SUMMARY
Vitamin D insufficiency is a worldwide epidemic affecting billions of individuals, including pregnant women and children. Despite its high incidence, the impact of active vitamin D3 (1,25(OH)D3) on embryonic development beyond osteo-regulation remains largely undefined. Here, we demonstrate that 1,25(OH)D3 availability modulates zebrafish hematopoietic stem and progenitor cell (HSPC) production. Loss of Cyp27b1-mediated biosynthesis or vitamin D receptor (VDR) function by gene knockdown resulted in significantly reduced runx1 expression and Flk1+cMyb+ HSPC numbers. Selective modulation in vivo and in vitro in zebrafish indicated that vitamin D3 acts directly on HSPCs, independent of calcium regulation, to increase proliferation. Notably, ex vivo treatment of human HSPCs with 1,25(OH)D3 also enhanced hematopoietic colony numbers, illustrating conservation across species. Finally, gene expression and epistasis analysis indicated that CXCL8 (IL-8) was a functional target of vitamin D3-mediated HSPC regulation. Together, these findings highlight the relevance of developmental 1,25(OH)D3 availability for definitive hematopoiesis and suggest potential therapeutic utility in HSPC expansion.
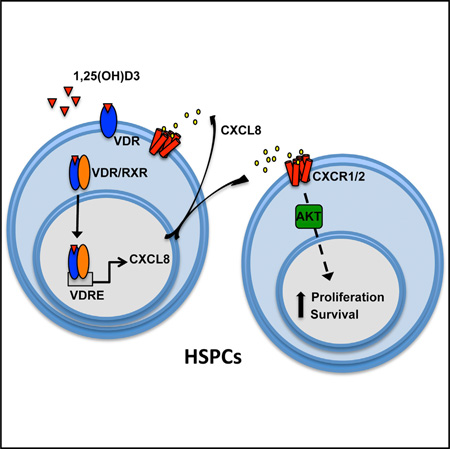
Graphical abstract
INTRODUCTION
Characterizing the impact of environmental modifiers on hematopoietic stem and progenitor cell (HSPC) formation and maintenance is of significant therapeutic interest because these extrinsic factors may influence both the onset and outcome of hematological disease. Active vitamin D (1,25(OH)D3), a fat-soluble hormone required for many physiological functions, is derived via sunlight and diet in humans. As such, factors including geographical location, lifestyle, and nutritional regimen can impact the level of vitamin D sufficiency. Recent studies indicate that vitamin D insufficiency is now a global epidemic, affecting over 1 billion people (Naeem, 2010). Among pregnant women, the worldwide incidence of 1,25(OH)D3 deficiency is estimated to be between 6% and 96% depending on geographical location and availability of supplementation (Weinert and Silveiro, 2015), with a particularly high occurrence in industrialized regions (40%–50%) (Bodnar et al., 2007). Severe 1,25(OH)D3 deficiency because of biosynthetic or signaling pathway mutations results in insufficient calcium (Ca2+) absorption and abnormal bone mineralization, leading to rickets in children and osteomalacia in adults. Interestingly, case studies of children with severe vitamin D deficiency present a variety of hematological disorders (Holick, 2006; Yetgin and Ozsoylu, 1982); however, the impact of vitamin D status on embryonic hematopoietic stem cell (HSC) production has not been elucidated.
De novo vitamin D synthesis begins with transformation of 7-dehydrocholesterol in the skin by UV radiation to the non-active vitamin D precursor cholecalciferol (D3). D3 is then modified by cytochrome P450 enzyme 2R1 (CYP2R1), primarily in the liver, to generate 25-hydroxy vitamin D (25(OH)D3, calcidiol), the circulating form of vitamin D. In the kidney, 25(OH)D3 is further hydroxylated by CYP27B1 to generate the active metabolite 1,25-dihydroxy vitamin D (1,25(OH)D3, calcitriol). 1,25(OH)D3 acts as a ligand for the vitamin D receptor (VDR), a member of the nuclear hormone receptor family (Mizwicki and Norman, 2009). Upon ligand binding, VDR forms a heterodimer with the retinoic acid X receptor (RXR), resulting in nuclear localization and transcriptional regulation of genes with vitamin D response elements (VDREs) (Plum and DeLuca, 2010). Genome-wide chromatin immunoprecipitation sequencing (ChIP-seq) studies identified more than 200 VDR-regulated genes (Ramagopalan et al., 2010). 1,25(OH)D3/VDR binding can also elicit non-genomic responses, including extracellular Ca2+ uptake (Norman, 2006).
In humans, mutations in genes of the vitamin D biosynthetic pathway are the most common cause of vitamin D-dependent rickets (VDDR), whereas VDR mutations result in hereditary vitamin D-resistant rickets (HVDR) (Holick, 2006). VDDR is treated with vitamin D supplementation, whereas HVDR is partially ameliorated with supplemental Ca2+. Children with vitamin D deficiency-associated rickets are clinically documented to exhibit a variety of hematopoietic defects, including anemia, extramedullary hematopoiesis, thrombocytopenia, myelofibrosis, and myelodysplasia. Some features improve with Ca2+ supplementation, suggestive of bone marrow (BM) niche dysregulation (Yetgin and Ozsoylu, 1982). Indeed, VDR loss in the mouse leads to extramedullary hematopoiesis because of abnormal bone mineralization (Jeanson and Scadden, 2010). In contrast, expression analyses indicate that VDR is one of 33 genes highly enriched in mouse HSCs (Riddell et al., 2014). VDR levels vary as immune cells mature, with monocytes/macrophages showing downregulation (Hewison et al., 2003) and T cells upregulation, respectively (Bruce and Cantorna, 2011). Subsets of T cells also express Cyp27b1, implying that local 1,25(OH)D3 synthesis may be important for T cell function (Ooi et al., 2014). Further, Cyp27b1-null mice show reductions in CD4 and CD8 T cells (Panda et al., 2001). Similar to mice, VDR is broadly expressed in human hematopoietic cells (Kizaki et al., 1991). Children with von Jaksch-Luzet syndrome, a severe vitamin D deficiency, are characterized by anemia with accumulation of erythroblasts and myeloblasts resembling chronic myeloid leukemia (Holick, 2006; Kassam et al., 1983). Despite multi-lineage abnormalities and frequent childhood onset, minimal investigation has been made into the impact of vitamin D status on developmental HSPC production.
Unlike adult HSPC homeostasis, which is strongly regulated by interactions with the BM microenvironment, embryonic hematopoiesis is initiated de novo in specialized vascular niches with transient hematopoietic potential (Carroll and North, 2014). Here we present a role for active vitamin D3 in embryonic HSPC production: 1,25(OH)D3 levels directly impact HSPC numbers in vivo and in vitro via VDR-mediated regulation of pro-proliferative responses independent of Ca2+ flux. Significantly, reduction in 1,25(OH)D3 production or function because of perturbations in biosynthetic or signaling genes decreased HSPCs in zebrafish embryos. In contrast, 1,25(OH)D3 supplementation expanded HSPCs in vivo and in vitro. Gene expression and epistasis studies indicated that 1,25(OH)D3 regulates cxcl8 (IL-8) signaling to control HSPC numbers. Finally, ex vivo treatment with 1,25(OH)D3 elicited significant elevations in survival, proliferation, and multi-lineage colony forming activity of CD34+ human umbilical cord blood HSCs. Together, these data highlight the conservation of 1,25(OH)D3 function in developmental HSC regulation and indicate the potential utility of 1,25(OH)D3 supplementation for HSPC expansion in clinical transplantation therapies.
RESULTS
VDR Signaling Is Essential for Hematopoietic Stem and Progenitor Cell Production
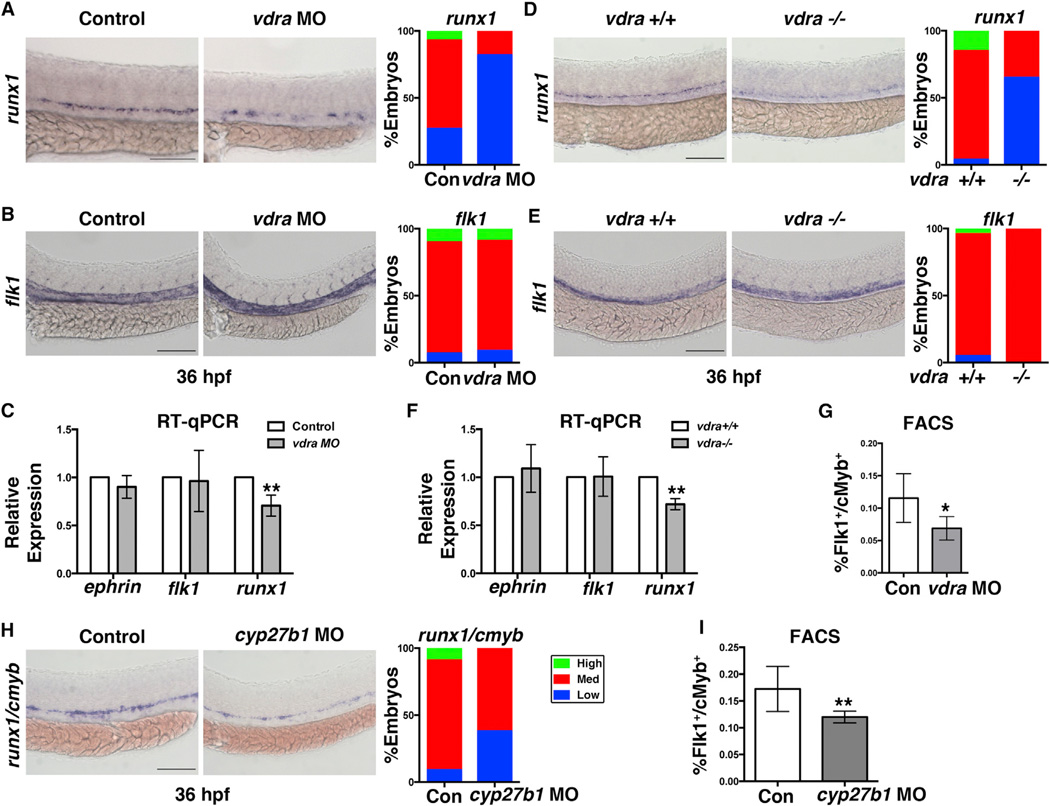
Despite case studies of hematological problems in children with severe 1,25(OH)D3 deficiency, the effects on embryonic hematopoiesis remain uncharacterized. Vitamin D was identified as a modulator of HSPC expression in a prior compound screen (North et al., 2007). We recently showed that accumulation of the inactive vitamin D precursor, cholecalciferol, negatively affected hemogenic endothelial formation independent of VDR activation by directly antagonizing Hedgehog signaling (Cortes et al., 2015). To investigate whether active 1,25(OH)D3-associated VDR signaling impacted definitive hematopoiesis, we examined the effect of VDR loss on HSPC development. The zebrafish genome encodes two VDRs, vdra and vdrb, with vdra alone acting as the canonical VDR in vivo (Lin et al., 2012). Fractions from Tg(flk1:dsRed;cmyb:GFP) embryos (1,000 embryos/sample × 3 replicate sorts) sorted with fluorescence-activated cell sorting (FACS) showed vdra expression in endothelial niche cells (Flk1:dsRed+/cMyb:GFP−) and HSPCs (Flk1:dsRed+/cMyb:GFP+) (Figure S1A). Morpholino (MO) knockdown of vdra strongly reduced runx1 expression in the aorta-gonad-meso-nephros (AGM) region 36 hr post fertilization (hpf) by whole-mount in situ hybridization (WISH) (Figure 1A) without overt defects in the vascular niche, as marked by flk1 (Figure 1B) and ephrinb2 (Figure S1B). This result was confirmed and quantified by qPCR analysis (runx1, p < 0.01; flk1, p = not significant [N.S.]; ephrinb2, p = N.S.) (Figure 1C). In contrast, vdrb knockdown had no effect on runx1 (Figure S1C). The specificity of the vdra MO was confirmed by splice product detection (Figure S1E) and rescued by addition of vdra, but not vdrb, mRNA (Figure S1F). Importantly, generation of a vdra mutant embryo by CRISPR-Cas9 genome editing (Figure S1G and S1H) resulted in the same phenotypic effects on both runx1 (decreased) and flk1 (unchanged) by WISH and qPCR (runx1, p < 0.01; flk1, p = N.S.; ephrinb2, p = N.S.) (Figures 1D-1F). Whole-embryo FACS quantification performed with the Tg(lmo2:GFP;gata1: dsRed) line to mark functional erythro-myeloid progenitors (EMPs) (Bertrand et al., 2007) and Tg(flk1:dsRed;cmyb:GFP) to mark HSPCs (Bertrand et al., 2010) indicated a 20% (p < 0.05) decrease at 30 hpf (Figure S1D) and 38% (p < 0.05) reduction by 48 hpf (Figure 1G), respectively, with vdra knockdown. Further, vdra morphants had sustained reductions in CD41:GFP+ HSCs colonizing the caudal hematopoietic tissue (CHT) at 72 hpf, as determined by fluorescence microscopy (Figure S1I) and FACS (Figure S1J ; p < 0.01). To confirm that the levels of vitamin D3/VDR activity correlated with embryonic HSPC output, the impact of reduced vitamin D synthesis was also examined. MO knockdown of cyp27b1, which controls the final hydroxylation step in 1,25(OH)D3 synthesis, diminished runx1/cmyb expression (Figure 1H). FACS analysis of cyp27b1 morphants confirmed a significant decrease (p < 0.01) in HSPCs (Figure 1I), consistent with a role for 1,25(OH)D3/VDR activity in embryonic HSPC production.
Figure 1. VDR Is Necessary for Zebrafish Definitive Hematopoiesis.
(A) Representative runx1 WISH images and qualitative phenotype distribution (high/medium/low, n ≥ 30 embryos/condition) of vdra MO-injected embryos and sibling controls at 36 hpf. Error bars, mean ± SD.
(B) WISH example and phenotype distribution for flk1 in vdra morphants (n ≥ 20 embryos/condition).
(C) qPCR analysis quantifying the impact on HSPCs (runx1, **p < 0.01) and hemogenic endothelium (flk1, ephrinb2, p = N.S.) in control and vdra morphants (30 embryos/sample 3 3 replicates).
(D–F) Representative WISH (D), phenotype distributions (E), and qPCR quantification (F) in vdra mutant embryos (runx1, **p < 0.01; flk1, ephrinb2, p = N.S.) phenocopied the impact on HSPCs but not on vessels.
(G) FACS analysis of vdra morphants indicated significant reductions in Flk1:dsRed+/cMyb:GFP+ HSPCs (*p < 0.05) at 48 hpf (5 embryos/sample 3 4 replicates/condition). Error bars, mean ± SD.
(H) WISH samples and phenotype distribution of runx1/cmyb expression in cyp27b1 MO-injected embryos at 36 hpf (n ≥ 30 embryos/condition).
(I) FACS analysis showed a significant decrease in HSPCs (**p < 0.01) with cyp27b1 MO injection (n value and error bars as in C).
Scale bars, 100 µm. See also Figure S1.
Vitamin D Supplementation Stimulates Embryonic HSPC Production
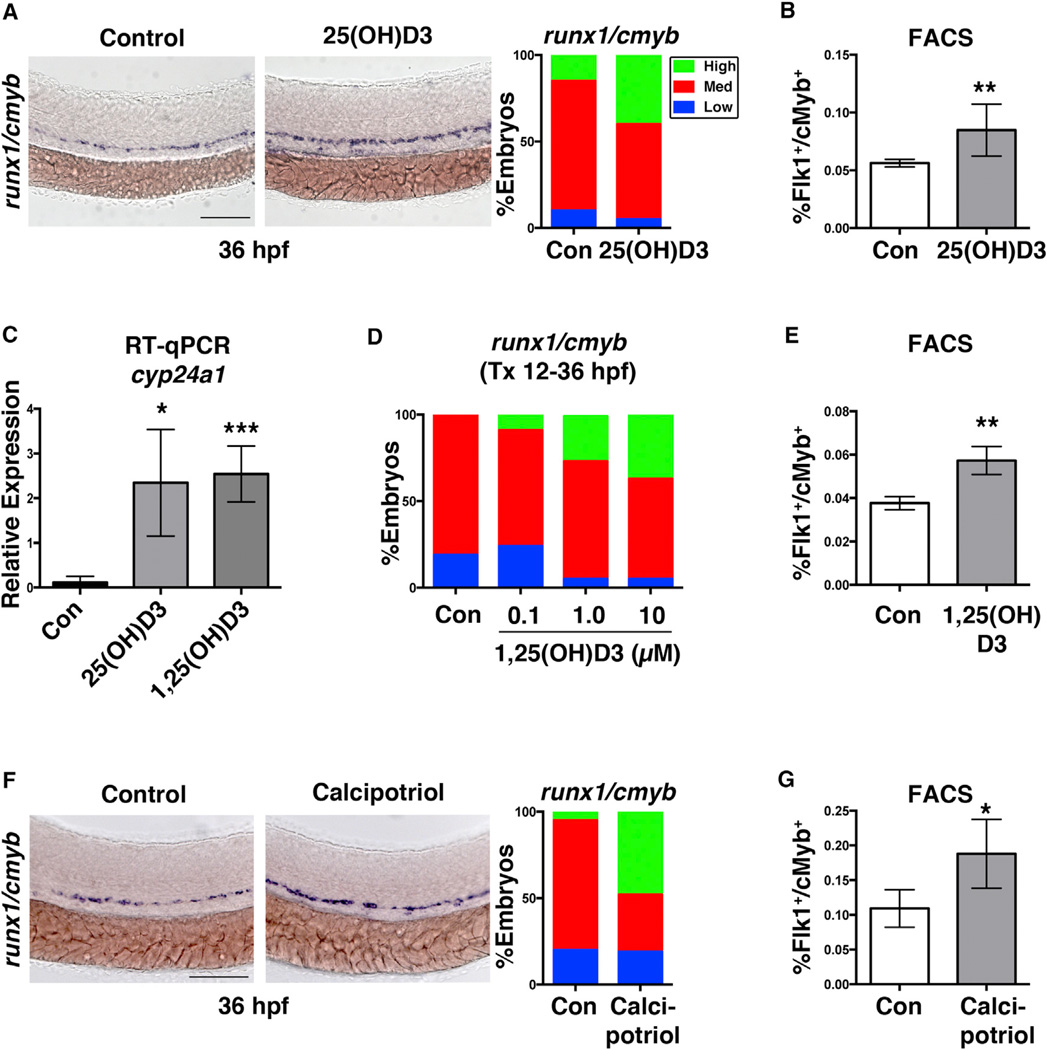
Because vitamin D synthesis and signaling appeared to be necessary for the establishment of normal embryonic HSPC numbers, we next examined whether supplementation was sufficient to stimulate production. We previously determined that cyp27b1 is expressed by 12 hpf (Cortes et al., 2015). Exposure to exogenous 25(OH)D3 (10 mM), the circulating form of vitamin D, enhanced runx1/cmyb expression (Figure 2A), which was confirmed and quantified as a 2-fold increase in Flk1+/cMyb+ HSPCs by FACS (p < 0.01; Figure 2B). Consistent with biosynthetic processing by Cyp27b1 and VDR activation, 25(OH)D3-treated embryos had elevated expression of the VDR target cyp24a1 by qPCR at 36 hpf (p < 0.05), similar to 1,25(OH)D3 (p < 0.001; Figure 2C). VDR activation was confirmed using a Tg(VDRE:mCherry) reporter line that showed enhanced mCherry expression in the AGM with both 25(OH)D3 and 1,25(OH)D3 exposure (Figure S2A). Likewise, FACS showed a significant increase in Flk1:GPF+/VDRE:mCherry+ cells with 1,25(OH)D3 (p < 0.0001; Figure S2B). To further examine correlations between active vitamin D3 levels and HSPC production, a dosage analysis was performed. A dose-responsive induction in the distribution of embryos with high runx1/cmyb expression was seen with 0.1–10 µM 1,25(OH)D3 exposure (Figure 2D). FACS quantification further revealed that exposure to 10 µM 1,25(OH)D3 caused a 25% (p < 0.01) increase in the number of EMPs at 30 hpf (Figure S2C) and a 20% (p < 0.01) increase in AGM-derived HSPCs at 48 hpf (Figure 2E). Together with enhanced HSPC production, a 2-fold increase in proliferation in the AGM was observed with 1,25(OH)D3 treatment (p < 0.001) compared with controls (Figure S2D) using the fluorescence ubiquitination cell cycle indicator (FUCCI) reporter Tg(EF1:mAG-zGEM(1/100) line (Sugiyama et al., 2009) crossed to Tg(flk1:dsred). In contrast, vdra knockdown caused a significant decrease in proliferation (p < 0.05; Figure S2E). Finally, to determine whether the effect of 1,25(OH)D3 was due to VDR-mediated transcriptional regulation or alterations in Ca2+ flux, embryos were treated with the vitamin D3 analog calcipotriol, documented to be 100-fold less calcemic than 1,25(OH)D3 (Binderup and Bramm, 1988).Calcipotriol (10 µM) shifted the distribution of embryos with increased runx1/cmyb expression in a manner phenotypically comparable with 1,25(OH)D3 (Figure 2F) and caused a 29% elevation in Flk1+cMyb+ HSPCs (p < 0.05) by FACS (Figure 2G). Furthermore, the impact of both 1,25(OH)D3 and calcipotriol was sustained in the CHT at 72 hpf, as determined by microscopy and FACS for CD41:GFP+ (control [con] versus 1,25(OH)D3, p < 0.05; con versus calcipotriol, p < 0.01) (Figures S2F and S2G). Together, these data indicate that vitamin D3-mediated regulation of embryonic HSPC production occurs via stimulation of VDR activity and cell proliferation independent of the impact on Ca2+ flux.
Figure 2. 1,25(OH)D3 Regulates HSPC Numbers via Vitamin D Receptor Signaling.
(A) Representative runx1/cmyb WISH images and qualitative phenotype distribution following 25(OH)D3 exposure from 12–36 hpf (n ≥ 40 embryos/condition).
(B) FACS analysis of 25(OH)D3-treated (10 µM) embryos showed a significant increase in HSPCs (**p < 0.01) (5 embryos/sample 3 4 replicates/condition). Error bars, mean ± SD.
(C) qPCR analysis indicated a significant induction in the VDR transcriptional target cyp24a1 at 36 hpf after exposure to 25(OH)D3 (*p < 0.05) or 1,25(OH)D3 (***p < 0.001) (12–36 hpf) (30 pooled embryos/condition 3 3 replicates).
(D) Phenotype distribution of runx1/cmyb expression in embryos exposed to increasing concentrations of 1,25(OH)D3 from 12–36 hpf (n ≥ 30 embryos/condition).
(E) FACS analysis of 1,25(OH)D3-treated (10 mM) embryos showed a 20% increase in HSPCs at 48 hpf (**p < 0.01) compared with controls (n value and error bars as in B).
(F) runx1/cmyb WISH and phenotype distribution after exposure to the non-calcemic vitamin D3 analog calcipotriol (n ≥ 30 embryos/condition).
(G) FACS analysis of calcipotriol-treated embryos showed a significantly more HSPCs (*p < 0.05) at 36 hpf (n value and error bars as in B). Scale bars, 100 µm. See also Figure S2.
1,25(OH)D3 Increases Adult HSPC Production and Function In Vivo and In Vitro
Unlike the mammalian BM niche, which is directly affected by vitamin D/VDR-mediated Ca2+ flux, adult zebrafish kidney marrow (KM) allows for analysis of 1,25(OH)D3 function independent of osteoregulation. To determine whether embryonic modulation of vitamin D production or signaling had long-term consequences, KM was dissected and subjected to FACS forward scatter (FSC)/side scatter (SSC) profiling (Stachura and Traver, 2016). KM from zebrafish exposed to exogenous 1,25(OH)D3 transiently (12–36 hpf) as embryos did not differ from control siblings. In contrast, both cyp2r1 and vdra mutants showed significant reductions in cells within the “lymphoid” gate (p < 0.05), which includes both lymphoid progenitors and HSC (Stachura and Traver, 2016), implying that vitamin D sufficiency is necessary to establish normal HSPC numbers (Figures S3A and S3B).
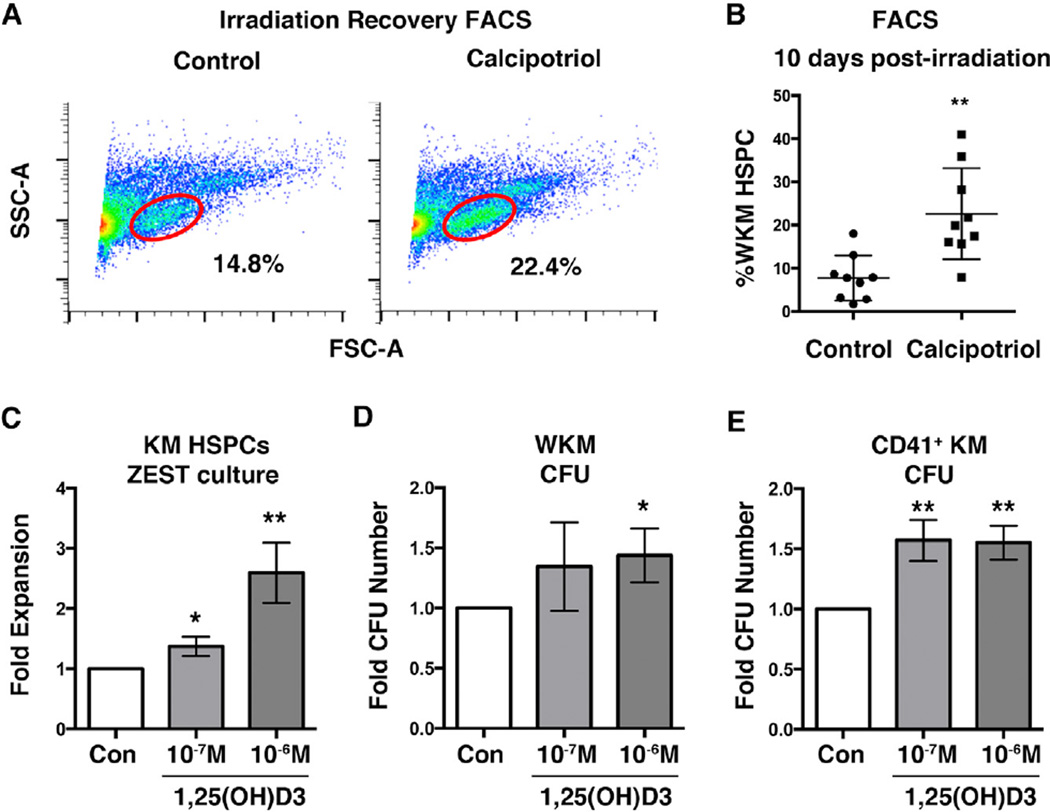
To investigate whether 1,25(OH)D3 supplementation could stimulate HSPC production in the adult, KM irradiation recovery experiments were performed (North et al., 2007). Consistent with adverse effects observed in the clinic (Leyssens et al., 2014), systemic treatment with 1,25(OH)D3 (10 µM) following irradiation was toxic, likely because of hypercalcemia, precluding further analysis. In contrast, exposure to calcipotriol for 24 hr at 2 days after sub-lethal irradiation caused a significant 34% enhancement (p < 0.01) in the recovery of HSPCs on day 10 compared with DMSO-treated controls (Figures 3A and 3B). To further characterize the impact of vitamin D3 supplementation, manually isolated whole KM was cultured on either zebrafish embryonic stromal trunk (ZEST) cells or zebrafish kidney stromal (ZKS) cells (Campbell et al., 2015). After 6 days in culture, a significant increase in total hematopoietic cells was observed with 1,25(OH)D3 exposure (ZEST, p < 0.01; ZKS, p < 0.01) (Figure 3C; Figure S3C), indicative of pro-proliferative stimulation. To determine whether 1,25(OH)D3 had a direct impact on HSPC function, methylcellulose hematopoietic colony-forming assays were performed (Stachura et al., 2011). Dissociated KM plated in the presence of 1,25(OH)D3 (1 × 10−6 M) showed a 40% increase (p < 0.05) in total colony forming unit, culture (CFU-C) compared with DMSO controls (Figure 3D) on day 10 after plating. Significantly, FACS-sorted CD41:GFP+ KM HSPCs cultured with 1,25(OH)D3 displayed a similar expansion (1 × 10−6 M, 55% increase, p <0.01; 1 × 10−7 M,57% increase, p <0.01) (Figure 3E), indicating that adult HSPCs can respond cell-autonomously to vitamin D3 stimulation to boost HSPC production and function independent of osteoregulation.
Figure 3. 1,25(OH)D3 Stimulates Cell-Autonomous HSPC Expansion.
(A) Representative FACS plots of DMSO- and calcipotriol-treated (20 µM) adult zebrafish at 10 dpi showing that calcipotriol enhanced the percentage of FSC/SSC-gated HSPCs(n = 9 adults/condition).
(B) Calcipotriol-treated adults had a 34% (**p < 0.01) increase in HSPCs compared with controls at 10 dpi (error bars, mean ± SD) by FACS.
(C) Adult KM HSPCs cultured with 1,25(OH)D3 for 6 days on ZEST cells demonstrated increased proliferation (**p < 0.01) compared with controls (n = 3). Error bars, mean ± SD.
(D) Methylcellulose CFU assay of adult whole KM (WKM) cells cultured with of 1,25(OH)D3 (1 × 10−7 M) displayed a 40% (*p < 0.05) increase in total colonies compared with DMSO controls (n = 3). Error bars, mean ± SD.
(E) CFU assay of CD41:GFP+ KM cultured in the presence of 1 × 10−6 and 1 × 10−7M 1,25(OH)D3 and sorted by FACS showed a 55% (**p < 0.01) and 57% (**p < 0.01) elevation, respectively, in colony numbers versus controls (n = 3). Error bars, mean ± SD.
See also Figure S3.
1,25(OH)D3 Enhances In Vitro Function of CD34+ Human Umbilical Cord Blood
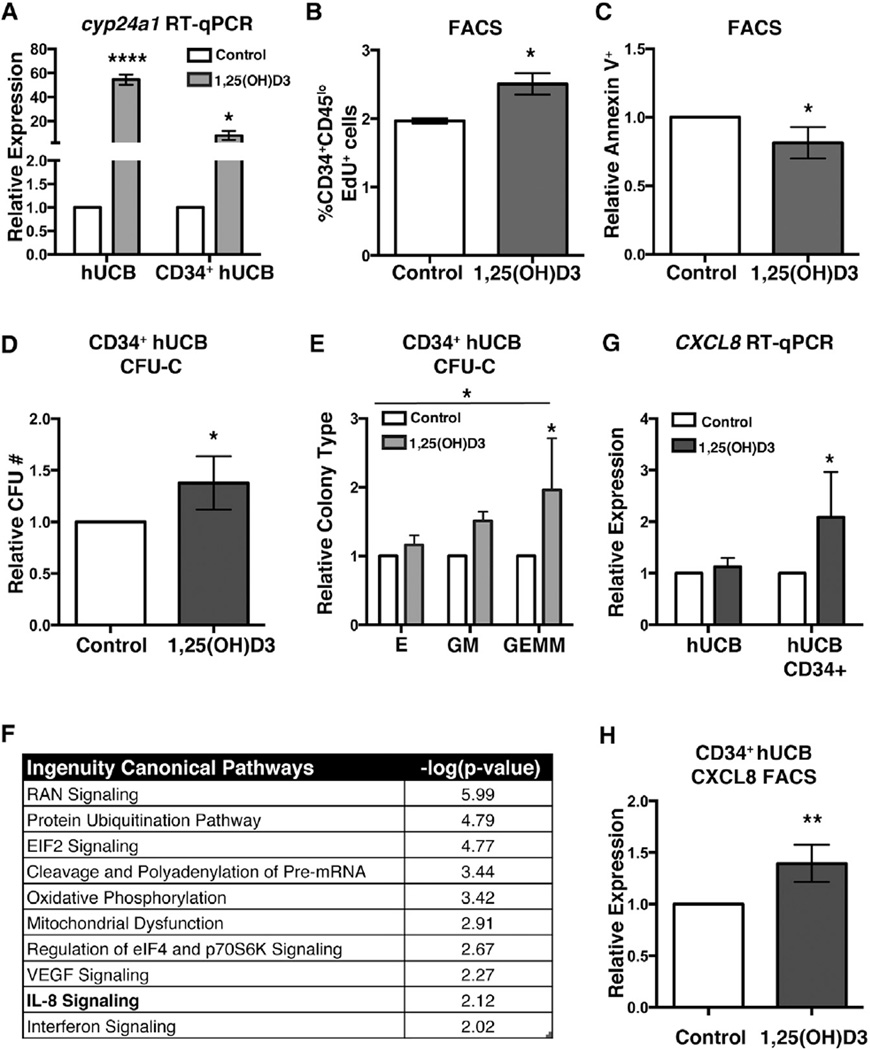
Given the strong pro-HSPC expansion effect observed in vivo and in vitro in zebrafish, we next investigated whether the regulatory impact of 1,25(OH)D3 was conserved in mammalian HSPCs. VDR is expressed on highly enriched murine HSCs (Riddell et al., 2014) as well as human CD34+ hematopoietic progenitors (Grande et al., 2002). Expression of the human VDR was confirmed in commercially available de-identified whole (unfractionated) and CD34+ human umbilical cord blood (hUCB) by qPCR (Figure S4A). Ex vivo treatment with 1,25(OH)D3 for 4 hr led to significant upregulation of CYP24A1 in both whole (p < 0.0001) and CD34+ (p < 0.05) hUCB cells (Figure 4A), indicative of VDR activation. Consistent with pro-proliferative effects in zebrafish, 5-ethyl-2’-deoxyuridine (EdU) labeling (10 µM, 1 hr) of whole hUCB cells exposed to 1,25(OH)D3 (1 µM, 4 hr) indicated a 35% increase (p < 0.05) in DNA synthesis in the CD34+/CD45lo HSPC population compared with controls (Figure 4B). 1,25(OH)D3-treated CD34+ hUCB samples also showed significantly decreased cell death (p < 0.05), as determined by FACS for the apoptosis marker Annexin V (Figure 4C). To assess whether vitamin D3 would elicit a positive impact on in vitro expansion and function of mammalian HSPCs, CFU-C assays were performed. Ex vivo incubation of CD34+ hUCB HSCs (n = 5 single donor hUCB units split for treatment and plated in replicate) with 1,25(OH)D3 for 4 hr at 37°C increased average total colony numbers at 7 days after plating by 38% (p < 0.05) compared with matched DMSO-treated controls (Figure 4D). This effect was concentration-dependent, where 1 × 10−7 and 1 × 10−6 M elicited a 39% (p < 0.05) and 56% elevation (p < 0.01) in colonies, respectively, whereas a higher dose of 1,25(OH)D3 (1 × 10−5 M) was refractory to expansion (Figure S4B). Analysis of the differentiation potential on day 10 after plating indicated that each progenitor fraction (colony forming unit, erythroid [CFU-E], colony forming unit, granulocyte/monocyte [CFU-GM], and colony forming unit, granulocyte/erythrocyte/monocyte/megakaryocyte [CFU-GEMM]) was increased by short-term, low-dose 1,25(OH)D3 exposure (1 × 10−6 M, p < 0.0.05) (Figure 4E). Further, the CFU-GEMM population in particular was significantly enhanced (p < 0.05), consistent with an impact on multipotent HSPCs.
Figure 4. Ex Vivo 1,25(OH)D3 Exposure Increases hUCB CD34+ HSPCs.
(A) qPCR analysis for the known VDR target CYP24A1 showed increased expression (****p < 0.0001) in individual whole and CD34+ (*p < 0.05) hUCB units split and treated with 1,25(OH)D3 versus DMSO (vehicle) control (n = 3 hUCB units). Error bars, mean ± SD.
(B) Whole (umbilical) cord blood (WCB) cells treated with 1,25(OH)D3 (4 hr) had significantly increased EdU labeling (*p < 0.05) of CD34+CD45lo HSCs compared with matched controls (n = 2). Error bars, mean ± SD.
(C) Annexin-V/7-AAD FACS analysis of CD34+ hUCB showed a significant decrease (*p < 0.05, n = 3) in apoptosis with 1,25(OH)D3 treatment.
(D) In vitro methylcellulose assays of CD34+ hUCB treated ex vivo with 1,25(OH)D3 (1 × 10−6 M) for 4 hr revealed a 38% (*p < 0.05) increase in total CFU numbers compared with DMSO controls on day 7 after plating (five independent single donor hUCB samples split for treatment and analysis). Error bars, mean ± SD.
(E) 1,25(OH)D3 treatment enhanced all colony types (CFU-E, CFU-GM, and CFU-GEMM) on day 10 versus matched controls (ANOVA, p < 0.05), with a significant increase in GEMMs (Fisher’s least significant difference [LSD] test, *p < 0.05). n = 5; error bars, ± SEM.
(F) Top canonical pathways enriched by 1,25(OH) D3 exposure based on IPA of significantly expressed genes. False discovery rate (FDR) < 0.05 (n = 2 single donor CD34+ hUCBs); IL-8 (CXCL8). Signaling is highlighted in bold type.
(G) qPCR analysis of CD34+ hUCB cells exposed to 1,25(OH)D3 (4 hr) showed a significant increase in CXCL8 expression (*p < 0.05) (n = 3). Error bars, mean ± SD.
(H) FACS quantification for CXCL8 protein content in CD34+ hUCBs showed a significant increase with 1,25(OH)D3 treatment (**p < 0.01 n = 4; error bars, mean ± SD).
See also Figure S4.
Because VDR is a known transcriptional regulator, changes in gene expression because of 1,25(OH)D3 exposure relevant to the observed in vitro hematopoietic phenotypes were examined. Response to short-term 1,25(OH)D3 (4-hr) exposure was validated by qPCR, where, in addition to enhanced expression of CYP24A1 (Figure 4A), the established VDR target and cell cycle regulator G0S2 (Singh et al., 2014), and the anti-apoptotic BCL2 (Vaux et al., 1988) were each elevated (Figure S4C). Further, although individual hUCB units showed differential responses to vitamin D3 stimulation, both Ingenuity Pathway (IPA) and MetaCore analyses revealed overlapping gene networks. In particular, IPA analysis indicated “IL-8 signaling” as a significantly regulated canonical pathway, whereas IL-8 (CXCL8) was a relevant component of three of the top ten MetaCore networks (Figure 4F; Figure S4D). The chemokine CXCL8 was shown previously to contain a functional VDRE in its promoter (Ryynänen and Carlberg, 2013) and exhibit an early transcriptional response to 1,25(OH)D3 stimulation in HL60 cells (Savli et al., 2002). The CXCL8 receptors CXCR1 and CXCR2 are expressed in hUCB, including the CD34+ fraction (Figure S4E). In response to 1,25(OH)D3 stimulation, CD34+ hUCB HSCs showed a significant induction in CXCL8 expression (p < 0.05) (Figure 4G). FACS analysis following monensin treatment to inhibit cytokine secretion confirmed a 40% increase (p < 0.01) in CXCL8 protein content in CD34+ hUCB cells with 1,25(OH)D3 exposure (Figure 4H), indicating CXCL8 as a relevant VDR target in HSPCs.
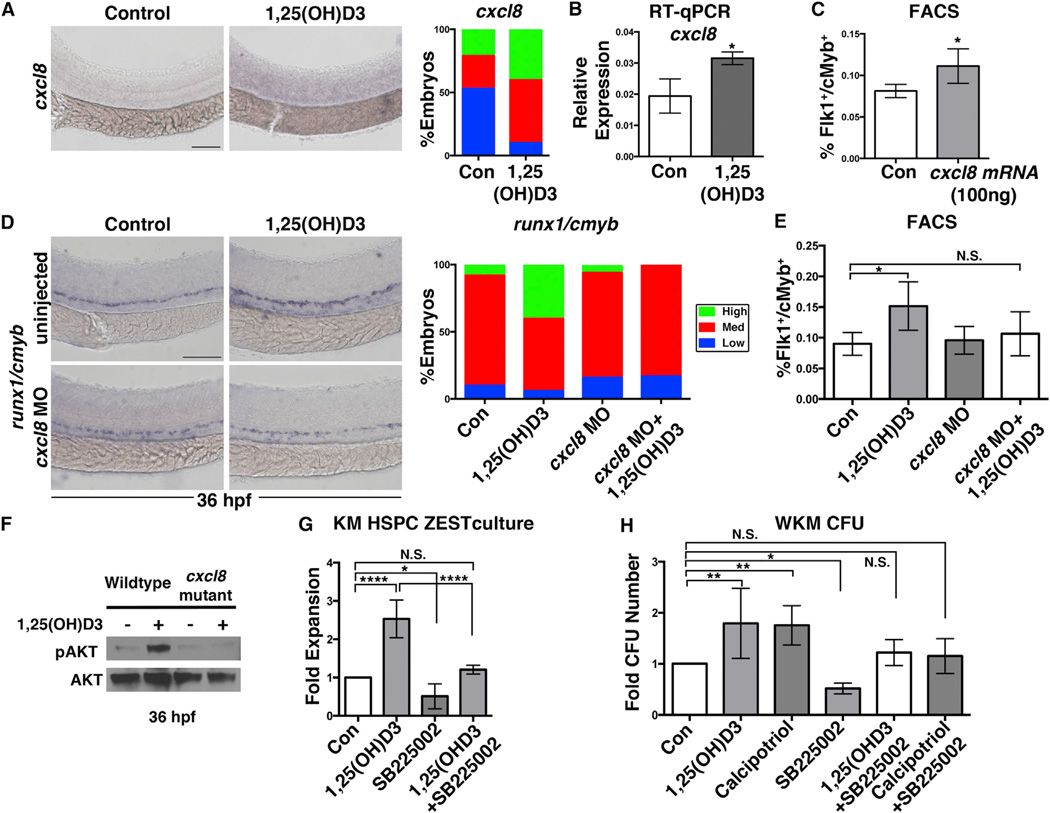
1,25(OH)D3 Regulates CXCL8 Signaling to Modulate HSPC Production
We recently showed inflammatory activity stimulates developmental HSC production in zebrafish and mice (Li et al., 2014). CXCL8 is a potent regulator of chemotaxis, proliferation, and survival in the hemato-vascular system in response to inflammatory stimuli (de Oliveira et al., 2013). To investigate whether the effect of 1,25(OH)D3 on HSPCs was mediated by Cxcl8 signaling, modified epistasis studies were conducted in zebrafish. Embryos treated with 1,25(OH)D3 displayed elevated cxcl8 expression, as assessed by WISH (Figure 5A) and quantified by whole-embryo qRT-PCR (p <0.05) (Figure 5B). Moreover, qRT-PCR analysis of sorted cell fractions showed a 4-fold increase in cxcl8 expression specifically in Flk1+cMyb+ HSPCs (Figure S5A). Consistent with autocrine or paracrine inflammatory stimulation of HSPCs, the Cxcl8 receptors cxcr1 and cxcr2 are expressed in the vascular and/or hematopoietic fractions of the embryo (Figure S5B). Further, injection of cxcl8 mRNA elicited a dose-dependent expansion in HSPCs (p < 0.05) reminiscent of 1,25(OH)D3 treatment (Figure 5C). Use of a previously validated morpholino to cxcl8 (Stoll et al., 2011) attenuated the shift in the fraction of embryos with elevated runx/cmyb expression (Figure 5D) as well as the boost in Flk1+cMyb+ HSPCs mediated by 1,25(OH)D3 (con versus 1,25(OH)D3, p < 0.05; con versus cxcl8 MO, N.S.; cxcl8 MO versus cxcl8 MO + 1,25(OH)D3, N.S.; 1,25(OH)D3 versus 1,25(OH)D3 + cxcl8 MO, N.S.) (Figure 5E), resulting in no difference from controls. Likewise, co-treatment with the CXCR1/2 inhibitor SB225002 (White et al., 1998) reduced the overall response of HSPCs to 1,25(OH)D3 stimulation, as determined by WISH (Figure S5C) and FACS (Figure S5D) (con versus 1,25(OH)D3, p < 0.01; 1,25(OH)D3 versus SB25002, p < 0.01; con versus 1,25(OH)D3 + SB25002, N.S.; 1,25(OH)D3 versus 1,25(OH)D3 + SB25002, N.S.). Cxcl8-Cxcr1/2 signaling elicits functional responses via activation of a number of intracellular mediators. In particular, AKT signaling downstream of Cxcr1/2 stimulation influences apoptosis and proliferation (Waugh and Wilson, 2008). Exposure to 1,25(OH)D3 (12–36 hpf) increased total phosphorylated AKT (pAKT) levels by western analysis (Figure 5F). Significantly, this effect was not observed in cxcl8 mutants. Likewise, in vitro exposure to the CXCL1/2 inhibitor SB225002 blocked KM HSPC expansion in the context of 1,25(OH)D3 stimulation in ZEST co-culture assays (Figure 5G) (con versus 1,25(OH)D3, p < 0.0001; con versus SB225002, p < 0.05; con versus 1,25(OH)D3 + SB25002, N.S.;1,25(OH)D3 versus 1,25(OH)D3 + SB25502, p < 0.0001). Finally, co-treatment with SB225002 antagonized functional enhancements in KM CFU numbers mediated by 1,25(OH)D3 or calcipotriol during in vitro methylcellulose culture (Figure 5H) (con versus 1,25(OH) D3, p < 0.01; con versus calcipotriol, p < 0.01; con versus SB225002, p < 0.05; con versus 1,25(OH)D3 + SB25502, N.S.; con versus calcipotriol + SB25502, N.S.). Together, our studies demonstrate that CXCL8-CXCR1/2 signaling functions downstream of 1,25(OH)D3-mediated VDR stimulation to directly regulate HSPC production and expansion.
Figure 5. 1,25(OH)D3 Mediates HSPC Expansion through CXCL8 Signaling.
(A) WISH for cxcl8 showing elevated expression with 1,25(OH)D3 treatment at 36 hpf (n ≥ 30 embryos/condition).
(B) Whole-embryo qPCR confirmed increased cxcl8 expression at 36 hpf after 1,25(OH)D3 exposure (*p < 0.05) (40 pooled embryos/condition 3 3 replicates). Error bars, mean ± SD.
(C) FACS analysis of embryos injected with cxcl8 mRNA (100 ng/embryo) showed increased Flk1:dsRed+/cMyb:GFP+ HSPCs at 36 hpf (*p < 0.05) (5 embryos/sample × 4 replicates/condition). Error bars, mean ± SD.
(D) WISH analysis and phenotype distribution indicated that the effect of 1,25(OH)D3 on runx1/cmyb expression was diminished in cxcl8 morphants (n ≥ 35 embryos/condition).
(E) FACS analysis of MO-injected embryos treated with 1,25(OH)D3 (con versus 1,25(OH)D3, *p < 0.05; con versus cxcl8 MO, N.S.; cxcl8 MO versus cxcl8 MO + 1,25(OH)D3, N.S.; 1,25(OH)D3 versus 1,25(OH)D3 +cxcl8 MO, N.S.)(5 embryos/sample3 4replicates/condition; error bars, mean ± SD) showed that loss of cxcl8 blocked vitamin D-mediated HSPC expansion.
(F) Western blot analysis for pAKT, with AKT as loading control, following 1,25(OH)D3 stimulation (12–36 hpf) in cxcl8 mutants versus WT siblings (60 embryos/condition).
(G) WKM stromal cell assay documenting changes in proliferation by 1,25(OH)D3 with and without co-incubation with SB25002 (con versus 1,25(OH)D3, ****p < 0.0001; con versus SB225002, p < 0.05; con versus 1,25(OH)D3 + SB25002, N.S.; 1,25(OH)D3 versus 1,25(OH)D3 + SB25502, ****p < 0.0001) (n = 4; error bars, mean ± SD).
(H) WKM methylcellulose CFU assay showing fold increase with and without co-treatment of 1,25(OH)D3 with SB25002 (con versus 1,25(OH)D3, **p < 0.01; con versus calcipotriol, **p<0.01; con versus SB225002, *p < 0.05; con versus 1,25(OH)D3+SB25502, N.S.; con versus calcipotriol + SB25502, N.S.).n =4(SB25503 is n = 6); error bars, mean ± SD.
Scale bars, 100 µm. See also Figure S5.
DISCUSSION
Vitamin D has an established role in bone maintenance; severe developmental 1,25(OH)D3 deficiency results in abnormal bone mineralization (rickets) that can be treated clinically with vitamin D2 or D3 supplementation. Interestingly, VDR is expressed in many cell types, implying that it may have additional roles in other organs, including the hematopoietic system (Christakos et al., 2013; Plum and DeLuca, 2010). However, important differences in vitamin D biology and its regulatory impact on mammalian cells have been observed. In particular, transcriptional target genes relating to immune regulation are differentially regulated by vitamin D in mice compared with humans (Dimitrov and White, 2015). Further, vitamin D synthesis in mice is not exclusively dependent on Cyp2r1 as in humans, likely explaining the unexpected lack of phenotypes in knockout models (Zhu et al., 2013). In this study, we took advantage of the conservation of the vitamin D synthesis and signaling pathway in teleosts (Lin et al., 2012) and the amenability of zebrafish to chemical and genetic manipulation to characterize the direct impact of 1,25(OH) D3 availability on HSPC development. Here we found that active vitamin D3 is both necessary and sufficient to modify embryonic HSPC production. Further, we revealed that this effect is due to VDR-mediated transcriptional activation of the inflammatory chemokine CXCL8, stimulating cell-autonomous regulation of HSPC expansion and viability via CXCR1/2 activity.
Although CXCL8 is a potent chemo-attractant for neutrophils and functions as part of the inflammatory response (Deng et al., 2013), recent studies in zebrafish have indicated that it can modulate hematopoietic stem cell formation (Jing et al., 2015). Our findings support a model in which vitamin D/VDR-mediated induction of CXCL8 acts in an autocrine/paracrine manner to promote HSPC survival and proliferation, similar to its function in endometrial stroma cells (Arici et al., 1998). Prior reports indicate that, in contrast to BM and mobilized peripheral blood populations, CXCR1 and CXCR2 expression is highly enriched in hUCB HSCs (Rosu-Myles et al., 2000), perhaps indicating a fundamental difference in responsiveness to CXCL8 signaling between adult and gestational HSPC sources. Interestingly, although we observe an increase in CXCL8 expression in both zebrafish and hUCB in response to 1,25(OH)D3, the impact of loss of Cxcl8-Cxcr1/2 signaling was most striking in the setting of vitamin D supplementation. These data imply that, although CXCL8 is a functional target of VDR stimulation, additional studies will be needed to identify whether other factors can contribute to overlapping or complementary aspects of VDR-mediated HSPC regulation in this or other contexts. Our findings also expand on the recent appreciation of the important role(s) of pro-inflammatory regulation in HSC induction and expansion during embryogenesis (Espín-Palazón et al., 2014; Li et al., 2014), which may serve as valid targets for therapeutic exploitation as proposed here.
Vitamin D has been investigated previously as a treatment for hematologic malignancy, albeit in a different context than presented here. Similar to use of retinoic acid for terminal differentiation of blasts in acute promyelocytic leukemia (APL), several in vitro studies showed that vitamin D treatment caused differentiation of leukemic precursors to the monocytic lineage (Hughes et al., 2010). These findings led to in vivo studies and phase 1 clinical trials for the use of vitamin D as a differentiation agent for acute myeloid leukemia (AML), which ultimately proved to be unsuccessful because of hypercalcemia and heterogeneity of the AML subtypes tested (Marchwicka et al., 2014). Interestingly, although treatment of the HL-60 leukemia cell line with 1,25(OH)D3 required 18–20 hr of exposure for differentiation to begin (Mangelsdorf et al., 1984), an initial burst in proliferation was seen during early phases (Brown et al., 1999), similar to the effect on HSPCs observed here. Our data indicate that 1,25(OH)D3 stimulates proliferative HSPC expansion. Consistent with this role, loss of 1,25(OH)D3 production or VDR function reduced HSPCs in vivo. Further, in vitro assays of both CD41 + zebrafish HSCs and CD34+ hUCB HSPCs revealed cell autonomous responses to short-term, low-dose 1,25(OH)D3 supplementation, independent of the niche, increasing multi-lineage CFU numbers via VDR-mediated alterations in proliferation and survival. These data are particularly relevant in the context of clinical observations of vitamin D-deficient pediatric and adult HSC transplant recipients who demonstrate a poor outcome, including graft versus host disease, delayed time to neutrophil engraftment, and overall survival (von Bahr et al., 2015; Wallace et al., 2015). Together, our data indicate that, beyond the published effects on lineage differentiation and immune-regulation, vitamin D has an important role in the foundation of the hematopoietic tree, regulating definitive HSPC numbers in the embryo.
Beyond the evolutionary conservation of 1,25(OH)D3/VDR-mediated regulation of HSPC numbers, cord-to-cord variability in our experimental and expression analyses highlight the potential clinical relevance of vitamin D status on hUCB function, particularly in regard to current ex vivo expansion and transplantation protocols. Vitamin D deficiency is a significant problem among pregnant women, ranging from 40%-50% in the northern United States (Bodnar et al., 2007). Extrapolating from these numbers, it is safe to assume that many hUCB samples are collected from vitamin D-deficient donors. In our hands, we observed variability in the magnitude of HSPC response among the treated hUCB samples, which we postulate may be attributed to the vitamin D status of the donor. Because ∼50% of transplanted HSC units cause treatment-related complications, including graft failure (10%) and/or delayed time to transplant recovery (Singh et al., 2014), there are clearly still significant gaps in our understanding of the full array of factors contributing to donor HSPC function. In future investigations, it will be of scientific and clinical interest to obtain the vitamin D status of the donor (or sample) to determine whether the magnitude of in vitro expansion, transplant efficacy, and/or response to 1,25(OH)D3 stimulation depends on the original status of the unit. In sum, we have elucidated a fundamental role of vitamin D availability in regulating embryonic HSPC production, highlighting the functional potential of nutritional vitamin D supplementation for clinical hUCB expansion.
EXPERIMENTAL PROCEDURES
Zebrafish Husbandry
Zebrafish lines were maintained and utilized in accordance with the Beth Israel Deaconess Medical Center (BIDMC) Institutional Animal Care and Use Committee (IACUC). The zebrafish lines used included AB, Tübingen (TU), and mutants and transgenics described in the Supplemental Experimental Procedures.
Chemical Treatments
Zebrafish embryos were exposed to chemical modulators in E3 fish medium from 12–36 hpf in multi-well plates unless noted otherwise. The following compounds (dose, supplier) were used: 1,25(OH)2D3 (1–10 µM, Cayman Chemical), Calcipotriol (1–10 µM, Cayman Chemical), SB225002 (1 µM, Cayman Chemical), and 25(OH)D3 (10 µM, Tocris). Treated embryos were analyzed by WISH based on established protocols and utilizing published probes (Cortes et al., 2015). Phenotypic variation (n ≥ 20 embryos/condition, n ≥ 3 replicate clutches) was qualitatively analyzed as relatively high (up), medium (normal), or low (down) expression compared with age/stage-matched sibling controls and graphically depicted as the percentage falling into each of the three phenotypic expression bins. Normal expression reflected the most representative phenotype in the bell curve distribution of each cohort of control embryos per experiment. Images were acquired using a Zeiss Axio Imager A1/Axio Cam MRC using Axio vision LE software.
Morpholino and mRNA Injection
Translation blocking or splice-site MOs (Gene Tools) against ZF vdra, vdrb, cyp27b1, and cxcl8 (Supplemental Experimental Procedures) were injected at the one-cell stage.
Embryo Dissociation and FACS Analysis
Fluorescent embryos (5 embryos/sample × 4 replicates/condition) were dissociated, resuspended in × PBS, and analyzed on a BD FACS Canto II in the presence of SYTOX Red dead cell stain (5 nM, Life Technologies) as described previously (Cortes et al., 2015). Data were analyzed using FlowJo X software (Tree Star). Double-negative, Flk1+/cMyb−, and Flk1+/cMyb+ cells were sorted (1,000 embryos/sample × 3 replicate sorts) on a BD SORP FACS Aria (BIDMC Flow Cytometry Core).
Expression Analysis
Total RNA was purified from zebrafish embryos (40 embryos/condition), human CD34+ cells (500,000 cells/condition), or mononuclear UCB (one million cells/condition) using the RNAqueous Micro kit (Life Technologies) followed by Turbo DNase-I treatment (Life Technologies). For sorted populations, cDNA amplification was performed using the NuGEN Ovation Pico WTA2 system. For embryos, 1 µg of total RNA was used to generate cDNA using Superscript III First Strand Synthesis Supermix (Life Technologies). Superscript VILO mastermix was used for human RNA samples (<1 µg of RNA). Quantitative real-time PCR was performed using SYBR Green PCR Master Mix (Life Technologies) on a Bio-Rad CFX384 Touch. Samples were run in triplicate with more than three biological replicates using published primers (Supplemental Experimental Procedures). Data analysis was performed using Real PCR Miner (http://ewindup.info/miner/).
Adult Kidney Marrow Analysis
KM from adult cyp2r1 and vdra mutants and their wild-type (WT) siblings was dissected and analyzed by SSC versus FCS FACS profiling after red blood cell lysis as described previously (Stachura and Traver, 2016). Irradiation recovery was performed as described previously (North et al., 2007). Adult male zebrafish were exposed to 20 Gy of γ-irradiation and treated at 2 days post irradiation (dpi) with calcipotriol (20 µM) in the fish water. KM was dissected and analyzed at 10 dpi by FACS profiling on a Beckman Coulter Gallios flow cytometer (BIDMC Flow Cytometry Core). Percent HSPC recovery was analyzed by FlowJo X.
In Vitro Functional Analysis
Hematopoietic in vitro function assays were performed as described previously for zebrafish (Campbell et al., 2015; Stachura et al., 2011) and human cells (Goessling et al., 2011) and are detailed in the Supplemental Experimental Procedures.
Statistical Analysis
Statistical analyses were performed using Prism 6 (GraphPad). Two-tailed Student’s t tests were used for pairwise comparisons and ANOVA for group analyses, with Holm-Sidak post hoc tests. Data are represented as mean ± SD. *p < 0.05; ** p < 0.01; ***p < 0.001; N.D., not detected.
Supplementary Material
Highlights.
Developmental 1,25(OH)D3 availability modulates definitive HSPC production
The effect of 1,25(OH)D3 on HSPCs is VDR-mediated and Ca2+-independent
Vitamin D supplementation significantly increases human UCB HSPCs in vitro
1,25(OH)D3 exposure promotes viability and proliferation via Cxcl8 (IL-8) activity
In Brief.
Cortes et al. elucidate a role for vitamin D signaling in hematopoietic stem and progenitor (HSPC) expansion and survival. Using zebrafish embryos and human umbilical cord blood, they demonstrate that HSPCs respond directly to 1,25(OH)D3 stimulation via vitamin D receptor-induced transcriptional activation of the inflammatory cytokine CXCL8.
Acknowledgments
We thank the BIDMC Flow Cytometry Core, Children’s Hospital Genomics Core, and HSCI Center for Stem Cell Bioinformatics for technical support; A. Huttenlocher (University of Wisconsin Madison) for the cxcl8 mutant, and D. Traver (University of California San Diego) for zebrafish in vitro culture reagents.
Footnotes
ACCESSION NUMBERS
The accession number for the microarray data reported in this paper is GEO: GSE86098.
SUPPLEMENTAL INFORMATION
Supplemental Information includes Supplemental Experimental Procedures, five figures, and three tables and can be found with this article online at http://dx.doi.org/10.1016/j.celrep.2016.09.012.
AUTHOR CONTRIBUTIONS
M.C. designed all experiments. M.C. and S.Y.L. made mutant lines. M.C., M.J.C., and L.T.V. performed hUCB CFU assays. M.C., L.N.T., S.Y.L., I.M.F., and V.E. performed MO injections and WISH. M.C. and W.K. ran qPCR. M.C., D.L.S., and F.W. conducted zebrafish in vitro assays. T.M.S., G.Q.D., and W.G. provided reagents and guidance. T.E.N. and M.C. analyzed data and wrote the manuscript.
REFERENCES
- Arici A, Seli E, Zeyneloglu HB, Senturk LM, Oral E, Olive DL. Interleukin-8 induces proliferation of endometrial stromal cells: a potential autocrine growth factor. J. Clin. Endocrinol. Metab. 1998;83:1201–1205. doi: 10.1210/jcem.83.4.4743. [DOI] [PubMed] [Google Scholar]
- Bertrand JY, Kim AD, Violette EP, Stachura DL, Cisson JL, Tra-ver D. Definitive hematopoiesis initiates through a committed erythro-myeloid progenitor in the zebrafish embryo. Development. 2007;134:4147–4156. doi: 10.1242/dev.012385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bertrand JY, Chi NC, Santoso B, Teng S, Stainier DYR, Traver D. Haematopoietic stem cells derive directly from aortic endothelium during development. Nature. 2010;464:108–111. doi: 10.1038/nature08738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Binderup L, Bramm E. Effects of a novel vitamin D analogue MC903 on cell proliferation and differentiation in vitro and on calcium metabolism in vivo. Biochem. Pharmacol. 1988;37:889–895. doi: 10.1016/0006-2952(88)90177-3. [DOI] [PubMed] [Google Scholar]
- Bodnar LM, Simhan HN, Powers RW, Frank MP, Cooperstein E, Roberts JM. High prevalence of vitamin D insufficiency in black and white pregnant women residing in the northern United States and their neo-nates. J. Nutr. 2007;137:447–452. doi: 10.1093/jn/137.2.447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown G, Choudhry MA, Durham J, Drayson MT, Michell RH. Monocytically differentiating HL60 cells proliferate rapidly before they mature. Exp. Cell Res. 1999;253:511–518. doi: 10.1006/excr.1999.4660. [DOI] [PubMed] [Google Scholar]
- Bruce D, Cantorna MT. Intrinsic requirement for the vitamin D receptor in the development of CD8αα-expressing T cells. J. Immunol. 2011;186:2819–2825. doi: 10.4049/jimmunol.1003444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell C, Su T, Lau RP, Shah A, Laurie PC, Avalos B, Aggio J, Harris E, Traver D, Stachura DL. Zebrafish embryonic stromal trunk (ZEST) cells support hematopoietic stem and progenitor cell (HSPC) proliferation, survival, and differentiation. Exp. Hematol. 2015;43:1047–1061. doi: 10.1016/j.exphem.2015.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll KJ, North TE. Oceans of opportunity: exploring vertebrate hematopoiesis in zebrafish. Exp. Hematol. 2014;42:684–696. doi: 10.1016/j.exphem.2014.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christakos S, Hewison M, Gardner DG, Wagner CL, Sergeev IN, Rut-ten E, Pittas AG, Boland R, Ferrucci L, Bikle DD. Vitamin D: beyond bone. Ann. N Y Acad. Sci. 2013;1287:45–58. doi: 10.1111/nyas.12129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cortes M, Liu SY, Kwan W, Alexa K, Goessling W, North TE. Accumulation of the Vitamin D Precursor Cholecalciferol Antagonizes Hedgehog Signaling to Impair Hemogenic Endothelium Formation. Stem Cell Reports. 2015;5:471–479. doi: 10.1016/j.stemcr.2015.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Oliveira S, Reyes-Aldasoro CC, Candel S, Renshaw SA, Mulero V, Calado A. Cxcl8 (IL-8) mediates neutrophil recruitment and behavior in the zebrafish inflammatory response. J. Immunol. 2013;190:4349–4359. doi: 10.4049/jimmunol.1203266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deng Q, Sarris M, Bennin DA, Green JM, Herbomel P, Hutten-locher A. Localized bacterial infection induces systemic activation of neutrophils through Cxcr2 signaling in zebrafish. J. Leukoc. Biol. 2013;93:761–769. doi: 10.1189/jlb.1012534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dimitrov V, White JH. Species-specific regulation of innate immunity by vitamin D signaling. J. Steroid Biochem. Mol. Biol. 2015 doi: 10.1016/j.jsbmb.2015.09.016. S0960-0760(15)30075-3. [DOI] [PubMed] [Google Scholar]
- Espín-Palazón R, Stachura DL, Campbell CA, García-Moreno D, Del Cid N, Kim AD, Candel S, Meseguer J, Mulero V, Traver D. Proinflammatory signaling regulates hematopoietic stem cell emergence. Cell. 2014;159:1070–1085. doi: 10.1016/j.cell.2014.10.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goessling W, Allen RS, Guan X, Jin P, Uchida N, Dovey M, Harris JM, Metzger ME, Bonifacino AC, Stroncek D, et al. Prostaglandin E2 enhances human cord blood stem cell xenotransplants and shows long-term safety in preclinical nonhuman primate transplant models. Cell Stem Cell. 2011;8:445–458. doi: 10.1016/j.stem.2011.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grande A, Montanari M, Tagliafico E, Manfredini R, Zanocco Marani T, Siena M, Tenedini E, Gallinelli A, Ferrari S. Physiological levels of 1alpha, 25 dihydroxyvitamin D3 induce the monocytic commitment of CD34+ hematopoietic progenitors. J. Leukoc. Biol. 2002;71:641–651. [PubMed] [Google Scholar]
- Hewison M, Freeman L, Hughes SV, Evans KN, Bland R, Eliopoulos AG, Kilby MD, Moss PAH, Chakraverty R. Differential regulation of vitamin D receptor and its ligand in human monocyte-derived dendritic cells. J. Immunol. 2003;170:5382–5390. doi: 10.4049/jimmunol.170.11.5382. [DOI] [PubMed] [Google Scholar]
- Holick MF. Resurrection of vitamin D deficiency and rickets. J. Clin. Invest. 2006;116:2062–2072. doi: 10.1172/JCI29449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes PJ, Marcinkowska E, Gocek E, Studzinski GP, Brown G. Vitamin D3-driven signals for myeloid cell differentiation-implications for differentiation therapy. Leuk. Res. 2010;34:553–565. doi: 10.1016/j.leukres.2009.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeanson NT, Scadden DT. Vitamin D receptor deletion leads to increased hematopoietic stem and progenitor cells residing in the spleen. Blood. 2010;116:4126–4129. doi: 10.1182/blood-2010-04-280552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jing L, Tamplin OJ, Chen MJ, Deng Q, Patterson S, Kim PG, Durand EM, McNeil A, Green JM, Matsuura S, et al. Adenosine signaling promotes hematopoietic stem and progenitor cell emergence. J. Exp. Med. 2015;212:649–663. doi: 10.1084/jem.20141528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kassam S, Vainsel M, Otten J, Fondu P. [Acute myeloblastosis in von Jaksch-Luzet syndrome] Arch. Fr. Pediatr. 1983;40:469–470. [PubMed] [Google Scholar]
- Kizaki M, Norman AW, Bishop JE, Lin CW, Karmakar A, Koeffler HP. 1,25-Dihydroxyvitamin D3 receptor RNA: expression in hematopoietic cells. Blood. 1991;77:1238–1247. [PubMed] [Google Scholar]
- Leyssens C, Verlinden L, Verstuyf A. The future of vitamin D analogs. Front. Physiol. 2014;5:122. doi: 10.3389/fphys.2014.00122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y, Esain V, Teng L, Xu J, Kwan W, Frost IM, Yzaguirre AD, Cai X, Cortes M, Maijenburg MW, et al. Inflammatory signaling regulates embryonic hematopoietic stem and progenitor cell production. Genes Dev. 2014;28:2597–2612. doi: 10.1101/gad.253302.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin C-H, Su C-H, Tseng D-Y, Ding F-C, Hwang P-P. Action of vitamin D and the receptor, VDRa, in calcium handling in zebrafish (Danio rerio) PLoS ONE. 2012;7:e45650. doi: 10.1371/journal.pone.0045650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mangelsdorf DJ, Koeffler HP, Donaldson CA, Pike JW, Haussler MR. 1,25-Dihydroxyvitamin D3-induced differentiation in a human pro-myelocytic leukemia cell line (HL-60): receptor-mediated maturation tomacrophage-like cells. J. Cell Biol. 1984;98:391–398. doi: 10.1083/jcb.98.2.391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marchwicka A, Cebrat M, Sampath P, Snieżewski L, Marcinkowska E. Perspectives of differentiation therapies of acute myeloid leukemia the search for the molecular basis of patients’ variable responses to 1,25-dihy-droxyvitamin d and vitamin d analogs. Front. Oncol. 2014;4:125. doi: 10.3389/fonc.2014.00125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mizwicki MT, Norman AW. The vitamin D sterol-vitamin D receptor ensemble model offers unique insights into both genomic and rapid-response signaling. Sci. Signal. 2009;2 doi: 10.1126/scisignal.275re4. re4-re4. [DOI] [PubMed] [Google Scholar]
- Naeem Z. Vitamin d deficiency- an ignored epidemic. Int. J. Health Sci (Qassim) 2010;4:V–VI. [PMC free article] [PubMed] [Google Scholar]
- Norman AW. Minireview: vitamin D receptor: new assignments for an already busy receptor. Endocrinology. 2006;147:5542–5548. doi: 10.1210/en.2006-0946. [DOI] [PubMed] [Google Scholar]
- North TE, Goessling W, Walkley CR, Lengerke C, Kopani KR, Lord AM, Weber GJ, Bowman TV, Jang I-H, Grosser T, et al. Pros-taglandin E2 regulates vertebrate haematopoietic stem cell homeostasis. Nature. 2007;447:1007–1011. doi: 10.1038/nature05883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ooi JH, McDaniel KL, Weaver V, Cantorna MT. Murine CD8+ T cells but not macrophages express the vitamin D 1α-hydroxylase. J. Nutr Biochem. 2014;25:58–65. doi: 10.1016/j.jnutbio.2013.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Panda DK, Miao D, Tremblay ML, Sirois J, Farookhi R, Hendy GN, Goltzman D. Targeted ablation of the 25-hydroxyvitamin D 1alpha -hydroxylase enzyme: evidence for skeletal, reproductive, and immune dysfunction. Proc. Natl. Acad. Sci. USA. 2001;98:7498–7503. doi: 10.1073/pnas.131029498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plum LA, DeLuca HF. Vitamin D, disease and therapeutic opportunities. Nat. Rev. Drug Discov. 2010;9:941–955. doi: 10.1038/nrd3318. [DOI] [PubMed] [Google Scholar]
- Ramagopalan SV, Heger A, Berlanga AJ, Maugeri NJ, Lincoln MR, Burrell A, Handunnetthi L, Handel AE, Disanto G, Orton S-M, et al. A ChIP-seq defined genome-wide map of vitamin D receptor binding associations with disease and evolution. Genome Res. 2010;20:1352–1360. doi: 10.1101/gr.107920.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riddell J, Gazit R, Garrison BS, Guo G, Saadatpour A, Mandal PK, Ebina W, Volchkov P, Yuan G-C, Orkin SH, Rossi DJ. Re-programming committed murine blood cells to induced hematopoietic stem cells with defined factors. Cell. 2014;157:549–564. doi: 10.1016/j.cell.2014.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosu-Myles M, Khandaker M, Wu DM, Keeney M, Foley SR, Howson-Jan K, Yee IC, Fellows F, Kelvin D, Bhatia M. Characterization of chemokine receptors expressed in primitive blood cells during human hematopoietic ontogeny. Stem Cells. 2000;18:374–381. doi: 10.1634/stemcells.18-5-374. [DOI] [PubMed] [Google Scholar]
- Ryynänen J, Carlberg C. Primary 1,25-dihydroxyvitamin D3 response of the interleukin 8 gene cluster in human monocyte- and macrophage-like cells. PLoS ONE. 2013;8:e78170. doi: 10.1371/journal.pone.0078170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Savli H, Aalto Y, Nagy B, Knuutila S, Pakkala S. Gene expression analysis of 1,25(OH)2D3-dependent differentiation of HL-60 cells: acDNA array study. Br. J. Haematol. 2002;118:1065–1070. doi: 10.1046/j.1365-2141.2002.03734.x. [DOI] [PubMed] [Google Scholar]
- Singh H, Nikiforow S, Li S, Ballen KK, Spitzer TR, Soiffer R, Antin JH, Cutler C, Chen Y-B. Outcomes and management strategies for graft failure after umbilical cord blood transplantation. Am. J. Hematol. 2014;89:1097–1101. doi: 10.1002/ajh.23845. [DOI] [PubMed] [Google Scholar]
- Stachura DL, Traver D. Cellular dissection of zebrafish hematopoiesis. Methods Cell Biol. 2016;133:11–53. doi: 10.1016/bs.mcb.2016.03.022. [DOI] [PubMed] [Google Scholar]
- Stachura DL, Svoboda O, Lau RP, Balla KM, Zon LI, Bartunek P, Traver D. Clonal analysis of hematopoietic progenitor cells in the zebrafish. Blood. 2011;118:1274–1282. doi: 10.1182/blood-2011-01-331199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stoll SJ, Bartsch S, Augustin HG, Kroll J. The transcription factor HOXC9 regulates endothelial cell quiescence and vascular morphogenesis in zebrafish via inhibition of interleukin 8. Circ. Res. 2011;108:1367–1377. doi: 10.1161/CIRCRESAHA.111.244095. [DOI] [PubMed] [Google Scholar]
- Sugiyama M, Sakaue-Sawano A, Iimura T, Fukami K, Kitaguchi T, Kawa-kami K, Okamoto H, Higashijima S, Miyawaki A. Illuminating cell-cycle progression in the developing zebrafish embryo. Proc. Natl. Acad. Sci. USA. 2009;106:20812–20817. doi: 10.1073/pnas.0906464106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vaux DL, Cory S, Adams JM. Bcl-2 gene promotes haemopoietic cell survival and cooperates with c-myc to immortalize pre-B cells. Nature. 1988;335:440–442. doi: 10.1038/335440a0. [DOI] [PubMed] [Google Scholar]
- von Bahr L, Blennow O, Alm J, Björklund A, Malmberg K-J, Mougiaka-kos D, Le Blanc A, Oefner PJ, Labopin M, Ljungman P, Le Blanc K. Increased incidence of chronic GvHD and CMV disease inpatients with vitamin D deficiency before allogeneic stem cell transplantation. Bone Marrow Transplant. 2015;50:1217–1223. doi: 10.1038/bmt.2015.123. [DOI] [PubMed] [Google Scholar]
- Wallace G, Jodele S, Howell J, Myers KC, Teusink A, Zhao X, Setchell K, Holtzapfel C, Lane A, Taggart C, et al. Vitamin D Deficiency and Survival in Children after Hematopoietic Stem Cell Transplant. Biol. Blood Marrow Transplant. 2015;21:1627–1631. doi: 10.1016/j.bbmt.2015.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waugh DJJ, Wilson C. The interleukin-8 pathway in cancer. Clin. Cancer Res. 2008;14:6735–6741. doi: 10.1158/1078-0432.CCR-07-4843. [DOI] [PubMed] [Google Scholar]
- Weinert LS, Silveiro SP. Maternal-fetal impact of vitamin D deficiency: a critical review. Matern. Child Health J. 2015;19:94–101. doi: 10.1007/s10995-014-1499-7. [DOI] [PubMed] [Google Scholar]
- White JR, Lee JM, Young PR, Hertzberg RP, Jurewicz AJ, Chaikin MA, Widdowson K, Foley JJ, Martin LD, Griswold DE, Sarau HM. Identification of a potent, selective non-peptide CXCR2 antagonist that inhibits interleukin-8-induced neutrophil migration. J. Biol. Chem. 1998;273:10095–10098. doi: 10.1074/jbc.273.17.10095. [DOI] [PubMed] [Google Scholar]
- Yetgin S, Ozsoylu S. Myeloid metaplasia in vitamin D deficiency rickets. Scand. J. Haematol. 1982;28:180–185. doi: 10.1111/j.1600-0609.1982.tb00512.x. [DOI] [PubMed] [Google Scholar]
- Zhu JG, Ochalek JT, Kaufmann M, Jones G, Deluca HF. CYP2R1 is a major, but not exclusive, contributor to 25-hydroxyvitamin D production in vivo. Proc. Natl. Acad. Sci. USA. 2013;110:15650–15655. doi: 10.1073/pnas.1315006110. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.