Abstract
Background
CPR training rates in the US are low, highlighting the need to develop CPR educational approaches that are simpler, with broader dissemination potential. The minimum training required to ensure long-term skill retention remains poorly characterized. We compared CPR skill retention among laypersons randomized to training with video-only (VO; no manikin) to those trained with a video self-instruction kit (VSI; with manikin). We hypothesized that VO training would be non-inferior to the VSI approach with respect to chest compression (CC) rate.
Methods and Results
We performed a prospective cluster randomized trial of CPR education for family members of high-risk cardiac patients on hospital cardiac units, using a multicenter pragmatic design. Eight hospitals were randomized to offer either VO or VSI training before discharge using volunteer trainers. CPR skills were assessed six months post-training. Mean CC rate among those trained with VO compared to VSI was assessed with a non-inferiority margin set at 8 CC per min (cpm); as a secondary outcome, mean differences in CC depth were assessed. From 2/2012 to 5/2015, 1464 subjects were enrolled and 522 subjects completed a skills assessment. The mean CC rates were 87.7(VO) cpm and 89.3 (VSI) cpm; we concluded non-inferiority for VO based on a mean difference of −1.6 (90% CI: −5.2, 2.1). The mean CC depth was 40.2 mm (VO) and 45.8 mm (VSI) with a mean difference of −5.6 (95% CI: −7.6, −3.7). Results were similar after multivariate regression adjustment.
Conclusions
In this large prospective trial of CPR skill retention, VO training yielded a non-inferior difference in CC rate compared to VSI training. CC depth was greater in the VSI group. These findings suggest a potential trade-off in efforts for broad dissemination of basic CPR skills; VO training might allow for greater scalability and dissemination, but with a potential reduction in CC depth.
Clinical Trial Registration
URL: ClinicalTrials.gov, Identifier: NCT01514656.
Keywords: Cardiopulmonary resuscitation, resuscitation, heart arrest, cardiovascular diseases
Prompt delivery of cardiopulmonary resuscitation (CPR) increases the probability of survival from sudden cardiac arrest (SCA) by 2–3 fold, yet over 60% of SCA victims in the U.S. do not receive bystander CPR.1–4 Despite the availability of CPR certification programs for the lay public, a recent investigation documented that training rates in the U.S. are strikingly low.5 Given that over 75% of SCA events occur in the home environment, training family members of at-risk cardiac patients could have a significant impact on initial care and survival from SCA, which leads to over 200,000 out-of-hospital deaths each year in the US.4,6–8 Highlighting the public health burden of SCA, the Institute of Medicine recently published a report entitled “Strategies to Improve Cardiac Arrest Survival: A Time to Act” that includes a call for increased engagement of the lay public as SCA first responders.9
A number of key barriers are inherent in the prevailing approach to layperson CPR training; these include the need for CPR-certified instructors, logistical constraints (such as course duration and costs), and low motivation for CPR training among the general public.10,11 Recent investigations have evaluated methods to disseminate CPR education that are simpler, less costly and more expedient. These approaches have included the use of “hands-only” CPR (chest compressions with no rescue breaths), video self-instruction (VSI) kits, and highly abbreviated training programs.12–18 The minimum training curriculum that reduces training barriers and provides adequate long-term CPR skill retention is unknown.
To address this knowledge gap, we conducted a multicenter pragmatic randomized trial of two educational strategies for CPR training of the lay public. Family members of hospitalized cardiac patients were offered either standard training via a kit that included a video along with an inflatable manikin (VSI), or video-only training without a manikin for psychomotor practice (VO). We hypothesized that trained laypersons who receive VO training would perform chest compressions (CC) six months post training, at a rate that is non-inferior to those who trained using a VSI kit. As a secondary outcome, we assessed the mean difference in CC depth between cohorts. If a VO CPR strategy yielded similar long-term skill retention, it would have important implications for dissemination to millions of potential layperson trainees worldwide.
Methods
Study population and setting
The CHIP (CPR Hospital-Initiated Project) trial was conducted on the inpatient wards at eight acute care hospitals in the southeastern Pennsylvania region (Hospital of the University of Pennsylvania, Penn Presbyterian Medical Center, Pennsylvania Hospital, Crozer-Chester Medical Center, Albert Einstein Medical Center Philadelphia, Temple University Hospital, Chester County Hospital, and Taylor Hospital). Adult family members of patients hospitalized with coronary disease on cardiology service line wards, telemetry or observation units were eligible for participation. The trial was conducted between February 2012 and May 2015.
This investigation was approved by the relevant Institutional Review Boards at each study site (University of Pennsylvania and Health System (includes three study sites), Crozer-Keystone Health System (includes two sites), Albert Einstein Healthcare Network, Temple University, and the Chester County Hospital) and was registered with the national clinical trials registry (NCT01514656, ClinicalTrials.gov, National Institutes of Health). Enrollment was conducted following written informed consent.
Study design
This study was structured as a pragmatic, randomized trial assessing the comparability of training individuals in CPR with VO (no manikin) to training with a VSI kit (manikin). Hospitals were randomized to sequential six month periods of training with either VSI or VO. To account for secular trends, the randomization scheme ensured that across all hospitals, the number of subjects receiving VO or VSI training at any point in time was similar.
Subject recruitment
Subjects were enrolled from February 2012 to December 2014 and underwent quantitative CPR skills assessment six months after the hospital-based training. Volunteer enrollers (registered nurses and students in the health sciences) at each study site offered video CPR instruction to family members of hospitalized patients; this pragmatic approach was used to assess generalizability for future broad implementation. Prior to participation in the study, the volunteer enrollers completed a one-hour training session led by study investigators. A reference manual containing training and study information was provided and study investigators were available on a daily basis for real-time enrollment-related questions. Details of the training process and volunteer recruitment are described in a recent publication.19 Subjects were eligible for enrollment if they met the following criteria: 1) the family member was physically present with the patient on the floor or unit; 2) the patient had an admission diagnosis potentially related to underlying coronary disease; 3) the patient was in stable condition; 4) the family member was 18 years of age or older; 5) the family member felt fit and able to perform moderate physical activity at the time of enrollment; and 6) the family member had sufficient English competency. Eligible family members who satisfied the inclusion criteria were enrolled using a standard written informed consent form, and completed a pre-training demographic survey.
CPR training intervention
We utilized a validated video training program and VSI kit (CPR Anytime for Family and Friends, American Heart Association (AHA), Dallas, Texas, and Laerdal Medical, Stavanger, Norway), described in previous investigations.20–21 In accordance with the 2010 AHA resuscitation guidelines, both study arms used hands-only CPR as the mode of instruction (CC without accompanying ventilations). The control group received a VSI kit that included an inflatable head/torso manikin and a 22-minute instructional DVD. The experimental video only (VO) group received a training video on DVD (no manikin). The DVD instruction was based on consensus CC goals of greater than 100 cpm and CC depth of greater than 50 mm. Following the training session, subjects completed a post-training survey designed to assess their comfort with the training process. Per trial protocol, volunteer registered nurses and students facilitated the family member training process, but refrained from coaching or teaching the subjects during training sessions.
Post-training assessment
Six months post-training, subjects were contacted and asked to complete a brief in-person interview where subjects’ perspectives on the training experience and perceived self-efficacy on performing CPR were captured. Subjects that lived greater than two hours away from the University of Pennsylvania were excluded from follow-up. Upon completion of the in-person interview, the subject was asked to perform a two-minute CPR skills assessment (skills test) using a CPR-recording manikin (SkillReporter ResusciAnne, Laerdal Medical, Stavanger Norway). The manikins were designed and calibrated to require consistent force to compress 50 mm. After approximately 25,000 compressions, the manikins were sent to the manufacturer for calibration testing to confirm ongoing consistency. Data from the CPR skills test were extracted from the recording software and imported into the study database for subsequent quantitative analysis.
Leading up to the six month skills assessment, the subject was not notified beforehand that they were being asked to perform a skills check (i.e. the skills test was a “surprise”), minimizing the likelihood that the subject would practice CPR skills immediately prior to the home visit. This surprise approach has been used in prior layperson resuscitation educational trials.22 Subjects who fulfilled the in-person interview were given $50 compensation.
Statistical approach and analysis
All demographic and CPR data were compiled in a secure, internet-based database application (REDCap Software Version 5.2.1, Vanderbilt University, Nashville, TN) and analyzed using statistical software packages (Stata 13, Statacorp, College Station, TX, and R version 3.3.0 with the ggplot2 package, The R Foundation for Statistical Computing, Vienna, Austria).
While our volunteer enrollers offered training to all family members interested in the study, our primary analysis included a single individual trainee per family. For families with more than one enrolled subject (the minority of enrollment instances), we randomly selected one individual per family to include in the primary analysis. The distribution of the data was visualized using a histogram, and smoothed using a kernel density estimator. Demographic data were compared between VO and VSI cohorts using a Pearson’s chi-squared test, as appropriate for categorical variables and a Student’s t-test for continuous variables. The primary analysis used a t-statistic to test the null hypothesis that mean CC rate in the VO group was more than 8 cpm lower than the CC rate in the VSI group. Non-inferiority was concluded based on a rejection of the null hypothesis. With a target sample size of 500, a Type I error rate of 0.05 and a projected standard deviation of 18 cpm, based on previous work,23–24 the study had 80% power to declare non-inferiority if VSI and VO differed by less than a mean of 3.5 cpm and 90% power to declare non-inferiority if VSI and VO differed by less than a mean of 2.8 cpm. With this sample size, the width of the 90% CI for mean CC rate was anticipated to be 2.6 cpm.
CC depth was considered a secondary outcome and in this case we tested the null hypothesis that the two approaches yielded indistinguishable mean depth at six months. This analysis used a 95% confidence interval.
The primary analysis was conducted with the subjects who agreed to a six month skills test. In a sensitivity analysis, we used inverse probability weighting (IPW) in the context of a linear model to estimate the mean differences in CPR skills. The propensity score for the likelihood of completing the six month follow-up included the following covariates: age, race, gender, highest education, previous training, number of subjects in a family, enrollment site, method of training, and method of training as an interaction with race, gender, age, and site. Between-group differences among those who agreed to follow-up and those who did not in baseline covariates before and after IPW were assessed to ensure that the propensity score was successful in achieving balance among the two groups. For individuals who were missing baseline covariates (<4% of all subjects), we imputed the value of each of these covariates using a simple means model for continuous variables or mode for categorical variables. The final IPW model included site as a fixed effect and was weighted by the propensity for completing the six month skills test.
Lastly, since the distribution of the original CC rate data appeared somewhat skewed, we assessed the differences in CC rate using a propensity-weighted over-dispersed Poisson model.
Results
Subject demographics
From February 2012 to December 2014, 1464 subjects were enrolled at eight hospitals; an additional 146 family members received CPR training but were not included in the primary analysis. Characteristics of the cohort at initial enrollment and six month follow-up appear in Table 1. The mean age of initial enrollees was 52±14 years, and 1083/1442 (75%) were female. Of those initially enrolled, 1037/1456 (71%) had either never been trained in CPR or had been trained more than 10 years ago and 1163/1441 (81%) were spouses or immediate family members of the hospitalized patient. Recruitment of subjects across hospitals differed (p=0.01), with sites A and B recruiting over 310 subjects each compared to sites C through H where fewer than 230 subjects were recruited.
Table 1.
Demographics of subjects who initially enrolled and who completed the six months skills assessment and were included in the final analysis.
| Initial enrollment | Six month skills assessment | |||||
|---|---|---|---|---|---|---|
| VO (n=695) | VSI (n=769) | p-value | VO (n=237) | VSI (n=285) | p-value | |
| Age, mean±(SD) | 52 ±14 | 52 ±14 | 0.68 | 52 ±14 | 52 ±14 | 0.89 |
| Race, n(%) | ||||||
| White | 402 (59) | 419 (55) | 0.33 | 131 (56) | 154 (55) | 0.79 |
| Black | 224 (33) | 270 (35) | 88 (38) | 109 (38) | ||
| Other | 60 (8) | 76 (10) | 14 (6) | 21 (7) | ||
| Gender, n(%) | ||||||
| Female | 499 (73) | 562 (74) | 0.94 | 174 (75) | 215(75) | 0.84 |
| Male | 180 (27) | 201 (26) | 59 (25) | 70 (25) | ||
| Relationship, n(%) | ||||||
| Spouse | 241 (35) | 264 (35) | 0.41 | 89 (38) | 103(37) | 0.90 |
| Immediate Family | 320 (47) | 338 (45) | 102 (43) | 122 (43) | ||
| Other | 122 (18) | 156 (20) | 44 (19) | 57 (20) | ||
| Education, n(%) | ||||||
| High School | 253 (37) | 296 (39) | 0.81 | 77 (32) | 101(35) | 0.41 |
| Some College | 163 (24) | 183 (24) | 54 (23) | 76 (27) | ||
| College | 185 (27) | 190 (25) | 70 (30) | 67 (24) | ||
| Graduate School | 86 (12) | 97 (12) | 35 (15) | 41 (14) | ||
| Previous Training, n(%) | ||||||
| Never | 330 (48) | 399 (52) | 0.13 | 109 (46) | 135 (48) | 0.20 |
| <2 years | 53 (8) | 54 (7) | 16 (7) | 30 (11) | ||
| 2–5 years | 98 (14) | 77 (10) | 35 (15) | 29 (10) | ||
| 6–10 years | 68 (10) | 69 (9) | 29 (12) | 26 (9) | ||
| >10 years | 143 (20) | 165 (22) | 47 (20) | 64 (22) | ||
| Location of Training, n(%) | ||||||
| A | 193 (28) | 194 (25) | 0.01 | 59 (25) | 58 (20) | 0.01 |
| B | 149 (21) | 170 (22) | 60 (25) | 75 (26) | ||
| C | 95 (14) | 83 (11) | 30 (12) | 31 (11) | ||
| D | 64 (9) | 54 (7) | 23 (10) | 16 (6) | ||
| E | 118 (17) | 117 (15) | 40 (17) | 38 (13) | ||
| F | 20 (3) | 45 (6) | 7 (3) | 19 (7) | ||
| G | 42 (6) | 83 (11) | 16 (7) | 40 (14) | ||
| H | 11(2) | 23 (3) | 2 (1) | 8 (3) | ||
Hospitals: A=Hospital of the University of Pennsylvania, B=Penn Presbyterian Medical Center, C=Pennsylvania Hospital, D=Crozer-Chester Medical Center, E=Einstein Medical Center Philadelphia, F=Temple University Hospital, G=Chester County Hospital, H=Taylor Hospital; Initial Missing Variables: Age – 60, Race-13, Gender-22, Relationship-23, Education-11, Previous Training-8; Missing variables from the skills assessment cohort: Age-13, Race-5, Gender-4, Relationship-5, Education-1, Previous Training-2. P-values represent a t-test for continuous variables and a chi-squared test for categorical variables. VO, video-only; VSI, video self-instruction.
As shown in Figure 1, 230 subjects were not eligible for in-person follow-up because they lived greater than two hours driving distance from the research institution or the patient or subject was deceased, while 533 could not be contacted or declined participation. From the initial enrollment cohort, 522 (36%) subjects completed a six-month follow-up interview and CPR skills testing. Among the 522 subjects, 285 (54%) received VSI training while 237 (46%) received VO training. Of those who did not complete a six month skills assessment, 44 subjects underwent the in-person interview process but declined skills testing. Excluding those not eligible for follow-up because of distance, the skills assessment follow-up rate was 522/1234 (42%).
Figure 1.
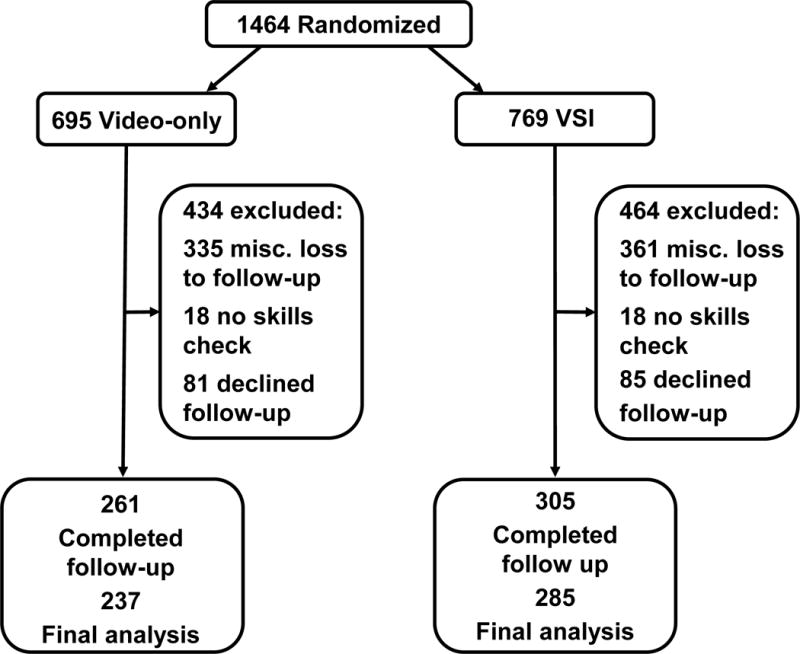
Consort diagram of the pragmatic clinical trial randomization and subsequent subject follow-up.
We examined the demographics of those who completed skills assessments compared to those who did not; race was associated with follow-up, with blacks being more likely to complete follow-up (p<0.01). Location of initial training was also significantly associated with follow-up (p=0.01), but age, gender, relationship to the patient, educational level or prior CPR training were not (see Table 2).
Table 2.
Characteristics of subjects who did and did not complete the six months skills assessment
| Did not complete the assessment (n=942) |
Six month skills assessment (n=522) |
p-value | |
|---|---|---|---|
| Age, mean±(SD) | 51±15 | 52±14 | 0.60 |
| Race, n(%) | |||
| White | 536 (57) | 285 (55) | <0.01 |
| Black | 297 (32) | 197 (38) | |
| Other | 101 (11) | 35 (7) | |
| Gender, n(%) | |||
| Female | 672 (73) | 389 (75) | 0.33 |
| Male | 252 (27) | 129 (25) | |
| Relationship, n(%) | |||
| Spouse | 313 (34) | 192 (37) | 0.37 |
| Immediate Family | 434 (47) | 224 (43) | |
| Other | 177 (19) | 101 (20) | |
| Education, n(%) | |||
| High School | 371 (40) | 178 (34) | 0.12 |
| Some College | 217 (23) | 129 (25) | |
| College | 237 (25) | 138 (26) | |
| Graduate School | 107 (12) | 76 (15) | |
| Previous Training, n(%) | |||
| Never | 486 (52) | 243 (47) | 0.23 |
| <2 years | 61 (6) | 46 (9) | |
| 2–5 years | 110 (12) | 65 (12) | |
| 6–10 years | 82 (9) | 55 (11) | |
| >10 years | 197 (21) | 111 (21) | |
| Hospital, n(%) | |||
| A | 272 (29) | 118 (23) | 0.01 |
| B | 184 (20) | 135 (26) | |
| C | 118 (12) | 60 (11) | |
| D | 79 (8) | 39 (7) | |
| E | 157 (17) | 78 (15) | |
| F | 39 (4) | 26 (5) | |
| G | 69 (7) | 56 (11) | |
| H | 24 (3) | 10 (2) | |
| Mode of teaching, n(%) | |||
| VSI Kit | 458 (49) | 237 (45) | 0.24 |
| Video-only | 484 (51) | 285 (55) |
Hospitals: A=Hospital of the University of Pennsylvania, B=Penn Presbyterian Medical Center, C=Pennsylvania Hospital, D=Crozer-Chester Medical Center, E=Einstein Medical Center Philadelphia, F=Temple University Hospital, G=Chester County Hospital, H=Taylor Hospital; VSI Kit=Video self-instruction kit; Missing variables: Age-47, Race-13, Gender-22, Relationship-23, Education-11, Previous Training-12; p-values represent a t-test for continuous variables and a chi-squared test for categorical variables.
CPR skills: CC rate and depth
The distribution of CC rate (A) and depth (B) appears in Figure 2. For both training groups, CC rate was skewed right while CC depth was skewed left. Among subjects who completed the 6-month skills assessment, mean CC rate in the VO cohort was 87.7 (90% CI: 85.1, 90.4) cpm and 89.3 (90% CI: 86.8, 91.8) cpm in the VSI cohort. The mean rate difference between cohorts was −1.6 (90% CI: −5.2, 2.1) cpm, well under the pre-defined 8 cpm threshold for non-inferiority; therefore these findings are consistent with non-inferiority at the 5% significance level.
Figure 2.
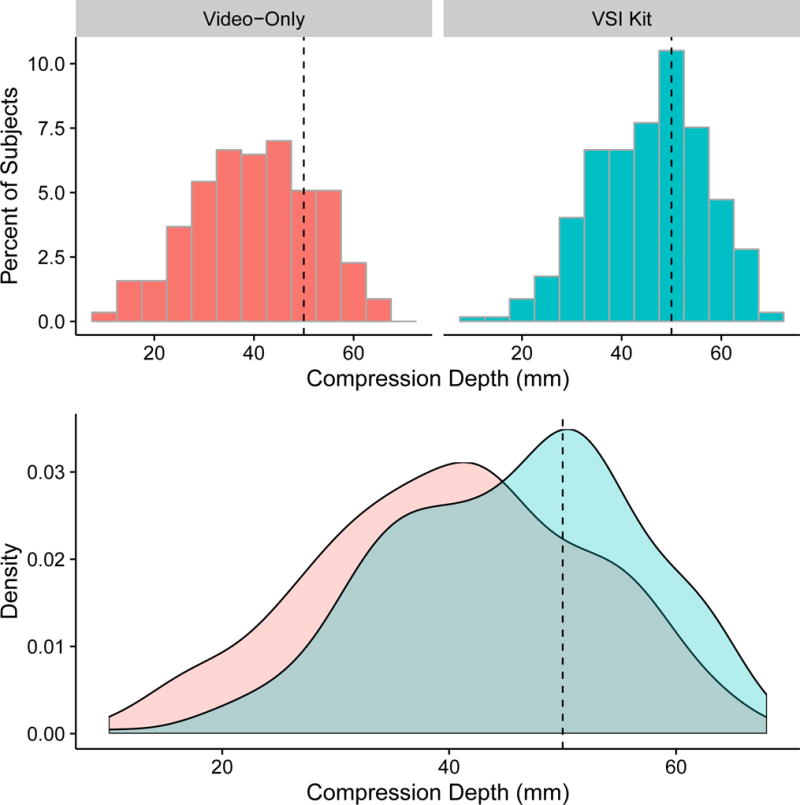
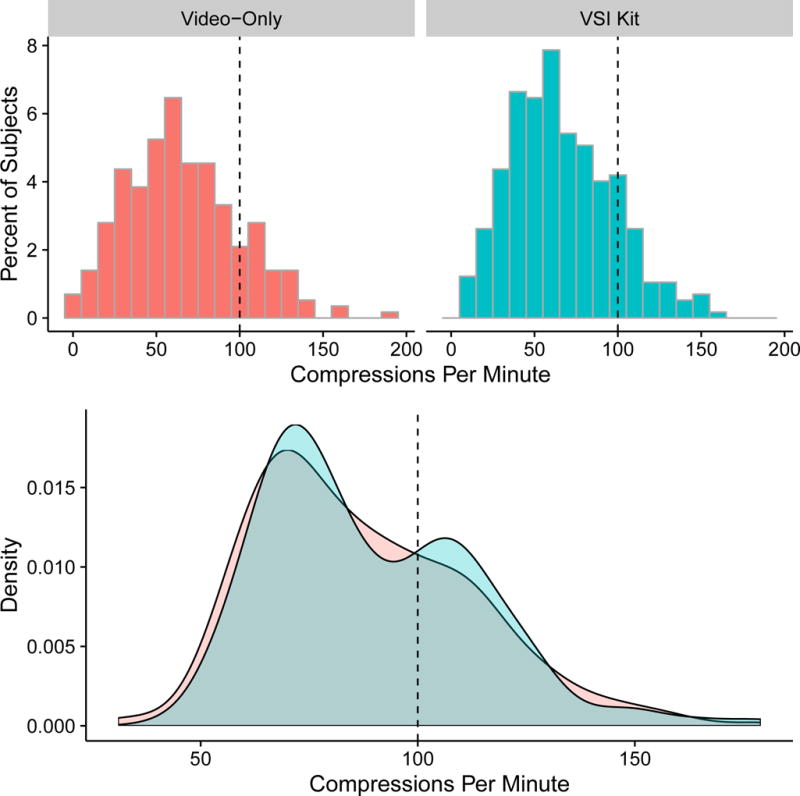
Histograms of A) chest compression rate and B) depth in VO and VSI stratified by training group. Vertical dashed lines show target rates of 100 compressions per minute and 50 mm respectively. The lower panel in each frame conveys the data from the two histograms overlaid, and smoothed with a kernel density estimator
The mean CC depth was 40.2 (95% CI: 38.7, 41.7) mm in the VO cohort and 45.8 (95% CI: 44.5, 47.1) mm in the VSI cohort (see Table 3). The mean depth was −5.6 (95% CI: −7.6, −3.7) mm shallower among the VO cohort, a difference that was statistically significant at the 5% significance level.
Table 3.
CC rate and depth in the two training cohorts.
| Cohort | Mean Difference | |||
|---|---|---|---|---|
| VO (n=237) | VSI (n=285) | Difference | Adjusted Difference* | |
| CC Rate (n/min) | 87.7 (85.1, 90.4) | 89.3 (86.8, 91.8) | −1.6 (−5.2, 2.1) | −1.9 (−5.6, 1.8) |
| CC Depth (mm) | 40.2 (38.7, 41.7) | 45.8 (44.5, 47.1) | −5.6 (−7.6, −3.7) | −5.2 (−7.4, −3.1) |
Values shown are means.
Inverse probability weighting propensity score adjusted with all of the demographic variables in Table 1. CC, chest compressions; VO, video-only; VSI, video self-instruction; Rate: Mean and 90% confidence interval; Depth: Mean and 95% confidence interval. Significance for both is established at the 5% significance threshold.
After using inverse probability weighting to adjust for loss to follow-up, the difference in both mean CC rate and depth was not significantly altered. Our main findings were also confirmed with an IPW, over-dispersed Poisson model (results not shown).
Discussion
In a pragmatic randomized multicenter trial of family CPR education, we assessed quantitative measures of CPR skill retention six months following training with either a standard VSI kit or VO education, without the use of a manikin for psychomotor practice. CC rate for the two cohorts demonstrated non-inferiority of the VO training approach, with mean CC rate difference of less than 2 cpm, and an upper bound on the difference of 5.2 cpm. By contrast, the difference in mean CC depth was 5.6 mm, with an upper bound (95% CI) of 7.6 mm. These results suggest that psychomotor practice with a manikin improves layperson CC depth during long-term skills assessment. To our knowledge, this represents the largest prospective trial of CPR training and long-term retention among lay providers. Findings from this investigation have important implications for future policy and education initiatives to improve layperson CPR, as VO training could be broadly disseminated at low cost.
A recent epidemiologic study demonstrated low CPR training incidence in the U.S., likely contributing to low bystander CPR delivery rates in most communities.5 Prior work has suggested that numerous barriers, including training access and logistics, have hampered public access to CPR training.10,11 To address these challenges, the AHA developed a low-cost approach to CPR education that relies upon video-facilitated learning in the form of a self-contained VSI kit. The promise for broad implementation using these kits has been demonstrated in a number of large-scale training experiences, yet public uptake of the VSI kits has been variable, and kit costs may still be prohibitive for large-scale training of the U.S. public.20 Other work has suggested that barriers to training might be further reduced by brief VO training, eschewing the use of training kits altogether, and adding to the potential for greater scalability of CPR education.18 It has been generally believed that psychomotor practice of CPR skills during training represents a crucial factor in long-term skill retention, although this hypothesis had never been prospectively tested in a randomized trial. Our work suggests that psychomotor practice may yield small benefits with regard to retention of adequate CC depth, but these differences in depth may be small compared to the enormous dissemination potential inherent in VO education. That is, our work highlights a public health “trade off” between somewhat better CPR skills or a tool with much broader implementation potential. Further work will be required to model this trade-off, and to determine whether training a greater proportion of the population would result in more lives saved compared to our current paradigm, that appears to yield somewhat higher CPR quality among a smaller population of trained individuals.
Our work also demonstrates an important CPR training opportunity that has been largely untapped, namely, hospital-based CPR education of the families of cardiac patients before discharge. Over one million people in the U.S. are admitted for acute coronary syndromes and myocardial infarction annually, yet no system exists to offer CPR training to spouses or other family members during the “point of capture” opportunity afforded by hospital admission.14 This gap is especially relevant given that patients with coronary events have a much higher annual risk of subsequent cardiac arrest than the general population.25,26 Estimates of annual SCA incidence in this population range from 3–11%, compared to the overall cardiac arrest annual incidence in the U.S. of approximately 0.1%.27–32 Since over 70% of arrest events occur in private residences, survival is dependent on the prompt action of spouses and other family members to deliver CPR until pre-hospital personnel arrive on scene.33–35 Our prior work has shown that CPR training is well-received by families, who reported satisfaction using the hospital-environment to offer such education before discharge.14
Other venues for CPR education could become feasible through VO education, such as in clinic waiting rooms, public locations such as motor vehicle licensing facilities, or in transit system locations such as train stations or airports. Additionally, VO training may allow for other methods of dissemination that remove the need for appropriate environmental settings. For example, the video curriculum could be incorporated into a mobile application for dissemination via mobile technology, or integrated into video education programs on television channels. Additionally, the video could be disseminated through the internet or various social media platforms.
When comparing the CPR skill retention within the two study cohorts, mean CC rate were almost identical, and yet CC depth was deeper in the VSI cohort (difference of 5.6 mm). While current studies examining CC rates and depths from in and out of hospital providers demonstrate poor CPR quality, few studies have gathered data from actual layperson CPR performance. When comparing our findings to that of clinical studies of CPR performance, our VO cohort’s mean CC depth was similar to that of CC depth as delivered during clinical care.23,36 Specifically, the CPR performance in our cohort was remarkably similar to actual professional CPR performance during clinical care (mean depth in one pre-hospital cohort was 42 mm compared to 40 mm in our VO cohort).36
While VSI training may yield improved psychomotor retention, VO training may afford cost savings and broad dissemination potential. Given the large effect size inherent in the delivery of bystander CPR, and the presumably increased likelihood that a layperson will perform CPR if trained in these skills, our work suggests that VO training may be a useful method to ensure a basic CPR competency to a broad swath of the public who might otherwise remain untrained.
A number of limitations are important to note regarding our investigation. Given our pragmatic design to test a low-cost generalizable approach to hospital-based CPR training, we did not embed research staff and CPR testing equipment at each training site. Thus, we did not test CPR skills at baseline immediately after training and could not compare these skills to the subsequent skills assessment at six months. It is therefore unknown whether shallow CC depths at six months represented skill deterioration or initial CPR quality with VO training. The work of Stiell et al has shown that inadequate CC depth is pervasive during CPR provision by pre-hospital professionals during actual cardiac arrest resuscitation; shallow depth performance in our cohort may be consistent with the physical limitations of CPR delivery.23,36 Another limitation of our work was the lack of clinical outcomes from any actual SCA events among the hospitalized patient cohort. Assuming a 5% annual incidence arrest rate among high-risk cardiac patients after hospital discharge, it is possible that 20–30 arrest events occurred among the families who received training in our study. While cardiac arrest events and successful resuscitations were reported by families to our team at follow-up, we did not design our work to allow verification of these reports by clinical pre-hospital records, nor would such verification have adequate statistical power to detect differences in the two arms. Further, the study was powered to detect non-inferiority in CC rate, but not CC depth.
Questions about generalizability also arise in our study due to the large loss to follow-up. Our study was powered to detect non-inferiority in CC rate for a sample size of 500 evaluable subjects. Despite the loss to follow-up, baseline characteristics of the original cohort and those evaluated at six months were reasonably similar. Using inverse-probability weighting to account for the missing data yielded very similar conclusions to using only complete cases. This sensitivity analysis suggests that our work has reasonable generalizability to the population of interest, specifically family members of patients hospitalized with a cardiac diagnosis, who agree to volunteer-initiated CPR training.
The enormous promise inherent in VO education will require further work to test implementation models. Whether VO training could be embedded into modern communication tools such as mobile tablets, smartphones or other delivery approaches, remains to be assessed in clinical investigations. Recent investigations have demonstrated the potential promise of using smartphone apps in the domain of SCA.37 The appropriate timing of CPR training for families before discharge, and the optimal model for staff proctoring of such training, also requires further study.
Conclusions
VO training yielded statistically indistinguishable CC rates and somewhat shallower CC depths compared to those trained with a VSI kit. If appropriate practical questions are further addressed, offering VO CPR training to families before hospital discharge could become a routine patient and family-centered health educational opportunity in over 4,000 acute care hospitals that care for cardiac patients in the U.S.38 If implemented broadly, CPR education could be well-matched to a large population at high risk of subsequent cardiac arrest, establishing an opportunity to make important gains in survival from cardiac arrest. Furthermore, being able to train individuals with VO may allow for broader, more scalable dissemination of CPR training to the lay public; however, shallower CC depth at six month suggests additional work to optimize VO strategies may be required.
Supplementary Material
What is known?
Bystander cardiopulmonary resuscitation (CPR) improves survival from sudden cardiac arrest, yet rates are low in many US communities.
Studies have suggested that simplified methods for CPR training may promote broader dissemination and increase bystander delivery rates, but the minimum CPR training curriculum to encourage broad implementation and to ensure long-term retention remains poorly understood.
What the study adds?
We have conducted the first large, prospective cluster randomized trial examining the effectiveness and long-term retention of lay bystanders trained with video-only education compared to video-self instruction paired with inflatable manikins.
Video-only training yielded a statistically indistinguishable difference in chest compression rate compared to video self-instruction training at six months post-training, while compression depth was more shallow at six months post-training.
When considering CPR education modalities, the current investigation presents a possible tradeoff; specifically, video-only training may confer broader dissemination potential at low cost with non-inferior chest compression rate, while manikin-based instruction may result in somewhat better CPR skill performance at higher cost (and possibly less broad dissemination).
Acknowledgments
We would like to thank the nurse and student volunteers at the Hospital of the University of Pennsylvania, Penn Presbyterian Medical Center, Pennsylvania Hospital, Crozer-Chester Medical Center, Taylor Hospital, Temple University Hospital, Albert Einstein Medical Center Philadelphia, and The Chester County Hospital. Additionally, we would like to thank Daniel Ikeda for his assistance with editing the manuscript, and the reviewers for their careful review and excellent suggestions.
Funding Sources: This work was supported by grants from the National Institutes of Health (R18HL107217) and the American Heart Association (Clinical Research Program award).
Appendix
This work is submitted on behalf of the CHIP (CPR Hospital-Initiated Project Study Group):
University of Arizona, Sarver Heart Center
Bentley J. Bobrow, MD
Einstein Medical Center Philadelphia
Kenneth Deitch, DO, FACEP
Kathia Damiron, MD
Penn Presbyterian Medical Center
James Kurtz, MPH, BSN, RN
Ryan Dos Reis, BSN, RN
The Chester County Hospital
Donna Taylor, BSN, RN
Janice Baker, MSN, RN
Shannon Delany, MSN, RN
Footnotes
Journal Subject Terms: Cardiopulmonary Arrest; Cardiopulmonary Resuscitation and Emergency Cardiac Care
Conflict of Interst Disclosures: Ms. Blewer has received research funding from the American Heart Association. Ms. Leary serves on the advisory committee of the American Heart Association’s Emergency Cardiovascular Care committee, and has research funding from the American Heart Association and the Laerdal Foundation. Dr. Abella has received research funding from Medtronic Foundation, the American Heart Association, PCORI and the NIH, research funding and honoraria from CR Bard, honoraria from Physio-Control, and in-kind research support from Laerdal Medical Corporation. The other authors report no relevant conflicts of interest.
References
- 1.Hasselgvist-Ax I, Riva G, Herlitz J, Rosenqvist M, Hollenberg J, Nordberg P, Ringh M, Jonsson M, Axelsson C, Lindqvist J, Karlsson T, Svensson L. Early cardiopulmonary resuscitation in out-of-hospital cardiac arrest. New Engl J Med. 2015;372:2307–2315. doi: 10.1056/NEJMoa1405796. [DOI] [PubMed] [Google Scholar]
- 2.Iwami T, Kawamura T, Hiraide A, Berg RA, Hayashi Y, Nishiuchi T, Kajino K, Yonemoto N, Yukioka H, Sugimoto H, Kakuchi H, Sase K, Yokoyama H, Nonogi H. Effectiveness of bystander-initiated cardiac-only resuscitation for patients with out-of-hospital cardiac arrest. Circulation. 2007;116:2900–2907. doi: 10.1161/CIRCULATIONAHA.107.723411. [DOI] [PubMed] [Google Scholar]
- 3.Chan PS, McNally B, Tang F, Kellermann A, CARES Surveillance Group Recent trends in survival from out-of-hospital cardiac arrest in the United States. Circulation. 2014;130:1876–1882. doi: 10.1161/CIRCULATIONAHA.114.009711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sasson C, Rogers MA, Dahl J, Kellermann AL. Predictors of survival from out-of-hospital cardiac arrest: a systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes. 2010;3:63–81. doi: 10.1161/CIRCOUTCOMES.109.889576. [DOI] [PubMed] [Google Scholar]
- 5.Anderson ML, Cox M, Al-Khatib SM, Nichol G, Thomas KL, Chan PS, Saha-Chaudhuri P, Fosbol EL, Eigel B, Clendenen B, Peterson ED. Rates of cardiopulmonary resuscitation training in the United States. JAMA Intern Med. 2014;174:194–201. doi: 10.1001/jamainternmed.2013.11320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nichol G, Thomas E, Callaway CW, Hedges J, Powell JL, Aufderheide TP, Rea T, Lowe R, Brown T, Dreyer J, Davis D, Idris A, Stiell I, Resuscitation Outcomes Consortium Investigators Regional variation in out-of-hospital cardiac arrest incidence and outcome. JAMA. 2008;300:1423–1431. doi: 10.1001/jama.300.12.1423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, de Ferranti S, Despres JP, Fullerton HJ, Howard VJ, Huffman MD, Judd SE, Kissela BM, Lackland DT, Lichtman JH, Lisabeth LD, Liu S, Mackey RH, Matchar DB, McGuire DK, Mohler ER, 3rd, Moy CS, Muntner P, Mussolino ME, Nasir K, Neumar RW, Nichol G, Palaniappan L, Pandey DK, Reeves MJ, Rodriquez CJ, Sorlie PD, Stein J, Towfighi A, Turan TN, Virani SS, Willey JZ, Woo D, Yeh RW, Turner MB, American Heart Association Statistics Committee and Stroke Statistics Subcommittee Heart disease and stroke statistics–2015 update: a report from the American Heart Association. Circulation. 2015;131:e29–e322. doi: 10.1161/CIR.0000000000000152. [DOI] [PubMed] [Google Scholar]
- 8.Zive D, Koprowicz K, Schmidt T, Stiell I, Sears G, Van Ottingham L, Idris A, Stephens S, Daya M, Resuscitation Outcomes Consortium Investigators Variation in out-of-hospital cardiac arrest resuscitation and transport practices in the Resuscitation Outcomes Consortium: ROC Epistry-Cardiac Arrest. Resuscitation. 2011;82:277–284. doi: 10.1016/j.resuscitation.2010.10.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Institute of Medicine. Strategies to Improve Cardiac Arrest Survival: A Time to Act Directions. Available at: http://iom.nationalacademies.org/~/media/Files/CardiacArrestReportBrief.pdf. Accessed July 6, 2015.
- 10.Abella BS, Aufderheide TP, Eigel B, Hickey RW, Longstreth WT, Jr, Nadkarni V, Nichol G, Sayre MR, Sommargren CE, Hazinski MF, American Heart Association Reducing barriers for implementation of bystander-initiated cardiopulmonary resuscitation: a scientific statement from the American Heart Association for healthcare providers, policymakers, and community leaders regarding the effectiveness of cardiopulmonary resuscitation. Circulation. 2008;117:704–709. doi: 10.1161/CIRCULATIONAHA.107.188486. [DOI] [PubMed] [Google Scholar]
- 11.Vaillancourt C, Stiell IG, Wells GA. Understanding and improving low bystander CPR rates: a systematic review of the literature. CJEM. 2008;10:51–65. doi: 10.1017/s1481803500010010. [DOI] [PubMed] [Google Scholar]
- 12.Sayre MR, Berg RA, Cave DM, Page RL, Potts J, White RD, American Heart Association Emergency Cardiovascular Care Committee Hands-only (compression-only) cardiopulmonary resuscitation: a call to action for bystander response to adults who experience out-of-hospital sudden cardiac arrest: a science advisory for the public from the American Heart Association Emergency Cardiovascular Care Committee. Circulation. 2008;117:2162–2167. doi: 10.1161/CIRCULATIONAHA.107.189380. [DOI] [PubMed] [Google Scholar]
- 13.Blewer AL, Leary M, Esposito EC, Gonzalez M, Riegel B, Bobrow BJ, Abella BS. Continuous chest compression cardiopulmonary resuscitation training promotes rescuer self-confidence and increased secondary training: a hospital-based randomized controlled trial*. Crit Care Med. 2012;40:787–792. doi: 10.1097/CCM.0b013e318236f2ca. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Blewer AL, Leary M, Decker CS, Andersen JC, Fredericks AC, Bobrow BJ, Abella BS. Cardiopulmonary resuscitation training of family members before hospital discharge using video self-instruction: a feasibility trial. J Hosp Med. 2011;6:428–432. doi: 10.1002/jhm.847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Panchal AR, Meziab O, Stolz U, Anderson W, Bartlett M, Spaite DW, Bobrow BJ, Kern KB. The impact of ultra-brief chest compression-only CPR video training on responsiveness, compression rate, and hands off time interval among bystanders in a shopping mall. Resuscitation. 2014;85:1287–90. doi: 10.1016/j.resuscitation.2014.06.013. [DOI] [PubMed] [Google Scholar]
- 16.Roppolo LP, Pepe PE, Campbell L, Ohman K, Kulkarni H, Miller R, Idris A, Bean L, Bettes TN, Idris AH. Prospective, randomized trial of the effectiveness and retention of 30-min layperson training for cardiopulmonary resuscitation and automated external defibrillators: The American Airlines Study. Resuscitation. 2007;74:276–285. doi: 10.1016/j.resuscitation.2006.12.017. [DOI] [PubMed] [Google Scholar]
- 17.Lynch B, Einspruch EL, Nichol G, Becker LB, Aufderheide TP, Idris A. Effectiveness of a 30-min CPR self-instruction program for lay responders: a controlled randomized study. Resuscitation. 2005;67:31–43. doi: 10.1016/j.resuscitation.2005.04.017. [DOI] [PubMed] [Google Scholar]
- 18.Bobrow BJ, Vadeboncoeur TF, Spaite DW, Potts J, Denninghoff K, Chikani V, Brazil PR, Ramsey B, Abella BS. The effectiveness of ultrabrief and brief educational videos for training lay responders in hands-only cardiopulmonary resuscitation: implications for the future of citizen cardiopulmonary resuscitation training. Circ Cardiovasc Qual Outcomes. 2011;4:220–226. doi: 10.1161/CIRCOUTCOMES.110.959353. [DOI] [PubMed] [Google Scholar]
- 19.Blewer AL, Li J, Ikeda DJ, Leary M, Buckler DG, Riegel B, Desai S, Groeneveld PW, Putt ME, Abella BS. Recruitment for a hospital-based pragmatic clinical trial using volunteer nurses and students. Clinical Trials. 2016;13:425–433. doi: 10.1177/1740774516643265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Isbye DL, Rasmussen LS, Ringsted C, Lippert FK. Disseminating cardiopulmonary resuscitation training by distributing 35,000 personal manikins among school children. Circulation. 2007;116:1380–1385. doi: 10.1161/CIRCULATIONAHA.107.710616. [DOI] [PubMed] [Google Scholar]
- 21.Isbye DL, Meyhoff CS, Lippert FK, Rasmussen LS. Skill retention in adults and in children 3 months after basic life support training using a simple personal resuscitation manikin. Resuscitation. 2007;74:296–302. doi: 10.1016/j.resuscitation.2006.12.012. [DOI] [PubMed] [Google Scholar]
- 22.Donnelly P, Assar D, Lester C. A comparison of manikin CPR performance by lay persons trained in three variations of basic life support guidelines. Resuscitation. 2000;45:195–199. doi: 10.1016/s0300-9572(00)00186-6. [DOI] [PubMed] [Google Scholar]
- 23.Stiell IG, Brown SP, Christenson J, Cheskes S, Nichol G, Powell J, Bigham B, Morrison LJ, Larsen J, Hess E, Vaillancourt C, Davis DP, Callaway CW, Resuscitation Outcomes Consortium (ROC) Investigators What is the role of chest compression depth during out-of-hospital cardiac arrest resuscitation? Crit Care Med. 2012;40:1192–1198. doi: 10.1097/CCM.0b013e31823bc8bb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Idris AH, Guffey D, Aufderheide TP, Brown S, Morrison LJ, Nichols P, Powell J, Daya M, Bigham BL, Atkins DL, Berg R, Davis D, Stiell I, Sopko G, Nichol G, Resuscitation Outcomes Consortium (ROC) Investigators Relationship between chest compression rates and outcomes from cardiac arrest. Circulation. 2012;125:3004–3012. doi: 10.1161/CIRCULATIONAHA.111.059535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Deo R, Albert CM. Epidemiology and genetics of sudden cardiac death. Circulation. 2012;125:620–637. doi: 10.1161/CIRCULATIONAHA.111.023838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Myerburg RJ, Castellanos A. Emerging paradigms of the epidemiology and demographics of sudden cardiac arrest. Heart Rhythm. 2006;3:235–239. doi: 10.1016/j.hrthm.2005.09.023. [DOI] [PubMed] [Google Scholar]
- 27.Giraldez RR, Clare RM, Lopes RD, Dalby AJ, Prabhakaran D, Brogan GX, Jr, Giugliano RP, James SK, Tanguay JF, Pollack CV, Jr, Harrington RA, Braunwald E, Newby LK. Prevalence and clinical outcomes of undiagnosed diabetes mellitus and prediabetes among patients with high-risk non-ST-segment elevation acute coronary syndrome. Am Heart J. 2013;165:918–925.e2. doi: 10.1016/j.ahj.2013.01.005. [DOI] [PubMed] [Google Scholar]
- 28.Buber J, Goldenberg I, Kimron L, Guetta V. One-year outcome following coronary angiography in elderly patients with non-ST elevation myocardial infarction: real-world data from the Acute Coronary Syndromes Israeli Survey (ACSIS) Coron Artery Dis. 2013;24:102–109. doi: 10.1097/MCA.0b013e32835c8f53. [DOI] [PubMed] [Google Scholar]
- 29.Selker HP, Udelson JE, Massaro JM, Ruthazer R, D’Agostino RB, Griffith JL, Sheehan PR, Desvigne-Nickens P, Rosenberg Y, Tian X, Vickery EM, Atkins JM, Aufderheide TP, Sayah AJ, Pirrallo RG, Levy MK, Richards ME, Braude DA, Doyle DD, Frascone RJ, Kosiak DJ, Leaming JM, Van Gelder CM, Walter GP, Wayne MA, Woolard RH, Beshansky JR. One-year outcomes of out-of-hospital administration of intravenous glucose, insulin, and potassium (GIK) in patients with suspected acute coronary syndromes (from the IMMEDIATE [Immediate Myocardial Metabolic Enhancement During Initial Assessment and Treatment in Emergency Care] Trial) Am J Cardiol. 2014;113:1599–1605. doi: 10.1016/j.amjcard.2014.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Arbel Y, Matetzky S, Gavrielov-Yusim N, Shlezinger M, Keren G, Roth A, Kopel E, Finkelstein A, Banai S, Klempfner R, Goldenberg I. Temporal trends in all-cause mortality of smokers versus non-smokers hospitalized with ST-segment elevation myocardial infarction. Int J Cardiol. 2014;176:171–176. doi: 10.1016/j.ijcard.2014.07.010. [DOI] [PubMed] [Google Scholar]
- 31.Genereux P, Madhavan MV, Mintz GS, Maehara A, Palmerini T, Lasalle L, Xu K, McAndrew T, Kirtane A, Lansky AJ, Brener SJ, Mehran R, Stone GW. Ischemic outcomes after coronary intervention of calcified vessels in acute coronary syndromes. Pooled analysis from the HORIZONS-AMI (Harmonizing Outcomes With Revascularization and Stents in Acute Myocardial Infarction) and ACUITY (Acute Catheterization and Urgent Intervention Triage Strategy) TRIALS. J Am Coll Cardiol. 2014;63:1845–1854. doi: 10.1016/j.jacc.2014.01.034. [DOI] [PubMed] [Google Scholar]
- 32.Seronde MF, Geha R, Puymirat E, Chaib A, Simon T, Berard L, Drouet E, Bataille V, Danchin N, Schiele F. Discharge heart rate and mortality after acute myocardial infarction. Am J Med. 2014;127:954–962. doi: 10.1016/j.amjmed.2014.06.034. [DOI] [PubMed] [Google Scholar]
- 33.Nakanishi N, Nishizawa S, Kitamura Y, Nakamura T, Matsumuro A, Sawada T, Matsubara H. The increased mortality from witnessed out-of-hospital cardiac arrest in the home. Prehosp Emerg Care. 2011;15:271–277. doi: 10.3109/10903127.2010.545475. [DOI] [PubMed] [Google Scholar]
- 34.Lorem T, Steen PA, Wik L. High school students as ambassadors of CPR–a model for reaching the most appropriate target population? Resuscitation. 2010;81:78–81. doi: 10.1016/j.resuscitation.2009.09.030. [DOI] [PubMed] [Google Scholar]
- 35.Swor R, Fahoome G, Compton S. Potential impact of a targeted cardiopulmonary resuscitation program for older adults on survival from private-residence cardiac arrest. Acad Emerg Med. 2005;12:7–12. doi: 10.1197/j.aem.2004.08.041. [DOI] [PubMed] [Google Scholar]
- 36.Stiell IG, Brown SP, Nichol G, Cheskes S, Vaillancourt C, Callaway CW, Morrison LJ, Christenson J, Aufderheide TP, Davis DP, Free C, Hostler D, Stouffer JA, Idris AH, Resuscitation Outcomes Consortium Investigators What is the optimal chest compression depth during out-of-hospital cardiac arrest resuscitation of adult patients? Circulation. 2014;130:1962–1970. doi: 10.1161/CIRCULATIONAHA.114.008671. [DOI] [PubMed] [Google Scholar]
- 37.Ringh M, Rosenqvist M, Hollenberg J, Jonsson M, Fredman D, Nordberg P, Jarnbert-Pettersson H, Hasselqvist-Ax I, Riva G, Svensson L. Mobile-phone dispatch of laypersons for CPR in out-of-hospital cardiac arrest. N Engl J Med. 2015;372:2316–2325. doi: 10.1056/NEJMoa1406038. [DOI] [PubMed] [Google Scholar]
- 38.American Hospital Association. Fast Facts on US Hospitals. Available at: http://www.aha.org/research/rc/stat-studies/fast-facts.shtml. Accessed January 12, 2016.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


