Abstract
Background and objectives
Older kidney transplant recipients are susceptible to cognitive impairment, frailty, comorbidities, immunosuppression-related complications, and chronic graft failure, however, there has been limited focus on their concerns and expectations related to transplantation. This study aims to describe the perspectives of older kidney transplant recipients about their experience of kidney transplantation, self-management, and treatment goals to inform strategies and interventions that address their specific needs.
Design, setting, participants, & measurements
Face-to-face semistructured interviews were conducted with 30 kidney transplant recipients aged 65–80 years from five renal units in Australia. Transcripts were analyzed thematically.
Results
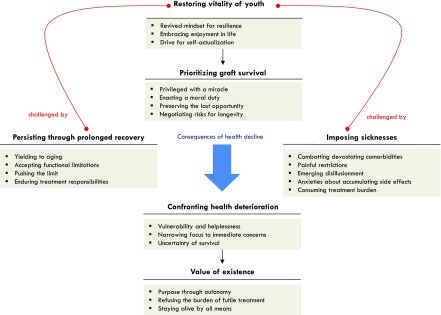
Six themes were identified: restoring vitality of youth (with subthemes of revived mindset for resilience, embracing enjoyment in life, drive for self-actualization); persisting through prolonged recovery (yielding to aging, accepting functional limitations, pushing the limit, enduring treatment responsibilities); imposing sicknesses (combatting devastating comorbidities, painful restrictions, emerging disillusionment, anxieties about accumulating side effects, consuming treatment burden); prioritizing graft survival (privileged with a miracle, negotiating risks for longevity, enacting a moral duty, preserving the last opportunity); confronting health deterioration (vulnerability and helplessness, narrowing focus to immediate concerns, uncertainty of survival); and value of existence (purpose through autonomy, refusing the burden of futile treatment, staying alive by all means).
Conclusions
Older kidney transplant recipients felt able to enjoy life and strived to live at their newly re-established potential and capability, which motivated them to protect their graft. However, some felt constrained by slow recuperation and overwhelmed by unexpected comorbidities, medication-related side effects, and health decline. Our findings suggest the need to prepare and support older recipients for self-management responsibilities, clarify their expectations of post-transplant risks and outcomes, and provide assistance through prolonged recovery after kidney transplantation.
Keywords: geriatric nephrology, quality of life, transplant outcomes, adolescent, aging, anxiety, Australia, cognition disorders, comorbidity, goals, graft survival, humans, immunosuppression, kidney transplantation, longevity, medical futility, moral obligations, motivation, negotiating, self-care, transplant recipients, uncertainty
Introduction
Kidney transplantation can confer survival and quality-of-life benefits compared with dialysis in older kidney transplant recipients (1–7), however, the effect of aging on post-transplant management is acknowledged as a considerable challenge (8–10). The number of prevalent older kidney transplant recipients is expected to grow due to improved graft and survival outcomes through to older age, and the last decade has seen a three-fold increase in the number of transplants in older adults above the age of 65 years in the United States (11,12). Physical and cognitive impairment, chronic comorbidities, and complications associated with immunosuppression may prolong postsurgical recovery (13–23), add complexity to post-transplant care, and impair capacity for self-management.
Older kidney transplant recipients value the survival gained by transplant, however, they also struggle with persistent limitations after transplant, the side effects of immunosuppressive medication, and worry about a possible return to dialysis should the transplant fail (24). Little is known about their expectations of kidney transplantation, how they cope with self-management responsibilities, and how they perceive their prognosis post-transplant. This study aims to describe the range and depth of the experiences and perspectives of older kidney transplant recipients about their expectations, self-management, and treatment goals while living and aging with a kidney transplant. A broad understanding may inform education, strategies, and interventions for improving transplant outcomes in older patients.
Materials and Methods
Study reporting is based on the Consolidated Criteria for Reporting Qualitative Health Research (25).
Participant Selection and Setting
Participants were eligible if they were kidney transplant recipients, aged 65 years and over, and English speaking. We used purposive sampling to obtain a maximum variation of demographics (age, sex) and clinical characteristics (including time since transplant, complications). The participants were recruited from Westmead Hospital in Sydney (Australia) and five referral dialysis units, which provide follow-up after transplant. Ethics approval was obtained from the Western Sydney Local Health District. All participants provided informed consent for study participation.
Data Collection
We developed an interview guide informed by a systematic review of older kidney transplant recipient perspectives on kidney transplantation (24) (Supplemental Table 1). A.T./J.P. conducted face-to-face semistructured interviews from April to June 2015 until data saturation, i.e., no new concepts were obtained. All interviews were audio-recorded and transcribed verbatim.
Data Analysis
Using thematic analysis, J.P. read each transcript line-by-line, then conceptualized and coded by hand all meaningful segments of text into concepts inductively identified from the data. Similar concepts were grouped into preliminary themes and subthemes. C.S.H. and A.T. read the transcripts independently and discussed the preliminary coding structure to enhance the analytic framework, and to ensure that it captured the full breadth and depth of data collected. The transcripts were imported into HyperRESEARCH (Version 2.8.3; ResearchWare Inc.). The software was used to generate a report of all of the themes and qualitative data coded to each theme. J.P., C.S.H., and A.T. identified and discussed conceptual patterns among the themes, which were mapped into a schema (Figure 1).
Figure 1.
Thematic schema of the perspectives of older kidney transplant recipients. Kidney transplantation restores vitality and autonomy for older kidney transplant recipients, which enables them to enjoy life, and strive to fulfill their now attainable goals. They prioritize the functioning of their graft, as they feel grateful, privileged, and responsible to preserve what could be their final chance of recuperation. However, “persisting through prolonged recovery,” and “imposing sicknesses” challenge the regained vitality. Some participants may experience the consequences of health decline. If they confront deterioration in health, older kidney transplant recipients may feel vulnerable and uncertain of their survival. This can lead some to question the value of their own existence.
Results
Of the 33 invited to participate, 30 (91%) were interviewed. Nonparticipation was due to refusal or sickness. The participant characteristics are shown in Tables 1 and 2. Participants were aged from 65 to 80 years (mean 70.1 years). Fifteen (50%) spoke English as their second language. The age they received their current transplant ranged from 50 to 71 years (mean 64.0 years), with the total duration since transplantation ranging from 0.5 to 25 years (mean 6.4 years). Four (13%) had received a transplant within the past 1 year. Fifteen (50%) were men, and 21 (70%) had a deceased donor kidney transplant. One participant had undergone a prior transplant. The average duration of the interview was 40 minutes and all participants were interviewed at their homes.
Table 1.
Participant demographic characteristics (n=30)
| Demographic Characteristics | n (%) |
|---|---|
| Age, yr | |
| 65–70 | 17 (57) |
| 71–75 | 12 (40) |
| 76–80 | 1 (3) |
| Sex | |
| Women | 15 (50) |
| Employment | |
| Retired | 26 (87) |
| Part-time | 4 (13) |
| Marital status | |
| Married | 23 (77) |
| Divorced | 2 (7) |
| Widowed | 3 (10) |
| Single | 2 (7) |
| Number of children | |
| 0 | 2 (7) |
| 1 | 2 (7) |
| 2 | 14 (47) |
| ≥3 | 12 (40) |
| Number of grandchildren | |
| 0 | 2 (7) |
| 1 | 2 (7) |
| 2 | 5 (17) |
| ≥3 | 21 (70) |
| Highest level of education | |
| Primary school | 6 (20) |
| Secondary school (Grade 10 or equivalent) | 8 (27) |
| Secondary school (Grade 12 or equivalent) | 6 (20) |
| Tertiary—certificate/diploma | 7 (23) |
| Tertiary—university degree | 3 (10) |
| Ethnicity | |
| White | 15 (50) |
| Maltese | 7 (23) |
| Othera | 5 (17) |
| Egyptian | 3 (10) |
| Place of residence | |
| Metropolitan | 27 (90) |
| Nonmetropolitan (regional, rural) | 3 (10) |
% may not total 100 due to rounding.
Grouped to protect identity.
Table 2.
Participant clinical characteristics (n=30)
| Clinical Characteristics | n (%) |
|---|---|
| Donor type | |
| Deceased | 21 (70) |
| Living (spouse) | 4 (13) |
| Living (nonrelated/nondirected donor) | 3 (10) |
| Living (sibling) | 2 (7) |
| Age at time of transplant, yr | |
| 50–55 | 3 (10) |
| 56–60 | 4 (13) |
| 61–65 | 9 (30) |
| 66–70 | 13 (43) |
| 71–75 | 1 (3) |
| Time on the waiting lista, yr | |
| <1 | 1 (3) |
| 1–5 | 16 (53) |
| 6–10 | 7 (23) |
| Previous RRTb | |
| Peritoneal dialysis | 15 (50) |
| In-center hemodialysis | 12 (40) |
| Home hemodialysis | 11 (37) |
| None (pre-emptive transplant) | 3 (10) |
| CKD diagnosis or cause | |
| Polycystic kidney disease | 12 (40) |
| Glomerulonephritis | 12 (40) |
| Diabetic nephropathy | 6 (20) |
| Comorbidities (since transplant)b | |
| Diabetes | 16 (53) |
| Cardiovascular disease | 12 (40) |
| Cancer (skin & solid) | 12 (40) |
| Infection | 10 (33) |
| Rheumatologic disorder | 9 (30) |
| Neurologic disorder (including dementia) | 9 (30) |
| Gastrointestinal conditions (including liver disease) | 6 (20) |
| Ophthalmologic condition | 4 (13) |
| Bone disease | 3 (10) |
| Respiratory disease | 3 (10) |
| Urologic condition | 2 (6) |
| Immunosuppressant medicationsb | |
| Prednisone | 28 (93) |
| Tacrolimus | 22 (73) |
| Mycophenolate | 19 (63) |
| Belatacept | 6 (20) |
| Cyclosporine | 5 (17) |
| Sirolimus | 3 (10) |
| Azathioprine | 2 (7) |
% may not total 100 due to rounding.
Time on the waiting list refers to recipients with a deceased donor transplant or living nonrelated donors (n=24).
Numbers may not total due to multiple categories or categories are not applicable to all participants.
Six themes were identified: restoring vitality of youth; persisting through prolonged recovery; imposing sicknesses; prioritizing graft survival; confronting health deterioration; and value of existence. The themes and respective subthemes are described in the following section and a selection of quotations for each subtheme is provided in Table 3. The patterns and relationships among themes are depicted in the thematic schema (Figure 1).
Table 3.
Illustrative quotations to reflect themes on older kidney transplant recipients’ perspectives on kidney transplantation
| Theme | Quotations |
|---|---|
| Restoring vitality of youth | |
| Revived mindset for resilience | “(Transplant) made a huge difference. This is the best I’ve felt for 20 yr, since before I started getting sick in the first place. (Transplant) has taken my mindset back to what it was, when I was young. When you’re young, and you get sick, you can say to yourself, ‘next week I’ll be fine again.’ You don’t even think about it. When you’re really sick, and you’ve got a chronic disease, you can’t say that to yourself, because you know it’s going to go on and on and on, forever. That’s the way I looked at it, until I got the transplant, and now I’m back to the stage of saying, hey, I got this flu, and it’s going to last a bit longer with me than with normal people, but hey, a couple of weeks and I’m going to be back to normal again.” (Man, 60s, ID 29) |
| Embracing enjoyment in life | “It is being alive, I have been free, I feel healthy and well and energetic and to feel like that when you haven’t is pretty marvelous. You’re living in the moment now, enjoying life. That’s a real benefit of transplant. It lets you do that. I’ve been given life.” (Woman, 70s, ID 18) |
| Drive for self-actualization | “Some people feel old, I feel young. I feel fresh. I’m hoping (and) I believe that I have a good activity through the kidney. I’m confident that it is a young kidney. I have all the future ahead of me. I have a lot of ambitions in my business and work, for my children, for the future. I can see myself starting today, I’ve got my plans what I’m going to do, what things will relax me, what I’m going to enjoy. I’m not getting old.” (Man, 60s, ID 13) |
| Persisting through prolonged recovery | |
| Yielding to aging | “I was 65 when I had transplant, and I think it takes us older (people) more (time), I’d spoken to people who had it in their 40s, boom, boom, done. But I think that’s because they’d be in their 40s. I was in my 60s and it takes you a bit longer. I don’t know what was usual. See, no one told me, but it took quite a while.” (Woman, 70s, ID 19) |
| Accepting functional limitations | “When I had the transplant I couldn’t do anything, and it used to frustrate me. But now, I just gotta take it, I’ve gotta realize that I can’t do things like I used to do.” (Man, 70s, ID 3) |
| “They told me to walk for an hour. I couldn’t walk for an hour. I can hardly walk from here to the letterbox and back again. I’d be puffing. And if they say to me, go and walk for an hour, impossible. They wouldn’t believe me.” (Man, 60s, ID 1) | |
| Pushing the limit | “They keep telling me I gotta push myself, but you can’t push yourself to walk if you can’t breathe. I went into hospital (because) I actually couldn’t walk. They say it’ll improve if I force myself to do more, but I can’t. I don’t mind trying, how far I can go. I have to try and force myself a bit more this time. I’ve got all the equipment now, haven’t I? I have the determination to get there.” (Woman, 70s, ID 10) |
| “I encourage myself, and I push myself all the time. Yes, I’ll have a cry some days, I get frustrated with myself for not being able to do more. Your brain wants to, but your body doesn’t help you to.” (Woman, 70s, ID 26) | |
| Enduring treatment responsibilities | “I didn’t know that there is so much work involved, like you’ve got to visit doctors, and things like that. I didn’t know that. But it doesn’t matter, you know. It doesn’t matter.” (Man, 60s, ID 4) |
| “It is very tiring to go to hospital every day to have your bloods taken, to be tested, and then you’ve gotta wait for 4 hours to get a result. You have to get up early, and your day is gone. You have to ask somebody to take you there, you’re infringing on other people. The hospital’s busy, the doctor’s visit everybody. Some of them weren’t well, some of them did have reactions. It’s very hard for people. Try and sit on a chair for 4 hours after an operation. Stuck in that room you have to do everything, because you’re so contagious in many ways.” (Woman, 60s, ID 17) | |
| Imposing sicknesses | |
| Combatting devastating comorbidities | “I try to get a bit of strength, I haven’t got strength. And put on weight. I’m losing it, I’m weak, and I get tired.” (Woman, 70s, ID 6) |
| “Since all this colostomy business, I’ve been very tired and I’m still not my old self, I haven’t got the energy, that last operation knocked me around. Out of hospital, I was down to 40 kilos, and I nearly had to be carried in. I used to be like a 50-year-old with energy. Now I’ve aged considerably, but nothing to do with the kidney, more to do with the colostomy, the bowel thing.” (Woman, 70s, ID 24) | |
| “It was good until I started to get sick with the bowel cancer. But I didn’t realize I had that. The last year has been a ****house.” (Woman, 70s, ID 19) | |
| Painful restrictions | “I’ve got vertebrae out at the back and it does need fusing. I’ve got a cyst in the spinal cord, which has grown very, very slowly. The circulation in the leg is poor. There’s no pulse in my foot. This causes the pain I’m having, the discomfort in the legs, when walking. I’m going to a neurologist next week. I can’t really walk very far because it’s painful.” (Woman, 70s, ID 18) |
| “I got shingles, and I’ve never been able to totally lose that pain. I’ve got some tablets to take for it, which I don’t like to take too much because it’ll make you lose your balance. It’s a horrible pain that won’t go away, and it’s apparently the nerve endings. That’s more of a worry than everything else. It was the worst thing I’ve ever had, shocking pains that won’t go away.” (Woman, 70s, ID 24) | |
| Emerging disillusionment | “I thought the problem (kidney disease) had fixed.” (Man, 60s, ID 4) |
| “I wasn’t going to go cranky at the doctor for not telling me. It’s just, part and parcel of what happens. (I felt) terrible that the tablets cause diabetes. They should tell you because it’s a risk. Diabetes isn’t a joke. You can go blind, you can get your leg cut off. You can get gangrene. The transplant’s ok, that’s kind of over. But now the diabetes is bothering me.” (Man, 60s, ID 1) | |
| Anxieties about accumulating side effects | “I often wonder, what the long-term effects of constantly taking immunosuppressants are, because nobody tends to tell you. It would be nice to know if, constantly being on immunosuppressants affects longevity. Does it shorten your life span in comparison to if you weren’t taking them? I’m a bit worried that you keep on taking different, stronger and stronger medications, until you reach a point where you build up a resistance to all of them.” (Man, 70s, ID 25) |
| “The long-term side effects like cancer worry me. I don’t like to go through a serious thing like this anymore. I don’t like to have this experience anymore. That’s it.” (Man, 70s, ID 8) | |
| Consuming treatment burden | “I’m forever having infections. I’ve got a lot of fungus. It’s coming everywhere. On my fingers, I have it on the side of my mouth. I’ve got a lot I have to get rid of. I’m losing weight because I haven’t got much of an appetite, I’m having a lot of problems swallowing, am burping a lot, and I can’t get the food down, I’m losing weight.” (Woman, 70s, ID 6) |
| “The only ill effect I had was with the Cellcept. I was getting a bit of diarrhea and I lost so much weight, 9 kilos, in a couple of months. This is not good, because I’d never lost weight like that before, without exercising and dieting, it just seemed to fall away.” (Man, 70s, ID 20) | |
| “I am running from one doctor to another, if it’s not for this, it’s for that. If it’s not for that, it’s for that. As I said, I had a prolapse after this as well, I had the sciatica after the transplant, and my back has been crook ever since, but they tell you, you have to learn to live. Sometimes it’s hard, because, you think, oh another appointment, that doctor, another appointment, that doctor. Really it shouldn’t be a big issue, but when you’re getting older, everything becomes a big issue. It’s very hard for an elderly person.” (Woman, 70s, ID 9) | |
| Prioritizing graft survival | |
| Privileged with a miracle | “It is absolutely a miracle to get it and that it works with no rejection.” (Man, 70s, ID 7) |
| “When I had it at my age, it was wonderful. I would’ve liked it 10 years earlier though, that would’ve been even more wonderful. But then I wouldn’t have appreciated it as much.” (Woman, 70s, ID 24) | |
| Negotiating risks for longevity | “I know the medication, it’s strong and it does have side effects, but in the meantime, it’s keeping me alive.” (Man, 70s, ID 7) |
| “About 4 months (after transplant) the doctor said, the medication’s starting to give you type 2 diabetes, I’m going to put you on this tablet, and it’s kept me in the safe range ever since. I don’t really have diabetes but if I stop taking that tablet, I probably would get it. It doesn’t worry me (because) I’m alive. I don’t have to go to hospital every second day and sit on bloody dialysis. I’m living, what I consider to be a normal life now for me. It’s just a nuisance taking all those tablets every day. At the opposite end of it, it could be a lot worse, so I just accept it.” (Man, 60s, ID 30) | |
| Enacting a moral duty | “We met a fellow who had two kidneys. He had two transplants, but he used to drink and smoke. If they do that, they don’t deserve another kidney because they abuse it. If you’re not going to look after yourself, the kidney can go to someone who is.” (Man, 70s, ID 3) |
| “I live with somebody who’s donated one of their kidneys for me. It’s like jumping out of a perfectly good aeroplane. I can’t see the sense in doing that, that’s the parachute. People have got a perfectly good and healthy kidney, and they’re prepared to donate it, and I think that’s a wonderful thing to do, and I will do anything to protect that kidney for them, for the person that donated to me, which I consider to be my wife, because she donated for me, not to me, but for me. So I will do everything I can to look after what that person’s done for me. It’s a massive responsibility.” (Man, 60s, ID 30) | |
| Preserving the last opportunity | “If I lost this kidney I don’t know whether I’d be prepared to go back on dialysis. I’m going to do everything possible not to lose the kidney. I would imagine older recipients would be more careful. Younger ones would be a bit more blasé, and expect that they’d just get another one if that one fails. Whereas elderly, wouldn’t probably get another one. Most people in my situation would think the same: if you lose it, it’s gone. This is your only chance.” (Man, 60s, ID 29) |
| “The most important thing to maintain my health is to take my immunosuppressants, because without them, you go downhill pretty quickly. I take them 12 hours apart. It probably helps if you do. The other thing I try is to keep a fairly good diet. I love fruit, I do a bit of walking, and I stay as active as I possibly can.” (Man, 70s, ID 25) | |
| Confronting health deterioration | |
| Vulnerability and helplessness | “No one said a word about anything. Who to see, where to go, who to ring.” (Man, 70s, ID 21) |
| “To tell you the truth, I’m reliant on him (husband). Because if he didn’t take me to all my appointments and everything, I wouldn’t be able to get there, I’m sure of it. Because I’d give up. I couldn’t look after myself. I’d manage a couple of hours a day. But for all day-to-day, I don’t think so.” (Woman, 70s, ID 10) | |
| Narrowing focus to immediate concerns | “If it’s in a couple of weeks’ time ask me a week before, I don’t want to think about it before then. So many times have things—health wise—gone wrong before it reached that stage. So I just like to work a week ahead. I don’t want to dwell on it until it’s time.” (Woman, 70s, ID 10) |
| “I don’t have any goals or priorities. Just to keep on going as good as I can go. Every day, what comes, comes, and be thankful for it.” (Woman, 70s, ID 26) | |
| Uncertainty of survival | “Don’t worry about it, just see what happens. I’m at that stage. You can’t do anything else. We can’t fix it. They can’t fix it. Every time I end up in hospital (and) I come home and survived, (I ask myself) ‘Will I make it this time?’” (Woman, 70s, ID 10) |
| “At my age, you’ve got to start thinking: what if my health worsens? My wife and I made our wills out and determined the power of attorney, our sons. That gives me a bit less pressure. I feel better knowing that that’s all been done. I’m hoping I go for quite a few years yet, but I’m prepared, if the worst comes to worst.” (Man, 70s, ID 20) | |
| Value of existence | |
| Purpose through autonomy | “The thing that bothers me is (if the house) is wheelchair accessible. If I couldn’t walk and use my hand, life wouldn’t worth be living. I like to do things, make things. The worst thing I expect (is) not being able to move, to be dependent on somebody to have to push you around.” (Woman, 70s, ID 18) |
| Refusing the burden futile treatment | “When I was on peritoneal, it was an every day issue, on hemo(dialysis) an every second day issue. You haven’t got a life, because you can’t do anything. All I could do was to crawl around the place and sit down and watch TV. Your life revolves around dialysis and you want it to stop. It would be horrible to have to go back onto dialysis. I would not want to go back. That’d be a killer. I wouldn’t do it. It’s not worth it because I’ll be a burden.” (Man, 60s, ID 1) |
| “I’m over 70, so I chose to have my fistula removed, because if anything happens again, that’s it. I never want to go back on dialysis again.” (Woman, 70s, ID 18) | |
| “I don’t have any goals. I have sort of given that away. If anything happens to me, just don’t restart me, no matter what they tell you. Because there is nothing I can do. I wouldn’t care less if I died. Makes no difference to me.” (Man, 70s, ID 21) | |
| Staying alive by all means | “The transplant’s been great. I’d hate to go back on dialysis, because of the time factor. But if you’ve got to do it, you’ve got to do it. I have no wish to die at this stage. I’d go back. In the beginning, I had trouble on dialysis, you always do, your BP drops, you do all sorts of weird and wonderful things, and I’m no different. But my body got used to it after a while and I coped quite well.” (Woman, 70s, ID 24) |
| “I’m hoping I go for quite a few years yet, but I’m prepared, if the worst comes to worst, I can touch the dog’s eye (fistula), I can feel it buzzing, so everything is good. I’m going to keep on going as long as I can.” (Man, 70s, ID 20) | |
ID, identification code.
Restoring Vitality of Youth
Revived Mindset for Resilience.
The kidney transplant “made a huge difference” and some claimed to feel “the best for 20 years.” Some felt “young” and revived with a sense of hope, reassurance, and confidence in their own capacity to overcome sicknesses and persist through setbacks. One participant believed that his mood and energy level was restored to that of an 18-year-old.
Embracing Enjoyment in Life.
Some felt energized by the mental and physical improvements after transplant. The transplant enabled them to live “in the moment now, enjoying life.” Others felt that “the whole world opened up.” Reversal of dietary and travel restrictions and being able “to just do what I want to do” provided enormous relief and the ability to live some “nice, easy remaining years of life.”
Drive for Self-Actualization.
Having a new lease on life, some participants suddenly had “all the future ahead” and gained confidence to achieve their potential. With transplant, they were given time, which they consciously utilized until “every moment was taken up to make up for the lost time on dialysis,” and immersed themselves in their work and hobbies.
Persisting through Prolonged Recovery
Yielding to Aging.
Some were conscious of their older age and believed that they would need a prolonged time of recuperation after transplant compared with younger transplant recipients. Some felt prone to experience more difficulties in recovery and health due to their “age factor.”
Accepting Functional Limitations.
After transplant, some felt frustrated when they continued to experience limitations in their mobility. They were unable to walk and exercise as they could not keep physically fit, and became fearful of sustaining injuries from falling. Some noted a marked deterioration in their physical abilities after transplant—“My feet are numb and have deformed from the diabetes. I’m a bit unstable in my walking and it has been getting worse since transplant.” Some believed that their physicians instructed “impossible” levels of physical activity after transplant such as walking for an hour, and felt exasperated. Some accepted their limitations and recalibrated their expectations to physical activity levels for which they were capable.
Pushing the Limit.
Encouraged by health care providers “to push themselves,” some were determined to overcome their bodily constraints. They persevered and challenged themselves despite feeling that “your brain wants to, but your body doesn’t help you to.” Some strived to the point of physical exhaustion and “pushed the limit intentionally too hard” until they “got physically so run down.”
Enduring Treatment Responsibilities.
Some participants felt unprepared for the ongoing self-management responsibilities, particularly with regards to attending follow-up appointments, navigating multispecialty services, and taking a complex regimen of immunosuppression medications—“I didn’t know that there is so much work involved, you’ve got to visit doctors and things like that.”
Imposing Sicknesses
Combatting Devastating Comorbidities.
For some, the well being gained through transplant was devastated by the diagnosis and treatment consequences of other serious comorbidities, such as bowel cancer that involved extensive abdominal surgery or chemotherapy.
Painful Restrictions.
Some participants experienced episodes of agonizing and persistent pain that restricted their mobility. Others felt distressed by stabbing facial sensations induced by the herpes zoster virus. Yet, some preferred to endure the pain and were determined to avoid analgesics as they feared it would potentially damage the graft or trigger distressful side effects, such as hallucinations.
Emerging Disillusionment.
Some were disappointed when the transplant did not meet their expectations of rapid and easy recovery with improved quality of life. Some believed that transplant would be a permanent cure and reverse their kidney disease “I thought the problem (of kidney disease) had fixed.” Thus, they felt inadequately prepared mentally to manage and cope with unexpected complications such as diabetes “I wasn’t going to go cranky at the doctor for not telling me. It’s just part and parcel of what happens. They should tell you because it’s a risk. Diabetes isn’t a joke. The transplant’s ok, that’s kind of over. But now the diabetes is bothering me.”
Anxieties about Accumulating Side Effects.
Some participants felt anxious that “taking heaps and heaps of tablets” could “shorten your life span” or trigger cumulative drug resistance. One woman was concerned of the increased risk of cancer. Some felt distressed if they experienced uncontrollable side effects such as severe weight loss secondary to diarrhea or fungal oral infections. Others fought against prednisone-induced hunger by eating less yes still gained weight “You’re damned if you do and you’re damned if you don’t.”
Consuming Treatment Burden.
Participants felt increasingly weary when the treatment of transplant-related complications coincided and interfered with treatment of their other comorbidities. One recipient believed that “running from one doctor to another (was) very hard for an older person.” For some, the “rocky road” of unpreventable and accumulating health “problems” led to regret where some questioned whether transplant had been the right decision.
Prioritizing Graft Survival
Privileged with a Miracle.
Transplant was described as a “gift” and a “miracle,” particularly as some had not expected to receive a transplant due to their older age. Their long-standing suffering on dialysis enabled some to appreciate the opportunity of transplant—“If people were thinking about having a transplant or staying on dialysis, I would tell them every time, go for the transplant, because it worked out beautifully for me.”
Negotiating Risks for Longevity.
Motivated to avoid dialysis, some willingly accepted the risks of immunosuppression for longevity. Those who were concerned about immunosuppressive side effects were challenged to overcome their anxieties and focus on enjoying the gift of a functioning graft.
Enacting a Moral Duty.
Some believed that they owed a “massive responsibility” to their donor to protect and maximize graft survival. “Wasting a perfectly good kidney” by not looking after oneself was deemed morally wrong, “idiotic and stupid” and an act of “abuse.”
Preserving the Last Opportunity.
Some were certain that their current transplant was their “last and only chance” and doubted that they would be eligible for another transplant due to their older age. Some thought that people aged 60–70 years would be precluded from transplantation. This motivated and sustained their efforts to preserve their current graft, such as adhering to their medication regimen, and making healthy lifestyle choices regarding diet and exercise.
Confronting Health Deterioration
Vulnerability and Helplessness.
A decline of health, imposed by other sicknesses or severe complications after transplant, caused emotional turmoil and uncertainty for some. This intensified their sense of vulnerability and helplessness, which some internalized. Some felt unable to continuously exercise self-management without the indispensable practical support from their partners. This was particularly challenging for participants whose partner had died.
Narrowing Focus to Immediate Concerns.
If their health deteriorated, some participants refused to be constantly reminded of their sicknesses, as they felt unable to cope. They abandoned long-term goals such as planning for vacation to avoid disappointment, and focused their attention to immediate day-to-day tasks.
Uncertainty of Survival.
Increasing hospitalization led to loss of hope—“They (physicians) can’t fix it”; and uncertainty about death and potential graft loss—“will I make it this time?” and “how long am I going to last with this kidney?” Some identified a health care power of attorney and made treatment decisions for the future while they still had autonomous capacity to do so. Others preferred not to dwell prematurely on end-of-life decisions.
Value of Existence
Purpose through Autonomy.
Some feared the unmanageable consequences of increasing physical immobility, and felt that confinement to bed, losing mobility, and having to depend on others, would rob their sense of purpose such that “life wouldn’t be worth living” anymore. Transplant had restored their independence and freedom, and the loss of such would diminish the value in having a transplant.
Refusing the Burden of Futile Treatment.
Some were unwilling to return to dialysis should the transplant fail. Some felt they had merely existed, deprived of any self- or life-value while on dialysis. Some chose to remove their fistula, or opted against all forms of life-sustaining therapies. Others described the difficulties of coping with sicknesses and would refuse curative therapy, such as chemotherapy for cancers, even if it meant risking graft loss. Further, some felt unable to discuss their concerns or decisions with others, including their nephrologist or other family members whom they did not want to cause concern.
Staying Alive by All Means.
In contrast, other participants prioritized survival to be of highest importance and viewed returning to dialysis to be the only available and valid option as they had “no wish to die at this stage.”
Discussion
Our study highlights the range and heterogeneity of experiences among older kidney transplant recipients, from being able to enjoy the extensive quality-of-life benefits of a transplant, to remaining constrained by functional limitations, or suffering from comorbidities or general health decline. Older kidney transplant recipients felt physically and mentally revived after kidney transplantation, and used their restored energy and autonomy to enjoy life and fulfill their new ambitious, but now attainable, goals. The current transplant was their last hope, which motivated their efforts to preserve graft function and manage their health. Age-related and functional limitations impeded rapid recovery yet some persisted by pushing their limit of physical activity. Some felt inadequately prepared for the multiple treatment responsibilities after transplantation and became disillusioned and devastated when they experienced severe and often unexpected complications, debilitating pain that impaired normal functioning, and accumulating side effects of medications that increased the burden of treatment and diminished the health that transplantation had restored.
Some older kidney transplant recipients were acutely aware of how their older age could prolong and complicate recovery. Others struggled to meet their physician’s recommended level of physical activity during post-transplant recovery due to pain, and functional impairment. A recent systematic review suggested that older transplant recipients regain strength and vitality, while they struggle with residual functional limitations (24). Some studies, albeit limited, suggest that the functional status of older kidney transplant recipients is an independent predictor of post-transplant survival (13,14,26,27). Older kidney transplant recipients with the lowest physical function scores pretransplantation have the highest mortality rates after transplantation compared with younger recipients (13,14). A study found that more than half of older kidney transplant recipients reported being disabled or required assistance for at least one daily-living activity, with housekeeping, grocery shopping, and laundry being the activities most commonly affected, and a fifth recalled having fallen more than once in the past year (28). A regular assessment of functional impairment and frailty (14), the provision of exercise training and physiotherapy (29) to prevent falls, as well as additional assistance with mobility restrictions such as walking aids, and arranged transport to and from health care facilities may sustain and foster the patient’s functional capacity after transplant.
Our findings have implications for education, communication, and advance care planning. We suggest that older kidney transplant candidates may have unique information needs compared with younger patients, as they may be more vulnerable to adverse effects of comorbidities, health decline, and limitations due to the aging process, and experience higher rates of hospitalization and skilled nursing facility care placements (30,31). Older recipients identified the need for specific advice regarding physical activity and exercise that considers their degree of functional limitations, and promotes achievable fitness goals. They wanted to be informed about the potential risk of unexpected complications, such as diabetes, the cumulative side effects of medication, and fears regarding pain management. They depended on others to attend follow-up appointments, and had to coordinate and navigate multispecialty services. Information about identifying pragmatic support for post-transplant follow-up appears critical to help older transplant recipients better self-manage, and coordinate their care post-transplantation. This may also include discussion about the increased risk of hospitalization and complications in older recipients. We suggest that transplant centers provide at least initial education addressing these specific transplant-related needs, which could subsequently be followed up by primary care providers (e.g., with geriatricians). Further studies may be needed to identify optimal strategies for delivering this information in clinical settings.
Our findings provide broad insights on the expectations and the existential angst related to aging, comorbidities, medication, and fear of losing the graft. Some older kidney transplant recipients felt disappointed when the transplant did not meet their expectation of rapid recovery. Others believed that transplant would be a permanent cure and reverse their kidney disease. As such, some felt inadequately prepared to continuously manage multiple treatment responsibilities after transplantation, and to cope with unexpected adverse complications. This highlights the need to clarify and ensure realistic expectations of recovery. Given the range and differences of experiences, we would suggest utilizing effective communication strategies in an individualized patient-centered approach to identify their specific priorities and concerns, and address their specific needs. Motivational interviewing techniques (32,33) and communication frameworks such as “SPIKES” (Setting, Perception, Invitation, Knowledge, Emotions, Summary) (34,35) have been developed to identify the patient’s concerns, and respond to informational and emotional concerns. An ongoing dialogue facilitated by patient-reported symptom measures and effective communication structures can inform decisions about managing side effects (36,37), define achievable goals for the period of recovery (38), and build rapport and trust, which may temper disillusionment if adverse side effects or complications occur. Proposed strategies for clinical practice derived from our findings are outlined in Table 4.
Table 4.
Proposed strategies for clinical practice
| Domain | Suggested Strategies and Action |
|---|---|
| Practical support | Assist with mobility if functional limitations are present e.g., walking aids, daily exercise training to prevent falls, assistance if help is needed in daily activities, and household management |
| Provide practical reminders for medication adherence e.g., blister packing medications, telephone reminders, establishing a system of daily routines, motivational interviewing, and mobile apps | |
| Organize transport to and from hospital to attend follow-up appointments | |
| Assess functional impairment, frailty, and cognitive impairment as needed | |
| Physician-patient communication | Engage in a process of shared decision-making in the choice for transplant |
| Acknowledge the older recipient’s goals, preferences, and priorities | |
| Discuss the benefits and harms of transplantation | |
| Provide directed education for older patients before kidney transplant | |
| Engage in a shared dialogue about realistic expectations and post-transplant outcomes, and define achievable goals for the period of recovery | |
| Use Motivational Interviewing Techniques to identify and respond to recipient’s concerns and elicit his or her perception of illness factors (33) | |
| Utilize communication frameworks such as “SPIKES” (Setting, Perception, Invitation, Knowledge, Emotions, Summary) (35) for tasks involving emotional as well informational concerns | |
| Setting up the interview, assessing the patient’s Perception, obtaining the patient’s Invitation, giving Knowledge and information to the patient, addressing the patient’s Emotions with emphatic responses, Strategy/Summary) | |
| Address informational concerns: “Ask-Tell-Ask” (34) | |
| Ask (“What is your understanding of your current illness?”) | |
| Tell (Tailor the information that it addresses patient concerns and needs) | |
| Ask (“To make sure that I explained things well, can you tell me what you understand of what I just said?”) | |
| Advance care planning | Discuss goals of care at sentinel events such as hospitalizations, acute illnesses, or decline of functional capacity. Involve family and caregivers as needed |
| Balance biomedical information with emotional, social, cultural, and spiritual issues | |
| Have open conversations about individual priorities regarding life-sustaining therapies, in particular any form of RRT and maintenance of access (e.g., fistula removal) | |
| Symptom assessment and management | Incorporate regular symptom screening and assessment into routine clinical practice |
| Symptom management requires a stepwise approach: | |
| Re-evaluate and redirect treatment plans aligned with recipient’s values and preferences | |
| Social support | Facilitate access to online and/or face-to-face patient support groups |
| Psychosocial support | Provide counseling and coping strategies to manage debilitating complications and side-effects |
| Healthcare delivery | If other comorbidities, distressing symptoms, and complications arise deliver coordinated and multidisciplinary care for adequate pain and symptom management |
“SPIKES”, Setting, Perception, Invitation, Knowledge, Emotions, Summary.
Some older transplant recipients decided they would not return to dialysis should their graft fail and elected to remove their fistula. Some felt uncertain about their prognosis and those who had debilitating and unexpected complications questioned whether transplant had been the right decision. Importantly, some recipients in our study had not explicitly discussed their decisions with anyone, as they were reluctant to burden others by expressing their treatment preference for conservative (nondialytic) management. We suggest to implement advance care planning at appropriate times, e.g., during hospitalization or deterioration of health, to prepare patients and their family/caregiver for future treatment decision-making (39).
In our study, we included prevalent older kidney transplant recipients with a broad range of demographics and comorbidities. However, there are some potential limitations. Older recipients were interviewed once and our data may not capture subsequent changes in perspectives. Older recipients were recruited from one major transplant center in Australia, which may limit the transferability of findings, although similar findings in the systematic review of qualitative studies of older transplant recipient perspectives suggest that the results may be relevant to other contexts (24). Critically ill patients were excluded for ethical reasons, and thus concerns or priorities specific to them, such as end-of-life care, could not be explored. We interviewed patients with a functioning transplant, and the effect of transplant failure on the perspectives of older patients who returned to dialysis could be explicitly addressed in future research.
In conclusion, kidney transplantation can restore vigor and vitality for older kidney transplant recipients, but some may feel constrained by slow and complicated recuperation, and overwhelmed by treatment burden due to comorbidities, side effects of drugs, and deteriorating health and mobility. Providing support through prolonged recovery, sustaining the patient’s functional capacity, addressing treatable side effects, and eliciting the recipient’s perception of prognosis, goals, and values, may improve satisfaction and empower older recipients to preserve what they perceive as their last opportunity for transplant.
Disclosures
None.
Supplementary Material
Acknowledgments
We sincerely thank all of the participants for taking the time to share their perspectives. We would like to thank Christoph Wanner for his valuable contribution in providing feedback on the manuscript.
This study was funded by Australian Research Council Grant DE120101710. A.T. is supported by National Health and Medical Research Council Fellowship ID 1106716.
The funding organizations had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript.
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
This article contains supplemental material online at http://cjasn.asnjournals.org/lookup/suppl/doi:10.2215/CJN.05890616/-/DCSupplemental.
References
- 1.Wolfe RA, Ashby VB, Milford EL, Ojo AO, Ettenger RE, Agodoa LYC, Held PJ, Port FK: Comparison of mortality in all patients on dialysis, patients on dialysis awaiting transplantation, and recipients of a first cadaveric transplant. N Engl J Med 341: 1725–1730, 1999 [DOI] [PubMed] [Google Scholar]
- 2.Tonelli M, Wiebe N, Knoll G, Bello A, Browne S, Jadhav D, Klarenbach S, Gill J: Systematic review: Kidney transplantation compared with dialysis in clinically relevant outcomes. Am J Transplant 11: 2093–2109, 2011 [DOI] [PubMed] [Google Scholar]
- 3.Rao PS, Merion RM, Ashby VB, Port FK, Wolfe RA, Kayler LK: Renal transplantation in elderly patients older than 70 years of age: Results from the scientific registry of transplant recipients. Transplantation 83: 1069–1074, 2007 [DOI] [PubMed] [Google Scholar]
- 4.Kasiske BL, Cangro CB, Hariharan S, Hricik DE, Kerman RH, Roth D, Rush DN, Vazquez MA, Weir MR; American Society of Transplantation : The evaluation of renal transplantation candidates: Clinical practice guidelines. Am J Transplant 1[Suppl 2]: 3–95, 2001 [PubMed] [Google Scholar]
- 5.Rebollo P, Ortega F, Baltar JM, Álvarez-Ude F, Alvarez Navascués R, Álvarez-Grande J: Is the loss of health-related quality of life during renal replacement therapy lower in elderly patients than in younger patients? Nephrol Dial Transplant 16: 1675–1680, 2001 [DOI] [PubMed] [Google Scholar]
- 6.Humar A, Denny R, Matas AJ, Najarian JS: Graft and quality of life outcomes in older recipients of a kidney transplant. Exp Clin Transplant 1: 69–72, 2003 [PubMed] [Google Scholar]
- 7.Cornella C, Brustia M, Lazzarich E, Cofano F, Ceruso A, Barbé MC, Fenoglio R, Cella D, Stratta P: Quality of life in renal transplant patients over 60 years of age. Transplant Proc 40: 1865–1866, 2008 [DOI] [PubMed] [Google Scholar]
- 8.Saran R, Li Y, Robinson B, Ayanian J, Balkrishnan R, Bragg-Gresham J, Chen JT, Cope E, Gipson D, He K, Herman W, Heung M, Hirth RA, Jacobsen SS, Kalantar-Zadeh K, Kovesdy CP, Leichtman AB, Lu Y, Molnar MZ, Morgenstern H, Nallamothu B, O’Hare AM, Pisoni R, Plattner B, Port FK, Rao P, Rhee CM, Schaubel DE, Selewski DT, Shahinian V, Sim JJ, Song P, Streja E, Kurella Tamura M, Tentori F, Eggers PW, Agodoa LY, Abbott KC: US Renal Data System 2014 annual data report: Epidemiology of kidney disease in the United States. Am J Kidney Dis 66[Suppl 1]: S1–S305, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pippias M, Stel VS, Abad Diez JM, Afentakis N, Herrero-Calvo JA, Arias M, Tomilina N, Bouzas Caamaño E, Buturovic-Ponikvar J, Čala S, Caskey FJ, Castro de la Nuez P, Cernevskis H, Collart F, Alonso de la Torre R, García Bazaga ML, De Meester J, Díaz JM, Djukanovic L, Ferrer Alamar M, Finne P, Garneata L, Golan E, González Fernández R, Gutiérrez Avila G, Heaf J, Hoitsma A, Kantaria N, Kolesnyk M, Kramar R, Kramer A, Lassalle M, Leivestad T, Lopot F, Macário F, Magaz A, Martín-Escobar E, Metcalfe W, Noordzij M, Palsson R, Pechter Ü, Prütz KG, Ratkovic M, Resić H, Rutkowski B, Santiuste de Pablos C, Spustová V, Süleymanlar G, Van Stralen K, Thereska N, Wanner C, Jager KJ: Renal replacement therapy in Europe: A summary of the 2012 ERA-EDTA registry annual report. Clin Kidney J 8: 248–261, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Knoll GA: Kidney transplantation in the older adult. Am J Kidney Dis 61: 790–797, 2013 [DOI] [PubMed] [Google Scholar]
- 11.Schäeffner ES, Rose C, Gill JS: Access to kidney transplantation among the elderly in the United States: A glass half full, not half empty. Clin J Am Soc Nephrol 5: 2109–2114, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Matas AJ, Smith JM, Skeans MA, Thompson B, Gustafson SK, Stewart DE, Cherikh WS, Wainright JL, Boyle G, Snyder JJ, Israni AK, Kasiske BL: OPTN/SRTR 2013 annual data report: Kidney. Am J Transplant 15[Suppl 2]: 1–34, 2015 [DOI] [PubMed] [Google Scholar]
- 13.Kutner NG, Zhang R, Bowles T, Painter P: Pretransplant physical functioning and kidney patients’ risk for posttransplantation hospitalization/death: Evidence from a national cohort. Clin J Am Soc Nephrol 1: 837–843, 2006 [DOI] [PubMed] [Google Scholar]
- 14.Reese PP, Bloom RD, Shults J, Thomasson A, Mussell A, Rosas SE, Johansen KL, Abt P, Levine M, Caplan A, Feldman HI, Karlawish J: Functional status and survival after kidney transplantation. Transplantation 97: 189–195, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kurella Tamura M, Yaffe K: Dementia and cognitive impairment in ESRD: Diagnostic and therapeutic strategies. Kidney Int 79: 14–22, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wu C, Evans I, Joseph R, Shapiro R, Tan H, Basu A, Smetanka C, Khan A, McCauley J, Unruh M: Comorbid conditions in kidney transplantation: Association with graft and patient survival. J Am Soc Nephrol 16: 3437–3444, 2005 [DOI] [PubMed] [Google Scholar]
- 17.Doyle SE, Matas AJ, Gillingham K, Rosenberg ME: Predicting clinical outcome in the elderly renal transplant recipient. Kidney Int 57: 2144–2150, 2000 [DOI] [PubMed] [Google Scholar]
- 18.Faravardeh A, Eickhoff M, Jackson S, Spong R, Kukla A, Issa N, Matas AJ, Ibrahim HN: Predictors of graft failure and death in elderly kidney transplant recipients. Transplantation 96: 1089–1096, 2013 [DOI] [PubMed] [Google Scholar]
- 19.Karim A, Farrugia D, Cheshire J, Mahboob S, Begaj I, Ray D, Sharif A: Recipient age and risk for mortality after kidney transplantation in England. Transplantation 97: 832–838, 2014 [DOI] [PubMed] [Google Scholar]
- 20.Kauffman HM, McBride MA, Cors CS, Roza AM, Wynn JJ: Early mortality rates in older kidney recipients with comorbid risk factors. Transplantation 83: 404–410, 2007 [DOI] [PubMed] [Google Scholar]
- 21.Wedel N, Brynger H, Blohmè I: Kidney transplantation in patients 60 years and older. Scand J Urol Nephrol Suppl 54: 106–108, 1980 [PubMed] [Google Scholar]
- 22.Ismail N, Hakim RM, Helderman JH: Renal replacement therapies in the elderly: Part II. Renal transplantation. Am J Kidney Dis 23: 1–15, 1994 [DOI] [PubMed] [Google Scholar]
- 23.Meier-Kriesche HU, Ojo A, Hanson J, Cibrik D, Lake K, Agodoa LY, Leichtman A, Kaplan B: Increased immunosuppressive vulnerability in elderly renal transplant recipients. Transplantation 69: 885–889, 2000 [DOI] [PubMed] [Google Scholar]
- 24.Pinter J, Hanson CS, Craig JC, Chapman JR, Budde K, Halleck F, Tong A: ‘I feel stronger and younger all the time’-perspectives of elderly kidney transplant recipients: Thematic synthesis of qualitative research. Nephrol Dial Transplant 31: 1531–1540, 2016 [DOI] [PubMed] [Google Scholar]
- 25.Tong A, Sainsbury P, Craig J: Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int J Qual Health Care 19: 349–357, 2007 [DOI] [PubMed] [Google Scholar]
- 26.Hartmann EL, Kitzman D, Rocco M, Leng X, Klepin H, Gordon M, Rejeski J, Berry M, Kritchevsky S: Physical function in older candidates for renal transplantation: An impaired population. Clin J Am Soc Nephrol 4: 588–594, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zelle DM, Corpeleijn E, Stolk RP, de Greef MHG, Gans ROB, van der Heide JJH, Navis G, Bakker SJL: Low physical activity and risk of cardiovascular and all-cause mortality in renal transplant recipients. Clin J Am Soc Nephrol 6: 898–905, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kasbia GS, Farragher J, Kim SJ, Famure O, Jassal SV: A cross-sectional study examining the functional independence of elderly individuals with a functioning kidney transplant. Transplantation 98: 864–870, 2014 [DOI] [PubMed] [Google Scholar]
- 29.Greenwood SA, Lindup H, Taylor K, Koufaki P, Rush R, Macdougall IC, Mercer TH: Evaluation of a pragmatic exercise rehabilitation programme in chronic kidney disease. Nephrol Dial Transplant 27[Suppl 3]: iii126–iii134, 2012 [DOI] [PubMed] [Google Scholar]
- 30.McAdams-Demarco MA, Grams ME, Hall EC, Coresh J, Segev DL: Early hospital readmission after kidney transplantation: Patient and center-level associations. Am J Transplant 12: 3283–3288, 2012 [DOI] [PubMed] [Google Scholar]
- 31.Dempster NJ, Ceresa CD, Aitken E, Kingsmore D: Outcomes following renal transplantation in older people: A retrospective cohort study. BMC Geriatr 13: 79, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Schell JO, Patel UD, Steinhauser KE, Ammarell N, Tulsky JA: Discussions of the kidney disease trajectory by elderly patients and nephrologists: A qualitative study. Am J Kidney Dis 59: 495–503, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pollak KI, Childers JW, Arnold RM: Applying motivational interviewing techniques to palliative care communication. J Palliat Med 14: 587–592, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Back AL, Arnold RM, Baile WF, Tulsky JA, Fryer-Edwards K: Approaching difficult communication tasks in oncology. CA Cancer J Clin 55: 164–177, 2005 [DOI] [PubMed] [Google Scholar]
- 35.Baile WF, Buckman R, Lenzi R, Glober G, Beale EA, Kudelka AP: SPIKES-A six-step protocol for delivering bad news: Application to the patient with cancer. Oncologist 5: 302–311, 2000 [DOI] [PubMed] [Google Scholar]
- 36.Barry MJ, Edgman-Levitan S: Shared decision making—Pinnacle of patient-centered care. N Engl J Med 366: 780–781, 2012 [DOI] [PubMed] [Google Scholar]
- 37.Peters TG, Spinola KN, West JC, Aeder MI, Danovitch GM, Klintmalm GB, Gorman KJ, Gordon JA, Kincaid CH, First MR: Differences in patient and transplant professional perceptions of immunosuppression-induced cosmetic side effects. Transplantation 78: 537–543, 2004 [DOI] [PubMed] [Google Scholar]
- 38.Reuben DB, Tinetti ME: Goal-oriented patient care—An alternative health outcomes paradigm. N Engl J Med 366: 777–779, 2012 [DOI] [PubMed] [Google Scholar]
- 39.O’Hare AM, Szarka J, McFarland LV, Taylor JS, Sudore RL, Trivedi R, Reinke LF, Vig EK: Provider perspectives on advance care planning for patients with kidney disease: Whose job is it anyway? Clin J Am Soc Nephrol 11: 855–866, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.