What motivates physicians to behave the way they do and make the decisions they make in the course of caring for patients? Given that a physician's proverbial pen dictates much of health care spending, possible answers to this question have serious implications not only for patients and their physicians, but also for payers, providers at large, policy makers, and the public.
Few would deny that external motivators like money influence human behavior. In the health care context, pay‐for‐volume incentives have contributed to wide variations in care and fueled the development of alternative ways of reimbursement, including most prominently pay‐for‐performance (P4P). Therefore, the issue is not whether financial incentives influence physician behavior, but whether they achieve their intended outcomes (e.g., high‐value care) and, probably just as importantly, whether they lead to unintended and unwelcomed outcomes (e.g., avoiding caring for sicker patients; disproportionately focusing on care processes that are being evaluated). One of these adverse outcomes is the potential for external motivators to undercut intrinsic motivation, commonly referred to as the “undermining” (Deci, Koestner, and Ryan 1999) or “crowding‐out” (Frey and Jegen 2001) effect. This phenomenon (referred to as the crowding‐out effect for the remainder of the commentary) has been observed in a variety of professionals from public school teachers (Fryer 2011) to West Point military cadets (Wrzesniewski et al. 2014), but it has not been well studied among physicians.
Three of the five papers commissioned by the Agency for Healthcare Research and Quality (AHRQ) allude to or explicitly reference the potential crowding‐out effect of P4P. Berenson and Rice (2015) advocate for “incentive neutrality” as a design principle for physician payment methods that promotes neither over‐ nor underutilization of health care services; Roland and Dudley (2015) consider it critical that financial incentives be aligned with professional values; Conrad (2015) argues for provider involvement in the development, implementation, and evaluation of P4P. In light of the increasing reliance on financial incentives to improve health care quality and cost, the motivational crowding‐out effect and its potential negative impact on care received by patients warrant deeper consideration by all who are committed to creating and sustaining a high‐value health care system.
Theories about work motivation have been validated by decades of empirical research by experimental psychologists and behavioral economists in non–health care settings (Grant and Shin 2011). Informed by Maslow's hierarchy of needs (Maslow 1943), self‐determination theory frames human behavior as being both intrinsically and extrinsically motivated. Ideally, physicians are intrinsically motivated to deliver care that is grounded in the best available science and the ethics of medicine. Intrinsic motivation is achieved or sustained when the following psychological needs are satisfied (Deci and Ryan 1985):
Autonomy, defined as feeling a sense of choice or freedom from coercion, as when a behavior is either interesting or personally meaningful;
Competence, defined as feeling effective and capable in one's actions, especially when feeling maximally challenged, as when one's ability is stretched or extended; and
Relatedness, defined as feeling reciprocally respected and cared for through connections with others.
These basic psychological needs are innate, self‐oriented drivers of human behavior that are not dependent on selfless ideals of altruism or morality.
How does motivation theory inform how we think about P4P in health care? Neoclassical economists have traditionally viewed performance‐contingent financial incentives as either the only motivator or as simply additive to preexisting intrinsic motivation (see Figure 1). Preexisting intrinsic motivation typically resides in activities that individuals consider inherently interesting and challenging (Deci, Koestner, and Ryan 1999). Laboratory and field studies have found that when performance‐contingent financial incentives are introduced, they may crowd out preexisting intrinsic motivation by undermining one's sense of autonomy and competence, resulting in poorer performance (as depicted by the left end of the solid line in Figure 2; Deci, Koestner, and Ryan 1999; Fryer 2011; Wrzesniewski et al. 2014). As opposed to the standard supply curve, where performance rises with payment (or the price effect), motivational crowding out works in the opposite direction. Therefore, the net effect of financial incentives on work performance depends on the relative size of the price effect and the crowding‐out effect (as depicted by the solid line in Figure 2). The crowding‐out effect is particularly evident when financial incentives are introduced for tasks that are cognitively complex (such as many of those that doctoring comprises) because such work is inherently interesting or challenging. The negative effect on incentivized and overall performance is also strong when financial incentives are very large (as depicted by the right end of the solid line in Figure 2) because the incentives themselves demand disproportionate attention, undermining one's sense of autonomy, and interfering with cognitive focus and creativity (Himmelstein, Ariely, and Woolhandler 2014).
Figure 1.
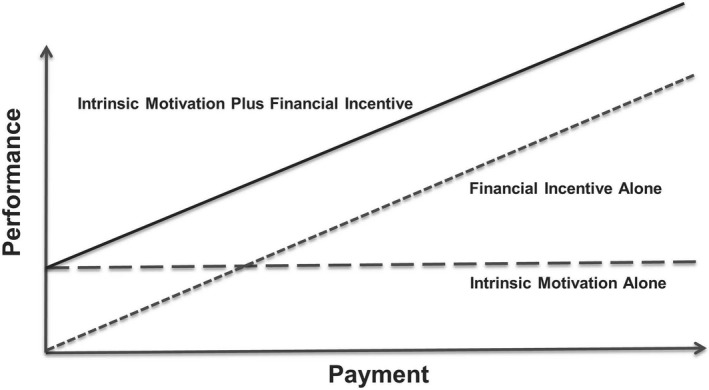
Financial Incentive Alone or as Additive to Preexisting Intrinsic Motivation
Figure 2.
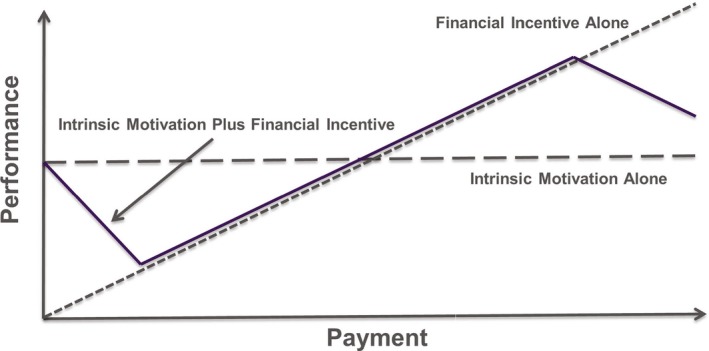
Financial Incentive Crowding Out Preexisting Intrinsic Motivation
Source: Figures from Woolhandler S, Ariely D. Will Pay for Performance Backfire? Insights from Behavioral Economics. Health Affairs Blog. October 11, 2012.
How, then, should one approach the design of P4P incentives to protect and support intrinsic motivation, and to avoid undermining the psychological work needs of physicians and others in the course of caring for patients? Scant empirical research has been conducted evaluating the crowding‐out effect in the health care context. That said, the current state of motivation science in the non–health care context provides a solid foundation for formulating testable hypotheses (Gagne and Forest 2008; Cerasoli, Nicklin, and Ford 2014).
By definition, financial incentives are not neutral. Berenson and Rice recognized that their idea of “incentive neutrality” is an idealized goal and that a more realistic goal is to minimize the unintended outcomes of P4P. In other words, how do we better align external incentives with intrinsic motivation? Several of the AHRQ‐commissioned papers highlight the necessary balance between simplicity and comprehensiveness of performance measures. While the minimum number of P4P measures required to strike such a balance is unclear, it is clear that not every aspect of work performance is measurable. And the more aspects of performance above the necessary minimum that are measured, the stronger the crowding‐out effect is likely to be because unnecessary measuring will undermine satisfaction of autonomy and competency needs. Currently, many P4P measures in health care are targeted to specific processes of care (e.g., glycosylated hemoglobin check). Targeted measures that break doctoring into distinct, piecemeal tasks may be perceived as more controlling and may undermine physicians’ sense of self‐efficacy than measures that are more global in scope. Beyond the number and scope of measures, the quality of P4P measures is potentially related to satisfying the psychological need to feel competent, thus affecting intrinsic work motivation (Cassel and Jain 2012). Measures that lack face validity are unlikely to be well accepted by those being held accountable for measure‐based performance.
Crowding out may be strongest when P4P financial incentives are large because they are perceived as more controlling. Compared to financial rewards, P4P financial penalties are likely to have a stronger price effect on performance by tapping into the individual's sense of loss aversion (Tversky and Kahneman 1991). However, such financial penalties could have an opposing crowding‐out effect by undermining physicians’ sense of autonomy and self‐efficacy (Gagne and Forest 2008). Finally, P4P incentives may undermine feelings of autonomy and competence when the physician lacks sufficient control to affect the performance outcome being measured (Cassel and Jain 2012).
Informed by the potential effect of P4P on psychological work needs, which is essential to supporting intrinsic motivation (Deci and Ryan 1985), the following hypotheses merit empirical evaluation and the findings of these evaluations would inform policy makers and payers in the design of financial incentives that minimize unintended consequences:
Crowding‐out effect increases with the number of pay‐for‐performance measures used above and beyond the minimum number of measures needed to sufficiently assess performance.
Crowding‐out effect is greater for pay‐for‐performance measures that are more targeted than those that are more global in scope.
Crowding‐out effect is greater for pay‐for‐performance measures that do not satisfy face validity than those that do.
Crowding‐out effect increases with the size of the pay‐for‐performance financial incentive.
Crowding‐out effect is greater for pay‐for‐performance incentives based on financial penalty than financial reward.
Crowding‐out effect is greater for pay‐for‐performance incentives when physicians’ ability to affect the performance outcome being measured is lower.
Each hypothesis above assumes that other P4P design features (e.g., number, scope, or validity of performance measures) is orthogonal or independent to the feature stated in the hypothesis in question.
Finally, while not the primary focus of most of the AHRQ‐commissioned papers, there are nonfinancial external motivators that should be taken into account. Schlesinger, Grob, and Shaller (2015) highlight the importance of public and private reporting of less quantifiable patient experiences (e.g., narrative data gathered in open‐ended comments on patient experience surveys) as nonfinancial inducements to improving quality of care delivered. Beyond quality reporting, health care delivery systems that foster clinical teams built on shared goals, clear roles, and mutual trust are likely to support competency and relatedness needs satisfaction (Mitchell et al. 2012); leaders who effectively communicate their vision and whose values are aligned with “front‐line” clinicians are more likely to create a work environment where professional judgment and autonomy are respected (Friedberg et al. 2013). Of the nine “levers” that Berenson and Rice propose to improve pay for value, only two involve financial incentives. They argue, as have others, that too much emphasis has been placed on financial incentives as a mechanism for holding physicians accountable, and relying on P4P may actually be counterproductive (Jain and Cassel 2010; Himmelstein, Ariely, and Woolhandler 2014). Others contend that the motivating potential of physician financial incentives is significantly constrained if workplace “hygiene” factors (e.g., electronic health records, administrative paperwork) are poorly designed and implemented (Herzberg 2003). Given that physicians are and will continue to be paid for their services, it is essential that we better understand how external motivators, financial as well as nonfinancial, support or undermine basic psychological needs of physicians and others who are charged with caring for us all.
References
- Berenson, R. , and Rice T.. 2015. “Beyond Measurement and Reward: Methods of Motivating Quality Improvement and Accountability.” Health Services Research 50 (6 Pt 2): 2155–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cassel, C. K. , and Jain S. H.. 2012. “Assessing Individual Physician Performance: Does Measurement Suppress Motivation?” Journal of the American Medical Association 307 (24): 2595–6. [DOI] [PubMed] [Google Scholar]
- Cerasoli, C. P. , Nicklin J. M., and Ford M. T.. 2014. “Intrinsic Motivation and Extrinsic Incentives: A 40‐Year Meta‐Analysis.” Psychological Bulletin 140 (4): 980–1008. [DOI] [PubMed] [Google Scholar]
- Conrad, D. 2015. “The Theory of Value‐Based Payment Incentives and Their Application to Health Care.” Health Services Research 50 (6 Pt 1): 2057–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deci, E. L. , Koestner R., and Ryan R. M.. 1999. “A Meta‐Analytic Review of Experiments Examining the Effects of Extrinsic Rewards on Intrinsic Motivation.” Psychological Bulletin 125: 627–68. [DOI] [PubMed] [Google Scholar]
- Deci, E. L. , and Ryan R. M.. 1985. Intrinsic Motivation and Self‐Determination in Human Behavior. New York: Plenum Press. [Google Scholar]
- Frey, B. S. , and Jegen R.. 2001. “Motivation Crowding Theory.” Journal of Economic Surveys 15 (5): 589–611. [Google Scholar]
- Friedberg, M. V. , Chen P. G., Van Busum K. R., Aunon F. M., Chau P., Caloyeras J. P., Mattke S., Pitchforth E., Quigley D. D., Brook R. H., Crosson F. J., and Tutty M.. 2013. Factors Affecting Physician Professional Satisfaction and Their Implications for Patient Care, Health Systems, and Health Policy. Santa Monica, CA: RAND; [accessed on April 21, 2015]. Available at http://www.rand.org/content/dam/rand/pubs/research_reports/RR400/RR439/RAND_RR439.pdf [PMC free article] [PubMed] [Google Scholar]
- Fryer, R. G. 2011. Teacher Incentives and Student Achievement: Evidence from New York City Public Schools. National Bureau of Economic Research Work Paper No 16850. Cambridge, MA: NBER; [accessed on March 3, 2015]. Available at http://www.nber.org/papers/w16850.pdf [Google Scholar]
- Gagne, M. , and Forest J.. 2008. “The Study of Compensation Systems through the Lens of Self‐Determination Theory: Reconciling 35 Years of Debate.” Canadian Psychology 49 (3): 225–32. [Google Scholar]
- Grant, A. M. , and Shin J.. 2011. “Work Motivation: Directing, Energizing, and Maintaining Effort (and Research)” In Oxford Handbook of Motivation, edited by Ryan R. M., pp. 505–19. New York: Oxford University Press. [Google Scholar]
- Herzberg, F. 2003. “One More Time: How Do You Motivate Employees?” Harvard Business Review 81 (1): 87–96. [PubMed] [Google Scholar]
- Himmelstein, D. U. , Ariely D., and Woolhandler S.. 2014. “Pay for Performance: Toxic to Quality? Insights from Behavioral Economics.” International Journal of Health Services 44: 203–14. [DOI] [PubMed] [Google Scholar]
- Jain, S. H. , and Cassel C. K.. 2010. “Societal Perceptions of Physicians: Knights, Knaves, or Pawns?” Journal of the American Medical Association 304 (9): 1009–10. [DOI] [PubMed] [Google Scholar]
- Maslow, A. H. 1943. “A Theory of Human Motivation.” Psychological Review 50: 370–96. [Google Scholar]
- Mitchell, P. , Wynia M., Golden R., McNellis B., Okun S., Webb C. E., Rohrbach V., and Von Kohorn I.. 2012. Core Principles & Values of Effective Team‐Based Health Care. Washington, DC: Institute of Medicine; [accessed on April 21, 2015]. Available at https://www.nationalahec.org/pdfs/VSRT-Team-Based-Care-Principles-values.pdf [Google Scholar]
- Roland, M. , and Dudley A. R.. 2015. “How Financial and Reputational Incentives Can Be Used to Improve Medical Care.” Health Services Research 50 (6 Pt 2): 2090–115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schlesinger, M. , Grob R., and Shaller D.. 2015. “Using Patient‐Reported Information to Improve Clinical Practice.” Health Services Research 50 (6 Pt 2): 2116–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tversky, A. , and Kahneman D.. 1991. “Loss Aversion in Riskless Choice: A Reference‐Dependent Model.” Quarterly Journal of Economics 106 (4): 1039–61. [Google Scholar]
- Wrzesniewski, A. , Schwartz B., Cong X., Kane M., Omar A., and Kolditz T.. 2014. “Multiple Types of Motives Don't Multiply the Motivation of West Point Cadets.” Proceedings of the National Academy of Sciences of the United States of America 111 (30): 10990–5. [DOI] [PMC free article] [PubMed] [Google Scholar]


