Significance
Interleukin 1 family member IL-37 is a naturally occurring inhibitor of inflammation. In this study, exogenous administration of recombinant human IL-37 reversed the decrease in exercise performance observed during systemic inflammation. IL-37 also increased exercise performance in healthy mice. IL-37 treatment acted through a dual mechanism of suppression of inflammation and modulation of metabolic pathways. The implications of the present findings impact on patients with chronic inflammatory diseases spanning from rheumatoid arthritis to cancer, in which fatigue is often incapacitating, and provide rationale for exploring recombinant IL-37 in the treatment of inflammation-mediated fatigue.
Keywords: inflammation, interleukin 37, metabolism, AMPK, fatigue
Abstract
IL-1 family member interleukin 37 (IL-37) has broad antiinflammatory properties and functions as a natural suppressor of innate inflammation. In this study, we demonstrate that treatment with recombinant human IL-37 reverses the decrease in exercise performance observed during systemic inflammation. This effect was associated with a decrease in the levels of plasma and muscle cytokines, comparable in extent to that obtained upon IL-1 receptor blockade. Exogenous administration of IL-37 to healthy mice, not subjected to an inflammatory challenge, also improved exercise performance by 82% compared with vehicle-treated mice (P = 0.01). Treatment with eight daily doses of IL-37 resulted in a further 326% increase in endurance running time compared with the performance level of mice receiving vehicle (P = 0.001). These properties required the engagement of the IL-1 decoy receptor 8 (IL-1R8) and the activation of AMP-activated protein kinase (AMPK), because both inhibition of AMPK and IL-1R8 deficiency abrogated the positive effects of IL-37 on exercise performance. Mechanistically, treatment with IL-37 induced marked metabolic changes with higher levels of muscle AMPK, greater rates of oxygen consumption, and increased oxidative phosphorylation. Metabolomic analyses of plasma and muscles of mice treated with IL-37 revealed an increase in AMP/ATP ratio, reduced levels of proinflammatory mediator succinate and oxidative stress-related metabolites, as well as changes in amino acid and purine metabolism. These effects of IL-37 to limit the metabolic costs of chronic inflammation and to foster exercise tolerance provide a rationale for therapeutic use of IL-37 in the treatment of inflammation-mediated fatigue.
The IL-1 family cytokine interleukin 37 (IL-37) functions as a natural suppressor of innate inflammation and acquired immunity (1). Reduction in endogenous IL-37 levels results in increased cytokine production induced by toll-like receptors (TLR) in human monocytes. In mice, IL-37 is truncated and not functional, but the human IL37 transgenic mouse exhibits reduced severity of systemic and local inflammation, as well as dampening of acquired immune responses (2–5). Moreover, administration of recombinant human IL-37 to wild-type mice also suppresses proinflammatory cytokines and curbs excessive inflammation, for example, in inflammatory arthritis (5). Recombinant IL-37 suppresses NLRP3 and IL-1β gene expression following acute lung injury (6). Recombinant IL-37 also increases insulin sensitivity in diet-induced obesity (7).
The mechanism of action for IL-37 is unique in the IL-1 family. IL-37 binds to the IL-18 receptor alpha chain (IL-18Rα), but then recruits IL-1R8. IL-1R8 functions to suppress local and systemic inflammation, as well as acquired immunity (8). Indeed, recombinant IL-37 administered to mice deficient for IL-1R8 does not suppress inflammation (5, 9). The complex of IL-18Rα with IL-37 plus IL-1R8 as the coreceptor signals the cell to reduce phosphorylation of proinflammatory kinases (1, 2, 7) and increase antiinflammatory cytokines (1, 3).
Here, we evaluated IL-37 treatment on exercise tolerance in mice subjected to systemic inflammation, and assessed whether IL-37 administration reduces the metabolic costs of inflammation. We further evaluated IL-37 monotherapy on exercise performance in healthy mice. The findings provide a rationale for exploring recombinant IL-37 as a therapy to combat fatigue in chronic inflammatory diseases.
Results
Recombinant Human IL-37 Reduces Local and Systemic Inflammatory Mediators and Improves Exercise Tolerance.
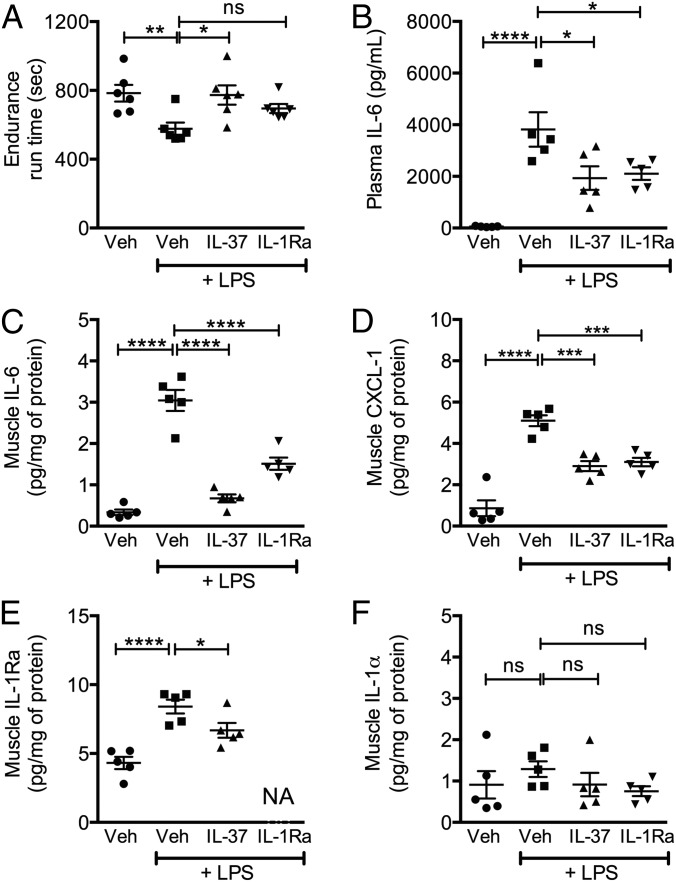
WT mice received recombinant human IL-37 or vehicle 24, 12, and 2 h before a single i.p. low dose of lipopolysaccharide (LPS) (10 µg per mouse, ∼0.33 mg/kg). Because IL-1 mediates inflammation-induced fatigue in mice (10), IL-37 treatment was compared with anakinra, the recombinant form of the naturally occurring human IL-1 receptor antagonist (IL-1Ra) (11, 12). Four hours after the administration of LPS, exercise tolerance was evaluated by using a Rota-Rod endurance test (13). As shown in Fig. 1A, vehicle-treated mice receiving LPS exhibited a 30% reduction in endurance running time (P = 0.008) compared with mice not receiving LPS. However, performance increased by 24% in mice treated with IL-37 before LPS challenge (P = 0.01). In fact, this increase restored performance to near baseline levels. An improvement over the LPS suppression was also observed with anakinra treatment, although that improvement did not reach statistical significance.
Fig. 1.
Effects of IL-37 treatment on systemic inflammation. (A) Mean ± SEM of endurance Rota-Rod run time in seconds. (B) Mean ± SEM plasma levels of IL-6. (C) Muscle content of IL-6. (D) CXCL-1. (E) IL-1Ra. (F) IL-1α. n = 5 mice per group. Statistical significance evaluated with the one-way ANOVA test. *P < 0.05; **P < 0.005; ***P < 0.001; ****P < 0.0001; ns, nonsignificant. Veh, vehicle.
Levels of IL-6, IL-1Ra, and the neutrophil chemotactic factor chemokine (C-X-C motif) ligand 1 (CXCL-1) were determined in muscle and plasma 1 h after the endurance challenge. IL-1β levels were below detection at this time point. However, as shown in Fig. 1, in mice treated with IL-37, levels of IL-6 were reduced by 50% in the plasma (Fig. 1B; P = 0.01) and by 79% in muscle homogenates (Fig. 1C; P < 0.0001). In muscle of IL-37–treated mice, CXCL-1 was reduced by 45% (Fig. 1D; P = 0.001). IL-1Ra was also reduced by 21% (Fig. 1E; P = 0.04). We observed no significant changes in the levels of muscle IL-1α, which is constitutively present as a precursor in muscle cells (Fig. 1F).
IL-37 Improves Exercise Tolerance.
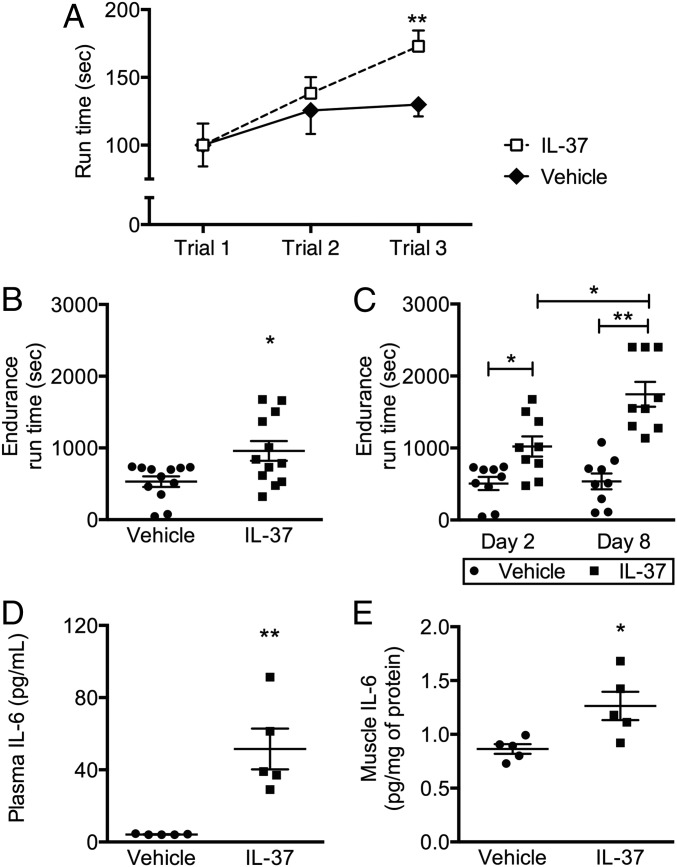
We next evaluated whether administration of IL-37 improved exercise tolerance in healthy mice. As shown in Fig. 2A, improved performance was clearly evident 1 day following IL-37 administration, at a time when mice were challenged with three consecutive tests of accelerating speed on the Rota-Rod apparatus. The performance of vehicle-treated mice initially improved because of learning of the testing; however, performance then reached a plateau. In contrast, mice receiving IL-37 exhibited a progressive improvement in the running time, with performance levels 33% higher than in vehicle-treated mice (P < 0.01). On day 2, mice treated with IL-37 exhibited an 82% increase in endurance running time compared with vehicle-treated mice (P = 0.01; Fig. 2B). We also challenged mice with treadmill stress testing and observed similar effects with IL-37 treatment (Fig. S1).
Fig. 2.
Effects of IL-37 treatment on physical performance. Mice receiving daily injections of IL-37 or vehicle control were subjected to accelerating Rota-Rod training sessions on day 1 and to an exercise tolerance test on day 2 and on day 8. (A) Mean ± SEM run time in seconds in three consecutive accelerating Rota-Rod training sessions (∼1 h apart). (B) Endurance run time in seconds on day 2. n = 12 mice per group. (C) Separate experiment for endurance run time in seconds on day 2 and day 8. n = 9 mice per group. (D) Circulating levels of IL-6 evaluated 1 h after the exercise tolerance test. (E) Muscle IL-6 1 h after the exercise tolerance test. n = 5 mice per group. Data expressed as mean ± SEM. Statistical significance evaluated with the Student’s unpaired t test and with the one-way ANOVA test. *P < 0.05, **P < 0.005.
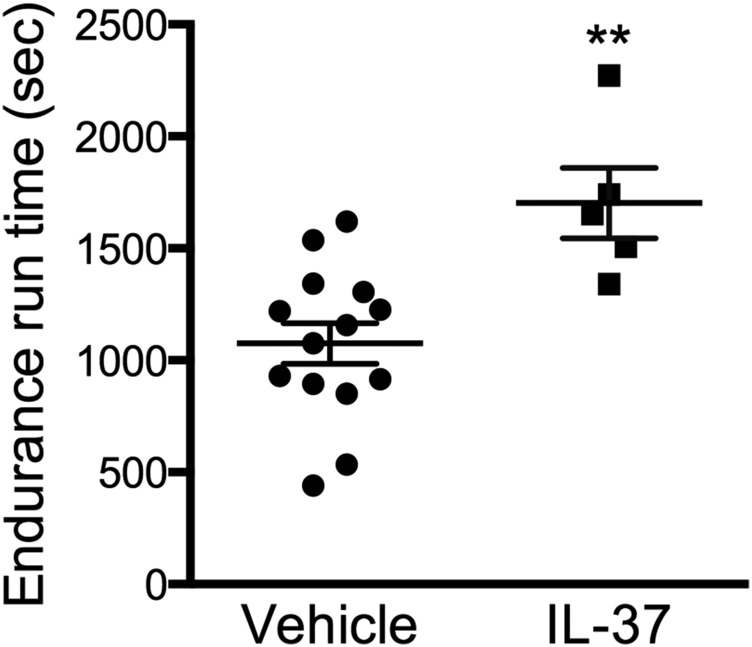
Fig. S1.
Effects of IL-37 treatment on physical performance on a treadmill. Mean ± SEM endurance run time on a treadmill in seconds. Statistical significance of differences was evaluated with the Student’s unpaired t test. **P < 0.005.
We then treated healthy mice with eight daily doses of 1 µg of IL-37, and exercise tolerance was assessed on days 2 and 8. As shown in Fig. 2C, on day 2, there was a 102% increase in the endurance run time of IL-37–treated mice, comparable to the improvement shown in Fig. 2B (P = 0.02). However, after eight daily doses of IL-37, we observed a 326% increase in endurance running time compared with vehicle-treated mice (P = 0.001). Compared with day 2, this finding represents a 71% further increase in endurance running time (P = 0.04).
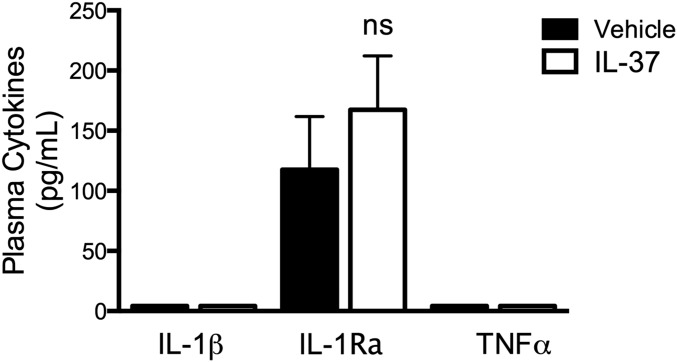
Cytokine levels were evaluated in plasma and in muscle homogenates 1 h after exercise tolerance testing. As shown in Fig. 2 D and E, levels of circulating and muscle IL-6 were moderately increased in mice treated with IL-37 (P = 0.003 and P = 0.04, respectively). This increase is consistent with production and release of IL-6 from skeletal muscle during exercise in humans (14). No significant differences were observed in the levels of circulating IL-1β, TNFα, and IL-1Ra (Fig. S2). We conclude that the effects of IL-37 in healthy mice do not solely depend on antiinflammatory properties.
Fig. S2.
Effects of IL-37 treatment on circulating cytokines. Mean ± SEM plasma levels of IL-1β, IL-1Ra, TNFα. Statistical significance of differences between groups was evaluated with the one-way ANOVA test. *P < 0.05, ns, nonsignificant.
AMP-Activated Protein Kinase and IL-1R8 Mediate the Effects of IL-37 on Exercise Tolerance.
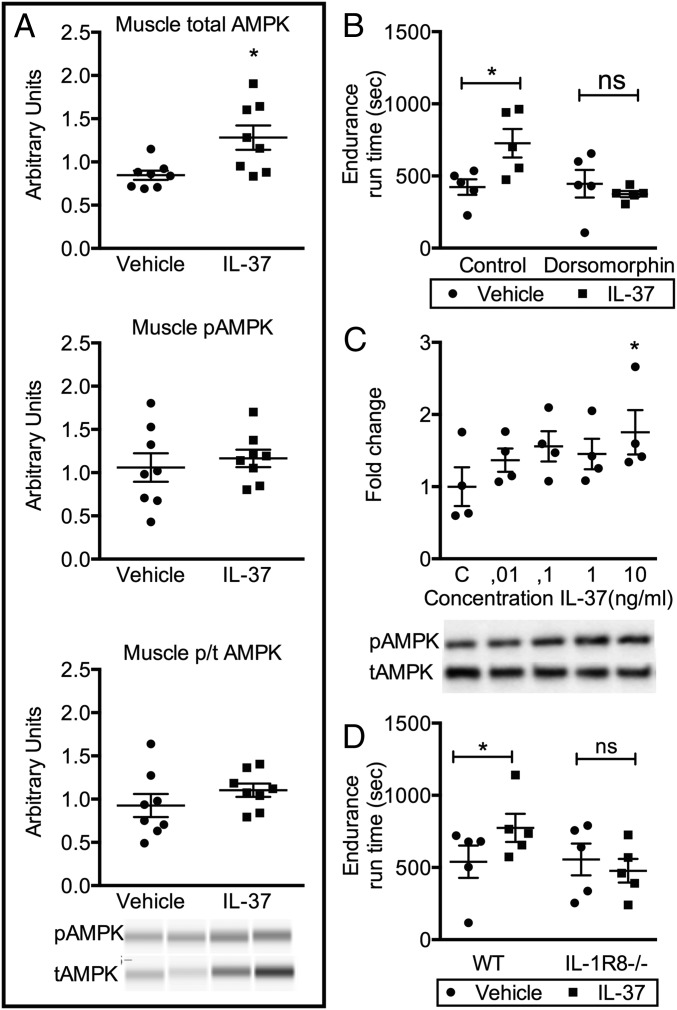
We reported that IL-37 increases AMP-activated protein kinase (AMPK) in adipocytes and macrophages (2, 4); we now investigated whether IL-37 increases AMPK in muscle tissue. First, we evaluated the effects of IL-37 treatment on muscle AMPK activation ex vivo. In gastrocnemius muscles of mice treated with IL-37, but not subjected to exercise, 8 days of IL-37 treatment significantly increased total AMPK (P = 0.01). However, at this time point, there was no significant difference in phosphorylated AMPK (Fig. 3A). Nevertheless, to assess a role for AMPK, we administered dorsomorphin (compound C), a transient inhibitor of AMPK (15, 16), to IL-37–treated mice 1 h before the exercise challenge. We observed that the increase in endurance run time of IL-37–treated mice was significantly reduced with inhibition of AMPK (Fig. 3B), whereas the performance of vehicle-treated mice was unaffected. We next examined the effect of IL-37 on AMPK in differentiated C2C12 mouse muscle cells in vitro. Short-term treatment with IL-37 for 1 h increased phosphorylated AMPK (Fig. 3C).
Fig. 3.
IL-37 activates the IL-1R8/AMPK axis. (A) In vivo levels of total AMPK, phosphorylated AMPK, and relative ratio in m. gastrocnemius (n = 8 mice per group). (B) Decline in exercise tolerance after in vivo inhibition of AMPK with a single i.p. dose of 0.2 mg/kg dorsomorphin 1 h before testing (n = 5 mice per group). (C) Western Blot and relative ratio for phospho-AMPK and total AMPK in differentiated C2C12 muscle cells stimulated with IL-37; total of four separate experiments. (D) Exercise tolerance test for WT or IL-1R8−/− mice treated with vehicle or IL-37 (n = 5 mice per group). Data expressed as mean ± SEM. Statistical significance evaluated with the Student’s unpaired t test and with the one-way ANOVA test. *P < 0.05, ns, nonsignificant. pAMPK, phosphorylated AMPK; tAMPK, total AMPK.
Deficiency of the IL-1R8 (formerly TIR8 or SIGIRR) in mice results in a hyperinflammatory phenotype (reviewed in ref. 8), and this receptor is required for the antiinflammatory properties of IL-37 (6, 7, 9). Mice deficient for IL-1R8 have similar baseline exercise tolerance as WT mice. However, treatment with IL-37 before Rota-Rod testing did not result in any improvement in IL-1R8–deficient mice (Fig. 3D), consistent with the requirement of IL-1R8 for the function of IL-37.
IL-37 Increases Mitochondrial Respiration in Skeletal Muscle.
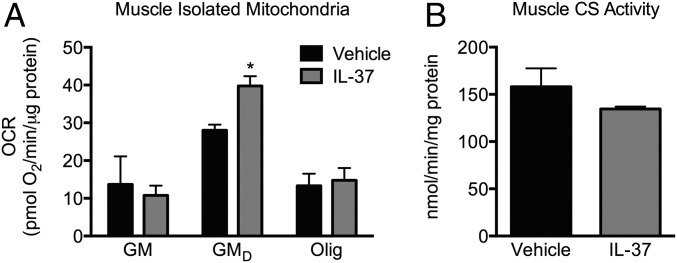
Activation of AMPK stimulates mitochondrial biogenesis and increases mitochondrial density and/or function in muscle (17). We therefore investigated whether treatment with IL-37 affected mitochondrial function. Fresh skeletal muscle mitochondria were isolated from the gastrocnemii of mice treated for 8 days with either IL-37 or vehicle but not subjected to an exercise challenge. As shown in Fig. 4A, there was a 25% increase in the state 3 oxygen consumption rate (OCR) in mitochondria isolated from IL-37–treated mice compared with vehicle-treated mice (P = 0.01). The OCR was assessed in the presence of glutamate + malate + ADP (GMD), representing oxidative phosphorylation substrate flux. State 4 (or basal) respiration in the presence of glutamate + malate (GM) was not different, nor was respiration in the presence of oligomycin (OLIG). These data indicate that basal respiration and proton leak were similar in IL-37– and vehicle-treated mice; however, oxidative phosphorylation (Fig. 4A; GMD) was increased only in IL-37–treated mice. Because IL-37 treatment did not affect proton leak, the data suggest that IL-37 does not increase metabolic capacity or metabolic rate by uncoupling mitochondrial oxidative respiration. Rather, IL-37 increases oxidative phosphorylation substrate flux.
Fig. 4.
IL-37 increases oxidative phosphorylation substrate flux. Oxygen consumption rate was evaluated by using isolated mitochondria from m. gastrocnemius of mice treated with IL-37 for 8 days. (A) Respiration rates under described substrate conditions. (B) Citrate synthase activity, measured as an index of mitochondrial content. Data expressed as mean ± SEM. n = 4 mice per group. Statistical significance evaluated with the Student’s unpaired t test and with the one-way ANOVA test. *P < 0.05. GM, glutamate + malate; GMD, glutamate + malate + ADP; OCR, oxygen consumption rate; Olig, oligomycin.
We next measured mitochondrial citrate synthase (CS) activity to determine whether changes in mitochondrial content account for IL-37-induced increases in oxidative phosphorylation (GMD). CS activity was not different between vehicle- and IL-37–treated mice (Fig. 4B). With mitochondrial protein content normalized, these data, together with measurement of oxidative phosphorylation, reveal that the increase in oxidative phosphorylation (Fig. 4A; GMD) is likely due to qualitative changes in mitochondrial respiration, rather than increased mitochondrial content.
IL-37 Treatment Induces Increased Amino Acid Catabolism and Nucleoside/Phosphocreatine Synthesis.
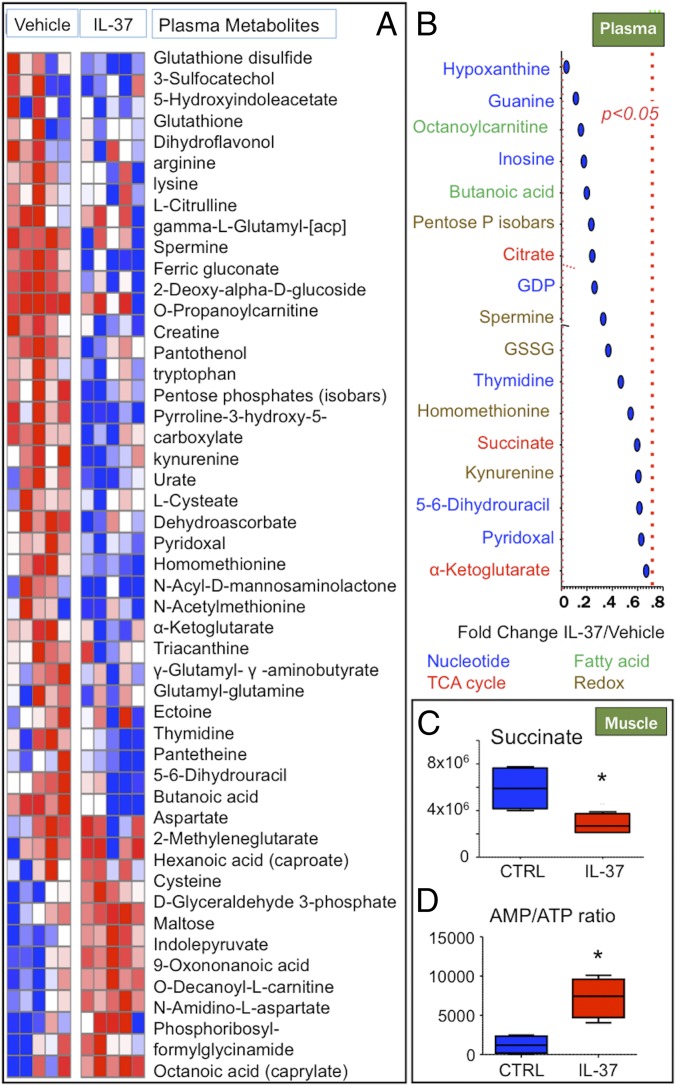
Because AMPK plays a key role in metabolic reprogramming (18, 19), metabolomic analyses was performed on m. gastrocnemius, plasma, and red blood cells from vehicle-treated and IL-37–treated mice. IL-37 treatment was associated with a decrease (P < 0.05) in circulating levels of nucleotides and nucleotide derivatives (particularly hypoxantine, guanine, and inosine) and oxidative stress-related metabolites (ribose phosphate and isobaric pentose phosphate compounds, oxidized glutathione, kynurenine, and spermine (Fig. 5 A and B). Notably, Krebs cycle intermediates citrate, α-ketoglutarate, and succinate were significantly (P < 0.05) lower in plasma and muscle from IL-37–treated mice (Fig. 5 B and C), as reported with reduced inflammation (20). Increases in AMP/ATP ratios trigger AMPK (21). Also in muscle, we observed increased AMP/ATP ratios in muscle from IL-37–treated mice (Fig. 5D).
Fig. 5.
Metabolome changes upon treatment with IL-37. M. gastrocnemius, red blood cells, and plasma were analyzed for metabolic profiles. (A) Heatmap for metabolites in plasma. (B) Significant plasma metabolites and their respective fold change IL-37/Control. (C) Succinate levels in muscle. (D) AMP/ATP ratio in muscle. n = 5 mice per group. Statistical significance evaluated with the Student’s unpaired t test. *P < 0.05.
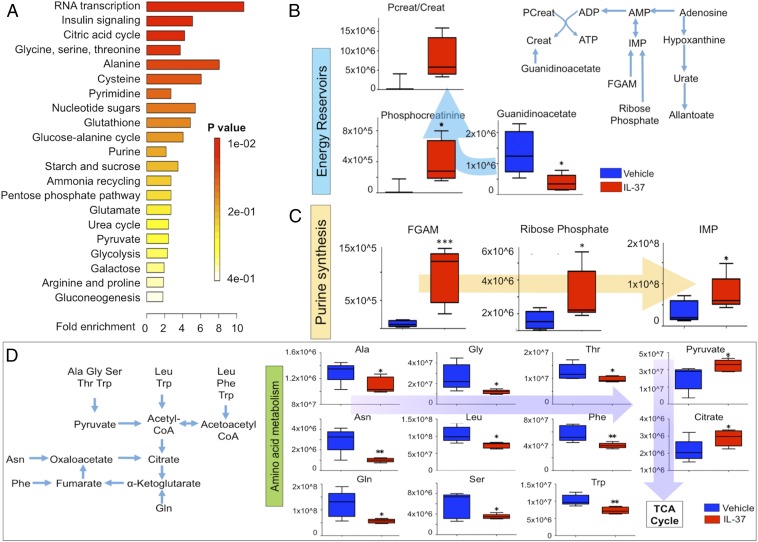
Top up-regulated pathways further suggested an increase in citric acid cycle and nucleoside and amino acid metabolism in the muscle of IL-37–treated mice (Fig. 6A). As shown in Fig. 6B, mice receiving IL-37 exhibited higher levels of phosphocreatine and higher phosphocreatine/creatine ratios compared with vehicle-treated mice. Also, steady-state levels of guanidinoacetate, a precursor for creatine, were lower in the muscle of IL-37 mice. Steady-state decreases of the precursor guanidinoacetate and increased levels of the final product, phosphocreatine, are indicative of increased fluxes through this anabolic pathway. As shown in Fig. 6C, total purine levels, including precursors phosphoribosylglycinamide (FGAM), ribose phosphate, and inosine monophosphate (IMP) were significantly increased by IL-37 treatment. IL-37 monotherapy also resulted in lower levels of amino acids, which serve as substrates to fuel pyruvate and citrate. Indeed, these Krebs cycle substrates were significantly increased in this group (P < 0.05; Fig. 6D).
Fig. 6.
Changes in energy reservoirs and amino acid catabolism in muscle of IL-37–treated mice. (A) MetaboAnalyst elaboration of the metabolic pathways up-regulated in muscles of IL-37–treated mice indicated an increase in citric acid cycle, amino acid metabolism, nucleoside (purine and pyrimidine), phosphocreatine, and glutathione homeostasis. (B) Phosphocreatine synthesis, phosphocreatine/creatine ratios. (C) Purine synthesis intermediates and products in IL-37 mouse muscles in comparison with controls. (D) Amino acids can fuel energy metabolism by providing substrates for late glycolysis and citric acid cycle at different levels. Free muscle amino acid levels decreased in IL-37–treated mice, whereas pyruvate and citrate levels increased. n = 5 mice per group. Statistical significance evaluated with the Student’s unpaired t test. *P < 0.05, **P < 0.005. Creat, creatine; PCreat, phosphocreatine.
Discussion
In this study, we demonstrate that activation of the AMPK pathway by IL-37 improves exercise tolerance with a dual mechanism of suppression of inflammation and modulation of metabolic pathways. The effects of IL-37 treatment on exercise tolerance were first evaluated during systemic inflammation induced by the administration of low-dose LPS (Fig. 1). Treatment with IL-37 reduced muscle and plasma levels of inflammatory cytokines and normalized endurance running performance. With suppression of systemic inflammation by IL-37 (1), it was not unexpected that exercise tolerance would improve upon IL-37 treatment during an inflammatory state. Additionally, however, there may be mechanisms of IL-37 action beyond suppression of inflammation that we investigated.
We did not expect that IL-37 treatment would improve exercise performance in healthy mice not subjected to LPS challenge (Fig. 2). IL-37–treated mice exhibited a marked increase in endurance run time, which improved further upon additional treatment with IL-37. These effects of IL-37 on exercise in healthy mice were not secondary to suppression of the inflammatory response: Indeed, in mice treated with IL-37, we observed a modest increase in muscle and circulating IL-6. Such increases are 100-fold lower compared with those observed during systemic inflammation (Figs. 1B and 2D) and reflect the known release of IL-6 from muscle during exercise (14).
The present study further suggests that the IL-1 family receptor IL-1R8 may be implicated in the transduction of the metabolic effects of IL-37, because the increase in exercise tolerance upon IL-37 treatment was absent in healthy mice deficient for this receptor (Fig. 3). IL-1R8 is required for the antiinflammatory effects of IL-37 by inhibiting the NFκB and cJun N-terminal kinases pathways (6, 7, 9).
Recombinant IL-37 directly activates AMPK (2), a central regulator of cellular energy homeostasis and exercise-regulated metabolism (reviewed in ref. 22). AMPK regulates several biochemical pathways to modulate energy expenditure and substrate utilization in response to various stresses, particularly in cancer (23), inflammatory diseases (24), and exercise (25). Here, we show that IL-37 activates AMPK specifically in muscle cells and that activation of AMPK mediates the improvement in physical performance induced by IL-37 in vivo. These findings are consistent with our previous observations that IL-37 activates AMPK in myeloid and nonmyeloid cells (2, 7). Specific pharmacologic blockade of AMPK precluded the benefit of IL-37 treatment in healthy mice.
Activation of AMPK stimulates mitochondrial biogenesis and function (17). In freshly isolated mitochondria from gastrocnemius muscles of mice treated with IL-37, we observed a significant increase in oxidative phosphorylation substrate flux, which was not secondary to differences in proton leak, nor associated with an increase in mitochondrial content in the same muscles. We conclude that the increased mitochondrial respiration in the muscles of IL-37–treated mice reflects qualitative changes in mitochondrial function, not content or quantity.
IL-37 treatment resulted in an increase in AMP/ATP ratio associated with reduced levels of succinate, a potent proinflammatory mediator typically elevated during anaerobic glycolysis and inflammatory states (20, 26, 27) (Fig. 5 C and D). These findings are related and consequential to the observed activation of AMPK. Specifically, activation of AMPK is known to follow increased AMP/ATP ratios, as observed during accelerated ATP consumption (e.g., muscle contraction) (21, 25), and result in increased oxidative phosphorylation and reduced levels of the proinflammatory mediator succinate (reviewed in ref. 24). Each of these mechanistic processes adds to the understanding of the improved exercise tolerance in mice treated with IL-37.
AMPK is also known to play a primary role in metabolic reprogramming (18, 19), and treatment with IL-37 is associated with marked metabolic changes (Figs. 5 and 6). For example, a decrease in oxidative stress-related metabolites with a corresponding increase in the antioxidant glutathione was observed. The production of reactive oxygen species during exercise promotes muscle contractile dysfunction, whereas administration of antioxidant agents delays muscle fatigue (reviewed in ref. 28). Thus, the antioxidant effects of IL-37 are consistent with the observed increase in exercise tolerance. Additional metabolic changes induced by IL-37 as depicted in Figs. 5 and 6 may represent contributing factors to the increase in exercise tolerance. These factors include phenomena augmenting muscle reserves and energy generation, such as catalysis of amino acid and synthesis of nucleosides and phosphocreatine, or consistent with increased AMPK activation and mitochondrial respiratory capacity, such as a decrease in the muscle levels of pyruvate, citrate, and hypoxanthine (29–31).
In summary, the present data demonstrate that IL-37 increases exercise tolerance by inducing metabolic reprogramming via activation of AMPK: Downstream effects include increased mitochondrial respiration, changes in redox state, increased oxidative phosphorylation, and reduction of proinflammatory mediators. Production of proinflammatory cytokines is associated with fatigue and decreased physical activity, as exemplified by the lethargy experienced during acute infections or chronic inflammatory diseases (10). Thus, the implications of the present findings impact on patients with chronic inflammatory diseases spanning from rheumatoid arthritis to cancer, in which fatigue is often incapacitating. Confirmation to the crucial role of cytokines in human fatigue comes from clinical experience: For example, inhibition of IL-1 reduces fatigue in patients with rheumatologic conditions (32, 33).
It was not unexpected that by inhibiting cytokine production, exogenous IL-37 would curb fatigue and ameliorate exercise tolerance. However, broad metabolic effects yielded an improvement in exercise tolerance even in healthy, unchallenged mice. This study demonstrates that administration of recombinant IL-37 ameliorates fatigue and improve exercise tolerance, via a dual mechanism of action of modulation of inflammation and metabolic reprogramming. In summary, the findings provide rationale for exploring the use of recombinant IL-37 in the treatment of inflammation-induced fatigue.
Methods
Mice.
Male C57BL/6 mice, 8–10 wk of age, were purchased from Jackson Laboratories. IL-1R8 deficient were generated as reported (34). Mice were age- and sex-matched and between 22 and 26 g of weight.
Recombinant IL-37 Purification.
IL-37 residues 46–218 were cloned into a pET21 vector (Novagen) with an N-terminal 6xHis tag and thrombin cleavage site. Protein was expressed in BL21/DE3 cells and purified via Ni affinity chromatography. Eluted fractions containing IL-37 were dialyzed into 50 mM Tris, pH 7.2, 100 mM NaCl, 1 mM EDTA, and applied onto an SP ion exchange using SP fast-flow resin (GE Healthcare). SP ion exchange eluted fractions were concentrated and cleaved with thrombin to remove the 6xHis tag for a final application to size-exclusion chromatography by using a Superdex-75 (GE Healthcare).
IL-37 and Other Treatments.
For doses and timing of injections, SI Methods.
Rota-Rod and Treadmill Testing.
Exercise tolerance was assessed by using two different methods: a rotating rod device (Rota-Rod, Ugo Basil) (13) and a treadmill Exer 3/6 model (Columbus Instruments) (35). SI Methods.
Tissue Processing and Cytokine Determinations.
Cell Culture.
Mitochondrial Respiration and Citrate Synthase Activity.
SI Methods for details on mitochondrial isolation (36), respiration experiments with the Seahorse Flux Analyzer (Seahorse Bioscience), and CS activity assay (37).
Western Blot.
Metabolomics Studies.
Targeted metabolomics analyses were performed as reported (38). Plasma (20 µL), red blood cells (100 µL of buffy-coat depleted packed erythrocytes) and m. gastrocnemius muscles (10 mg) were extracted in 1 mL of ice-cold lysis/extraction buffer (methanol:acetonitrile:water 5:3:2). After discarding protein pellets, water and methanol soluble fractions were injected into a C18 reversed phase column (phase A: water, 0.1% formic acid; B: acetonitrile, 0.1% formic acid - Phenomenex) through an ultra-high performance chromatographic system (UHPLC, Ultimate 3000; Thermo Fisher). UHPLC was coupled online with a high-resolution quadrupole Orbitrap instrument run in either polarity modes (QExactive, Thermo Fisher) at 70,000 resolution (at 200 m/z). Maven software (Princeton), KEGG pathway database, and an in-house validated standard library (>650 compounds; Sigma Aldrich; IROATech) were used for metabolite assignment and peak integration for relative quantitation. Integrated peak areas were exported into Excel (Microsoft) and elaborated for statistical analysis (t test, ANOVA) and hierarchical clustering analysis through the software GraphPad Prism (GraphPad Software) and GENE E (Broad Institute). Top up- and down-regulated metabolic pathways were determined through MetaboAnalyst 3.0 (www.metaboanalyst.ca/MetaboAnalyst/).
Statistics.
Study Approval.
The Institutional Animal Care and Use Committees of the University of Colorado Denver, Aurora, CO, approved the studies.
SI Methods
IL-37 and Other Treatments.
LPS (Sigma-Aldrich) was injected intraperitoneally (i.p.) at a dose of 10 µg per mouse (∼0.33 mg/kg), 4 h before testing (39). Treatments, administered i.p. in 200 µL of saline vehicle, were anakinra (Kineret, Swedish Orphan Biovitrum), water-soluble dorsomorphin (Compound C, Abcam), and a recombinant form of the naturally occurring human IL-37 isoform b with the N terminus at valine 46 and C terminus at 218. IL-37 was injected i.p. in three separate doses (1 µg per mouse per dose, ∼40 µg/kg) 24, 12, and 2 h before exercise testing.). Anakinra (IL-1Ra) was used as a treatment control at a single i.p. dose of 50 mg/kg (∼1.25 mg per mouse), administered 2 h before exercise testing.
Rota-Rod and Treadmill Testing.
Exercise tolerance was assessed by using two different methods: a rotating rod device (Rota-Rod, Ugo Basile) and a treadmill Exer 3/6 model (Columbus Instruments). Testing spanned over 2 or 8 days, by a protocol reported (13). Briefly, on day 1, mice were placed on the Rota-Rod accelerating from 4 to 40 rpm over the course of 5 min, with a maximum time limit set at 6 min (360 s). Three trials with an intertrial interval of ∼1 h were performed. During each trial, the accelerating Rota-Rod run time was recorded as time to fall in seconds. Endurance testing was performed on day 2 and/or on day 8, with mice placed on the Rota-Rod at incremental speeds equivalent to 25% (refresh, 2 min), 50% (warm-up, 5 min), 75% (endurance phase 1), and 100% (endurance phase 2) of the maximum accelerating Rota-Rod speed recorded on day 1. Endurance was measured as the latency to fall due to exhaustion during the endurance phases.
The treadmill horizontal belt was started at a slow speed (7 m/min), which was gradually increased by 1 m/min after a 5-min warm-up phase to acclimatize the animals. Treadmill endurance was defined as (i) more than 5 consecutive seconds on the shock grid without attempting to reengage the treadmill, (ii) more than 50% of time spent on the shock grid, or (iii) more than 2 s spent on the grid for three times (35).
Tissue Processing and Cytokine Determinations.
Mice were killed 1 h after the endurance tests. Blood was collected by orbital bleeding in EDTA-containing tubes, and plasma was obtained by centrifugation at 1,000 × g for 5 min. Muscles (m. quadriceps and m. gastrocnemius) were surgically removed and immediately frozen in liquid nitrogen. The samples were processed by using homogenization in RIPA buffer (Sigma-Aldrich) containing a PhosSTOP phosphatase inhibitor and complete ULTRA proteinase inhibitor mixture (Roche Diagnostics), and centrifuged at 20,000 × g for 20 min. Protein content in the supernatants was assessed with the Bradford Protein Assay (Bio-Rad Laboratories). Cytokine concentrations were determined by using specific ELISA (BioTechne); for muscle lysates, the values were normalized for protein content.
Cell Culture and Differentiation.
C2C12 cells were grown in DMEM supplemented with 10% FCS and Penicilin/Streptomycin. After growing to confluency, cells were cultured in DMEM with 2% horse serum for 3–5 additional days to enable differentiation toward muscle cells. After differentiation, cells were treated with increasing concentrations of recombinant IL-37 for 1 h.
Mitochondrial Respiration and Citrate Synthase Activity.
For mitochondrial isolation, 50 mg of freshly isolated gastrocnemius muscles were first placed in ice-cold Chappel-Perry buffer (100 mM KCl, 50 mM Mops, 0.5 mM EGTA, 5 mM MgSO4, and 1 mM ATP, pH 7.4 with KOH) and thoroughly minced. Mitochondria were isolated as described (36). Protein concentration of isolated mitochondria was determined by Bradford assay. Mitochondria were placed in Seahorse Flux Analyzer XF-24 culture plates at 3 µg per well (Seahorse Bioscience) in KCl-based respiration buffer. Respiration experiments were performed in triplicates per animal with sequential compound additions: 10 mM glutamate + 2 mM malate (GM), 4 mM ADP (GMD), 3 µM oligomycin (OLIG). Respiratory control ratios (GMD/GM) averaged 3.7 ± 1.1. As an index of mitochondrial content, CS activity was assayed spectrophotometrically from mitochondrial-enriched supernatants (post 600 × g) prepared from frozen m. gastrocnemius muscles as described (37). CS activity was normalized to the total protein content of the supernatants.
Western Blot.
Cell lysates were prepared by using a standard lysis buffer [50 mM Tris (pH 7.4), 150 mM NaCl, 2 mM EDTA,1% Nonidet P-40, 50 mM NaF and 0.25% sodium deoxycholate] supplemented with protease and phosphatase inhibitors (Roche). Samples were separated on a precasted SDS gradient gel (Bio-Rad) and proteins were blotted on a membrane by using the Turboblot system (Bio-Rad). pAMPK and AMPK were detected by using antibodies from Cell Signaling. After incubation with a secondary antibody, HRP signals were visualized by using Clarity reagent (Bio-Rad) and a chemiluminescence detection system (Bio-Rad).
Statistics.
Data are shown in mean ± SEM. Before primary analysis of the motor function outcomes, normality of each variable was assessed with the Kolmogorov–Smirnov test. No outliers (greater than 3 SD) were identified for accelerating Rota-Rod or endurance run tasks. Analyses other than the metabolomic studies were performed as follows: Differences between groups were tested with the Student’s t test, and differences among more than two groups were tested with ANOVA, with post hoc Bonferroni tests using GraphPad Prism 6.0.
Acknowledgments
We thank Benjamin Swartzwelter, Isak W. Tengedal, and Tania Azam for assistance. These studies were supported by NIH Grant AI-15614 (to C.A.D.) and AG033534 (Wake Forest School of Medicine) and AG00027912 (University of Colorado Boulder). G.C. was supported by grants from the Interleukin Foundation; D.B.B. was supported by Glenn/AFAR and the Interleukin Foundation.
Footnotes
The authors declare no conflict of interest.
This article contains supporting information online at www.pnas.org/lookup/suppl/doi:10.1073/pnas.1619011114/-/DCSupplemental.
References
- 1.Dinarello CA, et al. Suppression of innate inflammation and immunity by interleukin-37. Eur J Immunol. 2016;46(5):1067–1081. doi: 10.1002/eji.201545828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nold MF, et al. IL-37 is a fundamental inhibitor of innate immunity. Nat Immunol. 2010;11(11):1014–1022. doi: 10.1038/ni.1944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McNamee EN, et al. Interleukin 37 expression protects mice from colitis. Proc Natl Acad Sci USA. 2011;108(40):16711–16716. doi: 10.1073/pnas.1111982108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ballak DB, et al. IL-37 protects against obesity-induced inflammation and insulin resistance. Nat Commun. 2014;5:4711. doi: 10.1038/ncomms5711. [DOI] [PubMed] [Google Scholar]
- 5.Cavalli G, et al. Treating experimental arthritis with the innate immune inhibitor interleukin-37 reduces joint and systemic inflammation. Rheumatology (Oxford) 2016;55(12):2220–2229. doi: 10.1093/rheumatology/kew325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Moretti S, et al. IL-37 inhibits inflammasome activation and disease severity in murine aspergillosis. PLoS Pathog. 2014;10(11):e1004462. doi: 10.1371/journal.ppat.1004462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nold-Petry CA, et al. IL-37 requires the receptors IL-18Rα and IL-1R8 (SIGIRR) to carry out its multifaceted anti-inflammatory program upon innate signal transduction. Nat Immunol. 2015;16(4):354–365. doi: 10.1038/ni.3103. [DOI] [PubMed] [Google Scholar]
- 8.Molgora M, Barajon I, Mantovani A, Garlanda C. Regulatory role of IL-1R8 in immunity and disease. Front Immunol. 2016;7:149. doi: 10.3389/fimmu.2016.00149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lunding L, et al. IL-37 requires IL-18Rα and SIGIRR/IL-1R8 to diminish allergic airway inflammation in mice. Allergy. 2015;70(4):366–373. doi: 10.1111/all.12566. [DOI] [PubMed] [Google Scholar]
- 10.Dantzer R, O’Connor JC, Freund GG, Johnson RW, Kelley KW. From inflammation to sickness and depression: When the immune system subjugates the brain. Nat Rev Neurosci. 2008;9(1):46–56. doi: 10.1038/nrn2297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cavalli G, Dinarello CA. Treating rheumatological diseases and co-morbidities with interleukin-1 blocking therapies. Rheumatology (Oxford) 2015;54(12):2134–2144. doi: 10.1093/rheumatology/kev269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cavalli G, Fallanca F, Dinarello CA, Dagna L. Treating pulmonary silicosis by blocking interleukin 1. Am J Respir Crit Care Med. 2015;191(5):596–598. doi: 10.1164/rccm.201412-2150LE. [DOI] [PubMed] [Google Scholar]
- 13.Justice JN, et al. Battery of behavioral tests in mice that models age-associated changes in human motor function. Age (Dordr) 2014;36(2):583–592. doi: 10.1007/s11357-013-9589-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Febbraio MA, Pedersen BK. Muscle-derived interleukin-6: Mechanisms for activation and possible biological roles. FASEB J. 2002;16(11):1335–1347. doi: 10.1096/fj.01-0876rev. [DOI] [PubMed] [Google Scholar]
- 15.Zhou G, et al. Role of AMP-activated protein kinase in mechanism of metformin action. J Clin Invest. 2001;108(8):1167–1174. doi: 10.1172/JCI13505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kim YM, et al. Compound C independent of AMPK inhibits ICAM-1 and VCAM-1 expression in inflammatory stimulants-activated endothelial cells in vitro and in vivo. Atherosclerosis. 2011;219(1):57–64. doi: 10.1016/j.atherosclerosis.2011.06.043. [DOI] [PubMed] [Google Scholar]
- 17.Winder WW, et al. Activation of AMP-activated protein kinase increases mitochondrial enzymes in skeletal muscle. J Appl Physiol (1985) 2000;88(6):2219–2226. doi: 10.1152/jappl.2000.88.6.2219. [DOI] [PubMed] [Google Scholar]
- 18.Mihaylova MM, Shaw RJ. The AMPK signalling pathway coordinates cell growth, autophagy and metabolism. Nat Cell Biol. 2011;13(9):1016–1023. doi: 10.1038/ncb2329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Towler MC, Hardie DG. AMP-activated protein kinase in metabolic control and insulin signaling. Circ Res. 2007;100(3):328–341. doi: 10.1161/01.RES.0000256090.42690.05. [DOI] [PubMed] [Google Scholar]
- 20.Mills E, O’Neill LA. Succinate: A metabolic signal in inflammation. Trends Cell Biol. 2014;24(5):313–320. doi: 10.1016/j.tcb.2013.11.008. [DOI] [PubMed] [Google Scholar]
- 21.Wang W, Yang X, López de Silanes I, Carling D, Gorospe M. Increased AMP:ATP ratio and AMP-activated protein kinase activity during cellular senescence linked to reduced HuR function. J Biol Chem. 2003;278(29):27016–27023. doi: 10.1074/jbc.M300318200. [DOI] [PubMed] [Google Scholar]
- 22.Hardie DG, Ross FA, Hawley SA. AMPK: A nutrient and energy sensor that maintains energy homeostasis. Nat Rev Mol Cell Biol. 2012;13(4):251–262. doi: 10.1038/nrm3311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Faubert B, Vincent EE, Poffenberger MC, Jones RG. The AMP-activated protein kinase (AMPK) and cancer: Many faces of a metabolic regulator. Cancer Lett. 2015;356(2 Pt A):165–170. doi: 10.1016/j.canlet.2014.01.018. [DOI] [PubMed] [Google Scholar]
- 24.O’Neill LA, Hardie DG. Metabolism of inflammation limited by AMPK and pseudo-starvation. Nature. 2013;493(7432):346–355. doi: 10.1038/nature11862. [DOI] [PubMed] [Google Scholar]
- 25.Hardie DG. AMP-activated protein kinase: An energy sensor that regulates all aspects of cell function. Genes Dev. 2011;25(18):1895–1908. doi: 10.1101/gad.17420111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fedotcheva NI, Sokolov AP, Kondrashova MN. Nonezymatic formation of succinate in mitochondria under oxidative stress. Free Radic Biol Med. 2006;41(1):56–64. doi: 10.1016/j.freeradbiomed.2006.02.012. [DOI] [PubMed] [Google Scholar]
- 27.Tannahill GM, et al. Succinate is an inflammatory signal that induces IL-1β through HIF-1α. Nature. 2013;496(7444):238–242. doi: 10.1038/nature11986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Powers SK, Jackson MJ. Exercise-induced oxidative stress: Cellular mechanisms and impact on muscle force production. Physiol Rev. 2008;88(4):1243–1276. doi: 10.1152/physrev.00031.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Saraslanidis P, et al. Muscle metabolism and performance improvement after two training programmes of sprint running differing in rest interval duration. J Sports Sci. 2011;29(11):1167–1174. doi: 10.1080/02640414.2011.583672. [DOI] [PubMed] [Google Scholar]
- 30.Williams M. Dietary supplements and sports performance: Amino acids. J Int Soc Sports Nutr. 2005;2:63–67. doi: 10.1186/1550-2783-2-2-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zielinski J, Kusy K. Training-induced adaptation in purine metabolism in high-level sprinters vs. triathletes. J Appl Physiol (1985) 2012;112(4):542–551. doi: 10.1152/japplphysiol.01292.2011. [DOI] [PubMed] [Google Scholar]
- 32.Omdal R, Gunnarsson R. The effect of interleukin-1 blockade on fatigue in rheumatoid arthritis--a pilot study. Rheumatol Int. 2005;25(6):481–484. doi: 10.1007/s00296-004-0463-z. [DOI] [PubMed] [Google Scholar]
- 33.Cavalli G, et al. Efficacy and safety of biological agents in adult-onset Still’s disease. Scand J Rheumatol. 2015;44(4):309–314. doi: 10.3109/03009742.2014.992949. [DOI] [PubMed] [Google Scholar]
- 34.Garlanda C, et al. Intestinal inflammation in mice deficient in Tir8, an inhibitory member of the IL-1 receptor family. Proc Natl Acad Sci USA. 2004;101(10):3522–3526. doi: 10.1073/pnas.0308680101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bunnell TM, Jaeger MA, Fitzsimons DP, Prins KW, Ervasti JM. Destabilization of the dystrophin-glycoprotein complex without functional deficits in alpha-dystrobrevin null muscle. PLoS One. 2008;3(7):e2604. doi: 10.1371/journal.pone.0002604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Palmer JW, Tandler B, Hoppel CL. Biochemical properties of subsarcolemmal and interfibrillar mitochondria isolated from rat cardiac muscle. J Biol Chem. 1977;252(23):8731–8739. [PubMed] [Google Scholar]
- 37.Boyle KE, Newsom SA, Janssen RC, Lappas M, Friedman JE. Skeletal muscle MnSOD, mitochondrial complex II, and SIRT3 enzyme activities are decreased in maternal obesity during human pregnancy and gestational diabetes mellitus. J Clin Endocrinol Metab. 2013;98(10):E1601–E1609. doi: 10.1210/jc.2013-1943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.D’Alessandro A, Nemkov T, Hansen KC, Szczepiorkowski ZM, Dumont LJ. Red blood cell storage in additive solution-7 preserves energy and redox metabolism: A metabolomics approach. Transfusion. 2015;55(12):2955–2966. doi: 10.1111/trf.13253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Godbout JP, et al. Exaggerated neuroinflammation and sickness behavior in aged mice following activation of the peripheral innate immune system. FASEB J. 2005;19(10):1329–1331. doi: 10.1096/fj.05-3776fje. [DOI] [PubMed] [Google Scholar]