Abstract
Background and objectives
Waitlist inactivity is a barrier to transplantation, because inactive candidates cannot receive deceased donor organ offers. We hypothesized that temporarily inactive kidney transplant candidates living in linguistically isolated communities would be less likely to achieve active waitlist status.
Design, setting, participants, & measurements
We merged Organ Procurement and Transplantation Network/United Network for Organ Sharing data with five-digit zip code socioeconomic data from the 2000 US Census. The cumulative incidence of conversion to active waitlist status, death, and delisting before conversion among 84,783 temporarily inactive adult kidney candidates from 2004 to 2012 was determined using competing risks methods. Competing risks regression was performed to characterize the association between linguistic isolation, incomplete transplantation evaluation, and conversion to active status. A household was determined to be linguistically isolated if all members ≥14 years old speak a non-English language and also, speak English less than very well.
Results
A total of 59,147 candidates (70% of the study population) achieved active status over the study period of 9.8 years. Median follow-up was 110 days (interquartile range, 42–276 days) for activated patients and 815 days (interquartile range, 361–1244 days) for candidates not activated. The cumulative incidence of activation over the study period was 74%, the cumulative incidence of death before conversion was 10%, and the cumulative incidence of delisting was 13%. After adjusting for other relevant covariates, living in a zip code with higher percentages of linguistically isolated households was associated with progressively lower subhazards of activation both in the overall population (reference: <1% linguistically isolated households; 1%–4.9% linguistically isolated: subhazard ratio, 0.89; 95% confidence interval, 0.86 to 0.93; 5%–9.9% linguistically isolated: subhazard ratio, 0.83; 95% confidence interval, 0.80 to 0.87; 10%–19.9% linguistically isolated: subhazard ratio, 0.76; 95% confidence interval, 0.72 to 0.80; and ≥20% linguistically isolated: subhazard ratio, 0.71; 95% confidence interval, 0.67 to 0.76) and among candidates designated temporarily inactive due to an incomplete transplant evaluation.
Conclusions
Our findings indicate that candidates residing in linguistically isolated communities are less likely to complete candidate evaluations and achieve active waitlist status.
Keywords: kidney transplantation, ethnicity, language, waitlist, race
Introduction
The increasing size of the kidney transplant waiting list is well documented and supports a growing demand for a limited number of kidney organs. As of November of 2015, the Organ Procurement and Transplantation Network (OPTN) recorded 101,283 candidates on the kidney transplant waiting list in the United States. Of these, approximately 30% were patients with inactive status (1). Patients designated temporarily inactive (status 7) are not eligible for deceased donor organ offers but may accrue waiting time toward kidney transplantation (2). Since 2003, when a United Network for Organ Sharing (UNOS) policy change allowed status 7 candidates to gain waiting time toward kidney transplantation, there has been a sixfold increase in the representation of status 7 candidates on the waiting list (1).
Approximately one third of newly waitlisted patients are registered under temporarily inactive status, and 74% of these candidates are inactive due to “candidate workup incomplete” (1). These trends may reflect the incentive to register a patient for transplant early before the candidate has been formally deemed suitable for transplantation to maximize waiting time and increase the probability of kidney transplantation (3). This waitlist practice assumes that the candidate will eventually complete the evaluation and transition from inactive to active status. Prior data indicate, however, that approximately one third of patients initially listed as temporarily inactive never achieve active status and therefore, are not transplanted (4). Waitlist inactivity consumes transplant program resources, affects waitlist mortality outcomes, and most importantly, is a barrier to eventual transplantation.
Although referral rates among racial/ethnic minority candidates to kidney transplant centers are improving, racial/ethnic minority candidates are less likely than non-Hispanic whites to advance through the stages of kidney transplant evaluation necessary to receive a transplant and transition to active status (4,5). We postulate that language barriers may contribute to this disparity. Indeed, high percentages of racial/ethnic minorities do not speak English, are limited English proficient, or are linguistically isolated, which puts them at risk for poor access to health care services and inferior clinical outcomes (6–11). In the US Census, a household was determined to be linguistically isolated if all members 14 years of age and over speak a non-English language and also, speak English less than very well. The objectives of this study were to determine if linguistic isolation affects access to the active transplant waiting list and explore the interplay of race/ethnicity and linguistic isolation on the transition from temporarily inactive to active status on the kidney transplant waiting list.
Materials and Methods
Study Population
The clinical and research activities being reported are consistent with the Principles of the Declaration of Istanbul as outlined in the Declaration of Istanbul on Organ Trafficking and Transplant Tourism. This was a retrospective observational cohort study using data from the OPTN/UNOS Standard Transplant Analysis and Research (STAR) registry files with follow-up to September 5, 2014. The study population was restricted to candidates with an initial registration for kidney transplantation after January 1, 2004, which was the first recorded date on the STAR registry waitlist history file and the beginning of the first full year after the UNOS policy change allowed candidates to accrue waiting time on the kidney waiting list while listed as status 7. To allow for a sufficient follow-up period, candidates registered for transplantation up to September 5, 2012 (2 years before the date of last follow-up in the database) were included.
All adult (18 years old or older) candidates for kidney transplant alone who were designated status 7 within 90 days of initial registration were included in the study. Those with multiple listings or missing reason for inactive status were excluded. The final study population consisted of 84,783 temporarily inactive kidney transplant candidates.
Measures
Our primary waitlist outcome was conversion to active status (activation). Time to active status was defined as the number of days from initial registration to the first designation of active status on the UNOS waitlist history file. Patients who were waitlist inactive until receiving a living donor transplant were regarded as having been activated on the date of their transplant. We considered all candidates who were activated at least once to be in the activated group, regardless of whether the candidate later reverted back to inactive status. Competing waitlist outcomes were death before waitlist activation and removal from the waiting list (i.e., delisting). A waitlist death was determined if the waitlist file contained record of a date of death and the candidate was removed from the waiting list. Candidates who were removed from the waitlist without record of death or transplant were considered delisted.
Our primary predictor variable was linguistic isolation as defined according to the definition put forth by the US Census, which labels a linguistically isolated household as one in which all members 14 years of age and over speak a non-English language and also, speak English less than very well. Data from the 2000 US Census, the year closest to the beginning of the study time period, were merged to OPTN/UNOS data using the zip code of residence as the common identifier to characterize whether a candidate originated from a linguistically isolated community. The degree of linguistic isolation was categorized according to the percentage of linguistically isolated households within a zip code (<1%, 1%–4.9%, 5%–9.9%, 10%–19.9%, and ≥20%).
Statistical Analyses
We performed univariate statistics including means and frequencies for all variables. Bivariate statistics were performed to examine variable relationships by active versus inactive status using the chi-squared or t test as appropriate. The cumulative incidence of transition to active status, defined as the time to the first record of waitlist activation, was calculated using competing risks methods, with death before activation or waitlist removal (delisting) as competing events.
The relative effect of linguistic isolation on time to active status was assessed using Fine and Gray (12) competing risks regression, which is a semiparametric proportional hazards model for the subdistribution of a covariate in the presence of competing risks. Subjects were censored at the end of the study period on September 5, 2014. Those who did not experience any of the outcomes of interest were considered to be in continued inactive status throughout the study period. Two separate multivariate models were run. In the first model (model 1), candidate predictors included sex, age, race/ethnicity, blood type, body mass index at listing, percentage of panel reactive antibodies (<80% versus ≥80%), dialysis status at waitlist registration, highest education level achieved, primary cause of ESRD, primary insurance type, and history of previous transplant. Race/ethnicity was categorized according to designations within the OPTN/UNOS database, which include white, black, Hispanic, Asian, and all others (consisting of “American Indian or Alaska native” and “native Hawaiian and other Pacific Islander” candidates). In the OPTN/UNOS database, black race consists of black, African, West Indian, Haitian, or “other Black or African-American” candidates, and Hispanic ethnicity consists of Mexican, Puerto Rican, Cuban, or “other Hispanic/Latino” ethnicities. A second multivariate model (model 2) was then run to adjust for neighborhood-level characteristics and included all covariates included in model 1 in addition to the percentages of linguistically isolated households, households below poverty level, and households with less than high school education within the candidate’s zip code of residence. Potential correlation within clusters was adjusted for by obtaining the robust variance estimate using zip code as the cluster variable.
We then analyzed whether linguistic isolation was a predictor of failure to complete the transplant evaluation. For this analysis, the study population was restricted to those who were assigned candidate workup incomplete as the reason for inactive status at the time of the initial registration. Using multivariate competing risks regression, the association of linguistic isolation with conversion to active status among candidates with an incomplete evaluation was assessed.
All P values were two tailed, and a P<0.05 was considered statistically significant. Stata version 12 (Stata Corp., College Station, TX) was used for all analyses.
Results
Baseline Characteristics
A total of 84,783 status 7 candidates on the kidney transplant waitlist were included in the study population (Table 1). The majority (71%) of candidates lived in zip codes where <10% of households were linguistically isolated. A total of 59,147 (70%) candidates were activated at least once over the study period of 9.8 years, and the remaining 25,636 (30%) remained inactive for the duration of their waitlisting. The median follow-up was 110 days (interquartile range, 42–276 days) for activated patients and 815 days (interquartile range, 361–1244 days) for candidates not achieving active status.
Table 1.
Baseline characteristics of the overall study population comparing those activated with those remaining inactive
| Candidate Characteristic | Overall | Activated | Inactive/Never Activated | P Value |
|---|---|---|---|---|
| Candidates | 84,783 (100) | 59,147 (69.8) | 25,636 (30.2) | — |
| Median age (25th, 75th), yr | 53 (42, 61) | 52 (41, 60) | 54 (45, 62) | <0.001 |
| Men | 50,476 (59.5) | 35,581 (60.2) | 14,895 (58.1) | <0.001 |
| Race/ethnicity | <0.001 | |||
| White | 41,015 (48.4) | 29,975 (50.7) | 11,040 (43.1) | |
| Black | 25,215 (29.7) | 16,769 (28.4) | 8446 (33.0) | |
| Hispanic | 12,563 (14.8) | 8241 (13.9) | 4332 (16.9) | |
| Asian | 4622 (5.5) | 3283 (5.6) | 1339 (5.2) | |
| Other | 1368 (1.6) | 879 (1.5) | 489 (1.9) | |
| Blood type | <0.001 | |||
| A | 28,486 (33.6) | 20,251 (34.2) | 8235 (32.1) | |
| B | 12,220 (14.4) | 8441 (14.3) | 3779 (14.7) | |
| AB | 3489 (4.1) | 2533 (4.3) | 956 (3.7) | |
| O | 40,588 (47.9) | 27,922 (47.2) | 12,666 (49.4) | |
| BMI at listing, kg/m2 | <0.001 | |||
| ≤30 | 52,582 (62.0) | 37,796 (63.9) | 14,786 (57.7) | |
| 30–34.9 | 18,657 (22.0) | 13,389 (22.6) | 5268 (20.6) | |
| 35–39.9 | 9932 (11.7) | 6235 (10.5) | 3697 (14.4) | |
| 40–44.9 | 2709 (3.2) | 1322 (2.2) | 1387 (5.4) | |
| 45–64.9 | 903 (1.1) | 405 (0.7) | 498 (1.9) | |
| Diabetes mellitus | 37,553 (44.3) | 24,003 (40.6) | 13,550 (52.9) | <0.001 |
| PRA | ||||
| Median (25th, 75th) | 0 (0, 28) | 0 (0, 37) | 0 (0, 9) | <0.001 |
| >80% | 11,482 (13.5) | 8850 (15.0) | 2632 (10.3) | <0.001 |
| Dialysis at listing | 62,018 (73.2) | 42,233 (71.4) | 19,785 (77.2) | <0.001 |
| Education level | <0.001 | |||
| Below high school | 5171 (6.1) | 3250 (5.5) | 1921 (7.5) | |
| High school or GED | 34,142 (40.3) | 23,195 (39.2) | 10,947 (42.7) | |
| College or above | 36,612 (43.2) | 26,599 (45.0) | 10,013 (39.1) | |
| Unknown | 8858 (10.5) | 6103 (10.3) | 2755 (10.8) | |
| Previous transplantation | 11,916 (14.1) | 8636 (14.6) | 3280 (12.8) | <0.001 |
| Primary cause of ESRD, % | <0.001 | |||
| Diabetes | 28,760 (33.9) | 18,244 (30.9) | 10,516 (41.0) | |
| Hypertension | 17,775 (21.0) | 12,142 (20.5) | 5633 (22.0) | |
| GN | 13,429 (15.8) | 10,550 (17.8) | 2879 (11.2) | |
| Polycystic kidney disease | 5681 (6.7) | 4652 (7.9) | 1029 (4.0) | |
| Other | 19,138 (22.6) | 13,559 (22.9) | 5579 (21.8) | |
| Public insurance | 46,694 (55.1) | 30,430 (51.5) | 16,264 (63.4) | <0.001 |
| Zip code–level characteristics | ||||
| Linguistically isolated households | <0.001 | |||
| <1 | 8166 (9.6) | 6102 (10.3) | 2064 (8.1) | |
| 1–4.9 | 38,406 (45.30) | 27,626 (46.7) | 10,780 (42.10) | |
| 5–9.9 | 13,495 (15.9) | 9493 (16.1) | 4002 (15.6) | |
| 10–19.9 | 11,765 (13.9) | 7760 (13.1) | 4005 (15.6) | |
| ≥20 | 12,951 (15.3) | 8166 (13.8) | 4785 (18.7) | |
| Households below poverty level | <0.001 | |||
| <5 | 25,820 (30.5) | 18,827 (31.8) | 6993 (27.3) | |
| 5–9.9 | 23,666 (27.9) | 16,899 (28.6) | 6767 (26.4) | |
| 10–19.9 | 22,998 (27.1) | 15,597 (26.4) | 7401 (28.9) | |
| ≥20 | 12,299 (14.5) | 7824 (13.2) | 4475 (17.5) | |
| Households with < HS education | <0.001 | |||
| <5 | 33,147 (39.1) | 24,296 (41.1) | 8851 (34.5) | |
| 5–9.9 | 26,871 (31.7) | 18,766 (31.7) | 8105 (31.6) | |
| 10–19.9 | 18,109 (21.4) | 11,926 (20.2) | 6183 (24.1) | |
| ≥20 | 6656 (7.9) | 4159 (7.0) | 2497 (9.7) | |
| Reasons for inactive status | <0.001 | |||
| Transplant evaluation incomplete | 46,165 (54.5) | 30,956 (52.3) | 15,209 (59.3) | |
| Other | 38,618 (45.6) | 28,191 (47.7) | 10,427 (40.7) |
Values are presented as N (%) unless otherwise indicated. —, not applicable; BMI, body mass index; PRA, panel reactive antibody; GED, General Education Diploma; HS, high school.
Activated candidates were slightly younger and more often men compared with inactive/never activated candidates. A larger percentage of white candidates was activated, whereas the representation of black and Hispanic candidates was greater among those who were inactive/never activated. There were fewer diabetic and obese candidates and more candidates who were waitlisted before dialysis among the activated group. The inactive/never activated group was generally less educated and more likely to be primarily publically insured.
Zip code–level characteristics indicated that inactive/never activated candidates were more likely to originate from communities with higher degrees of linguistic isolation. Additionally, inactive/never activated candidates generally lived in communities with lower education and increased poverty.
The most common reason for inactive status in both groups was an incomplete transplant evaluation. Fewer activated candidates were inactive at waitlisting because of an incomplete transplant evaluation than inactivate/never activated candidates.
Table 2 shows the distribution of linguistic isolation across racial groups. More white candidates resided in communities that were not linguistically isolated (<1% linguistically isolated households). There was a markedly higher representation of Hispanic and Asian candidates compared with white and black candidates in linguistically isolated communities (10%–19.9% and ≥20% linguistically isolated households).
Table 2.
Distribution of candidates by race/ethnicity and percentage of linguistically isolated households
| Linguistically Isolated Households, N (%) | White, N (%) | Black, N (%) | Hispanic, N (%) | Asian, N (%) | Other, N (%) |
|---|---|---|---|---|---|
| <1 | 6110 (14.9) | 1843 (7.3) | 70 (0.6) | 68 (1.5) | 75 (5.5) |
| 1–4.9 | 22417 (54.7) | 13077 (51.9) | 1394 (11.1) | 969 (21.0) | 549 (40.1) |
| 5–9.9 | 6442 (15.7) | 4179 (16.6) | 1708 (13.6) | 929 (20.1) | 237 (17.3) |
| 10–19.9 | 3822 (9.3) | 3582 (14.2) | 2979 (23.7) | 1113 (24.1) | 269 (19.7) |
| ≥20 | 2224 (5.4) | 2534 (10.1) | 6412 (51.0) | 1543 (33.4) | 238 (17.4) |
| Total | 41,015 | 25,215 | 12,563 | 4622 | 1368 |
Cumulative Incidence of Conversion to Active Status
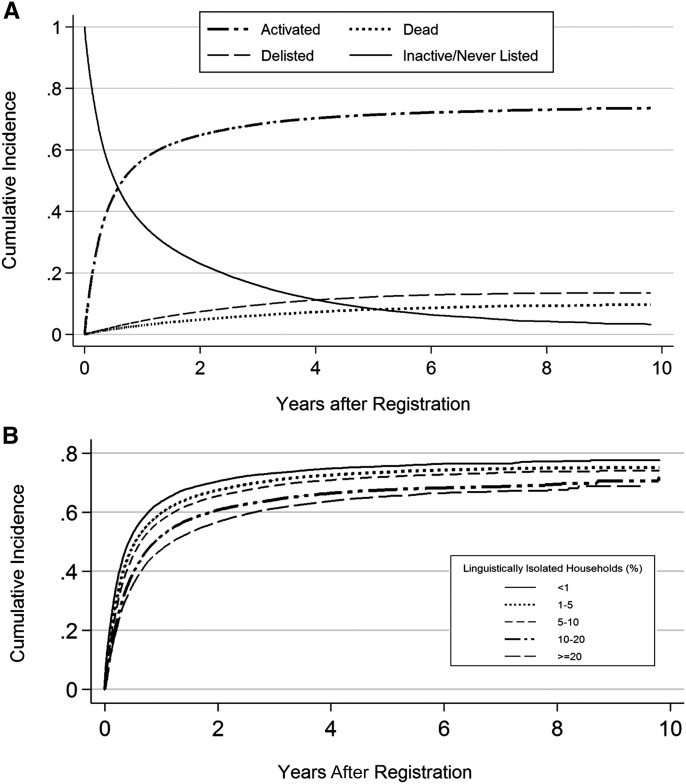
Figure 1A shows the cumulative incidence of conversion to active status, death, and delisting over the follow-up period. The cumulative incidence of death and delisting is a competing event among inactive candidates and does not reflect events that occurred after candidates were made active on the waitlist. The majority of candidates transitioned to active status within 1 year of registration, and comparatively few candidates transitioned to active status after being in inactive status >2 years. The cumulative incidence of conversion to active status was 64% at 2 years; by the end of the study period after 9.8 years of follow-up, the overall cumulative incidence of candidates transitioning to active status was 74%; 10% of candidates died before waitlist activation, and 13% were delisted.
Figure 1.
Cumulative incidence of conversion to active status. (A) Conversion to active status, death, and delisting in the overall study population. (B) Univariate effect of linguistic isoliation on the cumulative incidence of conversion to active status.
Figure 1B shows that the cumulative incidence of conversion to active status is inversely associated with the degree of linguistic isolation (P<0.001). The cumulative incidence of conversion to active status was 78% for candidates residing in communities that were <1% linguistically isolated compared with 69% among candidates from communities that were ≥20% linguistically isolated.
Competing Risks Regression
Table 3 shows the results of competing risks regression on time to transition to active status. Univariate analysis produced progressively lower subhazards of conversion to active status for candidates from zip codes with a higher percentage of linguistically isolated households. Black, Hispanic, and Asian candidates were less likely to convert to active status than white candidates on univariate analysis.
Table 3.
Univariate and multivariate competing risks regressions for conversion to active status in the overall population
| Variable (Reference) and Level | Univariate | Multivariate Model 1a | Multivariate Model 2b | |||
|---|---|---|---|---|---|---|
| Subhazard Ratio (95% CI) | P Value | Subhazard Ratio (95% CI) | P Value | Subhazard Ratio (95% CI) | P Value | |
| Sex (women) | ||||||
| Men | 1.05 (1.03 to 1.07) | <0.001 | 1.08 (1.06 to 1.10) | <0.001 | 1.08 (1.06 to 1.10) | <0.001 |
| Age (<40), yr | ||||||
| 40–49 | 0.91 (0.89 to 0.94) | <0.001 | 0.91 (0.89 to 0.94) | <0.001 | 0.92 (0.89 to 0.94) | <0.001 |
| 50–59 | 0.84 (0.82 to 0.86) | <0.001 | 0.85 (0.82 to 0.87) | <0.001 | 0.85 (0.83 to 0.87) | <0.001 |
| ≥60 | 0.80 (0.78 to 0.82) | <0.001 | 0.81 (0.79 to 0.83) | <0.001 | 0.81 (0.79 to 0.83) | <0.001 |
| Race/ethnicity, % (white) | ||||||
| Black | 0.78 (0.77 to 0.80) | <0.001 | 0.84 (0.82 to 0.87) | <0.001 | 0.87 (0.85 to 0.89) | <0.001 |
| Hispanic | 0.76 (0.73 to 0.79) | <0.001 | 0.86 (0.82 to 0.88) | <0.001 | 0.98 (0.95 to 1.02) | 0.36 |
| Asian | 0.88 (0.85 to 0.92) | <0.001 | 0.86 (0.82 to 0.90) | <0.001 | 0.96 (0.92 to 1.00) | 0.04 |
| Other | 0.75 (0.70 to 0.81) | <0.001 | 0.82 (0.76 to 0.88) | <0.001 | 0.87 (0.80 to 0.94) | <0.001 |
| Blood type (O) | ||||||
| A | 1.07 (1.06 to 1.09) | <0.001 | 1.04 (1.02 to 1.06) | <0.001 | 1.04 (1.02 to 1.06) | <0.001 |
| B | 1.00 (0.98 to 1.02) | 0.99 | 1.03 (1.00 to 1.05) | 0.05 | 1.03 (1.00 to 1.05) | 0.05 |
| AB | 1.10 (1.06 to 1.15) | <0.001 | 1.08 (1.03 to 1.13) | <0.001 | 1.08 (1.04 to 1.13) | <0.001 |
| BMI at listing (<30 kg/m2), % | ||||||
| 30–34.9 | 1.00 (0.98 to 1.02) | 0.85 | 1.03 (1.01 to 1.05) | 0.02 | 1.02 (1.00 to 1.04) | 0.07 |
| 35–39.9 | 0.76 (0.73 to 0.78) | <0.001 | 0.77 (0.75 to 0.80) | <0.001 | 0.77 (0.75 to 0.79) | <0.001 |
| 40–44.9 | 0.49 (0.47 to 0.52) | <0.001 | 0.50 (0.47 to 0.53) | <0.001 | 0.50 (0.47 to 0.52) | <0.001 |
| 45–64.9 | 0.44 (0.40 to 0.49) | <0.001 | 0.44 (0.40 to 0.48) | <0.001 | 0.44 (0.40 to 0.49) | <0.001 |
| PRA (<80%) | ||||||
| ≥80% | 1.20 (1.18 to 1.23) | <0.001 | 1.25 (1.22 to 1.28) | <0.001 | 1.24 (1.21 to 1.27) | <0.001 |
| Dialysis at listing (no) | ||||||
| Yes | 0.86 (0.85 to 0.88) | <0.001 | 0.99 (0.97 to 1.01) | 0.39 | 1.00 (0.98 to 1.02) | 0.76 |
| Education (college or above) | ||||||
| Less than high school | 0.75 (0.72 to 0.79) | <0.001 | 0.94 (0.88 to 0.99) | 0.03 | 0.95 (0.90 to 1.01) | 0.12 |
| High school or GED | 0.87 (0.86 to 0.89) | <0.001 | 0.95 (0.92 to 0.98) | 0.002 | 0.94 (0.91 to 0.97) | <0.001 |
| Unknown | 0.91 (0.88 to 0.94) | <0.001 | 1.02 (1.00 to 1.04) | 0.02 | 1.02 (1.00 to 1.04) | 0.01 |
| Primary cause of ESRD (diabetes) | ||||||
| Hypertension | 1.13 (1.10 to 1.15) | 1.14 (1.11 to 1.17) | <0.001 | 1.14 (1.11 to 1.17) | <0.001 | |
| GN | 1.49 (1.46 to 1.53) | <0.001 | 1.34 (1.31 to 1.38) | <0.001 | 1.33 (1.29 to 1.36) | <0.001 |
| Polycystic kidney | 1.63 (1.57 to 1.68) | <0.001 | 1.40 (1.35 to 1.45) | <0.001 | 1.39 (1.34 to 1.44) | <0.001 |
| Other | 1.22 (1.19 to 1.25) | <0.001 | 1.11 (1.08 to 1.14) | <0.001 | 1.11 (1.08 to 1.14) | <0.001 |
| Insurance type (private) | ||||||
| Public | 0.76 (0.75 to 0.77) | <0.001 | 0.80 (0.79 to 0.82) | <0.001 | 0.80 (0.78 to 0.81) | <0.001 |
| Previous transplant (no) | ||||||
| Yes | 1.07 (1.05 to 1.10) | <0.001 | 0.90 (0.88 to 0.93) | <0.001 | 0.90 (0.88 to 0.93) | <0.001 |
| Zip code–level characteristic | <0.001 | |||||
| Linguistically isolated households (<1%), % | ||||||
| 1–4.9 | 0.89 (0.85 to 0.92) | <0.001 | — | — | 0.89 (0.86 to 0.93) | <0.001 |
| 5–9.9 | 0.83 (0.79 to 0.87) | <0.001 | — | — | 0.83 (0.80 to 0.87) | <0.001 |
| 10–19.9 | 0.72 (0.69 to 0.76) | <0.001 | — | — | 0.76 (0.72 to 0.80) | <0.001 |
| ≥20 | 0.66 (0.63 to 0.69) | <0.001 | — | — | 0.71 (0.67 to 0.76) | <0.001 |
| Households below poverty level (<5%), % | ||||||
| 5–9.9 | 0.96 (0.93 to 0.99) | <0.01 | — | — | 1.03 (1.00 to 1.07) | 0.03 |
| 10–19.9 | 0.86 (0.83 to 0.89) | <0.001 | — | — | 1.03 (0.99 to 1.07) | 0.12 |
| ≥20 | 0.74 (0.71 to 0.77) | <0.001 | — | — | 1.00 (0.95 to 1.06) | 0.99 |
| Zip code households with less than high school education (<5%), % | ||||||
| 5–9.9 | 0.91 (0.88 to 0.93) | <0.001 | — | — | 0.98 (0.95 to 1.06) | 0.24 |
| 10–19.9 | 0.80 (0.77 to 0.83) | <0.001 | — | — | 0.95 (0.91 to 0.99) | 0.03 |
| ≥20 | 0.71 (0.67 to 0.75) | <0.001 | — | — | 0.98 (0.90 to 1.06) | 0.61 |
95% CI, 95% confidence interval; BMI, body mass index; PRA, panel reactive antibody; GED, General Education Diploma; —, not applicable.
Multivariate model 1 was adjusted for sex, age, race/ethnicity, blood type, BMI at listing, percentage of PRAs (<80% versus ≥80%), dialysis status at waitlist registration, highest education level achieved, primary cause of ESRD, primary insurance type, and history of previous transplant.
Multivariate model 2 was adjusted for all covariates in multivariate model 1 in addition to percentages of linguistically isolated households, households below poverty level, and households with less than high school education within the candidate’s zip code of residence.
Two separate multivariate models were then run to assess the effect of linguistic isolation and race/ethnicity on conversion to active status. The first model included all covariates examined on univariate analysis, except for the zip code–level characteristics of linguistic isolation, poverty level, and education. In this model, black, Hispanic, and Asian candidates remained less likely to convert to active status compared with white candidates (Table 3, model 1). When zip code–level characteristics were added to the model, Hispanic ethnicity was no longer associated with conversion to active status (Table 3, model 2). Asian candidates remained less likely to convert to active status than whites, but the magnitude of effect was small. The inference for black candidates did not change appreciably. This indicates that socioeconomic factors, such as linguistic isolation, poverty, and education, confound the effect of Hispanic ethnicity on conversion to active status.
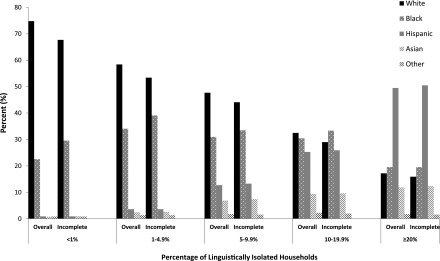
Incomplete Transplant Evaluations
The proportion of candidates designated status 7 due to candidate workup incomplete within each linguistic isolation category was progressively higher with higher degrees of linguistic isolation and ranged from 50% of candidates originating from zip codes with <1% of households that were linguistically isolated to 60% of candidates originating from zip codes with ≥20% linguistic isolation. Figure 2 compares the distribution of race/ethnicity across each linguistic isolation category in the overall status 7 population and among candidates who were designated status 7 because of candidate workup incomplete. Compared with the overall population, there were higher percentages of black candidates and corresponding lower percentages of white candidates designated status 7 due to an incomplete transplant evaluation who resided in neighborhoods with relatively lower degrees of linguistic isolation (<10% isolated). In neighborhoods with higher degrees of linguistic isolation (≥10% isolated), there was little difference in the distribution of race/ethnicity in the overall population and among those designated status 7 due to an incomplete transplant evaluation. The distribution of Hispanic and Asian candidates across all linguistic isolation categories was similar between the overall population and the subgroup of candidates with an incomplete evaluation.
Figure 2.
Race/ethnicity and linguistic isolation. Comparison of the distribution of race/ethnicity across linguistic isolation categories in the overall status 7 population and a subgroup of candidates designated status 7 because of candidate workup being incomplete.
The cumulative incidence of conversion to active status among candidates designated inactive at the time of waitlist registration due to candidate workup incomplete was 71% (data not shown); 10% of such candidates died without being active status, and 13% were delisted. These incidences were similar to those observed in the overall study population. Table 4 shows the results of univariate and multivariate competing risks regressions for the outcome of conversion to active status among candidates with an incomplete transplant evaluation. Similar to the overall population, candidates originating from communities with higher degrees of linguistic isolation were less likely to convert to active status after controlling for other covariates. In particular, black and Hispanic candidates were less likely to convert to active status than white candidates. There was no association between Asian race and conversion to active status on multivariate analysis.
Table 4.
Univariate and multivariate competing risks regressions for conversion to active status among patients designated inactive due to incomplete candidate evaluation
| Variable (Reference) and Level | Univariate | Multivariatea | ||
|---|---|---|---|---|
| Subhazard Ratio (95% CI) | P Value | Subhazard Ratio (95% CI) | P Value | |
| Sex (women) | ||||
| Men | 1.04 (1.02 to 1.07) | <0.001 | 1.08 (1.06 to 1.11) | <0.001 |
| Age (<40), yr | ||||
| 40–49 | 0.88 (0.86 to 0.92) | <0.001 | 0.89 (0.86 to 0.92) | <0.001 |
| 50–59 | 0.82 (0.80 to 0.85) | <0.001 | 0.83 (0.80 to 0.86) | <0.001 |
| ≥60 | 0.80 (0.78 to 0.83) | <0.001 | 0.81 (0.78 to 0.84) | <0.001 |
| Race/ethnicity, % (white) | ||||
| Black | 0.80 (0.77 to 0.82) | <0.001 | 0.86 (0.84 to 0.89) | <0.001 |
| Hispanic | 0.72 (0.69 to 0.75) | <0.001 | 0.90 (0.86 to 0.94) | <0.001 |
| Asian | 0.91 (0.86 to 0.96) | 0.001 | 0.98 (0.93 to 1.03) | 0.37 |
| Other | 0.72 (0.65 to 0.80) | <0.001 | 0.81 (0.73 to 0.90) | <0.001 |
| Blood type (O) | ||||
| A | 1.08 (1.05 to 1.11) | <0.001 | 1.04 (1.02 to 1.07) | 0.001 |
| B | 1.00 (0.96 to 1.03) | 0.80 | 1.01 (0.98 to 1.04) | 0.59 |
| AB | 1.11 (1.05 to 1.18) | <0.001 | 1.08 (1.03 to 1.15) | <0.01 |
| BMI at listing (<30 kg/m2), % | ||||
| 30–34.9 | 0.99 (0.96 to 1.02) | 0.41 | 1.02 (0.99 to 1.04) | 0.28 |
| 35–39.9 | 0.78 (0.75 to 0.81) | <0.001 | 0.79 (0.76 to 0.82) | <0.001 |
| 40–44.9 | 0.56 (0.52 to 0.61) | <0.001 | 0.55 (0.51 to 0.60) | <0.001 |
| 45–64.9 | 0.55 (0.48 to 0.64) | <0.001 | 0.55 (0.48 to 0.64) | <0.001 |
| PRA (<80%) | ||||
| ≥80% | 1.23 (1.20 to 1.27) | <0.001 | 1.26 (1.22 to 1.31) | <0.001 |
| Dialysis at listing (no) | ||||
| Yes | 0.85 (0.83 to 0.87) | <0.001 | 0.96 (0.93 to 0.99) | 0.003 |
| Education (college or above) | ||||
| Less than high school | 0.72 (0.69 to 0.76) | <0.001 | 0.89 (0.84 to 0.93) | <0.001 |
| High school or GED | 0.86 (0.83 to 0.88) | <0.001 | 0.90 (0.88 to 0.93) | <0.001 |
| Unknown | 0.83 (0.79 to 0.87) | <0.001 | 0.88 (0.84 to 0.92) | <0.001 |
| Primary cause of ESRD (diabetes) | ||||
| Hypertension | 1.12 (1.08 to 1.16) | <0.001 | 1.12 (1.09 to 1.16) | <0.001 |
| GN | 1.49 (1.44 to 1.55) | <0.001 | 1.32 (1.27 to 1.37) | <0.001 |
| Polycystic kidney | 1.59 (1.51 to 1.66) | <0.001 | 1.37 (1.30 to 1.43) | <0.001 |
| Other | 1.24 (1.20 to 1.28) | <0.001 | 1.11 (1.07 to 1.15) | <0.001 |
| Insurance type (private) | ||||
| Public | 0.77 (0.76 to 0.79) | <0.001 | 0.82 (0.80 to 0.85) | <0.001 |
| Previous transplant (no) | ||||
| Yes | 1.11 (1.08 to 1.15) | <0.001 | 0.91 (0.88 to 0.95) | <0.001 |
| Zip code–level characteristic | ||||
| Linguistically isolated households (<1%), % | ||||
| 1–4.9 | 0.93 (0.88 to 0.98) | <0.01 | 0.94 (0.89 to 0.98) | <0.01 |
| 5–9.9 | 0.91 (0.86 to 0.96) | 0.001 | 0.91 (0.86 to 0.95) | <0.001 |
| 10–19.9 | 0.80 (0.75 to 0.86) | <0.001 | 0.84 (0.79 to 0.89) | <0.001 |
| ≥20 | 0.70 (0.66 to 0.75) | <0.001 | 0.79 (0.74 to 0.85) | <0.001 |
| Households below poverty level (<5%), % | ||||
| 5–9.9 | 0.93 (0.90 to 0.97) | 0.001 | 1.01 (0.98 to 1.06) | 0.46 |
| 10–19.9 | 0.85 (0.81 to 0.88) | <0.001 | 1.02 (0.97 to 1.07) | 0.40 |
| ≥20 | 0.73 (0.70 to 0.76) | <0.001 | 0.99 (0.93 to 1.05) | 0.68 |
| Zip code households with less than high school education (<5%), % | ||||
| 5–9.9 | 0.89 (0.86 to 0.92) | <0.001 | 0.96 (0.93 to 1.00) | 0.08 |
| 10–19.9 | 0.80 (0.77 to 0.83) | <0.001 | 0.94 (0.89 to 0.99) | 0.03 |
| ≥20 | 0.69 (0.65 to 0.73) | <0.001 | 0.96 (0.87 to 1.05) | 0.36 |
95% CI, 95% confidence interval; BMI, body mass index; PRA, panel reactive antibody; GED, General Education Diploma.
Multivariate model 1 was adjusted for sex, age, race/ethnicity, blood type, BMI at listing, percentage of PRAs (<80% versus ≥80%), dialysis status at waitlist registration, highest education level achieved, primary cause of ESRD, primary insurance type, history of previous transplant, and percentages of linguistically isolated households, households below poverty level, and households with less than high school education within the candidate’s zip code of residence.
Discussion
This study investigated the effect of linguistic isolation on waitlist outcomes among temporarily inactive kidney transplant candidates in the United States. Progressively higher degrees of linguistic isolation were independently associated with a decrease in the subhazard of conversion to active status across all racial/ethnic groups and incomplete transplant evaluations. Among those designated temporarily inactive because of an incomplete transplant evaluation, black and Hispanic candidates were less likely to transition to active status.
Data from the OPTN over the last decade show that the growth in the number of candidates awaiting kidney transplantation is not due to an increase in the number of patients in active status, but rather, it is attributed to an increase in the inactive waitlist population (1). Prior data suggest that post-transplant survival among status 7 kidney recipients is comparable with that of recipients who have never been inactive (3,4,13). This suggests that many candidates in inactive status on the waitlist would derive a survival benefit from kidney transplantation similar to candidates in active status. Identification of factors that affect waitlist inactivity in patients from linguistically isolated communities is paramount for creating broader access to transplantation and reducing health disparities in underserved communities.
Linguistic isolation has been previously shown to be associated with a decrease in transplantation rates (14,15), even after adjustment for employment, income, and education (16). Our data indicate that candidates from linguistically isolated communities are more likely to remain in inactive waitlist status. Linguistic isolation is associated with incomplete transplant evaluations and may hinder patient-provider communication and education. Previous studies have shown that linguistic barriers are associated with reduced knowledge of health conditions and treatments (17,18), use of health services, and inferior medical outcomes (6–11,19–22). It has also been shown that the quality of transplant education measured by the amount of time spent by the patient talking to a doctor or medical staff or reading about transplantation is correlated with timely completion of the transplant evaluation (23). Improved patient-provider communication may also increase living donor transplantation rates. In a single-center, randomized, controlled trial, patients who received in-home discussions had a higher number of living donor inquiries and evaluations and a trend toward more living donor transplants (24). Patients who are linguistically isolated may have decreased access to educational resources in their primary language and may be limited in their ability to communicate with their providers and the transplant center. Examining whether or to what extent linguistically isolated patients have reduced access to education about transplant is a critical next direction for research.
There is likely a complex relationship between language and other sociodemographic factors, including race/ethnicity, health status, income, and education. Prior data indicate that blacks are generally less likely to be waitlisted than white candidates, but the disparity is not uniform across all UNOS regions (25). Hispanics are less likely to receive a deceased donor kidney transplant than non-Hispanic whites but do not differ with respect to waitlisting. These differences arise largely on the basis of geographic location (26). Our study shows that Hispanic ethnicity, as designated in the OPTN/UNOS database, is associated with decreased transition to active status, but the effect is confounded by socioeconomic factors. After adjusting for linguistic isolation, income, and education, Hispanic ethnicity is no longer associated with transition to active status. This suggests that disparities in access to the active transplant list among Hispanics are heavily influenced by these socioeconomic factors and that English language fluency may be an important predictor of active kidney waitlisting in the Hispanic population.
There are limitations to this study. The retrospective nature of the study allows us to only identify an association between linguistic isolation and transition to active status but does not prove causality. However, there is ample literature on education and access to transplantation, which is highly reliant on provider-patient communication (27–30). Linguistic isolation hinders the ability to educate through social media, mobile applications, internet resources, and patient-provider interaction. Studies are currently underway to use newer technologies to educate patients about kidney transplantation and may be extended to target patients with limited English proficiency (31–33). Additionally, this study used community-level measures of linguistic isolation as a marker of language proficiency. We have identified that linguistic isolation is associated with decreased access to the active waiting list; however, we cannot exclude the possibility of residual confounding by other unmeasured factors that may have been responsible for the association between linguistic isolation and lower access to the active waiting list. Nevertheless, the effect of linguistic isolation persisted, even after adjusting for important socioeconomic measures of income, insurance status, and education. It is important to note that many other biologic and sociodemographic factors were also independently associated in the multivariate models and work together to influence active waitlisting.
In summary, this study shows that linguistic isolation is associated with a lower likelihood of transitioning from inactive to active status on the kidney transplant waiting list and completing transplant evaluations in a timely manner. Additional interventional studies to improve communication with linguistically isolated candidates would be of use to improve access to transplantation for these candidates.
Disclosures
None.
Acknowledgments
E.T. was supported by Health Resources and Services Administration (HRSA) Institutional National Research Service Award at the University of California, Los Angeles (UCLA) grant T32HP19001, the UCLA and Charles Drew University Resource Centers for Minority Aging Research Center for Health Improvement of Minority Elderly under National Institutes of Health (NIH)/National Institute on Aging (NIA) grant P30-AG021684, and the UCLA Clinical and Translational Science Institute under NIH/National Center for Advancing Translational Sciences (NCATS) grant UL1TR000124. C.M.M. received support from the UCLA Resource Centers for Minority Aging Research Center for Health Improvement of Minority Elderly under NIH/NIA grant P30AG021684, National Institute of Diabetes and Digestive and Kidney Diseases of the NIH grant R18DK105464, Centers for Disease Control and Prevention grant U18DP006140, and NIH/NCATS UCLA Clinical and Translational Science Institute grant UL1TR000124. C.M.M. holds the Barbara A. Levey and Gerald S. Levey Endowed Chair in Medicine, which partially supported her work. G.M. received support from NIA grant K23 AG042961-01 (Paul B. Beeson Career Development Award), the American Federation for Aging Research, and the UCLA Resource Center for Minority Aging Research/Center for Health Improvement of Minority Elderly under NIH/NIA grant P30AG021684. This work was supported, in part, by HRSA contract 231-00-0115.
C.M.M. is a member of the US Preventive Services Task Force (USPSTF). This article does not necessarily represent the views and policies of the USPSTF. The content does not necessarily represent the official views of the NIA or the NIH. The content is the responsibility of the authors alone and does not necessarily reflect the views or policies of the Department of Health and Human Services, and the mention of trade names, commercial products, or organizations does not imply endorsement by the US Government.
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
See related editorial, “Is the End in Sight for the “Don’t Ask, Don’t Tell” Approach to Advance Care Planning?,” on pages 380–381.
References
- 1.Matas AJ, Smith JM, Skeans MA, Thompson B, Gustafson SK, Stewart DE, Cherikh WS, Wainright JL, Boyle G, Snyder JJ, Israni AK, Kasiske BL: OPTN/SRTR 2013 annual data report: Kidney. Am J Transplant 15[Suppl 2]: 1–34, 2015 [DOI] [PubMed] [Google Scholar]
- 2.Delmonico FL, McBride MA: Analysis of the wait list and deaths among candidates waiting for a kidney transplant. Transplantation 86: 1678–1683, 2008 [DOI] [PubMed] [Google Scholar]
- 3.Huang E, Shye M, Elashoff D, Mehrnia A, Bunnapradist S: Incidence of conversion to active waitlist status among temporarily inactive obese renal transplant candidates. Transplantation 98: 177–186, 2014 [DOI] [PubMed] [Google Scholar]
- 4.Grams ME, Massie AB, Schold JD, Chen BP, Segev DL: Trends in the inactive kidney transplant waitlist and implications for candidate survival. Am J Transplant 13: 1012–1018, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sequist TD, Narva AS, Stiles SK, Karp SK, Cass A, Ayanian JZ: Access to renal transplantation among American Indians and Hispanics. Am J Kidney Dis 44: 344–352, 2004 [DOI] [PubMed] [Google Scholar]
- 6.Derose KP, Bahney BW, Lurie N, Escarce JJ: Review: Immigrants and health care access, quality, and cost. Med Care Res Rev 66: 355–408, 2009 [DOI] [PubMed] [Google Scholar]
- 7.Clough J, Lee S, Chae DH: Barriers to health care among Asian immigrants in the United States: A traditional review. J Health Care Poor Underserved 24: 384–403, 2013 [DOI] [PubMed] [Google Scholar]
- 8.Flores G: Language barriers to health care in the United States. N Engl J Med 355: 229–231, 2006 [DOI] [PubMed] [Google Scholar]
- 9.Fernandez A, Schillinger D, Warton EM, Adler N, Moffet HH, Schenker Y, Salgado MV, Ahmed A, Karter AJ: Language barriers, physician-patient language concordance, and glycemic control among insured Latinos with diabetes: The Diabetes Study of Northern California (DISTANCE). J Gen Intern Med 26: 170–176, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Karliner LS, Jacobs EA, Chen AH, Mutha S: Do professional interpreters improve clinical care for patients with limited English proficiency? A systematic review of the literature. Health Serv Res 42: 727–754, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pérez-Stable EJ, Nápoles-Springer A, Miramontes JM: The effects of ethnicity and language on medical outcomes of patients with hypertension or diabetes. Med Care 35: 1212–1219, 1997 [DOI] [PubMed] [Google Scholar]
- 12.Fine JP, Gray RJ: A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc 94: 496–509, 1999 [Google Scholar]
- 13.Leeaphorn N, Sampaio MS, Natal N, Mehrnia A, Kamgar M, Huang E, Kalantar-Zadeh K, Kaplan B, Bunnapradist S: Renal transplant outcomes in waitlist candidates with a previous inactive status due to being temporarily too sick. Clin Transpl 2014: 117–124 [PubMed] [Google Scholar]
- 14.Hall YN, Choi AI, Xu P, O’Hare AM, Chertow GM: Racial ethnic differences in rates and determinants of deceased donor kidney transplantation. J Am Soc Nephrol 22: 743–751, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hall YN, O’Hare AM, Young BA, Boyko EJ, Chertow GM: Neighborhood poverty and kidney transplantation among US Asians and Pacific Islanders with end-stage renal disease. Am J Transplant 8: 2402–2409, 2008 [DOI] [PubMed] [Google Scholar]
- 16.Patzer RE, Plantinga L, Krisher J, Pastan SO: Dialysis facility and network factors associated with low kidney transplantation rates among United States dialysis facilities. Am J Transplant 14: 1562–1572, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sadler GR, Ryujin LT, Ko CM, Nguyen E: Korean women: Breast cancer knowledge, attitudes and behaviors. BMC Public Health 1: 7, 2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hsu WC, Cheung S, Ong E, Wong K, Lin S, Leon K, Weinger K, King GL: Identification of linguistic barriers to diabetes knowledge and glycemic control in Chinese Americans with diabetes. Diabetes Care 29: 415–416, 2006 [DOI] [PubMed] [Google Scholar]
- 19.Flores G, Abreu M, Tomany-Korman SC: Limited english proficiency, primary language at home, and disparities in children’s health care: How language barriers are measured matters. Public Health Rep 120: 418–430, 2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Garbers S, Chiasson MA: Inadequate functional health literacy in Spanish as a barrier to cervical cancer screening among immigrant Latinas in New York City. Prev Chronic Dis 1: A07, 2004 [PMC free article] [PubMed] [Google Scholar]
- 21.Timmins CL: The impact of language barriers on the health care of Latinos in the United States: A review of the literature and guidelines for practice. J Midwifery Womens Health 47: 80–96, 2002 [DOI] [PubMed] [Google Scholar]
- 22.Fiscella K, Franks P, Doescher MP, Saver BG: Disparities in health care by race, ethnicity, and language among the insured: Findings from a national sample. Med Care 40: 52–59, 2002 [DOI] [PubMed] [Google Scholar]
- 23.Waterman AD, Peipert JD, Hyland SS, McCabe MS, Schenk EA, Liu J: Modifiable patient characteristics and racial disparities in evaluation completion and living donor transplant. Clin J Am Soc Nephrol 8: 995–1002, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rodrigue JR, Paek MJ, Egbuna O, Waterman AD, Schold JD, Pavlakis M, Mandelbrot DA: Making house calls increases living donor inquiries and evaluations for blacks on the kidney transplant waiting list. Transplantation 98: 979–986, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Saunders MR, Lee H, Alexander GC, Tak HJ, Thistlethwaite JR Jr., Ross LF: Racial disparities in reaching the renal transplant waitlist: Is geography as important as race? Clin Transplant 29: 531–538, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Arce CM, Goldstein BA, Mitani AA, Lenihan CR, Winkelmayer WC: Differences in access to kidney transplantation between Hispanic and non-Hispanic whites by geographic location in the United States. Clin J Am Soc Nephrol 8: 2149–2157, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Waterman AD, Peipert JD, Goalby CJ, Dinkel KM, Xiao H, Lentine KL: Assessing transplant education practices in dialysis centers: Comparing educator reported and Medicare data. Clin J Am Soc Nephrol 10: 1617–1625, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Boulware LE, Hill-Briggs F, Kraus ES, Melancon JK, Falcone B, Ephraim PL, Jaar BG, Gimenez L, Choi M, Senga M, Kolotos M, Lewis-Boyer L, Cook C, Light L, DePasquale N, Noletto T, Powe NR: Effectiveness of educational and social worker interventions to activate patients’ discussion and pursuit of preemptive living donor kidney transplantation: A randomized controlled trial. Am J Kidney Dis 61: 476–486, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Patzer RE, Perryman JP, Pastan S, Amaral S, Gazmararian JA, Klein M, Kutner N, McClellan WM: Impact of a patient education program on disparities in kidney transplant evaluation. Clin J Am Soc Nephrol 7: 648–655, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kucirka LM, Grams ME, Balhara KS, Jaar BG, Segev DL: Disparities in provision of transplant information affect access to kidney transplantation. Am J Transplant 12: 351–357, 2012 [DOI] [PubMed] [Google Scholar]
- 31.Waterman AD, McSorley A-MM, Peipert JD, Goalby CJ, Peace LJ, Lutz PA, Thein JL: Explore transplant at home: A randomized control trial of an educational intervention to increase transplant knowledge for Black and White socioeconomically disadvantaged dialysis patients. BMC Nephrol 16: 150, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Waterman AD, Robbins ML, Paiva AL, Peipert JD, Kynard-Amerson CS, Goalby CJ, Davis LA, Thein JL, Schenk EA, Baldwin KA, Skelton SL, Amoyal NR, Brick LA: Your path to transplant: A randomized controlled trial of a tailored computer education intervention to increase living donor kidney transplant. BMC Nephrol 15: 166, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Patzer RE, Gander J, Sauls L, Amamoo MA, Krisher J, Mulloy LL, Gibney E, Browne T, Plantinga L, Pastan SO; Southeastern Kidney Transplant Coalition : The RaDIANT community study protocol: Community-based participatory research for reducing disparities in access to kidney transplantation. BMC Nephrol 15: 171, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]