Abstract
Vasculogenic defects of great vessels (GVs) are a major cause of congenital cardiovascular diseases. However, genetic regulators of endothelial precursors in GV vasculogenesis remain largely unknown. Here we show that Stat4, a transcription factor known for its regulatory role of pro-inflammatory signalling, promotes GV vasculogenesis in zebrafish. We find stat4 transcripts highly enriched in nkx2.5+ endothelial precursors in the pharynx and demonstrate that genetic ablation of stat4 causes stenosis of pharyngeal arch arteries (PAAs) by suppressing PAAs 3–6 angioblast development. We further show that stat4 is a downstream target of nkx2.5 and that it autonomously promotes proliferation of endothelial precursors of the mesoderm. Mechanistically, stat4 regulates the emerging PAA angioblasts by inhibiting the expression of hdac3 and counteracting the effect of stat1a. Altogether, our study establishes a role for Stat4 in zebrafish great vessel development, and suggests that Stat4 may serve as a therapeutic target for GV defects.
Stat4 is a transcription factor known to regulate pro-inflammatory signalling. Here, Meng et al. show that Stat4 is not only regulating inflammation but it is also crucial for great vessels development and endothelial precursor proliferation in zebrafish, by inhibiting the expression of hdac3 and counteracting the effect of Stat1a.
Great vessel defects (GVDs) are one of the major causes of congenital cardiovascular diseases, which lead to the death of millions of infants and children annually1,2. GVDs include carotid artery anomalies, aberrant subclavian arteries, interrupted aortic arch, coarctation of the aorta, patent ductus arteriosus, proximal pulmonary artery hypoplasia and others3,4. Cellular and genetic mechanisms of great vessel malformations remain largely unknown, partly due to the intricate structure and transformation of GVs in fetal growth5,6. Investigation of the vasculogenesis of great vessels may help clarify GVD etiologies7. During vasculogenesis, angioblasts, which originate from endothelial precursors of the mesoderm, coalesce and assemble into the primary structure of great vessels such as the aortic arch arteries (also known as pharyngeal arch arteries, PAAs)8,9. The PAAs connect the blood flow from the heart to the dorsal aorta in the embryo, and they provide an indispensable contribution to the carotid arteries and great vessels of the heart10,11.
Recent studies have found that the endothelium of great vessels is derived from mesodermal precursors expressing heart field markers, such as Nkx2.5. It has been reported that subpopulations of nkx2.5+ cells in the anterior lateral plate mesoderm (ALPM) condense to form four pairs of clusters that give rise to PAAs 3–6, but the function of Nkx2.5 is not required until the activation of the vasculogenesis programme of great vessels12. This finding suggests that spatiotemporally specific mediators regulate the angioblast fate of nkx2.5+ endothelial precursors to form great vessels. We previously found that repression of the second heart field (SHF) regulator Ltbp3 led to great vessel anomalies13. It is reported that the deletion of the SHF regulator FGF8 in the cardiogenic mesoderm also causes PAA phenotypes in mice14. Tcf21, together with Nkx2.5, marks a dispensable group of PAA progenitors for great vessel formation in zebrafish10. Although Tbx haploinsufficiency causes aortic arch defects in mice, it is involved in endoderm–mesenchyme interactions but not angioblast formation in the mesoderm15,16. Despite the roles of these cardiogenic regulators in the development of great vessels, the specific regulators of nkx2.5+ endothelial precursors of great vessels have not been revealed.
Using the transparent zebrafish embryo model, we are able to visualize the process of great vessel vasculogenesis, which is difficult to study in mice and humans due to gestation in the uterus13,17. This vasculogenesis programme in zebrafish lasts from 28 h post-fertilization (hpf) to 48 hpf, which is comparable to similar processes that occur in the fourth week of human embryo development11,12. Using this model, we conduct a transcriptional microarray analysis of nkx2.5+ cells at 30 hpf and identify signal transducer and activator of transcription factor 4 (stat4), which is highly expressed, as a potential regulator of nkx2.5+ endothelial precursors. As a pro-inflammatory signalling mediator, Stat4 has long been shown to direct the development of fully functional T helper 1 cells and is canonically activated by interleukin (IL)-12 receptor-associated JAK kinases18,19.
In this study, we generate a stat4 mutant line using the CRISPR/Cas system, and describe a pivotal role of Stat4 in regulating the proliferation of endothelial precursors during great vessel vasculogenesis. Furthermore, we uncover that stat4 is downstream of nkx2.5 and promotes angioblast formation by suppressing hdac3 and stat1a. Our findings elucidate a surprising and important function of Stat4 in the establishment of great vessels.
Results
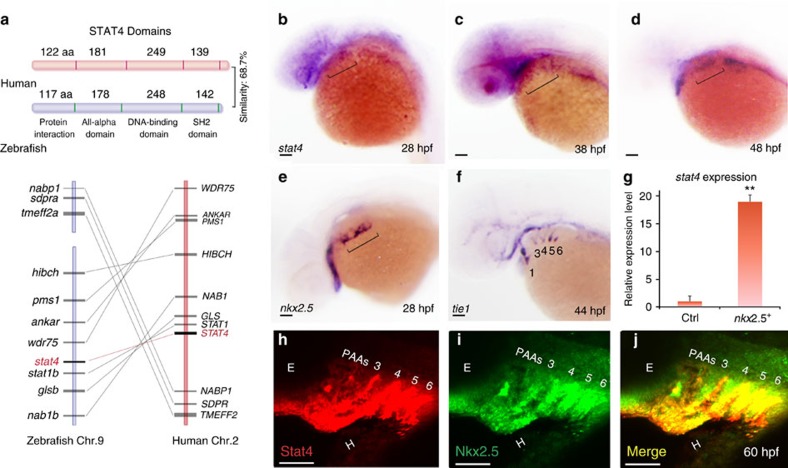
Conservation of Stat4 and its expression in the pharynx
The orthologues of all mammalian STAT genes in zebrafish have been identified with the high primary sequence conservation20. Zebrafish stat4 encodes a 731-aa protein, which contains four functional domains and shares 68.7% sequence similarity with human STAT4. Stat4 is located on Chromosome 9 in zebrafish, and no paralogs have been identified. The genes flanking zebrafish stat4 are syntenic with the STAT4 locus in humans. As evident from the domain structure and amino-acid sequence alignment, zebrafish stat4 is closely related to the corresponding mammalian homologues (Fig. 1a and Supplementary Fig. 1).
Figure 1. Conservation of Stat4 and its expression in nkx2.5+ PAA endothelial progenitors.
(a) Schematic diagram illustrates the STAT4 protein functional domains of Human (red) and Zebrafish (blue), and synteny analysis of Stat4 loci on the human (red) and zebrafish (blue) chromosomes. The width of the lines and their distances represent the relative sizes of the genes and loci distances, respectively. (b–d) Brackets indicate that stat4 expression resides in the pharynx at 28 hpf (b), 38 hpf and 48 hpf (d) by in situ hybridization. (e) nkx2.5+ cells locate in the pharynx at 28 hpf (f) tie1+ cells at 44 hpf following the appearance of nkx2.5 pharyngeal clusters. (g) The expression level of stat4 in nkx2.5+ cells compared with somatic cells at 30 hpf from microarray data. Error bars indicate s.d., unpaired two-tailed Student's t-test, **P=0.002 (triplicates for each group) (h,i) The immunohistochemistry staining of Stat4 (red) and Nkx2.5 (green) of wild-type embryos using anti-Stat4 and anti-Nkx2.5 antibodies at 60 hpf. (j) Co-localization of Stat4 and Nkx2.5 protein analysis by the merged image (yellow). Scale bars, 50 μm. n≥20 embryos per group for in situ, n=12 embryos per group for immunohistochemistry; hpf, hours post-fertilization.
The expression level of stat4 was found to be 18-fold higher in nkx2.5+ cells by transcriptional microarray analysis of the Tg(nkx2.5:Zsyellow) line at 30 hpf than in somatic cells (Fig. 1g). Pathway enrichment analysis showed that Jak-Stat signalling was a major upregulated pathway in nkx2.5+ cells (Supplementary Fig. 2A). The activated genes of the Jak-Stat pathway were listed in the heatmap and scatter plot, among which stat4 was the most highly activated (Supplementary Fig. 2B,C). In situ hybridization showed that expression of stat4 was enriched in the ALPM at 28 h post fertilization (hpf) and 48 hpf (Fig. 1b–d and Supplementary Fig. 3A–G). Stat4 transcripts were also distributed in the pharyngeal arch area at 60 hpf (Supplementary Fig. 3H,I). As shown in Supplementary Fig. 3E–I, stat4 is not expressed in the heart at 24 hpf or 48 hpf, but we could observe the weak expression of stat4 in the heart at 60 hpf.
Similar to stat4, nkx2.5 transcripts were co-localized in the pharyngeal clusters of the ALPM at 28 hpf, which subsequently differentiates into aortic arch angioblasts in the pharynx, as visualized by the angioblast marker tie1 (Fig. 1e,f). Later, nkx2.5+ ZsYellow populations from the mesoderm formed the primitive great vessels, the third to sixth pairs of PAAs (PAAs 3–6) visualized by the ZsYellow+/mCherry+ population of Tg(nkx2.5:ZsYellow);Tg(flk1:mCherry) embryos (Supplementary Fig. 4A–C). The Stat4 protein co-localized with Nkx2.5 proteins in PAAs 3–6 at 60 hpf, as revealed by double immunofluorescent staining (Fig. 1h–j).
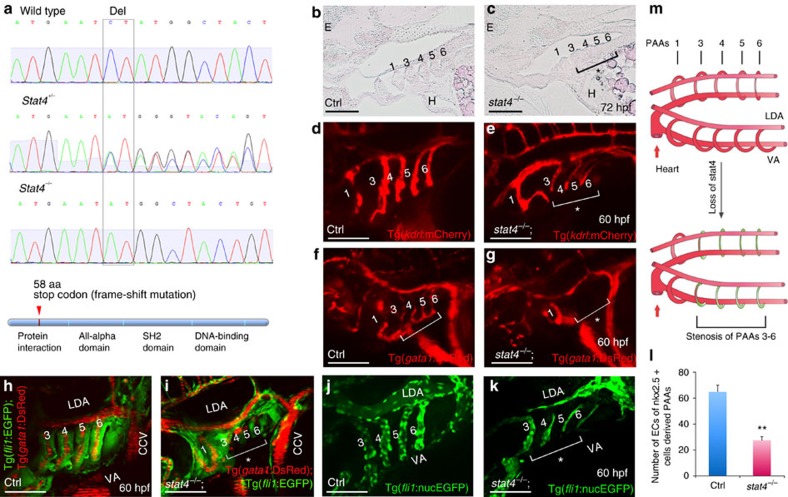
Loss of stat4 causes stenosis of the primitive great vessels
A splice morpholino, targeting the splice acceptor site for intron 3 of stat4, was employed to suppress normally spliced stat4 transcripts in zebrafish embryos, generating stat4 morphants. Reverse transcription PCR showed that the transcript was efficiently knocked down. Whereas control embryos expressed normal stat4 transcripts, the morphants expressed improperly spliced stat4 messenger RNAs (mRNAs) without exons 3 and 4 (Supplementary Fig. 5A). The stat4 morphants did not show obvious developmental abnormalities other than the stenosis of PAAs 3–6.
The CRISPR/Cas system was employed to generate stat4 zebrafish mutants by targeting exon 3 (Supplementary Fig. 5B). After CRISPR/Cas RNA injection, we detect the F1 generation heterozygotes and found robust induction of targeted insertion/deletion mutations by assessing the frequency of altered alleles (Supplementary Table 1). The selected homozygous stat4 mutant of the F3 generation shown in Fig. 2 had a two-base pair deletion that caused a frame-shift mutation and a premature stop codon in exon 3, leading to a truncated protein with 58 amino acids (Fig. 2a). The heterozygous and homozygous stat4 mutants were born at normal Mendelian ratios and showed atrophic pharyngeal regions and a slightly small head at 72 hpf compared with the wild-type siblings. The mutants had fewer and shorter arch arteries than their wild-type siblings, which have full-length arch arteries and plump necks. There were no apparent defects in the other tissues or the development of homozygotes (Supplementary Fig. 6A–C). The stat4 mutant and morphant embryos had the same phenotype, but the deficiency of mutants was stronger than that of morphants.
Figure 2. Loss of stat4 leads to stenosis of PAAs 3–6.
(a) Genomic sequences of wild-type zebrafish, stat4 heterozygous mutants and homozygous mutants. The stat4 mutant has a two-base pair deletion, which causes a frame-shift mutation and a premature stop codon to form a truncated protein with 58 amino acids. (b,c) Pathological sections (10 μm per section) of wild-type and mutant embryos with Haematoxylin-Eosin staining at 72 hpf (n=12). (d,e) Confocal images of PAAs in the control Tg(kdrl:mCherry) embryos and the stat4−/−;Tg(kdrl:mCherry) line (n=9). (f,g) Images of PAAs 3–6 vessels trafficking blood flow in the control and stat4−/−;Tg(gata1:DsRed) embryos (n=9). (h,i) Images of PAAs trafficking blood flow in the control and the stat4−/−;Tg(fli1:EGFP);Tg(gata1:DsRed) line (n=8). (j–l) Control and the stat4−/−;Tg(fli1:nucEGFP) embryos show PAA endothelial cells (green) with cell number counts at 60 hpf (n=9). Error bars indicate s.d., unpaired two-tailed Student's t-test, **P=0.003. (m) The model of PAAs 3–6 phenotype caused by stat4 deficiency is illustrated in the cartoon. Scale bars, 50 μm. LDA, lateral dorsal aorta; VA, ventral aorta; E, eye; H, heart. The brackets with asterisks highlight the malformed individual PAAs.
The defect of PAAs 3–6 can be seen in pathological sections of the mutants. The arch arteries in mutants lack lumen endothelium, but the surrounding smooth muscle of the vasculature did not have any evident abnormality compared with wild-type controls. The deficiency of PAAs 3–6 in the mutants led to atrophy of the pharynx, and the jaw defect can also be observed in tissue sections (Fig. 2b,c). The stenosis of PAAs 3–6 caused by stat4 deficiency can be clearly visualized by the stat4−/−;Tg(kdrl:mCherry) lines (Fig. 2d,e). Furthermore, the shunted blood flow labelled by gata1+ was undetectable in PAAs 3–6 vessels in the stat4−/−;Tg(gata1:DsRed) line, while the major vessels such as the lateral dorsal aorta and common cardinal vein retained robust blood flow (Fig. 2f,g). The stat4−/−;Tg(fli1:EGFP);Tg(gata1:DsRed) line indicated that the narrow and short PAAs 3–6 in the mutants were unable to support blood flow (Fig. 2h,i and Supplementary Fig. 7A). The lack of blood flow was due to stenosis of the arch artery lumens, visualized in the stat4−/−;Tg(fli1:nucEGFP) line. The cell count numbers revealed an ∼58% decrease in differentiated endothelial cells of PAAs 3–6 in stat4 mutants compared with the control (Fig. 2j-l). As shown in Supplementary Fig. 7B,C, the yellow cells remained in PAAs 3–6 of stat4 morphants in the Tg (nkx2.5:zsyellow);Tg(kdrl:mCherry) line, indicating that the remained structure of PAAs 3–6 was derived from nkx2.5+ cells. However, an insufficient number of nkx2.5+ cells led to the deficient growth of the arch arteries in the morphants compared with the controls.
Taken together, suppression of stat4 caused agrowth deficiency of PAAs 3–6, while the first pair of aortic arch arteries that is established before the initiation of circulation were not impaired in either the control or stat4 mutant/morphant embryos. The model of stenosis of the primitive great vessels (PAAs 3–6) caused by stat4 deficiency is shown in Fig. 2m.
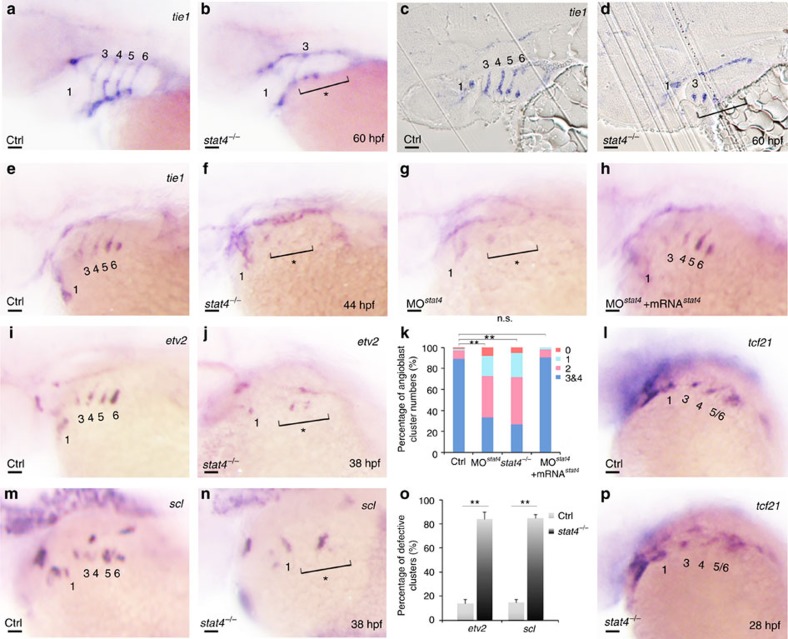
Lack of Stat4 prevents emergence of PAA angioblasts
In stat4 mutants, the lack of tie1 transcripts in arch arteries 3–6 of the stat4 mutants suggested a decline in the vasculogenesis programme of the nkx2.5+ cells derived from PAAs 3–6 compared with the control group at 60 hpf (Fig. 3a,b). The resin sections showed that the tie1 probe labelled the four cords of PAAs angioblasts in the control, while only minimal tie1+ angioblasts were observed in PAAs 3–6 of stat4 mutants (Fig. 3c,d). The vasculogenesis defect in stat4 mutants was observed as early as emergence of the four pairs of angioblastic cords (ACs) (as indicated by the asterisk and bracket). Loss of stat4 inhibited the emergence of tie1-labelled ACs, the number of which was significantly decreased in mutants at 44 hpf. The stat4 morphants phenocopied the tie1+ PAA angioblast deficiency seen in the mutants. The recruitment of stat4 mRNA specifically restored all four pairs of ACs in the morphants (Fig. 3e–h,k). Evaluation of endothelial precursors by etv2 and scl at the top of the signalling hierarchy of angioblast formation demonstrated that suppression of stat4 inhibited the emergence of both etv2 and scl clusters in stat4 mutants (Fig. 3i,j,m–o). The myoblast marker tcf21 was not affected in the mutants at 28 hpf (Fig. 3l,p) or in the Tg (tcf21:GFP) stat4 morphants at 30 hpf (Supplementary Fig. 8S,T). Evaluation of flk1 expression, the endothelial marker, showed the loss of ACs 3–6 at 38 hpf (Supplementary Fig. 7D–F). Angiogenesis represented by flk1+ inter-segmental vessels was not affected in the stat4 morphants (Supplementary Fig. 7G–I). Evaluation of the vascular mesoderm by etv2 demonstrated that other vasculatures such as the cranial21 or somatic vasculatures were not significantly impaired by suppression of stat4 (Supplementary Fig. 7J,K).
Figure 3. Lack of stat4 represses emergence of PAA angioblasts.
(a,b) tie1 transcripts expressing PAAs are visualized in the control and stat4 mutants at 60 hpf. (c,d) Resin sections (10 μm per section) of wild-type and stat4 mutant embryos with tie1 in situ hybridization at 60 hpf. (e–h) Analysis of tie1 expression in pharyngeal angioblastic cords is conducted in the control embryos (e), stat4 mutants (f), stat4 morphant embryos (g) and embryos with stat4 mRNA and stat4 morpholino injection (h) at 44 hpf by in situ hybridization. (k) Proportional quantification of embryos with defective PAA angioblast cords in tie1 staining assays, Kruskal–Wallis test with the Dunn's multiple comparison test, **P<0.01, n.s.: P>0.05. (i,j,m,n) The etv2 and scl transcripts are evaluated by in situ hybridization in the control and stat4 mutants at 38 hpf. (o) Percentage of embryos with defective PAA angioblastic cords in etv2 and scl staining assays, error bars indicate the s.d., Kruskal–Wallis test, **P=0.0058, n=30 per each group. (l,p) tcf21+ PAAs are visualized in the control and stat4 mutants at 28 hpf. Scale bars, 50 μm. a–d, n=23 embryos in each group; e–h, n=32 embryos in each group; l,p, n=26 embryos per group.
Embryonic haematopoiesis in the intermediate cell mass was not evidently disturbed by scl probe detection in morphants (Supplementary Fig. 8A,E). The gata1-labelled somatic blood flow was normal in stat4 morphants compared with the control group (Supplementary Fig. 8B,F). Rag1-labelled T cells of the thymus and the foxn1-labelled thymus epithelia are not interrupted in stat4 morphants compared with the control embryos (Supplementary Fig. 8C,D,G,H). Neural crest-derived pharyngeal mesenchyme is unaffected in stat4 morphants, as revealed by hand2 and dlx2a expression patterns (Supplementary Fig. 8I,J,M,N). The normal tbx1 expression pattern in morphants demonstrated that the loss of stat4 did not alter pharyngeal ectoderm or endoderm at 28 hpf, comparable to the controls (Supplementary Fig. 8K,O). Additionally, tbx1 expression in the pharyngeal mesoderm is not significantly impaired in the mutants at 28 hpf (Supplementary Fig. 8Q,R).
Meanwhile, the gata4+ cardiac progenitors in the ALPM remain normal in stat4 morphants (Supplementary Fig. 8L,P) at 18-somite stage (ss). Both the nkx2.5+ cardiac progenitors and the formation of the linear heart tube are normal in stat4 morphants (Supplementary Fig. 9A,B,D,E). No obvious differences are found in the ltbp3+ SHF of the control embryos and the morphants (Supplementary Fig. 9I,L). The heart morphology from 48 hpf to 60 hpf is not impaired in the embryos lacking stat4 compared with the control using the Tg(nkx2.5:ZsYellow) line (Supplementary Fig. 9C,F).
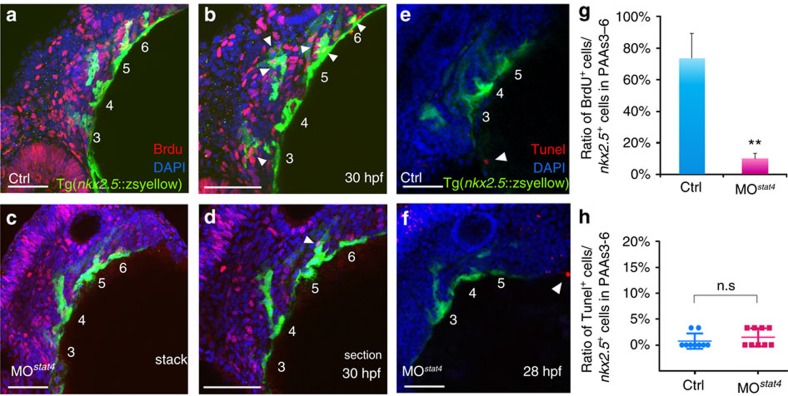
Stat4 promotes proliferation of nkx2.5 + endothelial precursors
Morphogenesis of the four clusters of nkx2.5+ endothelial precursors in the ALPM remained unchanged, despite the lack of stat4, as shown in the transverse sections of Tg(nkx2.5:ZsYellow) embryos at 30 hpf (Fig. 4a,c). However, the BrdU cooperation assay showed that the quantity of the co-localized BrdU+ (red) and nkx2.5+ (green) cells was significantly reduced in the stat4 morphants compared with the control embryos (Fig. 4a–d,g yellow). Cellular apoptotic evaluation of nkx2.5+ clusters by TdT-mediated dUTP nick end labelling (TUNEL) revealed that the lack of stat4 did not impair endothelial precursor survival (Fig. 4e,f,h).
Figure 4. Lack of stat4 inhibited proliferation of nkx2.5 PAA progenitors but not apoptosis.
(a–d) The control (a,b) and stat4 morphant (c,d) Tg(nkx2.5:ZsYellow) embryos at 30 hpf are stained by BrdU (red), 4',6-diamidino-2-phenylindole (DAPI) (blue) as well as immunohistochemistry for ZsYellow (yellow). The single confocal sections are shown in b,d. (e,f) Projections of the pharyngeal arch region of 28 hpf control (e) and stat4 morphant (f) Tg(nkx2.5:ZsYellow) embryos are assayed for TUNEL (red) and pharyngeal arch arteries for ZsYellow (yellow). (g) Ratios of BrdU+ cells/the nkx2.5+ cells in PAAs 3–6 region across three experimental replicates (n=6 embryos/replicate in each group); Error bars indicate the s.d. Kruskal–Wallis test, **P=0.0036. (h) Ratios of TUNEL+ cells/the nkx2.5+ cells in PAAs 3–6 region, n=9 per each group, n.s.: P>0.05. White arrowheads indicate BrdU+ or TUNEL+ cells. Scale bars, 50 μm.
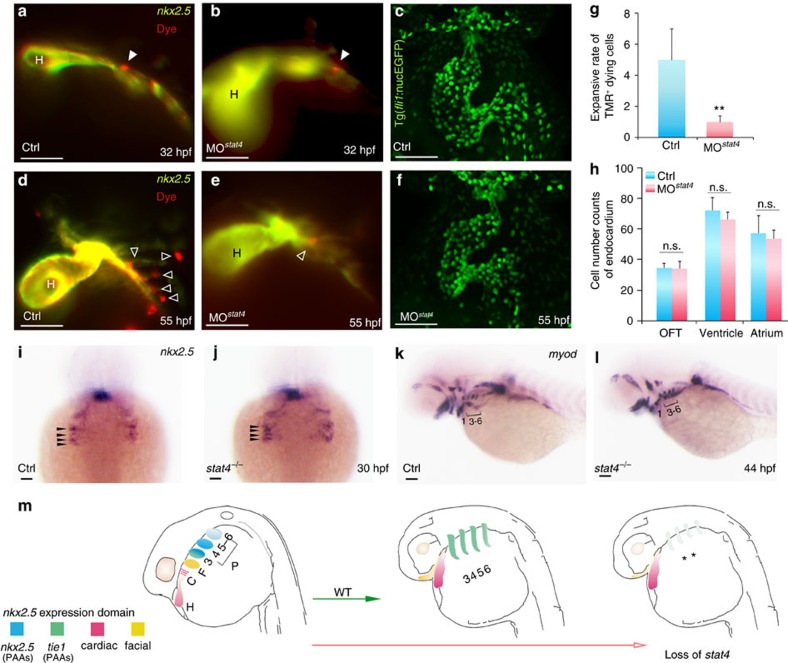
Cell-dye was used to label the nkx2.5+ endothelial precursors to further investigate their proliferation and migration in the absence of stat4. Tg(nkx2.5:ZsYellow) embryos were injected with CellTracker Red in the ZsYellow+ pharyngeal cluster region at 28 hpf. After culturing for 4 h, the single cell was labelled and imaged at 32 hpf as the starting point. At this time, the labelled cells in the control and morphant embryos did not show any obvious differences. The same embryos were imaged again at 55 hpf. As shown in Fig. 5a,b,d,e,g, the labelled cell forms multiple dye+ cells in the PAAs of control embryos, while the labelled cell remains in its original location without proliferation in the stat4 morphants, indicating repressed proliferation and migration of endothelial precursors in stat4 morphants.
Figure 5. Cell tracing of endothelial precursors.
(a,b,d,e) The control (a,d) and stat4 morphant (b,e) Tg(nkx2.5:ZsYellow) embryos injected with CellTracker Red (white arrowheads) in the non-heart ZsYellow region at 28 hpf are imaged at 32 hpf (a,b) and again at 55 hpf (d,e). The hollow arrowheads indicate the labelled cells. (c,f) Confocal Z-stacks captured fli1+ endothelial cells in the heart region at 55 hpf in the control (c) and stat4 morphants (f), respectively. (g) Quantification of TMR+ cells (n=12 per each group, Error bars indicate the s.d. Kruskal–Wallis test, **P=0.003). (h) Quantification of green endothelial cells at 55 hpf across three experimental replicates (n=6 embryos/replicate in each group. Analysis of variance (ANOVA) test with multiple comparison post-hoc test, P=0.9999 no significant (n.s.) difference in the outflow tract (OFT), P=0.6866 (n.s.) in the ventricle, P=0.9878 (n.s.) in the atrium between the control and stat4 morphants. (i,j) Morphogenesis of the four pairs of nkx2.5+ pharyngeal clusters between the wild-type control and stat4 mutants at 30 hpf (indicated by black arrows). (k,l) The myod transcripts expressing PAAs are visualized in the control and stat4 mutants at 44 hpf. (m) The schematic illustration shows the fate of nkx2.5+ cells in ALPM in wild-type (WT) and loss of stat4 embryos at 28 and 55 hpf. The first pair gives rise to the facial lineage, and 2 to 4 pairs had endothelial fate. ALPM nkx2.5+ clusters (H,C,F, PAAs 3–6). Blue: nkx2.5 expressing cells, Green: tie1 expressing cells, Red: cardiac lineage and Yellow: facial lineage. C: cardiac, F: facial, H: heart. Scale bars, 50 μm. n≥30 embryos per each group in i–l.
We also wondered whether stat4 regulated the fate equilibrium between the endocardium and great vessel endothelium derived from nkx2.5+ endothelial precursors. No labelled cells migrated to the heart tube in morphants, as shown in Fig. 5e. Using the Tg(fli: nucEGFP) line, we counted the endocardium cell numbers in the heart and outflow tract at 55 hpf and found no obvious changes in cell numbers in the morphants compared with the controls (Fig. 5c,f,h). Hence, stat4 was not involved in the fate determination between the great vessel endothelium and the endocardium. Evaluation of myod indicated no defects in the PAA- and facial-muscle lineage or in the somatic skeletal muscle of mutants (Fig. 5k,l). Only the distance between PAA- muscles and the ventral aorta muscles in stat4 mutants was shorter than that in the control embryos.
The specification of endothelial precursors in the ALPM was tested by comparing the morphogenesis of the four pairs of nkx2.5+ pharyngeal clusters between the controls and mutants. No evident change was found by 30 hpf between the two groups, suggesting that the specification of nkx2.5+ endothelial precursors was not prevented by the suppression of stat4 (Fig. 5i,j), consistent with the results in Fig. 4a–d and Supplementary Fig. 9G,H,J,K. The schematic illustration in Fig. 5m shows the fate of nkx2.5+ cells in the ALPM, and the loss of stat4 can inhibit the proliferation of nkx2.5+ endothelia precursor clusters 3–6 to cause insufficient assembly of the primitive great vessels.
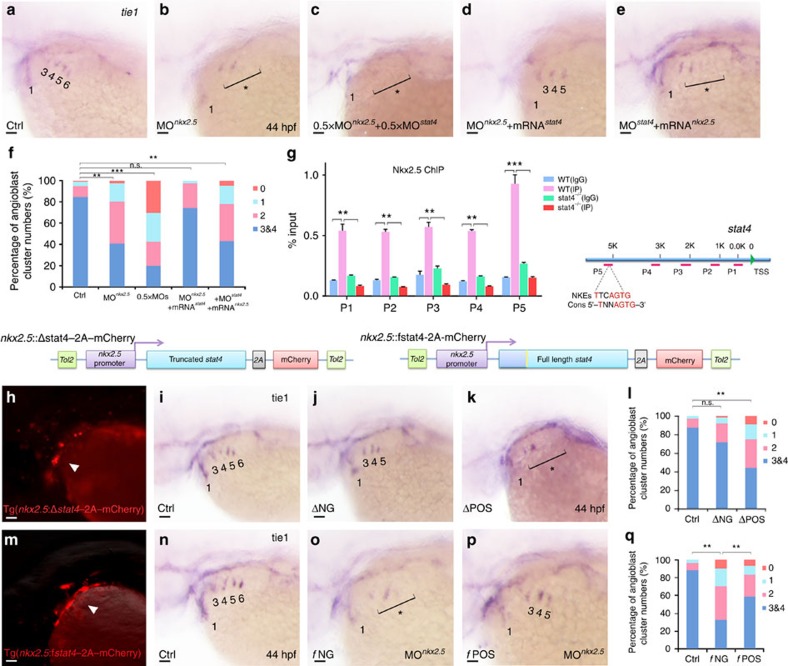
Stat4 acts downstream of Nkx2.5 to regulate PAA angioblasts
Notably, nkx2.5 knock down reduced the number of PAAs ACs, which showed a similar phenotype as the stat4 morphant embryos, consistent with the previous study12. Co-suppression of stat4 and nkx2.5 by half dosages of morpholinos caused a total depletion of ACs 3–6. Overexpression of nkx2.5 transcripts by injecting in vitro synthesized full-length nkx2.5 mRNA did not restore the tie1+ AC quantity of stat4 morphants. In contrast, replenishment of stat4 mRNA rescued the reduction in the number of ACs in nkx2.5 morphant embryos, as shown by the increase in the percentage of embryos with over two pairs of ACs 3–6 to control levels (Fig. 6a–f).
Figure 6. Cell-autonomous requirement of Stat4 downstream of Nkx2.5.
(a–e) In situ hybridization analysis of tie1 transcripts in the control (a), nkx2.5 morphant embryos (b), embryos with half doses of nkx2.5 and stat4 morpholinos (c), nkx2.5 morphants with stat4 mRNA (d) and stat4 morphants with nkx2.5 mRNA (e). (f) Proportional quantification of embryos with defective angioblastic cords, Kruskal–Wallis test with the Dunn's multiple comparison test, **P<0.01, ***P<0.001, n.s.: P>0.05, n≥30 per each group. (g) The ChIP analysis with anti-Nkx2.5 antibody for the promoter regions of stat4 in the wild-type and stat4 mutants at 44 hpf across six experimental replicates (n=30 embryos/replicate in each group, Kruskal–Wallis test with the Dunn's multiple comparison test, **P<0.01, ***P<0.001). The binding enrichment region at the stat4 locus is indicated by primers (P1–P5). The minimal DNA-binding consensus (Cons) for Nkx2.5 contains a 5'-TNNAGTG-3' sequence motif. (h,m) Cellular autonomous analysis of stat4 is carried out by utilizing an nkx2.5 promoter to generate chimeric embryos with transient truncated (Δ) and full-length (f) stat4 gene expression in nkx2.5+ cells. The schematic diagram shows tol2-mediated transient transgenesis of nkx2.5 promoting mCherry expression. (h) Specific mCherry fluorescence expresses as pharyngeal clusters in the transgenic embryos with nkx2.5 promoter driving variant N-terminal 51 amino-acids residues truncated zebrafish stat4. (m) Exclusive mCherry fluorescence in the pharynx is observed in the transgenic nkx2.5 promoter driving full-length wild-type form of zebrafish stat4 in nkx2.5 morphants embryos. (i–k) tie1+ PAA angioblastic cords are appraised by in situ hybridization in the controls (i), negative mCherry fluorescence expressing embryos (ΔNG) (j) and positive mCherry fluorescent embryos (ΔPOS). (l) Proportional quantification data. Kruskal–Wallis test with the Dunn's multiple comparison test, **P<0.01, n.s.: P>0.05, n≥30 per each group. (n–p) The control (n), negative mCherry fluorescence expressing embryos with nkx2.5 MO (fNG) (o) and positive mCherry fluorescence expressing embryos with nkx2.5 MO (fPOS) (p). (q) Proportional quantification data, Kruskal–Wallis test with the Dunn's multiple comparison test, **P<0.01, n≥30 per each group. Scale bars, 50 μm.
The chromatin immunoprecipitation (ChIP) assay showed that Nkx2.5 can bind to the promoter region of stat4, and the binding can be inhibited by nkx2.5 knock down. The Nkx2.5 DNA-binding site (NKE)22 was found in the binding enrichment region at the stat4 locus using primer 5, suggesting that stat4 was a direct target of Nkx2.5 (Fig. 6g).
Cellular autonomous analysis of Stat4 was carried out by utilizing an nkx2.5 promoter and the tol2 transposon to generate chimeric embryos with transient gene expression in nkx2.5+ cells, as shown in Fig. 6h,m. Driven by the nkx2.5 promoter, full-length (f) or N-terminal truncated forms (Δ) of Stat4 were expressed with high fidelity in nkx2.5+ cells, as indicated by the mCherry fluorescence, within bilateral ACs at 32 hpf. The tie1 in situ hybridization of the positive transgenic embryos (ΔPOS) with dominant-truncated Stat4 in nkx2.5+ cells and the negative embryos (ΔNG) reveals that ΔPOS embryos displayed a reduced number of ACs compared with ΔNG and controls. Overexpression of full-length Stat4 in nkx2.5+ cells (fPOS) can sufficiently reverse the reduced number of ACs caused by the nkx2.5 morpholino (fNG) (Fig. 6h–q).
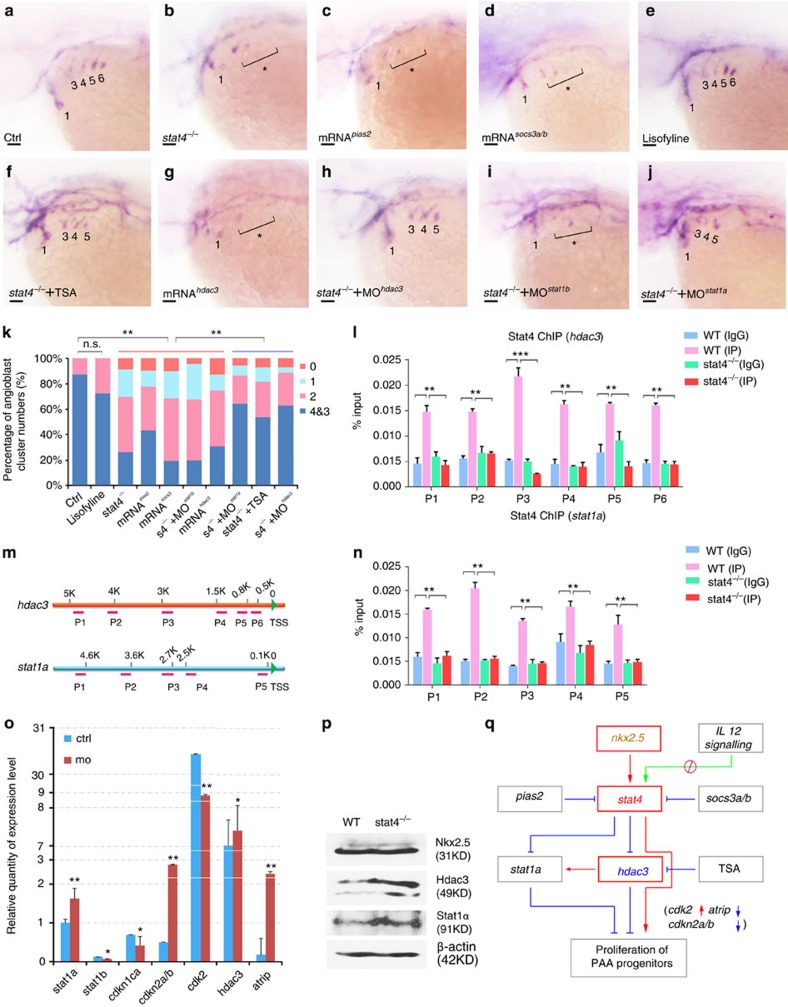
Stat4 regulates angioblasts by suppressing Stat1a and Hdac3
To understand the downstream signalling of Stat4 in this process, a small molecule lisofylline, the canonical inhibitor of IL-12-mediated stat4 activation23, was used to treat the embryos. The tie1 in situ hybridization of lisofylline-treated embryos showed that the number of PAA angioblast cords did not decline, indicating that IL-12 signalling was not involved in the angioblast formation. However, overexpression of the Stat4-specific inhibitor Socs3a/b24 did reduce the number of tie1-expressing cords. Similarly, overexpression of another Stat4-specific inhibitor, Pias2 (previously known as Piasx25), also resulted in a decrease of tie1-expressing cords, mimicing the phenotype of stat4 mutants (Fig. 7a–e,k).
Figure 7. stat4 promoted the PAA angioblast programme by suppressing stat1a and hdac3.
(a–k) In situ hybridization analysis of tie1 transcripts in the control (a), stat4 mutants (b), embryos with 50 ng μl−1 pias2 mRNA injection (c), embryos with 50 ng μl−1 socs3a and socs3b mRNAs injection (d), embryos treated with 85 μM lisofylline (e), stat4 mutants with 0.2 μM TSA treatment (f), embryos with 50 ng μl−1 hdac3 mRNA injection (g), stat4 mutants with 4 ng μl−1 hdac3 morpholino (h), stat4 mutants with 4 ng μl−1 stat1b morpholino (i), stat4 mutants with 4 ng μl−1 stat1a morpholino (j) at 44 hpf. Scale bars, 50 μm. (k) Proportional quantification of indicated tie1+ expressing cords number (s4−/−: stat4 mutants), Kruskal–Wallis test with the Dunn's multiple comparison test, **P<0.01, n.s.: P>0.05, n ≥30 embryos per each group. (l–n) The ChIP analysis with anti-Stat4 antibody for the promoter regions of hdac3 and stat1a in the wild-type control and stat4 mutants at 44 hpf across six experimental replicates (n=30 embryos/replicate in each group, analysis of variance (ANOVA) test with multiple comparison post-hoc test, **P<0.01, ***P<0.001). (m) The binding enrichment regions at the hdac3 and stat1a locus are indicated by primers (P1–P6). (o) Q-PCR results of related genes expression in the control and stat4 morphants at 44 hpf across six experimental replicates (n=10 embryos/replicate in each group. Error bars indicate s.d., unpaired two-tailed Student's t-test, *P<0.05, **P<0.01. (p) Protein levels of Nkx2.5, Hdac3 and Stat1a in the wild-type control and stat4 mutants detected by western blots at 44 hpf. β-actin is used as the internal control. (q) A network is drawn to illustrate the stat4 pathway in controlling PAA proliferation. Red: activation, Blue: suppression.
Many studies have confirmed the association of the Stat4-Stat1 locus in chronic inflammation diseases26, and Stat4 can counteract the function of Stat1 in T cells27. Hence, we knocked down stat1a and stat1b in stat4 mutants and found that the knockdown of stat1a can partially rescue the loss of ACs but not stat1b (Fig. 7i,j). It has been reported that Hdac3 deacetylates Stat1, thus permitting its phosphorylation and ability to inhibit proliferation. Notably, HDAC type I and II inhibitor Trichostatin A (TSA)-treated embryos rescues the PAA angioblast cluster loss seen in mutants. It has been reported that HDACs 3 is responsive to TSA treatment in vascular endothelium28. We found that the injection of hdac3 mRNA can efficiently inhibit vasculogenesis of the great vessels. Moreover, morpholino-mediated hdac3 knock down can rescue the PAAs phenotype of the stat4 mutant (Fig. 7f–h,k).
The ChIP assays showed that Stat4 can target the promoter regions of hdac3 and stat1a, and the binding was mostly enriched in the hdac3 promoter region identified by primer 3 (Fig. 7l–n). Furthermore, the levels of Hdac3 and Stat1 proteins were upregulated in stat4 mutants, as shown in the western blot, while the Nkx2.5 protein level was not affected (Fig. 7p and Supplementary Fig. 10). Expression level changes of these genes were confirmed by quantitative PCR (Q-PCR) results. The cell proliferation-related gene cdk2 was significantly downregulated, whereas the expression levels of its inhibitors cdkn2a/b and atrip were elevated in the absence of stat4 (Fig. 7o). Based on the described results, we show a schematic representation of the signalling pathway regulated by stat4 and involved in PAA angioblast formation (Fig. 7q).
Discussion
The deficiency of primitive great vessels is a key predisposing factor for cardiovascular disease29,30. Unlike the relatively advanced knowledge of endothelial development, little information about the regulation of endothelial precursors of the great vessels has been available to date. Our findings demonstrate that Stat4 has a critical role in promoting vasculogenesis of the great vessels. Several lines of evidence support this conclusion: (1) stat4 transcripts are located specifically in the pharynx and persisted throughout PAA vasculogenesis; (2) loss of stat4 selectively causes the stenosis of PAAs 3–6 by suppressing angioblast emergence of the great vessels in mutants; (3) lack of stat4 inhibits the proliferation but not the apoptosis, fate equilibrium or specification of nkx2.5+ endothelial precursors; (4) Stat4 expression is regulated by Nkx2.5 to autonomously promote PAA angioblast formation; and (5) Stat4 promotes PAA angioblast emergence by inhibiting epigenetic regulator hdac3 expression and counteracting the effects of stat1a.
PAA endothelial progenitors derive from the caudal nkx2.5+ clusters in the ALPM12. We found that the proliferation of these progenitors is Stat4 dependent. The nkx2.5+ PAA endothelial progenitors could still differentiate into arch artery endothelium without Stat4. However, lack of stat4 prevents proliferation of nkx2.5+ cells and eventually results in stenosis of the primitive GVs. A previous study showed that tcf21, together with nkx2.5, marked a group of PAA progenitor cells, but the tcf21+ nkx2.5+ progenitors were not required for PAA formation10. In this study, we found that genetic ablation of stat4 did not affect the tcf21-expressing PAA cells. The PAA- and facial-muscle also remained normal in stat4 mutants, indicating that the muscle cell lineage of PAAs was not affected by the loss of stat4. This evidence implicated that stat4 might specifically regulate the PAA endothelial cell lineage rather than other cell lineages of PAAs.
Although Stat4 has been most extensively investigated as a critical mediator for several pro-inflammatory cytokines and chemokines such as IL-12 and type I interferon in T lymphocytes, it was unknown whether it had any role in vasculogenesis. Several studies have provided clues that the Stat4-mediated inflammation is involved in cardiovascular diseases. STAT4 has been demonstrated to be one of the strongest genetic susceptibility factors for systemic lupus erythematosus, and notably, patients with systemic lupus erythematosus with the STAT4 risk allele have a strikingly increased risk of cardiovascular disease31. Stat4 has been found to be involved in the development of cardiac allograft vasculopathy in mice32. Also, PIAS2, the specific inhibitor of STAT4, has a critical role in human umbilical vein endothelial cells33. This evidence implicates a genetic predisposition via STAT4 to some cardiovascular diseases.
Some of the Stat4-related pro-inflammatory factors may participate in the vasculogenesis of great vessels. Recent studies have highlighted a paradigm where the endogenous mechanisms of pro-inflammatory factors function to maintain normal tissue homeostasis34. Pro-inflammatory cytokines and chemokines are also reported to be expressed in the hearts of infants with congenital heart disease with GVDs35. Low levels of STAT4 are expressed in cultured human umbilical vein endothelial cells and are tyrosine-phosphorylated by interferon but not IL-12 (ref. 36). We show here that canonical IL-12-Stat4 signalling does not participate in Stat4-mediated PAA vasculogenesis, however, Stat4-specific inhibition-by Pias2, Socs3a and Socs3b suppresses PAA angioblasts formation. Most SOCS proteins act in a classical negative-feedback loop to inhibit cytokine signal transduction37. Socs3 can specifically inhibit the activation of Stat4 by binding to the Stat4 docking site in its upstream receptor through the SH2 domain. In addition, socs3a and socs3b are found to be highly expressed in nkx2.5+ cells, together with the upregulation of stat4 in this study (Supplementary Fig. 2).
Since previous studies have confirmed the association of STAT4-STAT1 locus on chromosome 2 (Fig. 1a) in inflammatory diseases18,26, and stat1a was enriched in the nkx2.5+ cells in our microarray, we speculated that Stat1 may be involved in the Stat4 signalling network. Indeed, repression of stat1a can partially rescue GVDs caused by the absence of stat4. Previous studies have shown that stat1 has anti-proliferation roles in pro-inflammatory cells and vasculatures38. Moreover, Stat4 acts as a key molecule in overcoming the Stat1-dependent inhibition of proliferation in T cells27. Hence, it is possible that Stat4 can activate the proliferation of PAAs by inhibiting Stat1a.
It is reported that HDAC can modulate the pro-inflammatory response39, thus it was conceivable to hypothesize that HDAC may be involved in the Stat4 signalling in GV vasculogenesis. Indeed, we show that treatment with the HDAC type I and II specific inhibitor TSA can reverse the PAA phenotype of stat4 mutant embryos, and Hdac3 has an important role in PAA vasculogenesis downstream of Stat4. A recent study showed that TSA could enhance vascular repair by recruiting human endothelial progenitors and increasing the expression of SCL-dependent genes, which may support our findings here40. It is reported that the HDAC3 inhibitor has no significant effect on the heart28,41. We also confirmed that stat4 deficiency did not have evident effects on the heart during PAAs formation. Meanwhile, Stat1 can be deacetylated by Hdac3, thus permitting its phosphorylation42. Based on our data and the previous reports, Hdac3 seems to be an important target of Stat4 in mediating the proliferation of the endothelial precursors of great vessels.
In summary, our study provides insights into a potential role of the pro-inflammatory regulator Stat4 in great vessel establishment and endothelial precursor proliferation. Therefore, Stat4 can possibly serve as a diagnostic marker or a therapeutic target for GVD.
Methods
Zebrafish strains maintenance
Zebrafish embryos were raised at 28.5 °C and morphologically staged. The wild-type lines AB/Tubingen, Tg(nkx2.5:ZsYellow), Tg(gata1:DsRed), Tg(flk1:mCherry), Tg(fli1:eGFP), Tg (tcf21: GFP) and Tg(fli1:nucGFP) lines have been previously reported13. Embryos or tail fins were collected for genotyping. All zebrafish in this study were treated in strict accordance with the recommendations in the Guide for the Care and Use of Laboratory Animals of the National Institutes of Health. The experimental protocols were approved by the Review Board on the Ethics of Animal Experiments of Institute of Health Sciences, Shanghai Institutes of Biological Sciences, Chinese Academy of Sciences (Shanghai, China).
FAC sorting and microarray analysis
The embryos of Tg(nkx2.5:ZsYellow) at 30 hpf were dissociated by incubation in 1 × PBS supplemented with 0.125% dispase (Life Technologies, NY, USA) for 30 to 45 min at 28.5 °C. The cells were washed and resuspended in ice-cold 0.9 × PBS plus 5% FBS and were passed through a filter with a 40 μm pore size. Samples were sorted twice into lysis buffer via a triple-LASER fluorescence-activated cell sorting instrument (FACSAria, BD Biosciences, CA, USA) to ensure cell purities of >95%, maximal RNA integrity, and minimal loss of material. Two independent sets of purified RNA from nkx2.5+ cells and nkx2.5− somatic cells were prepared and labelled according to the manufacturer's instructions (Affymetrix, Santa Clara, CA, US). Samples were then hybridized onto a Zebrafish Oligonucleotide Microarray (AffymetrixGeneChip). The Affymetrix(R) software and GeneSpring software7.3 were used to analyse the data and visualize differential expression, respectively.
Construction and microinjection of CRISPR/Cas
The stat4 target sites of CRISPR/Cas were determined online (http://zifit.partners.org/ZiFiT/CSquare9Nuclease.aspx). For the efficient induction of mutagenesis in stat4, one target site was finally selected from the candidate sites. Stat4 guide RNA (gRNA) was targeted to exon 3 (CRISPR/Cas stat4 E3, GGCATCAAACCATGAATCTATGG) with forward (5′-ATAGGCAT CAAACCATGAATCTAGT-3′) and reverse (5′-TAAAACTAGATTCATGGTTTGATGC-3′) primers. Stat4 gRNA was obtained by in vitro transcription with the MAXISCRIPT T7 Kit (Ambion, Thermo Fisher Scientific Inc., US) and then purified using the mirVana miRNA Isolation Kit (Ambion) following the manufacturer's instructions. CRISPR capped nls-zCas-nls RNA was synthesized using SP6 mMessage mMachine Transcription Kit (Ambion). A mixture of RNAs (500 ng μl−1 of nls-zCas-nls RNA and 90 ng μl−1 of gRNA) in 0.05% phenol red and 120 mM KCl was injected into the cellular portion of one-cell stage embryos, resulting in an ∼60% rate of deformity at 24 hpf.
Generation of zebrafish stat4 mutant lines
The surviving embryos after injection with CRISPR/Cas RNAs were raised to adulthood and screened for founders with germ-line mutations in the stat4 locus. The T7 endonuclease I (T7E1) enzyme was used to screen for mutations (New England Biolabs, MA, USA) according to the manufacturer's instructions. After the outcross between the founders and wild-type zebrafish, the outcross between the F1 and the wild-type, and the subsequent incross between the heterozygous F2 generation, we obtained several mutant lines for further investigation.
Microinjection of zebrafish embryos
Knockdown of genes was achieved by the injection of corresponding anti-sense morpholinos into one-cell-stage embryos. Morpholinos were purchased from Gene Tools (USA). Nkx2.5 morphants were obtained via the injection of 1 nl of nkx2.5 morpholino (4 ng μl−1) targeting the nkx2.5 splicing site43. To generate stat4 morphants, one-cell stage embryos were injected with 1 nl of anti-sense morpholino (6 ng μl−1) targeting the third-intron fourth exon splice acceptor sequence (MOstat4: 5′-GTATTTCACCTGGGAGAATAGAAGA-3′). To validate the effectiveness of MOstat4-mediated stat4 splicing inhibition, we obtained first strand complementary DNAs (cDNAs) from control and MOstat4 embryos and performed PCR to amplify the sequence spanning MOstat4 target region with forward (5′-TTCAGCAACTGGATATTAAGTTCCTCGAA-3′) and reverse (5′-TGAACGCTGCTTCTTATCACA GCC-3′) primers. Then, agarose gel electrophoresis of the PCR products was used to visualize the bands.
Capped tol2 transposase and nkx2.5, stat4, socs3a, socs3b and pias2 mRNAs were synthesized in vitro from linearized plasmid templates by SP6 mMessage mMachine Transcription Kit (Ambion) (Supplementary Table 2). Rescue assays were carried out by co-injection of 50 ng μl−1 mRNA into one-cell-stage embryos. A 4.8 kb nkx2.5 promoter was prepared from Tubigen genome using the forward (5′-GTAGACTGAGTATTCGTTGCGTTAT-3′) and the reverse (5′-TTCCTGACAACAGCCGA-3′) primers44. The N-terminal 51 amino-acid residues truncated stat4 fragment were amplified from cDNA library with the forward primer (5′-CTAGCTAGCATGGCTACTGTACTCTTCAAT-3′) and the reverse primer (5′-CTAGCTAGCGGGTGAACTCATAGCGCTCTC-3′). The full-length and truncated stat4 cDNA were driven by the nkx2.5 promoter, and the constructs were injected into the cellular portion of the one-cell-stage embryos at 50 ng μl−1.
RNA probe synthesis and whole mount in situ hybridization
Zebrafish wild-type cDNA was used for amplifying stat4, tie1, nkx2.5, hand2, gata4, scl, etv2, flk1, tbx1, foxn1 and rag1 sequences that were subcloned into pCS2+ vector (Supplementary Table 2). T3 RNA polymerase (Roche Applied Science, IN, USA) was used to generate RNA probes transcripts from linearized DNA templates.
Whole-mount in situ hybridizations were conducted using digoxygenin (DIG) labelled anti-sense RNA probes (Roche Applied Science, Mannheim, Germany). Embryos were collected and fixed in 4% paraformaldehyde. Following dehydration and rehydration in a decreasing methanol series, the embryos were digested with 10 μg ml−1 proteinase K and hybridized overnight at 70 °C. After blocking and washing, the embryos were stained with nitro-blue tetrazolium chloride/5-bromo-4-chloro-3′-indolyphosphate p-toluidine (Roche Applied Science, Mannheim, Germany).
Compound inhibitor treatment
Inhibition of IL-12 signalling was performed by incubating wild-type Tubingen zebrafish embryos in 85 μM lisofylline egg water (Caymanchem) or an equivalent amount of dimethylsulphoxide (DMSO) as a control, starting at the 18-somite stage. Both DMSO and lisofylline-treated wild-type embryos were fixed for tie1 in situ hybridizations at 44 hpf and imaged. Similarly, 0.2 μM TSA was used to inhibit the function of HDACs type I and II starting at 28 hpf, and the treated embryos were fixed and subjected to tie1 in situ hybridizations at 44 hpf.
Immunohistochemistry
Fixed embryos were rehydrated in 1 × PBS/0.5% Triton X-100 (PBSTx) and blocked with PBSTx/1% BSA/0.1% DMSO for 3 h. The embryos were then incubated with primary antibodies and secondary antibodies diluted in blocking solution for 2 h. Primary antibodies for GFP (IgG2a mouse monoclonal, Life technology), ZsYellow (anti-RCFP rabbit polyclonal antibody, Clontech), Nkx2.5 (Thermo Fisher, US) and Stat4 (Sigma, US) were incubated at a 1:50 dilution. Secondary antibodies (Alexa Fluor 488 goat α-mouse IgG, Alexa Fluor 546 goat-rabbit IgG (Invitrogen) were used at a 1:500 dilution.
BrdU staining and TUNEL immunostaining
Control and MOstat4 Tg(nkx2.5:ZsYellow) embryos at 30 hpf were incubated in a pre-chilled 10 mM BrdU/15% DMSO solution on ice for 20 min, transferred to pre-warmed egg water and incubated for 15 min at 28.5 °C before fixation. The embryos were digested with 1 mg ml−1 Proteinase K for 30 min at room temperature. Mouse α-BrdU (Roche Applied Science, Mannheim, Germany) and α-mouse Alexa Fluor 546 (Invitrogen, Carlsbad, CA) primary and secondary antibodies were both used at dilutions of 1:500. Following antibody staining and washes, the embryos were incubated with 0.5 μg ml−1 4′,6-diamidino-2-phenylindole in 1 × PBS for 10 min in the dark at room temperature. After three 1 × PBS washes, the embryos were mounted and imaged.
The TUNEL assay was performed with the In Situ Cell Death Detection Kit TMR red (Roche). The morpholino injected Tg(nkx2.5:ZsYellow) embryos and wild-type embryos at 28 hpf were fixed and stored in 100% methanol at −20 °C. After rehydration, Proteinase K digestion and acetone treatment, embryos were permeated with a permeabilization solution (0.5% Triton X–100, 0.1% sodium citrate in PBS) at room temperature for 1 h. Then, the embryos were stained by the enzyme solution and photographed.
Cell tracker red labelling
Cell Tracker Red dye was purchased from Invitrogen and diluted to 10 μM in egg water. Tg(nkx2.5:ZsYellow) embryos at 28 hpf were injected with an 1 nl drop of dye in the pharyngeal ZsYellow region outside the heart tube. Following the injection, images were taken at ∼32 hpf and again at 55 hpf.
Chromatin immunoprecipitation (ChIP)
Chromatin was prepared from zebrafish embryos at 44 hpf and fragmented by sonication with Fisher Scientific's Sonic Dismembrator (6% amplitude, pulse for 10 s on and 30 s off for a total sonication ‘on' time of 2 min 40 s) to produce fragments ranging from 100 to 500 bp. Then, five percent chromatin was removed from each sample and used as the input control. ChIP was performed using antibodies specific for Nkx2.5 (PA5-49431, Thermo Fisher, US), Stat4 (WH0006775M1, Sigma, US) and IgG control (2719s, Cell Signaling, US) at dilutions of 1:100, 1:100 and 1:1,000, respectively. The bound DNA and mock DNA were used for SYBR green Q-PCR analyses.
Western blot analysis
Western blot was performed with the standard protocols. Protein was prepared from zebrafish embryos at 44 hpf and dissolved in 4 × protein SDS–polyacrylamide gel electrophoresis Loading Buffer (Takara). Nkx2.5, Stat1a and Hdac3 were detected with anti-Nkx2.5 (PA5-49431, Thermo Fisher, US), anti-Stat1a (SAB3500364, Sigma, US) and anti-Hdac3 (ab32369, Abcam, US) at the dilution of 1:1,000, followed by incubation with an anti-rabbit IgG-horseradish peroxidase antibody (ab97069, Abcam, US) at a dilution of 1:5,000. β-actin was used as the internal control using an anti-β-actin antibody (A2228, Sigma, US), followed by an anti-mouse IgG antibody (62-6520, Invitrogen, US) diluted 1:1,000 and 1:5,000 in the block solution, respectively. Full scans of all western blots are presented in Supplementary Fig. 10.
Confocal fluorescent imaging
Whole mount transgenic embryos were prepared in 3% agarose in a glass-bottomed culture dish, and the images were captured using an Olympus FV10-ASW confocal microscope system (Olympus, Tokyo, JP)45. EGFP was excited with a 488-nm Argon laser and imaged through a 505-536-nm filter. ZsYellow protein was excited with a 514-nm Argon laser and imaged through a 530-nm long pass filter. DsRed was excited with a 543-nm HeNe laser and imaged through a 560-nm long pass filter. mCherry was excited with a 564-nm HeNe laser and imaged through a 595-nm filter. The cells were counted in Z-stack confocal images using the ImageJ software.
Quantitative PCR analysis
Total RNA was reverse transcribed into cDNA with SuperScript III Reverse Transcriptase (Invitrogen). Quantitative real-time PCR (qPCR) was performed with SYBR Green (TOYOBO) on a 7900HT Fast Real-Time PCR System (Applied Biosystems). The relative RNA amount was calculated with the ΔΔCt method and normalized with gapdh (the primers are listed in Supplementary Table 2).
Statistical analysis
All biological experiments were performed at least three times. Data were analysed using Graphpad Prism 6 software. Quantitative data were presented as the mean±s.e.m. The normality of data was examined by the Shapiro-Wilk test. The data with normal distributions were analysed by the unpaired Student's two-tailed t-test between two groups, while the analysis of variance test with the multiple comparison post-hoc test was used to compare three or more groups. The data of non-normal distributions were analysed by the Kruskal–Wallis test with adjustments for multiple comparisons46. Statistical significance was denoted by *P<0.05, **P<0.01, ***P<0.001. The number of ACs (1 to 4) on the same side of the pharynx was counted to evaluate the deficiency of PAAs 3–6. Dysmorphic animals due to unknown developmental delays were excluded equally from the control and experimental groups.
Data availability
Microarray data have been deposited in ArrayExpress with the accession number E-MTAB-5406. All relevant data supporting the findings of this study are available within the paper and its supplementary information files, or from the authors on request.
Additional information
How to cite this article: Meng, Z.-Z. et al. The pro-inflammatory signalling regulator Stat4 promotes vasculogenesis of great vessels derived from endothelial precursors. Nat. Commun. 8, 14640 doi: 10.1038/ncomms14640 (2017).
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Material
Supplementary Figures and Supplementary Tables.
Acknowledgments
This work was supported by the National Natural Science Foundation of China [31322038, 81172694, 81370232, 81670115, 81573174], the Strategic Priority Research Program of the Chinese Academy of Science [XDA12020220], the Outstanding Youth Fund of Jiangsu Province [SBK2014010296], the Research Project of Chinese Ministry of Education [213015A], the Priority Academic Program Development of Jiangsu Higher Education Institutions (PAPD) and Qinglan project [JX2161015124].
Footnotes
The authors declare no competing financial interests.
Author contributions Z.-Z.M., W.L., Y.X., H.-M.Y., C.-Y.Z., D.S., L.-F.Y., A.-H.G. and Y.Z. performed experiments and analysed data; A.-H.G. and Y.Z. designed research plan and wrote the paper.
References
- Global Burden of Disease Study C. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 386, 743–800 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- van der Linde D. et al. Birth prevalence of congenital heart disease worldwide: a systematic review and meta-analysis. J. Am. Coll. Cardiol. 58, 2241–2247 (2011). [DOI] [PubMed] [Google Scholar]
- Srivastava D. Genetic assembly of the heart: implications for congenital heart disease. Annu. Rev. Physiol. 63, 451–469 (2001). [DOI] [PubMed] [Google Scholar]
- Berguer R. Function and Surgery of the Carotid and Vertebral Arteries 1st edn LWW (2013). [Google Scholar]
- Brown M. L. et al. Coarctation of the aorta: lifelong surveillance is mandatory following surgical repair. J. Am. Coll. Cardiol. 62, 1020–1025 (2013). [DOI] [PubMed] [Google Scholar]
- Congdon E. D. Transformation of the aortic-arch system during the development of the human embryo. Contrib. Embryol. 14, 49–U47 (1922). [Google Scholar]
- Graham A. Development of the pharyngeal arches. Am. J. Med. Genet. A 119A, 251–256 (2003). [DOI] [PubMed] [Google Scholar]
- De Val S. & Black B. L. Transcriptional control of endothelial cell development. Dev. Cell 16, 180–195 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmidt A., Brixius K. & Bloch W. Endothelial precursor cell migration during vasculogenesis. Circ. Res. 101, 125–136 (2007). [DOI] [PubMed] [Google Scholar]
- Nagelberg D. et al. Origin, specification, and plasticity of the great vessels of the heart. Curr. Biol.: CB 25, 2099–2110 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore K. L., Persaud T. V. N. & Torchia M. G. The Developing Human: Clinically Oriented Embryology 10th edn Saunders (2015). [Google Scholar]
- Paffett-Lugassy N. et al. Heart field origin of great vessel precursors relies on nkx2.5-mediated vasculogenesis. Nat. Cell Biol. 15, 1362–U1225 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou Y. et al. Latent TGF-beta binding protein 3 identifies a second heart field in zebrafish. Nature 474, 645–648 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watanabe Y. et al. Role of mesodermal FGF8 and FGF10 overlaps in the development of the arterial pole of the heart and pharyngeal arch arteries. Circ. Res. 106, 495–U413 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Z. et al. Tbx1 expression in pharyngeal epithelia is necessary for pharyngeal arch artery development. Development 132, 5307–5315 (2005). [DOI] [PubMed] [Google Scholar]
- Vokes S. A. & Krieg P. A. Endoderm is required for vascular endothelial tube formation, but not for angioblast specification. Development 129, 775–785 (2002). [DOI] [PubMed] [Google Scholar]
- Hiruma T., Nakajima Y. & Nakamura H. Development of pharyngeal arch arteries in early mouse embryo. J. Anat. 201, 15–29 (2002). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korman B. D., Kastner D. L., Gregersen P. K. & Remmers E. F. STAT4: genetics, mechanisms, and implications for autoimmunity. Curr. Allergy Asthma Rep. 8, 398–403 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watford W. T. et al. Signaling by IL-12 and IL-23 and the immunoregulatory roles of STAT4. Immunol. Rev. 202, 139–156 (2004). [DOI] [PubMed] [Google Scholar]
- Gorissen M., de Vrieze E., Flik G. & Huising M. O. STAT genes display differential evolutionary rates that correlate with their roles in the endocrine and immune system. J. Endocrinol. 209, 175–184 (2011). [DOI] [PubMed] [Google Scholar]
- Proulx K., Lu A. & Sumanas S. Cranial vasculature in zebrafish forms by angioblast cluster-derived angiogenesis. Dev. Biol. 348, 34–46 (2010). [DOI] [PubMed] [Google Scholar]
- Ferdous A. et al. Nkx2-5 transactivates the Ets-related protein 71 gene and specifies an endothelial/endocardial fate in the developing embryo. Proc. Natl Acad. Sci. USA 106, 814–819 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coon M. E., Diegel M., Leshinsky N. & Klaus S. J. Selective pharmacologic inhibition of murine and human IL-12-dependent Th1 differentiation and IL-12 signaling. J. Immunol. 163, 6567–6574 (1999). [PubMed] [Google Scholar]
- Tortorella C. et al. Impaired interleukin-12-dependent T-cell functions during aging: role of signal transducer and activator of transcription 4 (STAT4) and suppressor of cytokine signaling 3 (SOCS3). J. Gerontol. A Biol. Sci. Med. Sci. 61, 125–135 (2006). [DOI] [PubMed] [Google Scholar]
- Arora T. et al. PIASx is a transcriptional co-repressor of signal transducer and activator of transcription 4. J. Biol. Chem. 278, 21327–21330 (2003). [DOI] [PubMed] [Google Scholar]
- Remmers E. F. et al. STAT4 and the risk of rheumatoid arthritis and systemic lupus erythematosus. N. Engl. J. Med. 357, 977–986 (2007). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gil M. P. et al. Regulating type 1 IFN effects in CD8 T cells during viral infections: changing STAT4 and STAT1 expression for function. Blood 120, 3718–3728 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rafehi H. et al. Vascular histone deacetylation by pharmacological HDAC inhibition. Genome Res. 24, 1271–1284 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- van der Bom T. et al. The changing epidemiology of congenital heart disease. Nat. Rev. Cardiol. 8, 50–60 (2011). [DOI] [PubMed] [Google Scholar]
- Khairy P. et al. Changing mortality in congenital heart disease. J. Am. Coll. Cardiol. 56, 1149–1157 (2010). [DOI] [PubMed] [Google Scholar]
- Svenungsson E. et al. A STAT4 risk allele is associated with ischaemic cerebrovascular events and anti-phospholipid antibodies in systemic lupus erythematosus. Ann. Rheum. Dis. 69, 834–840 (2010). [DOI] [PubMed] [Google Scholar]
- Koglin J., Glysing-Jensen T., Gadiraju S. & Russell M. E. Attenuated cardiac allograft vasculopathy in mice with targeted deletion of the transcription factor STAT4. Circulation 101, 1034–1039 (2000). [DOI] [PubMed] [Google Scholar]
- Meinert C. et al. Identification of intracellular proteins and signaling pathways in human endothelial cells regulated by angiotensin-(1-7). J. Proteomics 130, 129–139 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruneau S., Nakayama H., Woda C. B., Flynn E. A. & Briscoe D. M. DEPTOR regulates vascular endothelial cell activation and proinflammatory and angiogenic responses. Blood 122, 1833–1842 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qing M. et al. Intramyocardial synthesis of pro- and anti-inflammatory cytokines in infants with congenital cardiac defects. J. Am. Coll. Cardiol. 41, 2266–2274 (2003). [DOI] [PubMed] [Google Scholar]
- Torpey N., Maher S. E., Bothwell A. L. & Pober J. S. Interferon alpha but not interleukin 12 activates STAT4 signaling in human vascular endothelial cells. J. Biol. Chem. 279, 26789–26796 (2004). [DOI] [PubMed] [Google Scholar]
- Yoshimura A., Naka T. & Kubo M. SOCS proteins, cytokine signalling and immune regulation. Nat. Rev. Immunol. 7, 454–465 (2007). [DOI] [PubMed] [Google Scholar]
- Fan H. B. et al. miR-142-3p acts as an essential modulator of neutrophil development in zebrafish. Blood 124, 1320–1330 (2014). [DOI] [PubMed] [Google Scholar]
- Shakespear M. R., Halili M. A., Irvine K. M., Fairlie D. P. & Sweet M. J. Histone deacetylases as regulators of inflammation and immunity. Trends Immunol. 32, 335–343 (2011). [DOI] [PubMed] [Google Scholar]
- Palii C. G. et al. Trichostatin A enhances vascular repair by injected human endothelial progenitors through increasing the expression of TAL1-dependent genes. Cell Stem Cell 14, 644–657 (2014). [DOI] [PubMed] [Google Scholar]
- McKinsey T. A. Therapeutic potential for HDAC inhibitors in the heart. Annu. Rev. Pharmacol. Toxicol. 52, 303–319 (2012). [DOI] [PubMed] [Google Scholar]
- Kramer O. H. et al. A phosphorylation-acetylation switch regulates STAT1 signaling. Genes Dev. 23, 223–235 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Targoff K. L., Schell T. & Yelon D. Nkx genes regulate heart tube extension and exert differential effects on ventricular and atrial cell number. Dev. Biol. 322, 314–321 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grajevskaja V., Balciuniene J. & Balciunas D. Chicken beta-globin insulators fail to shield the nkx2.5 promoter from integration site effects in zebrafish. Mol. Genet. Genomics 288, 717–725 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang L. et al. miR-34b regulates multiciliogenesis during organ formation in zebrafish. Development 140, 2755–2764 (2013). [DOI] [PubMed] [Google Scholar]
- Mei Y. et al. Adult restoration of Shank3 expression rescues selective autistic-like phenotypes. Nature 530, 481–484 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Figures and Supplementary Tables.
Data Availability Statement
Microarray data have been deposited in ArrayExpress with the accession number E-MTAB-5406. All relevant data supporting the findings of this study are available within the paper and its supplementary information files, or from the authors on request.