Abstract
Orthopedic trauma surgery is a critical component of resident education. Surgical case logs obtained from the Accreditation Council of Graduate Medical Students from 2009 to 2013 for orthopedic surgery residents were examined for variability between the 90th and 10th percentiles in regards to the volume of cases performed. There was an upward trend in the mean number of cases performed by senior residents from 484.4 in 2009 to 534.5 in 2013, representing a 10.3% increase. There was a statistically significant increase in the number of cases performed for humerus/elbow, forearm/wrist, and pelvis/hip during this period (P<0.05). Although the difference between the 10th and 90th percentile case volumes narrowed over the study period, the difference between these groups remained significant in 2013 (P=0.02). In 2013, all categories of trauma cases had a greater than 2.2-fold difference between the 10th and 90th percentile of residents for numbers of trauma cases performed. Although case volume is not the sole determinant of residency education and competency, evidence suggests that case volume plays a crucial role in surgeon confidence and efficiency in performing surgery. Further studies are needed to better understand the effect of this variability seen among residents performing orthopedic trauma surgery.
Key words: Variability, Orthopedic trauma surgery, Resident education
Competing interest statement
Conflict of interest: the authors declare no potential conflict of interest.
Introduction
The Accreditation Council of Graduate Medical Students (ACGME) is the responsible organization for accreditation of orthopedic surgery residency training within the United States. Due to the fact that case volume has been identified as an important aspect of surgeon training, the ACGME has implemented an electronic case report system in order to track operative volume of residents from postgraduate year (PGY)-2 to the PGY-5 year.1
In 2014, the ACGME and American Academy of Orthopaedic Surgeons (AAOS) instituted case minimums for specific surgeries over the course of a resident’s training which include 30 hip fractures, 25 femur/tibial shaft fractures, and 15 ankle fractures. Although the effects of case minimum requirements remain unknown, previous evaluation of resident case logs for both spine surgery and arthroscopic surgery have revealed significant variability in the case volume among current orthopedic residents.2-4 Similarly, case logs for general surgery residents performing trauma surgery have been evaluated and have shown a decline in case volume since the introduction of the duty-hour restriction.5
To date, there has been a lack of data specifically analyzing the case volume of residents performing orthopedic trauma surgery in the United States. The purpose of this investigation was to analyze the variability and case volume trends within orthopedic trauma surgery.
Materials and Methods
ACGME surgical case logs from 2009 to 2013 for graduating orthopedic surgery residents were assessed.6 The national averages of orthopedic trauma procedures logged each year were examined with respect to particular categories. These categories include shoulder, humerus/elbow, forearm/wrist, hand/fingers, pelvis/hip, femur/knee, leg/ankle, foot/toes, and total trauma. Trauma in each category was sub-categorized as fracture/dislocation and manipulation. Additionally, the fracture/dislocation procedures of the Spine category were examined. The numbers of procedures from the 10th and 90th resident percentiles were compared. Subsequently, the difference in the number of procedures performed between the 10th and 90th resident percentile were compared from 2009-2013.
Statistical analysis
Linear regression analysis was performed to assess the trend in each surgical subspecialty category. Analysis of variance was performed to assess the statistical significance of these trends. Linear regression analysis was also performed to examine the differences in procedures logged by the bottom and top 10% of graduating residents in 2009 and 2013 in each category. A Student’s was performed to directly compare the case volume between the 10th and 90th percentile in 2013. P<0.05 was set as a cutoff for statistical significance. Statistical analysis was performed using Microsoft Excel (Microsoft, Redmond, WA, USA) and StatPlus:mac LE (AnalystSoft, Walnut, CA, USA).
Results
The number of orthopedic surgery residency programs assessed in the United States ranged from 147-150 with an increase from 635 to 678 residents per year Nationwide from 2009 to 2013 (Table 1). The mean number of total trauma procedures logged per graduating resident in 2009 was 484.4, which increased to 534.5 in 2013, representing a 10.3% increase (P=0.072). The upward trend of procedures per graduating resident from 2009 to 2013 was statistically significant for the humerus/elbow, forearm/wrist, and pelvis/hip (P<0.05) (Table 2). From 2009-2013 the mean number of humerus/elbow cases increased by 5 cases per graduating resident, forearm/wrist by 14 cases per graduating resident, and pelvis/hip by 7 cases per graduating resident. When the case logs were analyzed for specific fracture/dislocation codes, only the pelvis/hip category showed a significant increase over this time period increasing from 69.2 to 75.2 cases/year (P=0.013), whereas utilizing manipulation codes humerus/elbow and forearm/wrist were significantly greater increasing from 7 to 8.9 (P=0.035) and 28.8 to 43.8 (P=0.046) respectively from 2009 to 2013 (Table 2).
Table 1.
Demographics of orthopedic surgery Accreditation Council for Medical Education case log survey respondents.
| Graduating year | Residency programs (n) | Residents (n) |
|---|---|---|
| 2009 | 148 | 635 |
| 2010 | 147 | 653 |
| 2011 | 148 | 650 |
| 2012 | 149 | 675 |
| 2013 | 150 | 678 |
Table 2.
Average number of cases completed by senior residents between 2009-2013.
| Total trauma | 2009 | 2010 | 2011 | 2012 | 2013 | P |
|---|---|---|---|---|---|---|
| Shoulder | 23.6 | 25.2 | 27.8 | 30.2 | 30.1 | 0.064 |
| Humerus/elbow | 54.4 | 55.4 | 57.3 | 59.2 | 59.4 | 0.042* |
| Forearm/wrist | 85.7 | 89.8 | 91.3 | 96.6 | 99.5 | 0.020* |
| Hand/fingers | 32.1 | 33.5 | 36 | 37.7 | 37.4 | 0.097 |
| Pelvis/hip | 77.5 | 77.1 | 79.6 | 83.4 | 84.5 | 0.019* |
| Femur/knee | 74.2 | 73.8 | 73.4 | 75.9 | 74.3 | 0.52 |
| Leg/ankle | 111.6 | 116.1 | 119.1 | 124.8 | 120.6 | 0.32 |
| Foot/toes | 25.2 | 26.1 | 27.9 | 29.5 | 28.7 | 0.17 |
| Spine (fx/dislocate) | 4.5 | 5.6 | 6 | 6.3 | 5.9 | 0.46 |
| Total | 484.4 | 497 | 512.5 | 537.3 | 534.5 | 0.072 |
| Fracture/dislocation | ||||||
| Shoulder | 18.3 | 19.5 | 21.7 | 23.7 | 23.9 | 0.046 |
| Humerus/elbow | 47.4 | 47.1 | 48.9 | 50.5 | 50.4 | 0.069 |
| Forearm/wrist | 56.9 | 55.6 | 56.5 | 58 | 55.7 | 0.79 |
| Hand/fingers | 26 | 25.9 | 27.4 | 28.6 | 28.4 | 0.090 |
| Pelvis/hip | 69.8 | 68.7 | 70.8 | 74 | 75.2 | 0.013* |
| Femur/knee | 64.1 | 62.1 | 61.9 | 63.7 | 61.6 | 0.96 |
| Leg/ankle | 97.5 | 97 | 99.3 | 103.1 | 98.9 | 0.52 |
| Foot/toes | 23.3 | 23.8 | 25.3 | 26.6 | 25.8 | 0.20 |
| Manipulation | ||||||
| Shoulder | 5.3 | 5.7 | 6.1 | 6.5 | 6.2 | 0.26 |
| Humerus/elbow | 7 | 8.3 | 8.4 | 8.8 | 8.9 | 0.035* |
| Forearm/wrist | 28.8 | 34.2 | 34.8 | 38.7 | 43.8 | 0.046* |
| Hand/fingers | 6.1 | 7.6 | 8.6 | 9 | 9 | 0.10 |
| Pelvis/hip | 7.7 | 8.4 | 8.8 | 9.3 | 9.3 | 0.052 |
| Femur/knee | 10.1 | 11.6 | 11.6 | 12.2 | 12.7 | 0.053 |
| Leg/ankle | 14.2 | 19.1 | 19.8 | 21.7 | 21.7 | 0.059 |
| Foot/toes | 1.9 | 2.3 | 2.6 | 2.9 | 2.9 | 0.056 |
*Analysis of variance analysis of trends.
The difference between the 10th and 90th percentile of resident case logs trended downward over time in the majority of trauma categories from 2009 to 2013 (Figure 1); however, these downward trends were not found to be statistically significant, except for in humerus/elbow with a decrease from 3.6-fold to 2.8-fold (P=0.013) and forearm/wrist from 4.1-fold to 2.9-fold when comparing the 10th to 90th percentiles (P=0.011) (Table 3, Figure 2).
Figure 1.
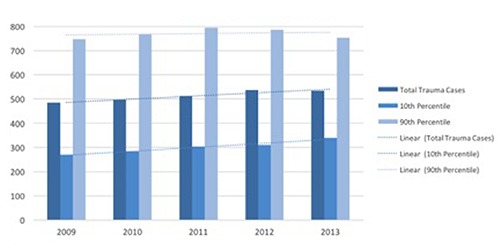
Volume of cases reported from 2009-2013, comparing the average number of total trauma cases, the 90th percentile of case reported, and the 10th percentile of cases reported.
Table 3.
Percent differences between the 10th and 90th percentile of orthopedic residents.
| Fold-difference | 2009 | 2010 | 2011 | 2012 | 2013 | P |
|---|---|---|---|---|---|---|
| Shoulder | 4.7 | 4.6 | 4.2 | 4.5 | 3.9 | 0.29 |
| Humerus/elbow | 3.6 | 3.5 | 3.3 | 2.9 | 2.8 | 0.013* |
| Forearm/wrist | 4.1 | 4.1 | 3.6 | 3.4 | 2.9 | 0.011* |
| Hand/fingers | 5.4 | 5.5 | 5.6 | 5.2 | 5.8 | 0.84 |
| Pelvis/hip | 3.2 | 3.3 | 3.4 | 3.1 | 2.6 | 0.13 |
| Femur/knee | 3.1 | 2.9 | 3.1 | 2.8 | 2.5 | 0.24 |
| Leg/ankle | 2.9 | 2.7 | 2.7 | 2.7 | 2.6 | 0.24 |
| Foot/toes | 5.5 | 5.3 | 5.9 | 5.3 | 5.2 | 0.59 |
| Total | 2.8 | 2.7 | 2.6 | 2.5 | 2.2 | 0.062 |
*Analysis of variance analysis of trends with statistically significance.
Figure 2.
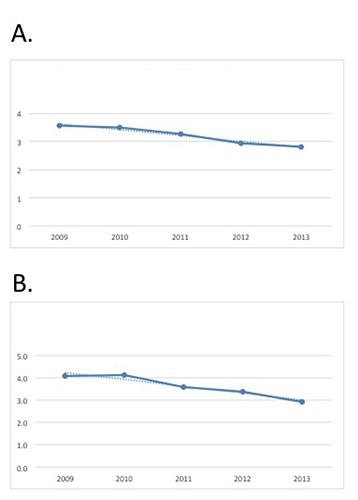
Graphic representation of the statistically significant decrease in the fold-difference from 2009-2013 for humerus/elbow (A) and forearm/wrist (B).
Overall, the difference between the 10th and 90th percentile residents in trauma cases decreased from 2.8-fold to 2.2-fold between over this 5 year period, but was not significant from 2009-2013 (P=0.062). Although the fold-difference between the 10th and 90th percentile narrowed over time, the difference between these groups remained significant in 2013 (P=0.02). In 2013, all categories of trauma had a greater than 2.2-fold difference between the 10% percentile and 90% percentile in cases performed, ranging from 2.2 to 5.8, with the greatest difference being in cases logged under hand/fingers (5.8-fold difference). Shoulder procedures had the next largest difference with 3.9 times more cases performed for 90th percentile residents compared to the 10th percentile residents.
Discussion
The implementation of the ACGME case log system was designed to allow for an objective record of the operative volume of orthopedic surgery residents as they progressed through their training.1 Although resident training consists of didactic education, preoperative and postoperative patient care, non-operative care and educational courses, repetitive surgical experience in the operating room continues to be essential.2,7,8 When analyzing self reported surveys of case volume and the objective ACGME case log data of general surgery residents, it was found that increasing surgical volume correlates with resident comfort level in the operating room.9 Therefore the more experience a resident can obtain in a given procedure or subspecialty, the more comfortable and knowledgeable the resident will be with the intricacies of the case when he or she encounters it in independent practice.
In 2012, the United Kingdom and Ireland reported data from a similar case log system, Orthopedic eLogbook, and found that orthopedic residents in the middle years of specialty training (Years 3-8) performed an average of 643 orthopedic cases.10 The results of this investigation reveal that although there has been a significant increase in upper extremity trauma and pelvic trauma reported by residents over a 5-year period, a substantial variability in resident case volume in orthopedic trauma still exists. The variability that was observed between the 10th percentile and 90th percentile is the most concerning from a resident training standpoint. There was a greater than 2-fold difference between these groups in regards to overall trauma cases reported and when analyzed in regards to subspecialty, the most remarkable difference was a 5.8 fold difference in case volume of hand/finger cases. This variability within the subspecialties is concerning because the residents from the lower percentile of case volume may be receiving a suboptimal number of cases. As orthopedic surgery training transition from an apprenticeship model towards proficiency based approach, further research needs to be done to analyze why such discrepancies in case volumes exist.11 One possibility is that as residents decide on their individual pathway towards fellowship within a specific area of expertise, they are concentrating their efforts in these areas and paying less attention to other areas of training.
The American Board of Orthopaedic Surgery (ABOS) and the Residency Review Committee for Orthopaedic Surgery (RRC) seeks to make training of orthopedic residents more objective and uniform.11 As these governing bodies in orthopedic education strive to fulfill these objectives, they will have to better understand why such a significant gap in training exists between programs. More importantly, they will have to create a way for training to be more uniform. In 2013-2014, The ABOS and RRC began to require that orthopedic surgery programs begin to implement a laboratory-based surgical skills simulation training program.12
Surgical simulation has been identified as an education tool that may help training deficiencies associated with the apprenticeship training model by allowing trainees to practice a technique or procedure until competency is achieved.11 This allows residents to prepare efficiently and safely hone their skills while minimizing risk to patients. Karam et al. identified deficiencies in fracture simulation, which prompted them to create a articular fracture reduction simulation training program.11 They chose to create an articular fracture model of a tibial plafond injury because they recognized that the first time an orthopedic resident has to overcome the challenges of articular fracture management is in the operating room. They also recognized the patient morbidity of inadequate articular fracture reduction and fixation. In pilot testing, they found that senior residents had more deliberate hand motions and more accurate fragment reduction than junior residents.
Leong et al. created and attempted to validate three fracture fixation models including application of a dynamic compression place, insertion of tibial intramedullary nail, and application of a forearm fixation.13 Three groups of participants (i.e. novice, intermediate and expert) were recorded performing the three tasks and two experts using a standardized global rating scale graded the videos. They demonstrated that the three groups had significantly different video scores corresponding to the skill level of the group. Simulation models in orthopedic trauma may be the solution for reduced case volume because if residents are trained to become proficient on these models, then it may enhance their operating room training.
While the ACGME has set minimum requirements for resident training for hip fractures, femur and tibia fractures, ankle fractures, and supracondylar pediatric fractures, there are no minimums set for many of the categories of orthopaedic trauma surgery.14 Although case logs are a useful tool to track a resident’s progress through training, a trainees ability cannot be solely interpreted on the number of cases performed.15 The case numbers assigned as minimums by the ACGME are arbitrary and little data support when a resident is capable or comfortable performing a particular case on their own. However, variability in reported case volume suggests that surgical simulators and surgical laboratories may need to be used to address a resident’s lack of case volume. Karam et al.11 found that both attending physicians and residents agreed that surgical skill simulation should be a required part of training and both groups favored the implementation of a standardized surgical skills curriculum. Program directors and residents agree that more time should be spent in the operating room and outside the operating room focusing on surgical skills than doing clerical work.16 Further investigation is needed to reveal if surgical simulation can close the gap between resident ability between residents performing the greatest and least amount of cases. There are several potential limitations of this investigation. First, the accuracy of the ACGME case log data has been scrutinized. Residents may under-report or over-report case numbers which would alter the true exposure based on how accurately residents reported their cases.1 Some of the variability seen in this study may also arise from the underreporting of CPT codes by residents compared to physicians. In many surgical cases, multiple CPT codes are reported based on the number of billable components and residents who have less experience with CPT coding structure may underreport some of these cases, which in turn would decrease their overall case volume. However, ACGME resident case logs are currently utilized by both the ACGME and individual institutions to track resident case exposure, and are currently the best data available for examining resident case volume. Furthermore, there is no way to assess the level of resident participation within a given case, as this can vary from case to case depending on several factors including experience, surgeon, and complexity. The ACGME also does not provide additional information on the specifics of the case logs in regards to region, program size, patient population, or residency demographics therefore no analysis could be performed. Lastly, there is no way to determine if the difference between the 10th and 90th percentiles actually equates to significant differences in surgical skills among residents.
Conclusions
This study examined ACGME case logs for orthopedic surgery residents and found that trauma cases have increased by 10% from 2009 to 2013. However, the large variability in cases between the 10th and 90th percentile of orthopedic residents remains a substantial concern. Although surgical case volume is not the sole determinant of resident competency, evidence suggests that case volume does play a fundamental role in surgeon confidence and efficiency in performing surgery. Further studies are needed to better understand the effect of this variability seen among residents performing orthopedic trauma surgery and to evaluate if changes in case volume have occurred following implementation of case minimums by the ACGME.
References
- 1.Salazar D, Schiff A, Mitchell E, Hopkinson W. Variability in accreditation council for graduate medical education resident case log system practices among orthopaedic surgery residents. J Bone Joint Surg Am 2014;96:e22. [DOI] [PubMed] [Google Scholar]
- 2.Daniels AH, Ames CP, Smith JS, Hart RA. Variability in spine surgery procedures performed during orthopaedic and neurological surgery residency training: an analysis of ACGME case log data. J Bone Joint Surg Am 2014;96:e196. [DOI] [PubMed] [Google Scholar]
- 3.Hinds RM, Gottschalk MB, Strauss EJ, Capo JT. Trends in arthroscopic procedures performed during orthopaedic residency: an analysis of accreditation council for graduate medical education case log data. Arthrosc J Arthrosc Relat Surg 2016;32:645-50. [DOI] [PubMed] [Google Scholar]
- 4.Hinds RM, Gottschalk MB, Capo JT. National trends in carpal tunnel release and hand fracture procedures performed during orthopaedic residency: an analysis of ACGME case logs. J Grad Med Educ 2016;8:63-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Drake FT, Van Eaton EG, Huntington CR, et al. ACGME case logs: surgery resident experience in operative trauma for two decades. J Trauma Acute Care Surg 2012;73:1500-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Accreditation Council for Graduate Medical Education. Orthopaedic surgery case logs: national data report. Available from: http://www.acgme.org/Portals/0/PDFs/ORSNatData0910.pdf
- 7.Hinds RM, Gottschalk MB, Capo JT. National trends in carpal tunnel release and hand fracture procedures performed during orthopaedic residency: an analysis of ACGME case logs. J Grad Med Educ 2015;8:63-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gil JA. Variability in surgical case volume of orthopaedic surgery residents 2007 to 2013. J Am Acad Orthop Surg 2016;24:207. [DOI] [PubMed] [Google Scholar]
- 9.Suwanabol PA, McDonald R, Foley E, Weber SM. Is surgical resident comfort level associated with experience? J Surg Res 2009;156:240-4. [DOI] [PubMed] [Google Scholar]
- 10.Jameson SS, Gupta S, Lamb A, et al. The United Kingdom and Ireland trauma & orthopaedic elogbook: an evidence base for enhancing training. Surgeon 2012;10:249-56. [DOI] [PubMed] [Google Scholar]
- 11.Karam MD, Pedowitz RA, Natividad H, et al. Current and future use of surgical skills training laboratories in orthopaedic resident education: a national survey. J Bone Jt Surg 2013;95: e4. [DOI] [PubMed] [Google Scholar]
- 12.McKee J. “Rebooting” orthopaedic resident education. Rosemont, IL, USA: American Academy of Orthopaedic Surgeons; 2014. [Google Scholar]
- 13.Leong JJH, Leff DR, Das A, et al. Validation of orthopaedic bench models for trauma surgery. J Bone Joint Surg Br 2008;90:958-65. [DOI] [PubMed] [Google Scholar]
- 14.Accreditation Council for Medical Education. Orthopaedic surgery minimum numbers. Chicago, IL: Accreditation Council for Medical Education; 2014. Available from: www.acgme.org/LinkClick.aspx?link=PFAssets%2fProgramResources%2f260_ORS_Case_Log_Minimum_Numbers.pdf&articleId=1157 [Google Scholar]
- 15.Jeray KJ, Frick SL. A survey of resident perspectives on surgical case minimums and the impact on milestones, graduation, credentialing, and preparation for practice: AOA critical issues. J Bone Joint Surg Am 2014;96:e195. [DOI] [PubMed] [Google Scholar]
- 16.Camp CL, Martin JR, Karam MD, et al. Orthopaedic surgery residents and program directors agree on how time is currently spent in training and targets for improvement. Clin Orthop 2016; 474:915-25. [DOI] [PMC free article] [PubMed] [Google Scholar]


