Abstract
Introduction
As a consequence of sepsis and intensive care, considerable proportions of patients but also of their spouses develop a post-traumatic stress disorder (PTSD). However, only a very small number receive psychotherapeutic treatment. Internet-based cognitive–behavioural writing therapy (IB-CBWT) has proven to be an effective treatment option for PTSD. It seems to fit the specific needs of this cohort and to overcome treatment barriers. Aim of the REPAIR trial is to examine the efficacy, safety and applicability of IB-CBWT for PTSD in patients and their spouses after intensive care for sepsis.
Methods and analysis
Participants will be assigned randomly either to a treatment or a wait-list (WL) control group. The treatment group receives IB-CBWT for PTSD, actively involving the partners of the participants. IB-CBWT will be guided by a therapist and comprises two written assignments per week over a 5 week period. After completing the assignments, the participants obtain individual responses from the therapist. Participants of the WL control group will receive treatment after a waiting period of 5 weeks. The primary outcome is PTSD symptom severity in self-rated PTSD Checklist for Diagnostic and Statistical Manual Fifth Edition at the end of treatment and waiting time, respectively. Secondary outcomes are remission of PTSD, depression, anxiety, and somatisation measured by the Brief Symptom Inventory-18, marital satisfaction measured by the Relationship Assessment Scale, health-related quality of life measured by the EQ-5D-5L, and the feasibility of IB-CBWT for this cohort (ie, dropout rate). Statistical analysis will be performed according to the intent-to-treat principle.
Ethics and dissemination
The study is conducted according to the principles of Good Clinical Practice and has been approved by the ethics committee of the Friedrich-Schiller University Jena, Germany. Results will be disseminated at scientific conferences, published in peer-reviewed journals, and provided to consumers of healthcare.
Trial registration number
Pre-results, DRKS00010676.
Keywords: Posttraumatic stress disorder, Sepsis, Internet, Cognitive behavior therapy, Randomized controlled trial
Strengths and limitations of this study.
This randomised-controlled trial will provide new evidence concerning the treatment of post-traumatic stress disorder (PTSD) after intensive care for sepsis in patients and their spouses.
For the first time also the spouses of patients with PTSD will be involved in their partners' internet-based cognitive–behavioural writing therapy.
Intervention effects will be compared against a wait-list control group.
It is not possible to ensure a complete blinding of patients and therapists.
Introduction
Psychopathological reactions, that is, acute stress disorder (International Classification of Diseases 10th Revision: F43.0) and post-traumatic stress disorder (PTSD; F43.1), are common consequences of life-threatening events such as sepsis and negatively affect patients' long-term functioning and quality of life.1–4 Critical illness can also be a traumatic and stressful experience for family members as a result of uncertainty and the fear of the patient's physical disability or death. Diagnostic and Statistical Manual Fifth Edition (DSM-5)5 explicitly defined the diagnostic criteria of a traumatic event as an exposure to actual death or serious injury experienced in person or which has occurred to a close family member. Family members, particularly spouses, who care for the critically ill patient during the time of intensive care, are therefore a vulnerable cohort.6–8 In a recent study, up to 69% of the patients, who had survived sepsis and 62% of the spouses of sepsis survivors suffered from clinically relevant PTSD symptoms.9 It has been further shown that both physical and mental health of patients and their spouses are interrelated. More specifically, results of a dyadic analysis indicated that the mental quality of life of a person (patient or spouse) is negatively impacted by post-traumatic stress symptoms of the respective partner. Furthermore, it has been shown that PTSD symptoms of the patient who survived sepsis are a significant predictor of PTSD symptoms of the respective spouse.10 Based on these results, it has been concluded that couples react as a dyadic system with interdependent emotional responses to critical illness. Thus, the inclusion of spouses in the treatment of mental long-term consequences of critical illness appears to be inevitable.9 However, patients suffering from PTSD after critical illness are often untreated or undertreated hereof. Accordingly, Mehlhorn et al11 suggest in their review of interventions for the postintensive care syndrome, that “postintensive care patients may benefit from interventions like trauma-focused cognitive–behavioural therapy […] but often they do not have access to those interventions”. (p. 1268)
With regard to the treatment of PTSD, several evidence-based interventions exist. There is striking evidence for the efficacy of trauma-focused cognitive–behavioural therapy with large effect sizes (standardised mean difference=1.62; 95% CI (1.21 to 2.03) in a meta-analysis of 28 studies) compared against wait-list (WL) control.12 Nevertheless, only a minority of individuals suffering from PTSD seeks psychological treatment due to different barriers (eg, fear of stigmatisation, embarrassment, lack of availability of specialised therapists). In recent years, internet-based interventions based on CBT techniques have overcome these face-to-face treatment barriers by treating mobility-impaired patients, being independent in space and time as well as easily accessible and due to visual anonymity being low-threshold.13–15 The internet-based approach is usually based on a manualised, therapist-assisted treatment which is operationalised via written assignments. In general, treatment as well as the diagnostic screenings (before and after the treatment) are conducted without any face-to-face contact in a secure web portal.13 16 17 Meta-analytic evidence has proven the efficacy of internet-based cognitive–behavioural writing therapy (IB-CBWT) to be large (Hedges′ g=0.95; 95% CI (0.46 to 1.43); 8 studies) in PTSD symptom reduction compared to WL control.15
Up to now, IB-CBWT has not been considered as a treatment approach for PTSD after critical illness and intensive care. Moreover, therapeutic approaches for PTSD that include spouses in addition to the patients are very scarce.
Objectives
Primary aims of the REPAIR trial are to investigate the efficacy, safety and applicability of IB-CBWT for post-traumatic stress after intensive care for sepsis in patients and their spouses compared to a WL control group and to assess maintenance of possible treatment gains at 3, 6 and 12 months post-treatment. Second, the study aims at examining dyadic concordance in treatment effects, that is, indirect effects of the treatment in the respective spouse of the participant of the treatment. Third, the influence of dyadic coping on the treatment effects will be explored.
Methods and analysis
Study design and setting
REPAIR is a randomised-controlled, parallel group, superiority trial. The current study will be conducted at the Jena University Hospital, recruiting participants from German speaking countries (eg, Germany, Austria and Switzerland) at least 1 month after discharge from the intensive care unit (ICU). Participants will be contacted via telephone for initial screening and via internet for delivering the treatment and conducting assessments.
Eligibility criteria
We will include adult (18+ years) patients after intensive care (>5 days) for sepsis18 and their spouses (married or cohabited) who are fluent in written German. A patient–spouse dyad will be included if at least one of them (patient or spouse or both) scores above the PCL-5 cut-off (score ≥33)19 for a presumptive PTSD diagnosis. PTSD should be based on a trauma, which is associated with the critical illness and/or ICU stay. Patients will be excluded, if they do not have a spouse. According to the German clinical guideline on the treatment of PTSD20 acute psychosis and suicidal ideation will be criteria for exclusion. Furthermore, the use of neuroleptics, or an ongoing psychotherapeutic treatment elsewhere will be reasons for exclusion.
Procedures
Recruitment
Since the treatment is delivered internet-based, German speaking patients/spouses could participate from all over the world. For recruitment, we follow a multipartite strategy. First, all persons, that is, patients or spouses, who request free of charge advice from the German Sepsis Aid's National Helpline (http://www.sepsis-hilfe.org) or had requested advice in the past 2 years (altogether about 600 requests), will be contacted and informed about the study. Second, patients of the Mid-German Sepsis Cohort (MSC; trial registration: German Clinical Trials Register, no. DRKS00010050) who are positively screened for PTSD at one of the MSC study assessments will be informed about the study. The MSC aims at following-up about 1000 patients after sepsis per year, of whom we expect about 20% to have PCL scores ≥33 points at least at one follow-up assessment. Third, participants will be recruited via advertisements in health journals and distribution of information brochures in hospitals and rehabilitation centres. In a first telephone contact, participants will be screened for eligibility by using the Life Event Checklist for DSM-5 (LEC 5)21 and the PTSD checklist for DSM-5 (PCL-5).19 Written informed consent will be obtained by the patients and their spouses (see figure 1). One signed version of the informed consent will be sent back to the study centre. After that, an appointment for a second telephone interview will be terminated. In this second telephone contact, patients and their spouses will complete the Clinician-Administered PTSD Scale for DSM-5 (CAPS-5)22 and the Structured Clinical Interview for DSM-IV (SCID-I)23 conducted by a trained psychologist. Medical data will be assessed (eg, length of intensive care and (if) length of mechanical ventilation, time since ICU discharge).
Figure 1.
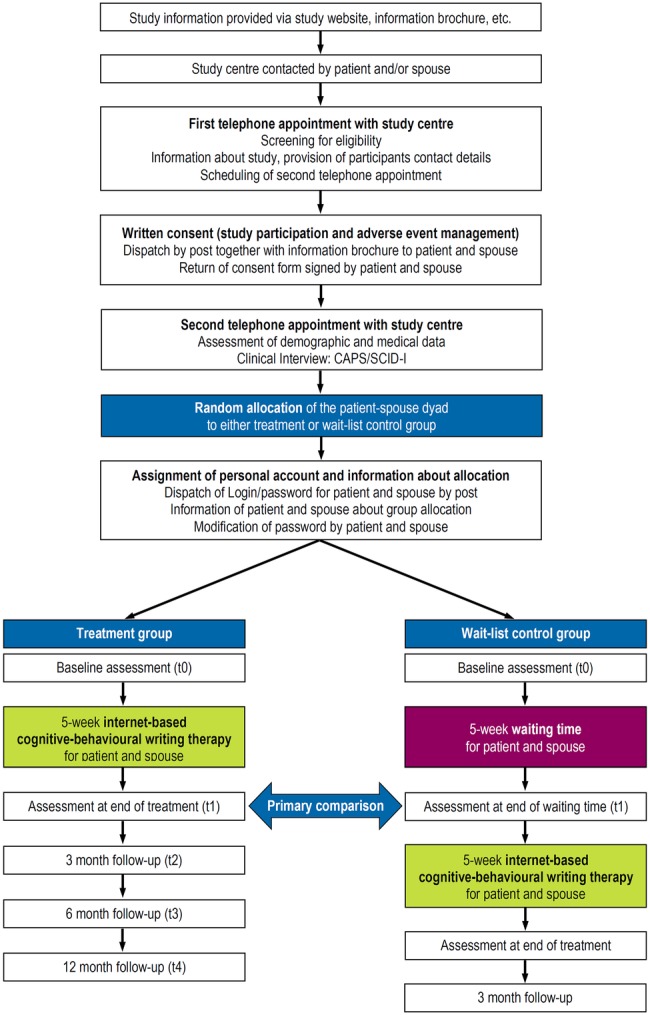
Study flow chart. CAPS/SCID-I, Clinician-Administered PTSD Scale for DSM-5/Structured Clinical Interview for DSM-IV DSM, Diagnostic and Statistical Manual; PTSD, post-traumatic stress disorder.
Randomisation
All eligible patient–spouse dyads consenting to participation will be randomly assigned to either IB-CBWT or to a WL control group (allocation ratio 1:1) with the patient–spouse dyad being the unit of randomisation. Randomisation will be conducted using a central internet-based registration system provided by the Center for Clinical Studies of the Jena University Hospital. This system automatically randomises patients and generates a message noting the assigned treatment. The underlying randomisation list will be developed by an independent biometrician using a computer-based algorithm. Allocation will be concealed and stratified by the occurrence of PTSD symptoms within the dyads of sepsis survivor and the spouse: strata 1—both, sepsis survivor and spouse with PTSD; strata 2—sepsis survivor with PTSD/spouse without, and strata 3—spouse with PTSD/sepsis survivor without.
Baseline assessment (t0)
Before the start of the treatment participants, that is, patients and their spouses, will be asked to complete the following questionnaires: PTSD checklist for DSM-5 (PCL-5),19 Brief Symptom Inventory (BSI),24 Resilience Scale (RS13),25 Proactive Coping Inventory (PCI),26 Multidimensional Fatigue Inventory (MFI),27 EQ-5D-5L health questionnaire,28 Index for Measuring Limitations of Social Participation (IMET),29 Dyadic Coping Inventory (DCI),30 Relationship Assessment Scale (RAS)31 and Internet Literacy Questionnaire (ILQ; subscale technical expertise).32 Additionally, Posttraumatic Cognitions Inventory (PTCI)33 will be assessed only in participants with PCL scores ≥33 points (table 1).
Table 1.
Schedule of the assessments
| Study period |
||||||||
|---|---|---|---|---|---|---|---|---|
| Enrolment | Allocation | Intervention |
Follow-up |
|||||
| Timepoint | tx | t0 | S3 | S7 | t1 | t2 | t3 | t4 |
| Enrolment | ||||||||
| Informed consent | x | |||||||
| Eligibility screen | x | |||||||
| Allocation | x | |||||||
| Interventions | ||||||||
| IB-CBWT |  |
|||||||
| Wait-list control group |  |
|||||||
| Assessments | ||||||||
| Demographic and medical information | x | |||||||
| ILQ | x | |||||||
| CAPS-5 | x | x | ||||||
| SCID-I | x | |||||||
| PCL-5 | x | x | x | x | x | x | x | x |
| LEC-5 | x | |||||||
| BSI | x | x | x | x | x | x | x | |
| RAS | x | x | x | x | x | x | x | |
| IMET | x | x | x | x | x | |||
| RS-13 | x | x | x | x | x | |||
| EQ-5D-5L | x | x | x | x | x | |||
| MFI | x | x | x | x | x | |||
| DCI | x | x | x | x | x | |||
| PTCI | x | x | x | x | x | |||
| PCI | x | x | x | x | x | |||
| SEWIP* | x | x | x | |||||
| Adverse events | x | x | x | |||||
*SEWIP is only applied to patients with PCL scores ≥33.
BSI, Brief Symptom Inventory; CAPS-5, Clinician-Administered PTSD Scale for DSM-5; DCI, Dyadic Coping Inventory; EQ-5D-5L, health questionnaire of the EuroQol group; IB-CBWT, Internet-based cognitive–behavioural writing therapy; ILQ, Internet Literacy Questionnaire; IMET, Index for Measuring Limitations of Social Participation; LEC-5, Life Event Checklist for DSM-5; MFI, Multidimensional Fatigue Inventory; PCI, Proactive Coping Inventory; PCL-5, Post-traumatic stress disorder checklist; PTCI, Post-traumatic Cognitions Inventory; RAS, Relationship Assessment Scale; RS13, Resilience Scale; S3, after treatment session 3; S7, after treatment session 7; SCID-I, Structured Clinical Interview for DSM-IV; SEWIP, Multiperspective Assessment of General Change Mechanisms in Psychotherapy; t0, Baseline, before start of treatment/waiting; t1, after end of treatment/waiting; t2, 3 months after end of treatment; t3, 6 months after end of treatment; t4, 12 months after end of treatment, (t2–t4 only for intervention group); tx, time of enrolment.
Intervention phase
Internet-based writing therapy
Patients and/or spouses with PCL scores ≥33 points, who are allocated to the treatment condition, will participate in an IB-CBWT. They will be asked to complete two 50 min writing assignments per week over a 5-week period (10 essays in total). The therapy consists of three treatment modules (table 2): (1) resource-oriented biographical reconstruction (three essays), (2) in sensu trauma exposure sessions (four essays) and (3) cognitive reconstruction (three essays).
Table 2.
Framework of the 10 writing assignments delivered during IB-CBWT after sepsis for patients and their spouses
| Session number | Session goals | Suggested structure | Suggested tools |
|---|---|---|---|
| 1–3 | Resource-oriented biographical reconstruction. | Explaining the reason of the reconstruction. Provide a list of life-events. Provide a summary and give individual feedback. |
Provide list of possible important personal life events “What problems did you have and how do you solve it?” |
| 4–7 | In sensu exposure. Detailed description of the trauma with all sensations. |
Explain the need of exposure. Explain how to describe the trauma in a written way. Provide a summary and give individual feedback. |
Provide a list of questions due to the traumatic event and the sensations. |
| Text of partner (between 7 and 8) | Supportive letter: acknowledgment of traumatic event. Strength of partner. Joint future. |
Explaining reason of participation. Explain the session goals. | Provide a list of questions due to the goals of the letter. |
| 8–10 | Cognitive reconstruction: writing a letter to an imaginary friend. Writing a letter to oneself. |
Explaining reason of reconstruction. Explain session goals. Provide a summary and give individual feedback. |
Provide a list of questions due to the goals of the letter. eg, “Has something positive resulted from the events?” |
IB-CBWT, Internet-based cognitive–behavioural writing therapy.
Integrated in the third module, the respective partner of the treated participant diagnosed with PTSD receives instructions to write a supportive letter to him/her. Here, the respective partner should announce acknowledgement for the participant as well as his/her strengths and the shared future. Partners without clinically relevant PTSD symptoms will also receive access to an individual web portal where they complete the assessments and write the supportive letter. They further receive psychoeducational information about mental health problems after traumatic events (ie, explanation of PTSD symptoms and treatment options).
At the beginning of each writing assignment, participants propose individual timetables as to when they plan to write. After completion of each assignment, therapists provide individual feedback and further writing instructions within one workday. Important aspects of this feedback are acknowledgement of the participant's courage to disclose and describe their traumatic experiences, reinforcement of the participant's work on the essays, positive feedback and motivation and frequent summaries and encouragement of participants to voice their questions and doubts. Study participants will complete writing assignments through a secure web portal, ensuring that all correspondence is confidential and encrypted. Communication between participants and their therapist will occur asynchronously.
Every participant (patient and spouse) will receive access to a private, secure user account within the web portal. During treatment, all communication will be conducted within this account. Additionally, the therapist accounts are located in the web portal being secure and only accessible for the therapists. A database located at the server of the Jena University Hospital is connected with the web-portal, saving data using anonymous codes meeting the highest security standards.
Therapists
Therapists will be licensed clinical psychologists with previous experience in IB-CBWT. They will receive specialised training in the administration of the treatment and will be supervised continuously throughout the trial. Participants will be consecutively assigned to the therapists. When both, patient and spouse, have clinically relevant PTSD symptoms, they will have different therapists.
Measurement during the course of treatment
During treatment, that is, after assignments 3, 7 and 10, the Multiperspective Assessment of General Change Mechanisms in Psychotherapy (SEWIP),34 measuring resource activation, problem actuation, mastery, clarification of meaning, emotional bond and agreement on collaboration, will be applied to participants of the IB-CBWT group. Additionally, PCL-5, BSI and RAS will be administered during therapy (after assignments 3 and 7).
Measurement at the end of treatment/waiting (t1)
At the end of treatment or waiting time, respectively, the following measures will be applied to the participants: PCL-5, BSI, RS13, PCI, MFI, EQ-5D-5L, IMET, DCI and RAS. Again, PTCI will be assessed only in participants with PCL scores ≥33 points (table 1). Additionally, participants will be interviewed by using the Clinician-Administered PTSD Scale for DSM-5 (CAPS-5).
Wait-list control group
Treatment effects will be compared against a WL control group to allow for the provision of care (if delayed) to all trial participants. After 5 weeks of waiting (duration of treatment), participants allocated to the WL control group will receive IB-CBWT. During and after this delayed application of IB-CBWT, the same measures as in the treatment condition will be assessed. However, these participants will not receive a supportive letter from their spouses. This will allow for evaluating the effect ascribed to the supportive letter.
Follow-up phase
Participants assigned to the treatment group will be followed up 3, 6 and 12 months after treatment, respectively. Participants assigned to the WL control group will be followed up 3 months after treatment. Outcome measures will be assessed again (table 1).
Discontinuation
If a participant meets any of the following criteria, the study intervention will be discontinued: withdrawal of consent to receive the study intervention, emergence of an adverse event (suicidal ideation, severe symptom increase) or start of psychotherapy elsewhere. The participant will be invited to continue completing the planned assessments. If participants withdraw consent to study participation, they will not be contacted for assessments in the future. Participants have the right to initiate deletion of their study data. If a participant does not make use of this right, all data will be included in the analyses.
If either the spouse or patient drops out of the study for any reason, the other participant will be allowed to continue with the intervention and study participation.
Outcome measures
Primary outcome
Primary outcome is the change in PTSD symptom severity score from baseline to 5 weeks after randomisation (t1; at the end of treatment/waiting time) measured via the PTSD Checklist (PCL-5) covering the four DSM-5 clusters.19
Secondary outcomes
Secondary outcomes will be remission at t1 and the percentage of participants leaving the study early (during treatment phase) due to any reason (until t1). Furthermore, anxiety, depression and somatisation (Brief Symptom Inventory-1824), marital satisfaction (Relationship Assessment Scale31) and health-related quality of life (EQ-5D-5L28) all measured as summary scores at t1 and at follow-up (t2–t4: 3, 6, and 12 months).
Other measures
Additionally, we will assess dyadic coping with stress in the patient–spouse dyads using the Dyadic Coping Inventory,30 coping with stress on an individual level using the Proaactive Coping Inventory,26 social participation using the Index for Measuring Limitations of Social Participation,29 resilience (defined as the capacity to withstand life stressors and to thrive and make meaning from challenges35) using the Resilience Scale-13,25 fatigue using the Multidimensional Fatigue Inventory27 and post-traumatic cognitions using the Posttraumatic Cognitions Inventory.33 All of these measures will be applied at baseline (t0), at the end of treatment/waiting time (t1) and at follow-up (t2–t4). During (S3, S7) and at the end of treatment (t1), we will assess common therapeutic factors in patients with PCL scores ≥33 using the Multiperspective Assessment of General Change Mechanisms in Psychotherapy.34
Sample size estimation
The sample size calculation is based on the parametric evaluation of a two-group comparison using Students' t-test, though a more complex statistical model will be used as the primary test. To detect large effect sizes as revealed by a meta-analysis,15 that is, effects of Cohen's d=0.95, while requiring α=0.05 (two-sided) while aiming at a comparison-wise power of 1—β=0.9 (a higher power was chosen to address the problem that a more complex statistical analysis will be used), a sample size of n=2×34=68 patient–spouse dyads is necessary for the intent-to-treat (ITT) analysis. Dropout rates in IB-CBWT are encouragingly low; in a previous study with older adults (65+ years, comparable in age to the population of the proposed study), 89% of the participants completed every step of treatment.16 However, additional dropouts in a sample of sepsis survivors may be due to medical reasons, that is, health impairment or sudden death. Thus, we decided to increase the power by assuming a dropout rate of 30%, so that altogether 98 dyads have to be randomised to either IB-CBWT or WL control group.
Methods against bias
Selection bias will be minimised by random and concealed central allocation of the patient–spouse dyads to treatment and control group using a centralised randomisation by the Center for Clinical Studies of the Jena University Hospital. However, performance bias might not be ruled out because blinding of patients/spouses could not be realised due to intervention characteristics. Similarly, therapists cannot be fully blinded to group assignment since participants receiving treatment the first weeks of recruitment must have been automatically allocated to the treatment group. Treatments will be carefully manualised and predefined in terms of the content and number of sessions. To assure treatment fidelity, verbatim scripts of the correspondence between participants and therapists will be reviewed. Treatment fidelity checks will be performed based on a random selection of 30% of treatment sessions. Data will be analysed using an ITT approach. To ensure data quality, diagnoses will be made on the basis of a validated clinical interview conducted by a clinically experienced and trained psychologist. Questionnaires that will be used in the proposed study have been proven to be psychometrically sound instruments. To reduce the risk of sampling bias and to assure external validity, we will use a multipartite recruitment strategy and apply less restrictive eligibility criteria.
Statistical analyses
The primary end point of the efficacy assessment (PCL-5 change score at the end of the treatment, t1, ie, ∼6 weeks after randomisation; relative to the randomisation t0) will be compared between both groups (ie, experimental group and WL control group). The null hypothesis μEXP=μWL, which implies that the PCL-5 change scores are identical in expectation, will be tested against the (two-sided) alternative hypothesis that there will be a difference between the groups (μEXP ≠ μWL). The confirmatory analysis will be performed in the ITT population. These hypotheses will be tested using a general linear model for the primary outcome and the group factor adjusted for PCL-5 at baseline (t0) with generalised estimating equations component to address the possible intradyad clustering. The null hypothesis will be rejected when the two-sided p value for the group variable is equal to or less than the two-sided significance level α=0.05. The average mean difference in the PCL-5 change scores at t1 is assumed to be clinically relevant when the mean PCL-5 score is more than 10 points lower for the experimental group than for the WL control group.19
We will address missing values by replacing all missing change scores with the worst change observed. Furthermore, we will explore the potential impact of dropouts (ie, missingness not completely at random) on the results in sensitivity analyses that will be outlined in the statistical analysis plan (SAP).
Additionally, there will be sensitivity analyses, for example, in the per-protocol (PP) population or stratified by patient and spouse. All additional analyses and the analyses of secondary end points will be carried out exploratively, that is, without adjustment for multiplicity. We will use adequate standard descriptive and inferential statistical techniques that are described in detail in the SAP. For the third explorative objective—dyadic interference in mental health—we will use a longitudinal Actor-Partner-Interdependence Model. To examine the impact of dyadic coping on treatment effects, we will extend the previously applied regression models.
Data collection and management
Data collection
Relevant data will be collected via telephone and using questionnaires delivered via the web-portal. Telephonically assessed data will be documented in writing and transferred to the study management software ‘OpenClinica’. Data assessed by using standardised questionnaires within the web-portal, will be collected via a secure network (HTTPS) using input forms in the web browser. Data will be saved by using anonymised codes on a server of the Jena University Hospital ensuring highest safety standards.
Data management
Data management will be conducted by using the study management software ‘OpenClinica’ meeting common regulatory requirements (GCP, 21CFRPart11). To ensure a pseudonymised data analysis, every participant will receive a distinct ID. Data will be checked regularly for accuracy, implausible or missing data will be enquired in the study centre.
Study monitoring
The current study will be monitored by an independent data manager of the Centre for Clinical Studies of the Jena University Hospital including periodic inspections of the completeness and correctness of study documents and study data.
Premature termination of the study
Reasons for a premature termination of the study will be unjustifiable risks of continuation, new scientific findings during study duration or inadequate recruiting rate. Decision about discontinuation will be taken jointly by the principal investigators, the study biometrician and the Data Safety and Monitoring Board.
Reporting of adverse events
Assessment of safety will include recording any adverse effects during the treatment period by asking participants for experienced adverse events at the end of the treatment. In addition, during treatment participants are provided a telephone contact for emergency cases. In such a case, adverse events will be documented by the study team.
Ethical considerations and dissemination
Informed consent
All eligible participants will be informed orally by a trained clinical psychologist about aims, content, procedure and length of the study; and about any potential risks and advantages in a true manner. After providing the opportunity to ask questions, written consent will be obtained by sending the informed consent document back to the study centre. Participants further receive a brochure with detailed information about the study. Participation is voluntary at any time. Participants will be informed about the voluntariness of study participation and the opportunity to interrupt or prematurely terminate study participation without giving reasons.
Ethics review
The study has been approved by the ethics committee of the Friedrich-Schiller University Jena, Germany (number 4777-04/16, 11 May 2016). The trial is registered in the German Clinical Trials Register (DRKS); number DRKS00010676. Modifications in the study protocol will be communicated to the ethics committee as well as the DRKS.
Access to data
Principal investigators and the study statistician will have access to the final data set. To ensure confidentiality, data dispersed to project team members will be blinded of any identifying participant information.
Dissemination
Results of this study will be presented at scientific conferences and published in peer-reviewed journals. Furthermore, we will disseminate results and conclusions to consumers of healthcare. The study will be implemented and reported in line with the CONSORT statement. Authorship is granted to authors who make important contributions to the creation of the final publication.
Discussion
This study aims to provide new evidence of treatment approaches particularly designed for patients after critical illness such as sepsis. The current study also involves the spouse of the affected patient since critical illness has consequences not only for the patient itself, but also for his/her spouse who shares concerns, sorrows and problems.
The limitation of this study is that the intervention effects will be compared against a WL control group which might overestimate the efficacy of the treatment to a certain degree.36 This will be taken into account in the interpretation of the results. Moreover, evidence-based treatment approaches of in post-ICU patients are rare.11 This argues against an active control condition. Alternatively, psychological treatment placebo faces the problem that the development of such a control condition in PTSD trials ‘is very difficult, if not impossible’.12
Moreover, performance bias will possibly influence the effects since participants cannot be blinded because they are aware of their group allocation. Additionally, therapists will not be blinded to group assignment. However, manualisation of the treatment and treatment fidelity checks will counter the risk of bias.
Despite these limitations, this is the first randomised controlled trial to assess the efficacy, safety and applicability of an IB-CBWT after sepsis in patients and their spouses. Given the sparse number of existing treatment approaches for this group of patients IB-CBWT might be a valuable addition in the treatment of PTSD after sepsis. The results of this study will hopefully improve healthcare after sepsis for patients and their spouses. Given the efficacy, safety and applicability of this approach, the treatment could be easily transferred to other languages and thereby disseminated internationally.
Acknowledgments
The authors would like to thank Ulrike Redlich and Monique Vogel from the German Sepsis Aid for their support in recruitment. Thanks are also due to Thomas Lehmann for providing the randomisation tool and Margit Leitner for her help with the design of the information material and the website. The authors very much appreciate the informatics support provided by Uwe Ziegler, Cornelia Baumgart, Sebastian Burchert and Florian Rissner. The authors would also like to thank Cornelia Platzer, Stephanie Platzer, Isabella Schiller and Cornelia Eichhorn for their support regarding the study management.
Footnotes
Contributors: JR and CK conceived and designed the study, and drafted the grant proposal. RG and JR drafted the protocol of the study, and organise and supervise study implementation. HN, MB, AS and CK refined the study protocol and study implementation. HN, MB and CK developed the treatment manual. AS provides methodological and statistical expertise. CK supervises the therapists. All authors critically reviewed and approved the final version of the manuscript.
Funding: This study is funded by the German Federal Ministry of Education and Research, grant number 01EO1002.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Davydow DS, Gifford JM, Desai SV et al. Posttraumatic stress disorder in general intensive care unit survivors: a systematic review. Gen Hosp Psychiatry 2008;30:421–34. 10.1016/j.genhosppsych.2008.05.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Needham DM, Davidson J, Cohen H et al. Improving long-term outcomes after discharge from intensive care unit: report from a stakeholders’ conference. Crit Care Med 2012;40:502–9. 10.1097/CCM.0b013e318232da75 [DOI] [PubMed] [Google Scholar]
- 3.Parker AM, Sricharoenchai T, Raparla S et al. Posttraumatic stress disorder in critical illness survivors: a metaanalysis. Crit Care Med 2015;43:1121–9. 10.1097/CCM.0000000000000882 [DOI] [PubMed] [Google Scholar]
- 4.Boer KR, van Ruler O, van Emmerik AA et al. Factors associated with posttraumatic stress symptoms in a prospective cohort of patients after abdominal sepsis: a nomogram. Intensive Care Med 2008;34:664–74. 10.1007/s00134-007-0941-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5®). 5th edn Washington DC: American Psychiatric Association, 2013. [Google Scholar]
- 6.Hickman RL Jr, Douglas SL. Impact of chronic critical illness on the psychological outcomes of family members. AACN Adv Crit Care 2010;21:80–91. 10.1097/NCI.0b013e3181c930a3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Davidson JE, Jones C, Bienvenu OJ. Family response to critical illness: postintensive care syndrome-family. Crit Care Med 2012;40:618–24. 10.1097/CCM.0b013e318236ebf9 [DOI] [PubMed] [Google Scholar]
- 8.Petrinec AB, Daly BJ. Post-traumatic stress symptoms in post-ICU family members: review and methodological challenges. West J Nurs Res 2016;38:57–78. 10.1177/0193945914544176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rosendahl J, Brunkhorst FM, Jaenichen D et al. Physical and mental health in patients and spouses after intensive care of severe sepsis: a dyadic perspective on long-term sequelae testing the Actor-Partner Interdependence Model. Crit Care Med 2013;41:69–75. 10.1097/CCM.0b013e31826766b0 [DOI] [PubMed] [Google Scholar]
- 10.Wintermann GB, Weidner K, Strauss B et al. Predictors of posttraumatic stress and quality of life in family members of chronically critically ill patients after intensive care. Ann Intensive Care 2016;6:69 10.1186/s13613-016-0174-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mehlhorn J, Freytag A, Schmidt K et al. Rehabilitation interventions for postintensive care syndrome: a systematic review. Crit Care Med 2014;42:1263–71. 10.1097/CCM.0000000000000148 [DOI] [PubMed] [Google Scholar]
- 12.Bisson JI, Roberts NP, Andrew M et al. Psychological therapies for chronic post-traumatic stress disorder (PTSD) in adults. Cochrane Database Syst Rev 2013;(12):CD003388 10.1002/14651858.CD003388.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Knaevelsrud C, Maercker A. Internet-based treatment for PTSD reduces distress and facilitates the development of a strong therapeutic alliance: a randomized controlled clinical trial. BMC Psychiatry 2007;7:13 10.1186/1471-244X-7-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.van Emmerik AA, Reijntjes A, Kamphuis JH. Writing therapy for posttraumatic stress: a meta-analysis. Psychother Psychosom 2013;82:82–8. 10.1159/000343131 [DOI] [PubMed] [Google Scholar]
- 15.Küster A, Niemeyer H, Knaevelsrud C. Internet-based interventions for posttraumatic stress: a meta-analysis of randomized controlled trials. Clin Psychol Rev 2016;43:1–16. 10.1016/j.cpr.2015.11.004 [DOI] [PubMed] [Google Scholar]
- 16.Knaevelsrud C, Böttche M, Pietrzak R et al. Integrative testimonial therapy: an Internet-based, therapist-assisted therapy for German elderly survivors of the World War II with posttraumatic stress symptoms. J Nerv Ment Dis 2014;202:651–8. 10.1097/NMD.0000000000000178 [DOI] [PubMed] [Google Scholar]
- 17.Knaevelsrud C, Brand J, Lange A et al. Web-based psychotherapy for posttraumatic stress disorder in war-traumatized Arab patients: randomized controlled trial. J Med Internet Res 2015;17:e71 10.2196/jmir.3582 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Singer M, Deutschman CS, Seymour CW et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 2016;315:801–10. 10.1001/jama.2016.0287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Weathers FW, Litz BT, Keane TM et al. The PTSD Checklist for DSM-5 (PCL-5). National Center for PTSD, 2013. http://www.ptsd.va.gov [Google Scholar]
- 20.Flatten G, Gast U, Hofmann A et al. [S3—guideline for posttraumatic stress disorder ICD-10: F43.1]. Stuttgart: Schattauer, 2013. [Google Scholar]
- 21.Weathers FW, Blake DD, Schnurr PP et al. The Life Events Checklist for DSM-5 (LEC-5). National Center for PTSD, 2013. http://www.ptsd.va.gov [Google Scholar]
- 22.Weathers FW, Blake DD, Schnurr PP et al. The Clinician-Administered PTSD Scale for DSM-5 (CAPS-5). National Center for PTSD, 2013. http://www.ptsd.va.gov [Google Scholar]
- 23.Wittchen HU, Zaudig M, Fydrich T. [Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I)]. Göttingen: Hogrefe, 1997. [Google Scholar]
- 24.Derogatis LR. Brief Symptom Inventory (BSI) 18. Administration, scoring and procedures manual. Minneapolis, MN: NCS Pearson, 2000. [Google Scholar]
- 25.Leppert K, Koch B, Brähler E et al. [Resilience scale—evaluation of a long (RS-25) and a short version (RS-13)]. Klinische Diagnostik und Evaluation 2008;2:226–43. [Google Scholar]
- 26.Greenglass ER, Schwarzer R, Taubert S. The Proactive Coping Inventory (PCI): a multidimensional research instrument. Toronto: York University, 1999. http://estherg.info.yorku.ca/greenglass-pci/ [Google Scholar]
- 27.Smets EMA, Garssen B, Bonke B et al. The Multidimensional Fatigue Inventory (MFI): psychometric qualities of an instrument to assess fatigue. J Psychosom Res 1995;39:315–25. 10.1016/0022-3999(94)00125-O [DOI] [PubMed] [Google Scholar]
- 28.Herdman M, Gudex C, Lloyd A et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res 2011;20:1727–36. 10.1007/s11136-011-9903-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Deck R, Mittag O, Hüppe A et al. [Index for Measuring Limitations of Social Participation (IMET)—first results of an ICF-based assessment instrument]. Praxis Klinische Verhaltensmedizin und Rehabilitation 2007;20:113–20. [Google Scholar]
- 30.Bodenmann G. [Dyadic Coping Inventory (DCI). Test manual] Bern: Huber, 2008. [Google Scholar]
- 31.Hendrick SS. A generic measure of relationship satisfaction. J Marriage Fam 1988;50:93–8. 10.2307/352430 [DOI] [Google Scholar]
- 32.Wegmann E, Stodt B, Brand M. Addictive use of social networking sites can be explained by the interaction of Internet use expectancies, Internet literacy, and psychopathological symptoms. J Behav Addict 2015;4:155–62. 10.1556/2006.4.2015.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Foa EB, Ehlers A, Clark DM et al. The Posttraumatic Cognitions Inventory (PTCI): development and validation. Psychol Assess 1999;11:303–14. 10.1037/1040-3590.11.3.303 [DOI] [Google Scholar]
- 34.Mander JV, Wittorf A, Schlarb A et al. Change mechanisms in psychotherapy: multiperspective assessment and relation to outcome. Psychother Res 2013;23:105–16. 10.1080/10503307.2012.744111 [DOI] [PubMed] [Google Scholar]
- 35.Wagnild GM, Young HM. Development and psychometric evaluation of the Resilience Scale. J Nurs Meas 1993;1:165–78. [PubMed] [Google Scholar]
- 36.Furukawa TA, Noma H, Caldwell DM et al. Waiting list may be a nocebo condition in psychotherapy trials: a contribution from network meta-analysis. Acta Psychiatr Scand 2014;130:181–92. 10.1111/acps.12275 [DOI] [PubMed] [Google Scholar]


