Abstract
Background
Korean American women have among the lowest rates of cervical cancer screening in the United States (US). We evaluated a multi-component intervention combining community education with navigation services to reduce access barriers and increase screening rates in this underserved population. It was hypothesized that cervical cancer screening rates would be higher among women receiving the intervention program compared to women in the control program.
Methods
Korean American women (N=705) were recruited from 22 churches. Using a matched-pair, group-randomized design, 347 women received the intervention, which consisted of a culturally-relevant cancer education program combined with provision of navigation services. The control group (N=358) received general health education including information about cervical cancer risk and screening and where to obtain low- or no-cost screening. Screening behavior was assessed 12-months post-program.
Results
Screening behavior data were obtained from 588 women at 12-months post-program. In both site-level and participant-level analyses, the intervention program contributed to significantly higher screening rates than the control program (Odds Ratio [OR] = 25.9, 95% CI=10.1-66.1, p< 0.001). In sensitivity analysis, the treatment effect remained highly significant (OR = 16.7, 95% CI =8.1-34.4, p< 0.001).
Conclusion
A multi-component intervention combining community cancer education with navigation services yielded significant increases in cervical cancer screening rates among underscreened Korean American women. Community-accessible programs that incorporate cancer education with delivery of key navigation services can be highly effective in increasing cervical cancer screening rates in this underserved population.
Keywords: cervical cancer screening, CBPR, intervention, Korean American, navigation
Graphical Abstract
Condensed Abstract: Korean American women experience numerous access and linguistic barriers to cervical cancer screening and have one of the lowest rates of screening relative to other US subgroups. A multi-component, community-based intervention that combined cancer education with delivery of key navigation services was highly effective in increasing cervical cancer screening rates in this underserved population.
The introduction of the Pap test has led to significant reductions in cervical cancer incidence and mortality in the United States (US).1 However, screening rates are suboptimal in many Asian American subgroups, and Asian American women are less likely than non-Hispanic White women to be diagnosed with cervical cancer at a localized stage.2 Studies consistently report that Korean American women have the lowest rates of cervical cancer screening,3-6 with only 63.4% adherent to current screening guidelines,7 well below the Healthy People 2020 target of 93.0% screening compliance. In light of these statistics, programs to enhance screening rates in this population are urgently needed.
Factors associated with screening among Korean American women are varied and can include lack of knowledge, psychosocial beliefs that may discourage screening, and barriers to healthcare access. For example, many Korean American women did not know the recommended screening schedule, nor who should undergo screening.8, 9 Psychosocial beliefs, such as low perceived risk,10 are also associated with low screening rates. In addition, the belief that one only seeks healthcare for the treatment of illness or specific symptoms contributes to low uptake of screening in the absence of symptoms.6, 11 Indeed, the concept of preventive medicine has not been strongly endorsed in Korean culture,12 and therefore, the value of cancer screening may not be fully recognized.
Importantly, access barriers (e.g., lack of insurance, language difficulties) are the most often cited factors associated with low screening rates.6, 10, 11 Korean American women who lack health insurance are less likely than insured women to obtain screening.13 National statistics indicate that over 30% of Korean Americans are uninsured,14 and Korean Americans are disproportionately self-employed or work in small businesses, employment situations that are less likely to offer health benefits.15 Further, Korean American women with limited English language proficiency experience many difficulties not only in obtaining insurance coverage, but also in accessing health care services, scheduling appointments, and communicating with healthcare professionals.16
Given that a high proportion of Korean American women are foreign-born, have limited English proficiency, and report no usual source of health care,7 this confluence of factors creates a formidable challenge for Korean American women to overcome. Yet, few intervention programs have been developed for this population.17-19 A non-randomized trial of a mobile phone text messaging intervention among 30 Korean American women yielded a screening rate of 23%19; and large-scale trials involving community workshops and health counselor support reported no or limited improvement in Pap test rates,17, 18 underscoring the extreme difficulty in moving the needle on increasing cervical cancer screening rates in this population. Therefore, we sought to evaluate a multi-component intervention program that combined culturally-relevant cancer education with navigation services in an effort to increase screening rates among Korean American women. The intervention components were designed to increase awareness of cervical cancer risk, as well as address both individual-level beliefs and healthcare access barriers, in order to promote screening behaviors in this population that experiences considerable barriers to screening.
METHODS
Study Design and Participants
Korean American communities tend to be centered around churches, and more than 70% of first-generation Korean Americans are churchgoers.20, 21 Because Korean American churches offer an important opportunity to partner on health promotion activities,22 we implemented this study across 22 Korean churches located in southeastern Pennsylvania and New Jersey. From interviews with Korean church leaders, it was noted that the number of female church members in each of these churches ranged from 80 to over 2,000 women. A matched-pair design was used to stratify the 22 Korean churches by size and geographic location. Although no data exist to suggest that church size and geographic location are related to screening behavior, we opted to balance these variables across intervention and control groups. Matching has been successfully used in community intervention trials to reduce potential bias, increase power, and improve face validity.23, 24
The study was approved by the Institutional Review Board at Fox Chase Cancer Center and Temple University in accordance with federal regulations, and is registered on ClinicalTrials.gov (ClinicalTrials.gov identifier NCT02594826). Informed consent was obtained from each participant prior to study participation. Women were eligible to participate in the study if they met the inclusion criteria of: (1) self-identified Korean ethnicity; (2) age 21 or older; (3) not adherent to current Pap test guidelines; and (4) no current or prior diagnosis of cervical cancer or other cervical abnormality.
Procedures
The study utilized a two-arm, group-randomized design. The experimental unit was the church, with 11 churches assigned to receive the intervention program and 11 churches assigned to the control condition. Randomization was performed as follows: churches were randomly ordered within each matched pair, and then each church within a matched pair was randomly assigned to the experimental or control condition using a computerized coin flip. This double randomization procedure has been used in COMMIT25 and other community intervention trials,26 and prevents any one person from assigning church sites in a subjective, non-randomized way.
Intervention
The intervention content was guided by an overarching framework that integrated concepts from the Health Belief Model (HBM)27 and Social Cognitive Theory (SCT)28-30 to address individual beliefs and expectancies regarding cervical cancer screening (e.g., perceived risk of developing cervical cancer; perceived benefits and barriers to screening; social and cultural norms regarding screening). Intervention participants met in small groups and received one 2-hour educational session conducted by bilingual community health educators (CHEs). Each educational session was held at church sites and focused on cervical cancer risk factors; screening guidelines and procedures; a discussion of possible barriers to screening relevant to Korean American women; and follow-up and clinical management if an abnormal result is identified. Information on available low-cost or free screening sites was provided to participants, and all participants were offered navigation assistance for screening. A follow-up reminder letter for screening was sent six months after the educational session.
Participants in the control condition also received a 2-hour education session delivered by bilingual CHEs. This session included topics on general health and cancer education including tobacco, nutrition, benefits of obtaining routine medical checkups, and descriptions of cancer screening tests (e.g. cervical, breast, and colon cancer screening) along with recommended screening guidelines. Control group participants received recommendations to seek regular preventive healthcare and a list of healthcare sites that offer free or low-cost cervical cancer screening.
Measures
At study entry, participants completed a baseline assessment containing items regarding demographic background (e.g, age, education level, marital status), prior screening history, and healthcare access (e.g., has health insurance; has a regular physician).31
The primary outcome was cervical cancer screening (receipt of a Pap test) in the 12 months following study entry. Bilingual interviewers contacted participants at 12-month follow-up and assessed screening behavior via self-report (“Have you had a Pap test during the past 12 months?” Yes/No). Those participants who reported that they had not had a Pap test were asked to complete an open-ended item regarding reasons why they did not obtain screening (“Please describe your reasons for why you did not get a Pap test.”). Women could provide multiple reasons for non-screening. Participants who reported receiving a Pap test were asked to provide a medical release consent to allow project staff to contact their healthcare providers to validate self-reported testing.
Finally, intervention participants who reported receiving a Pap test were also asked to complete a brief assessment regarding their utilization of navigation services.32 Specifically, participants were asked whether someone helped them obtain screening (Yes/No); and if yes, whether that individual was a relative/family member, friend/neighbor, or the study navigator. Participants who received assistance were also asked to indicate what assistance was provided from a checklist of activities (e.g., help in arranging transportation, scheduling medical appointments, arranging language interpretation or translation services, etc.).
Statistical Analyses
Descriptive statistics were used to characterize participants in terms of demographic background. Given that the randomization assignment was made at the church-level, this design was taken into consideration during data analysis. We first ran a site-based analysis using a randomization test, where we compared the observed outcome to its distribution under the null hypothesis by permuting the intervention/control status of each pair. We then ran a patient-level analysis using a mixed-effects logistic regression model, to account for the within-site effect. As the site-level randomization did not perfectly balance all individual-level characteristics, we included these factors as covariates in the model. This primary analysis included only complete cases with follow-up information. To test the sensitivity of our conclusions, we re-ran both analysis procedures, conservatively assuming that all subjects who dropped out were non-screeners. Analyses were conducted using SAS (Cary, NC) version 9.4 and specified a two-sided significance level of 0.05.
RESULTS
Participants
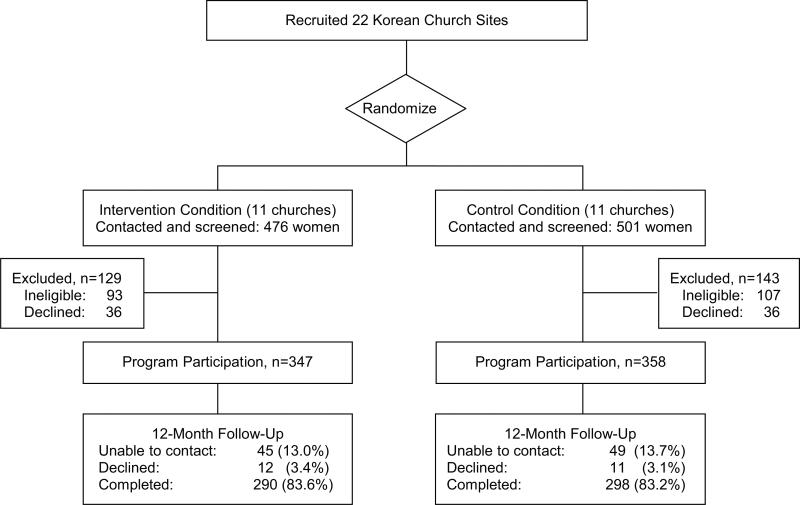
The study was conducted from February, 2009 through December, 2014. Korean American women (n=977) were identified from 22 churches. Specifically, 476 women were contacted and screened from the 11 churches in the Intervention condition; and 501 women were contacted and screened from the 11 churches in the control condition. Of the 777 women who were eligible to participate, 705 (90.7% study acceptance rate) provided written informed consent and enrolled in the study (Figure 1).
Figure 1.
Study Design.
Participant baseline characteristics are summarized in Table 1. Nearly 40% of participants had a high school education or below, and over 72% did not speak English well or at all. Most participants were foreign-born and had lived in the US for approximately 17 years. The two groups were similar across many demographic factors, with no significant differences observed in education level, English language speaking ability, employment status, country of birth, and mean number of years living in the US. However, there were significant differences in participant age, marital status, having health insurance, having a regular physician, and history of prior screening. Intervention group participants were slightly younger (M=51.9 years, SD=9.5) than control group participants (M=53.9 years, SD=11.6), F(1,704)=6.87, p<0.01. A greater proportion of intervention group participants were married (85.4%), compared to control group participants (75.7%), χ2(2)=10.6, p<0.01; but fewer intervention group participants had health insurance (37.6%) or a regular physician (50.0%) compared to control group participants (58.8% and 61.5%, respectively). A greater proportion of control group participants had never had a Pap test (37.9%) compared to intervention group participants (27.2%), χ2(2)=8.84, p < 0.01.
Table 1.
Demographic Characteristics by Study Condition
| Demographic Factors | Control Group (N=358) Mean (SD) |
Intervention Group (N=347) Mean (SD) |
Difference between Groups |
|---|---|---|---|
| Mean Age, years (SD) | 53.9 (11.6) | 51.9 (9.5) | p < 0.01 |
| Mean # of years living in US (SD) | 18.54 (10.9) | 16.97 (10.6) | n.s. |
| N (%) | N (%) | ||
| Education level | N§=346 | N=339 | n.s. |
| Below high school | 38 (11.0%) | 26 (7.7%) | |
| High school | 113 (32.7%) | 104 (30.7%) | |
| Some college or beyond | 195 (56.4%) | 209 (61.7%) | |
| Marital status | N=350 | N=343 | p < 0.01 |
| Married/Living as married | 265 (75.7%) | 293 (85.4%) | |
| Divorced/Separated/Widowed | 51 (14.6%) | 32 (9.3%) | |
| Never married | 34 (9.7%) | 18 (5.2%) | |
| English speaking ability | N=353 | N=341 | n.s. |
| Not at all | 27 (7.6%) | 26 (7.6%) | |
| Not well | 230 (65.2%) | 225 (66.0%) | |
| Well | 96 (27.2%) | 90 (26.4%) | |
| Employment status | N=350 | N=339 | n.s. |
| Employed | 183 (52.3%) | 187 (55.2%) | |
| Homemaker/Retired | 128 (36.6%) | 128 (37.8%) | |
| Unemployed | 17 (4.9%) | 8 (2.4%) | |
| Student | 22 (6.3%) | 16 (4.7%) | |
| Born in US | N=350 | N=341 | n.s. |
| No | 345 (98.6%) | 338 (99.1%) | |
| Yes | 5 (1.4%) | 3 (0.9%) | |
| Have health insurance | N=354 | N=343 | p < 0.001 |
| No | 146 (41.2%) | 214 (62.4%) | |
| Yes | 208 (58.8%) | 129 (37.6%) | |
| Have a physician | N=343 | N=330 | p < 0.01 |
| No | 132 (38.5%) | 165 (50.0%) | |
| Yes | 211 (61.5%) | 165 (50.0%) | |
| Ever had PAP test | N=343 | N=338 | p < 0.01 |
| No | 130 (37.9%) | 92 (27.2%) | |
| Yes | 213 (62.1%) | 246 (72.8%) |
Note:
N represents the number of responses and may differ across variables due to missing or incomplete responses.
We were able to re-contact 588 participants (83.4% retention rate) at the 12-month follow-up assessment: 290 participants in the intervention group, and 298 participants in the control group. There were no differences in drop-out rate by treatment condition. In addition, there were no significant differences in baseline demographic characteristics between study completers and those lost at follow-up, with the exception of age. Participants lost at follow-up were younger (M=50.4 years, SD=8.9) compared to study completers (M=53.4 years, SD=10.9), F(1,704) = 8.00, p < 0.01.
Screening Outcomes
Table 2 summarizes screening rates by church pair among all participants and among uninsured women only. Among all women, the average rate of screening in the intervention group was 72.1% (209 women screened) compared to only 10.1% (30 women screened) in the control group. Differences in screening rates between the two groups were heightened when examined among uninsured women only. Specifically, among women reporting no health insurance, the average rate of screening was 77.8% in the intervention group compared to 6.7% in the control group.
Table 2.
Cervical Cancer Screening Rates at 12-Months Post-Intervention by Community Site
| Control Group | Intervention Group | Rate Difference between Intervention and Control Group | ||||||
|---|---|---|---|---|---|---|---|---|
| Matched Pair | Church ID | Among All Women (%) | Among Uninsured (%) | Church ID | Among All Women (%) | Among Uninsured (%) | Among All Women (%) | Among Uninsured (%) |
| 1 | 2003 | 6/20 (30.0%) | 2/7 (28.6%) | 2001 | 37/37 (100%) | 22/22 (100%) | 70.0% | 71.4% |
| 2 | 2002 | 5/18 (27.8%) | 1/8 (12.5%) | 2022 | 14/23 (60.9%) | 14/19 (73.7%) | 33.1% | 61.2% |
| 3 | 2032 | 4/20 (20.0%) | 0/9 (0%) | 2045 | 31/43 (72.1%) | 20/27 (74.1%) | 52.1% | 74.1% |
| 4 | 2031 | 7/28 (25.0%) | 2/13 (15.4%) | 2049 | 12/16 (75.0%) | 12/16 (75.0%) | 50.0% | 59.6% |
| 5 | 2021 | 1/25 (4.0%) | 0/7 (0%) | 2013 | 11/20 (55.0%) | 5/6 (83.3%) | 51.0% | 83.3% |
| 6 | 2006 | 0/48 (0.0%) | 0/18 (0%) | 2042 | 19/27 (70.4%) | 14/17 (82.4%) | 70.4% | 82.4% |
| 7 | 2012 | 1/19 (5.3%) | 1/15 (6.7%) | 2048 | 23/27 (85.2%) | 9/10 (90.0%) | 79.9% | 83.3% |
| 8 | 2023 | 0/18 (0.0%) | 0/4 (0%) | 2047 | 18/25 (72.0%) | 14/15 (93.3%) | 72.0% | 93.3% |
| 9 | 2016 | 3/30 (10.0%) | 1/11 (9.1%) | 2014 | 14/24 (58.3%) | 12/20 (60.0%) | 48.3% | 50.9% |
| 10 | 2026 | 0/27 (0.0%) | 0/13 (0%) | 2046 | 23/31 (74.2%) | 16/20 (80.0%) | 74.2% | 80.0% |
| 11 | 2004 | 3/45 (6.7%) | 1/14 (7.1%) | 2010 | 7/17 (41.2%) | 6/13 (46.2%) | 34.5% | 39.1% |
| Total | 30/298 (10.1%) | 8/119 (6.7%) | 209/290 (72.1%) | 144/185 (77.8%) | 62.0% | 71.1% | ||
In both site-level and individual-level analyses, the intervention led to significantly higher screening rates (OR=25.9, 95% CI=10.1-66.1, p< 0.001).1 In covariate-adjusted analyses (see Table 3), the OR was strengthened (adjusted odds ratio [aOR]=35.8, 95% CI=11.1-114.9, p < 0.001). Model statistics also indicated good model fit, including the pseudo-R2 value of 0.54 and the C-statistic of 0.92. Of the covariates, absence of prior screening and having health insurance were both associated with lower odds of obtaining screening at 12-month follow-up. Although counter-intuitive, the finding that health insurance was associated with lower odds of screening likely reflects the fact that women in the intervention group were less likely to have health insurance, but had higher screening rates.
Table 3.
Mixed-Methods Logistic Regression Model for Cervical Cancer Screening Receipt at 12-Months Post-Program
| Variable | Categories | Odds Ratio | 95% CI | p-value |
|---|---|---|---|---|
| Treatment | Control | Ref | -- | -- |
| Intervention | 35.8 | 11.13-114.90 | <0.001 | |
| Age | Continuous | 1.03 | 1.00-1.06 | 0.06 |
| Marital status | Married | Ref | -- | -- |
| Divorced/Separated | 2.15 | 0.61-7.57 | 0.23 | |
| Never married | 1.52 | 0.46-5.00 | 0.49 | |
| Ever had Pap | Yes | Ref | -- | -- |
| No | 0.19 | 0.04–0.82 | 0.03 | |
| Health insurance | Uninsured | Ref | -- | -- |
| Insured | 0.44 | 0.22-0.90 | 0.03 | |
| Have physician | No | Ref | -- | -- |
| Yes | 0.93 | 0.46–1.86 | 0.85 |
Pseudo-R2 = 0.535
Intraclass correlation coefficient (ICC) = 0.29
Model C-statistic = 0.92
In sensitivity analysis, the intervention effect was attenuated, but remained highly statistically significant (OR=16.7, 95% CI=8.1-34.4, p< 0.001), including in covariate-adjusted analyses (aOR= 21.6, 95% CI=9.6-49.0, p< 0.001). We also conducted post-hoc analyses to account for the fact that, during the course of the study, updated screening guidelines were released and modified to once every 3 years. Thus, to address concerns that there may have been women included in the study who were not adherent at study entry, but for whom screening may not have been necessary within the 12-month interval following study entry, all women who had had screening within the past three years were excluded in this post-hoc analysis. Among the remaining women (n=340), differences remained statistically significant. Specifically, of 168 women in the intervention group, 110 (65.5%) had obtained screening by the follow-up assessment. In comparison, only 8 of 172 women in the control group (4.7%) had obtained screening by the follow-up assessment (OR=546.0, 95% CI=73.9-4031.5, p< 0.001).
Medical record review was used to validate self-reported screening among intervention group participants who reported obtaining a Pap test following program participation. Participants were asked to provide information about their healthcare provider and consent for medical record verification. Identified healthcare facilities were then contacted to confirm screening uptake. Of the 209 intervention group participants who reported being screened, we were able to request and verify medical record reports for 189 women (90.4%). From chart review, 91.5% (173 of 189 women) of the medical records matched self-reported screening.
Reasons for Not Screening
All women who self-reported that they had not obtained screening were asked to describe why they did not undergo screening. Within the intervention group, 81 women reported that they had not obtained screening. The primary reasons for not obtaining screening included the perception that they were healthy or had no health problems (72 women; 80.9%), followed by having no time or being too busy to obtain screening (42 women; 47.2%). Relatively fewer women indicated that a lack of insurance (18 women; 20.2%) was the reason why they had not obtained screening. Other reasons provided included the doctor not mentioning screening (1 woman), no transportation to obtain screening (1 woman), and forgetting to obtain screening (1 woman).
Among the 268 unscreened women in the control group, 97 women (36.2%) reported that they did not undergo screening because they were healthy or had no problems, and 70 women (26.1%) reported that the reason they did not have screening was due to a lack of insurance. Other commonly reported reasons for not screening included not knowing where to go or how to obtain screening (20 women; 7.4%) and a lack of time (18 women; 6.7%). Three women indicated that they did not like the Pap test. Other reasons provided included forgetting to obtain screening (1 woman), being too shy to undergo screening (2 women), and not having a doctor (1 woman).
Navigation
In the intervention group, 161 women (55.6%) reported that they received assistance in order to obtain cervical cancer screening. Of those, the majority (132 women; 82%) utilized the study navigator; the remainder called upon a family member or friend for assistance. Of the 161 women who received help from someone, 152 women (94.4%) needed assistance with more than one task. The most commonly requested support involved assistance in scheduling medical appointments (94.4%) and language/translation services (84.5%). Other assistance that was requested included arranging childcare (21.7%), transportation assistance (18%), needing additional information about medical services (7.5%), and needing information on financial support or services to help pay for screening (6.8%).
DISCUSSION
This study is one of the first, large-scale randomized trials to evaluate the effects of a multi-component intervention that combined community education with navigation services to increase cervical cancer screening among Korean American women. The intervention program yielded higher screening rates than the control program, and this effect remained robust in covariate-adjusted sensitivity analysis. These findings confirm prior results obtained in a pilot study of 102 Korean American women, which demonstrated that a community intervention program that combined cancer education with navigation support can significantly increase screening rates.31 Our present findings are also consistent with a recent study of 1,416 Vietnamese American women that utilized a similar multi-component intervention of community education plus navigation support to enhance participation in cervical cancer screening.26
A notable observation from this study is the large proportion of women who needed navigation support. The provision of navigation support likely played a critical role in facilitating access to screening, particularly in our sample of predominantly foreign-born women.33 In addition, the majority of women who received navigation support required assistance with more than one task, suggesting the complexity of arranging screening in this population. Language difficulties, lack of insurance, and lack of familiarity with the US healthcare system are considerable barriers to screening for Korean American women.6, 10, 11, 13 National data indicate that women who are unable to speak or read English face many difficulties in scheduling appointments and accessing health care services.16 Thus, among the Korean American women in our study, many of whom were foreign-born, speak limited English, and were uninsured and unfamiliar with the US healthcare system, navigation support was essential for overcoming significant language and access barriers to screening. Thus, formally adapting the navigator concept for use in the prevention context may serve an extremely important public health function in this community.
Despite the success of this intervention program, screening rates remain well below the Healthy People 2020 target goal. In order to help refine intervention effectiveness, we explored women's reasons for not obtaining screening. Among the majority of participants, the belief that screening is unnecessary if one is healthy or asymptomatic was a predominant reason for not screening. This finding is consistent with observational studies that have reported low cancer screening rates among Asian Americans, including Korean Americans, even after controlling for socioeconomic status and access to care factors,34, 35 suggesting that financial factors and access to care can only partially explain the low screening rates in this population. Qualitative studies report that Korean cultural beliefs tend to emphasize primary prevention (such as maintaining a healthy diet) to prevent cancer and other illness, rather than secondary prevention (screening for cancer in the absence of symptoms).7, 12, 36 Indeed, in a recent review, a lack of preventive health orientation (e.g., only going to the doctor when one is sick or when one has symptoms) was consistently associated with low rates of cancer screening.12 In addition, embarrassment has been reported to be a significant barrier to cervical cancer screening in this population.12 Korean American women have expressed embarrassment about discussing cervical cancer screening with others and with exposing one's body to a healthcare provider, particularly a male physician.6, 37 Future programs will need to evaluate how to develop effective messages regarding the benefits of screening among healthy individuals in order to promote or maintain future good health, particularly among the approximately 30% of Korean women who continue to be resistant to screening despite intensive intervention efforts.
A lack of time was also reported to be a substantial barrier to screening in this population. Many Korean Americans report working more than one job or have long working hours, thereby making it difficult to schedule clinic screening appointments, which normally occur during weekday work hours. A survey of Korean immigrant workers found that nearly 65% reported working more than 50 hours per week, with almost half (47%) working 60 hours/week or more, and 31% reported holding more than one job.38 As a result, a lack of time or inflexible work schedule becomes a difficult barrier to address within the constraints of normal clinic hours.
Thus, it may be time to consider innovative approaches to screening that can address such barriers. For example, emerging technologies supporting self-sampling for human papillomavirus (HPV) testing may offer a promising option for increasing screening among non-compliant women.39 Among women who had not received a Pap test in 9 years, response rates were three times higher among those offered self-sampling compared to a flexible clinic appointment.40 Other studies have demonstrated that self-sampling can be feasibly offered in a community setting with US populations that have traditionally had limited access to health care or experienced cultural barriers to screening.41 In light of data suggesting that this approach may yield several advantages that are relevant to Korean American women who have limited access to care, experience sociocultural barriers to screening, and/or reside in low-resource communities, future studies that offer multiple options for promoting participation in screening may be warranted.
We acknowledge several limitations to the present study. First, verification of self-reported screening was performed only in the intervention group and not in the control group. Therefore, the true screening rate in the control group may have been somewhat lower or higher. It is unlikely, however, that a significant proportion of women in the control condition were under-reporting screening. Second, despite the randomization procedures, the two groups differed on several demographic variables. However, women in the control group were more likely to have health insurance and a regular physician, key factors that generally facilitate access to care.11, 42 Third, recruitment was conducted in church venues; thus, results may not be generalizable to women who do not regularly attend church. Nevertheless, Korean American churches represent an essential channel for cancer education and health promotion among first-generation Koreans.22 By capitalizing on established church networks and an existing social infrastructure, we were able to have a broader reach into the community, and in particular, access those members who may not typically interact with the US healthcare system.
Despite these limitations, several important strengths are worth highlighting. This study built upon a strong partnership with Korean faith-based community leaders, community organizations, and academic institutions and utilized a community-based participatory research (CBPR) approach to engage community partners in project planning, recruitment, and program implementation. Further, navigation services that provided assistance with language translation, appointment scheduling, and arranging transportation helped address key barriers faced by this population. Moving forward, these findings can inform the development and implementation of future cancer screening programs. Community-accessible programs that incorporate cancer education with navigation support to target multiple, diverse factors within one cohesive program can be highly effective in increasing cervical cancer screening rates. Because disparities result from the complex interplay of numerous social, environmental, and institutional factors, a multicomponent approach can be effective in overcoming the considerable challenges faced by individuals in underserved and low-resource communities.
Acknowledgements and Funding Source
This research was supported by American Cancer Society grant RSGT CPPB-115763, and National Cancer Institute grants P30 CA006927 and U54 CA153513.
Footnotes
Conflict of Interest Disclosure
The authors received grant support from the American Cancer Society and the National Cancer Institute during the conduct of this study. The authors have no other disclosures to report.
Author Contributions
Carolyn Y. Fang: Conceptualization, methodology, investigation, resources, data curation, writing-original draft, visualization, supervision, project administration, and funding acquisition. Grace X. Ma: Conceptualization, methodology, investigation, resources, data curation, writing-review and editing, supervision, project administration, and funding acquisition. Elizabeth A. Handorf: Formal analysis, data curation, and writing-original draft. Ziding Feng: Methodology, formal analysis, and writing-original draft. Yin Tan: Investigation, data curation, supervision, and project administration. Joanne Rhee: Investigation, data curation, and project administration. Suzanne M. Miller: Writing-review and editing. Charles Kim: Investigation and project administration. Han Seung Koh: Conceptualization, investigation, resources, supervision, and project administration.
On the log-odds scale, the effect size and 95% confidence interval is as follows: log-OR=3.58, 95% CI (2.41-4.74). When the results are then transformed to the odds ratio scale, the final effect size and confidence interval is therefore magnified and much larger (OR=35.8, 95% CI=11.13-114.9).
Contributor Information
Carolyn Y. Fang, Cancer Prevention and Control Program, Fox Chase Cancer Center.
Grace X. Ma, Center for Asian Health and Department of Clinical Sciences, Lewis Katz School of Medicine, Temple University.
Elizabeth A. Handorf, Department of Biostatistics and Bioinformatics, Fox Chase Cancer Center.
Ziding Feng, Department of Biostatistics, The University of Texas M.D. Anderson Cancer Center.
Yin Tan, Center for Asian Health, Lewis Katz School of Medicine, Temple University.
Joanne Rhee, Center for Asian Health, Lewis Katz School of Medicine, Temple University.
Suzanne M. Miller, Cancer Prevention and Control Program, Fox Chase Cancer Center.
Charles Kim, Center for Asian Health, Lewis Katz School of Medicine, Temple University.
Han Seung Koh, First Korean United Methodist Church of Cherry Hill.
REFERENCES
- 1.Adegoke O, Kulasingam S, Virnig B. Cervical cancer trends in the United States: a 35-year population-based analysis. J Womens Health (Larchmt) 2012;21:1031–1037. doi: 10.1089/jwh.2011.3385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.ACS. Cancer Facts & Figures, 2016: Special Section on Cancer in Asian Americans, Native Hawaiians, and Pacific Islanders. American Cancer Society; Atlanta: 2016. [Google Scholar]
- 3.Kagawa-Singer M, Pourat N, Breen N, et al. Breast and cervical cancer screening rates of subgroups of Asian American women in California. Med Care Res Rev. 2007;64:706–730. doi: 10.1177/1077558707304638. [DOI] [PubMed] [Google Scholar]
- 4.Lee S, Chen L, Jung MY, Baezconde-Garbanati L, Juon HS. Acculturation and cancer screening among asian americans: role of health insurance and having a regular physician. J Community Health. 2014;39:201–212. doi: 10.1007/s10900-013-9763-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Juon HS, Choi Y, Kim MT. Cancer screening behaviors among Korean-American women. Cancer Detect Prev. 2000;24:589–601. [PubMed] [Google Scholar]
- 6.Lee MC. Knowledge, barriers, and motivators related to cervical cancer screening among Korean-American women. A focus group approach. Cancer Nurs. 2000;23:168–175. doi: 10.1097/00002820-200006000-00003. [DOI] [PubMed] [Google Scholar]
- 7.Kandula NR, Wen M, Jacobs EA, Lauderdale DS. Low rates of colorectal, cervical, and breast cancer screening in Asian Americans compared with non-Hispanic whites: Cultural influences or access to care? Cancer. 2006;107:184–192. doi: 10.1002/cncr.21968. [DOI] [PubMed] [Google Scholar]
- 8.Kim H, Lee KJ, Lee SO, Kim S. Cervical cancer screening in Korean American women: findings from focus group interviews. Taehan Kanho Hakhoe Chi. 2004;34:617–624. doi: 10.4040/jkan.2004.34.4.617. [DOI] [PubMed] [Google Scholar]
- 9.Lee EE, Tripp-Reimer T, Miller AM, Sadler GR, Lee SY. Korean American women's beliefs about breast and cervical cancer and associated symbolic meanings. Oncol Nurs Forum. 2007;34:713–720. doi: 10.1188/07.ONF.713-720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kim K, Yu ES, Chen EH, Kim J, Kaufman M, Purkiss J. Cervical cancer screening knowledge and practices among Korean-American women. Cancer Nurs. 1999;22:297–302. doi: 10.1097/00002820-199908000-00006. [DOI] [PubMed] [Google Scholar]
- 11.Juon HS, Seung-Lee C, Klassen AC. Predictors of regular Pap smears among Korean-American women. Prev Med. 2003;37:585–592. doi: 10.1016/j.ypmed.2003.09.006. [DOI] [PubMed] [Google Scholar]
- 12.Lee S-Y. Cultural Factors Associated with Breast and Cervical Cancer Screening in Korean American Women in the US: An Integrative Literature Review. Asian Nursing Research. 2015;9:81–90. doi: 10.1016/j.anr.2015.05.003. [DOI] [PubMed] [Google Scholar]
- 13.Juon HS, Seo YJ, Kim MT. Breast and cervical cancer screening among Korean American elderly women. Eur J Oncol Nurs. 2002;6:228–235. doi: 10.1054/ejon.2002.0213. [DOI] [PubMed] [Google Scholar]
- 14.Carrasquillo O, Carrasquillo AI, Shea S. Health insurance coverage of immigrants living in the United States: differences by citizenship status and country of origin. Am J Public Health. 2000;90:917–923. doi: 10.2105/ajph.90.6.917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cook WK, Tseng W, Ko Chin K, John I, Chung C. Identifying vulnerable Asian Americans under Health Care Reform: working in small businesses and health care coverage. J Health Care Poor Underserved. 2014;25:1898–1921. doi: 10.1353/hpu.2014.0164. [DOI] [PubMed] [Google Scholar]
- 16.Jacobs EA, Karavolos K, Rathouz PJ, Ferris TG, Powell LH. Limited English proficiency and breast and cervical cancer screening in a multiethnic population. Am J Public Health. 2005;95:1410–1416. doi: 10.2105/AJPH.2004.041418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wismer BA, Moskowitz JM, Min K, et al. Interim assessment of a community intervention to improve breast and cervical cancer screening among Korean American women. J Public Health Manag Pract. 2001;7:61–70. doi: 10.1097/00124784-200107020-00009. [DOI] [PubMed] [Google Scholar]
- 18.Moskowitz JM, Kazinets G, Wong JM, Tager IB. “Health is strength”: a community health education program to improve breast and cervical cancer screening among Korean American Women in Alameda County, California. Cancer Detect Prev. 2007;31:173–183. doi: 10.1016/j.cdp.2007.02.002. [DOI] [PubMed] [Google Scholar]
- 19.Lee HY, Koopmeiners JS, Rhee TG, Raveis VH, Ahluwalia JS. Mobile phone text messaging intervention for cervical cancer screening: changes in knowledge and behavior pre-post intervention. J Med Internet Res. 2014;16:e196. doi: 10.2196/jmir.3576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hurh WM, Kim KC. Religious Participation of Korean Immigrants in the United States. Journal for the Scientific Study of Religion. 1990;29:19–34. [Google Scholar]
- 21.Kwon H-Y, Kim KC, Warner RS. Korean Americans and Their Religions: Pilgrims and Missionaries from a Different Shore. Pennsylvania State University Press; University Park, PA: 2001. [Google Scholar]
- 22.Koh HC. Cultural Perspectives on Korean American Cancer Control. Korean Korean Am Stud Bull. 2003;13:16–39. [PMC free article] [PubMed] [Google Scholar]
- 23.Feng Z, Diehr P, Peterson A, McLerran D. Selected statistical issues in group randomized trials. Annu Rev Public Health. 2001;22:167–187. doi: 10.1146/annurev.publhealth.22.1.167. [DOI] [PubMed] [Google Scholar]
- 24.Feng Z, Thompson B. Some design issues in a community intervention trial. Control Clin Trials. 2002;23:431–449. doi: 10.1016/s0197-2456(02)00206-4. [DOI] [PubMed] [Google Scholar]
- 25.Community Intervention Trial for Smoking Cessation (COMMIT) I. Cohort results from a four-year community intervention. Am J Public Health. 1995;85:183–192. doi: 10.2105/ajph.85.2.183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ma GX, Fang C, Tan Y, Feng Z, Ge S, Nguyen C. Increasing cervical cancer screening among Vietnamese Americans: a community-based intervention trial. J Health Care Poor Underserved. 2015;26:36–52. doi: 10.1353/hpu.2015.0064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Strecher VJ, Rosenstock IM. The health belief model. In: Glanz K, Lewis FM, Rimer BK, editors. Health behavior and health education:Theory, research, and practice. Jossey-Bass; San Francisco: 2002. pp. 41–56. [Google Scholar]
- 28.Bandura A. Social cognitive theory: An agentic perspective. Annual Review of Psychology. 2001;52:1–26. doi: 10.1146/annurev.psych.52.1.1. [DOI] [PubMed] [Google Scholar]
- 29.Bandura A. Health promotion by social cognitive means. Health Educ Behav. 2004;31:143–164. doi: 10.1177/1090198104263660. [DOI] [PubMed] [Google Scholar]
- 30.Baranowski T, Perry CL, Parcel GS. How individuals, environments, and health behavior interact: Social cognitive theory. In: Glanz K, Lewis FM, Rimer BK, editors. Health behavior and health education:Theory, research, and practice. Jossey-Bass; San Francisco: 2002. pp. 153–178. [Google Scholar]
- 31.Fang CY, Ma GX, Tan Y, Chi N. A multifaceted intervention to increase cervical cancer screening among underserved Korean women. Cancer Epidemiol Biomarkers Prev. 2007;16:1298–1302. doi: 10.1158/1055-9965.EPI-07-0091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dohan D, Schrag D. Using navigators to improve care of underserved patients: current practices and approaches. Cancer. 2005;104:848–855. doi: 10.1002/cncr.21214. [DOI] [PubMed] [Google Scholar]
- 33.Shommu NS, Ahmed S, Rumana N, Barron GR, McBrien KA, Turin TC. What is the scope of improving immigrant and ethnic minority healthcare using community navigators: A systematic scoping review. Int J Equity Health. 2016;15:6. doi: 10.1186/s12939-016-0298-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lee HY, Im H. Colorectal cancer screening among Korean American immigrants: unraveling the influence of culture. J Health Care Poor Underserved. 2013;24:579–598. doi: 10.1353/hpu.2013.0087. [DOI] [PubMed] [Google Scholar]
- 35.Ward E, Jemal A, Cokkinides V, et al. Cancer disparities by race/ethnicity and socioeconomic status. CA Cancer J Clin. 2004;54:78–93. doi: 10.3322/canjclin.54.2.78. [DOI] [PubMed] [Google Scholar]
- 36.Tang TS, Solomon LJ, Yeh CJ, Worden JK. The role of cultural variables in breast self-examination and cervical cancer screening behavior in young Asian women living in the United States. J Behav Med. 1999;22:419–436. doi: 10.1023/a:1018653306776. [DOI] [PubMed] [Google Scholar]
- 37.Lee EE, Fogg L, Menon U. Knowledge and beliefs related to cervical cancer and screening among Korean American women. West J Nurs Res. 2008;30:960–974. doi: 10.1177/0193945908319250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Asian American Legal Defense and Education Fund “Forgotten Workers”: A Study of Low-Wage Korean Immigrant Workers in the Metropolitan New York Area. 2006 [Google Scholar]
- 39.Wikstrom I, Lindell M, Sanner K, Wilander E. Self-sampling and HPV testing or ordinary Pap-smear in women not regularly attending screening: a randomised study. Br J Cancer. 2011;105:337–339. doi: 10.1038/bjc.2011.236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Darlin L, Borgfeldt C, Forslund O, et al. Comparison of use of vaginal HPV self-sampling and offering flexible appointments as strategies to reach long-term non-attending women in organized cervical screening. Journal of Clinical Virology: The Official Publication of the Pan American Society for Clinical Virology. 2013;58:155–160. doi: 10.1016/j.jcv.2013.06.029. [DOI] [PubMed] [Google Scholar]
- 41.De Alba I, Anton-Culver H, Hubbell FA, et al. Self-sampling for human papillomavirus in a community setting: Feasibility in Hispanic women. Cancer Epidemiol Biomarkers Prev. 2008;17:2163–2168. doi: 10.1158/1055-9965.EPI-07-2935. [DOI] [PubMed] [Google Scholar]
- 42.De Alba I, Hubbell FA, McMullin JM, Sweningson JM, Saitz R. Impact of U.S. citizenship status on cancer screening among immigrant women. J Gen Intern Med. 2005;20:290–296. doi: 10.1111/j.1525-1497.2005.40158.x. [DOI] [PMC free article] [PubMed] [Google Scholar]