Abstract
Fracture sequelae of the proximal humerus poses a complex management decision due to the frequent deformity and its consequences on the peri-articular soft tissues. These patients are frequently elderly with significant medical comorbidities. Due to the age of the patient there is frequently rotator cuff deficiency and therefore the reverse shoulder arthroplasty (RSA) becomes the arthroplasty of choice. We have performed a systematic review of the literature and report nine studies presenting RSA for the treatment of fracture sequelae of the proximal humerus. It is clear that RSA can improve the range of movement and function following proximal humerus fracture sequelae. However, there is a risk of significant complications including dislocation (16.7%), infection (6.7%), intra-operative fracture (3%) and neurological injury (2.6%). There is a need to invest in future prospective comparative studies and randomised trials to further test RSA in fracture sequelae patients. This will provide us with information regarding the longevity of different prosthesis, outcomes and cost-effectiveness of treatment.
Key words: RSA, Fracture sequelae, Humeral fracture
Competing interest statement
Conflict of interest: the authors declare no potential conflict in interest.
Introduction
Proximal humerus fractures are the third most common fracture in patients over 65 years after wrist and femoral neck fractures.1 The incidence of proximal humerus fractures rapidly increases with age with women being affected twice as frequently as men.2 This is most likely to be due to the increasing risk of osteoporosis with age and female sex.2-4 A prospective study over a twenty-eight year period by Kannus et al. showed an increase in proximal humerus fractures by 15% per year in patients over the age of sixty, highlighting age as a risk factor.5 Palvanen et al. estimated that the number of shoulder fractures to increase three fold in the next 30 years largely due to the increase in the elderly population.6
Management of these fractures in older patients can be difficult due to a variety of fracture patterns, coexisting rotator cuff pathology and associated arthrosis. Osteoporosis increases the complexity of the fracture configuration and is a reported risk factor for non-union.2,7 The poor bone quality in the elderly can also challenge the reduction of the fracture and ability to achieve stable fixation.5
Patients who develop non-union or malunion typically report pain, stiffness, and disability associated with shoulder dysfunction.8 Arthroplasty is a treatment option for reconstruction in this age group. The decision to perform unconstrained arthroplasty (hemiarthroplasty, total shoulder arthroplasty) is dependent on the degree of osteopenia, the viability of the humeral head, tuberosity integrity and the functional status of the rotator cuff.9 Total shoulder replacement is considered in the setting of concomitant glenohumeral arthritis with a functional rotator cuff. Reverse shoulder arthroplasty (RSA) is a treatment option in proximal humerus nonunion or malunion with humeral head collapse and/or a non-functioning rotator cuff.10 Few studies in the literature focus on RSA for proximal humerus non-union and established fracture sequelae.
Aims
Our aim is to perform a systematic review of the literature where RSA has been used following non-union and established fracture sequelae and review the key issues including the procedure, functional and reported outcomes as well as risk and complications experienced.
Literature search strategy
The literature review was conducted using the PubMed, Cochrane library database and Medline OVID database. The PRISMA 2009 checklist was followed for assessment of systematic reviews. Inclusion criteria included all studies using reverse shoulder arthroplasty to manage established proximal humerus fracture sequelae written in English between 2001 and July 2016. The search criteria used the following search terms; Reverse shoulder arthroplasty, RSA, fracture sequelae, proximal humerus non-union and proximal humerus mal-union. All articles were screened for eligibility by two independent authors (JH and TY). Articles focusing solely on the management of proximal humeral nonunion using hemiarthroplasty, total shoulder arthroplasty, anatomic shoulder arthroplasty or rotator cuff impingement following proximal humeral fracture were excluded. Articles with less than five patients were also excluded from the search.
Data extraction and statistical analysis
Data was extracted from each of the selected articles. This focused on the type of study, number of patients in the study, age of the participants, follow up, the prosthesis, surgical approach, outcome and scoring methods used. Where possible we collected data related to the functional assessment of the individuals in the study including abduction, forward flexion, internal and external rotation, the primary outcome score used and documented any complications that were reported. The mean/median and range were provided where possible as well as P values. All statistical analysis was performed using IBM SPSS Statistics Version 22 (IBM SPSS Statistics for MAC, Version 22., IBM Corp., Armonk, NY, USA). Assessment of normally distributed data was performed using means.
Study identification
Two authors (JH and TY) reviewed the title and abstract from each study from the results list independently. Any disagreement was resolved by discussion with the senior author. Full text papers of relevant studies were subsequently obtained and reviewed against the eligibility criteria (Figure 1).
Figure 1.
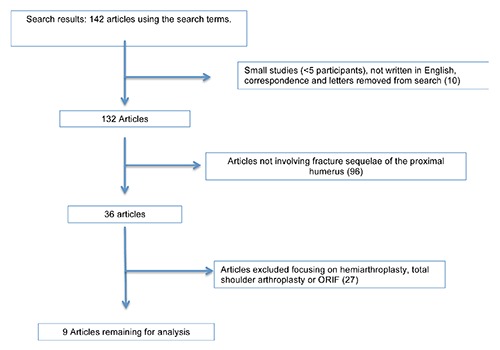
Flow diagram to represent the search process.
Critical appraisal
Two authors using the Critical Appraisal Skills Program checklist independently appraised eligible studies. For the purpose of narrative review, relevant studies were included irrespective of methodology or level of evidence.
Risk of bias
A summary of the articles reviewed is present in Table 1. Each article was reviewed for its risk of bias. In 2007 Willis et al. had a small study (16 patients), which was a single surgeon series.11 There was some alteration of the surgical technique for the prosthesis in that retroversion of the humeral components was greater than 30 degrees to accommodate the boney deformity. Although not a true bias it may influence the longevity of the implant and may have contributed to the two reported accounts of radiological loosening.
Table 1.
| Study | Willis et al.11 | Kilic et al.12 | Wall et al.15 | Raiss et al.13 | Hattrup et al.17 | Martinez et al.18 | Zafra et al.16 | Hussey et al.20 | Raiss et al.14 |
|---|---|---|---|---|---|---|---|---|---|
| Type | Retrospective | Retrospective | Retrospective | Retrospective | Retrospective | Retrospective | Prospective | Prospective | Retrospective |
| Case series | Single surgeon | Many surgeons | 2 surgeons | Multicentre, many surgeons | Multicentre, many surgeons | Not stated | 3 surgeons | Single surgeon + center | Multicentre, many surgeons |
| Patients (n) | 16 | 19 | 33 | 32 | 20 | 18 | 35 | 19 | 42 |
| Mean age, years (range) | 65 (52-83) | 70.1 (60-81) | 75.3 (26-86) | 68 (48-83) | 67 (31-89) | 78.8 (75-84) | 69 (46-83) | 66 (52-82) | 68 (27-83) (median 70 years) |
| Mean follow up, months (range) | 37 (24-62) | 18.3 (8-56) | 42 (24-97) | 48 (24-144) | 44 (27-97) | 28 (24-32) | 51 (24-99) | 36 (25-60) | 48(4) (2-13) (median 3.5 years) |
| Pathology | FS | FS | FS | FS | FS | FS | FS | FS | FS |
| Prosthesis used | RSA (delta III) | RSA (delta III) | RSA (delta III in 209/aequalis system in 31) | RSA aequalis 26/delta 6 | Delta 9, delta Xtend 7, biomet comprehensive 6, zimmer trabecular metal 4 | Lima | Delta III | DJO surgical reverse shoulder prosthesis (RSP) | Aequalis reversed shoulder system for 37 patients, delta in 5 cases |
| Surgical approach | Delto-pectoral approach | Delto-pectoral approach | Delto-pectoral approach | Delto-pectoral approach | Delto-pectoral approach | Delto-pectoral approach | Delto-pectoral approach | Delto-pectoral approach | Delto-pectoral approach |
| Primary clinical scores | ASES | Constant score | Constant score | Constant score | ASES | Constant score | Constant score | VAS, ASES, SST | Constant score |
| Other outcome measures | VAS, simple shoulder test complications, radiological assessment, satisfaction score | Complications | Complications Radiological | Radiological Complications | Neer score, simple shoulder test complications | Complications | Radiological Complications | Radiological Complications | Radiological Complications |
FS, fracture sequelae; RSA, reverse shoulder arthroplasty; DJO, DJO Global, Vista, CA, USA; RSP, reverse shoulder prosthesis; ASES, American shoulder and elbow surgeons score; VAS, visual analogue score; SST, simple shoulder test.
Kilic et al. reviewed 55 patients but only 19 received RSA with the other receiving anatomic prosthesis.12 The main bias being that RSA was only used for fracture sequelae types 3 and 4 whereas anatomic prosthesis was used in types 1 and 2. Conclusions were then made that anatomic prosthesis were better for types 1 and 2 fractures and RSA for 3 and 4 although they were not directly comparable.
Raiss et al. reviewed 32 patients with RSA for fracture sequelae.13 The study has disclosed that one or more of the authors received payments or services either directly or indirectly from a third party and at least one author had a financial relationship prior to submission of the work. Although the disclosure is clear, the risk of bias exists. Raiss et al. also declared royalties and one author received stock options for this study.14 One or more of the authors had a financial relationship or activities that could be perceived to influence the study. The article by Wall et al. used two different RSA brands and had not accounted for this in the analysis.15 Zafra et al., Kilic et al., Raiss et al. and Hattrup et al. are all multi-surgeon and multi-centre studies which can have bias to surgery, rehabilitation and follow up.12-14,16,17 Indeed this does highlight that RSA is a relatively infrequent procedure and often requires multi-centre data to account for a modest study number. Martinez et al did not provide information regarding the surgeon or study centre, which may be of interest given the high rate of complications (27.7% overall complication rate).18
The retrospective nature of the studies (except Zafra et al., which was prospective) also causes an inbuilt element of bias and a threat to validity of the data due to the lack of comparison or control group.19
Literature review results
All reviewed articles were case series (level 4 evidence) (Table 1). In total there were 234 patients included across 9 studies, all for fracture sequelae. The mean age across the reviewed articles was 69.7 years with a mean follow up time of 39 months. A delto-pectoral approach was used in all cases.
Patient outcomes for all the reviewed articles are shown in Table 2. From the literature review all studies reported an improvement in forward flexion from pre-operative scores and were statistically significant with a mean change of 38-71 degrees (Figure 2). Abduction was recorded in five of the nine studies with modest but statistically significant improvement from pre-operative scores of between 50 and 57.3 degrees. External rotation improved in each of the studies ranged between 2 and 39 degrees with only the results from Wall et al. not being statistically significant (Figure 3).15 Internal rotation was recorded in five of the seven studies and had variable success post operatively. Constant score was used as a scoring system in six of the nine studies and showed a statistically significant improvement following surgery with RSA with a mean change in score ranging from 29-42.5. The American Shoulder and Elbow surgeons Shoulder score (ASES) was used in the remaining three studies although the study by Hattrup et al. had incomplete pre and post operative ASES.17 The studies by Hussey et al. and Willis et al. had post operative changes (mean) in ASES of 22.3 and 35 respectively.11,20
Table 2.
Comparing the average range of movement, outcome score and complications across the literature review.11-18,20
| Study | Willis et al.11 | Kilic et al.12 | Wall et al.15 | Raiss et al.13 | Hattrup et al.17 | Martinez et al.18 | Zafra et al.16 | Hussey et al.20 | Raiss et al.14 |
|---|---|---|---|---|---|---|---|---|---|
| Abduction pre-post operation (degrees) | Pre: 48 Post: 105 (mean) (P=0.002) (P<0.001) |
Pre: 36.4 Post: 86.4 (median) (P<0.001) |
Not tested Not tested |
Not tested Not tested |
Not tested Not tested |
Pre: 35 Post: 85 (mean) (P<0.0001) |
Pre: 38.8 (Post: 96.1 (mean) (P<0.0001) |
Pre: 58.7 Post: 89.1 (mean) (P=0.012) |
Not tested Not tested |
| Forward flexion (degrees) | Pre: 53 Post: 105 (mean) (P=0.002) |
Pre: 41 Post: 91 (median) (P<0.001) |
Pre: 77 Post: 115 (mean) (P<0.001) |
Pre: 43 Post: 110 (mean) (P<0.001) |
Pre: 41 Post: 137 (mean) (P<0.001) |
Pre: 35 Post: 90 (mean) (P<0.0001) |
Pre: 45.4 Post: 116.7 (mean) (P<0.001) |
Pre: 58.7 Post: 101.1 (mean) (P=0.001) |
Pre: 53.6 Post: 120.5 (mean) (P<0.0001) |
| Average external rotation pre-post operation (degrees) |
Pre: 5 (mean) Post: 30 (mean)(P=0.015) |
Pre: 1.5 (median) Post: 6.1(median) (P<0.001) |
Pre: 4 at 0 degrees 22 at 90 degrees (mean) Post: 6 at 0 degrees 35 at 90 degrees (mean) |
Pre: 0.5 (mean) Post: 13.1 (mean)(P<0.005) |
Pre: 0 (mean) Post: 39 (mean) (P=0.0002) |
Pre: 15 (mean) Post: 30 (mean) (P<0.0001) |
Pre :4.55 (mean) Post: 15.5 (mean) (P<0.001) |
Pre: 10.7 (mean) Post: 23.1 (mean) (P=0.043) |
Pre: -5.4 (mean) Post: 8.5 (mean) |
| Internal rotation | Pre: S1 Post: L3 (mean) (P=0.015) |
Not tested Not tested |
Pre: sacrum Post: L4 (mean) |
Pre: 2 Post: 6 (buttock to waist) (mean) (P<0.0001) |
Not tested | Pre: 25 Post: 55 (mean) (P<0.0001) |
Pre: 1 Post: 1 (median) (P=0.1796) |
Pre: 1.5 Post: 2.6 (mean) (change in vertebral levels) |
Pre: 3.1 Post: 4.0 (mean) (change in vertebral levels) |
| Outcome score | ASES pre: 28 (mean) |
Constant score (median) pre: 9 |
Constant score (mean) pre:19.7 |
Constant score pre: 14.1 |
ASES pre: -/ASES post: 65 (mean) |
Constant score pre: 26 (mean) |
Constant score pre: 23 (mean) |
ASES: 27.8 VAS: 6.8 SST: 0.7 (mean) |
Constant score pre:19.7 |
| ASES post: 63 (mean) (P=0.001) |
Constant score (median) post: 47.5 (P<0.001) |
Constant score (mean) post: 53 |
Constant score post: 46.6 (P<0.001) |
SST: 6 post operation (mean) |
Constant score post: 55 (mean) (P<0.0001) |
Constant score post: 65.5 (mean) (P<0.001) |
ASES: 50.1 (0.019), VAS: 4.3 (P=0.012) SST: 3.2 (P=0.020) |
Constant score post: 54.9 (P<0.001) |
|
| Complications | 2 radiological pieces of evidence of loosening (not clinical signs) =12.5% | Overall complication rate 36% =1xacromion fracture, 5x infection, 4xhaematoma needing surgery, 1xneuropraxia, 3 luxations, 2 disconnection of components | 19.1% including 8 revisions, 15 dislocations, 8 infections, nerve palsy, loosening and fractures Note not specific to fracture sequelae | Overall complication rate of 41% =11 dislocations, 2 infections | Overall complication rate of 25% =1 deep infection, 2 transient brachial plexopathies, 2 dislocations | Overall complication rate of 27.7% =1 axillary neuropathy, 2 dislocation, 2 infections | Overall complication rate of 20% =6 dislocations, 1 axillary nerve palsy | Overall complication rate of 26%-2x humeral loosening, 4x periprosthetic fracture, 1 x intra-op fracture, 1x radial nerve palsy | Overall complication rate of 9.5%-1x humeral shaft fracture, 1x infection, 1x dislocation, 1x aseptic loosening |
ASES, American shoulder and elbow surgeons score; VAS, visual analogue score; SST, simple shoulder test.
Figure 2.
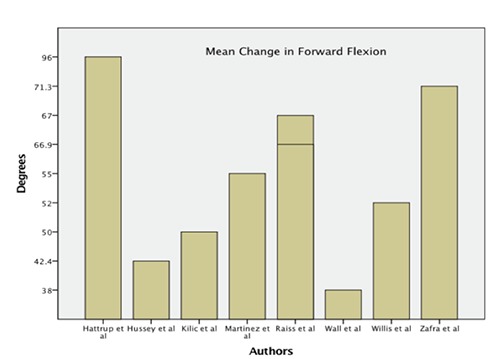
Mean change in forward flexion (in degrees) among the studies.
Figure 3.
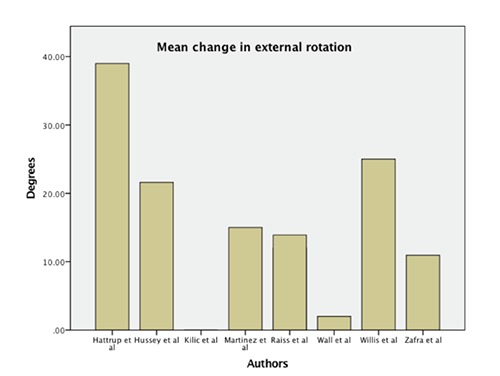
Mean change in external rotation (in degrees) among the studies.
The most frequently observed complication was dislocation at 16.7% (39/234) and infection 6.8% (16/234). There was an overall 3% (7/234) risk of fracture. Nerve injury, ranging from neuropraxia to a plexopathy, occurred in 2.6% (6/234).
Forest plots and tests of heterogenicity were not produced due to the retrospective nature of the studies and only the studies by Raiss et al. and Zafra et al. provided information regarding the mean and standard deviation.14,16 Without this information and the standard error or confidence intervals could not be calculated.
Discussion
Our literature review identified nine eligible studies reporting the management of fracture sequelae of the proximal humerus with RSA. All studies were retrospective with the exception of Zafra et al. which was prospective.16 We reviewed baseline demographics, surgical procedure and outcomes for each study.
All papers reported statistically significant improvement of forward flexion resulting from the anterior deltoid function. Also, all studies showed statistically significant improvement in abduction with reverse geometry prosthesis. Willis et al. attributed this to the use of a lateral-offset prosthesis whereby lateralization of the glenosphere improves deltoid action and working length.11 This lateralization also allows for increased retroversion of the humeral stem without impingement and facilitates external rotation.11 Our review of the literature found improvement in external rotation in all studies with only the study by Wall et al. not reaching statistical significance.15
Internal rotation improved in six of the seven studies that reported post-operative internal rotation. The varied measurement of degrees and associated improvement in spinal level made comparison difficult. After reviewing the operative methodology for the selected studies it was apparent that in some cases repair of the subscapularis and indeed the tuberosities was not always possible. This clearly would affect rotator cuff function and in particular external and internal rotation. The approaches used may also affect post-operative function. In our reviewed cases the delto-pectoral approach was used. This approach places the anterior deltoid fibres at risk from devascularisation thereby affecting its ability to act as an internal rotator once the glenosphere has been lateralized. An alternative approach would be to use the antero-superior Neviaser-MacKenzie or a modified deltopectoral approach as described by Levy et al. to try and preserve anterior deltoid function by reducing the risk of devascularisation.21 The Constant score is a validated shoulder score as was used by six studies all reporting a statistically significant improvement from pre-operative scores. This tool has been shown to be reliable for detecting improvement after intervention in a variety of shoulder pathologies.22 The American Shoulder and Elbow Surgeons Score (ASES) is a functional score that was used by Willis et al., Hattrup et al. and Hussey et al..11,17,20 This has been shown to be a reliable, valid and responsive outcome tool in patients with shoulder dysfunction. Unfortunately, the study by Hattrup et al. only provided post-operative results although the Willis et al. and Hussey et al. studies both showed statistically significant improvements in the ASES.11,17,20
Of the 234 patients reviewed across 9 studies the most frequently reported complications were dislocation 16.7% (39/234) and infection 6.8% (16/234). There was an overall risk of fracture of 3% (7/234) and nerve injury, ranging from neuropraxia to a plexopathy of 2.6% (6/234).
This clearly raises concerns as an RSA for fracture sequelae provides opportunity of functional benefits with impressive outcomes but with risk of significant complications. In order to reduce dislocation rates patient education and counselling is important pre-operatively and post-operatively in order for them to understand the operation and the precautions needed to prevent dislocation. The development and recent publication of the PROFHER trial may influence the management of 3- and 4-part humeral fractures.23 This multicenter randomized trial comparing surgical fixation vs conservative therapy found no significant difference in patient related outcome scores, complications or need for further surgical intervention. The conclusion was that a more conservative approach should be favoured.23
There is conflicting evidence in the literature with Iyenger et al. that reported that 3- and 4-part humeral fractures had complication rates of 48% and malunion in 23%.24 This is particularly interesting as the PROFHER trial was hailed as a landmark paper by the British Orthopaedic Trainees Association (BOTA). This may lead to a trend to conservative management and may lead to increased rates of fracture sequelae in proximal humerus fractures.
Conclusions
Despite the limitations and complications reported in the literature, RSA can improve the range of movement and function following proximal humerus fracture sequelae. This is a complex group of patients who pose a challenge to the surgeon. We recommend that surgery be provided in centers that provide a regular RSA service and encounter fracture sequelae of the proximal humerus on a regular basis. This study justifies investing in future prospective comparative studies and randomized trials to further test RSA in fracture sequelae patients. This will provide us with information regarding the life span of different prosthesis, outcomes and cost-effectiveness of treatment.
References
- 1.Cooper C, Campion G, Melton LJ., 3rd Hip fractures in the elderly: a worldwide projection. Osteoporos Int J Establ 1992;2:285-9. [DOI] [PubMed] [Google Scholar]
- 2.Handoll HH, Ollivere BJ. Interventions for treating proximal humeral fractures in adults. Cochrane Database Syst Rev 2012;12:CD000434. [DOI] [PubMed] [Google Scholar]
- 3.Gaebler C, McQueen MM, Court-Brown CM. Minimally displaced proximal humeral fractures: epidemiology and outcome in 507 cases. Acta Orthop Scand 2003;74:580-5. [DOI] [PubMed] [Google Scholar]
- 4.Tingart MJ, Bouxsein ML, Zurakowski D, et al. Three-dimensional distribution of bone density in the proximal humerus. Calcif Tissue Int 2003;73: 531-6. [DOI] [PubMed] [Google Scholar]
- 5.Kannus P, Palvanen M, Niemi S, et al. Osteoporotic fractures of the proximal humerus in elderly Finnish persons: sharp increase in 1970-1998 and alarming projections for the new millennium. Acta Orthop Scand 2000;71:465-70. [DOI] [PubMed] [Google Scholar]
- 6.Palvanen M, Kannus P, Niemi S, Parkkari J. Update in the epidemiology of proximal humeral fractures. Clin Orthop 2006;442:87-92. [DOI] [PubMed] [Google Scholar]
- 7.Beredjiklian PK, Iannotti JP, Norris TR, Williams GR. Operative treatment of malunion of a fracture of the proximal aspect of the humerus. J Bone Joint Surg Am 1998;80:1484-97. [DOI] [PubMed] [Google Scholar]
- 8.Boileau P, Trojani C, Walch G, et al. Shoulder arthroplasty for the treatment of the sequelae of fractures of the proximal humerus. J Shoulder Elb Surg 2001;10:299-308. [DOI] [PubMed] [Google Scholar]
- 9.Ferrel JR, Trinh TQ, Fischer RA. Reverse total shoulder arthroplasty versus hemiarthroplasty for proximal humeral fractures: a systematic review. J Orthop Trauma 2015;29:60-8. [DOI] [PubMed] [Google Scholar]
- 10.Wang J, Zhu Y, Zhang F, et al. Meta-analysis suggests that reverse shoulder arthroplasty in proximal humerus fractures is a better option than hemiarthroplasty in the elderly. Int Orthop 2016;40:531-9. [DOI] [PubMed] [Google Scholar]
- 11.Willis M, Min W, Brooks JP, et al. Proximal humeral malunion treated with reverse shoulder arthroplasty. J Shoulder Elb Surg Am 2012;21:507-13. [DOI] [PubMed] [Google Scholar]
- 12.Kilic M, Berth A, Blatter G, et al. Anatomic and reverse shoulder prostheses in fracture sequelae of the humeral head. Acta Orthop Traumatol Turc 2010;44:417-25. [DOI] [PubMed] [Google Scholar]
- 13.Raiss P, Edwards TB, da Silva MR, et al. Reverse shoulder arthroplasty for the treatment of nonunions of the surgical neck of the proximal part of the humerus (type-3 fracture sequelae). J Bone Joint Surg Am 2014;96:2070-6. [DOI] [PubMed] [Google Scholar]
- 14.Raiss P, Edwards TB, Collin P, et al. Reverse shoulder arthroplasty for malunions of the proximal part of the humerus (type-4 fracture sequelae). J Bone Joint Surg Am 2016;98:893-9. [DOI] [PubMed] [Google Scholar]
- 15.Wall B, Nove-Josserand L, O’Connor DP, et al. Reverse total shoulder arthroplasty: a review of results according to etiology. J Bone Joint Surg Am 2007;89: 1476-85. [DOI] [PubMed] [Google Scholar]
- 16.Zafra M, Uceda P, Flores M, Carpintero P. Reverse total shoulder replacement for nonunion of a fracture of the proximal humerus. Bone Jt J 2014;96-B:1239-43. [DOI] [PubMed] [Google Scholar]
- 17.Hattrup SJ, Waldrop R, Sanchez-Sotelo J. Reverse total shoulder arthroplasty for post-traumatic sequelae. J Orthop Trauma 2016;30:e41-7. [DOI] [PubMed] [Google Scholar]
- 18.Martinez AA, Bejarano C, Carbonel I, et al. The treatment of proximal humerus nonunions in older patients with reverse shoulder arthroplasty. Injury 2012;43(Suppl.2):3-6. [DOI] [PubMed] [Google Scholar]
- 19.Tofthagen C. Threats to validity in retrospective studies. J Adv Pract Oncol 2012;3:181-3. [PMC free article] [PubMed] [Google Scholar]
- 20.Hussey MM, Hussey SE, Mighell MA. Reverse shoulder arthroplasty as a salvage procedure after failed internal fixation of fractures of the proximal humerus: outcomes and complications. Bone Jt J 2015;97-B:967-72. [DOI] [PubMed] [Google Scholar]
- 21.Levy O, Pritsch M, Oran A, Greental A. A wide and versatile combined surgical approach to the shoulder. J Shoulder Elb Surg 1999;8:658-9. [DOI] [PubMed] [Google Scholar]
- 22.Roy J-S, MacDermid JC, Woodhouse LJ. Measuring shoulder function: a systematic review of four questionnaires. Arthritis Rheum 2009;61:623-32. [DOI] [PubMed] [Google Scholar]
- 23.Rangan A, Handoll H, Brealey S, et al. Surgical vs nonsurgical treatment of adults with displaced fractures of the proximal humerus: the PROFHER randomized clinical trial. J Am Med Assoc 2015;313:1037-47. [DOI] [PubMed] [Google Scholar]
- 24.Iyengar JJ, Devcic Z, Sproul RC, Feeley BT. Nonoperative treatment of proximal humerus fractures: a systematic review. J Orthop Trauma 2011;25: 612-7. [DOI] [PubMed] [Google Scholar]


