Abstract
Background and objectives
Patient centeredness is widely advocated as a cornerstone of health care, but it is yet to be fully realized, including in nephrology. Our study aims to describe nephrologists’ perspectives on defining and implementing patient-centered outcomes in hemodialysis.
Design, setting, participants, & measurements
Face-to-face, semistructured interviews were conducted with 58 nephrologists from 27 dialysis units across nine countries, including the United States, the United Kingdom, Australia, Austria, Belgium, Canada, Germany, Singapore, and New Zealand. Transcripts were thematically analyzed.
Results
We identified five themes on defining and implementing patient-centered outcomes in hemodialysis: explicitly prioritized by patients (articulated preferences and goals, ascertaining treatment burden, defining hemodialysis success, distinguishing a physician-patient dichotomy, and supporting shared decision making), optimizing wellbeing (respecting patient choice, focusing on symptomology, perceptible and tangible, and judging relevance and consequence), comprehending extensive heterogeneity of clinical and quality of life outcomes (distilling diverse priorities, highly individualized, attempting to specify outcomes, and broadening context), clinically hamstrung (professional deficiency, uncertainty and complexity in measurement, beyond medical purview, specificity of care, mechanistic mindset [focused on biochemical targets and comorbidities], avoiding alarm, and paradoxical dilemma), and undermined by system pressures (adhering to overarching policies, misalignment with mandates, and resource constraints).
Conclusions
Improving patient-centered outcomes is regarded by nephrologists to encompass strategies that address patient goals and improve wellbeing and treatment burden in patients on hemodialysis. However, efforts are hampered by ambiguities about how to prioritize, measure, and manage the plethora of critical comorbidities and broader quality of life outcomes in a care setting that is technically demanding and driven by biochemical targets. Identifying critical patient–important outcomes and mechanisms for integrating them into practice may help to deliver patient-centered care in hemodialysis and other chronic disease settings.
Keywords: hemodialysis, qualitative research, Australia, Austria, Belgium, Canada, Chronic Disease, Comorbidity, Decision Making, Germany, Goals, Great Britain, Humans, nephrology, New Zealand, Patient Selection, Patient-Centered Care, Physician-Patient Relations, quality of life, renal dialysis, Singapore, Uncertainty, United States
Introduction
Patient centeredness is widely advocated as a cornerstone of health care. Since being espoused in the Institute of Medicine landmark report Crossing the Quality Chasm: A New Health System for the 21st Century in 2001 (1), there have been increasing calls to integrate patient priorities and values in health care and research (2–11). Although major investments have been directed toward system redesign and patient–centered outcomes research (12–16), the vision of patient-centered care is yet to be fully realized (10,13,17–20).
Patient-centered care is defined as “providing care that is respectful of, and responsive to, individual patient preferences, needs and values, and ensuring that patient values guide all clinical decisions,” (1) and in the context of research, it is the “evaluation of questions and outcomes that are meaningful and important to patients and caregivers” (12). However, the ability to enact patient-centered care has been limited by uncertainties about what constitutes patient-centered outcomes and how to measure and apply them (13). Also, clinicians must negotiate complex tradeoffs between patient satisfaction and uncertainties around treatment effectiveness and safety (21,22). Other barriers include regulatory, organizational, and resource constraints and the omission of patient-important outcomes in research (2–5,13,19,23–26).
Achieving patient centeredness is highly relevant and particularly challenging in the context of hemodialysis—an intrusive intervention that inflicts a substantial burden on patients and health care systems. Globally, an estimated 2 million people with ESRD receive hemodialysis (27–31). Although lifesaving, high mortality, frequent treatment complications, and poor quality of life are profoundly evident (20,32–35). As the primary physicians caring for patients on hemodialysis, nephrologists have a critical role in facilitating shared decision making and delivering health care that integrates patients’ preferences and values (10,36). Their approach and decisions may be underpinned by the attitudes and assumptions about patient centeredness and how they contend with tensions within the health care systems and clinical and policy priorities. This study aims to describe nephrologists’ perspectives on defining and implementing patient-centered outcomes in patients receiving hemodialysis to inform appropriate and efficient strategies to improve patient-centered care in hemodialysis.
Materials and Methods
We used the Consolidated Criteria for Reporting Qualitative Health Research (37).
Participant Selection
Nephrologists with experience in providing care for adults on hemodialysis were eligible to participate. The investigators nominated a nephrologist at each city as well as potential participants who were purposively selected to include a range of age, sex, years of clinical experience in nephrology, practice locations, and size of hemodialysis units. Also, A.T. emailed the contact nephrologist, who suggested other colleagues who had relevant and different perspectives on patient-centered outcomes. The University of Sydney approved the study.
Data Collection
The interview guide was developed on the basis of a literature review on patient-centered outcomes (4,5,10,12,13,15,17,26,38–41) and discussion among the investigators (Supplemental Table 1). A.T. conducted in–person, semistructured interviews at hospital, university, or conference locations from May to October of 2015 until data saturation. All interviews were audiorecorded and transcribed verbatim.
Data Analyses
Using principles of grounded theory (42) and thematic analysis, A.T. coded the transcripts line by line and inductively identified concepts relating to participant perspectives on the meaning and implementation of patient-centered outcomes. We grouped similar concepts into themes; searched for patterns, broader overarching concepts, and links among the concepts; and mapped these into a thematic schema in Microsoft PowerPoint. This was discussed with the investigators and revised. To enhance the analytic framework, we used investigator triangulation, whereby the coding structure was discussed and revised with A.J. and E.O., who read the transcripts. A.T. coded the transcripts using HyperRESEARCH software (version 3.3; ResearchWare Inc.). The preliminary findings were sent to participants to provide feedback within a 2-week timeframe. Additional perspectives were incorporated into the final analysis (i.e., member checking).
Results
Of the 60 invited nephrologists, 58 (97%) from 27 dialysis units across nine countries were interviewed (Table 1). Nonparticipation was due to unavailability. The average duration of interviews was 40 minutes.
Table 1.
Participant demographic characteristics (n=58)
| Characteristics | N | Percentage |
|---|---|---|
| Sex | ||
| Men | 43 | 74 |
| Women | 15 | 26 |
| Age group, yr | ||
| 30–39 | 14 | 24 |
| 40–49 | 20 | 34 |
| 50–59 | 18 | 31 |
| 60–69 | 5 | 7 |
| 70–79 | 1 | 2 |
| Years of experience in hemodialysis | ||
| ≤10 | 14 | 24 |
| 11–20 | 22 | 38 |
| 21–30 | 14 | 24 |
| >30 | 8 | 14 |
| Country | ||
| United Kingdom | 14 | 24 |
| Australia | 13 | 22 |
| Belgium | 8 | 14 |
| United States | 7 | 12 |
| Austria | 5 | 7 |
| Canada | 4 | 7 |
| Germany | 4 | 7 |
| Singapore | 2 | 3 |
| New Zealand | 1 | 2 |
| Size of dialysis unit—no. of current patients on hemodialysis | ||
| 1–50 | 5 | 7 |
| 51–100 | 5 | 7 |
| 101–200 | 10 | 17 |
| 201–300 | 9 | 16 |
| 301–400 | 4 | 7 |
| >400 | 25 | 43 |
| Private practice | ||
| Yes | 12 | 21 |
| No | 46 | 79 |
| Interview venue | ||
| Hospital (office or meeting room) | 50 | 86 |
| Conference | 8 | 14 |
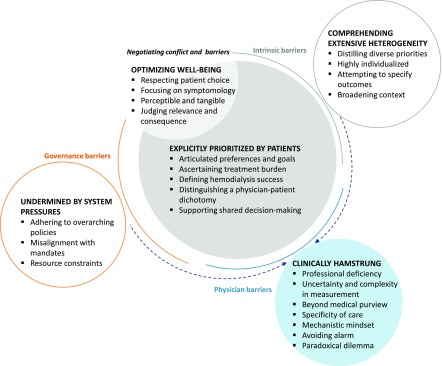
The diverse range and differences in opinion among the participants are presented in the five major themes that we identified: explicitly prioritized by patients, optimizing wellbeing, comprehending extensive heterogeneity, clinically hamstrung, and undermined by system pressures (Figure 1). Selected quotations to support each theme are provided in Table 2.
Figure 1.
Thematic schema of nephrologists' perspectives on patient-centered outcomes. Patient-centered outcomes were broadly conceptualized by nephrologists as outcomes that were explicitly prioritized by patients as important and relevant or relevant for their wellbeing, which could include symptoms or broader life effects. Identifying patient-centered outcomes was perceived to support shared decision making. However, some believed that patients may not have been able to identify certain outcomes as critical if they were not aware of the risk and consequences. Barriers to identifying and optimizing patient-centered outcomes included the heterogeneous and diverse range of outcomes that were perceived as difficult to measure, feasibility and resource constraints, and system pressures.
Table 2.
Selected participant quotations for each theme
| Theme | Selected Quotationsa |
|---|---|
| Explicitly prioritized by patients | |
| Articulated preferences and goals | “Outcomes that are important to the patient, therefore you have patient input as to what those outcomes are, not us figuring out what they are for the patient. That’s patriarchal. We know what’s best for you, let us tell you. It should be driven from the patients.” (Canada) |
| “I would define it as a holistic outcome, as defined by, or as chosen by the individual. So that might be holistic in the sense of spiritual or physical or family related.” (United Kingdom) | |
| “It comes down to being less paternalistic and trying to allow patients to express what they would like out of life, and trying to achieve those goals.” (Australia) | |
| Ascertaining treatment burden | “What part of burden of kidney disease is so onerous, what in their dialysis treatment is so bad to their physical functioning and mental functioning, and then, we can come back and develop a list priorities on how to improve what they think is causing their most burden. That would be the most patient–centered way to approach it.” (United States) |
| “A measure of burden of illness or intrusiveness of disease would also be a very important one in hemodialysis; it’s an intensive, time–consuming, life–altering intervention. Strategies to minimize that would also be very important to capture within a measure, measures of quality of life in hemodialysis.” (Canada) | |
| Defining hemodialysis success | “Going systematically to the patients and saying we’re going to try and make dialysis better, what is it that worries you about it?” (United Kingdom) |
| “I would imagine are outcomes that are important to the patient, so if you ask a patient ‘if we’re going to improve your health care or give you some new therapy, what would make a difference that would help you?’” (Australia) | |
| “Something that might change their journey, their experience of being on dialysis.” (Australia) | |
| Distinguishing a physician-patient dichotomy | “We think of something more medical as far as outcomes day to day, but you forget that patients have difficulty sleeping and will complain to you.” (United States) |
| “If you take a group of doctors and asked them how you’ve measured the quality of dialysis, they’d tell you about survival, BP control, hemoglobin levels, whereas patients will talk about completely different things, like do they manage to do what they want to do. Many patients will tell you that it’s quality of life rather than survival.” (United Kingdom) | |
| “It’s we as doctors who feel numbers, because we’ve got nothing else to feel.” (Singapore) | |
| Supporting shared decision making | “I give them the pros of doing what I think are this, this, and this, we recognize the downside of this for you is that, try and give them a little bit of a decision in how they want to approach it then. I feel like I’m there to guide them a bit through that choice, but I’m not going to make them do it. They’re living with the disease and the therapies.” (Canada) |
| “Through negotiation, you give in a little. When it comes to people on dialysis who will remain on dialysis for the remainder of their time, I generally give in, because I believe that the only thing you can do is provide some information and let them choose. If a high phosphorous is against current guidelines, but it means that at least the patient enjoys his life, can eat what he wants, then why do I care about the phosphorous? That is also because probably my conviction of how much that influence of survival is much weaker than some of my fellow physicians who have been trained completely differently.” (Belgium) | |
| “It’s usually a compromise; you say to them, I think so many hours of dialysis is just not enough for you, and in the long term, it’s going to have a bad effect on your survival. And then you’ve got to balance that against what they say to you; they say, ‘yes, but I feel so crummy with dialysis, I can’t do that long.’ So instead of going for four and a half hours, they’re going for four, and we end up compromising on four and a quarter.” (Australia) | |
| Optimizing wellbeing | |
| Respecting patient choice | “If someone’s phosphorus is 5.1, I don’t berate them to death, because it should be 4.5, because there’s no evidence that getting them to 4.5 does anything, so I live with it. Why am I going to torture someone an additional 30 minutes on dialysis if it doesn’t really mean anything, it’s just helping me out to meet my targets, so I don’t get into trouble with CMS.” (United States) |
| “I was always taught to treat the patient and not the numbers or not the target.” (Canada) | |
| “As a young doctor, one is tied to surrogate parameters. Now I focus more on what would the patient like. That’s more and more important for me to see the whole picture, not only the disease, but be in charge for the whole patient as a human being. I have to stand back and accept the patient’s will and not be too strict or egoistic of my goals.” (Austria) | |
| Focusing on symptomology | “Symptoms are anything that affects your life. Symptoms mean and might also mean, how often am I admitted to hospital? I’m not thinking of a specific symptom like pain, or tiredness, or fatigue, although those things are important if they’re intrusive, and I don’t think that any one symptom matters any more than others; it’s just generally how functionally people feel, whether they have distracting symptoms that stop them from feeling comfortable, and whether they have an unpredictable, hectic lifestyle, because they’re constantly getting so sick they have to come in to hospital.” (United Kingdom) |
| “Given our limited ability to reduce the mortality of dialysis, it’s more powerful to use symptoms that are meaningful on a daily basis, because some of those have a close relationship to morbidity and mortality but aren’t necessarily the drivers for that.” (United Kingdom) | |
| Perceptible and tangible | “I recognize the things that are important to us, because they are on the dashboard that we can see, and they’re surrogates for how well we’re treating the patients. The patient might say, I feel fine, I don’t care I’ve got a phosphate of two and I’ve had a weight gain of four, and my predialysis BP was 170 on 110, I don’t feel any of that. But I do want to get rid of my itch, and I don’t like this feeling of feeling yuck when I go home after dialysis. So we use all these as kind of surrogates.” (United Kingdom) |
| “Patients don’t feel numbers.” (Singapore) | |
| Judging relevance and consequence | “Mortality would be number 1, and we’d focus on things we can see—parathyroid, potassium, acidosis. Things that matter, even to the patient, but they don’t know that.” (United States) |
| “Patients probably underestimate the consequences of an infection. We know that’s what kills our patients.” (United Kingdom) | |
| “These patient-centered outcomes don’t necessarily represent the outcomes that truly matter to patients, because what I subconsciously consider a patient-important outcome is fracture risk. I’m not necessarily certain that it is the outcome that patients value most, because they will probably think the polyneuropathy and the time spent on dialysis is more important than a theoretical fracture risk, yet I consider that a patient-centered outcome.” (Belgium) | |
| Comprehending extensive heterogeneity | |
| Distilling diverse priorities | “The perceptions of an older patient who has outlived some of their friends and relatives, has seen their family grow up, maybe quality of life for a shorter period is right for them. People earlier in their lives with responsibilities for children and income and family may be prepared to put up with a lower quality of life to see their family grow up or be able to maintain some sort of income. So I’m not sure that there is a one outcome that fits all.” (United Kingdom) |
| “Rather than specific symptoms, there’s no one symptom that I’d say all trials should report this symptom, because we don’t have a symptom-led kind of specialty. There are a lot of different symptoms; it’s very heterogeneous. Perhaps some kind of general symptom freedom or general quality score.” (United Kingdom) | |
| Highly individualized | “Not all the patients are the same, they’re not cookie cutter, it’s tough to just draw guidelines and say that this is what everybody should do. Patient-centered outcomes would make me think of more individualized patient care.” (United States) |
| “Patient-centered outcomes [are] at an individual level that brings a lot of layers of heterogeneity into it. So you can’t apply statistical models to it very easily.” (United Kingdom) | |
| “This is very individual. Some of them have big problems, some of them don’t. They feel the same after dialysis as they felt before, and some of them, for the rest of the day, they are knocked out. I don’t know why it’s like that, there is such an individual difference.” (Germany) | |
| Attempting to specify outcomes | “Things like not phosphorus, not albumin, but more like mortality, hospitalizations, quality of list—honestly, I’m guessing.” (United States) |
| “[Patient-centered outcome] has been, just fledgling. So it’s starting to emerge, but I don’t think it has really hit the dialysis world at all.” (Canada) | |
| “I’m going to edge off into areas that I’m less comfortable with here. I would say, from my group of patients, their desire is to remain well rehabilitated and independent. So if we had a measure of independence, autonomy, a sense of personal control, these are all things that I hear patients saying they’d like to see and they regret losing.” (United Kingdom) | |
| “The problem with quality of life is that we don’t know what it actually means.” (Australia) | |
| Broadening context | “Maybe we don’t deal with them, because we see them as less medical, the areas that we would intervene for a patient, where if you have an isolated symptom, you think maybe I can try something to treat your cramps, or maybe I can try something to treat your restless leg. But ability to travel, how am I going to impact that? There are all of these real world barriers to traveling. Or impact on family, that’s kind of beyond my control, so maybe it’s just a sphere of influence thing that influences that.” (Canada) |
| “You need to look at the whole pathway of care essentially—everything around it, broader things—transport, how often they have to come, where the dialysis unit is, who brings them, what financial impact there is, how long they have to come for, did they have a choice of when, how, where patients dialyze.” (United Kingdom) | |
| “That’s really complex and there’s so many things that influence happiness, with most of which are beyond our control.” (United States) | |
| “And improving the overall health in a dialysis patient, that overall health is defined by defined by whatever the WHO definition of health is.” (Austria) | |
| Clinically hamstrung | |
| Professional deficiency | “If we can’t move the needle on mortality, if you’re middle aged and you’re diabetic, you have 5 years to live on dialysis, your mortality’s roughly 20% a year, how can I make those 5 years as productive as meaningful as possible for that patient? If we can’t get quantity of life, we should focus on quality of life.” (United States) |
| “Every nephrologist you’ll ever talk to will agree that we should work harder to make our patients feel better, but I think we’re hamstrung by the fact that (a) we don’t know how to make our patients feel better, (b) we don’t even know how to measure what is better or not better.” (United States) | |
| “I often feel deficient in addressing them, because we don’t have good evidence around different strategies that I know will be effective for them.” (Canada) | |
| “We’re correcting electrolytes, but if people say we don’t feel any difference, this is bothering me, and I don't know the solution.” (Belgium) | |
| “You are a bit emasculated by the things you can’t do anything about, you just feel a bit impotent. What use am I really? And all you can really do is turn up the dials and so—turn up the hours or fiddle with a few medicines, and none of which tends to make huge amounts of difference. Having said that, that’s therapeutic nihilism, isn’t it?” (Australia) | |
| Uncertainty and complexity in measurement | “It’s a lot harder to measure things like impact on family or ability to travel. There’s been a dearth of research on these outcomes. We need to find better tools to quantify the priorities that our patients think are important to them so that then you can use some science and either develop an intervention.” (United States) |
| “It’s a crime of opportunity. You go into a jurisdiction, there’s a demand for accountability, and then people say, well what can we measure, and usually you lean on the data sets you have available to you, and there are certain things that are easier to measure than others, and those tend to be the things that we go after.” (Canada) | |
| “How would you commission for these outcomes? And that means you have to measure them relatively easily. We’re really talking about things that are responsive as well.” (United Kingdom) | |
| “The problem is the quality of life is really hard to measure in a dialysis setting, because the dialysis process itself impacts so much on quality of life.” (Australia) | |
| Beyond medical purview | “I rarely ask my patients, because I don’t know what I’d do if they said, ‘I’m not sleeping well.’ And impact on the family. It’s not quite clear what control we have over that.” (United Kingdom) |
| “We need to reaffirm those decisions, if not on an early basis, then on a regular basis, in our dialysis patients, what do you value, what’s important to you, are we meeting your needs. We need to say these are the options available to you in our expert view. We don’t do that remotely well enough, and part of that is because it’s an extraordinary time commitment.” (United Kingdom) | |
| “We need to be looking at whether a patient sleeps well at night. We need to be looking at restless legs. We need to be looking at pruritus. We need to be looking at the ability to take your grandson or granddaughter out for a walk or some equivalent. We need to be looking at a happiness index as a result within the hemodialysis population, as a result of a new therapy that has come out. That’s really complex, and there’s so many things that influence happiness, with most of which are beyond our control.” (United States) | |
| Specificity of care | “We’re very segmented in our view of our patients. CMS and KDIGO said look at these things, like Kt/V, anemia, phosphorus, those are the only things we care about.” (United States) |
| “I get the sense from patients that they feel like, we come in, we don’t pay a whole lot of attention to what their priorities are, and we zip on by and check our boxes but aren’t really invested in listening to them, and it’s a challenge, because the way care is structured is such that when I do dialysis rounds, I have to see 100 people in a half day. You can only spend so much time and get through and see everybody.” (Canada) | |
| “I go to my satellite unit once a week and see 30 patients; it’s quite hard to take a holistic view. One focuses very much on very specific things, like their access for dialysis, whether they’re on a line or a fistula, what’s their fluid status, what are the parameters, are they suitable for a transplant; it’s a very regimented set of review parameters.” (United Kingdom) | |
| Mechanistic mindset | “Nephrologists count bodies, count death, complications, admission rates. So we go for these. We have these hard outcomes, BP, phosphate levels, bicarbonate levels. Nephrologists are an obsessive-compulsive bunch, we’re very early potty trained, and we want everything to be clean.” (United Kingdom) |
| “The patient who’s really badly washed out at the end of dialysis is the patient who simply goes home to try and sleep afterward. That impinges on their intradialytic time and is an indicator to me of fatigue. It’s interesting how the technical thing that I as a doctor would link into some of the more subjective things that patients put as lower importance.” (United Kingdom) | |
| Avoiding alarm | “You don’t necessarily want to say to a new patient there’s a 20% chance of you ding in the first 12 months, and there’s a 10%–15% chance of you dying in every 12 months after that. So your mortality rate at 5 years is well over half. Patients don’t entirely realize it to begin with. Once they’ve been on dialysis for a few years and they see the guy in the next bed has disappeared, they realize that dialysis carried a very, very high death rate. We don’t want to upset them and frighten them.” (United Kingdom) |
| “If patients knew what their cardiovascular risk was, they’d be completely shocked, and there’s a question about how much we disclose to patients about what’s likely to happen to them. You could frighten the living daylights out of them if you tell them black and white truths.” (United Kingdom) | |
| “Not a lot of dialysis patients are aware their death risk being as high as some serious sort of cancers. It’s interesting how they can ignore it, because they see people around them dying all the time. I don’t think they really see that clock ticking once they start on the dialysis. We say, ‘they’re going to have a mortality risk of 10%, 15% a year?’ It’s confronting.” (Austria) | |
| Paradoxical dilemma | “I’m all for patient-centered outcomes, but they don’t know that short dialysis, infrequent dialysis, free diets, might well impact on something else.” (United Kingdom) |
| “It’s always really hard for them to [do] an extra half an hour if they are already on 4 hours or if you want to prolong from 3.4 to 4 hours. But on the other hand, I saw tremendous results on everyday long–time dialysis, had amazing results with dialysis every day, 8 hours. The patient was off their hypotensive drugs.” (Austria) | |
| Undermined by system pressures | |
| Adhering to overarching policies | “We’re always pushing for fistulas on our patients, and there’s certainly a subset of patients who would benefit from a graft, and this has been published, in older patients certainly, the lack of maturation of a fistula is something that’s been cited or using grafts or even catheters in those patient populations.” (United States) |
| “There’s a problem with the structure, the way we’re incentivized to treat patients, like McDonald’s; everyone’s treated the same way, where it should be more customized.” (United States) | |
| “The guidelines say you should; we still often don’t, because we feel that patient is not going to have a functional fistula, because he’s old and he will have bad blood vessels.” (Belgium) | |
| Misalignment with mandates | “A lot of patients, in my own opinion, don’t need three times a week dialysis. It’s a very rigid requirement; it’s a one size fits all prescription, but it shouldn’t be that way.” (United States) |
| “The main pressure for physicians is CMS dictating certain outcomes, and the top ten outcomes for patients are not even involved in what CMS are dictating. We’re not trying very hard to improve patient-centered outcomes, because the financial incentives that are essentially driving us to develop improved outcomes dictated by CMS, so everyone has to have a Kt/V over 1.2, everybody has to have fistula, to have phosphorus level 5, a hemoglobin between 9 and 11, nobody really cares what the KDQOL of the patient is.” (United States) | |
| “If we really cared about what patients want, we would persuade the government and other people who fund these things to build in extra capacity, so people can actually not just survive but actually enjoy what they’re doing. That’s where we’ve let patients down, because there’s no trial, nobody cares, because that’s not going to extend their life, but the quality of life, if we were able to measure it for having those holidays and looking forward to them, might be measureable. Well of course it would cost money, and therefore, in fact, if you have neutral quality of life, no extension of survival and additional resource, NHS will throw it out, because that’s the world you live in with NHS.” (United Kingdom) | |
| Resource constraints | “If you’re looking at optimizing the service so that it’s more patient centered, it might sometimes conflict with what the management of a service think needs to happen, but that tends to be a financial thing.” (United Kingdom) |
| “In the United States, there’s an enormous pressure on keeping the hours short to fit everyone in to the things in the way [they are] funded. Even here we’re not funded per hour of dialysis we’re doing, we’re funded per episode dialysis.” (Australia) | |
| “When I was [at my previous hospital], I had vascular surgeons and trained professionals. Whereas where I work now, general surgeons do the fistulas, and the quality is very different.” (United States) |
CMS, Centers for Medicare and Medical Services; WHO, World Health Organization; KDIGO, Kidney Disease Improving Global Outcomes; KDQOL, Kidney Disease Quality of Life; NHS, National Health Service.
Quotations tagged by country only to maintain anonymity.
Explicitly Prioritized by Patients
Articulated Preferences and Goals.
Some participants believed that patient-centered outcomes should be “systematically” identified by patients. Nephrologists “were not the ones on the dialysis machine,” so attempting to make “judgments” without asking patients what outcomes mattered was considered “patriarchal” and “paternalistic.” They suggested that patients needed a “platform for expressing their concerns” routinely.
Ascertaining Treatment Burden.
In recognizing the burden of hemodialysis as “intensive, time-consuming, and life-altering,” some participants interpreted patient-centered outcomes as understanding treatment “intrusiveness.” This meant knowing what caused the most burden and intervening to improve the patients’ “independence and greater tolerability of the life.” The ongoing and onerous “commitment” and “discipline” required of patients were thought to be particularly demanding, because the hemodialysis population was generally older with comorbidities.
Defining Hemodialysis Success.
Patient-centered outcomes were conceptualized as the patients’ treatment goals in terms of “what dialysis does for them and what it doesn’t do for them” and “what they want out of the dialysis.” This was phrased as “something that might change their journey, their experience of being on dialysis” to increase the “value” of hemodialysis.
Distinguishing a Physician-Patient Dichotomy.
Participants reiterated a distinction between patient-centered outcomes and outcomes that nephrologists would traditionally focus on—“we care about anemia, we care about phosphorus, patients don’t give a lick about any of those.” There was a delineation between lifestyle, feelings, and quality of life versus clinical and biochemical parameters. Participants reflected that “it’s we as doctors who feel numbers, because we’ve got nothing else to feel” and that they may “forget” outcomes that mattered to patients, such as ability to travel.
Supporting Shared Decision Making.
Actively involving the patient in decision making, building rapport, and showing empathy were seen as key strategies to reconcile the apparent conflict between patient-centered outcomes and clinical recommendations. Some participants viewed that their role was to explain the benefits and “downsides,” “guide patients through that choice,” and “take into account their circumstances.” This was particularly relevant in terms of adhering to the dialysis prescription, taking phosphate binders, dietary restrictions, and choosing a type of vascular access. They believed that it was necessary to understand and tailor practice to integrate patients’ preferences (such as time off dialysis and dietary freedom) in decision making.
Optimizing Wellbeing
Respecting Patient Choice.
When patients did not meet targets (for example, phosphorus or Kt/V) or adhere to prescribed therapy (including dialysis duration), participants were conscious to avoid “berating” patients and instead, be “a doctor not to be the teacher pointing at the patient.” To “force” patients on therapy to meet mandated targets was deemed inappropriate: “If I’m making the patient uncomfortable trying to reach that goal, it’s pyrrhic, it’s fruitless.” Patient-centered outcomes were about “treating the patient and not the numbers or not the target.” Some allowed more flexibility for older patients but emphasized the importance of minimizing mortality and morbidity in younger patients who were eligible for kidney transplantation. For some, this realization came with experience—“the older I get, the more I realize there’s a balance to be had between these guidelines and the patient’s actual life.”
Focusing on Symptomology.
For some participants, patient-centered outcomes were synonymous with symptoms that frequently occurred or were observed to have a serious effect—“many of the symptoms are what we hear our patients complaining of, fatigue, cramping, feeling drawn out at the end of dialysis, difficulty with memory and concentration, skin itch.” They reiterated that “symptomology was huge” among patients on hemodialysis and could impair quality of life and functioning, and these were what patients wanted them to “fix.” Some observed improvements in symptoms and quality of life were not “really related to biochemistry.”
Perceptible and Tangible Experience.
Some defined patient-centered outcomes as those that patients could feel, experience, and understand—“patients don’t feel numbers” and “don’t see what is inside their body.”
Judging Relevance and Consequence.
Outcomes, such as bone disease, hospitalization, infection, and death, were regarded by some as critically relevant to patients. However, they thought that patients may not be aware or interested in the “theoretical risk” of outcomes that could lead to severe prognostic consequences—“patients probably underestimate the consequences of an infection. We know that’s what kills our patients.”
Comprehending Extensive Heterogeneity
Distilling Diverse Priorities.
Patient-centered outcomes were perceived to reflect a broad and disparate spectrum of potential outcomes, such that it was difficult to “pin down” ones on which to target their efforts. Quality of life, symptoms, and patient goals were all characterized as inherently variable, complex, and multifaceted. Some suggested “globalizing” them or constructing “tiers” as a way of capturing the range of outcomes that mattered to patients.
Highly Individualized.
Patient-centered outcomes were seen as subjective and meaning laden, which should be considered at an individual level to inform tailored patient care. Some participants argued that outcomes could not be standardized or addressed at a “population level” as “a statistically significant difference in a parameter, which [is] like in population studies.”
Attempting to Specify Outcomes.
Some had a vague notion of patient-centered outcomes but broadly related the concept to wellbeing, independence, autonomy, and quality of life—“the problem with quality of life is that we don’t know what it actually means.” They surmised specific outcomes, because they did not “know the literature behind how patients perceived the importance of those things,” the outcomes were rarely reported in research, they varied among individual patients, or they were yet to be elicited from patients. Some believed the concept was only “fledgling” and had not “really hit the hemodialysis world.”
Broadening Context.
For some, addressing patient-centered outcomes would challenge participants to expand their scope of clinical responsibility to improve “overall health” and view “the whole pathway of care” and the “health landscape.” This meant considering aspects peripheral to the hemodialysis treatment, such as transport, ability to travel, burden on family, and financial effect, and addressing “real life, real world barriers” that were “beyond their sphere of influence.”
Clinically Hamstrung
Professional Deficiency.
Being unable to “move the needle on mortality,” “treat symptoms effectively,” and improve dialysis was frustrating. Hemodialysis was “a form of biological stunning, a hinterland existence,” and “correcting electrolytes” did not translate into any meaningful difference for patients. Nephrologists felt “deficient,” “emasculated,” and “impotent” given the lack of new or effective treatments and could only “keep striving to improve in little incremental bits.”
Uncertainty and Complexity in Measurement.
Patient-centered outcomes in terms of quality of life and experience were regarded by some as difficult and impossible to measure, report in a robust and meaningful way, and interpret. The perceived absence of actionable data on patient-centered outcomes meant that they tended to be overlooked in practice. The pursuit of “things that are easier to measure” was a “crime of opportunity” and detracted from the “quality of health away from the machine.” Current measures to assess patient-centered outcomes were regarded as “cumbersome and difficult” or did not capture kidney-specific aspects. Participants urged for feasible and validated tools to quantify patient values to inform interventions and strategies.
Beyond Medical Purview.
For some, patient-centered outcomes were beyond their core clinical capacity, control, and resources to manage. Outcomes related to broader life effect were seen as “less medical” and not “the areas that we would intervene for a patient.” Some were more confident about addressing isolated physical symptoms—“I can try something to treat your cramps, or maybe I can try something to treat your restless leg. But ability to travel, how am I going to impact that? There’s all of these real life, real world barriers to travelling. Or impact on family, that’s kind of beyond my control.” Some were wary that conceding to patient preferences could force them to compromise as a physician (for example, in reducing time on dialysis to below the recommended prescription).
Specificity of Care.
Provision of care for patients on hemodialysis was structured in a regimented and “segmented” way, with a focus on achieving targets set by regulatory agencies and guidelines. They had to “zip on by and check boxes.” Another participant said, “one focuses very much on very specific things, like their access for dialysis, whether they’re on a line or a fistula, what’s their fluid status like, what are the parameters, are they suitable for a transplant; it’s a very regimented set of review parameters.”
Mechanistic Mindset.
Participants postulated that a “mechanistic” mindset was generally entrenched in nephrologists, such that they instinctively concentrated on “low-hanging fruit” that could be “counted” rather than going for the outcomes that mattered—“the home runs.” They characterized nephrologists as “obsessive compulsive” who would be more inclined to “target things around cardiovascular disease, bone health, parathyroid hormone, because they are measurable and because they think they can understand them and because they think they can make an impact in that direction.” Also, participants believed that nephrologists had the tendency to try and determine a physiologic cause for outcomes that mattered to patients (for example, understanding causality of fatigue in terms of cardiac output or hemoglobin) or resolve their issues with medical intervention—“we’re doctors so we prescribe drugs for sleep; they’re nasty drugs, because they’re addictive, they’re benzodiazepines. You start to stereotype your patients rather than actually looking at other aspects for sleep and what might be important.”
Avoiding Alarm.
Although mortality and cardiovascular disease were considered important in patients on hemodialysis, some were reluctant to confront patients with risks—“you don’t necessarily want to say to a new patient there’s a 20% chance of you dying in the first 12 months, and there’s a 10%–15% chance of you dying in every 12 months after that.” They were conscious of potentially “frighten[ing] the living daylights out of them if you tell them black and white truths.” Therefore, they believed some patients were not aware of life-threatening outcomes. Some indirectly framed the risk of outcomes “in terms of things they can do to reduce the risk.”
Paradoxical Dilemma.
Patient priorities that mutually conflicted with or worsened other “problems” posed a dilemma. Participants stated that patients “fought” for “short, infrequent dialysis and free diets” and found it challenging to explain the severe and longer-term repercussions and reconcile this with benefits achieved with longer hours of hemodialysis—“what is an acceptable tradeoff? So the burden versus the benefit.”
Undermined by System Pressures
Adhering to Overarching Policies.
Incentive structures on the basis of restrictive targets, blanket policies, and guidelines were deemed “not applicable to everybody” and deterred efforts from achieving patient-centered outcomes. Some were convinced that policies, such as Fistula First, were driven by cost and were not necessarily formed in the best interest of patients. Also, payment systems, notably in the United States, meant dialysis was “like McDonald’s; everyone’s treated the same way, where it should be more customized.”
Misalignment with Mandates.
Some participants felt that quality indicators did not “represent how good or bad a dialysis experience” was for patients. In the United States, the Centers for Medicare and Medical Services (CMS) was perceived to be “dictating” outcomes that were “easily measured, easily available, and easily monitorable” but were not a “surrogate for quality of life or outcomes that patients would prioritize highly.” The rigid policy requirements for “three times a week dialysis,” for example, were incongruent with patient-centered outcomes and did not account for the individual circumstances of the patient.
Resource Constraints.
Cost and resource constraints were identified as barrier to “optimizing the services so that it’s more patient centered.” Some speculated that facility remuneration models, particularly in the United States, could put “enormous pressure on keeping the hours short to fit everyone in.” One participant specifically mentioned that the quality of vascular access could also depend on the availability of vascular surgeons at their unit.
Discussion
In this era of shared decision making, integrating patient–centered outcomes in clinical care remains a critical challenge. Nephrologists subscribed to the moral responsibility of improving patient-centered outcomes, which they unequivocally regarded as those that were important to the patients’ wellbeing. However, there were differences in how they conceptualized, defined, and applied patient-centered outcomes. They emphasized that the outcomes should be explicitly defined by patients on the basis of their preferences and treatment goals; others believed that patients may not be aware of critical outcomes, such as infection or bone disease, and therefore, they were unable to identify all relevant outcomes that participants would regard as an important patient outcome. For some nephrologists, patient-centered outcomes were thought to encompass specific symptoms in contrast to others, who identified broader life effects, such as ability to travel and burden on family. Some believed that they held some responsibility to address these outcomes, whereas others regarded them as nonmedical and thus, not necessarily within their clinical purview to intervene. Nephrologists placed higher importance on biochemical outcomes if they were convinced of their causal association with clinical or quality of life outcomes, whereas some argued that biochemical end points should not be used as a surrogate for patient-prioritized outcomes given the lack of evidence. The only differences by country that we identified were related to barriers in trying to address patient-centered outcomes in terms of how dialysis was incentivized, which was unique to the United States.
Some nephrologists questioned the feasibility of measuring and managing the diverse and highly individualized range of outcomes important to patients on hemodialysis and capacities to broaden their clinical purview. Delivering patient-centered care in terms of addressing the patients’ broader life effects was constrained by the prevailing focus on traditional biochemical parameters of hemodialysis treatment, the dialysis-related procedures (e.g., vascular access), limited evidence on patient preferences, and lack of novel and effective interventions. Resolving tensions between patient priorities (such as dialysis-free time) and clinical targets as well as communicating theoretical risks of what nephrologists regarded as important to patients (e.g., cardiovascular disease and mortality) versus provoking unwarranted anxiety also posed as challenges.
Similar barriers in implementing patient-centered outcomes in nephrology and other medical specialties have been previously identified, including rigid regulatory structures, disease–centric incentivization schemes on the basis of laboratory parameters (e.g., Kt/V and hemoglobin), resource constraints, emphasis on biochemical targets and technical procedures, and lack of mechanisms for patients to communicate their priorities (10,43–46). A study in mental health professionals also found that clinicians were concerned about being held accountable for managing the array of needs and goals that a patient may have (47). Our findings add to existing literature by highlighting some of the unique challenges in the context of hemodialysis. Nephrologists in our study believed that the plethora of symptoms, comorbidities, and treatment complications in patients on hemodialysis obscured judgment about what outcomes to prioritize, measure, and address. They had to address tensions, such as the burden of dialysis on patients versus patient preferences for dialysis-free time and achieving phosphate targets versus dietary restrictions. Also, some nephrologists were apprehensive about directly informing patients of the risks of life-threatening outcomes, and a survey suggests a knowledge deficit in patients with CKD about their risk of comorbidities (48).
Of note, studies have consistently shown that patients on hemodialysis consistently prioritize fatigue, ability to travel, dialysis-free time, effect on family, ability to work, sleep, and anxiety/depression highly (10,49–56). A recent study noted that these broader lifestyle or life participation outcomes were ranked of higher importance than comorbid conditions, complications (including death) or specific symptoms (e.g., pruritus, restless legs syndrome, cramps, or nausea), and biochemical parameters (49). Such findings may challenge current assumptions that patient-centered outcomes are only symptom focused, which are perhaps perpetuated by time–limited clinical consultations with patients who may only report specific symptoms that they deem warranted to mention to their nephrologist in a medical setting.
Recently, the Standardized Outcomes in Nephrology Initiative was established to identify consensus–based core outcomes for trials on the basis of the shared priorities of patients, caregivers, and health professionals (57). Mortality, cardiovascular disease, vascular access complications, and fatigue were prioritized to be of critical importance across all stakeholder groups, including patients (57–59). Distilling patient-prioritized outcomes is possible and may inform targeted efforts toward outcomes that are consistently of high importance to patients, which encompasses both quality of life and clinical outcomes.
The push for patient-centered care is also apparent in the policy arena. The US CMS has identified patient experience and engagement as priorities and highlighted the need for patient–centered quality metrics in the ESRD quality incentive program (45,60). Also, the US Food and Drug Administration (FDA) Patient Report Outcomes Consortium was convened to develop and evaluate patient–reported outcome measures (PROMS) for use in clinical trials to support labeling claims of medical products (40,61), and both the US FDA and the European Medicines Agency have released several guidance documents on PROMS. In nephrology, the European Renal Association–European Dialysis and Transplantation Association recently held a consensus meeting and agreed on the routine use of PROMS using generic and disease–specific quality of life and utility instruments (e.g., Short Form–12, Kidney Disease Quality of Life–36, and EuroQoL-5D-5L) (62). Some nephrologists emphasized that relevant and patient–centered outcome measures were needed to inform care. Indeed, PROMS should be on the basis of outcomes that are of explicit relevance and importance to patients. Given the paucity of validated instruments for use in patients on dialysis (41), efforts must ensue to develop rigorous, robust, and sensitive to change outcome measures as well as mechanisms to facilitate routine and meaningful assessment of patient-centered outcomes.
Our study elucidates diverse and detailed perspectives from nephrologists about the meaning and application of patient-centered outcomes in hemodialysis. We achieved saturation and conducted member checking by obtaining feedback from participants on the preliminary results. However, there are potential limitations. The participants were English-speaking nephrologists practicing in high-income countries, which may limit the transferability of the findings. To elicit tradeoffs between what might be perceived as patient-important outcomes versus standard clinical outcomes, we asked direct questions about potential mismatches and tensions between outcomes as prompts in the interview guide. Thus, we acknowledge that responses may reflect either the participants’ long-standing beliefs or perspectives that were developed during the interview. This study only included nephrologists, and future studies could elicit patients’ perspectives on patient-centered outcomes.
Nephrologists uphold patient-centered care as a moral responsibility to improve wellbeing and treatment burden in patients on hemodialysis. However, efforts are hampered by uncertainties in how to prioritize, measure, and manage the plethora of critical comorbidities and broader quality of life outcomes in a clinical setting that is already technically demanding with a prevailing focus on biochemical parameters. There seems to be a need to identify core patient–important outcomes and develop robust mechanisms for integrating them into practice and policy, which may help to advance patient-centered care in hemodialysis.
Disclosures
None.
Supplementary Material
Acknowledgments
We thank all participants for sharing their interesting and thoughtful perspectives in this study. With permission, we acknowledge them by name: Aine Burns, Annemie Dhondt, Balaji Hiremagular, Biruh Workeneh, Bruno Watschinger, Chris Pugh, Chris Wenearls, Cormac Breen, Damien Ashby, Daniel Cejka, David Goldsmith, David Harris, Donal O’Donaghue, Edwina Brown, Evi Nagler, Francis Verbeke, George Mangos, Gregor Bond, Hamish Dobbie, Helen Alston, Jennifer MacRae, Jill Vanmassenhove, John Agar, Jose Perez, Katrien Blanckaert, Kevan Polkinghorne, Klemens Budde, Lina Choon Hui Lin, Manfred Hecking, Mark Brown, Matthew James, Matthew Jose, Matthew Roberts, Medha Airy, Neil Ashman, Nigel Toussaint, Norbert Lameire, Oliver Staeck, Paramit Chowdhury, Pascale Bernaert, Paul Lawton, Peter Kerr, Pietro Ravani, Prabir Roy-Chaudhury, Rainer Oberbauer, Rajeev Raghavan, Raymond Vanholder, Rob Quinn, Rosemary Masterson, Sai Kaumudi Saridey, Sajeda Youssouf, Sandip Mitra, Sreedhar Mandayam, Steve Holt, Suetonia Palmer, Sufi Suhail, Susanne Kron, and Torsten Slowinski. At the time of the study, three participants were involved as investigators in Standardized Outcomes in Nephrology Initiative–related projects.
This work was supported by National Health and Medical Research Council (NHMRC) project grant APP1098815. A.T. is supported by NHMRC Career Development Fellowship APP1106716.
The funding organizations had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; or preparation, review, or approval of the manuscript.
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
See related editorial, “When All You Have Is a Hammer: The Need for Tools to Define and Apply Patient-Centered Outcomes in Hemodialysis,” on pages 382–384.
This article contains supplemental material online at http://cjasn.asnjournals.org/lookup/suppl/doi:10.2215/CJN.08370816/-/DCSupplemental.
References
- 1.National Research Council : Crossing the Quality Chasm: A New Health System for the 21st Century, Washington, DC, Institute of Medicine, 2001 [Google Scholar]
- 2.Gandhi GY, Murad MH, Fujiyoshi A, Mullan RJ, Flynn DN, Elamin MB, Swiglo BA, Isley WL, Guyatt GH, Montori VM: Patient-important outcomes in registered diabetes trials. JAMA 299: 2543–2549, 2008 [DOI] [PubMed] [Google Scholar]
- 3.Yudkin JS, Lipska KJ, Montori VM: The idolatry of the surrogate. BMJ 343: d7995, 2011 [DOI] [PubMed] [Google Scholar]
- 4.Barry MJ, Edgman-Levitan S: Shared decision making--pinnacle of patient-centered care. N Engl J Med 366: 780–781, 2012 [DOI] [PubMed] [Google Scholar]
- 5.Bardes CL: Defining “patient-centered medicine.” N Engl J Med 366: 782–783, 2012 [DOI] [PubMed] [Google Scholar]
- 6.Laine C, Davidoff F: Patient-centered medicine. A professional evolution. JAMA 275: 152–156, 1996 [PubMed] [Google Scholar]
- 7.Howard-Anderson J, Lonowski S, Vangala S, Tseng CH, Busuttil A, Afsar-Manesh N: Readmissions in the era of patient engagement. JAMA Intern Med 174: 1870–1872, 2014 [DOI] [PubMed] [Google Scholar]
- 8.Nelson EC, Dixon-Woods M, Batalden PB, Homa K, Van Citters AD, Morgan TS, Eftimovska E, Fisher ES, Ovretveit J, Harrison W, Lind C, Lindblad S: Patient focused registries can improve health, care, and science. BMJ 354: i3319, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Oshima Lee E, Emanuel EJ: Shared decision making to improve care and reduce costs. N Engl J Med 368: 6–8, 2013 [DOI] [PubMed] [Google Scholar]
- 10.O’Hare AM, Armistead N, Schrag WL, Diamond L, Moss AH: Patient-centered care: An opportunity to accomplish the “Three Aims” of the National Quality Strategy in the Medicare ESRD program. Clin J Am Soc Nephrol 9: 2189–2194, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tinetti ME, Fried T: The end of the disease era. Am J Med 116: 179–185, 2004 [DOI] [PubMed] [Google Scholar]
- 12.Frank L, Basch E, Selby JV; Patient-Centered Outcomes Research Institute : The PCORI perspective on patient-centered outcomes research. JAMA 312: 1513–1514, 2014 [DOI] [PubMed] [Google Scholar]
- 13.Epstein RM, Street RL Jr.: The values and value of patient-centered care. Ann Fam Med 9: 100–103, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Herzlinger RE, Schleicher SM, Mullangi S: Health care delivery innovations that integrate care? Yes! But integrating what? JAMA 315: 1109–1110, 2016 [DOI] [PubMed] [Google Scholar]
- 15.Selby JV, Beal AC, Frank L: The Patient-Centered Outcomes Research Institute (PCORI) national priorities for research and initial research agenda. JAMA 307: 1583–1584, 2012 [DOI] [PubMed] [Google Scholar]
- 16.Cukor D, Cohen LM, Cope EL, Ghahramani N, Hedayati SS, Hynes DM, Shah VO, Tentori F, Unruh M, Bobelu J, Cohen S, Dember LM, Faber T, Fischer MJ, Gallardo R, Germain MJ, Ghahate D, Grote N, Hartwell L, Heagerty P, Kimmel PL, Kutner N, Lawson S, Marr L, Nelson RG, Porter AC, Sandy P, Struminger BB, Subramanian L, Weisbord S, Young B, Mehrotra R: Patient and other stakeholder engagement in patient-centered outcomes research institute funded studies of patients with kidney diseases. Clin J Am Soc Nephrol 11: 1703–1712, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Audet AM, Davis K, Schoenbaum SC: Adoption of patient-centered care practices by physicians: Results from a national survey. Arch Intern Med 166: 754–759, 2006 [DOI] [PubMed] [Google Scholar]
- 18.Davis K, Schoenbaum SC, Audet AM: A 2020 vision of patient-centered primary care. J Gen Intern Med 20: 953–957, 2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bergeson SC, Dean JD: A systems approach to patient-centered care. JAMA 296: 2848–2851, 2006 [DOI] [PubMed] [Google Scholar]
- 20.Di Lullo L, Rivera R, Barbera V, Bellasi A, Cozzolino M, Russo D, De Pascalis A, Banerjee D, Floccari F, Ronco C: Sudden cardiac death and chronic kidney disease: From pathophysiology to treatment strategies. Int J Cardiol 217: 16–27, 2016 [DOI] [PubMed] [Google Scholar]
- 21.Heidenreich PA: Time for a thorough evaluation of patient-centered care. Circ Cardiovasc Qual Outcomes 6: 2–4, 2013 [DOI] [PubMed] [Google Scholar]
- 22.Olsen LA, Saunders RS, McGinnis JM: Patients Charting the Course. Citizen Engagement and the Learning Health System. Workshop Summary, Washington, DC, Institute of Medicine, 2011 [PubMed] [Google Scholar]
- 23.Munjal K, Carr B: Realigning reimbursement policy and financial incentives to support patient-centered out-of-hospital care. JAMA 309: 667–668, 2013 [DOI] [PubMed] [Google Scholar]
- 24.Bray-Hall ST: Transitional care: Focusing on patient-centered outcomes and simplicity. Ann Intern Med 157: 448–449, 2012 [DOI] [PubMed] [Google Scholar]
- 25.Spatz ES, Spertus JA: Shared decision making: A path toward improved patient-centered outcomes. Circ Cardiovasc Qual Outcomes 5: e75–e77, 2012 [DOI] [PubMed] [Google Scholar]
- 26.Mullins CD, Vandigo J, Zheng Z, Wicks P: Patient-centeredness in the design of clinical trials. Value Health 17: 471–475, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Thomas B, Wulf S, Bikbov B, Perico N, Cortinovis M, Courville de Vaccaro K, Flaxman A, Peterson H, Delossantos A, Haring D, Mehrotra R, Himmelfarb J, Remuzzi G, Murray C, Naghavi M: Maintenance dialysis throughout the world in years 1990 and 2010. J Am Soc Nephrol 26: 2621–2633, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Robinson BM, Zhang J, Morgenstern H, Bradbury BD, Ng LJ, McCullough KP, Gillespie BW, Hakim R, Rayner H, Fort J, Akizawa T, Tentori F, Pisoni RL: Worldwide, mortality risk is high soon after initiation of hemodialysis. Kidney Int 85: 158–165, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Karopadi AN, Mason G, Rettore E, Ronco C: The role of economies of scale in the cost of dialysis across the world: A macroeconomic perspective. Nephrol Dial Transplant 29: 885–892, 2014 [DOI] [PubMed] [Google Scholar]
- 30.Wyld M, Morton RL, Hayen A, Howard K, Webster AC: A systematic review and meta-analysis of utility-based quality of life in chronic kidney disease treatments. PLoS Med 9: e1001307, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Collins AJ, Foley R, Herzog C, Chavers B, Gilbertson D, Ishani A, Kasiske B, Liu J, Mau LW, McBean M, Murray A, St Peter W, Xue J, Fan Q, Guo H, Li Q, Li S, Li S, Peng Y, Qiu Y, Roberts T, Skeans M, Snyder J, Solid C, Wang C, Weinhandl E, Zaun D, Zhang R, Arko C, Chen SC, Dalleska F, Daniels F, Dunning S, Ebben J, Frazier E, Hanzlik C, Johnson R, Sheets D, Wang X, Forrest B, Constantini E, Everson S, Eggers P, Agodoa L: Excerpts from the United States Renal Data System 2007 annual data report. Am J Kidney Dis 51[Suppl 1]: S1–S320, 2008 [DOI] [PubMed] [Google Scholar]
- 32.Krishnan M, Weinhandl ED, Jackson S, Gilbertson DT, Lacson E Jr.: Comorbidity ascertainment from the ESRD medical evidence report and medicare claims around dialysis initiation: A comparison using US Renal Data System data. Am J Kidney Dis 66: 802–812, 2015 [DOI] [PubMed] [Google Scholar]
- 33.Goodkin DA, Bragg-Gresham JL, Koenig KG, Wolfe RA, Akiba T, Andreucci VE, Saito A, Rayner HC, Kurokawa K, Port FK, Held PJ, Young EW: Association of comorbid conditions and mortality in hemodialysis patients in Europe, Japan, and the United States: The Dialysis Outcomes and Practice Patterns Study (DOPPS). J Am Soc Nephrol 14: 3270–3277, 2003 [DOI] [PubMed] [Google Scholar]
- 34.Tentori F, Blayney MJ, Albert JM, Gillespie BW, Kerr PG, Bommer J, Young EW, Akizawa T, Akiba T, Pisoni RL, Robinson BM, Port FK: Mortality risk for dialysis patients with different levels of serum calcium, phosphorus, and PTH: The Dialysis Outcomes and Practice Patterns Study (DOPPS). Am J Kidney Dis 52: 519–530, 2008 [DOI] [PubMed] [Google Scholar]
- 35.Almasri J, Alsawas M, Mainou M, Mustafa RA, Wang Z, Woo K, Cull DL, Murad MH: Outcomes of vascular access for hemodialysis: A systematic review and meta-analysis. J Vasc Surg 64: 236–243, 2016 [DOI] [PubMed] [Google Scholar]
- 36.Cavanaugh KL: Prioritizing patient-centered care implementation and research for patients with kidney disease. Semin Dial 28: 131–140, 2015 [DOI] [PubMed] [Google Scholar]
- 37.Tong A, Sainsbury P, Craig J: Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int J Qual Health Care 19: 349–357, 2007 [DOI] [PubMed] [Google Scholar]
- 38.Booth CM: Evaluating patient-centered outcomes in the randomized controlled trial and beyond: Informing the future with lessons from the past. Clin Cancer Res 16: 5963–5971, 2010 [DOI] [PubMed] [Google Scholar]
- 39.Duggan PS, Geller G, Cooper LA, Beach MC: The moral nature of patient-centeredness: Is it “just the right thing to do”? Patient Educ Couns 62: 271–276, 2006 [DOI] [PubMed] [Google Scholar]
- 40.US Department of Health and Humans Services, US Food and Drug Administration: The Patient-Reported Outcomes (PRO) Consortium, 2010. Available at: http://www.fda.gov/aboutfda/partnershipscollaborations/publicprivatepartnershipprogram/ucm231129.htm. Accessed July 14, 2016
- 41.Flythe JE, Powell JD, Poulton CJ, Westreich KD, Handler L, Reeve BB, Carey TS: Patient-reported outcome instruments for physical symptoms among patients recieving maintenance dialysis: A systematic review. Am J Kidney Dis 66: 1033–1046, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Corbin F, Strauss A: Basic of Qualitative Research: Techniques and Procedures for Developing Grounded Theory, Los Angeles, CA, Sage, 2008 [Google Scholar]
- 43.Wong SP, Vig EK, Taylor JS, Burrows NR, Liu CF, Williams DE, Hebert PL, O’Hare AM: Timing of initiation of maintenance dialysis: A qualitative analysis of the electronic medical records of a national cohort of patients from the department of veterans affairs. JAMA Intern Med 176: 228–235, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Naik N, Hess R, Unruh M: Measurement of health-related quality of life in the care of patients with ESRD: Isn’t this the metric that matters? Semin Dial 25: 439–444, 2012 [DOI] [PubMed] [Google Scholar]
- 45.Moss AH, Davison SN: How the ESRD quality incentive program could potentially improve quality of life for patients on dialysis. Clin J Am Soc Nephrol 10: 888–893, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kimmel PL: The weather and quality of life in ESRD patients: Everybody talks about it, but does anybody do anything about it? Semin Dial 26: 260–262, 2013 [DOI] [PubMed] [Google Scholar]
- 47.Dobscha SK, Cromer R, Crain A, Denneson LM: Qualitative analysis of US Department of Veterans Affairs mental health clinician perspectives on patient-centered care. Int J Qual Health Care 28: 355–362, 2016 [DOI] [PubMed] [Google Scholar]
- 48.Lopez-Vargas PA, Tong A, Phoon RK, Chadban SJ, Shen Y, Craig JC: Knowledge deficit of patients with stage 1-4 CKD: A focus group study. Nephrology (Carlton) 19: 234–243, 2014 [DOI] [PubMed] [Google Scholar]
- 49.Urquhart-Secord R, Craig JC, Hemmelgarn B, Tam-Tham H, Manns B, Howell M, Polkinghorne KR, Kerr PG, Harris DC, Thompson S, Schick-Makaroff K, Wheeler DC, van Biesen W, Winkelmayer WC, Johnson DW, Howard K, Evangelidis N, Tong A: Patient and caregiver priorities for outcomes in hemodialysis: An international nominal group technique study. Am J Kidney Dis 68: 444–454, 2016 [DOI] [PubMed] [Google Scholar]
- 50.Morton RL, Tong A, Howard K, Snelling P, Webster AC: The views of patients and carers in treatment decision making for chronic kidney disease: Systematic review and thematic synthesis of qualitative studies. BMJ 340: c112, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Morton RL, Tong A, Webster AC, Snelling P, Howard K: Characteristics of dialysis important to patients and family caregivers: A mixed methods approach. Nephrol Dial Transplant 26: 4038–4046, 2011 [DOI] [PubMed] [Google Scholar]
- 52.Walker RC, Howard K, Morton RL, Palmer SC, Marshall MR, Tong A: Patient and caregiver values, beliefs and experiences when considering home dialysis as a treatment option: A semi-structured interview study. Nephrol Dial Transplant 31: 133–141, 2016 [DOI] [PubMed] [Google Scholar]
- 53.Walker RC, Howard K, Tong A, Palmer SC, Marshall MR, Morton RL: The economic considerations of patients and caregivers in choice of dialysis modality. Hemodial Int 20: 634–642, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Flythe JE, Mangione TW, Brunelli SM, Curhan GC: Patient-stated preferences regarding volume-related risk mitigation strategies for hemodialysis. Clin J Am Soc Nephrol 9: 1418–1425, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Tong A, Crowe S, Chando S, Cass A, Chadban SJ, Chapman JR, Gallagher M, Hawley CM, Hill S, Howard K, Johnson DW, Kerr PG, McKenzie A, Parker D, Perkovic V, Polkinghorne KR, Pollock C, Strippoli GF, Tugwell P, Walker RG, Webster AC, Wong G, Craig JC: Research priorities in CKD: Report of a national workshop conducted in Australia. Am J Kidney Dis 66: 212–222, 2015 [DOI] [PubMed] [Google Scholar]
- 56.Manns B, Hemmelgarn B, Lillie E, Dip SC, Cyr A, Gladish M, Large C, Silverman H, Toth B, Wolfs W, Laupacis A: Setting research priorities for patients on or nearing dialysis. Clin J Am Soc Nephrol 9: 1813–1821, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Tong A, Manns B, Hemmelgarn B, Wheeler DC, Tugwell P, Winkelmayer WC, van Biesen W, Crowe S, Kerr PG, Polkinghorne KR, Howard K, Pollock C, Hawley CM, Johnson DW, McDonald SP, Gallagher MP, Urquhart-Secord R, Craig JC; SONG-HD Collaboration : Standardised outcomes in nephrology - Haemodialysis (SONG-HD): Study protocol for establishing a core outcome set in haemodialysis. Trials 16: 364, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Standardised Outcomes in Nephrology—Haemodialysis (SONG-HD). Available at: http://songinitiative.org/about-us/song-hd/. Accessed July 14, 2016
- 59.Tong A, Manns B, Hemmelgarn B, Wheeler DC, Evangelidis N, Tugwell P, Crowe S, Van Biesen W, Winkelmayer WC, O’Donoghue D, Tam-Tham H, Shen JI, Pinter J, Larkins N, Youssouf S, Mandayam S, Ju A, Craig JC; SONG-HD Investigators : Establishing core outcomes domains in hemodialysis: Report of the Standardized outcomes in nephrology-hemodialysis (SONG-HD) consensus workshop [published online ahead of print August 3, 2016]. Am J Kidney Dis 10.1053/j.ajkd.2016.05.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Conway PH, Mostashari F, Clancy C: The future of quality measurement for improvement and accountability. JAMA 309: 2215–2216, 2013 [DOI] [PubMed] [Google Scholar]
- 61.FDA : Guidance for Industry. Patient-Reported Outcome Measures: Use in Medical Product Development to Support Labeling Claims, Silver Spring, MD, US Department of Health and Human Services Food and Drug Administration, 2009 [Google Scholar]
- 62.Breckenridge K, Bekker HL, Gibbons E, van der Veer SN, Abbott D, Briançon S, Cullen R, Garneata L, Jager KJ, Lønning K, Metcalfe W, Morton RL, Murtagh FE, Prutz K, Robertson S, Rychlik I, Schon S, Sharp L, Speyer E, Tentori F, Caskey FJ: How to routinely collect data on patient-reported outcome and experience measures in renal registries in Europe: An expert consensus meeting. Nephrol Dial Transplant 30: 1605–1614, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.