Abstract
This article describes the primary health care offered to 8118 service users with diabetes in Brazil based on data from the PMAQ (Program to Improve Primary Care Access and Quality) first survey. Structure, access, service organization and management, and clinical care quality were analyzed. Prevalence of self-reported receipt of appropriate treatment was 14.3% (95% confidence interval [CI]: 13.4-15.2). Following adjustment, it was 26% higher (prevalence ratio [PR] = 1.26; 95% CI: 1.04-1.54) when primary health care centers had all the structure items investigated, it was 13% higher (PR = 1.13; 95% CI: 1.00-1.29) when the teams' work process for service organization and management was adequate and it was 14% higher (PR = 1.14; 95% CI: 1.00-1.30) when the teams' clinical practice was adequate.
Keywords: diabetes mellitus, health services evaluation, medical care, primary health care, quality of health care
DIABETES MELLITUS (DM) affects 6% of the adult population (Iser et al., 2015) and around 20% of elderly people in Brazil (Costa et al., 2011). Randomized clinical trials have found that people with diabetes having clinical and metabolic control have shown delay in the appearance and/or progression of complications (UK Prospective Diabetes Study Group, 1998a, 1998b). The treatment approach for detected cases, blood glucose monitoring and control, and education process initiation are fundamental for preventing complications and maintaining patients' quality of life (Ministério da Saúde, Brasil, 2013).
The Brazilian Unified Health System (Sistema Único de Saúde [SUS]) is a decentralized public health system. In 1994, the Ministry of Health (MOH) launched the Family Health Strategy (FHS) for improving primary health care delivery and SUS performance regarding universal and comprehensive care. The FHS delivers health actions addressing health promotion, preventive examinations, and health care to poorer and vulnerable population groups (Facchini et al., 2015). Regarding diabetic care, the work processes assume that trained health professionals work in an interdisciplinary manner, link with service users, and take on responsibility for ensuring the provision of comprehensive health care, including (a) screening, classification, and diagnosis of diabetes; (b) initial assessment and guidance on healthy lifestyles provided in appointments with nurses; (c) initial assessment and follow-up medical appointments—history, physical examination, and assessment through complementary examinations; (d) blood glucose control and treatment with or without medication; (e) prevention and management of acute and chronic complications; (f) care of feet; (g) recommendations on nutrition and physical activity; and (h) oral health care (Ministério da Saúde, Brasil, 2013).
According to the National Health Survey (2014), 73% of people with diabetes attended an appointment in the last 12 months and 47% of them had their appointments at primary health care centers (PHCs) (Instituto Brasileiro de Geografia e Estatística, 2014). Adequate management of people with diabetes at PHCs can reduce expenditure on specialized and urgent care services (Alfradique et al., 2009; Organização Pan-Americana da Saúde, 2010).
Evaluating the quality of PHCs is important for choosing priorities, health action targets, and service organization (Habicht et al., 1999). In 2011, the MOH created the Program to Improve Primary Care Access and Quality (PMAQ), aiming at scaling up access and qualifying care offered by means of financial incentives directed toward municipal health management, conditioned on formal agreements on commitments and indicator evaluation made between PHC teams, municipal health service managers, and the MOH (Ministério da Saúde, Brasil, 2015a). A total of 3935 of the total of Brazilian municipalities (71%) took part in the first cycle of PMAQ in 2012 when the total number of FHS teams in Brazil was 32 337. Of these, 17 202 (53.2%) adhered to the program. One of its components is external evaluation of service performance from the point of view of health care professionals and service users.
Scientific production regarding PMAQ is still incipient and little analysis has been performed in the country as a whole. Standing out thus far is access (Alves et al., 2014), team work process characteristics (Cruz et al., 2014; Mendes et al., 2014; Seidl et al., 2014), health promotion (Medina et al., 2014; Teixeira et al., 2014), oral health (Casotti et al., 2014), and cervical cancer prevention (Tomasi et al., 2015).
Specifically in relation to evaluating diabetes care using primary data, available literature is scarce and limited to studies within a given health service facility or municipality (Araújo et al., 1999; Assunção et al., 2001; Gonçalves et al., 2013; Paiva et al., 2006). In turn, the use of secondary data coming from the PHC Information System (SIAB) and from the HIPERDIA system—which is intended for the registration and follow-up of patients with arterial hypertension and/or DM receiving SUS outpatient care—has been restricted owing to the low coverage of these systems and the quality of available data (Cavalcante et al., 2015; Jardim & Leal, 2009).
From PMAQ data, this article describes the adequacy of primary health care structure and work process, as well as aspects of care as perceived by users with DM, according to the characteristics of the municipalities. In addition, it investigates the association between receipt of care and adequacy of structure and team work processes.
METHODS
The survey was conducted by 41 federal research institutions and was headed by 6 of them.1 Data collection took place in 2012 by around 1000 trained interviewers and supervisors.
Primary health care center teams indicated by municipal management for external evaluation were interviewed, as was a sample of service users attending PHCs on the day of the evaluation in the whole country. For each team, 4 service users were selected from among those waiting to be seen, according to the following criteria: not being their first attendance at the service and not having had an interval of more than 12 months without attending. Data were collected using tablets with electronic forms and were sent automatically to a central server.
Three instruments were administered. The first instrument assessed structure issues (Donabedian, 1988) considered to be essential for care for people with diabetes: sphygmomanometer, adult stethoscope, monofilament kit, ophthalmoscope, weighing scales, tape measure, glucometer, capillary blood glucose strips, and the B-DIA form (SIAB). The presence of all 9 items at the PHC was considered to be adequate structure.
The second instrument investigated aspects of the work process relating to access and quality of care provided by the teams. Access was assessed by booking of appointments for service users at any time and on any week day that the health centers were open. Quality was assessed by service organization and management and clinical care. The questions used for the first aspect were as follows: “does the primary health care team have a record of people with diabetes mellitus with greater risk/severity?”; “does the team schedule the appointments and examinations of people with diabetes mellitus based on case stratification?”; and “does the team coordinate the waiting list of service users with diabetes who need appointments and examinations at other points of care?” The questions for clinical care were as follows: “does the team perform diabetic foot examinations periodically?”; “does the team perform fundoscopic examinations periodically?”; and “does the team request glycated haemoglobin tests regularly?” The teams that answered yes to all the questions of both aspects were classified with adequate service organization and management and adequate clinical care, respectively.
The third instrument was used to investigate intermediary results (Donabedian, 1988; Facchini et al., 2015), considering user access to appointments at a given health center in the last 6 months. Quality of service organization and management, as perceived by service users, was determined by a positive reply to the question asking whether their next appointment had been booked at the end of their current appointment. Quality of clinical care was based on service users reporting having had a blood glucose test, having had their feet examined by a member of the health team, and having received guidance from a member of the team about taking care of their feet, in the last 6 months. Finally, satisfaction with the service was estimated indirectly by a negative reply to the question: “if you could, would you change your health team or health center?”
A synthetic outcome was built—self-reported receipt of appropriate care—based on service user affirmative replies to 4 questions: reporting having received a blood test, having received guidance on foot care, having had their feet examined, and having been able to book an appointment.
The 8 care indicators and the synthetic outcome were described according to users' characteristics: sex (male; female), age in quartiles (18-52; 53-60; 61-67; 68-92 years), skin color (white, black, brown, yellow, or indigenous), living with a partner (yes; no), literate (yes; no), family income per capita—quartiles in US dollars (0-47.7; 47.8-95.4; 95.5-184.0; 184.1-2300), as well as according to the characteristics of the municipalities: geopolitical region (North, Northeast, Midwest, Southeast, and South); municipality size by the number of inhabitants (Instituto Brasileiro de Geografia e Estatística, 2010) (up to 10,000; 10,001-30,000; 30,001-100,000; 100,001-300,000; more than 300,000), the Municipal Human Development Index (HDI-M) (Programa das Nações Unidas para o Desenvolvimento, 2016), classified in quartiles (0.480-0.696; 0.697-0.779; 0.780-0.832; 0.833-0.920), and municipal coverage of the FHS (Ministério da Saúde, Brasil, 2015b) classified in terciles (up to 47.6%; 47.7%-82.0%; 82.1%-100%).
Analysis was performed using Stata 12.0 statistical software (StataCorp LP, College Station, Texas). The chi-square test was used to evaluate associations between the independent variables and 8 indicators, as well as the synthetic outcome. Using multivariate Poisson regression analysis, the crude prevalence ratios (PRs) of self-reported receipt of appropriate care were adjusted—in model 1—for municipality size, HDI-M, FHS population coverage, and sex of the users; model 2 adjusted for these variables and also for region. This adjusted analysis took into consideration those variables that were associated with the outcome in the univariate analysis, also taking a P value < .05.
The study was approved by the Federal University of Pelotas, Faculty of Medicine Research Ethics Committee under number 21494013.0.0000.5317. All study participants signed the informed consent form.
RESULTS
Out of a total of 38 812 PHCs evaluated in a service census, 17 202 health teams from 13 843 PHCs adhered to the PMAQ. A total of 65 391 users were interviewed, and 8118 of them reported having medical diagnosis of diabetes; 6309 (87.2%) of these had an appointment at 4546 of the PHCs in the last 6 months.
The majority of the service users were women, half were older than 60 years, and some 56% self-reported their skin color as being brown or black. Two-thirds of the sample reported being married or living with a partner and just over a quarter were illiterate. Slightly more than half the service users lived in families with per capita income of less than US$95 (Table 1). More than half the service users were concentrated in the Southeast region (53.5%) and around a third of them lived in municipalities with more than 300 000 inhabitants (31.5%). In addition, 50.6% lived in municipalities with HDI-M up to 0.779 and 33% lived in municipalities with FHS coverage of up to 47.6% (Table 1).
Table 1. Distribution of Users With Diabetes According to Sociodemographic Characteristics and Municipality Context (Ministério da Saúde, Brasil, 2015a).
| Variable | n | % |
|---|---|---|
| Age in years (quartiles) (n = 6264) | ||
| 18-52 | 1700 | 27.1 |
| 53-60 | 1514 | 24.2 |
| 61-67 | 1496 | 23.9 |
| 68-92 | 1554 | 24.8 |
| Sex (n = 6309) | ||
| Male | 1985 | 31.5 |
| Female | 4324 | 68.5 |
| Skin color/race (n = 6242) | ||
| White | 2540 | 40.7 |
| Black | 851 | 13.6 |
| Brown | 2659 | 42.6 |
| Yellow/indigenous | 192 | 3.1 |
| Lives with a partner (n = 6306) | ||
| Yes | 4211 | 66.8 |
| No | 2095 | 33.2 |
| Literate (6305) | ||
| Yes | 4622 | 73.3 |
| No | 1683 | 26.7 |
| Family income per capita (US$a) (quartiles) (n = 5693) | ||
| 0-47.7 | 1424 | 25.0 |
| 47.8-95.4 | 1568 | 27.5 |
| 95.5-184.0 | 1464 | 25.8 |
| 184.1-2300 | 1238 | 21.7 |
| Region (n = 6186) | ||
| North | 234 | 3.8 |
| Northeast | 1282 | 20.7 |
| Southeast | 3307 | 53.5 |
| South | 872 | 14.1 |
| Midwest | 491 | 7.9 |
| Population size (inhabitants) (n = 6186) | ||
| Very small: up to 10,000 | 832 | 13.4 |
| Small: 10,001-30,000 | 1465 | 23.7 |
| Medium: 30,001-100,000 | 1204 | 19.5 |
| Large: 100,001-300,000 | 734 | 11.9 |
| Very large: over 300,000 | 1951 | 31.5 |
| HDI-M and quartiles (n = 6120) | ||
| 0.480-0.696 | 1556 | 25.4 |
| 0.697-0.779 | 1542 | 25.2 |
| 0.780-0.832 | 1529 | 25.0 |
| 0.833-0.920 | 1493 | 24.4 |
| FHS municipal coverage—terciles (%) (n = 6185) | ||
| Up to 47.6 | 2064 | 33.4 |
| 47.7-82.0 | 2063 | 33.4 |
| 82.1-100 | 2058 | 33.2 |
Abbreviations: FHS, Family Health Strategy; HDI-M, Municipal Human Development Index.
a1 US$ = R$ 3.26.
With regard to the 9 items used to evaluate service structure, 7 of them presented prevalence higher than 80%, with the exception of monofilament kits and ophthalmoscopes, which were found in 36.2% and 21.2% of PHCs, respectively (Figure 1). Applying the study criteria, only 9.4% of PHCs were considered to have adequate structure, with higher proportions in the Southeast region (15.9%) and larger municipalities with higher HDI-M. An inverse relationship was found between FHS municipal coverage and better structure (Table 2).
Figure 1.
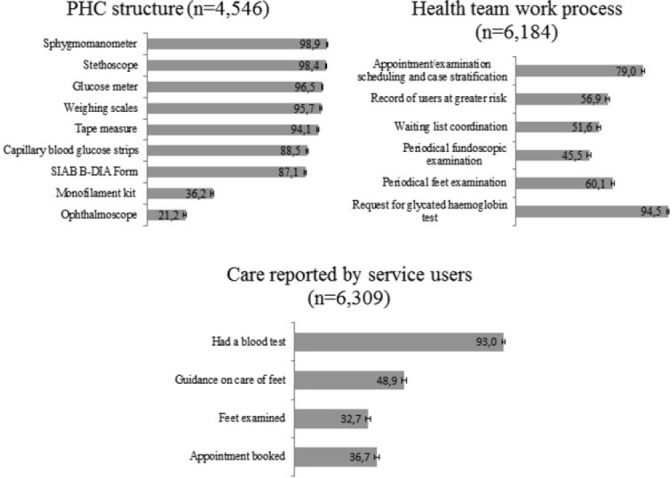
Structure, work process, and care indicator prevalence reported by users with diabetes (Ministério da Saúde, Brasil, 2015a).
Table 2. Distribution of Users With Diabetes With Adequate Structure of PHC, Access and Quality Reported by Health Teams, According to Independent Variables (Ministério da Saúde, Brasil, 2015a).
| Variable | Adequate Structurea (%) | Access to PHCb (%) | PHC Organization and Management Qualityc (%) | Quality of Clinical Care Contentd (%) |
|---|---|---|---|---|
| Region | P < .001 | P < .001 | P < .001 | P < .001 |
| North | 1.7 | 41.5 | 25.0 | 17.7 |
| Northeast | 1.7 | 39.2 | 29.7 | 26.4 |
| Southeast | 15.9 | 63.6 | 39.4 | 42.4 |
| South | 2.2 | 53.4 | 30.4 | 27.8 |
| Midwest | 4.9 | 54.2 | 24.8 | 24.2 |
| Population size (inhabitants) | P < .001 | P < .001 | P < .001 | P < .001 |
| Very small | 5.3 | 54.7 | 29.6 | 20.3 |
| Small | 3.1 | 52.1 | 29.6 | 21.4 |
| Median | 2.5 | 50.5 | 29.2 | 24.5 |
| Large | 4.4 | 52.7 | 33.9 | 32.3 |
| Very large | 22.7 | 62.6 | 43.5 | 57.8 |
| HDI-M quartiles | P < .001 | P < .001 | P < .001 | P < .001 |
| 0.480-0.696 | 2.7 | 43.7 | 31.3 | 19.2 |
| 0.697-0.779 | 4.5 | 54.2 | 27.8 | 24.1 |
| 0.780-0.832 | 3.4 | 58.1 | 32.9 | 36.2 |
| 0.833-0.920 | 28.9 | 67.4 | 46.6 | 59.4 |
| FHS municipal coverage—terciles (%) | P < .001 | P < .001 | P < .001 | P < .001 |
| Up to 47.6 | 19.0 | 65.5 | 41.7 | 51.8 |
| 47.7-82.0 | 5.9 | 52.4 | 30.2 | 31.0 |
| 82.1-100 | 3.8 | 48.7 | 31.4 | 21.1 |
| Total | 9.4 | 55.5 | 33.8 | 34.0 |
Abbreviations: FHS, Family Health Strategy; HDI-M, Municipal Human Development Index; PHC, primary health care center.
aAll 9 items: sphygmomanometer, adult stethoscope, monofilament kit, ophthalmoscope, weighing scales, tape measure, glucometer, capillary blood glucose strips, and the B-DIA form used for the Primary Health Care Information System (SIAB).
bAppointment any day and at any time health center open.
cRecords of users at greater risk/appointment scheduling/waiting list coordination and follow-up by the health network.
dPeriodical foot examination/periodical fundoscopic examination/request for glycated haemoglobin test.
Access to appointments on any day and time during opening hours was reported by 56% of health teams. Prevalence was higher in the Southeast and Midwest regions, in municipalities with more than 300 000 inhabitants, and as HDI-M increased. The best access indices were found in municipalities with less than 100% FHS coverage (Table 2).
The evaluation items relating to service organization and management had the following prevalence: appointment scheduling 79.0%, records of service users at greater risk 56.9%, and waiting list coordination 51.6%. Adequacy, as assessed on the basis of all the service organization and management items, was 34% for the sample as a whole. The proportion was higher in the Southeast region, in municipalities with more than 300 000 inhabitants, with higher HDI and lower FHS coverage.
The items relating to clinical care showed 94.5% for glycated haemoglobin test requests, 60.1% for periodical foot examination, and 45.5% for periodical fundoscopic examination (Figure 1). In addition, 34% of the teams answered the set of questions positively and the same pattern of association as with the previous variable was found (Table 2).
Almost 90% of interviewed users had access to appointments for diabetes at PHC in the last 6 months. Lower access proportions were found in the Northern region, in municipalities with fewer than 300 000 inhabitants, lower HDI-M, and higher FHS coverage (Table 3).
Table 3. Proportion of Users With Diabetes According to Access, Perception of Care Quality, Satisfaction With PHCs and Self-reported Receipt of Appropriate Care (Ministério da Saúde, Brasil, 2015a) (n = 6.309).
| Variable | Access to Appointment at PHC in Last 6 Monthsa (%) | Organization and Management Qualityb (%) | Clinical Care Qualityc (%) | Satisfaction With Serviced (%) | Self-reported Receipt of Appropriate Caree |
|---|---|---|---|---|---|
| Region | P < .05 | P < .001 | P < .05 | P < .05 | P < .001 |
| North | 83.9 | 38.0 | 18.3 | 85.0 | 10.7 |
| Northeast | 86.2 | 37.6 | 22.2 | 88.3 | 12.3 |
| Southeast | 88.4 | 35.2 | 31.4 | 90.4 | 16.2 |
| South | 86.6 | 27.9 | 23.7 | 91.1 | 10.0 |
| Midwest | 85.8 | 33.2 | 26.6 | 89.0 | 15.9 |
| Population size (inhabitants) | P < .05 | P < .001 | P < .001 | P < .05 | P < .001 |
| Very small: up to 10,000 | 86.9 | 29.9 | 25.9 | 91.2 | 12.6 |
| Small: 10 001-30 000 | 85.6 | 33.7 | 24.6 | 91.0 | 12.0 |
| Median: 30 001-100 000 | 86.6 | 34.6 | 24.2 | 89.7 | 12.6 |
| Large: 100 001-300 000 | 85.9 | 37.5 | 28.2 | 89.2 | 16.4 |
| Very large: Over 300 000 | 89.7 | 36.2 | 32.3 | 88.4 | 14.3 |
| HDI-M quartiles | P < .001 | P = .063 | P < .001 | P = .786 | P < .001 |
| 0.480-0.696 | 86.7 | 37.9 | 21.9 | 89.2 | 11.6 |
| 0.697-0.779 | 84.7 | 33.8 | 25.8 | 89.6 | 13.1 |
| 0.780-0.832 | 86.9 | 37.5 | 30.5 | 90.1 | 15.2 |
| 0.833-0.920 | 90.7 | 37.4 | 34.0 | 90.2 | 17.4 |
| FHS municipal coverage terciles (%) | P < .05 | P < .001 | P < .001 | P = .070 | P < .001 |
| Up to 47.6 | 88.9 | 40.9 | 32.8 | 89.2 | 17.7 |
| 47.7-82.0 | 86.8 | 36.0 | 25.7 | 89.1 | 12.9 |
| 82.1-100 | 86.1 | 33.2 | 25.3 | 91.0 | 12.1 |
| Total | 87.2 | 34.6 | 27.9 | 89.7 | 14.3 |
Abbreviations: FHS, Family Health Strategy; HDI-M, Municipal Human Development Index; PHC, primary health care center.
aQuestion is valid for those reporting diagnosis of diabetes (n = 8118).
bAt the end of one appointment, the next one is always booked.
cPositive answers to all items: blood glucose test/foot examination/guidance on caring for feet.
dIf they could, they would not change their health team or health center.
eReporting having received a blood test, received guidance on foot care, had their feet examined, and having been able to book an appointment.
Thirty-five percent of service users in the sample reported that their next appointment was always booked at the end of their current appointment. Proportions were higher in the North and Northeast regions, in larger municipalities, and municipalities with lower FHS coverage. No difference was found with regard to HDI (Table 3).
Having blood tests was the most prevalent reference (93.0%), while guidance on care of feet was mentioned by 48.9% and having had their feet examined was reported by 32.7% (Figure 1). When using a score for these variables as a whole, 28% of respondents mentioned all items, with higher proportions in the Southeast and Midwest regions, as well as in larger municipalities and in municipalities with higher HDI and lower FHS coverage (Table 3).
Ninety percent of users replied that they would not change their health teams or health centers, even if they could, lower in the Northern region and decreased as municipality size increased (Table 3).
Users self-reporting receipt of appropriate care were 14.3%, significantly more present in the Southeast and Midwest regions and in municipalities with larger populations, higher HDI, and lower Family Health coverage and men users (Table 3). Following adjustment, the outcome was 26% (PR = 1.26; 95% confidence interval [CI]: 1.04-1.54) greater when the PHC offered all the structure items assessed. It was 13% (PR = 1.13; 95% CI: 1.00-1.29) greater when work process was adequate with regard to service organization and management and it was 14% (PR = 1.14; 95% CI: 1.00-1.30) greater when clinical practice was appropriate. When the region variable was added, the PR decreased and lost statistical significance in all associations (Table 4).
Table 4. Prevalence and Prevalence Ratios—Crude and Adjusted—for Self-reported Receipt of Appropriate Care According to Service Structure and Team Work Process (Ministério da Saúde, Brasil, 2015a) (n = 6309).
| Prevalencea (%) | PR (95% CI)b Crude | PR (95% CI) Adjustedc | PR (95% CI) Adjustedd | |
|---|---|---|---|---|
| Service has all 9 structure items | ||||
| No | 13.7 | 1.00 | 1.00 | 1.00 |
| Yes | 20.0 | 1.47 (1.23-1.74) | 1.26 (1.04-1.54) | 1.18 (0.96-1.44) |
| High-quality service organization and management | ||||
| No | 13.4 | 1.00 | 1.00 | 1.00 |
| Yes | 15.9 | 1.18 (1.05-1.34) | 1.13 (1.00-1.29) | 1.12 (0.98-1.27) |
| High-quality clinical practice | ||||
| No | 13.2 | 1.00 | 1.00 | 1.00 |
| Yes | 16.4 | 1.25 (1.11-1.41) | 1.14 (0.99-1.30) | 1.11 (0.97-1.27) |
Abbreviations: CI, confidence interval; HDI, Human Development Index; PR, prevalence ratio.
aSelf-reported receipt of appropriate care: in the last 6 months, had a blood glucose control test, had feet examined, received guidance on care of feet and left one appointment with the next one already booked.
bPrevalence ratio and 95% confidence interval.
cAdjusted for population size, municipal HDI and municipal Family Health coverage, and user's sex.
dAdjusted for population size, municipal HDI and municipal Family Health coverage, region, and user's sex.
DISCUSSION
The findings of this study show that care for people with diabetes in PHCs is still falling short of expectations with regard to both structure and work process, despite the impressive increase in coverage of FHS in the last 20 years (Ministério da Saúde, Brasil, 2015b).
The availability of some of the items indicated an improvement, given that previous studies found shortfalls in PHCs structure, such as scarcity of capillary blood glucose strips and glucose meters (Assunção et al., 2001; Facchini et al., 2006). Even so, this study still found a small number of health centers with ophthalmoscopes and monofilament kits available.
Despite shortage of kits, the adequate foot examination requires musculoskeletal, vascular, neurological, and skin assessment (Ministério da Saúde, Brasil, 2013) and can be performed without auxiliary equipment. Therefore, the low prevalence of this examination, also reported in relation to elderly Brazilians by Facchini et al. (2014), is a cause for concern, given that foot ulcers and limb amputations are among the most serious chronic complications of DM with higher socioeconomic impact (Boulton et al., 2008).
Many PHCs organize their working week by allocating specific shifts to given groups, such as pregnant women and people with hypertension or diabetes. This practice is not recommended by official protocols and may jeopardize links between the health team and the population they serve, in addition to reducing coverage of health actions.
Keeping records of more serious cases, scheduling appointments and examinations by case stratification, and coordinating and following up on service users with diabetes in the health network are included among the attributes of PHCs (Ministério da Saúde, Brasil, 2013; Starfield, 2002). These actions extrapolate clinical management, involving administrative and organizational aspects, and are the responsibility of the entire team. To optimize their effects, PMAQ should stimulate the support and supervision by municipal management, with emphasis on enhancing information systems, facilitating communication and contact flows.
With regard to the quality of clinical care, health teams should offer fundoscopic and feet examination, as well as guidance on taking care of the feet to all people with diabetes with the aim of achieving maximum coverage, encouraging self-care and health education (Ministério da Saúde, Brasil, 2013). If the benefits of all the actions were achieved, the effectiveness of care would also be scaled up. Consideration must also be given to gaps in medical training providing doctors with little experience in eyes and feet examination. Besides PMAQ efforts, medical schools should encourage skills to basic preventive procedures in diabetes care.
The indicators showed better performance in richest context, as well as the Southeast region, in municipalities with larger populations, higher HDI, and FHS coverage less than 50% (Giovanella et al., 2015). In Brazil, small municipalities have higher FHS coverage and, generally, lower HDI-M (Facchini et al., 2015).
Although the provision of high-quality care to people with diabetes is known to involve aspects such as guidance on nutrition, physical activity and smoking, control of cholesterol levels and weight, as well as cardiovascular risk stratification (Ministério da Saúde, Brasil, 2013; Nicolucci et al., 2006); all 4 variables available were selected from PMAQ data as being markers of diabetes care quality.
Results from synthetic outcome confirm the direct relationship between health service structure and health team work process and health system performance—represented here by service user access and the quality of care received by them—regardless of the contextual differences of the municipalities (Donabedian, 1988; Facchini et al., 2015; Starfield, 2002). When including the region variable in the adjusted model, regional differences above all were found to particularly influence the relationship of the outcome with the forms of exposure in a consistent manner. Given that in Brazil such regional differences express important economic, social, and cultural differences, the results analyzed here confirm that macrostructural conditions overwhelmingly determine health system performance (Facchini et al., 2006; Travassos et al., 2006).
Municipalities and health teams adhered voluntarily to PMAQ and there may have been a tendency to enroll the best services. Health care professionals were aware of the evaluation and had access to its instruments beforehand, and this may have influenced their answers, indicating inducement of good practices. In view of the fact that the sample of users was interviewed at health service facilities, the need exists to assess the occurrence of selection bias, affecting the results of satisfaction. The respondents were regular users of PHC and this allows the assumption to be made that they were representative of the overall set of users of those services. Moreover, studies about typical users of PHC show a similar demographic and socioeconomic profile (Pimentel et al., 2011; Tomasi et al., 2011). Furthermore, most of the findings were similar to those obtained by population-based studies, making evident their critical judgment with regard to the care received (Facchini et al., 2014), and this reinforces the validity of the findings in relation to the proposed objectives.
By evaluating the service via its users, the study provides an important panorama for identifying what can be improved. This is a strong point of the study, since it is the regular user who is in the best position to evaluate the service. Another positive highlight of the study is that fact of it having been conducted by teaching institutions recognized for their competency to undertake this task, as well as being a nationwide study using standardized instruments. The health information systems do not address the systematic recording of care promotion and quality actions, even less so from the point of view of service users, and this implies gaps in knowledge. Evaluations of PHC structure, work process, and results as reported by primary care service users involving a national sample are scarce. This makes the findings of this study relevant and useful for formulating policies and for planning.
Bearing in mind that diabetes prevalence may increase 3-fold in forthcoming years (Schmidt et al., 2011; Wild et al., 2004), if the effectiveness of care increases, this can contribute to minimizing the disease's population impact. The PMAQ survey has provided a comprehensive view of access to and quality of care and this can be institutionalized and extended to other health actions and groups of service users. In a context of political threats to the Unified Health System and its achievement of universal coverage, primary health care needs to be strengthened, thus improving the quality of Brazilian public services.
Universidade Federal do Rio Grande do Norte, Universidade Federal de Pelotas, Universidade Federal do Rio Grande do Sul, Universidade Federal de Minas Gerais, Universidade Federal da Bahia and Fundação Osvaldo Cruz.
We thank the Brazilian Government's Ministry of Health for the financial support.
The authors hereby state that there are no conflicts of interest.
REFERENCES
- Alfradique M. E., Bonolo P. D. F., Dourado I., Lima-Costa M. F., Macinko J., Mendonça C. S., Turci M. A. (2009). Internações por condições sensíveis à atenção primária: a construção da lista brasileira como ferramenta para medir o desempenho do sistema de saúde (Projeto ICSAP-Brasil). Cadernos de Saúde Pública, 25(6), 1337–1349. [DOI] [PubMed] [Google Scholar]
- Alves M. G. D. M., Casotti E., Oliveira L. G. D. D., Machado M. T. C., Almeida P. F. D., Corvino M. P. F., Montenegro L. A. A. (2014). Fatores condicionantes para o acesso às equipes da Estratégia Saúde da Família no Brasil. Saúde debate, 38(Spec.), 34–51. [Google Scholar]
- Araújo R. B., Santos I. D., Cavaleti M. A., Costa J. D., Béria J. U. (1999). Avaliação do cuidado prestado a pacientes diabéticos em nível primário. Revista de Saúde Pública, 33(1), 24–32. [DOI] [PubMed] [Google Scholar]
- Assunção M. C. F., Santos I. S., Gigante D. P. (2001). Atenção primária em diabetes no Sul do Brasil: estrutura, processo e resultado. Revista de Saúde Pública, 35(1), 88–95. [DOI] [PubMed] [Google Scholar]
- Boulton A. J., Armstrong D. G., Albert S. F., Frykberg R. G., Hellman R., Kirkman M. S., Wukich D. K. (2008). Comprehensive foot examination and risk assessment a report of the task force of the foot care interest group of the American Diabetes Association, with endorsement by the American Association of Clinical Endocrinologists. Diabetes Care, 31(8), 1679–1685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casotti E., Contarato P. C., Fonseca A. B. M., Borges P. K. D. O., Baldani M. H. (2014). Atenção em saúde bucal no Brasil: uma análise a partir da avaliação externa do PMAQ-AB. Saúde Debate, 38(Spec.), 140–157. [Google Scholar]
- Cavalcante R. B., Silva J. J., de Alcantara Azevedo J., Salomé H. S., Diniz F. A. (2015). Percepções sobre instrumentos de coleta de um Sistema de Informação. Journal of Health Informatics, 7(1), 16–22. [Google Scholar]
- Costa M. F. L., Matos D. L., Camargos V. P., Macinko J. (2011). Tendências em dez anos das condições de saúde de idosos brasileiros: evidências da Pesquisa Nacional por Amostra de Domicílios (1998, 2003, 2008). Ciência & Saúde Coletiva, 16(9), 3689–3696. [DOI] [PubMed] [Google Scholar]
- Cruz M. M. D., Souza R. B. C. D., Torres R. M. C., Abreu D. M. F. D., Reis A. C., Gonçalves A. L. (2014). Usos do planejamento e autoavaliação nos processos de trabalho das equipes de Saúde da Família na Atenção Básica. Saúde Debate, 38(Spec.), 124–139. [Google Scholar]
- Donabedian A. (1988). The quality of care: How can it be assessed? JAMA, 260(12):1743–1748. [DOI] [PubMed] [Google Scholar]
- Facchini L. A., Nunes B. P., Duro S. M. S., Thumé E., Siqueira F. C. V., Fripp J. C., Tomasi E. (2014). Iniquidades socioeconômicas no acesso e na qualidade da atenção ao diabetes entre idosos brasileiros Brasília. In: CONASS debate: a crise contemporânea dos modelos de atenção à saúde (1st ed., Vol. 1, pp. 88–106). Brasília, DF: CONASS. [Google Scholar]
- Facchini L. A., Piccini R. X., Tomasi E., Thumé E., Silveira D. S., Siqueira F. V., Rodrigues M. A. (2006). Desempenho do PSF no Sul e no Nordeste do Brasil: avaliação institucional e epidemiológica da Atenção Básica à Saúde. Ciência & Saúde Coletiva, 11(3), 669–681. [Google Scholar]
- Facchini L. A., Thumé E., Nunes B. P., Duro S. M. S., Fassa A. G., Garcia L. P., Tomasi E. (2015). Governance and health system performance: National and municipal challenges to the Brazilian family health strategy. In: Reich M. R., Takemi K. (Eds.), Governing health systems for nations and communities around the world (1st ed., pp. 203–236.). Boston, MA: Lamprey, & Lee. [Google Scholar]
- Giovanella L., Bousquat A., Fausto M. C. R., Fusaro E. R., Mendonça M. H. M., Gagno J. (2015). Tipologia das Unidades Básicas de Saúde Brasileiras. Região e Redes. Nota Técnica 5. Disponível em. Retrieved from http://www.resbr.net.br/wp-content/uploads/2015/09/NovosCaminhos05_ValeEste.pdf
- Gonçalves M. R., Harzheim E., Zils A. D. A., Duncan B. B. (2013). A qualidade da atenção primária e o manejo do diabetes mellitus. Revista Brasileira de Medicina de Família e Comunidade, 8(29), 235–243. [Google Scholar]
- Habicht J. P., Victora C., Vaughan J. P. (1999). Evaluation designs for adequacy, plausibility and probability of public health programme performance and impact. International Journal of Epidemiology, 28(1), 10–18. [DOI] [PubMed] [Google Scholar]
- Instituto Brasileiro de Geografia e Estatística. (2010). Censo 2010 [internet database]. Retrieved from http://www.ibge.gov.br/home/estatistica/populacao/censo2010
- Instituto Brasileiro de Geografia e Estatística. (2014). Pesquisa Nacional de Saúde, 2013: percepção do estado de saúde, estilos de vida e doenças crônicas. Rio de Janeiro-RJ, 181. [Google Scholar]
- Iser B. P. M., Stopa S. R., Chueiri P. S., Szwarcwald C. L., Malta D. C., Monteiro H. O. D. C., Schmidt M. I. (2015). Prevalência de diabetes autorreferido no Brasil: resultados da Pesquisa Nacional de Saúde 2013. Epidemiologia e Serviços de Saúde, 24(2), 305–314. [Google Scholar]
- Jardim A. D. I., Leal A. M. (2009). Qualidade da informação sobre diabéticos e hipertensos registrada no Sistema HIPERDIA em São Carlos-SP, 2002–2005. Physis (Rio J.), 19(2), 405–417. [Google Scholar]
- Medina M. G., Aquino R., Vilasbôas A. L. Q., Mota E., Júnior P., Pereira E., Pinto I. C. D. M. (2014). Promoção da saúde e prevenção de doenças crônicas: o que fazem as equipes de Saúde da Família?. Saúde Debate, 38(Spec.), 69–82. [Google Scholar]
- Mendes L. V., Campos M. R., Chaves G. C., Silva R. D., Freitas P. D. S., Costa K. S., Luiza V. L. (2014). Disponibilidade de medicamentos nas unidades básicas de saúde e fatores relacionados: uma abordagem transversal. Saúde Debate, 38(Spec.), 109–123. [Google Scholar]
- Ministério da Saúde, Brasil. (2013). Estratégias para o cuidado da pessoa com doença crônica—Diabetes Mellitus (p. 162). Brasília-DF: Departamento de Atenção Básica, Cad. n°36. [Google Scholar]
- Ministério da Saúde, Brasil. (2015a). Programa Nacional de Melhoria do Acesso e da Qualidade da Atenção Básica [internet database]. Retrieved from http://dab.saude.gov.br/sistemas/pmaq/faq.php
- Ministério da Saúde, Brasil. (2015b). Histórico de cobertura da saúde da família [Internet database]. Retrieved from http://dab.saude.gov.br/portaldab/historico_cobertura_sf.php
- Nicolucci A., Greenfield S., Mattke S. (2006). Selecting indicators for the quality of diabetes care at the health systems level in OECD countries. International Journal for Quality in Health Care, 18(Suppl. 1), 26–30. [DOI] [PubMed] [Google Scholar]
- Organização Pan-Americana da Saúde. (2010). Linhas de cuidado: hipertensão arterial e diabetes (p. 232). Brasília, DF: Author.s [Google Scholar]
- Paiva D. C. P. D., Bersusa A. A. S., Escuder M. M. L. (2006). Avaliação da assistência ao paciente com diabetes e/ou hipertensão pelo Programa Saúde da Família do Município de Francisco Morato, São Paulo, Brasil. Cadernos de Saúde Pública, 22(2), 377–385. [DOI] [PubMed] [Google Scholar]
- Pimentel Í. R. S., Coelho B. C., Lima J. C., Ribeiro F. G., de Castro Sampaio F. P., Pinheiro R. P., Rocha Filho F. S. (2011). Caracterização da demanda em uma Unidade de Saúde da Família. Revista Brasileira de Medicina de Família e Comunidade, 6(20), 175–181. [Google Scholar]
- Programa das Nações Unidas para o Desenvolvimento. (2016). Evolução do desenvolvimento humano nos municípios brasileiros [internet database]. Retrieved from www.pnud.org.br
- Schmidt M., Duncan B., Silva G., Menezes A., Monteiro C., Barreto S., Menezes P. R. (2011). Chronic non communicable diseases in Brazil: Burden and current challenges. The Lancet, 377(9781), 1949–1961. [DOI] [PubMed] [Google Scholar]
- Seidl H., Vieira S. D. P., Fausto M. C. R., Lima R. D. C. D., Gagno J. (2014). Gestão do trabalho na Atenção Básica em Saúde: uma análise a partir da perspectiva das equipes participantes do PMAQ-AB. Saúde Debate, 38(Spec.), 94–108. [Google Scholar]
- Starfield B. (2002). Atenção primária: equilíbrio entre necessidades de saúde, serviços e tecnologia. Brasila, DF: UNESCO. [Google Scholar]
- Teixeira M. B., Casanova A., Oliveira C. C. M. D., Ensgtrom E. M., Bodstein R. C. D. A. (2014). Avaliação das práticas de promoção da saúde: um olhar das equipes participantes do Programa Nacional de Melhoria do Acesso e da Qualidade da Atenção Básica. Saúde Debate, 38(Spec.), 52–68. [Google Scholar]
- Tomasi E., Facchini L. A., Thumé E., Piccini R. X., Osório A., Silveira D. S. D., Maia M. D. F. S. (2011). Características da utilização de serviços de Atenção Básica à Saúde nas regiões Sul e Nordeste do Brasil: diferenças por modelo de atenção. Ciência & Saúde Coletiva, 16(11), 3689–3696. [DOI] [PubMed] [Google Scholar]
- Tomasi E., Fischer Oliveira T., Fernandes P. A. A., Thumé E., Silveira D. S., Vinholes Siqueira F., Facchini L. A. (2015). Estrutura e processo de trabalho na prevenção do câncer de colo de útero na Atenção Básica à Saúde no Brasil: Programa de Melhoria do Acesso e da Qualidade-PMAQ. Revista Brasileira de Saúde Materno Infantil, 15(2), 171–180. [Google Scholar]
- Travassos C., Oliveira E. D., Viacava F. (2006). Desigualdades geográficas e sociais no acesso aos serviços de saúde no Brasil: 1998 e 2003. Ciência & Saúde Coletiva, 11(4), 975–986. [Google Scholar]
- UK Prospective Diabetes Study Group. (1998a). Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). The Lancet, 352(9131), 837–853. [PubMed] [Google Scholar]
- UK Prospective Diabetes Study Group. (1998b). Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. BMJ, 317(7160), 703. [PMC free article] [PubMed] [Google Scholar]
- Wild S., Roglic G., Green A., Sicree R., King H. (2004). Global prevalence of diabetes estimates for the year 2000 and projections for 2030. Diabetes Care, 27(5), 1047–1053. [DOI] [PubMed] [Google Scholar]


