Abstract
Objectives
We compared the effectiveness of the Gold Standard Programme (a comprehensive smoking cessation intervention commonly used in Denmark) with other face-to-face smoking cessation programmes in Denmark after implementation in real life, and we identified factors associated with successful quitting.
Design
Prospective cohort study.
Setting
A total of 423 smoking cessation clinics from different settings reported data from 2001 to 2013.
Participants
In total, 82 515 patients were registered. Smokers ≥15 years old and attending a programme with planned follow-up were included. Smokers who did not want further contact, who intentionally were not followed up or who lacked information about the intervention they received were excluded. A total of 46 287 smokers were included.
Interventions
Various real-life smoking cessation interventions were identified and compared: The Gold Standard Programme, Come & Quit, crash courses, health promotion counselling (brief intervention) and other interventions.
Main outcome
Self-reported continuous abstinence for 6 months.
Results
Overall, 33% (11 184) were continuously abstinent after 6 months; this value was 24% when non-respondents were considered smokers. The follow-up rate was 74%. Women were less likely to remain abstinent, OR 0.83 (CI 0.79 to 0.87). Short interventions were more effective among men. After adjusting for confounders, the Gold Standard Programme was the only intervention with significant results across sex, increasing the odds of abstinence by 69% for men and 31% for women. In particular, compliance, and to a lesser degree, mild smoking, older age and not being disadvantaged were associated with positive outcomes for both sexes. Compliance increased the odds of abstinence more than 3.5-fold.
Conclusions
Over time, Danish smoking cessation interventions have been effective in real life. Compliance is the main predictor of successful quitting. Interestingly, short programmes seem to have relatively strong effects among men, but the absolute numbers are very small. Only the comprehensive Gold Standard Programme works across sexes.
Keywords: smoking cessation, national database, effectiveness, smoking cessation interventions, Denmark
Strengths and limitations of this study.
This study was based on a large cohort of smokers from all regions and settings in Denmark; 46 287 smokers were included in the study, and the follow-up rate was high (74%).
The study was based on routinely collected health data with high completeness and precision, and the implications were considered minimal, as the research question was in line with the purposes of the database.
Confounding effects were carefully considered and adjusted for, but we cannot exclude the possibility of residual confounding from other potential confounders, such as genetic predispositions, comorbidities, competing addictions and lifestyle factors not considered due to a lack of information.
A limitation is that the results were based on self-reporting since patients are likely to overestimate their success; we assumed that overestimations were evenly distributed and that the groups were thus comparable in spite of potentially slightly overestimated quit rates.
Owing to varying cultural traditions, smoking habits and socioeconomic conditions, generalisations should be considered carefully.
Introduction
Tobacco is the most damaging and preventable lifestyle factor affecting public health globally and nationally.1 2 Its harmful effects are well documented.3 Globally, the WHO estimates that ∼6 million people die from smoking-related diseases yearly.1 Many countries, including Denmark, have introduced restrictive laws and strategies to reduce smoking.4 More than 12 800 people in Denmark die as a consequence of smoking annually, corresponding to 1 in 4 deaths.4
Over the past 15–20 years, many initiatives have been launched to help smokers quit. Smoking cessation programmes are one of many initiatives. Additionally, tobacco control and policy measures have been implemented, including smoking bans, higher tobacco taxes, and restrictions on tobacco sales and advertising. Recently, Denmark signed on to the WHO's goal to reduce smoking by 30% by 2025,5 and specific regions are working towards implementing a tobacco endgame.6 Furthermore, there are many other resources to help smokers quit, such as a quit line, national campaigns, training materials and recently, aid based on information technology tools. These efforts have contributed to an overall change in smoking climates and attitudes. In Denmark, smoking prevalence has declined by 0.5–1 percentage point per annum during the past decade. In 2013, 17% of the Danish population over 15 years of age smoked daily, and an additional 6% smoked occasionally.7
Since 1995, the Gold Standard Programme (GSP) has become routine in Denmark, and the vast majority of smoking cessation interventions offered are the GSP.8 It is a comprehensive intervention comprising five meetings over 6 weeks and fulfilling intensive clinical intervention requirements.9 Programme counsellors are specially trained to provide this manual-based patient education programme. Smokers are either referred to the intervention by health practitioners, or they can contact programme providers themselves. The GSP has proven to be highly effective and cost-effective, even across subgroups,10–15 but its effectiveness has not yet been compared with that of other programmes. In addition to the GSP, other face-to-face methods (eg, crash courses, health promotion counselling, alternative treatments and Come & Quit programmes) have been used and evaluated through the national Danish Smoking Cessation Database (SCDB). The aim of this study was to compare the effectiveness of the GSP with the effectiveness of other face-to-face smoking cessation programmes used in Denmark. The main hypothesis was that the GSP would be the most effective intervention after 6 months. We also aimed to identify factors associated with successful smoking cessation.
Methods
Study design
This prospective cohort study on the SCDB included patients treated from 2001 to 2013 with follow-up until 2014. The SCDB lists ∼80–90% of all clinics performing face-to-face interventions used in Denmark,16 and we thus consider this a representative sample.
Setting
During the study, 423 smoking cessation clinics reported data from municipal clinics, pharmacies, hospitals, midwives, primary care facilities and other private providers. Smokers could attend smoking cessation interventions free of charge with or without referrals. Approximately 10% attended an intervention at a private provider with payment. From 2001 to 2005, this proportion was 19%, and from 2006 to 2012, it was 4%, likely due to structural changes made in the Danish healthcare system.16
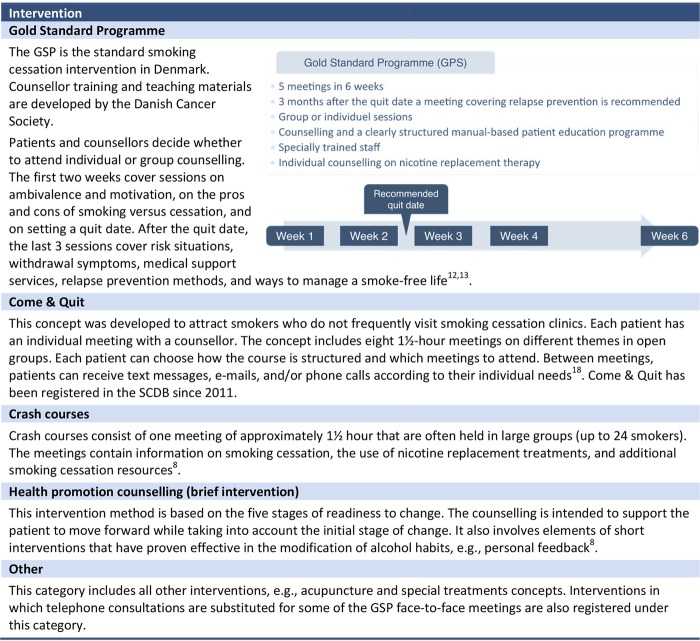
Intervention
Different real-life smoking cessation interventions were identified and compared with the data registered in the SCDB (figure 1).
Figure 1.
Descriptions of smoking cessation interventions examined in this study. GSP, Gold Standard Programme; SCDB, Smoking Cessation Database.
In accordance with the guidelines, patients who attended at least 75% of the scheduled meetings were considered compliant.17 For Come & Quit18 (figure 1), four meetings corresponded to 75% of the GSP.8
Participants
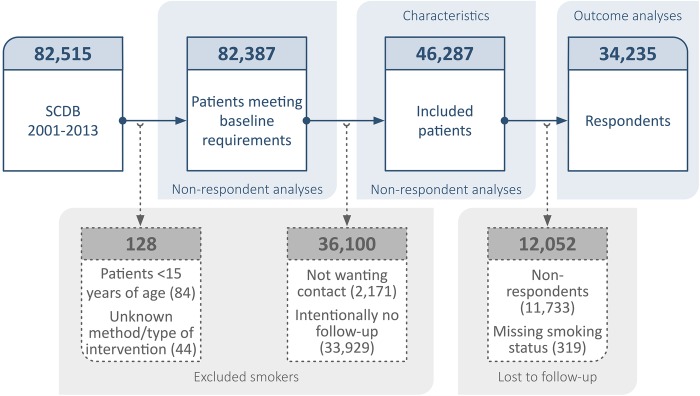
In 2001–2013, 82 515 smokers were registered in the SCDB after providing informed consent (see figure 2).
Figure 2.
Flow chart. In total, 82 515 smokers were registered in the SCDB and 36 228 were excluded, leaving 46 287 smokers in the study population. Of them, 26% of the study population were lost to follow-up, leaving 34 235 smokers included in the outcome analyses. SCDB, Smoking Cessation Database.
Inclusion criteria: Patients ≥15 years old at the beginning of the programme who attended a smoking cessation programme with planned follow-up.
Exclusion criteria: Patients <15 years; patients not wanting to be contacted after 6 months; patients who were intentionally not followed up because the smoking cessation clinic decided beforehand not to; and patients without information on which intervention they received.
In total, 46 287 smokers who were followed up for 6 months were included (figure 2). Of them, 26% were lost to follow-up because they did not respond or because their smoking status was missing. The remaining 34 235 patients were included in the outcome analyses. Overall, 82 387 patients were included in the non-respondent analyses.
Data
We used data from the SCDB.8 The database was established in 2000 as a research database. The SCDB is available to all providers of smoking cessation intervention, and it is free of charge. Data are reported to the SCDB using standardised questionnaires on smoking histories, sociodemographic characteristics, treatments and follow-up.
Beginning in 2006, minor adjustments were made to the questionnaires and follow-up procedures. No validation of self-reported smoking status was required.8 Follow-up was 6 months after the scheduled quit date or, secondarily, the date of course completion. From 2001 to 2005, the information was collected by mail or telephone, and at least one reminder was required. For 2006 and later, the data were collected by telephone exclusively. After four attempts to reach the patient, of which at least one was made in the evening, the patient was reported as a non-respondent.
Outcomes
Primary outcome
Continuous abstinence for 6 months, defined as not smoking from the intended quit date (or previous treatment date) to the 6-month follow-up ±1 month.
Other variables
Factors associated with a positive outcome were studied after controlling for interventions, the time of collection, age, disadvantaged patients, heavy smoking, compliance, living with a smoker, setting, geographic region, programme format and medication offered for free.
Most variables were collected in categories. Age, daily tobacco consumption data (grams/day) and Fagerström scores on nicotine dependency (from 0 to 10 points)19 were collected as continuous data. The data were categorised as shown in table 1.
Table 1.
Characteristics of the 46 287 included smokers by intervention type
| GSP | Health promotion counselling | Crash courses | Come & Quit | Other | |
|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | n (%) | n (%) | |
| Total* | 40 651 (100) | 140 (100) | 183 (100) | 1592 (100) | 3721 (100) |
| Time for data collection | |||||
| 2001 | 1341 (3.3) | − | 37 (20.2) | − | 172 (4.6) |
| 2002–2003 | 6221 (15.3) | − | 109 (59.6) | − | 814 (21.9) |
| 2004–2005 | 7933 (19.5) | − | 37 (20.2) | − | 529 (14.2) |
| 2006–2007 | 7747 (19.1) | 1 (0.7) | − | − | 415 (11.2) |
| 2008–2009 | 8062 (19.8) | 42 (30.0) | − | − | 618 (16.6) |
| 2010–2011 | 5772 (14.2) | 46 (32.9) | − | 211 (13.3) | 550 (14.8) |
| 2012–2013 | 3575 (8.8) | 51 (36.4) | − | 1381 (86.8) | 623 (16.7) |
| Participants | |||||
| Sex | |||||
| Men | 15 655 (38.5) | 71 (50.7) | 75 (41.0) | 638 (40.1) | 1532 (41.2) |
| Women | 24 992 (61.5) | 69 (49.3) | 108 (59.0) | 954 (59.9) | 2186 (58.8) |
| Age (years) | |||||
| 15–24 years | 1892 (4.7) | 7 (5.0) | 6 (3.3) | 118 (7.4) | 335 (9.0) |
| 25–34 years | 5173 (12.7) | 25 (17.9) | 24 (13.1) | 140 (8.8) | 523 (14.1) |
| 35–44 years | 8471 (20.8) | 28 (20.0) | 34 (18.6) | 225 (14.1) | 772 (20.8) |
| 45–54 years | 10 985 (27.0) | 19 (13.6) | 51 (27.9) | 395 (24.8) | 860 (23.1) |
| 55+ years | 14 031 (34.5) | 61 (43.6) | 68 (37.2) | 714 (44.9) | 1213 (32.6) |
| Education | |||||
| Low level | 20 764 (51.1) | 40 (28.6) | 168 (91.8) | 521 (32.7) | 2084 (56.0) |
| High level | 18 425 (45.3) | 96 (68.6) | 12 (6.6) | 1024 (64.3) | 1429 (38.4) |
| Employment | |||||
| Unemployed | 6885 (16.9) | 32 (22.9) | 31 (16.9) | 522 (32.8) | 830 (22.3) |
| Not unemployed | 32 750 (80.6) | 106 (75.7) | 146 (79.8) | 1035 (65.0) | 2779 (74.7) |
| Disadvantaged smokers (by work situation and education) | |||||
| Yes | 23 654 (58.2) | 55 (39.3) | 172 (94.0) | 825 (51.8) | 2417 (65.0) |
| No | 15 526 (38.2) | 82 (58.6) | 9 (4.9) | 729 (45.8) | 1113 (29.9) |
| Smoking | |||||
| <20 pack-years | 13 615 (33.5) | 48 (34.3) | 56 (30.6) | 507 (31.9) | 1391 (37.4) |
| ≥20 pack-years | 26 368 (64.9) | 91 (65.0) | 119 (65.0) | 1063 (66.8) | 2274 (61.1) |
| Fagerström 1–6 points | 29 264 (72.0) | 102 (72.9) | 124 (67.8) | 1139 (71.6) | 2600 (69.9) |
| Fagerström 7–10 points | 11 142 (27.4) | 38 (27.1) | 56 (30.6) | 445 (28.0) | 1093 (29.4) |
| <20 cigarettes per day | 17 230 (42.4) | 53 (37.9) | 82 (44.8) | 725 (45.5) | 1528 (41.1) |
| ≥20 cigarettes per day | 22 950 (56.5) | 87 (62.1) | 96 (52.5) | 867 (54.5) | 2155 (57.9) |
| Heavy smokers (based on pack-years, Fagerström scores and daily consumption levels) | |||||
| No | 9845 (24.2) | 30 (21.4) | 46 (25.1) | 356 (22.4) | 988 (26.6) |
| Yes | 30 591 (75.3) | 109 (77.9) | 135 (73.8) | 1213 (76.2) | 2711 (72.9) |
| Compliance with programme (based on attendance) | |||||
| Not compliant | 14 479 (35.6) | 44 (31.4) | 1 (0.6) | 691 (43.4) | 1064 (28.6) |
| Compliant | 25 731 (63.3) | 89 (63.6) | 182 (99.4) | 825 (51.8) | 2470 (66.4) |
| Living with a smoker | |||||
| No | 25 802 (63.5) | 101 (72.1) | 120 (65.6) | 1117 (70.2) | 2316 (62.2) |
| Yes | 14 410 (35.5) | 38 (27.1) | 61 (33.3) | 451 (28.3) | 1358 (36.5) |
| Living with others† | |||||
| Living alone | 8754 (21.5) | 52 (37.1) | − | 656 (41.2) | 744 (20.0) |
| Living with children (±adults) | 7717 (19.0) | 38 (27.1) | − | 365 (22.9) | 744 (20.0) |
| Living with adults (no children) | 8436 (20.8) | 49 (35.0) | − | 543 (34.1) | 692 (18.6) |
| Housing situation† | |||||
| Residential property | 11 811 (29.1) | 63 (45.0) | − | 556 (34.9) | 844 (22.7) |
| Cooperative dwelling | 2172 (5.3) | 6 (4.3) | − | 139 (8.7) | 184 (4.9) |
| Rented accommodation | 10 464 (25.7) | 64 (45.7) | − | 828 (52.0) | 1070 (28.8) |
| Other housing | 248 (0.6) | 4 (2.9) | − | 34 (2.1) | 62 (1.7) |
| Referral | |||||
| No | 16 509 (40.6) | 35 (25.0) | 82 (44.8) | 459 (28.8) | 1544 (41.5) |
| Yes, from healthcare personal | 18 927 (46.6) | 100 (71.4) | 53 (29.0) | 1069 (67.2) | 1770 (47.6) |
| Yes, from others | 4047 (10.0) | − | 48 (26.2) | − | 305 (8.2) |
| Attempts to quit | |||||
| No previous attempts | 12 258 (30.2) | 55 (39.3) | 38 (20.8) | 565 (35.5) | 1121 (30.1) |
| 1–3 previous attempts | 20 605 (50.7) | 74 (52.9) | 85 (46.5) | 813 (51.1) | 1835 (49.3) |
| >3 previous attempts | 5526 (13.6) | 11 (7.9) | 38 (20.8) | 178 (11.2) | 543 (14.6) |
| Yes unknown number of attempts | 1397 (3.4) | − | 20 (10.9) | − | 137 (3.7) |
| Smoking cessation clinic | |||||
| Setting | |||||
| Publicly oriented‡ | 31 008 (76.3) | 91 (65.0) | 97 (53.0) | 1592 (100) | 1780 (47.8) |
| Hospital (including midwives) | 8198 (20.2) | 17 (12.1) | 82 (44.8) | 0 | 1415 (38.0) |
| Other | 1445 (3.6) | 32 (22.9) | 4 (2.2) | 0 | 526 (14.1) |
| Geographic area | |||||
| Capital Region of Denmark | 13 353 (32.9) | 23 (16.4) | 69 (37.7) | 368 (23.1) | 1845 (49.6) |
| Region Zealand | 5856 (14.4) | 4 (2.9) | 78 (42.6) | 131 (8.2) | 248 (6.7) |
| Region of Southern Denmark | 10 378 (25.5) | 27 (19.3) | 17 (9.3) | 318 (20.0) | 601 (16.2) |
| Central Denmark Region | 9237 (22.7) | 80 (57.1) | 16 (8.7) | 569 (35.7) | 868 (23.3) |
| North Denmark Region | 1827 (4.5) | 6 (4.3) | 3 (1.6) | 206 (12.9) | 159 (4.3) |
| Smoking cessation intervention | |||||
| Programme format | |||||
| Individual | 5878 (14.5) | 127 (90.7) | 28 (15.3) | 166 (10.4) | 1707 (45.9) |
| Group | 34 773 (85.5) | 13 (9.3) | 155 (84.7) | 1426 (89.6) | 2014 (54.1) |
| Target audience | |||||
| Patients and relations | 3647 (9.0) | 31 (22.1) | 20 (10.9) | 44 (2.8) | 978 (26.3) |
| Employees (workplace course) | 10 060 (24.8) | 4 (2.9) | 44 (24.0) | 76 (4.8) | 649 (17.4) |
| Ordinary citizens | 22 132 (54.4) | 71 (50.7) | 107 (58.5) | 1259 (79.1) | 1386 (37.3) |
| Mixed | 2516 (6.2) | 1 (0.7) | 6 (3.3) | 76 (4.8) | 84 (2.3) |
| Pregnant women (and partners) | 1156 (2.8) | 2 (1.4) | 4 (2.2) | 4 (0.3) | 80 (2.2) |
| Other | 1125 (2.8) | 31 (22.1) | 2 (1.1) | 133 (8.4) | 543 (14.6) |
| Medication offered for free | |||||
| No free medication | 15 324 (37.7) | 120 (85.7) | 60 (32.8) | 1342 (84.3) | 1641 (44.1) |
| Free for days (<1 week) | 17 367 (42.7) | 8 (5.7) | 97 (53.0) | 39 (2.5) | 880 (23.7) |
| Free for ≥1 week | 4843 (11.9) | 12 (8.6) | 26 (14.2) | 205 (12.9) | 976 (26.2) |
| Counselling free of charge | |||||
| Yes | 36 544 (89.9) | 137 (97.9) | 183 (100) | 1589 (99.8) | 3318 (89.2) |
| No | 4066 (10.0) | 3 (2.1) | 0 | 0 | 400 (10.8) |
| Planned relapse prevention† | |||||
| No | 13 413 (33.0) | 58 (41.4) | − | 945 (59.4) | 898 (24.1) |
| Yes | 11 751 (28.9) | 82 (58.6) | − | 647 (40.6) | 1308 (35.2) |
Dashes indicate that the variable was not measured
*Owing to missing values, not all variables add up to the total number (and 100%).
†Data obtained from 2006 and to the present.
‡Covers interventions in the municipalities and pharmacies.
GSP, Gold Standard Programme.
Data on GPS and other interventions were available throughout the study period, but data on crash courses were only provided before 2006. Finally, Come & Quit data were recorded from 2011.
A low education level was defined as no education except primary school or short work-related courses.13 Unemployment meant without a job, on sick leave or receiving compensation (in contrast to everyone else, including employees, students/patients under education, retirees and parents on maternity/paternity leave).13
Patients were defined as disadvantaged if they had been unemployed or had a low level of education.13 Heavy smokers were defined as follows: ≥20 pack-years, smoking ≥20 g of tobacco/day or reaching ≥7 points on the Fagerström score.12 19
Statistical analyses
Results are reported as absolute numbers and percentages, including missing data, loss to follow-up and non-respondent analyses according to the RECORD guidelines20 for population and clinical databases (base case). To compare these data to randomised controlled trials, the results were also reported according to the Russell Standards,21 whereby non-respondents were presumed to have relapsed (worst case).
ORs were estimated using logistic regression analyses for men and women separately to test for differences in continuous abstinence levels. Initial analyses included selected prognostic factors from table 1 adjusted for sex and age. Hereafter, the multivariable mixed-effect regression model for clustered data was fitted, and predictors were included based on the initial analyses and established knowledge. The final analyses were adjusted for the time of data collection, geographic regions, age, being a disadvantaged smoker, heavy smoking, compliance, living with a smoker, setting, individual or group format, and supportive medication offered for free, and all predictors were entered together. Patients with missing values were excluded from the analyses. A multivariable analysis was also performed for all patients together to obtain the OR for women compared with that for men. Statistically significant predictors of continuous abstinence were identified. The results are displayed as OR values and as corresponding 95% CIs. Non-respondent analyses were performed using a χ2 test to compare respondents with non-respondents; compliant patients with non-compliant patients and patients who were intentionally not followed up with followed up patients according to the characteristics listed in table 1.
A two-sided p value of <0.05 was considered statistically significant. All statistical calculations were performed using Stata/IC V.14 (StataCorp LP).
Data access and cleaning
In this study, we had full access to the entire SCDB population. All Civil Registration System (CPR) numbers (CPR; a unique 10-digit number including the date of birth and sex assigned to every Dane at birth or to immigrants) were checked according to official validation rules. Invalid CPRs were corrected according to the Civil Registration System.22 Age and sex were corrected accordingly.
Data from 2001 to 2005 were checked manually prior to registration. Questionnaires with missing or invalid data were returned to the smoking cessation units with instructions on how to correct the data. In 2006, data validation rules were established in the online registration application. Dates were validated to avoid non-excising dates, and rules were applied to ensure that required data were entered.
Multiple quit attempts
It was possible for patients to enrol repeatedly and to thereby be registered in the database with two (or more) different entries specifying the intervention, baseline data and a follow-up for each intervention.
Owing to the collection of the CPR, it was possible to identify patients who had multiple interventions from 2006 to 2013. Before 2006, this was not possible. Patients participating in multiple interventions were therefore not excluded from either period.
The extent of duplicates for the 29 102 patients from 2006 to 2013 was 1607 corresponding to 6.6% of the entries. We assumed that this value was similar before 2006 and take this into account in our interpretation of the findings.
Results
This study initially included 46 287 patients. Subsequently 12 052 (26%) patients were lost to follow-up, and 34 235 patients were included in the analyses. This number of missing values was considered small (0–5%), except for free supportive medication, which was 7.2%. The characteristics are given in table 1.
Overall, 33% (11 184) of the responding patients reported being continuously abstinent after 6 months. If the non-respondents were considered to be smokers, this proportion was 24%. Crude quit rates by intervention type and sex are shown in table 2.
Table 2.
Continuous abstinence after 6 months by smoking cessation intervention not adjusted for participant characteristics
| Base case (RECORD criteria20) |
Worst case (Russell criteria21) |
|||||||
|---|---|---|---|---|---|---|---|---|
| All |
Men | Women | All |
Men | Women | |||
| Smoking cessation intervention | n | Per cent | Per cent | Per cent | n | Per cent | Per cent | Per cent |
| Come & Quit | 960 | 22.5 | 21.7 | 23.0 | 1592 | 13.6 | 14.1 | 13.3 |
| Gold Standard Programme | 30 400 | 32.8 | 35.0 | 31.5 | 40 651 | 24.5 | 26.1 | 23.6 |
| Health promotion counselling | 71 | 32.9 | 47.4 | 17.1 | 140 | 17.1 | 25.4 | 8.7 |
| Crash courses | 159 | 27.7 | 36.4 | 21.5 | 183 | 24.0 | 32.0 | 18.5 |
| Other | 2645 | 34.8 | 35.9 | 34.1 | 3721 | 24.8 | 25.3 | 24.4 |
The worst case counted the non-respondents as smokers.
Predictors of abstinence
In the fully adjusted model, women were significantly less likely to remain abstinent than men (17% (OR=0.83, 95% CI 0.79 to 0.87)).
The GSP was the only intervention to present significant outcomes for men and women (table 3).
Table 3.
Explanatory variables included in the final multivariable logistic regression analyses.
| Multivariable analyses OR (95% CI) | Multivariable analyses OR (95% CI) | Interaction with sex | |
|---|---|---|---|
| Men n=11 724 | Women n=18 184 | p Value | |
| Smoking cessation intervention | |||
| Come & Quit | 1 | 1 | |
| Gold Standard Programme | 1.69 (1.27 to 2.24) | 1.31 (1.03 to 1.68) | 0.079 |
| Health promotion counselling | 2.64 (1.21 to 5.72) | 0.48 (0.17 to 1.34) | 0.013* |
| Crash courses | 1.08 (0.58 to 2.02) | 0.49 (0.28 to 0.87) | 0.054 |
| Other | 1.50 (1.09 to 2.06) | 1.20 (0.91 to 1.58) | 0.244 |
| Participants | |||
| Age (years) | |||
| 15–24 years | 1 | 1 | |
| 25–34 years | 1.22 (0.91 to 1.62) | 1.29 (1.06 to 1.57) | 0.918 |
| 35–44 years | 1.37 (1.04 to 1.80) | 1.28 (1.06 to 1.55) | 0.413 |
| 45–54 years | 1.49 (1.14 to 1.96) | 1.31 (1.08 to 1.57) | 0.193 |
| 55+ years | 1.48 (1.13 to 1.94) | 1.35 (1.12 to 1.63) | 0.337 |
| Disadvantaged smokers† | |||
| No | 1 | 1 | |
| Yes | 0.81 (0.73 to 0.89) | 0.82 (0.76 to 0.89) | 0.594 |
| Heavy smokers‡ | |||
| No | 1 | 1 | |
| Yes | 0.73 (0.65 to 0.81) | 0.65 (0.60 to 0.70) | 0.021* |
| Compliance with programme§ | |||
| No | 1 | 1 | |
| Yes | 3.65 (3.29 to 4.04) | 3.58 (3.30 to 3.89) | 0.430 |
| Living with a smoker | |||
| No | 1 | 1 | |
| Yes | 0.94 (0.86 to 1.02) | 0.92 (0.86 to 0.99) | 0.590 |
| Smoking cessation clinic | |||
| Setting | |||
| Citizen aimed | 1 | 1 | |
| Hospital (including midwives) | 1.02 (0.85 to 1.21) | 1.09 (0.94 to 1.27) | 0.982 |
| Other | 1.13 (0.89 to 1.45) | 1.05 (0.84 to 1.31) | 0.191 |
| Smoking cessation intervention | |||
| Programme format | |||
| Individual | 1 | 1 | |
| Group | 0.96 (0.84 to 1.10) | 0.97 (0.87 to 1.08) | 0.696 |
| Medication offered for free | |||
| No free medication | 1 | 1 | |
| Free for days (<1 week) | 0.87 (0.78 to 0.97) | 0.87 (0.80 to 0.96) | 0.199 |
| Free for ≥1 week | 0.97 (0.82 to 1.14) | 0.95 (0.83 to 1.10) | 0.163 |
| Hierarchical cluster | Variance (95% CI) | Variance (95% CI) | |
| Smoking cessation clinic | |||
| Variance of random intercepts | 0.06 (0.04 to 0.11) | 0.07 (0.04 to 0.11) | |
In addition, the model was also adjusted for the time of data collection and for geographic regions. Statistically significant results are marked with an *.
†Disadvantaged smokers: unemployed and receiving unemployment benefits and/or low education (no education except primary schooling and/or only short work-related courses).13
Though applying to very few patients, health promotion counselling seemed to be the most effective intervention for men (OR=2.64; 1.21 to 5.72), followed by the GSP (OR=1.69; 1.27 to 2.24) and other interventions (OR=1.50; 1.09 to 2.06). The effect of crash courses was not significant for men. For women, only the GSP increased the effect significantly (OR=1.31; 1.03 to 1.68).
For men and women, programme compliance was the most pronounced predictor of success, and more advanced age and not being disadvantaged or a heavy smoker were other predictors (see table 3).
An effect of the time of data collection was present, and the likelihood of remaining continuously abstinent for 6 months was slightly higher at the start of the data collection period (data not shown).
Non-respondent analyses
We performed a non-respondent analysis of the 46 287 smokers included in the study by comparing respondents (34 235 smokers) with non-respondents (12 052 smokers lost to follow-up). Respondents and non-respondents were significantly different in regard to every variable tested (see online supplementary appendix). The largest difference between the two groups (16.8 percentage points) was seen in regard to compliance, where the smokers lost to follow-up were less likely to be compliant with the programme. In addition, time of data collection, age, education, employment, pack-years, housing situation, setting, geographic area and planned relapse prevention differed by more than 5 percentage points.
bmjopen-2016-013553supp_appendix.pdf (783.1KB, pdf)
Another analysis performed on 82 387 smokers comparing patients not wanting to be contacted or who were intentionally not followed up (36 100 smokers) with those who were (46 287 smokers) showed differences of up to 8.4 percentage points (see online supplementary appendix). The largest difference was geographic area, but time of collection, and planned relapse prevention also differed by more than 5 percentage points between the compared groups.
Discussion
Overall, every third GSP intervention resulted in a successful outcome after 6 months. Compared with women, men were more successful, with an additional one in six patients being continuously abstinent. Only the GSP showed a significant result regardless of sex even after adjusting for independent variables affecting the outcomes.
Interestingly, the short interventions seemed to be highly effective for men, while women halved their odds of success following short interventions. For both sexes, compliance, as well as advanced age and not being a disadvantaged or a heavy smoker were predictors of successful quitting.
The high effectiveness of the GSP for men and women in our study was also observed in randomised and controlled trials evaluating the programme against typical treatments.23 24 A review found intensive group interventions to be the most effective compared with other formats.25
Compliance was the most important predictor, increasing the odds of abstinence more than 3.5-fold regardless of sex. An earlier study showed a dose-dependent response between compliance and continuous abstinence for GSP; the more sessions attended, the greater the chance of succeeding.17 It should be noted that compliant patients included in our study had several characteristics that were associated with high quit rates.
In line with other studies, we found that even though women were more likely to attend a smoking cessation intervention, they were significantly less likely to succeed than men.25 26 Bohadana et al27 also confirmed these findings, which could be explained by differences in nicotine and behavioural dependence between women and men. Other studies have found no differences in regard to sex28 29 or that women are more likely to quit smoking.30
Though only a few patients undertook short programmes, men showed more promising results, while women showed significantly worse results. Brief interventions are generally recommended, though their overall effect is low. In addition, the setting could be of relevance, as a recent review found no effect of short interventions among surgical patients.31
Interestingly, offering free nicotine replacement therapy (NRT) or other supportive medicine had a negative effect on outcomes. The literature is contradictory on this matter. A recent study from England showed no effect of free NRT in combination with a supportive quit line for patients who wanted to quit.32 In contrast, another study found that offering free NRT increased the chances of success significantly.33 A possible explanation could be the influence of other non-individual variables, such as the type of health system, local general dental practices or the availability of over-the-counter drugs. Further studies are needed to clarify which group of smokers under which conditions would benefit from free NRT.
During the study period from 2001 to 2013, smoking prevalence in Denmark dropped from 30% to 17% daily smokers, corresponding to 1230–780 000 people. Over this period, 82 431 smokers aged 15 years or older received a face-to-face smoking cessation intervention programme registered in the SCDB, corresponding to ∼7–11% of all daily smokers. Converted to a yearly basis, fewer than 1% of the smokers in Denmark have received a face-to-face smoking cessation intervention. This number is very low compared with that of England, where 5–10% of the smokers are treated by the Stop Smoking Service,29 as well as compared with national and international guidelines recommending that 5% of all smokers should receive a smoking cessation intervention yearly. It is difficult to compare the present data to other countries since, to the best of our knowledge, no other countries have clinical registers with national coverage.
This study has limitations as well as strengths. The non-respondent analyses showed that the respondents were more compliant, indicating that the respondents were more likely to be continuously abstinent. Therefore, the results based on the RECORD criteria may overestimate the quit rate when extrapolated to non-respondents. In contrast, the compliance of patients with and without intended follow-up was more similar. Some of the differences identified could be attributed to the large sample size. The follow-up rate was relatively high (74%), and the large number of patients from across the country and across settings was a strength of this study. Even though the coverage was high, the SCDB may not cover all activities. However, only 3 of the 98 municipalities never reported to the database. Smoking cessation intervention activities across regions of Denmark differed more than the distribution of smokers.34 Relatively, the North Denmark Region treated fewer smokers, while the Capital Region of Denmark treated more patients than expected based on the number of smokers in each region. However, even the most active region has treated only 0.6% of all smokers annually which is far lower than the recommended 5%.35 An additional strength was the low amount of missing data. We addressed missing data according to RECORD guidelines.20 Some of the programmes were only recorded in the database in a limited part of the study period. Two of the programmes only had a very low number of participants (0.3% and 0.4%) and the influence on the overall result is therefore very limited. The programme Come & Quit was established in 2011 but includes 3.4% of the smokers and may potentially affect the comparative analyses. However, time for data collection only showed a minor reduction of successful quitting overtime. Thus, the effect of the crash courses recorded only in the beginning of the period may be slightly overestimated. We also reported continuous abstinence as the primary outcome, in contrast to point prevalence, which has several limitations.36 The self-reporting was a limitation, as patients are likely to overestimate their success by 3–6% compared with co-validated outcomes.37–39 We had no reason to assume that this overestimation was unevenly distributed among the different interventions. Therefore, the groups should be comparable, even though the quit rates may be slightly overestimated in general. Owing to different cultural traditions, smoking habits and socioeconomic conditions, generalisations should be considered carefully. The implications of using the routinely collected health data from the SCDB in this study must be considered minimal, as the study is in line with the purposes of the database. Only minor changes in data collection took place over time to include new supportive medicine, and the eligibility has changed over time due to changes in the Danish healthcare system.16 We consider the completeness and precision of the data to be high.8 We are not able to identify possible misclassifications, but we expect their occurrence to be very low. We are also aware of other potential confounders such as genetic predisposition, comorbidities, competing addictions and lifestyle factors that are not included in the analysis due to a lack of information.
From a societal perspective, it is highly interesting that the GSP is effective across different socioeconomic groups. A systematic implementation of the GSP would therefore be highly effective among lower socioeconomic groups with the highest smoking prevalence. Only by collecting nationwide data in a clinical database such as the SCDB it is possible to document this important effect. Furthermore, free NRTs, other supportive medications and self-payment counselling did not show any association with the quit rate, in agreement with a recent publication on financial incentives for smoking cessation.40
This study has raised a new hypothesis on the effectiveness of short interventions among men that should be investigated further.
Another area requiring further investigation is the effectiveness of smoking cessation among groups with very high smoking prevalence, such as mentally ill patients. Recent research indicates that smoking is associated with the development of psychosis because psychosis develops earlier and more frequently among smokers than among non-smokers.41 The high prevalence of smoking among psychiatric patients has traditionally been interpreted as a form of self-medication, but this has now been questioned by a meta-analysis showing that smoking cessation improves the mental conditions of smokers with and without a psychiatric diagnosis.42
A final area of major interest is that smoking cessation databases can be used for early detection, that is, to follow the effects of smoking cessation interventions across a country rather than waiting to see the effect directly on smoking-related illness and death. We recommend that other countries establish national smoking cessation databases for these purposes and for comparing effects between countries.
Conclusion
Over time, Danish smoking cessation interventions have been shown to be effective in real life. Ultimately, one in three smokers are still abstinent at 6 months of follow-up (or one in four if non-respondents are judged as smokers). Compliance is the main predictor of successful quitting. We expected to find that the GSP would be the most effective intervention, but interestingly, short programmes also seem to have relatively strong effect among men, though the absolute numbers are very small. Only the comprehensive standard programme in Denmark, the GSP, works across sexes.
Acknowledgments
The authors thank all participants who agreed to register their data. They thank all staff at the participating smoking cessation units and at the coordination office. The authors also thank the Ministry of Health, the Danish Health Authority, and Bispebjerg and Frederiksberg Hospital for financing the Danish Smoking Cessation Database. EF is partly supported by Grant RTICC RD12/0036/0053 (Instituto de Salud Carlos III, Subdirección General de Evaluación y Fomento de la Investigación, co-funded by the European Regional Development Fund, FEDER).
Footnotes
Twitter: Follow Mette Rasmussen @mettemyr
Contributors: MR and HT contributed to the conception, design and acquisition of data. MR and EF contributed to the analysis of data. MR, EF and HT contributed to the interpretation of data. MR drafted the manuscript and EF and HT revised it critically for important intellectual content. All the authors gave final approval of the version to be published. HT is the guarantor.
Competing interests: None declared.
Ethics approval: The Danish Data Protection Agency (2014–41–3370) and Scientific Ethics Committee (H–C–FSP–2010–049) approved this study and the Danish Data Protection Agency (2000–54–0013) also approved the SCDB.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: Data from the SCDB are archived in the Danish Data Archive. Project descriptions, anonymised data sets and statistical codes used in this study are available from the corresponding author.
All authors, external and internal, had full access to all of the study data (including statistical reports and tables) and take responsibility for the integrity of the data and for the accuracy of the data analysis.
References
- 1.WHO report on the global tobacco epidemic. Raising taxes on tobacco 2015. http://apps.who.int/iris/bitstream/10665/178574/1/9789240694606_eng.pdf?ua=1 (accessed 25 Apr 2016).
- 2.Lim SS, Vos T, Flaxman AD et al. . A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2013;380:2224–60. 10.1016/S0140-6736(12)61766-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.The Health Consequences of Smoking—50 Years of Progress A Report of the Surgeon General. United States Department of Health and Human Services 2014. http://www.surgeongeneral.gov/library/reports/50-years-of-progress/full-report.pdf. (accessed 25 Apr 2016).
- 4.Eriksen M, Mackay J, Schluger NW et al. . The Tobacco Atlas, 5th edition 2015. http://www.tobaccoatlas.org. (accessed 3 May 2016)
- 5.World Health Organisation. Draft comprehensive global monitoring framework and targets for the prevention and control of noncommunicable diseases (A66/8) 2013. http://apps.who.int/gb/ebwha/pdf_files/WHA66/A66_8-en.pdf. (accessed 3 May 2016)
- 6.Thomson G, Edwards R, Wilson N et al. . What are the elements of the tobacco endgame? Tob Control 2012;21:293–5. 10.1136/tc.2010.040881 [DOI] [PubMed] [Google Scholar]
- 7.Danish smoking habits [Danskernes rygevaner]. Copenhagen: Danish Health Authority, The Danish Cancer Society, Danish Heart Foundation, Danish Lung Association, 2013. http://sundhedsstyrelsen.dk/da/sundhed/tobak/tal-og-undersoegelser/danskernes-rygevaner/2013. (accessed 3 May 2016).
- 8.Rasmussen M, Tønnesen H. The Danish Smoking Cessation Database. Clin Health Promot 2016;6:36–41. [Google Scholar]
- 9.Clinical Practice Guideline Treating Tobacco Use and Dependence 2008 Update Panel, Liaisons and Staff. A clinical practice guideline for treating tobacco use and dependence: 2008 update. Am J Prev Med 2008;35:158–76. 10.1016/j.amepre.2008.04.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kjaer NT, Evald T, Rasmussen M et al. . The effectiveness of nationally implemented smoking interventions in Denmark. Prev Med (Baltim) 2007;45:12–14. 10.1016/j.ypmed.2007.04.001 [DOI] [PubMed] [Google Scholar]
- 11.Olsen KR, Bilde L, Juhl HH et al. . Cost-effectiveness of the Danish smoking cessation interventions: subgroup analysis based on the Danish Smoking Cessation Database. Eur J Health Econ 2006;7:255–64. 10.1007/s10198-006-0362-1 [DOI] [PubMed] [Google Scholar]
- 12.Neumann T, Rasmussen M, Heitmann BL et al. . Gold standard program for heavy smokers in a real-life setting. Int J Environ Res Public Health 2013;10:4186–99. 10.3390/ijerph10094186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Neumann T, Rasmussen M, Ghith N et al. . The Gold Standard Programme: smoking cessation interventions for disadvantaged smokers are effective in a real-life setting. Tob Control 2013;22:e9 10.1136/tobaccocontrol-2011-050194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rasmussen M, Heitmann BL, Tønnesen H. Effectiveness of the Gold Standard Programmes (GSP) for smoking cessation in pregnant and non-pregnant women. Int J Environ Res Public Health 2013;10:3653–66. 10.3390/ijerph10083653 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kehlet M, Schroeder TV, Tønnesen H. The gold standard program for smoking cessation is effective for participants over 60 years of age. Int J Environ Res Public Health 2015;12:2574–87. 10.3390/ijerph120302574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rasmussen M, Ammari ABH, Pedersen B et al. . Smoking cessation intervention activities and outcome before, during and after the National Healthcare Reform in Denmark. Clin Health Promot 2012;2:26–35. [Google Scholar]
- 17.Ghith N, Ammari ABH, Rasmussen M et al. . Impact of compliance on quit rates in a smoking cessation intervention: population study in Denmark. Clin Health Promot 2012;2:111–19. [Google Scholar]
- 18.Danish Cancer Association. About Kom & Kvit (Come & Quit). https://www.cancer.dk/komogkvit/engelsk. (accessed 25 Apr 2016)
- 19.Heatherton TF, Kozlowski LT, Frecker RC et al. . The Fagerström test for nicotine dependence: a revision of the Fagerström tolerance questionnaire. Br J Addict 1991;86:1119–27. 10.1111/j.1360-0443.1991.tb01879.x [DOI] [PubMed] [Google Scholar]
- 20.Benchimol EI, Smeeth L, Guttmann A et al. . The REporting of studies Conducted using Observational Routinely-collected health Data (RECORD) statement. PLoS Med 2015;12:e1001885 10.1371/journal.pmed.1001885 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.West R, Hajek P, Stead L et al. . Outcome criteria in smoking cessation trials: proposal for a common standard. Addiction 2005;100:299–303. 10.1111/j.1360-0443.2004.00995.x [DOI] [PubMed] [Google Scholar]
- 22.Pedersen CB. The Danish Civil Registration System. Scand J Public Health 2011;39(Suppl 7):22–5. 10.1177/1403494810387965 [DOI] [PubMed] [Google Scholar]
- 23.Møller AM, Villebro N, Pedersen T et al. . Effect of preoperative smoking intervention on postoperative complications: a randomised clinical trial. Lancet 2002;359:114–17. 10.1016/S0140-6736(02)07369-5 [DOI] [PubMed] [Google Scholar]
- 24.Borglykke A, Pisinger C, Jørgensen T et al. . The effectiveness of smoking cessation groups offered to hospitalised patients with symptoms of exacerbations of chronic obstructive pulmonary disease (COPD). Clin Respir J 2008;2:158–65. 10.1111/j.1752-699X.2008.00055.x [DOI] [PubMed] [Google Scholar]
- 25.Bauld L, Bell K, McCullough L et al. . The effectiveness of NHS smoking cessation services: a systematic review. J Public Health (Oxf) 2010;32:71–82. 10.1093/pubmed/fdp074 [DOI] [PubMed] [Google Scholar]
- 26.Martínez C, Martínez-Sánchez JM, Ballbè M et al. . Smoking cessation in hospital workers: effectiveness of a coordinated program in 33 hospitals in Catalonia (Spain). Cancer Nurs 2012;35:327–36. 10.1097/NCC.0b013e3182321389 [DOI] [PubMed] [Google Scholar]
- 27.Bohadana A, Nilsson F, Rasmussen T et al. . Gender differences in quit rates following smoking cessation with combination nicotine therapy: influence of baseline smoking behavior. Nicotine Tob Res 2003;5:111–16. 10.1080/1462220021000060482 [DOI] [PubMed] [Google Scholar]
- 28.Puente D, Cabezas C, Rodriguez-Blanco T et al. . The role of gender in a smoking cessation intervention: a cluster randomized clinical trial. BMC Public Health 2011;11:369 10.1186/1471-2458-11-369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dobbie F, Hiscock R, Leonardi-Bee J et al. . Evaluating Long-term Outcomes of NHS Stop Smoking Services (ELONS): a prospective cohort study. Health Technol Assess 2015;1:1–156. 10.3310/hta19950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fidler J, Ferguson SG, Brown J et al. . How does rate of smoking cessation vary by age, gender and social grade? Findings from a population survey in England. Addiction 2013;108:1680–5. 10.1111/add.12241 [DOI] [PubMed] [Google Scholar]
- 31.Thomsen T, Villebro N, Møller AM. Interventions for preoperative smoking cessation. Cochrane Database Syst Rev 2014;(3):CD002294 10.1002/14651858.CD002294.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ferguson J, Docherty G, Bauld L et al. . Effect of offering different levels of support and free nicotine replacement therapy via an English national telephone quitline: randomised controlled trial. BMJ 2012;344:e1696 10.1136/bmj.e1696 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.An LC, Schillo BA, Kavanaugh AM et al. . Increased reach and effectiveness of a statewide tobacco quitline after the addition of access to free nicotine replacement therapy. Tob Control 2006;15:286–93. 10.1136/tc.2005.014555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.van der Meer R, Wagena E, Ostelo RW. Smoking cessation for chronic obstructive pulmonary disease. Database Syst Rev 2003;(2):CD002999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Public health guideline: Stop smoking services (PH10). NICE National Institute for Health and Care Excellence 2013. https://www.nice.org.uk/guidance/ph10. (accessed 25 Apr 2016).
- 36.Poulsen PB, Dollerup J, Møller AM. Is a percentage a percentage? Systematic review of the effectiveness of Scandinavian behavioural modification smoking cessation programmes. Clin Respir J 2010;4:3–12. 10.1111/j.1752-699X.2009.00144.x [DOI] [PubMed] [Google Scholar]
- 37.Ferguson J, Bauld L, Chesterman J et al. . The English smoking treatment services: one-year outcomes. Addiction 2005;(Suppl 100):59–69. 10.1111/j.1360-0443.2005.01028.x [DOI] [PubMed] [Google Scholar]
- 38.Judge K, Bauld L, Chesterman J et al. . The English smoking treatment services: short-term outcomes. Addiction 2005;(Suppl 100):46–58. 10.1111/j.1360-0443.2005.01027.x [DOI] [PubMed] [Google Scholar]
- 39.Pisinger C, Vestbo J, Borch-Johnsen K et al. . Acceptance of the smoking cessation intervention in a large population-based study: the Inter99 study. Scand J Public Health 2005;33:138–45. 10.1080/14034940410028370 [DOI] [PubMed] [Google Scholar]
- 40.Halpern SD, French B, Small DS et al. . Randomized trial of four financial-incentive programs for smoking cessation. N Engl J Med 2015;372:2108–17. 10.1056/NEJMoa1414293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gurillo P, Jauhar S, Murray RM et al. . Does tobacco use cause psychosis? Systematic review and meta-analysis. Lancet Psychiatry 2015;2:718–25. 10.1016/S2215-0366(15)00152-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Taylor G, McNeill A, Girling A et al. . Change in mental health after smoking cessation: systematic review and meta-analysis. BMJ 2014;348:g1151 10.1136/bmj.g1151 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2016-013553supp_appendix.pdf (783.1KB, pdf)