Highlights
-
•
Glioblastoma is the most common and most aggressive type of brain tumors. Prognosis is poor: death occurs within 12–18 months from diagnosis.
-
•
There is however a small percentage of Patients affected by glioblastoma who survive 3 years or longer.
-
•
There are some exceptional cases when people have survived decades after surgical removal of a glioblastoma without any recurrence.
-
•
We report a case of a 44 year-old man operated for a glioblastoma. 22 years after surgery the patient has no recurrence of the tumor.
-
•
Long-survival depends on young age, complete surgical excision, good Karnofsky index score, radiotherapy and molecular make-up of glioma.
Keywords: Case report, Glioblastoma multiforme, Primary brain tumor, Long-survival, Treatment, Prognostic factors
Abstract
Introduction
Glioblastoma multiforme is the most aggressive type of primary brain tumors, but there is a small percentage of patients who have a long-term survival and some exceptional cases who survive decades after surgical removal of tumor.
Presentation of case
In 1994, a 44 year-old man, suffering from intense headache and loss of strength of the left arm, was operated for a glioblastoma multiforme in the posterior part of the right frontal lobe. After the operation the patient underwent whole-brain radiotherapy and chemotherapy. 22 years after surgery the patient has no recurrence of the tumor.
Discussion
A very small percentage of glioblastoma cases showed >3 years survival. There have been exceptional cases of long-survival spanning 10 years or more, without tumor recurrence, so as to deem those affected ‘cured’. The long-survival for glioblastoma multiforme is linked to young age, to aggressive and complete surgical excision, a good Karnofsky index score before surgery, the application of radiotherapy after surgery and to the molecular make-up of a specific glioma.
Conclusion
The fact that there are extremely rare cases of long-term survival and even zero recurrence of the glioblastoma should serve as a stimulus to continue the research effort and not give up the fight against this tumor on a day-to-day basis.
1. Introduction
Glioblastoma multiforme is the most common and most aggressive type of primary brain tumors. Despite improved surgical techniques, therapies and radiotherapies, prognosis for this type of pathology remains very poor: most patients die within 12–18 months from diagnosis [1].
There is however a small percentage of Patients affected by glioblastoma multiforme who survive 3 years or longer [2], [3]. Finally there are some exceptional cases, such as the one we are describing in this article, when people have survived decades after surgical removal of a glioblastoma without any recurrence.
This work has been reported in line with the SCARE criteria [4].
2. Presentation of case
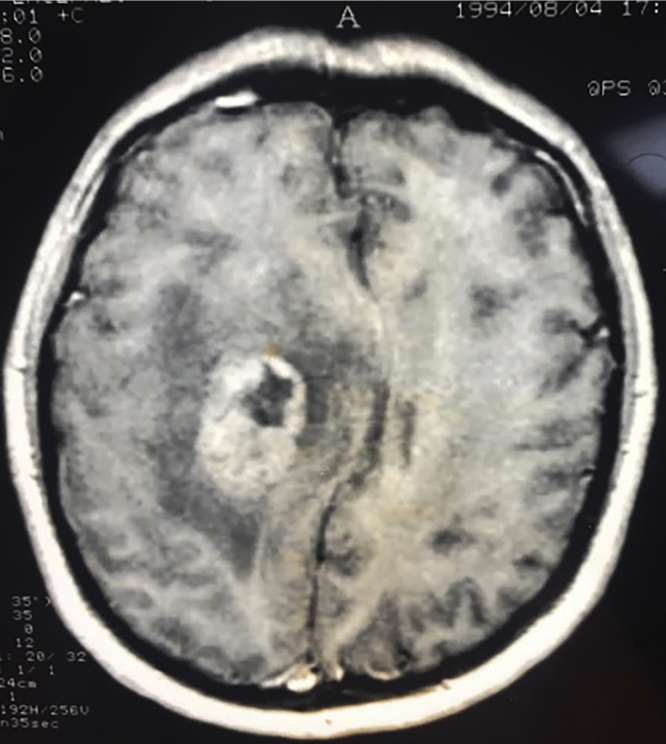
In 1994, a 44 year-old man was admitted to the Neurosurgical department of the Military Hospital of Rome; for about a month he had been suffering from intense headache and loss of strength of the left arm. An MRI scan showed the presence of a tumor in the posterior part of the right frontal lobe (Fig. 1).
Fig. 1.
The MRI scan shows the presence of a tumor in the posterior part of the right frontal lobe. The tumor absorbs the contrast medium, in its interior it can be seen an area of necrosis,and it is surrounded by cerebral edema.
The Patient underwent surgery: the tumor was intraparenchymal and looked like a glioma. It was removed seemingly in-toto. Histological examination showed the neoplasia to be a glioblastoma multiforme.
The patient’s postoperative course was uneventful and the loss of strength in the left arm disappeared within three weeks.
After the operation the patient underwent whole-brain radiotherapy (total dose 55 Gy) and nitrosurea-based chemotherapy.
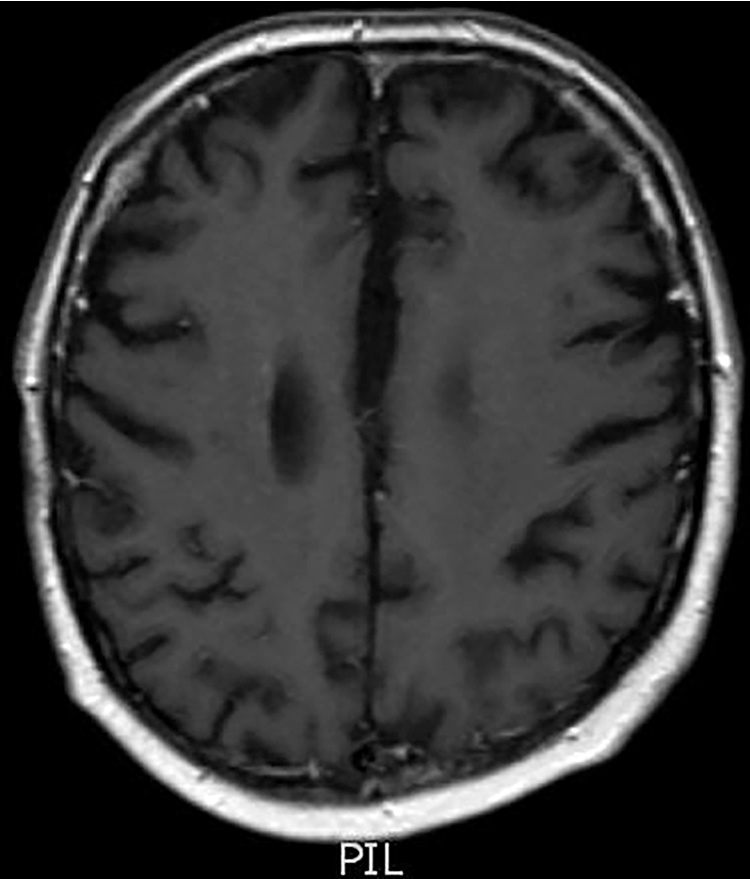
Three months after surgery the patient had a first check up CT scan to see if there was any recurrence of the tumor. Since then, he has had regular scans, further and further apart in time, which to-date have shown no presence of the pathology. Fig. 2 shows the last MRI scan carried out in July 2016, 22 years after the operation. The neurological conditions of the patient, who is currently 66, are normal.
Fig. 2.
The MRI scan showed no presence of the pathology.
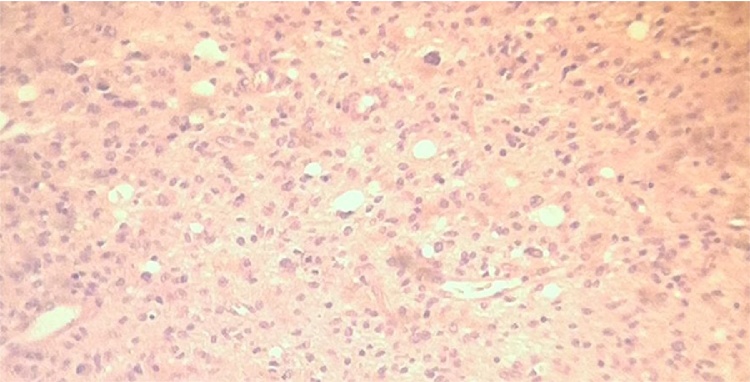
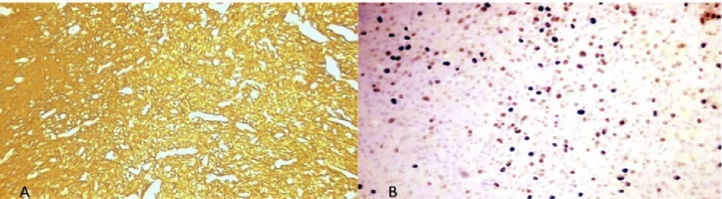
In the Anatomic Pathology Archive of our hospital we kept the microscope slides with the cell samples of this case. Before writing this article we have showed the slides to three neuropathologists who have all confirmed that the morphological appearance of the histological samples is that typical of a glioblastoma, thus confirming the original histological report (Fig. 3, Fig. 4)
Fig. 3.
(10x) Hematoxilin and Eosin, demonstrating an hypercellular cluster of the glioma with microcystic degeneration, bizarre pleomorphic cells; high grade nuclear atypia with prominent nucleoli.
Fig. 4.
(10x) The lesion shows (A) a strong GFAP immunoreactivity and 3–(B) high proliferating index (Ki67 immunostaining).
3. Discussion
In the last ten years neuronavigation techniques associated also with functional NMR [5], as well as the use of substances like 5-Aminolevulinic acid hydrochloride [6], which mark and thus make tumoral tissue easier to identify during an operation, have improved surgery for cerebral gliomas; in fact they allow for a more thorough excision and they also lower the risk of causing functional damage during surgery.
Therapy for gliomas has also evolved, as indicated by the introduction of monoclonal chemotherapy [7] and telozolomide treatment combined with radiotherapy [8].
Together with the traditional fractionated external beam RT (EBRT), nowadays there are new radiotherapy techniques like the intensity-modulated RT (IMRT) and stereotactic radiosurgery [9].
Despite the advancements, median survival, especially for Grade 4 gliomas and for glioblastomas doesn’t exceed 12–18 months from diagnosis [10]. A very small percentage of cases showed >3 years survival, in other words long-survival. There have been exceptional cases [11], [12] of long-survival spanning 10 years or more, without tumor recurrence, so as to deem those affected ‘cured’. The possibility of a complete recovery from glioblastoma was suggested by the Yamada et al. case [13]: after dying of skull trauma, an autopsy limited to the brain was performed on a patient who had undergone surgery for a glioblastoma multiforme 6.5 years before; the team carefully searched for the presence of cancer without success, despite collecting numerous histological samples. There was simply no trace of the tumor. Cases like ours, with more than 20 years survival span and no recurrence are extremely rare [14], [15], [16], [17] (Table 1).
Table 1.
20-plus-year survival cases.
| Authors | Age and Sex | Survival Time and Status |
|---|---|---|
| ELVIDGE, BARONE | 30 yrs, W | 22 yrs alive |
| JOHNSON et al | 32 yrs, M | 22 yrs alive |
| BUCY et al | 30 yrs, M | 25 yrs alive |
| SALFORD et al | 8 yrs, M | 23 yrs alive |
| CARUSO et al | 44 yrs, M | 22 yrs alive |
M = man, W = woman, yrs = years
In the Literature [1], [2] it has been noted that long-survival for glioblastoma multiforme is linked to age, with better rates for those below 65 years of age, but also to aggressive and complete surgical excision, a good Karnofsky index score before surgery and the application of radiotherapy after surgery.
Some authors remarked that the occurrence of a bacterial infection in the location of the operation after the removal of a glioma can improve a patient’s longevity, probably due to a stronger immune response from the body [18], [19]. Other authors have linked long-survival after surgery to the molecular make-up of a specific glioma, for example the abscence of epidermal growth factor receptor gene amplification, the presence of MGMT promotor hypermethylation, IDH1 mutation [20]. There is so far no satisfactory explanation as to why certain cases can be deemed cured, but total – gross resection of the tumor followed by radiotherapy and a Patient’s individual immune response certainly play an important role.
4. Conclusion
Despite research and improved therapies, today a glioblastoma diagnosis equates to a death sentence. However the fact that there are extremely rare cases of long-term survival and even zero recurrence of the pathology should serve as a stimulus to continue the research effort and not give up the fight against this tumor on a day-to-day basis.
Conflict of interest
We wish to confirm that there are no known conflicts of interest associated with this publication.
Funding
We wish to confirm that there has been no significant financial support for this work that could have influenced its outcome.
Ethical approval
None.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Authors contribution
Riccardo Caruso: study concept, writing the paper.
Alessandro Pesce: data analysis.
Venceslao Wierzbicki: data collection.
We confirm that the manuscript has been read and approved by all named authors and that there are no other persons who satisfied the criteria for authorship but are not listed. We further confirm that the order of authors listed in the manuscript has been approved by all of us.
Registration of research studies
We don’t need to register this work.
Guarantor
We understand that the Corresponding Author is the sole contact for the Editorial process (including Editorial Manager and direct communications with the office).He is responsible for communicating with the other authors about progress, submissions of revisions and final approval of proofs. We confirm that we have provided a current, correct email address which is accessible by the Corresponding Author and which has been configured to accept email from riccardo.caruso@uniroma1.it.
References
- 1.Stark A.M., van de Bergh J., Hedderich J., Mehdorn H.M., Glioblastoma Nabavi A. Clinical characteristics, prognostic factors and survival in 492 patients. Clin. Neurol. Neurosurg. 2012;114:840–845. doi: 10.1016/j.clineuro.2012.01.026. [DOI] [PubMed] [Google Scholar]
- 2.Salvati M., Cervoni L., Artico M., Caruso R., Gagliardi F.M. Long-term survival in patients with supratentorial glioblastoma. J. Neurooncol. 1998;36(1):61–64. doi: 10.1023/a:1017926603341. [DOI] [PubMed] [Google Scholar]
- 3.Smoll N.R., Schaller K., Gautschi O.P. Long-term survival of patients with glioblastoma multiforme (GBM) J. Clin. Neurosci. 2013;20(5):670–675. doi: 10.1016/j.jocn.2012.05.040. [DOI] [PubMed] [Google Scholar]
- 4.Agha R.A., Fowler A.J., Saeta A., Barai I., Rajmohan S., Orgill D.P. The SCARE Statement: consensus-based surgical case report guidelines. Int. J. Surg. 2016;34:180–186. doi: 10.1016/j.ijsu.2016.08.014. [DOI] [PubMed] [Google Scholar]
- 5.Kubben P.L., ter Meulen K.J., Schijns O.E., ter Laak-Poort M.P., van Overbeeke J.J., van Santbrink H. Intraoperative MRI-guided resection of glioblastoma multiforme: a systematic review. Lancet Oncol. 2011;12(11):1062–1070. doi: 10.1016/S1470-2045(11)70130-9. [DOI] [PubMed] [Google Scholar]
- 6.Stummer W., Pichlmeier U., Meinel T., Wiestler O.D., Zanella F., Reulen H.J. Fluorescence-guided surgery with 5-aminolevulinic acid for resection of malignant glioma: a randomised controlled multicentre phase III trial. Lancet Oncol. 2006;7(5):392–401. doi: 10.1016/S1470-2045(06)70665-9. [DOI] [PubMed] [Google Scholar]
- 7.McLendon R.E., Halperin E.C. Is the long-term survival of patients with intracranial glioblastoma multiforme overstated? Cancer. 2003;98(8):1745–1748. doi: 10.1002/cncr.11666. [DOI] [PubMed] [Google Scholar]
- 8.Barbagallo G.M., Paratore S., Caltabiano R., Palmucci S., Parra H.S., Privitera G. Long-term therapy with temozolomide is a feasible option for newly diagnosed glioblastoma: a single-institution experience with as many as 101 temozolomide cycles. Neurosurg. Focus. 2014;37(6):E4. doi: 10.3171/2014.9.FOCUS14502. [DOI] [PubMed] [Google Scholar]
- 9.Chan M.F., Schupak K., Burman C., Chui C.S. Clifton Ling C: comparison of intensity-modulated radiotherapy with three-dimensional conformal radiation therapy planning for glioblastoma multiforme. Med. Dosim. 2003;28(4):261–265. doi: 10.1016/j.meddos.2003.08.004. [DOI] [PubMed] [Google Scholar]
- 10.Adamson C., Kanu O.O., Mehta A.I., Di C., Lin N., Mattox A.K. Glioblastoma multiforme: a review of where we have been and where we are going. Expert. Opin. Invest. Drugs. 2009;18(8):1061–1083. doi: 10.1517/13543780903052764. [DOI] [PubMed] [Google Scholar]
- 11.Puzzilli F., Ruggeri A., Mastronardi L., Di Stefano D., Lunardi P. Long-term survival in cerebral glioblastoma: Case report and critical review of the literature. Tumori. 1998;84(1):69–74. doi: 10.1177/030089169808400115. [DOI] [PubMed] [Google Scholar]
- 12.Yoshida T., Kawano N., Oka H., Fujii K., Nakazato Y. Clinical cure of glioblastoma. Two case reports. Neurol. Med. Chir. 2000;40:224–229. doi: 10.2176/nmc.40.224. [DOI] [PubMed] [Google Scholar]
- 13.Yamada S., Endo Y., Hirose T., Takada K., Usui M., Hara M. Autopsy findings in a long-term survivor with glioblastoma multiforme: case report. Neurol. Med. Chir. 1998;38:95–99. doi: 10.2176/nmc.38.95. [DOI] [PubMed] [Google Scholar]
- 14.Elvidge A.R., Barone B.M. Long-Term postoperative survival in two cases of glioblastoma multiforme. J. Neurosurg. 1965;22:382–386. doi: 10.3171/jns.1965.22.4.0382. [DOI] [PubMed] [Google Scholar]
- 15.Johnson A.C. Malignant intracranial tumor: report of three cases with long-term postoperative survival. Surg. Neurol. 1981;15(3):217–219. doi: 10.1016/0090-3019(81)90147-6. [DOI] [PubMed] [Google Scholar]
- 16.Bucy P.C., Oberhill H.R., Siqueira E.B., Zimmerman H.M., Jelsma R.K. Cerebral glioblastomas can Be cured!! Neurosurrgery. 1985;16(5):714–717. doi: 10.1227/00006123-198505000-00027. [DOI] [PubMed] [Google Scholar]
- 17.Salford L.G., Brun A., Nirfalk S. Ten-year survival among patients with supratentorial astrocytomas grade III and IV. J. Neurosurg. 1988;69:506–509. doi: 10.3171/jns.1988.69.4.0506. [DOI] [PubMed] [Google Scholar]
- 18.Di Lorenzo N., Palma L., Nicole S. Lymphocytic infiltration in long-survival glioblastomas: possible host’s resistance. Acta Neurochir. (Wien) 1977;39(1-2):27–33. doi: 10.1007/BF01405238. [DOI] [PubMed] [Google Scholar]
- 19.Bowles A.P.J., Perkins E. Long-term remission of malignant brain tumors after intracranial infection: a report of four cases. Neurosurgery. 1999;44(3):636–642. doi: 10.1097/00006123-199903000-00110. [DOI] [PubMed] [Google Scholar]
- 20.Krex D., Klink B., Hartmann C., von Deimling A., Pietsch T., Simon M. Long-term survival with glioblastoma multiforme. Brain. 2007;130(Pt 10):2596–2606. doi: 10.1093/brain/awm204. [DOI] [PubMed] [Google Scholar]