1.Dong J-Y, Zhang Y-H, Qin L-Q. Obstructive sleep apnea and cardiovascular risk: meta-analysis of prospective cohort studies. Atherosclerosis. 2013;229(2):489–495. doi: 10.1016/j.atherosclerosis.2013.04.026. [DOI] [PubMed] [Google Scholar]
- 2.Ip MS, Lam B, Ng MM, Lam WK, Tsang KW, Lam KS. Obstructive sleep apnea is independently associated with insulin resistance. Am J Respir Crit Care Med. 2002;165(5):670–676. doi: 10.1164/ajrccm.165.5.2103001. [DOI] [PubMed] [Google Scholar]
- 3.Moyer CA, Sonnad SS, Garetz SL, Helman JI, Chervin RD. Quality of life in obstructive sleep apnea: a systematic review of the literature. Sleep Med. 2001;2(6):477–491. doi: 10.1016/s1389-9457(01)00072-7. [DOI] [PubMed] [Google Scholar]
- 4.Saunamäki T, Jehkonen M. Depression and anxiety in obstructive sleep apnea syndrome: a review. Acta Neurol Scand. 2007;116(5):277–288. doi: 10.1111/j.1600-0404.2007.00901.x. [DOI] [PubMed] [Google Scholar]
- 5.Antic NA, Catcheside P, Buchan C, et al. The effect of CPAP in normalizing daytime sleepiness, quality of life, and neurocognitive function in patients with moderate to severe OSA. Sleep. 2011;34(1):111–119. doi: 10.1093/sleep/34.1.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Barbé F, Durán-Cantolla J, Capote F, et al. Long-term effect of continuous positive airway pressure in hypertensive patients with sleep apnea. Am J Respir Crit Care Med. 2010;181(7):718–726. doi: 10.1164/rccm.200901-0050OC. [DOI] [PubMed] [Google Scholar]
- 7.Weaver TE, Grunstein RR. Adherence to continuous positive airway pressure therapy: the challenge to effective treatment. Proc Am Thorac Soc. 2008;5(2):173–178. doi: 10.1513/pats.200708-119MG. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.2005 Adult Sleep Habits and Styles. Summary of findings. National Sleep Foundation Web site. [Accessed January 4, 2017]. https://sleepfoundation.org/sleep-polls-data/sleep-in-america-poll/2005-adult-sleep-habits-and-styles. Published March 2005.
- 9.Ulfberg J, Carter N, Talback M, Edling C. Adverse health effects among women living with heavy snorers. Health Care Women Int. 2000;21(2):81–90. doi: 10.1080/073993300245311. [DOI] [PubMed] [Google Scholar]
- 10.Virkkula P, Bachour A, Hytönen M, Malmberg H, Salmi T, Maasilta P. Patient-and bed partner-reported symptoms, smoking, and nasal resistance in sleep-disordered breathing. Chest. 2005;128(4):2176–2182. doi: 10.1378/chest.128.4.2176. [DOI] [PubMed] [Google Scholar]
- 11.McArdle N, Kingshott R, Engleman H, Mackay T, Douglas N. Partners of patients with sleep apnoea/hypopnoea syndrome: effect of CPAP treatment on sleep quality and quality of life. Thorax. 2001;56(7):513–518. doi: 10.1136/thorax.56.7.513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Henry D, Rosenthal L. “Listening for his breath:” The significance of gender and partner reporting on the diagnosis, management, and treatment of obstructive sleep apnea. Soc Sci Med. 2013;79:48–56. doi: 10.1016/j.socscimed.2012.05.021. [DOI] [PubMed] [Google Scholar]
- 13.Luyster FS, Dunbar-Jacob J, Aloia MS, Martire LM, Buysse DJ, Strollo PJ. Patient and partner experiences with obstructive sleep apnea and cpap treatment: a qualitative analysis. Behav Sleep Med. 2016;14(1):67–84. doi: 10.1080/15402002.2014.946597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Beninati W, Harris CD, Herold DL, Shepard JW. The effect of snoring and obstructive sleep apnea on the sleep quality of bed partners. Mayo Clin Proc. 1999;74(10):955–958. doi: 10.4065/74.10.955. [DOI] [PubMed] [Google Scholar]
- 15.Sharief I, Silva GE, Goodwin JL, Quan SF. Effect of sleep disordered breathing on the sleep of bed partners in the sleep heart health study. Sleep. 2008;31(10):1449–1456. [PMC free article] [PubMed] [Google Scholar]
- 16.Smith AKA, Togeiro SMG, Tufik S, Roizenblatt S. Disturbed sleep and musculoskeletal pain in the bed partner of patients with obstructive sleep apnea. Sleep Med. 2009;10(8):904–912. doi: 10.1016/j.sleep.2008.08.013. [DOI] [PubMed] [Google Scholar]
- 17.Cartwright RD, Knight S. Silent partners: the wives of sleep apneic patients. Sleep. 1987;10(3):244–248. doi: 10.1093/sleep/10.3.244. [DOI] [PubMed] [Google Scholar]
- 18.Billmann SJ, Ware JC. Marital satisfaction of wives of untreated sleep apneic men. Sleep Med. 2002;3(1):55–59. doi: 10.1016/s1389-9457(01)00118-6. [DOI] [PubMed] [Google Scholar]
- 19.Doherty LS, Kiely JL, Lawless G, McNicholas WT. Impact of nasal continuous positive airway pressure therapy on the quality of life of bed partners of patients with obstructive sleep apnea syndrome. Chest. 2003;124(6):2209–2214. doi: 10.1378/chest.124.6.2209. [DOI] [PubMed] [Google Scholar]
- 20.Breugelmans JG, Ford DE, Smith PL, Punjabi NM. Differences in patient and bed partner-assessed quality of life in sleep-disordered breathing. Am J Respir Crit Care Med. 2004;170(5):547–552. doi: 10.1164/rccm.200310-1421OC. [DOI] [PubMed] [Google Scholar]
- 21.Parish JM, Lyng PJ. Quality of life in bed partners of patients with obstructive sleep apnea or hypopnea after treatment with continuous positive airway pressure. Chest. 2003;124(3):942–947. doi: 10.1378/chest.124.3.942. [DOI] [PubMed] [Google Scholar]
- 22.Stålkrantz A, Broström A, Wiberg J, Svanborg E, Malm D. Everyday life for the spouses of patients with untreated OSA syndrome. Scand J Caring Sci. 2012;26(2):324–332. doi: 10.1111/j.1471-6712.2011.00937.x. [DOI] [PubMed] [Google Scholar]
- 23.Siccoli MM, Pepperell JC, Kohler M, Craig SE, Davies RJ, Stradling JR. Effects of continuous positive airway pressure on quality of life in patients with moderate to severe obstructive sleep apnea: data from a randomized controlled trial. Sleep. 2008;31(11):1551–1558. doi: 10.1093/sleep/31.11.1551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kiely JL, McNicholas WT. Bed partners' assessment of nasal continuous positive airway pressure therapy in obstructive sleep apnea. Chest. 1997;111(5):1261–1265. doi: 10.1378/chest.111.5.1261. [DOI] [PubMed] [Google Scholar]
- 25.Acar M, Kaya C, Catli T, Hancı D, Bolluk O, Aydin Y. Effects of nasal continuous positive airway pressure therapy on partners' sexual lives. Euro Arch Otorhinolaryngol. 2016;273(1):133–137. doi: 10.1007/s00405-015-3546-4. [DOI] [PubMed] [Google Scholar]
- 26.McFadyen T, Espie C, McArdle N, Douglas N, Engleman H. Controlled, prospective trial of psychosocial function before and after continuous positive airway pressure therapy. Eur Respir J. 2001;18(6):996–1002. doi: 10.1183/09031936.01.00209301. [DOI] [PubMed] [Google Scholar]
- 27.Baron KG, Smith TW, Czajkowski LA, Gunn HE, Jones CR. Relationship quality and CPAP adherence in patients with obstructive sleep apnea. Behav Sleep Med. 2009;7(1):22–36. doi: 10.1080/15402000802577751. [DOI] [PubMed] [Google Scholar]
- 28.Izci B, McDonald JP, Coleman EL, Mackay TW, Douglas NJ, Engleman HM. Clinical audit of subjects with snoring & sleep apnoea/hypopnoea syndrome fitted with mandibular repositioning splint. Respir Med. 2005;99(3):337–346. doi: 10.1016/j.rmed.2004.07.007. [DOI] [PubMed] [Google Scholar]
- 29.Bates C, McDonald J. Patients' and sleeping partners' experience of treatment for sleep-related breathing disorders with a mandibular repositioning splint. Br Dent J. 2006;200(2):95–101. doi: 10.1038/sj.bdj.4813149. [DOI] [PubMed] [Google Scholar]
- 30.Tegelberg A, Nohlert E, Bergman L-E, Andrén A. Bed partners' and patients' experiences after treatment of obstructive sleep apnoea with an oral appliance. Swed Dent J. 2011;36(1):35–44. [PubMed] [Google Scholar]
- 31.Gauthier L, Laberge L, Beaudry M, Laforte M, Rompré PH, Lavigne GJ. Efficacy of two mandibular advancement appliances in the management of snoring and mild-moderate sleep apnea: a cross-over randomized study. Sleep Med. 2009;10(3):329–336. doi: 10.1016/j.sleep.2008.03.011. [DOI] [PubMed] [Google Scholar]
- 32.Gauthier L, Laberge L, Beaudry M, Laforte M, Rompré PH, Lavigne GJ. Mandibular advancement appliances remain effective in lowering respiratory disturbance index for 2.5-4.5 years. Sleep Med. 2011;12(9):844–849. doi: 10.1016/j.sleep.2011.05.004. [DOI] [PubMed] [Google Scholar]
- 33.Dort L, Brant R. A randomized, controlled, crossover study of a noncustomized tongue retaining device for sleep disordered breathing. Sleep Breath. 2008;12(4):369–373. doi: 10.1007/s11325-008-0187-5. [DOI] [PubMed] [Google Scholar]
- 34.Uloza V, Balsevičius T, Sakalauskas R, Miliauskas S, Zemaitienė N. Changes in emotional state of bed partners of snoring and obstructive sleep apnea patients following radiofrequency tissue ablation: a pilot study. Sleep Breath. 2010;14(2):125–130. doi: 10.1007/s11325-009-0293-z. [DOI] [PubMed] [Google Scholar]
- 35.Tarasiuk A, Reznor G, Greenberg-Dotan S, Reuveni H. Financial incentive increases CPAP acceptance in patients from low socioeconomic background. PLoS One. 2012;7(3):e33178. doi: 10.1371/journal.pone.0033178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lewis KE, Seale L, Bartle IE, Watkins AJ, Ebden P. Early predictors of CPAP use for the treatment of obstructive sleep apnea. Sleep. 2004;27(1):134–138. doi: 10.1093/sleep/27.1.134. [DOI] [PubMed] [Google Scholar]
- 37.Gagnadoux F, Le Vaillant M, Goupil F, et al. Influence of marital status and employment status on long-term adherence with continuous positive airway pressure in sleep apnea patients. PLoS One. 2011;6(8):e22503. doi: 10.1371/journal.pone.0022503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Russo-Magno P, O'Brien A, Panciera T, Rounds S. Compliance with CPAP therapy in older men with obstructive sleep apnea. J Am Geriatr Soc. 2001;49(9):1205–1211. doi: 10.1046/j.1532-5415.2001.49238.x. [DOI] [PubMed] [Google Scholar]
- 39.Simon-Tuval T, Reuveni H, Greenberg-Dotan S, Oksenberg A, Tal A, Tarasiuk A. Low socioeconomic status is a risk factor for CPAP acceptance among adult OSAS patients requiring treatment. Sleep. 2009;32(4):545–552. doi: 10.1093/sleep/32.4.545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cartwright R. Sleeping together: a pilot study of the effects of shared sleeping on adherence to CPAP treatment in obstructive sleep apnea. J Clin Sleep Med. 2008;4(2):123–127. [PMC free article] [PubMed] [Google Scholar]
- 41.Brin YS, Reuveni H, Greenberg S, Tal A, Tarasiuk A. Determinants affecting initiation of continuous positive airway pressure treatment. Isr Med Assoc J. 2005;7(1):13–18. [PubMed] [Google Scholar]
- 42.Baron KG, Smith TW, Berg CA, Czajkowski LA, Gunn H, Jones CR. Spousal involvement in CPAP adherence among patients with obstructive sleep apnea. Sleep Breath. 2011;15(3):525–534. doi: 10.1007/s11325-010-0374-z. [DOI] [PubMed] [Google Scholar]
- 43.Baron KG, Gunn HE, Czajkowski LA, Smith TW, Jones CR. Spousal involvement in CPAP: does pressure help? J Clin Sleep Med. 2012;8(2):147–153. doi: 10.5664/jcsm.1766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Broström A, Nilsen P, Johansson P, et al. Putative facilitators and barriers for adherence to CPAP treatment in patients with obstructive sleep apnea syndrome: a qualitative content analysis. Sleep Med. 2010;11(2):126–130. doi: 10.1016/j.sleep.2009.04.010. [DOI] [PubMed] [Google Scholar]
- 45.Sawyer AM, Deatrick JA, Kuna ST, Weaver TE. Differences in perceptions of the diagnosis and treatment of obstructive sleep apnea and continuous positive airway pressure therapy among adherers and nonadherers. Qual Health Res. 2010;20(7):873–892. doi: 10.1177/1049732310365502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Elfström M, Karlsson S, Nilsen P, Fridlund B, Svanborg E, Broström A. Decisive situations affecting partners' support to continuous positive airway pressure-treated patients with obstructive sleep apnea syndrome: a critical incident technique analysis of the initial treatment phase. J Cardiovasc Nurs. 2012;27(3):228–239. doi: 10.1097/JCN.0b013e3182189c34. [DOI] [PubMed] [Google Scholar]
- 47.Lyons KS, Bennett JA, Nail LM, Fromme EK, Dieckmann N, Sayer AG. The role of patient pain and physical function on depressive symptoms in couples with lung cancer: a longitudinal dyadic analysis. J Fam Psychol. 2014;28(5):692–700. doi: 10.1037/fam0000017. [DOI] [PubMed] [Google Scholar]
- 48.Martire LM, Keefe FJ, Schulz R, Stephens MAP, Mogle JA. The impact of daily arthritis pain on spouse sleep. Pain. 2013;154(9):1725–1731. doi: 10.1016/j.pain.2013.05.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Polenick CA, Martire LM, Hemphill RC, Stephens MAP. Effects of change in arthritis severity on spouse well-being: the moderating role of relationship closeness. J Fam Psychol. 2015;29(3):331–338. doi: 10.1037/fam0000093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Strawbridge WJ, Shema SJ, Roberts RE. Impact of spouses' sleep problems on partners. Sleep. 2004;27(3):527–535. doi: 10.1093/sleep/27.3.527. [DOI] [PubMed] [Google Scholar]
- 51.Hasler BP, Troxel WM. Couples' nighttime sleep efficiency and concordance: Evidence for bidirectional associations with daytime relationship functioning. Psychosom Med. 2010;72(8):794–801. doi: 10.1097/PSY.0b013e3181ecd08a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Monroe LJ. Transient changes in EEG sleep patterns of married good sleepers: the effects of altering sleeping arrangement. Psychophysiology. 1969;6(3):330–337. doi: 10.1111/j.1469-8986.1969.tb02910.x. [DOI] [PubMed] [Google Scholar]
- 53.Pankhurst FP, Horne JA. The influence of bed partners on movement during sleep. Sleep. 1994;17(4):308–315. doi: 10.1093/sleep/17.4.308. [DOI] [PubMed] [Google Scholar]
- 54.Dittami J, Keckeis M, Machatschke I, Katina S, Zeitlhofer J, Kloesch G. Sex differences in the reactions to sleeping in pairs versus sleeping alone in humans. Sleep Biol Rhythms. 2007;5:271–276. [Google Scholar]
- 55.DiMatteo MR. Social support and patient adherence to medical treatment: a meta-analysis. Health Psychol. 2004;23(2):207–218. doi: 10.1037/0278-6133.23.2.207. [DOI] [PubMed] [Google Scholar]
- 56.Franks MM, Stephens MAP, Rook KS, Franklin BA, Keteyian SJ, Artinian NT. Spouses' provision of health-related support and control to patients participating in cardiac rehabilitation. J Fam Psychol. 2006;20(2):311–318. doi: 10.1037/0893-3200.20.2.311. [DOI] [PubMed] [Google Scholar]
- 57.Helgeson VS, Novak SA, Lepore SJ, Eton DT. Spouse social control efforts: Relations to health behavior and well-being among men with prostate cancer. J Soc Pers Relat. 2004;21:53–68. [Google Scholar]
- 58.Khan CM, Stephens MAP, Franks MM, Rook KS, Salem JK. Influences of spousal support and control on diabetes management through physical activity. Health Psychol. 2013;32(7):739–747. doi: 10.1037/a0028609. [DOI] [PubMed] [Google Scholar]
- 59.Lewis MA, Butterfield RM. Social control in marital relationships: effect of one's partner on health behaviors. J Appl Soc Psychol. 2007;37:298–319. [Google Scholar]
- 60.Stephens MAP, Fekete EM, Franks MM, Rook KS, Druley JA, Greene K. Spouses' use of pressure and persuasion to promote osteoarthritis patients' medical adherence after orthopedic surgery. Health Psychol. 2009;28(1):48–55. doi: 10.1037/a0012385. [DOI] [PubMed] [Google Scholar]
- 61.Stephens MAP, Franks MM, Rook KS, Iida M, Hemphill RC, Salem JK. Spouses' attempts to regulate day-to-day dietary adherence among patients with type 2 diabetes. Health Psychol. 2013;32(10):1029–1037. doi: 10.1037/a0030018. [DOI] [PubMed] [Google Scholar]
- 62.Stephens MAP, Rook KS, Franks MM, Khan C, Iida M. Spouses use of social control to improve diabetic patients' dietary adherence. Fam Syst Health. 2010;28(3):199–208. doi: 10.1037/a0020513. [DOI] [PubMed] [Google Scholar]
- 63.Hoy CJ, Vennelle M, Kingshott RN, Engleman HM, Douglas NJ. Can intensive support improve continuous positive airway pressure use in patients with the sleep apnea/hypopnea syndrome? Am J Respir Crit Care Med. 1999;159(4 Pt 1):1096–1100. doi: 10.1164/ajrccm.159.4.9808008. [DOI] [PubMed] [Google Scholar]
- 64.Ye L, Malhotra A, Kayser K, et al. Spousal involvement and CPAP adherence: a dyadic perspective. Sleep Med Rev. 2014;19:67–74. doi: 10.1016/j.smrv.2014.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Martire LM, Schulz R, Helgeson VS, Small BJ, Saghafi EM. Review and meta-analysis of couple-oriented interventions for chronic illness. Ann Behav Med. 2010;40(3):325–342. doi: 10.1007/s12160-010-9216-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Richards D, Bartlett DJ, Wong K, Malouff J, Grunstein RR. Increased adherence to CPAP with a group cognitive behavioral treatment intervention: a randomized trial. Sleep. 2007;30(5):635–640. doi: 10.1093/sleep/30.5.635. [DOI] [PubMed] [Google Scholar]


