Abstract
Continuous positive airway pressure (CPAP) intolerance remains a persistent problem for many obstructive sleep apnea patients. Clinicians and researchers continue to search for other effective treatment modalities given the well-documented sequelae associated with untreated obstructive sleep apnea.
A multidisciplinary “Alternatives to CPAP program” (ALT) can facilitate systematic evaluation of non-CPAP therapies appropriate for an individual patient. We review successful strategies and barriers encountered during implementation of an ALT at our institution. Creation of similar programs in private practice and academic settings can help medical, dental, and surgical sleep medicine specialists coordinate evaluation and treatment of CPAP-intolerant patients.
Citation:
Shelgikar AV, Aronovich S, Stanley JJ. Multidisciplinary alternatives to CPAP program for CPAP-intolerant patients. J Clin Sleep Med. 2017;13(3):505–510.
Keywords: alternative treatments, CPAP intolerance surgery, multidisciplinary, obstructive sleep apnea, oral appliance
INTRODUCTION
Multidisciplinary treatment approaches are used for chronic disease management in adult and pediatric patients.1–3 Multidisciplinary care may provide benefits to patients with obstructive sleep apnea (OSA),4 a complex disease process with anatomic and neurologic etiologies. Although continuous positive airway pressure (CPAP) therapy remains the gold standard treatment for OSA, many CPAP-intolerant patients often discontinue therapy and thus go untreated.5 When patients explore non-CPAP treatments for OSA, communication between providers and patients can generate confusion because of the variety of non-CPAP treatment options currently available. Integrated care models with dentistry and sleep medicine have been previously described,6 as have examples of coordinated dental and surgical care for treatment of OSA.7 Optimal and personalized treatment of CPAP-intolerant patients requires the skills and knowledge of medical and dental professionals from a variety of specialties, including sleep medicine, dentistry, oral and maxillofacial surgery, and otolaryngology.
A multidisciplinary “Alternatives to CPAP program” (ALT) was started at our institution to address these potential issues and to improve the care of CPAP-intolerant patients. We discuss the operational planning of an ALT, descriptions of each provider's role, and experiences from our ALT. We also review opportunities within an ALT to enhance interprofessional education.
WHY AN ALT WAS ESTABLISHED
The University of Michigan's ALT was established to enhance patient-provider and provider-provider communication and to reduce fragmentation of care. The stated goals of this program are to (1) facilitate evaluation and treatment of patients who are unable or unwilling to use CPAP, (2) improve communication between surgeons, dentists, and sleep medicine physicians, and (3) educate fellows and residents in sleep medicine, dentistry, oral and maxillofacial surgery, and otolaryngology.
LOGISTICAL CONSIDER ATIONS WHEN STARTING AN ALT
A dedicated program coordinator is charged with (1) patient scheduling, (2) confirmation of insurance prior authorization when necessary, (3) requisition of outside records (including sleep studies and previous surgical notes), (4) appointment coordination, and (5) maintenance of an ALT database.
To optimize ALT efficiency and effectiveness, patients are scheduled for consultation in the “ALT screening clinic” with a sleep medicine specialist to determine whether an ALT visit is the appropriate next step. Those patients who are willing to troubleshoot difficulties with and continue using CPAP are not scheduled into the ALT.
Patients who are unable or unwilling to use CPAP further are then scheduled for an ALT visit. These patients must have polysomnographically confirmed OSA within the past 3 y, or more recently for patients with a significant interval change in weight or health status. Home sleep apnea test results are considered on a case-by-case basis; some patients are requested to have an attended polysomnogram before an ALT treatment recommendation is finalized. There is no body mass index (BMI) or OSA severity cutoff for a patient to be scheduled for ALT evaluation, but these factors are considered in the development of an ALT treatment plan.
Insurance prior authorization requirements are often region-specific and should be carefully addressed when starting and sustaining an ALT. Need for prior authorizations is clearly discussed with patients before an ALT visit is scheduled, and the ALT program coordinator ensures that all needed prior authorizations are obtained before ALT treatment is implemented.
ALT team members must agree on available days and clinic space. Fiberoptic endoscopes, cephalometric radiography, cone-beam computed tomography, and related support staff must also be available to maintain efficient patient throughput in the ALT.
ROLE OF EACH PROVIDER IN AN ALT
Table 1 summarizes the role of each provider in a multidisciplinary “Alternatives to CPAP program.” Every ALT patient is seen by each ALT provider during the appointment.
Table 1.
Role of each specialist in a multidisciplinary “Alternatives to CPAP program.”
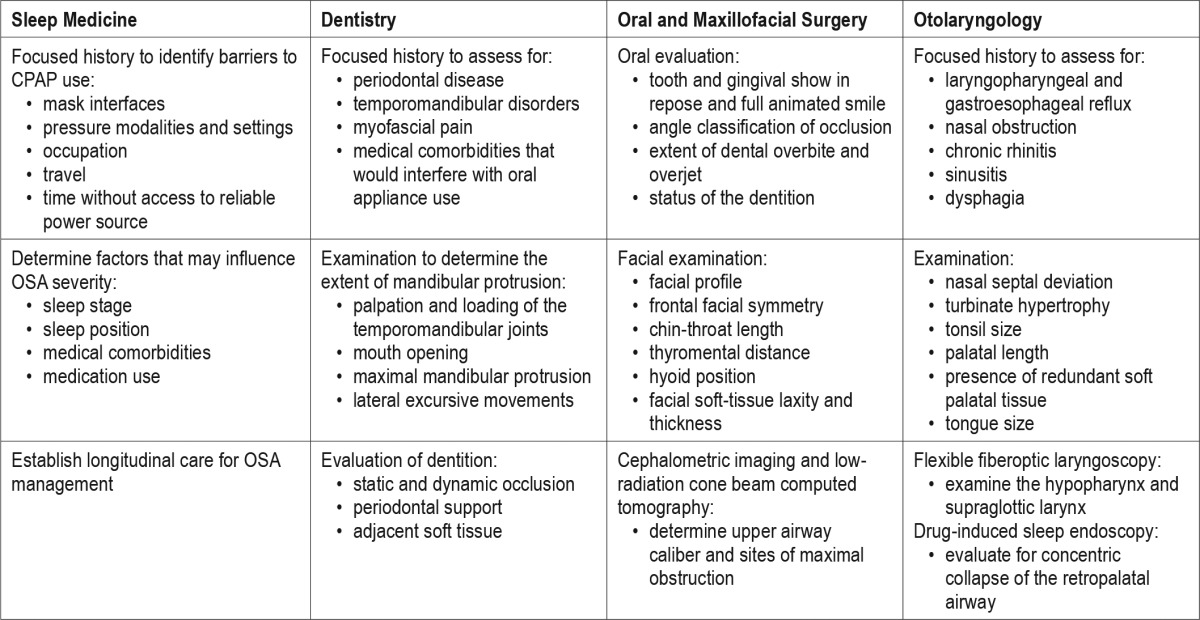
Sleep Medicine
The sleep medicine specialist meets with each patient to discuss sleep study results and review the patient's barriers to CPAP, then presents this information at the multidisciplinary ALT conference so that all ALT providers have a shared understanding of the patient's history. Patients with morbid obesity (BMI > 40 kg/m2) and associated co-morbidities may be referred for formal evaluation by the bariatric surgery program. Others with a BMI > 30 may be referred to the medical weight loss program as a component of their OSA management. Referral to medical weight loss programs may be considered on a case-by-case basis. Positional therapy is discussed for appropriate patients. Last, the sleep medicine specialist reinforces to ALT patients the importance of effective, long-term OSA treatment.
Dentistry
A dental sleep medicine specialist determines an ALT patient's candidacy for oral appliance therapy. Patients with mild to moderate OSA are most likely to benefit.8 Relative contraindications to treatment include seizure disorders, spastic cerebral palsy, rheumatoid arthritis involving the temporomandibular joints, Sjögren syndrome with xerostomia, certain psychiatric disorders, or fibromyalgia with associated myofascial pain of the head and neck. Location of any head and neck pain, type of diet tolerated, presence of limited mouth opening, history of lockjaw, difficulty with chewing or talking, history of facial trauma, and history of bruxism or periodontal disease may influence a patient's candidacy for oral appliance therapy.9 ALT patients are evaluated for extent of mouth opening, maximal mandibular protrusion, and lateral excursive movements to determine the feasibility of obtaining impressions and the extent of mandibular protrusion.
Oral and Maxillofacial Surgery
Unique components of the maxillofacial examination include the facial profile, projection of the mandible and maxilla, frontal facial symmetry, chin-throat length, thyromental distance, hyoid position, and facial soft-tissue laxity and thickness.10 Patients in the ALT undergo a two- and three-dimensional radiographic survey of the upper airway that helps identify sites of maximal obstruction. A panoramic radiograph screens for dental, temporomandibular joint, or maxillofacial pathology that may require treatment prior to surgical intervention. A lateral cephalogram is obtained in natural head position to assess skeletal relations of the maxilla and mandible, hyoid position, airway length, soft palate length, anterior skull base angle, and the posterior airway space.11 A low-radiation cone beam computed tomography scan provides three-dimensional data to determine the upper airway volume from the hard palatal plane (superior boundary) to the base of the epiglottis (inferior boundary), as well as the minimal cross-sectional area and its location.
Oral and maxillofacial surgeons may offer maxillomandibular advancement surgery and/or genioglossus advancement to ALT patients. Although maxillomandibular advancement is typically reserved for select patients with moderate to severe OSA,12 genioglossus advancement alone may have utility in select patients with mild or moderate OSA. These procedures expand the facial skeleton anteriorly and displace all associated soft-tissue and muscle attachments to achieve multilevel (via maxillomandibular advancement) or retroglossal (via genioglossus advancement) expansion of the upper airway.13 Negative postoperative alterations in facial appearance are typically minimized by selecting patients with a retrognathic maxillomandibular complex and undersupported or lax facial soft tissues.
Otolaryngology
Laryngopharyngeal and gastroesophageal reflux symptoms,14 nasal obstruction, and chronic rhinitis and sinusitis symptoms are explored. Nasal septal deviation, turbinate hypertrophy, tonsil size, palatal length, presence of redundant palatal tissue and macroglossia (a tongue that resides above the occlusal plane), or relative macroglossia (a size disproportion between the width of the tongue versus the mandibular arch) are identified. Tongue position is rated with the Friedman classification (tongue in a natural, neutral position within the mouth) and the modified Mallampati classification (tongue at maximal protrusion). The tongue position with the Friedman classification has been correlated with surgical outcomes15 and the tongue position with the Mallampati classification has been associated with likelihood of difficult endotracheal intubation.16
All patients seen in the ALT undergo flexible fiberoptic laryngoscopy, which evaluates the hypopharynx and supraglottic larynx for significant narrowing of the posterior airway space. Currently, only those ALT patients who are possible candidates for hypoglossal nerve stimulation undergo drug-induced sleep endoscopy; these patients may consider hypoglossal nerve stimulation if the absence of concentric retropalatal collapse is confirmed during drug-induced sleep endoscopy17 and the other United States Food and Drug Administration-approved criteria are met, including apnea-hypopnea index of 20–65 events/h and BMI < 32 kg/m2.
The otolaryngologic surgeries offered to ALT patients can be adjunctive, salvage, or curative. Adjunctive nasal surgery may facilitate improved postoperative CPAP adherence due to lower CPAP requirements (average of 2–3 cm H2O) or improved tolerance of nasal-type masks without necessity for a chin strap.18 Salvage surgeries, such as isolated palatal surgeries and multilevel procedures combining palatal and hypopharyngeal surgeries,19,20 have been shown to reduce OSA severity and improve quality-of-life measures. Curative otolaryngologic surgery has historically been limited to tracheostomy, which may be indicated for patients with severe OSA and associated comorbidities.21 Hypoglossal nerve stimulation may effectively treat some patients with moderate to severe OSA.22
PATIENT FLOW THROUGH AN ALT
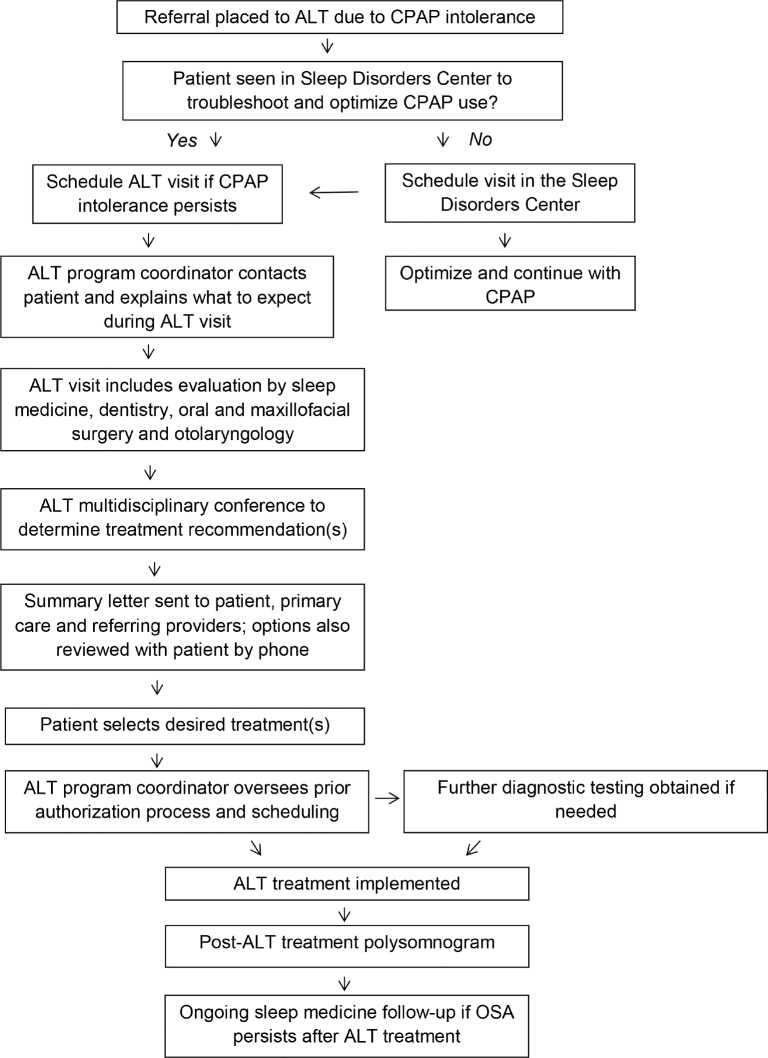
Figure 1 depicts the ALT process flow. During the multidisciplinary case conference at the conclusion of each clinic, the sleep medicine specialist guides the group discussion in a standardized format. An individual treatment plan is formulated, taking into account (1) the patient's physical examination findings including BMI and identified site(s) of obstruction, (2) polysomnography findings with attention to the severity and positional/sleep stage dependence, (3) general medical status, and importantly, (4) patient preference.
Figure 1. Alternatives to CPAP program flow algorithm.
ALT = Alternatives to CPAP program, CPAP = continuous positive airway pressure, OSA = obstructive sleep apnea.
A summary letter with treatment options prioritized as ALT team consensus recommendations is sent to the patient, primary care provider, and referring provider. The sleep medicine specialist calls the patient to review the proposed treatment options. After the patient agrees to a treatment plan, further testing (if needed) and appointments are scheduled through the appropriate service (e.g., operating room scheduling, dental moldings, etc.). Sleep clinic follow-up is also arranged to ensure posttreatment polysomnography and longitudinal management of each patient's OSA.
DATA FROM OUR ALT
The University of Michigan ALT database was reviewed from January 1, 2006 through December 1, 2015. Potential treatment options offered to ALT patients during this time period are summarized in Table 2. This work received an exemption from the University of Michigan institutional review board, identification number HUM00120049.
Table 2.
Treatment options offered to patients seen in the University of Michigan Alternatives to CPAP program from 2006-2015.
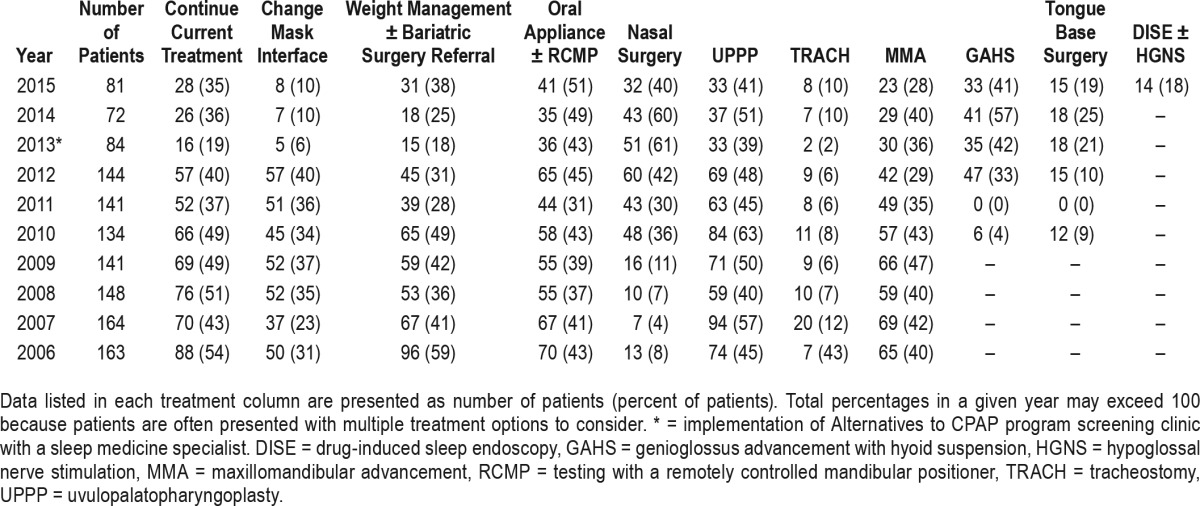
The data presented include 7 y (2006–2012) during which all patients referred to the ALT were scheduled for an ALT visit, along with 3 y (2013–2015) in which patients were seen in an ALT screening clinic with a sleep medicine specialist to determine if evaluation by all ALT providers was appropriate. Implementation of the ALT screening clinic nearly halved the total number of patients seen in the ALT. In turn, the percentage of patients advised to try a new mask interface or continue with current therapy decreased and the percentage of patients offered certain non-CPAP treatment options increased. It has been our experience that an effective ALT screening clinic identifies patients who should continue efforts with CPAP versus those patients unwilling or unable to use CPAP who should receive a comprehensive ALT evaluation to consider non-CPAP treatments for OSA. The overall utility of the ALT experience is subsequently enhanced for both patients and providers.
Some of the variability in non-CPAP treatments offered to ALT patients may reflect different practice styles of ALT providers. Multiple providers from each specialty have participated in our ALT since its establishment. Differences in individual preferences, evolution of surgical techniques, and incorporation of new technologies may also add to variations in the ALT treatment options offered to patients over time.
PREINTERVENTION AND POSTINTERVENTION POLYSOMNOGR APHY
As previously noted, ALT patients should have a baseline polysomnogram within the past 3 y or more recently if there has been an interval change in weight or health status. The ALT program coordinator obtains insurance authorization before postintervention polysomnography is scheduled. After insurance authorization is obtained, patients who are candidates for mandibular advancement devices should undergo a titration study with various degrees of mandibular protrusion to determine the therapeutic potential of oral appliance therapy.23 Following surgical intervention, a postoperative polysomnogram may be obtained at 3 to 6 mo to allow for resolution of pharyngeal edema and stabilization of the airway as lengthened suprahyoid and parapharyngeal muscles assume their new resting lengths after skeletal surgery.24
EDUCATIONAL OPPORTUNITIES IN AN ALT
Interprofessional education is an essential component of health professional education and has been endorsed by the Institute of Medicine as a means to improve quality of care.25 The ALT allows attending physicians from different specialties to learn from and work with each other, and also provides the same benefit to trainees at various points in their education. Students, residents, and fellows from multiple departments spend time in the ALT, where they have the opportunity for direct interaction with specialists outside of their own field. Learners are expected to present portions of the multidisciplinary conference to improve their medical knowledge and patient care capabilities, and to sharpen their peer-teaching skills.
Trainees in a sleep medicine fellowship program accredited by the Accreditation Council for Graduate Medical Education are required to have training in “practice management of sleep medicine.”26 Participation in the ALT provides learners with unique exposure and real-life examples of how clinical factors, patient preference, cost, and effective resource utilization are all important in formulation of each patient's treatment plan. Learners also gain understanding of logistical considerations (e.g. personnel, equipment, prior authorizations, and billing specifications) required to establish an ALT should they choose to do so later in their respective careers.
CONCLUSIONS
The ALT program described enables direct communication between medical, dental, and surgical specialists who treat CPAP-intolerant OSA patients and provides these patients with an organized, resourceful consideration of non-CPAP treatment modalities. ALT evaluation is but one component of longitudinal OSA management. Patients need continued follow-up if OSA persists after an ALT treatment.
Ongoing communication with third-party payers is needed to improve insurance coverage for non-CPAP treatment modalities; only then will patients be able to truly consider all medically reasonable treatments available to each individual.
The experience gained from an ALT can be applied to develop other multidisciplinary programs to enhance the care of patients with sleep disorders. Optimized process efficiency will help an ALT serve a greater number of patients. As more ALT are established across geographic regions, in private practice and academic settings, experiences can be shared to further expand the potential of these programs. Multidisciplinary collaboration within a program and across institutions will facilitate development of best practices, creation of appropriate quality measures and educational competencies, and tracking of patient outcomes.
DISCLOSURE STATEMENT
This was not an industry supported study. The authors have indicated no financial conflicts of interest.
REFERENCES
- 1.Bushby K, Finkel R, Birnkrant DJ, et al. Diagnosis and management of Duchenne muscular dystrophy, part 2: implementation of multidisciplinary care. Lancet Neurol. 2010;9(2):177–189. doi: 10.1016/S1474-4422(09)70272-8. [DOI] [PubMed] [Google Scholar]
- 2.Berger R, Moertl D, Peter S, et al. N-terminal pro-b-type natriuretic peptide-guided, intensive patient management in addition to multidisciplinary care in chronic heart failure a 3-arm, prospective, randomized pilot study. J Am Coll Cardiol. 2010;55(7):645–653. doi: 10.1016/j.jacc.2009.08.078. [DOI] [PubMed] [Google Scholar]
- 3.Grosse SD, Schechter MS, Kulkarni R, Lloyd-Puryear MA, Strickland B, Trevathan E. Models of comprehensive multidisciplinary care for individuals in the united states with genetic disorders. Pediatrics. 2009;123(1):407–412. doi: 10.1542/peds.2007-2875. [DOI] [PubMed] [Google Scholar]
- 4.Shelgikar AV, Durmer JS, Joynt KE, Olson EJ, Riney H, Valentine P. Multidisciplinary sleep centers: strategies to improve care of sleep disorders patients. J Clin Sleep Med. 2014;10(6):693–697. doi: 10.5664/jcsm.3808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Russell T. Enhancing adherence to positive airway pressure therapy for sleep disordered breathing. Semin Respir Crit Care Med. 2014;35(5):604–612. doi: 10.1055/s-0034-1390070. [DOI] [PubMed] [Google Scholar]
- 6.Sharma S, Essick G, Schwartz D, Aronsky AJ. Sleep medicine care under one roof: a proposed model for integrating dentistry and medicine. J Clin Sleep Med. 2013;9(8):827–833. doi: 10.5664/jcsm.2934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.L'Estrange PR, Battagel JM, Nolan PJ, Harkness B, Jorgensen GI. The importance of a multidisciplinary approach to the assessment of patients with obstructive sleep apnoea. J Oral Rehabil. 1996;23(1):72–77. doi: 10.1111/j.1365-2842.1996.tb00815.x. [DOI] [PubMed] [Google Scholar]
- 8.Ferguson KA, Cartwright R, Rogers R, Schmidt-Nowara W. Oral appliances for snoring and obstructive sleep apnea: a review. Sleep. 2006;29(2):244–262. doi: 10.1093/sleep/29.2.244. [DOI] [PubMed] [Google Scholar]
- 9.Doff MHJ, Veldhuis SKB, Hoekema A, et al. Long-term oral appliance therapy in obstructive sleep apnea syndrome: a controlled study on temporomandibular side effects. Clin Oral Invest. 2012;16(3):689–697. doi: 10.1007/s00784-011-0555-6. [DOI] [PubMed] [Google Scholar]
- 10.Balaji SM. Textbook of Oral and Maxillofacial Surgery. New Delhi, India: Elsevier; 2007. [Google Scholar]
- 11.Liu YH, Lowe AA, Fleetham JA, Park YC. Cephalometric and physiologic predictors of the efficacy of an adjustable oral appliance for treating obstructive sleep apnea. Am J Orthod Dentofacial Orthop. 2001;120(6):639–647. doi: 10.1067/mod.2001.118782. [DOI] [PubMed] [Google Scholar]
- 12.Caples SM, Rowley JA, Prinsell JR, et al. Surgical modifications of the upper airway for obstructive sleep apnea in adults: a systematic review and meta-analysis. Sleep. 2010;33(10):1396–1407. doi: 10.1093/sleep/33.10.1396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.El AS, El H, Palomo JM, Baur DA. A 3-dimensional airway analysis of an obstructive sleep apnea surgical correction with cone beam computed tomography. J Oral Maxillofac Surg. 2011;69(9):2424–2436. doi: 10.1016/j.joms.2010.11.046. [DOI] [PubMed] [Google Scholar]
- 14.Vela MF, Kramer JR, Richardson PA, Dodge R, El-Serag HB. Poor sleep quality and obstructive sleep apnea in patients with GERD and Barrett's esophagus. Neurogastroent Motil. 2014;26(3):346–352. doi: 10.1111/nmo.12265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Friedman M, Ibrahim H, Bass L. Clinical staging for sleep-disordered breathing. Otolaryngol Head Neck Surg. 2002;127(1):13–21. doi: 10.1067/mhn.2002.126477. [DOI] [PubMed] [Google Scholar]
- 16.Singhal V, Sharma M, Prabhakar H, Ali Z, Singh GP. Effect of posture on mouth opening and modified Mallampati classification for airway assessment. J Anesth. 2009;23(3):463–465. doi: 10.1007/s00540-009-0761-4. [DOI] [PubMed] [Google Scholar]
- 17.Strollo PJ, Jr., Soose RJ, Maurer JT, et al. Upper-airway stimulation for obstructive sleep apnea. N Engl J Med. 2014;370(2):139–149. doi: 10.1056/NEJMoa1308659. [DOI] [PubMed] [Google Scholar]
- 18.Poirier J, George C, Rotenberg B. The effect of nasal surgery on nasal continuous positive airway pressure compliance. Laryngoscope. 2014;124(1):317–319. doi: 10.1002/lary.24131. [DOI] [PubMed] [Google Scholar]
- 19.Lin HC, Friedman M, Chang HW, Gurpinar B. The efficacy of multilevel surgery of the upper airway in adults with obstructive sleep apnea/hypopnea syndrome. Laryngoscope. 2008;118(5):902–908. doi: 10.1097/MLG.0b013e31816422ea. [DOI] [PubMed] [Google Scholar]
- 20.Weaver EM, Woodson T, Yueh B, et al. Studying Life Effects & Effectiveness of Palatopharyngoplasty (SLEEP) study: subjective outcomes of isolated uvulopalatopharyngoplasty. Otolaryng Head Neck. 2011;144(4):623–631. doi: 10.1177/0194599810394982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Thatcher GW, Maisel RH. The long-term evaluation of tracheostomy in the management of severe obstructive sleep apnea. Laryngoscope. 2003;113(2):201–204. doi: 10.1097/00005537-200302000-00001. [DOI] [PubMed] [Google Scholar]
- 22.Woodson BT, Soose RJ, Gillespie MB, et al. Three-year outcomes of cranial nerve stimulation for obstructive sleep apnea: the STAR trial. Otolaryngol Head Neck Surg. 2016;154(1):181–188. doi: 10.1177/0194599815616618. [DOI] [PubMed] [Google Scholar]
- 23.Remmers J, Charkhandeh S, Grosse J, et al. Remotely controlled mandibular protrusion during sleep predicts therapeutic success with oral appliances in patients with obstructive sleep apnea. Sleep. 2013;36(10):1517–1525. doi: 10.5665/sleep.3048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Caples SM, Rowley JA, Prinsell JR, et al. Surgical modifications of the upper airway for obstructive sleep apnea in adults: a systematic review and meta-analysis. Sleep. 2010;33(10):1396–1407. doi: 10.1093/sleep/33.10.1396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Buring SM, Bhushan A, Broeseker A, et al. Interprofessional education: definitions, student competencies, and guidelines for implementation. Am J Pharm Educ. 2009;73(4):59. doi: 10.5688/aj730459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.ACGME Program Requirements for Graduate Medical Education in Sleep Medicine (Internal Medicine, Neurology, Pediatrics, or Psychiatry) Accreditation Council for Graduate Medical Education Web site. [Accessed December 8, 2016]. http://www.acgme.org/Specialties/Program-Requirements-and-FAQs-and-Applications/pfcatid/37/Neurology. Updated February 8, 2016.