Abstract
We present a case of recurrent upper gastrointestinal (GI) bleeding in a man aged 57 years with primary biliary cholangitis who was ultimately diagnosed with an isolated duodenal variceal bleed, which was successfully treated with histoacryl glue injection. Duodenal varices are an uncommon presentation of portal hypertension and can result in significant GI bleeding with a high mortality. Diagnosis can be difficult and therapeutic options limited. Endoscopic variceal sclerotherapy with histoacryl glue provides an effective treatment, though endoscopists need to remain aware of and vigilant for the serious complications of this treatment option.
Background
Portal hypertension is the progressive complication of liver cirrhosis, and gives rise to the development of portosystemic collaterals commonly at the oesophagogastric junction, the abdominal wall and the rectum. Ectopic varices are a term reserved for varices, which exist outside the oesophagogastric region.1 Although a rare cause of gastrointestinal (GI) bleeding, they are reported to have a high mortality, around 40%.1–7 Up to 17% of ectopic varices occur in the duodenum,3 4 but they are not a common cause of variceal bleeding.
Case presentation
A man aged 57 years presented with a 2-day history of melaena, right-sided chest pain, abdominal pain and shortness of breath. He had a background of antimitochondrial antibody-positive primary biliary cholangitis diagnosed 10 years previously. He reported an alcohol intake of 23 units (∼200 g) per week and was an ex-smoker. His only medication was urseodeoxycholic acid (15 mg/kg). He had previously declined a screening gastroscopy. Ultrasound scan 10 months prior to this admission showed a cirrhotic liver with hepatopetal flow of the portal vein.
At presentation, he was and remained cardiovascularly stable. Examination of his abdomen elicited mild tenderness in the epigastrium, with no evidence of guarding. Digital rectal examination confirmed the presence of melaena. Investigations were as follows: haemoglobin (Hb) 135 g/L (range 135–170 g/L), WCC 12×109/L, platelets 219×109/L, MCV 91 fL, clotting, U&Es and LFTs normal. His vital signs on admission were: blood pressure 153/104 mm Hg, heart rate 140 bpm, temperature 36.5°C and saturations >96%. He underwent an oesophagogastroduodenoscopy (OGD) 21 hours after admission, which confirmed the presence of a small amount of altered blood in the stomach and 4 grade 2 oesophageal varices without any stigmata of recent bleeding (fibrin plugs) but with red spots (figure 1A).
Figure 1.
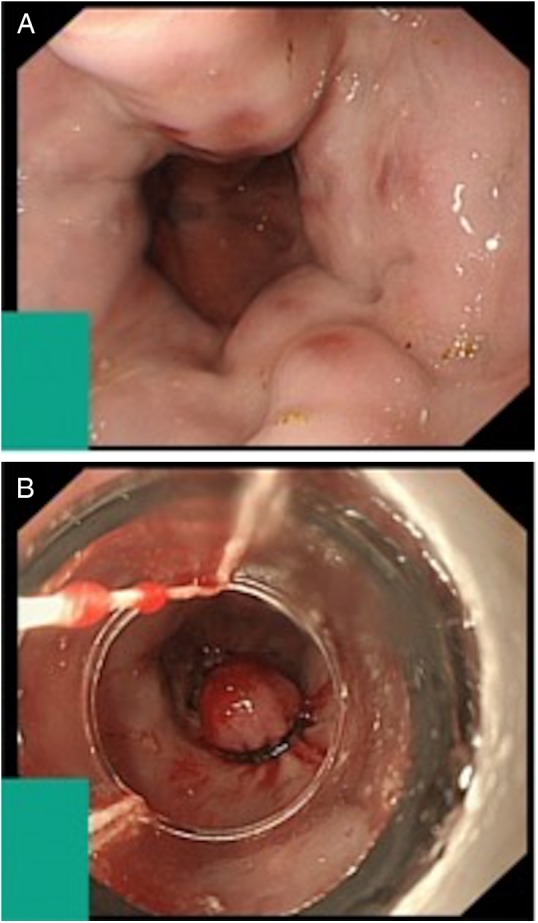
(A) Grade 2 oesophageal varices. (B) Banding of oesophageal varices.
The duodenum was reported to be normal. Ligation bands were applied to the oesophageal varices (figure 1B). Treatment was started with terlipressin and broad-spectrum antibiotics. Although his haemoglobin began to slowly drop, he remained stable until 3 days after the first gastroscopy, when he experienced further melaena and a number of presyncopal episodes. His Hb dropped to 77 g/L, urea 8.6 mmol/L and all other blood results were normal. The Blatchford score8 was 17. Once stable, he underwent a second OGD under general anaesthesia (4 hours after the episode of melaena). There was no visible blood in the upper GI tract. Banding-induced ulceration was present in the oesophagus and the brisk self-limiting bleeding was presumed to be due to oesophageal ulceration. The endoscopist reported a possible 2 cm polyp/lipoma in the second part of the duodenum. Again, the melaena settled and he remained stable postendoscopy (Hb 70 g/L). Two days later, he had two further episodes of melaena and failed to augment his Hb, despite 2 units of blood. A third OGD was carried out under conscious sedation on day 7 of his admission. Again, the upper GI tract was blood-free and the findings were similar to the second OGD (figure 2A). The endoscopist thought the previously described duodenal polyp could be a prominent ampulla, which prompted the request for an abdominal CT scan (figure 2B) to exclude a potential cause for haemobilia.
Figure 2.
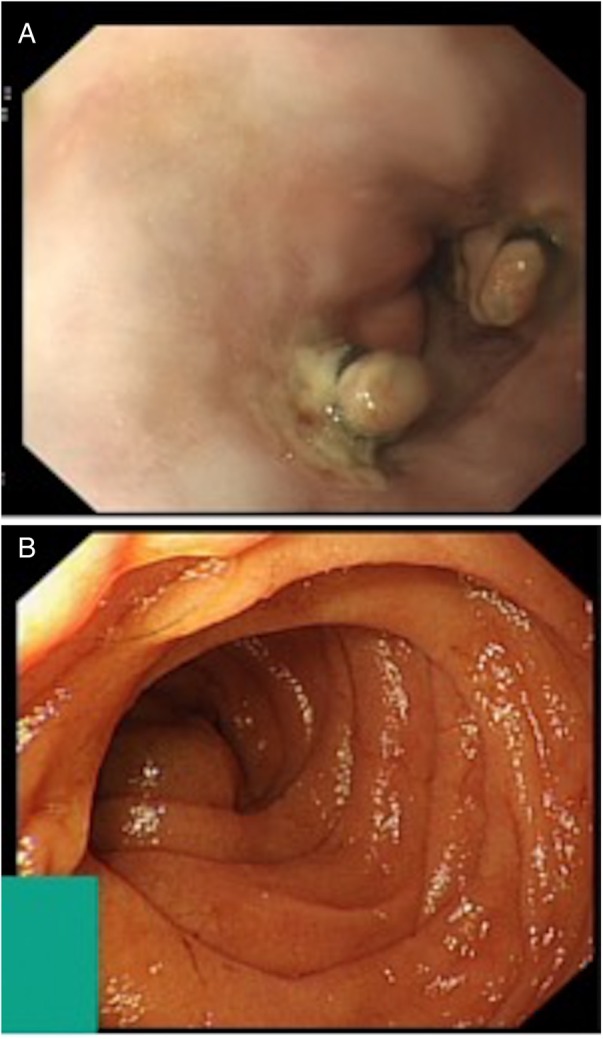
(A) Postbanding ulceration of oesophageal varices. (B) Duodenal polyp—suspected prominent ampulla.
The next day, his Hb continued to drop to 55g/L, and he reported ongoing melaena. His vital signs at this point were: blood pressure 125/66 mm Hg, heart rate 125 bpm, temperature 38.9°C and saturations >96%. The decision was made to resuscitate with blood and proceed to an urgent fourth OGD. On this examination, there was altered blood in the stomach but again no obvious actively bleeding point. It was noted that the tip of the duodenal lesion was red (figure 3). The endoscopist was pondering over this finding when the lesion briefly spurted blood (figure 4).
Figure 3.

Duodenal lesion tip.
Figure 4.

Duodenal lesion actively spurting blood.
The possible diagnosis of haemobilia crossed the endoscopist's mind and a side viewing scope (duodenoscope) was used to attempt further therapy. The duodenal lesion was felt to be in the third part of the duodenum and indeed, on closer inspection, the ampulla was located in the second part of the duodenum and found to be normal (figure 5).
Figure 5.
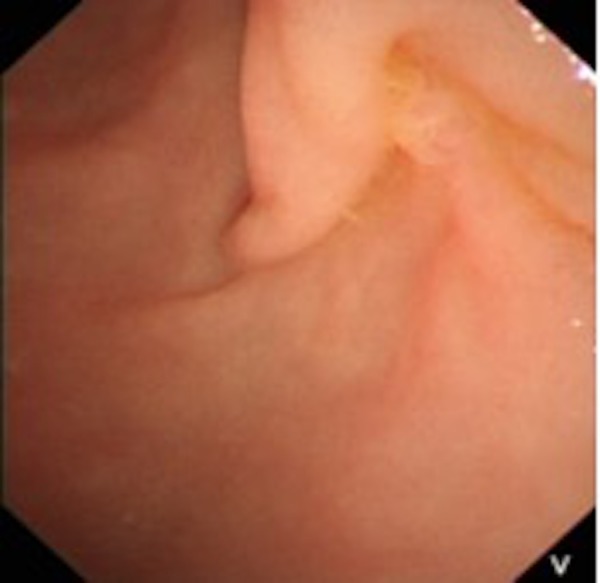
Ampulla.
It is at this point that the diagnosis of duodenal variceal bleed was made. The varix was treated successfully with 2.4 mL histoacryl glue using a normal gastroscope. The patient subsequently remained stable and free of any further GI bleeding. He was discharged 48 hours later. His Hb remained stable at 92 g/L.
Outcome and follow-up
A repeat OGD was planned for 2 weeks postdischarge, but the patient declined this. He did proceed to an OGD 4 months after discharge and the duodenal varix had completely resolved (figure 6A, B). The patient remained well and asymptomatic of any GI bleed. A CT scan post-treatment confirmed the presence of retroperitoneal glue around the third part of the duodenum, the retroperitoneal veins and aorto-caval space (figure 7). Of note, there was translocation of glue to the pelvis, but the patient was asymptomatic.
Figure 6.
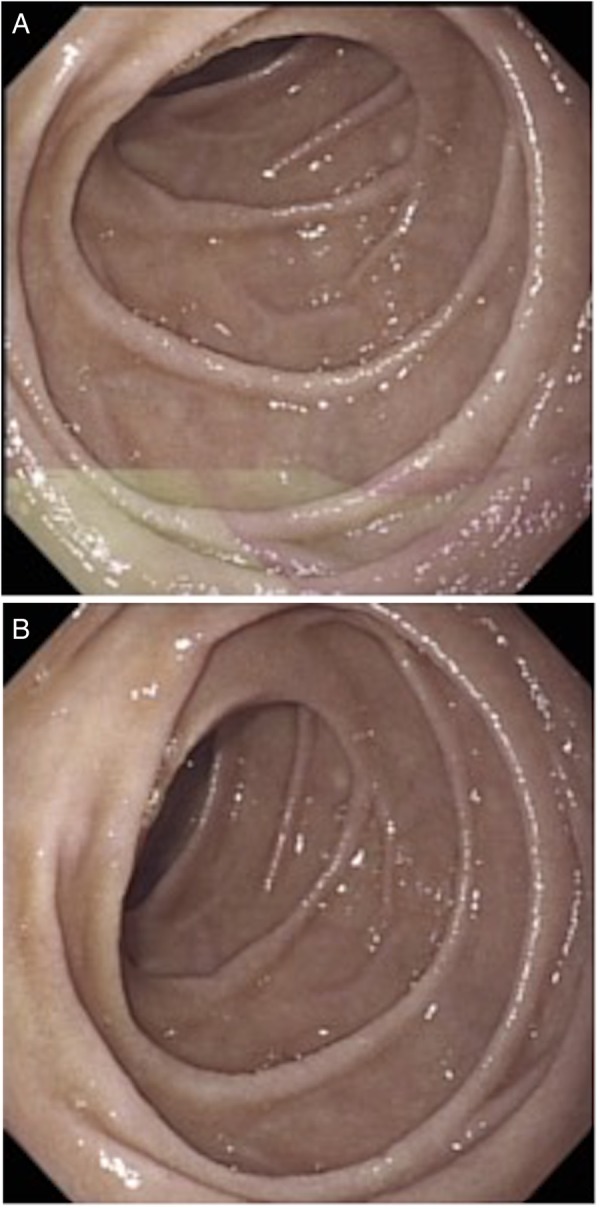
(A) Follow-up endoscopy, view from D2. (B) Follow-up endoscopy, view from D3.
Figure 7.
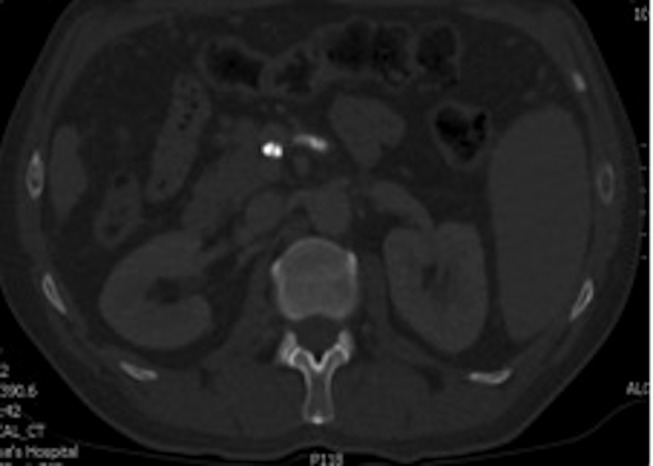
Abdominal CT showing retroperitoneal glue.
Discussion
Liver disease in the UK is an exception to the vast improvements made in health and life expectancy over the past 30 years, with mortality increasing by 400% since 1970, and a fivefold increase in those under 65.9 The prevalence of cirrhosis is estimated to be around 100 cases per 100 000 people, with equal incidence in men and women. The UK saw a steep rise in the rate of cirrhosis in the 1990s due to the surge in alcohol consumption.10 Variceal bleeding is a life-threatening presentation of portal hypertension, a progressive complication of liver cirrhosis,7 with inhospital mortality estimated at 15%.11
Portal hypertension is a result of increased resistance to portal flow, commonly due to distortion in liver architecture. Portosystemic collaterals form due to splanchnic hypertension, commonly in the oesophagus, rectum and umbilical regions. Additionally, portosystemic communications can occur between the pancreaticoduodenal veins and systemic veins via the veins of Retizus, bringing rise to venous dilation at the duodenum, resulting in duodenal varices.3 4 12–14
Duodenal varices were first described by Alberti,15 and visualised endoscopically in 1973 by Kunisaki et al.16 Duodenal varices can result in massive GI bleeding, reported at around 40% mortality; diagnosis and treatment is often difficult and controversial as experience is limited.17 They most commonly arise at the duodenal bulb, and less frequently more distally.6 18 19 Two-thirds of duodenal varices are a result of portal vein hypertension due to hepatic cirrhosis, and the remaining third are due to extrahepatic portal hypertension, for example, portal vein thrombosis.
Pharmacological therapy is recommended and can be initiated as soon as variceal bleeding is suspected. Vasopressin analogues, such as terlipressin, are potent splanchnic vasoconstrictors reducing blood flow to all splanchnic organs, thereby decreasing portal pressure. In addition, the use of short-term prophylactic antibiotics has been shown to decrease the rate of bacterial infections and the rate of mortality. The British Society of Gastroenterology guidelines recommends initiation of vasoconstrictors such as terlipressin as soon as variceal bleeding is suspected, and antibiotics within 1 day.11
OGD can be limited as the scope is unable to stretch to the distal end of the duodenum and often the varix is buried in the submucosal or serosal layer making visualisation difficult.3 4 6 The thin nature of the duodenal wall compared with the rest of the GI tract increases the risk of perforation with any intervention.6 12 13 There are no currently randomised controlled trials related to the management of this relatively uncommon presentation and the evidence available is based on small studies and case reports. Table 1 summarises the benefits and risks of the therapeutic interventions used in the treatment of duodenal varices.20–25
Table 1.
Summary of risks and benefits of the current therapeutic options in management of duodenal varices
| Therapeutic options |
Benefits | Risks | |
|---|---|---|---|
| Endoscopic | Variceal banding | ||
| Variceal sclerotherapy | |||
| Interventional radiology | Transjugular intrahepatic portosystemic shunt (TIPSS) | ||
| Balloon occluded retrograde transvenous obliteration (BRTO) | |||
| Surgical | Variceal ligation | ||
| Duodenectomy | |||
| Shunt surgery | |||
Our case exemplifies the difficulties of identifying the source of duodenal variceal bleeding. It took four OGDs to locate the source of bleeding and this was possible because of active bleeding at the time of the fourth OGD. Had this not been the case, the next option would have been a CT angiogram or red cell scan at the time of bleeding.
Injection of histoacryl glue is not without risk. In our case, glue migrated to the pelvis with no consequence to the patient. There are well-documented cases of glue causing pulmonary embolism.26 27 We therefore urge caution with the use of histoacryl glue. This should ideally be performed by an experienced endoscopist.
Learning points.
Duodenal varices are a rare manifestation of portal hypertension in patients with cirrhosis and can lead to life-threatening haemorrhage.
Duodenal varices should be considered in patients presenting with melaena with no identifiable cause of bleeding on visualisation of the oesophagus and presence of hepatofugal flow on ultrasound.
Although treatment of duodenal varices is not well researched, endoscopic variceal sclerotherapy with histoacryl glue is effective in the management of this life-threatening presentation.
Injection of histoacryl glue can lead to complications such as migration to the lungs, abdomen and pelvis.
Footnotes
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Norton ID, Andrews JC, Kamath PS. Management of ectopic varices. Hepatology 1998;28:1154–8. 10.1002/hep.510280434 [DOI] [PubMed] [Google Scholar]
- 2.Sistla SC, Karthikeyan VS, Ram D et al. Endoscopic variceal ligation as a safe and effective alternative to endoscopic sclerotherapy in bleeding ectopic duodenal varix—report of a rare case. Indian J Gastroenterol 2013;32:419–20. 10.1007/s12664-012-0289-7 [DOI] [PubMed] [Google Scholar]
- 3.Malik A, Junglee N, Khan A et al. Duodenal varices successfully treated with cyanoacrylate injection therapy. BMJ Case Rep 2011: doi:10.1136/bcr.02.2011.3913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Larson JV, Steensma EA, Burke LH et al. A case report of fatal upper gastrointestinal bleed arising from duodenal varices secondary to undiagnosed portal hypertension. J Surg Radiol 2012;3:230–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Moitinho E, Escorsell A, Bandi JC et al. Prognostic value of early measurements of portal pressure in acute variceal bleeding. Gastroenterology 1999;117:626–31. 10.1016/S0016-5085(99)70455-5 [DOI] [PubMed] [Google Scholar]
- 6.Park SB, Lee SH, Kim JH et al. Successful treatment of duodenal variceal bleeding by endoscopic clipping. Clin Endosc 2013;46:403–6. 10.5946/ce.2013.46.4.403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Garcia-Tsao G, Sanyal AJ, Grace ND et al. Prevention and management of gastroesophageal varices and variceal hemorrhage in cirrhosis. Hepatology 2007;46:922–38. 10.1002/hep.21907 [DOI] [PubMed] [Google Scholar]
- 8.Stanley AJ, Ashley D, Dalton HR et al. Outpatient management of patients with low-risk upper-gastrointestinal haemorrhage: multicentre validation and prospective evaluation. Lancet 2009;373:42–7. 10.1016/S0140-6736(08)61769-9 [DOI] [PubMed] [Google Scholar]
- 9.Moriarty KJ, Cassidy P, Dalton D, et al Alcohol related disease. Meeting the challenge of improved quality of care and better use of resources. A joint position paper on behalf of the British Society of Gastroenterology, Alcohol Health Alliance UK & British Association for Study of the Liver 2010. [Google Scholar]
- 10.Georgalas C, Eleftherios M. Cirrhosis. The right clinical information, right where it's needed. BMJ Best Pract 2015. http://bestpractice.bmj.com/best-practice/monograph-pdf/278.pdf.
- 11.Jalan R, Hayes PC et al. UK guidelines on the management of variceal haemorrhage in cirrhotic patients. Gut 2015;46(Suppl 3):1–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McChesney L, Jensen D, Matalon T et al. Duodenal varices: a case report and review of the literature. HPB Surg 1995;9:31–5. 10.1155/1995/97496 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kang HY, Lee WK, Kim YH et al. Ruptured duodenal varices arising from the main portal vein successfully treated with endoscopic injection sclerotherapy: a case report. Korean J Hepatol 2011;17:152–6. 10.3350/kjhep.2011.17.2.152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bosch A, Marsano L, Varilek GW. Successful obliteration of duodenal varices after endoscopic ligation. Dig Dis Sci 2003;48:1809–12. 10.1023/A:1025402411557 [DOI] [PubMed] [Google Scholar]
- 15.Alberti W. Uberden roentgenologischen nachweis von varizen in buolbus duodeni. Fortschro Geb Koentgenstr 1931;43:60–5. [Google Scholar]
- 16.Kunisaki T, Someya N, Shimokava Y. Varices in the distal duodenum seen with a fiberduodenoscope. Endoscopy 1973;5:101–4. 10.1055/s-0028-1098222 [DOI] [Google Scholar]
- 17.Ibrahim S, Tay KH, Tan NC. Successful management of a bleeding duodenal varix by endoscopic banding. Singapore Med J 2005;46:723–5. [PubMed] [Google Scholar]
- 18.Gurung A, Jaffe PE, Zhang X. Duodenal polyposis secondary to portal hypertensive duodenopathy. World J Gastrointest Endosc 2015;7:1257 10.4253/wjge.v7.i17.1257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hwang S, Sohn JH, Kim TY et al. Long-term successful treatment of massive distal duodenal variceal bleeding with. Korean J Gastroenterol 2014;63:248–52. 10.4166/kjg.2014.63.4.248 [DOI] [PubMed] [Google Scholar]
- 20.Costa M, Ramos G. Duodenal variceal bleeding successfully treated by endoscopic N-butyl-2-cyanoacrylate Injection. GE Port J Gastroenterol 2015;22:180–1. 10.1016/j.jpge.2015.03.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.D'Amico G, Pietrosi G, Tarantino I et al. Emergency sclerotherapy versus vasoactive drugs for variceal bleeding in cirrhosis: a Cochrane meta-analysis. Gastroenterology 2003;124:1277–91. 10.1016/S0016-5085(03)00269-5 [DOI] [PubMed] [Google Scholar]
- 22.Dai C, Liu WX, Jiang M et al. Endoscopic variceal ligation compared with endoscopic injection sclerotherapy for treatment of esophageal variceal hemorrhage: a meta-analysis. World J Gastroenterol 2015;21:2534–41. 10.3748/wjg.v21.i8.2534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dulic M, Dulic-Lakovic E, Hellmich B et al. Successful treatment of a bleeding duodenal varix by endoscopic band ligation. J Gastrointest Liver Dis 2011;20:234. [PubMed] [Google Scholar]
- 24.Hashimoto R, Sofue K, Takeuchi Y et al. Successful balloon-occluded retrograde transvenous obliteration for bleeding duodenal varices using cyanoacrylate. World J Gastroenterol 2013;19:951–4. 10.3748/wjg.v19.i6.951 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Merli M, Salerno F, Riggio O et al. Transjugular intrahepatic portosystemic shunt versus endoscopic sclerotherapy for the prevention of variceal bleeding in cirrhosis: a randomized multicenter trial. Gruppo Italiano Studio TIPS (G.I.S.T.) . Hepatology 1998;27:48–53. 10.1002/hep.510270109 [DOI] [PubMed] [Google Scholar]
- 26.Singer AD, Fananapazir G, Maufa F et al. Pulmonary embolism following 2-octyl-cyanoacrylate/lipiodol injection for obliteration of gastric varices: an imaging perspective. J Radiol Case Rep 2012;6:17–22. 10.3941/jrcr.v6i2.845 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chew JR, Balan A, Griffiths W et al. Delayed onset pulmonary glue emboli in a ventilated patient: a rare complication following endoscopic cyanoacrylate injection for gastric variceal haemorrhage. BMJ Case Rep 2014;2014:bcr2014206461 10.1136/bcr-2014-206461 [DOI] [PMC free article] [PubMed] [Google Scholar]


