Abstract
Objective
To explore parents' views of extending the human papillomavirus (HPV) vaccination programme to also include boys.
Design
Explorative qualitative design using individual, face-to-face, interviews and inductive thematic analysis.
Setting
11 strategically chosen municipalities in central Sweden.
Participants
Parents (n=42) who were offered HPV vaccination for their 11–12 years old daughter in the national school-based vaccination programme.
Results
The key themes were: equality from a public health perspective and perception of risk for disease. Parents expressed low knowledge and awareness about the health benefits of male HPV vaccination, and they perceived low risk for boys to get HPV. Some parents could not see any reason for vaccinating boys. However, many parents preferred gender-neutral vaccination, and some of the parents who had not accepted HPV vaccination for their daughter expressed that they would be willing to accept vaccination for their son, if it was offered. It was evident that there was both trust and distrust in authorities' decision to only vaccinate girls. Parents expressed a preference for increased sexual and reproductive health promotion such as more information about condom use. Some parents shared that it was more important to vaccinate girls than boys since they believed girls face a higher risk of deadly diseases associated with HPV, but some also believed girls might be more vulnerable to side effects of the vaccine.
Conclusions
A vaccine offered only to girls may cause parents to be hesitant to vaccinate, while also including boys in the national vaccination programme might improve parents' trust in the vaccine. More information about the health benefits of HPV vaccination for males is necessary to increase HPV vaccination among boys. This may eventually lead to increased HPV vaccine coverage among both girls and boys.
Keywords: Parents, Vaccination programme, HPV vaccination, Boys, Human papillomavirus, Views
Strengths and limitations of this study.
This is the first interview study about parents' views of including boys in the national school-based human papillomavirus vaccination programme in Sweden.
Our study includes parents who had declined as well as parents who had accepted vaccination for their daughter, and the included parents' represent a broad variation of urban and rural areas in different regions.
The study provides new insights and reports a diverse range of views, including favourable and negative examples of adaption.
It would have been even better if we had been able to include more parents with an immigrant background and parents with lower educational levels, as well as more fathers.
This is a qualitative study and the results cannot be generalised to the whole population. The results may however be transferable to other settings.
Introduction
Human papillomavirus (HPV) is a significant contributor to the global cancer burden. The virus is transmitted through sexual contact, and both men and women can be affected. The high-risk HPV types can cause precancerous lesions, which, in turn, may progress to cancer, mainly cervical cancer, the third most common cancer among women worldwide. HPV is also a major cause of cancer in the head and neck, anus, vulva, vagina and penis.1 2 Thus, men are also affected by HPV infection and HPV-related cancer.3–5 Head and neck cancer is rapidly increasing.4 6 7 HPV infections are common among both women and men; the estimated lifetime probability of an infection is over 80%.8
National vaccination programmes against HPV are implemented in almost all European countries and a large number of countries worldwide.9 10 The HPV vaccine is highly efficient and safe,11–13 resulting in a reduction in cervical lesions and condy loma.14–16 However, the vaccine uptake in most countries is suboptimal.9 In Sweden, the vaccine has been included in the national vaccination programme since 2012, offered to young girls 10–12 years of age. The vaccine is provided by the school health services free of charge and requires parental consent. The vaccination coverage for dose 1 is about 80% and even lower for the full course, which is significantly lower compared with other childhood vaccinations reaching an uptake above 95%.17 Most countries only include girls in the national vaccination programmes; however, a few countries, such as Australia, Austria, USA and some provinces in Canada have implemented gender-neutral vaccinations against HPV.18 19
Trust in governmental recommendations and vaccine efficacy and safety are important factors for successful vaccination programmes.20 21 According to a recent web-based survey22 among European parents, most seem to be in favour of HPV vaccination of their sons. Studies from the USA23 24 also indicate that parents are reasonably willing to vaccinate their sons against HPV. The main reasons for acceptance are concerns for their health and to protect their sons against HPV-related diseases.22 24–26 Another important factor associated with vaccine acceptance is low concern about side effects.24 On the other hand, scepticism about the vaccine and fear of side effects are barriers for vaccine acceptance for boys.22 Lack of knowledge and awareness are other barriers.22 24 Knowledge about HPV and HPV vaccine is low among the general population as well as among adolescents and parents, and few are aware of HPV vaccinations for boys.24 25 27–29
There is currently a discussion about how to strengthen HPV vaccination programmes in order to achieve herd immunity and reduce global burden of HPV-related cancer. One way to strengthen the vaccination programme and to accelerate reduction of HPV prevalence is by including boys.30 31 Previous studies22 24 28 on parents' beliefs and attitudes towards including the vaccinations for boys have focused on the intention to vaccinate. This study, on the other hand, is directed to parents who had already made an active decision about HPV vaccination for their daughters in a school-based setting. In order to increase the knowledge gap regarding parents' views about HPV vaccination of boys, the aim of this qualitative study was to explore parents' views of extending the national vaccination programme to also include boys.
Methods
Study design
An explorative qualitative design using individual, face-to-face interviews with parents of young children, where the results are reported according to COREQ.32
Setting and participants
We recruited parents in 11 strategically chosen municipalities in the central regions of Sweden. In the chosen municipalities, the vaccination programme had started in all schools, in some other areas the vaccination programme started later. Parents who were offered HPV vaccination for their young daughter were eligible and invited to participate.
Data collection
The heads of the school health services in the different municipalities informed school nurses about the study and asked them to assist in the recruitment of parents. Nurses who agreed to assist distributed an invitation letter to all parents of 11–12 years old girls in their schools. Approximately 3000 invitation letters were distributed to the school nurses for further distribution. Parents interested in sharing their views about HPV vaccination in an interview were asked to contact the researchers for more information and to suggest a time and place for the interview. Interviews took place at a location most convenient for the parent, for example, at their homes or the parent's or the researcher's workplace. No one besides the researcher and the parent were present at the interview. Every interview started with verbal information about the aim of the study and acknowledging that participation was voluntary. Parents were asked to sign a consent form and to fill in a short questionnaire with demographic questions. Thereafter, the interview started, see interview guide below. If the parents had questions to the researcher about the subject, those were responded to and discussed after the interview.
We audio-recorded the interviews, and the recorded time of the interviews was in general between 30 and 45 min. The parents received a movie ticket in return for their participation. We continued with data collection until little new information emerged from the interviews. Interviews were conducted between March 2012 and April 2013, and each interview was transcribed verbatim soon thereafter. No repeat interviews were carried out. The three authors conducted the main part of the interviews; in addition, two other female researchers (PhD) from the research group conducted a few interviews. The interviewers were registered nurses or midwives and experienced in qualitative interviewing, and they had similarities with the informants in that they were also mothers. No previous relationship between the researcher and the informant existed before the informant contacted the researcher about the interview.
Interview guide
A semistructured interview guide was used. The main question asked was: What is your view on vaccinating boys against HPV? Follow-up questions and probes, such as Can you please explain more about that? were also used. Three pilot interviews were conducted by MGr in February 2012, before the start of the study. These interviews are not included in the present study. No significant changes were made in the interview guide after the pilot interviews.
Analysis
The interviews were analysed with thematic content analysis.33 The transcripts were read several times to get an overall picture of what was said. Notes, which function as the initial codes, were made in the margin of the transcripts. The codes were then extracted from the transcripts, and reduction of codes was made through removing duplicates; thereafter, categorisation was done by grouping together overlapping or similar codes. The transcripts were then read again, and meaning units were sorted into suitable categories. We used Excel to manage the data. An example of the analytical process is presented in table 1.
Table 1.
Example of the analytical process
| Meaning unit from interview transcript | Subcategory | Category | Theme |
|---|---|---|---|
| “It is quite characteristic of our society…that experiments are conducted on girls and young women and that it is they who must take responsibility [for sexual and reproductive health].” (Mother, interview #24, no) | Distrust: women responsible by tradition | Trust and distrust in authorities' decision | Equality from a public health perspective |
| “So, it is about cervical cancer, and a guy cannot get that, so there's not so much to think about.” (Mother, interview #21, yes) | Unaware of low knowledge | Inadequate knowledge about HPV and HPV vaccine | Perception of risk for disease |
HPV, human papillomavirus.
The initial analysis was made separately by MGo and MGr. The analysis process was rigorous and systematic; the researchers returned to the transcripts to make sure that all data were thoroughly analysed. In order to avoid lone researcher bias,33 two researchers individually read the transcripts to identify categories. All researchers took part in discussing the categories and themes until a consensus was reached. The criteria for assessing the quality and trustworthiness of the conducted studies, as described by Guba and Lincoln,34 including credibility, dependability, confirmability and transferability were considered. Results have been presented as close to original interviews as possible, quotations are included for trustworthiness of the analysed data.35 The informants did not provide feedback on the results, but respondent validations were performed at end of each interview when the researcher summarised what parents had said to see if the information had been understood correctly. As in all qualitative research, the aim is not to generalise, but to provide a better understanding of the informants' perspective.35
Since little is known about parents' view on extending the vaccination programme to include HPV vaccination of boys, we used an inductive approach and no predetermined theory was considered in the analysis. However, the results are discussed from a public health perspective in light of the principles of justice.36
Results
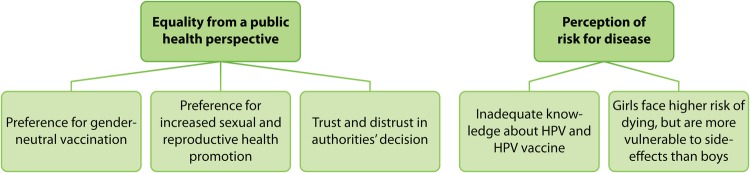
A total of 42 parents (38 women, 4 men) were included in this study. Characteristics of the participants are presented in table 2. The qualitative content analysis resulted in two main themes: equality from a public health perspective and perception of risk for disease. Each theme includes two to three categories (see figure 1).
Table 2.
Characteristics of parents (N=42)
| Characteristic | Consenting HPV vaccine (n=22) | Declining HPV vaccine (n=20) |
|---|---|---|
| Age, mean | 43.7 (range 36–52) | 43.3 (range 37–55) |
| Relationship to daughter | ||
| Mother | 20 | 18 |
| Father | 2 | 2 |
| Country of birth | ||
| Sweden | 19 | 19 |
| Other country | 3 (1 non-European) | 1 |
| Highest level of education | ||
| College/university | 18 | 14 |
| Primary education/secondary school | 4 | 5 |
| Vocational training/education | 0 | 1 |
| Civil status | ||
| Married or cohabiting | 21 | 17 |
| Single or other civil status | 1 | 3 |
| More than one child | 21 | 19 |
| Have a son | 16 | 15 |
HPV, human papillomavirus.
Figure 1.
Themes and categories that emerged through the analysis. HPV,human papillomavirus.
Equality from a public health perspective
Preference for gender-neutral vaccination
Many of the interviewed parents were in favour of a gender-neutral vaccination programme for HPV. Some of the parents who had not accepted HPV vaccination for their daughters were willing to accept vaccination for their sons if they were offered the vaccine. It was also expressed that if boys were also offered the vaccine, parents who had declined for their daughter would more easily accept the vaccine, both for their daughter and son.
We felt like this, maybe we should wait a year or so until there is also a vaccine for boys, because that is on its way, we know that…and then we can think that boys should actually do it too, because we know that boys are the ones who are transmitting the virus to girls…so we would have vaccinated him if it had been offered, without a doubt…Because I think we would not hesitate if it is so, that it is available for boys. Yes, then it's fine, then we know that it is a generally decided programme, that there is no gender quotas, but both boys and girls are to be vaccinated. (Mother, interview #40, no)
Some parents were not sure of the fact that boys could transmit this virus but said that if they could, they should, of course, also be vaccinated, even if they were not at risk of getting cancer. Some parents were, however, aware of the fact that boys can also be affected by HPV and believed they should be vaccinated, both to decrease the transmission of HPV and to decrease their own risk of getting HPV-related disease. It was also mentioned by a few that boys should also be vaccinated to minimise the transmission of condyloma.
Because girls get it from boys, so that’s an interesting question, why are they not all vaccinated? It is actually really strange. (Mother, interview #1, yes)
I think boys should also be vaccinated, because, I mean, if a girl does not get vaccinated and she has it and the boy transmits it to someone else. I mean, I don't get it really, when you can vaccinate both sexes. (Mother, interview #10, yes)
Preference for increased sexual and reproductive health promotion
Parents expressed that vaccination should be complemented by information given to young people about other preventive measures such as condom use and delay of sexual debut, because they believed that information could also have a preventative effect. Some parents felt that boys were excluded from this campaign and discussion and that they should receive more information about the risk for boys to get HPV and how it could affect them.
What I have missed and what makes me really sad is that the information is so bad, I think…that we don't talk to our children and young people about preventative measures…why can we not propagate more to inform more and not to be in such a rush…this has to do with your health, wait, and use a condom and all that. Why don't the authorities work more like that, I think? (Mother, interview #40, no)
However, one parent was not in favour of either information or vaccination.
I just think that this is also some kind of pointer for the young people really, to think for themselves now. I think this is a great big pointer just to scare. And I also think it's really overrated. (Mother, interview #42, no)
Trust and distrust in authorities decision
Many parents could understand why only girls receive the vaccine for free in the national programme and expressed a trust in the authorities’ ability to make good decisions. They believed economical assessments and cost-effectiveness had played a big role in the decision.
I guess that there has been some economic assessment, how much money we will spend on it and then they have made a choice, and one is forced to do that. (Mother, interview #9, yes)
There must be some research that shows that it is most effective to give it to girls. (Mother, interview #14, yes)
Taking care of girls' health and knowing that girls now had the opportunity to get protection from some types of cancer was seen as very positive by parents. One parent saw this positive special treatment as surprising.
I think it's great…I think girls have it pretty tough…so I thought this was like a positive thing, to protect girls, their needs and so on. It's very new to me. (Mother, interview #37, no)
However, not all parents were positive to the decision and felt rather distrustful of the authorities' decision—the vaccination programme was viewed as an experiment on girls. Some parents also felt that this was a gender issue in that research was being done on women because we live in a male-dominated society. Another gender issue that was expressed was that girls often, and by tradition, have to take responsibility for sexual and reproductive health issues.
It is quite characteristic of our society…that experiments are conducted on girls and young women and that it is they who must take responsibility [for sexual and reproductive health]. (Mother, interview #24, no)
Perception of risk for disease
Inadequate knowledge about HPV and HPV vaccine
Inadequate knowledge about the virus and the vaccine was apparent in some interviews. Some parents could not see any reason for including boys in the HPV vaccination programme since they believed the vaccine gave protection against a type of cancer that only women could be affected with and therefore, boys were not at risk for developing HPV-related disease.
If it is about cervical cancer then it is not a vaccine that is something that one needs to waste on boys, it is well understood that if you don't have a cervix you should not have this vaccine. (Father, interview #2, yes)
So, it is about cervical cancer, and a guy cannot get that, so there's not so much to think about. (Mother, interview #21, yes)
Several parents expressed they did not know that boys could be vaccinated against HPV and felt that they had very little knowledge about the vaccine and what it protects from.
Girls face higher risk of dying but are more vulnerable to side effects than boys
Parents expressed that even if boys could be affected by the virus and contract condyloma, girls were more vulnerable and faced higher risk of deadly diseases associated with HPV.
Very few parents mentioned that HPV could cause cancer in boys.
So, there's the risk of cancer for girls and that is a greater risk. And I know too little about what it would mean for men. So, if men were to also get vaccinated, it's about…if it's some kind of disease transmission then or if there are types of cancers that may arise. I know too little about it. (Father, interview #12, yes)
It was also mentioned that girls were more exposed to hormones, such as contraceptive pills and that it might be dangerous to mix the vaccine with too many drugs or hormones. Therefore, some parents preferred male vaccinations since boys, in contrast to girls, would not become pregnant later in life and carry a child.
Discussion
Principal findings
The parents in our interview study had low awareness about the health benefits of HPV vaccination of boys, and some could not see any point in vaccinating boys against a female disease. This indicates that parents have limited awareness of what types of cancers HPV can cause. However, protection against condyloma was specifically mentioned as a reason for vaccinating boys. Some parents were aware of their low knowledge and some were not. Yet, the main reason most parents could see for vaccinating boys was to decrease transmission of the virus. This reason made them positive towards including boys in the vaccination programme despite their low knowledge regarding the serious effects that HPV could have in men. It is also interesting that several parents declared that they would more easily accept vaccination for their sons than for their daughters. The fact that many of the interviewed parents were in favour of a gender-neutral vaccination programme for HPV is encouraging from a public health perspective, since public opinion is of great importance for successful implementation.
Comparison with existing literature
From a public health perspective, there is a societal demand for high vaccine uptake. However, the HPV vaccine uptake in many countries is not satisfactory.9 In Sweden today, 80% of girls in the programme receive the first injection and even fewer receive the second dose.17 According to Elfstrom et al,31 including boys in the programme would speed up the reduction of HPV prevalence and improve the resilience of the programme. The question of whether to include boys in the programme is currently being discussed in Sweden.
Parents in our study generally had low knowledge and awareness regarding HPV-related diseases in men. Even if the interviews were undertaken in 2012–2013, at an early stage of the national vaccination programme, our clinical experience is that the knowledge about HPV, including how it is transmitted, what it can cause and how one can be protected against the virus is still very limited among Swedish parents. This is in line with Perez et al,25 who also found that parents were unaware that HPV vaccine could be given to boys, and they highlight the need for more information. Although some countries recommend HPV vaccination of boys and have implemented gender-neutral vaccination programmes, there is still a knowledge gap regarding this in many countries.22 24 25
Noteworthy in our study is that several parents declared that they would more easily accept the vaccination for their sons than for their daughters. Even parents who had declined HPV vaccination of their daughter expressed they would be willing to vaccinate their son if it was offered. Some parents expressed scepticism towards the female-only vaccination programme and compared it to an experiment on girls. A gender-neutral vaccination was seen as more reliable and safe, which could indicate that making this vaccination gender-neutral could increase the trust in the vaccine and by that also increase vaccine uptake among girls. Trust in vaccine safety and trust in authorities' recommendations are important aspects in a successful vaccination programme.21 37–39 Some parents in our study believed that girls face higher risk of dying from HPV-related disease and that they are more vulnerable to side effects than boys. Vaccine safety is commonly discussed in studies regarding parental attitudes and beliefs about vaccination.22 24 25 40
A vaccine directed only to girls may create curiosity about differences between boys and girls and sexuality. Many parents in our study brought up that male vaccination might be a way to stop the transmission of HPV. This is in line with what was found in a study by Schuler et al,41 where they conclude that efforts to improve vaccine uptake in boys should ‘explore the benefits of highlighting potential female partner protection’, since this was found to be an important aspect for parents with a high intention to vaccinate their son.
As mentioned, there are several reasons for including boys in the HPV vaccination programme. Parents in our study felt that girls always had to take responsibility for sexual and reproductive health issues. In this case, both women and men can suffer from HPV-caused cancer, and it is important to note that cancer related to HPV, such as head and neck cancer, and anal cancer is rapidly increasing, especially among men who have sex with men (MSM).3–5 This could be seen as society having reinforced the traditional notion of women being responsible for sexual and reproductive health. The overall aim of public health is to create good health on equal terms for the entire population. Thus, from a public health perspective, it would be beneficial to also include boys in the vaccination programme. Furthermore, according to principles of justice,36 it could also be considered a moral duty, as discussed by Malmqvist et al42 and Gottvall et al.43 Since both boys and girls can be affected, it is a moral duty to protect both sexes. Furthermore, the findings in our population-based study among the providers, the school nurses, indicate a high level of approval for extending the national HPV vaccination programme to also include boys.20
It needs to be considered that even if a higher vaccine uptake among girls is reached, boys are neither protected on individual level nor on public health level, and a group of males, MSM, would be left unprotected by a female-only programme. Additionally, men who have sex with unvaccinated women from countries with low HPV vaccine uptake are also at risk of HPV infection and HPV-related cancer. It would be beneficial for these vulnerable groups to be included in national health interventions such as vaccination programmes in order to decrease health disparities among the population, which can also be seen as an aspect of justice.36
In conclusion, our study indicates that parents are in favour of including boys in the national school-based HPV vaccination programme, despite low knowledge about HPV infection in men. Authorities need to direct information about the health benefits of HPV vaccination also to parents of young boys to bridge the knowledge gap. More information is necessary to increase HPV vaccination among boys. A vaccine offered only to girls may cause parents to be reluctant to vaccinate, while also including boys in the national vaccination programme might be beneficial to improve parents' trust in the vaccine. This may lead to increased HPV vaccine coverage among both girls and boys eventually and thereby also to a further reduction of the burden of HPV-related disease. Future studies should focus on educational interventions aiming to increase parental knowledge and awareness about HPV as well as transmission, what HPV can cause and how HPV can be prevented by the vaccine among both boys and girls.
Strengths and weaknesses of the study
One strength of the study is that the interviewed parents had very recently made a decision about vaccinating his or her daughter, at the time of the interview. Another strength is that parents who had declined as well as parents who had accepted vaccination for their daughter are represented in the sample. The parents represent a broad variation of different regions and wide variety of levels from urban and rural areas. Furthermore, the interviewers are registered nurses in addition to researchers in the field of HPV, and with experience of conducting interviews. This might have led to a willingness among the participants to share their view on the subject during the interviews. A weakness of this study is that not all of the interviewed parents had a son; therefore, they may have found it difficult to discuss this issue. As in all qualitative research, the aim is not to generalise, which might be seen as a methodological limitation. However, individual face-to-face interviews with 42 parents were considered sufficient in order to reach saturation and to provide a better understanding of the informants' perspective, which is considered an aim in qualitative research. The results may however be transferable to other settings. Moreover, a higher proportion of parents with immigrant backgrounds and with lower educational levels would have been preferable.
Acknowledgments
The authors would like to thank all the participating parents and the heads of the school health in each municipality. They would also like to thank the head of the research group, Professor Tanja Tydén, Uppsala University, for help with funding.
Footnotes
Contributors: MGo conceptualised and designed the study, recruited participants, managed the data collection, completed data analysis and interpretation, wrote the draft manuscript and obtained funding. CS assisted in design, participant recruitment, data collection, data interpretation, manuscript preparation and funding. MGr conceptualised and designed the study, recruited participants, managed the data collection, completed data analysis and interpretation, wrote the draft manuscript and obtained funding. All authors had full access to all of the data in the study and can take responsibility for the integrity of the data and the accuracy of the data analysis.
Funding: This work was supported by the Swedish Cancer Society (grant number 130 744 ) and Uppsala-Örebro Regional Research Council (grant number RFR-387561/476021).
Competing interests: None declared.
Ethics approval: Uppsala University, Department of Public Health and Caring Sciences and the Regional Ethical Committee in Uppsala, Sweden, D.nr. 2012/48 approved this study.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1.Jemal A, Bray F, Center MM et al. Global cancer statistics. CA Cancer J Clin 2011;61:69–90. 10.3322/caac.20107 [DOI] [PubMed] [Google Scholar]
- 2.Forman D, de Martel C, Lacey CJ et al. Global burden of human papillomavirus and related diseases. Vaccine 2012;30(Suppl 5):F12–23. 10.1016/j.vaccine.2012.07.055 [DOI] [PubMed] [Google Scholar]
- 3.Du J, Nordfors C, Ahrlund-Richter A et al. Prevalence of oral human papillomavirus infection among youth, Sweden. Emerg Infect Dis 2012;18:1468–71. 10.3201/eid1809.111731 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chaturvedi AK, Engels EA, Pfeiffer RM et al. Human papillomavirus and rising oropharyngeal cancer incidence in the United States. J Clin Oncol 2011;29:4294–301. 10.1200/JCO.2011.36.4596 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Machalek DA, Grulich AE, Jin F et al. The epidemiology and natural history of anal human papillomavirus infection in men who have sex with men. Sex Health 2012;9:527–37. 10.1071/SH12043 [DOI] [PubMed] [Google Scholar]
- 6.Young D, Xiao CC, Murphy B et al. Increase in head and neck cancer in younger patients due to human papillomavirus (HPV). Oral Oncol 2015;51:727–30. 10.1016/j.oraloncology.2015.03.015 [DOI] [PubMed] [Google Scholar]
- 7.Hong A, Lee CS, Jones D et al. Rising prevalence of human papillomavirus-related oropharyngeal cancer in Australia over the last 2 decades. Head Neck 2016;38:743–50. 10.1002/hed.23942 [DOI] [PubMed] [Google Scholar]
- 8.Chesson HW, Dunne EF, Hariri S et al. The estimated lifetime probability of acquiring human papillomavirus in the United States. Sex Transm Dis 2014;4:660–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bruni L, Diaz M, Barrionuevo-Rosas L et al. Global estimates of human papillomavirus vaccination coverage by region and income level: a pooled analysis. Lancet Glob Health 2016;4:e453–63. 10.1016/S2214-109X(16)30099-7 [DOI] [PubMed] [Google Scholar]
- 10.Markowitz LE, Tsu V, Deeks SL et al. Human papillomavirus vaccine introduction--the first five years. Vaccine 2012;30(Suppl 5):F139–48. 10.1016/j.vaccine.2012.05.039 [DOI] [PubMed] [Google Scholar]
- 11.Arnheim-Dahlstrom L, Pasternak B, Svanstrom H et al. Autoimmune, neurological, and venous thromboembolic adverse events after immunisation of adolescent girls with quadrivalent human papillomavirus vaccine in Denmark and Sweden: cohort study. BMJ 2013;347:f5906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Langer-Gould A, Qian L, Tartof SY et al. Vaccines and the risk of multiple sclerosis and other central nervous system demyelinating diseases. JAMA Neurol 2014;71:1506–13. 10.1001/jamaneurol.2014.2633 [DOI] [PubMed] [Google Scholar]
- 13.European Medicals Agency. EMA to further clarify safety profile of human papillomavirus (HPV) vaccines Secondary European Medicals Agency. EMA to further clarify safety profile of human papillomavirus (HPV) vaccines 2015. http://www.ema.europa.eu/ema/index.jsp?curl=pages/news_and_events/news/2015/07/news_detail_002365.jsp&mid=WC0b01ac058004d5c1 (accessed 12 Jun 2016).
- 14.Herweijer E, Sundstrom K, Ploner A et al. Quadrivalent HPV vaccine effectiveness against high-grade cervical lesions by age at vaccination: a population-based study. Int J Cancer 2016;138:2867–74. 10.1002/ijc.30035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Herweijer E, Leval A, Ploner A et al. Association of varying number of doses of quadrivalent human papillomavirus vaccine with incidence of condyloma . JAMA 2014;311:597–603. 10.1001/jama.2014.95 [DOI] [PubMed] [Google Scholar]
- 16.Ali H, Donovan B, Wand H et al. Genital warts in young Australians five years into national human papillomavirus vaccination programme: national surveillance data. BMJ 2013;346:f2032. [DOI] [PubMed] [Google Scholar]
- 17.Public Health Agency of Sweden. Statistics for HPV vaccinations. Secondary Public Health Agency of Sweden. Statistics for HPV vaccinations 2015. https://www.folkhalsomyndigheten.se/folkhalsorapportering-statistik/statistikdatabaser-och-visualisering/vaccinationsstatistik/statistik-for-hpv-vaccinationer/ (accessed 18 Aug 2016).
- 18.Australian Government Department of Health. Immunise Australia Program. Human Papillomavirus (HPV). Secondary Australian Government Department of Health. Immunise Australia Program. Human Papillomavirus (HPV). 31 May 2016. http://www.health.gov.au/internet/immunise/publishing.nsf/Content/immunise-hpv (accessed 12 Jun 2016).
- 19.Prue G. Vaccinate boys as well as girls against HPV: it works, and it may be cost effective. BMJ 2014;349:g4834. [DOI] [PubMed] [Google Scholar]
- 20.Grandahl M, Tyden T, Rosenblad A et al. School nurses’ attitudes and experiences regarding the human papillomavirus vaccination programme in Sweden: a population-based survey. BMC Public Health 2014;14:540 10.1186/1471-2458-14-540 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gottvall M, Grandahl M, Hoglund AT et al. Trust versus concerns-how parents reason when they accept HPV vaccination for their young daughter. Ups J Med Sci 2013;118:263–70. 10.3109/03009734.2013.809039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lee Mortensen G, Adam M, Idtaleb L. Parental attitudes towards Male human papillomavirus vaccination: a pan-European cross-sectional survey. BMC Public Health 2015;15:624 10.1186/s12889-015-1863-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Perkins RB, Tipton H, Shu E et al. Attitudes toward HPV vaccination among low-income and minority parents of sons: a qualitative analysis. Clin Pediatr (Phila) 2013;52:231–40. 10.1177/0009922812473775 [DOI] [PubMed] [Google Scholar]
- 24.Moss JL, Reiter PL, Brewer NT. HPV vaccine for teen boys: dyadic analysis of parents’ and sons’ beliefs and willingness. Prev Med 2015;78:65–71. 10.1016/j.ypmed.2015.07.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Perez S, Shapiro GK, Brown CA et al. ‘I didn't even know boys could get the vaccine’: parents’ reasons for human papillomavirus (HPV) vaccination decision making for their sons. Psychooncology 2015. 10.1002/pon.3894doi: 10.1002/pon.3894. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 26.Alexander AB, Stupiansky NW, Ott MA et al. Parent-son decision-making about human papillomavirus vaccination: a qualitative analysis. BMC Pediatr 2012;12:192 10.1186/1471-2431-12-192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mattebo M, Grun N, Rosenblad A et al. Sexual experiences in relation to HPV vaccination status in female high school students in Sweden. Eur J Contracept Reprod Health Care 2014;19:86–92. 10.3109/13625187.2013.878021 [DOI] [PubMed] [Google Scholar]
- 28.Lindley MC, Jeyarajah J, Yankey D et al. Comparing human papillomavirus vaccine knowledge and intentions among parents of boys and girls. Hum Vaccin Immunother 2016;12:1519–27. 10.1080/21645515.2016.1157673 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Perez S, Tatar O, Ostini R et al. Extending and validating a human papillomavirus (HPV) knowledge measure in a national sample of Canadian parents of boys. Prev Med 2016;91:43–9. 10.1016/j.ypmed.2016.07.017 [DOI] [PubMed] [Google Scholar]
- 30.Schmeler KM, Sturgis EM. Expanding the benefits of HPV vaccination to boys and men. Lancet 2016;387:1798–9. 10.1016/S0140-6736(16)30314-2 [DOI] [PubMed] [Google Scholar]
- 31.Elfstrom KM, Lazzarato F, Franceschi S et al. Human papillomavirus vaccination of boys and extended catch-up vaccination: effects on the resilience of programs. J Infect Dis 2016;213:199–205. 10.1093/infdis/jiv368 [DOI] [PubMed] [Google Scholar]
- 32.Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care 2007;19:349–57. 10.1093/intqhc/mzm042 [DOI] [PubMed] [Google Scholar]
- 33.Burnard P, Gill P, Stewart K et al. Analysing and presenting qualitative data. Br Dent J 2008;204:429–32. 10.1038/sj.bdj.2008.292 [DOI] [PubMed] [Google Scholar]
- 34.Guba E, Lincoln Y. Fourth generation evaluation. Newbury Park, CA: Sage publications, 1989. [Google Scholar]
- 35.Graneheim UH, Lundman B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today 2004;24:105–12. 10.1016/j.nedt.2003.10.001 [DOI] [PubMed] [Google Scholar]
- 36.Beauchamp T, Childress J. Principles of biomedical ethics. 6th edn Oxford University Press, 2009. [Google Scholar]
- 37.Grandahl M, Oscarsson M, Stenhammar C et al. Not the right time: why parents refuse to let their daughters have the human papillomavirus vaccination. Acta Paediatr 2014;103:436–41. 10.1111/apa.12545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Marlow LA, Waller J, Wardle J. Trust and experience as predictors of HPV vaccine acceptance. Hum Vaccin 2007;3:171–5. [DOI] [PubMed] [Google Scholar]
- 39.Robbins SC, Bernard D, McCaffery K et al. “I just signed”: factors influencing decision-making for school-based HPV vaccination of adolescent girls. Health Psychol 2010;29:618–25. 10.1037/a0021449 [DOI] [PubMed] [Google Scholar]
- 40.Ogilvie G, Anderson M, Marra F et al. A population-based evaluation of a publicly funded, school-based HPV vaccine program in British Columbia, Canada: parental factors associated with HPV vaccine receipt. PLoS Med 2010;7: e1000270 10.1371/journal.pmed.1000270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Schuler CL, DeSousa NS, Coyne-Beasley T. Parents’ decisions about HPV vaccine for sons: the importance of protecting sons’ future female partners. J Community Health 2014;39:842–8. 10.1007/s10900-014-9859-1 [DOI] [PubMed] [Google Scholar]
- 42.Malmqvist E, Natunen K, Lehtinen M et al. Just implementation of human papillomavirus vaccination. J Med Ethics 2012;38:247–9. 10.1136/medethics-2011-100090 [DOI] [PubMed] [Google Scholar]
- 43.Gottvall M, Tyden T, Larsson M et al. Challenges and opportunities of a new HPV immunization program perceptions among Swedish school nurses. Vaccine 2011;29:4576–83. 10.1016/j.vaccine.2011.04.054 [DOI] [PubMed] [Google Scholar]