Abstract
Importance
Providing culturally competent care to the growing number of limited English proficiency (LEP) Latinos with diabetes in the United States is challenging.
Objective
Evaluate changes in risk factor control among LEP Latinos with diabetes who switched from language discordant (English-only) to language concordant (Spanish-speaking) primary care providers or vice versa.
Design
Pre-post, difference-in-differences study.
Setting
Kaiser Permanente Northern California (KPNC), an integrated healthcare delivery system with access to bilingual providers and/or professional interpreter services.
Participants
Adult diabetes patients (n=1,605), self-identifying as Latino, whose preferred language was Spanish (LEP) and switched providers between 2007-2013. Spanish-speaking and English-only providers were identified by self-report or utilization data.
Exposure
Change in patient-provider language concordance after switching providers.
Outcomes
Glycemic control (HbA1c < 8%), poor glycemic control (HbA1c > 9%), LDL control (LDL < 100 mg/dL), and systolic blood pressure control (sBP < 140 mmHg).
Results
There was a significant net improvement in glycemic and LDL control among LEP Latinos who switched from language discordant to concordant providers relative to those who switched from one discordant to another discordant provider. After adjustment and accounting for secular trends, the prevalence of glycemic control increased by 10% (95% CI: 2% to 17%; p=0.01), poor glycemic control decreased by 4% (95% CI: −10% to 2%; p=0.16) and LDL control increased by 9% (95% CI: 1% to 17%; p=0.03). No significant changes were observed in SBP control. Prevalence of LDL control increased 15% (95% CI: 7% to 24%; p=0.0004) among LEP Latinos who switched from concordant to discordant providers. Risk factor control did not worsen following a provider switch in any group.
Conclusions and Relevance
We observed significant improvements in glycemic control among LEP Latino diabetes patients who switched from language discordant to concordant providers. Facilitating language concordant care may be a strategy for diabetes management among LEP Latinos.
Keywords: Latino/Hispanic, diabetes, limited English proficiency, physician-patient language concordance, glycemic control, low-density lipoprotein
Introduction
Thirty to forty percent of the more than 50 million U.S. Latinos speak English less than “very well” and may have limited English proficiency (LEP).1,2 For LEP Latinos seen by providers who do not speak Spanish, language discordance may impede delivery of culturally competent health care.3-5 Patients with language concordant providers have potentially better communication, interpersonal process of care, patient-centeredness, trust and satisfaction with quality of care.6-11 However, the effectiveness of matching LEP patients to language concordant providers to improve health outcomes or reduce health inequalities has not been evaluated and will unlikely be studied in a randomized trial due to ethical and legal constraints.
Among diabetes patients, LEP Latinos have higher rates of poor glycemic control than English-speaking Latinos or whites but this inequality might be mitigated by care from Spanish-speaking (i.e., language concordant) providers.12 In an integrated health care system with access to interpreter services, we previously reported that LEP Latinos with language concordant providers had lower rates of poor glycemic control compared to LEP Latinos with English-only providers (16% vs 28%).12 LEP Latinos with language concordant providers have been found to have better adherence to cardiometabolic medications than those with discordant providers.13 However, causal inferences from such cross-sectional studies are limited by the inability to establish that the exposure (i.e., language barriers) preceded the outcome of interest (i.e., health outcomes).
We used a natural experiment to examine changes in glycemic, lipid, and systolic blood pressure control among diabetes patients who switched primary care providers, focusing on LEP Latinos who switched from English-only (discordant) to Spanish-speaking (concordant) primary care providers (and vice versa) and compared to other provider switches.
Methods
Study setting & cohort construction
Kaiser Permanente Northern California (KPNC) provides care to approximately 3.9 million members in Northern California. Professional interpreter services are available at all medical facilities and departments, including the pharmacy and laboratory; some facilities offer clinics staffed with bilingual providers and employees and many written materials are available in Spanish.
Eligible study subjects were adults from the KPNC Diabetes Registry,14 who self-identified as Latino, whose preferred language was Spanish, and who switched providers at least once. Patients were identified as LEP if Spanish was indicated as their preferred spoken language in the KPNC electronic medical record (EMR).
There were 3,511 patients who: (1) switched providers between January 1, 2007 and December 31, 2013, (2) were empaneled with both the pre- and post-switch provider for at least 12 months, and (3) had continuous membership and prescription drug benefits. The switch date was the administrative start date (i.e., date of empanelment) with a new provider and marked the end of care with the previous provider. We excluded 525 patients who did not have at least one outpatient visit with each provider and 1,381 for whom we lacked Spanish proficiency data for either the pre- or post-switch provider. This left a cohort of 1,605 subjects (1,760 provider switches).
Providers were identified as Spanish-speaking if they self-reported “high” fluency in Spanish15,16 or there was evidence from utilization data that the provider delivered care in Spanish without the aid of interpreters. Self-report data came from KPNC Human Resources, which inquired about language proficiency at the time of hire or, secondarily, a provider language research survey administered in 2012.17
In the absence of self-report, we relied on utilization data which identified encounters with bilingual providers. If a provider had ≥5 visits with LEP Latinos during the year and at least 80% of those visits were coded “in-language care provided from bilingual provider”, then the provider was categorized as Spanish-speaking. If no visits were coded in that way, then the provider was categorized as English-only (i.e., did not speak Spanish). Providers who did not fall into either category were classified as missing Spanish language proficiency. We conducted a sensitivity analysis among providers for whom we had both self-reported Spanish fluency (assumed to be gold standard) as well as utilization data and found that this algorithm had 93% sensitivity and 91% specificity. Of the 1,498 providers who cared for the 3,511 eligible patients, we identified Spanish language proficiency for 1,044 (44% from self-report and 56% from utilization data). One hundred sixty providers (15%) were Spanish-speaking and 884 (85%) were English-only.
Each LEP patient was classified as having either a language concordant (“concordant”, i.e., bilingual Spanish-speaking) provider or language discordant (“discordant”, i.e., English-only) provider during the pre- and post-switch periods. The KPNC and UCSF Institutional Review Boards approved this study.
Exposures
The exposure of interest was a change in language concordance as a result of switching providers (i.e., from discordant to concordant or from concordant to discordant). LEP Latinos who experienced a change in provider language concordance were compared to reference patients made up of LEP Latinos who switched providers with no change in concordance (i.e., from discordant to discordant or from concordant to concordant).
Outcomes
We collected each patient’s glycated hemoglobin (HbA1c), low-density lipoprotein (LDL) and systolic blood pressure (sBP) at two time points: the last recorded value prior to the switch date and the last value within 12 months post-switch. The mean time between the pre and post measures was approximately one year. These continuous measures were categorized using recognized cut-points based on the Healthcare Effectiveness Data and Information Set (HEDIS) and American Diabetes Association (ADA) guidelines: glycemic control (HbA1c < 8%), poor glycemic control (HbA1c > 9%), LDL control (LDL < 100 mg/dL), and systolic blood pressure control (sBP < 140 mmHg).18,19
Covariates
Data were collected from the KPNC EMR and administrative databases. Patient demographics were self-reported in the EMR. Provider age, sex and race/ethnicity came from the human resources database. The reason for each provider switch was obtained from the administrative database and we categorized these as: administrative (e.g., provider changed medical facility or left health plan), language or communication issues (e.g., member language preference), other member requests (e.g., member desired same provider as family) or unknown. We calculated the previously validated neighborhood deprivation index,20 a contextual measure of socioeconomic status, by linking each patient’s geocoded residential address to census tract level socioeconomic indicators from the 2010 American Community Survey.
Statistical analysis
We used a difference-in-differences (DID) framework to study how changes in patient-provider language concordance impacted the change in risk factors pre- to post-switch. DID is a quasi-experimental approach which measures the change in an outcome due to an intervention/exposure (1st difference), after subtracting the background change (2nd difference, e.g., due to secular trends or discontinuity in care due to switching irrespective of language concordance).21,22 DID rests on the counterfactual assumption; viz, if LEP Latinos who switched from discordant to concordant providers had instead switched to other discordant providers, we assume that the changes in their clinical measures would be similar to the changes observed in the reference group (i.e., LEP Latinos who did not change concordance status). To adjust for case mix imbalances between exposure and reference groups, we included patient (age, sex and socio-economic status) as well as provider characteristics (age, sex, and race/ethnicity), the year and the reason for the provider switch as fixed effects.
Our repeated measures data had a hierarchical structure. Some patients switched providers more than once and all patients were nested within providers (i.e., multiple patients were empaneled with each provider). We specified hierarchical linear mixed models to estimate the net DID effect. Both patient and provider were specified as random effects in random intercept models to account for non-independence of the residual error and correctly adjust the variance estimates. We also conducted three sensitivity analyses. We modeled changes in glycemic control after excluding 121 patients whose pre- and post-switch measures were less than 90 days apart since glycated hemoglobin measures average plasma glucose levels during the prior 3-4 months. We also ran the models in the subset of patients who switched providers due to administrative changes only; this restricted the analysis to patients who were less vulnerable to self-selection bias because they did not initiate the provider switch on their own. In the third sensitivity analysis, we required a “wash-out” period after the switch (i.e., only utilizing post-switch measures which were at least 30 days after the first in-person visit with the post-switch provider), to ensure that the post-switch measure was collected after the patient had established a relationship with the new provider.
Results
The cohort consisted of 1,605 LEP Latinos. Before switching, 46% of the LEP Latinos were empaneled with a concordant provider and 54% with a discordant provider; 59% of LEP Latinos with concordant providers switched to another concordant provider, while 48% of LEP Latinos with discordant providers switched to a concordant provider. LEP Latinos with discordant providers who switched to concordant providers were more likely to have changed due to language or communication issues than patients who switched to another discordant provider (30% vs 9%, respectively). These two groups were similar in regards to demographics and baseline risk factor control (Table 1). LEP Latinos with concordant providers who switched to discordant providers had better rates of pre-switch LDL and systolic BP control than patients who switched to another concordant provider. However, they were mostly similar in regards to demographics and there were no differences in the prevalence of pre-switch glycemic control. Spanish-speaking providers were more likely to identify as Latino (51%) than English-only providers (2%) but were similar in terms of gender (54% female) and age (29% ≥45 years old)
Table 1.
Characteristics of 1,605 LEP Latino patients with diabetes who switched primary care providers; stratified by patient-provider language concordance pre- and post-switch†.
| Characteristic | Language Discordant to Concordant (n=418) |
Language Discordant to Discordant (n=445) |
Language Concordant to Discordant (n=301) |
Language Concordant to Concordant (n=441) |
All (n=1,605) |
|---|---|---|---|---|---|
| Patient characteristics | |||||
| Age a,b
< 45 45-64 65-74 75+ |
35 (8) 221 (53) 100 (24) 62 (15) |
54 (12) 216 (49) 81 (18) 94 (21) |
49(16) 136 (45) 66 (22) 50(17) |
41 (9) 229 (52) 92 (21) 79 (18) |
179 (11) 802 (50) 339 (21) 285 (18) |
| Female | 226 (54) | 225 (51) | 176 (58) | 260 (59) | 887 (55) |
| Neighborhood Deprivation Index 1st Q (least deprived) 2nd Q 3rd Q 4th Q (most deprived) |
35 (8) 77 (19) 131 (32) 172 (41) |
40 (9) 72 (16) 140 (32) 189 (43) |
28 (9) 53 (18) 94 (32) 123 (41) |
26 (6) 81 (19) 118 (27) 211 (48) |
129 (8) 283 (18) 483 (30) 695 (44) |
| Years empaneled with pre-switch provider, mean(SD) b |
4.6 (3.9) | 4.7 (3.4) | 4.4 (2.9) | 5.0 (3.4) | 4.7 (3.5) |
| Year of provider switch b
2007 2008 2009 2010 2011 2012 2013 |
59 (14) 46 (11) 41 (10) 65 (16) 58 (14) 67 (16) 82 (20) |
61 (14) 48 (11) 66 (15) 58 (13) 67 (15) 67 (15) 78 (18) |
21 (7) 25 (8) 35 (12) 39 (13) 74 (25) 67 (22) 40 (13) |
27 (6) 37 (8) 32 (7) 30 (7) 92 (21) 112 (25) 111 (25) |
168 (10) 156 (10) 174 (11) 192 (12) 291 (18) 313 (20) 311 (19) |
| Reason for provider switch *
a
Administrative change Language or communication issue Other member request Unknown |
120 (29) 124 (30) 62 (15) 112 (27) |
203 (46) 38 (9) 61 (14) 143 (32) |
174 (58) 12 (4) 40 (13) 75 (25) |
229 (52) 28 (6) 54 (12) 130 (29) |
726 (45) 202 (13) 217 (14) 460 (29) |
| Pre-Switch Provider characteristics | |||||
| Race/ethnicity a,b
Asian Black Hispanic White Non-Hispanic Other/UNK |
170 (41) 20 (5) 34 (8) 161 (39) 33 (8) |
237 (53) 32 (7) 20 (4) 130 (29) 26 (6) |
50 (17) 2 (1) 206 (68) 41 (14) 2 (1) |
61 (14) 3 (1) 278 (63) 87 (20) 12 (3) |
518 (32) 57 (4) 538 (34) 419 (26) 73 (5) |
| Age < 45 45-64 65+ |
222 (53) 191 (46) 5 (1) |
250 (56) 194 (44) 1 (<1) |
146 (49) 150 (50) 5 (2) |
212 (48) 225 (51) 4 (1) |
830 (52) 760 (47) 15 (1) |
| Female a | 223 (53) | 199 (45) | 165 (55) | 268 (61) | 855 (53) |
| Pre-Switch Clinical measures | |||||
| Glycemic control (HbA1c < 8%) | 256 (63) | 287 (69) | 200 (70) | 291 (68) | 1034 (67) |
| Poor glycemic control (HbA1c > 9%) | 85 (21) | 69 (17) | 46 (16) | 77 (18) | 277 (18) |
| LDL control (< 100 mg/dL) b | 259 (65) | 286 (69) | 187 (66) | 318 (76) | 1050 (69) |
| Systolic Blood Pressure control (< 140 mmHg) b |
312 (78) | 341 (81) | 227 (77) | 365 (84) | 1245 (80) |
N (Column %) reported unless otherwise noted.
For patients who switched providers more than once (n=142), data from the first provider switch were used.
p-value < 0.05 for LD-LC vs. LD-LD
p-value < 0.05 for LC-LD vs. LC-LC
P-values from chi-square statistics for categorical variables and ANOVA (F-test statistics) for continuous variables
LEP: Limited English proficiency; HbA1c: Glycated Hemoglobin; LDL: Low density lipoprotein
Missing data: Neighborhood deprivation index (n=15), HbA1c (n=69), LDL (n=90), sBP (n=58)
Administrative change includes: Provider leaving KPNC or changing medical facilities or schedule. Other member request includes: change due to location or gender preference or due to concerns about provider care or accessibility.
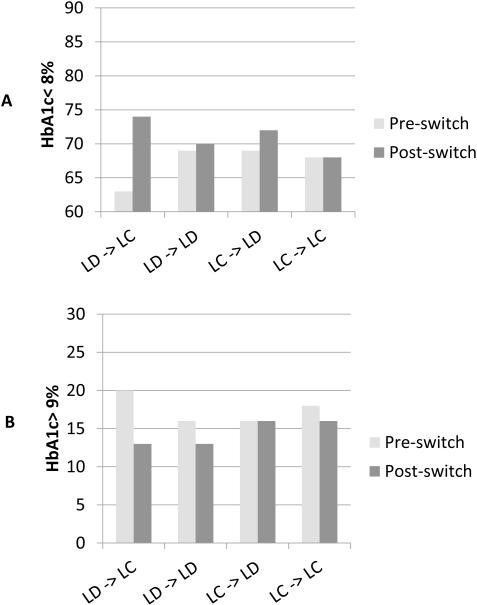
Most groups experienced slight improvements in the prevalence of glycemic control (HbA1c < 8%) and poor glycemic control (HbA1c > 9%) in the year after switching providers regardless of the change in language concordance (Figure 1). However, the largest improvement was observed among LEP Latinos who switched from discordant to concordant providers; glycemic control increased 11% (from 63% to 74%) while poor glycemic control decreased 7% (from 20% to 13%). In adjusted DID models, there was a 10% (95% CI: 2% to 17%; p-value=0.01) net increase in the prevalence of good glycemic control and a −4% (95% CI: −10% to 2%; p-value=0.16) net decrease in the prevalence of poor control among LEP patients switching from discordant to concordant providers (Table 2). When modeled as a continuous outcome, the change in mean HbA1c was −0.22 (95% CI: −0.45, 0.01; p-value=0.06; data not shown). Among LEP patients who switched from a concordant to a discordant provider, there were no significant changes in the prevalence of glycemic control or poor glycemic control. Results did not change substantively in a sensitivity analysis that excluded patients with pre- and post-switch HbA1c measures that were less than 90 days apart (Data not shown).
Figure 1.
Percentage of LEP Latino Diabetes Patients with Hemoglobin A1c < 8% (Panel A) and Hemoglobin A1c > 9% (Panel B) in the Year Before and After Switching Providers, Stratified by Patient-Provider Language Concordance (unadjusted)†.
Footnote:
† LEP: Limited English proficiency; LD: Language discordant; LC: Language concordant
Table 2.
Difference-in-differences (DID) estimates‡ of the net change in prevalence of risk factor control among 1,605¥ LEP Latino patients who switched providers, from adjusted mixed models∫.
| Outcome | Language Discordant to Concordant (Relative to: Discordant to Discordant)* |
Language Concordant to Discordant (Relative to: Concordant to Concordant)† |
||
|---|---|---|---|---|
| DID estimate‡
(95% CI) |
p-value | DID estimate‡
(95% CI) |
p-value | |
| HbA1c < 8% | +10% (2%, 17%) | 0.01 | +4% (−3%, 11%) | 0.24 |
| HbA1c > 9% | −4% (−10%, 2%) | 0.16 | +2% (−4%, 8%) | 0.53 |
| LDL < 100 mg/dL | +9% (1%, 17%) | 0.03 | +15% (7%, 24%) | 0.0004 |
| Systolic BP < 140 mmHg | +4% (−3%, 11%) | 0.25 | +6% (−1%, 13%) | 0.07 |
Difference-in-differences models estimate the adjusted, absolute change in the prevalence of the outcome among patients experiencing a change in language concordance status with their providers (i.e., discordant to concordant switches, or concordant to discordant switches) after subtracting the expected (background) changes observed in those patients who switched providers but language concordance status remained unchanged (i.e., from discordant to discordant or concordant to concordant (reference groups)).
Reference group: LEP Latinos who switched from one language discordant provider to another language discordant provider
Reference group: LEP Latinos who switched from one language concordant provider to another language concordant provider
Fixed effects included: Patient-Provider language concordance status, patient gender and age, neighborhood deprivation index, year of provider switch, reason for provider switch, provider gender, age and race. Patient and provider were modeled as random effects.
Includes 1,760 provider switches made by 1,605 patients.
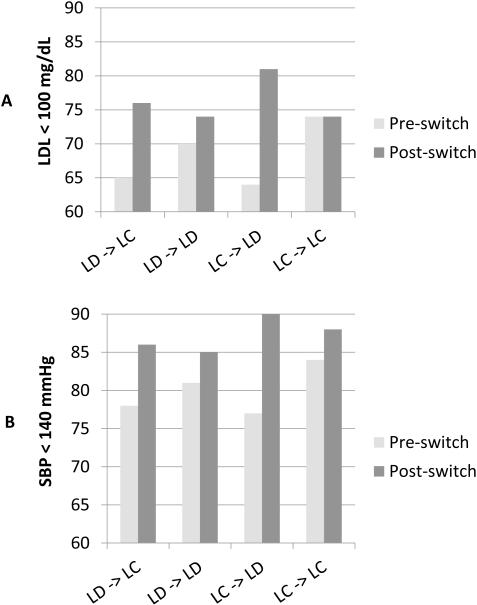
LDL cholesterol and sBP also improved following a provider switch for most groups (Figure 2). In adjusted DID models, the prevalence of LDL control (LDL < 100 mg/dL) increased by 9% (95% CI: 1% to 17%; p=0.03) among LEP patients switching from a discordant to concordant provider and by 15% (95% CI: 7% to 24%; p=0.0004) among LEP patients switching from a concordant to discordant provider. Mean LDL decreased (by −6.1 mg/dL , 95% CI: −11.4, −0.8; p=0.02) in the latter group but not the former. We did not find evidence of significant differences in changes in sBP control by concordance status.
Figure 2.
Percentage of LEP Latino Diabetes Patients with LDL < 100 mg/dL (Panel A) and Systolic Blood Pressure < 140 mmHg (Panel B) in the Year Before and After Switching Providers, Stratified by Patient-Provider Language Concordance (unadjusted)†.
Footnote:
†LEP: Limited English proficiency; LD: Language discordant; LC: Language concordant
There were qualitatively similar effect sizes in the subset of patients who switched providers due to administrative changes but the estimates were not statistically significant: 11% (95% CI: 2% to 24%, p=0.08), 8% (95% CI:-5% to 22%, p=0.24) and 11% (95% CI: −3% to 14%, p=0.23) net increases for glycemic, LDL and sBP control, respectively among LEP Latinos switching from discordant to concordant providers and a mean drop of −0.27% points (p=0.17) in HbA1c. Among LEP Latinos switching from concordant to discordant providers, there was a 24% (95% CI: 12% to 35%, p< 0.0001) net increase in LDL control and non-significant changes of 9% (95% CI: −1% to 18%, p=0.07) and 11% (95% CI: −2% to 24%, p=0.11) in the prevalence of glycemic and systolic blood pressure control, respectively. The sensitivity analyses that required a “wash-out” period after the switch also generated qualitatively similar results as the main models but the 8% increase in the prevalence of LDL control among LEP patients who switched from discordant to concordant providers was no longer significant (p=0.08, data not shown).
Discussion
In this study of LEP Latino diabetes patients cared for in a large, integrated health care delivery system, those who switched from language discordant (i.e., English only) to language concordant (i.e., bilingual, Spanish-speaking) providers experienced a 10% increase in the prevalence of glycemic control after accounting for changes observed among LEP patients switching from one discordant provider to another. There was no significant change in systolic blood pressure control and overall we found no deleterious effects on any of the three clinical outcomes following any provider switch, including those patients switching from concordant to discordant providers. Unexpectedly, we also observed an increase in the prevalence of good LDL control among those switching from concordant to discordant providers. To our knowledge, this is the first report to use a longitudinal, quasi-experimental study design to examine the impact of changes in language concordance on risk factor control among LEP Latinos with diabetes.
We found clinically meaningful effects with respect to improvement in glycemic control. These findings are generally consistent with those from a study of Latino youth with Type 1 diabetes which found a 0.5 point decrease in mean HbA1c in the year after joining a Spanish language clinic.23 We found a 0.22 point decrease in mean HbA1c following a switch to a language concordant provider. Improvements in risk factor control after switching to a language concordant provider were previously documented in a small cohort of Russian immigrants with diabetes.24 While not a randomized controlled trial, our difference-in-differences study design has strong causal validity. As health plans and regulatory agencies strive to improve population health and reduce disparities, it is noteworthy that a 10% improvement in prevalence of HbA1c < 8% among language discordant LEP Latinos was achieved by simply switching providers and without the creation of costly new programs; in short, it suggests a practical strategy for improving HEDIS measures for glycemic control in settings with relatively large numbers of Spanish-speaking providers.25
There are a few possible explanations for our findings. Latino patients with concordant providers were previously shown to be twice as likely to receive counseling about diet and exercise as Latino patients with discordant providers.26 LEP patients switching to concordant providers may find it easier to discuss diet and exercise recommendations or complex treatments compared to using interpreters. Patients with concordant providers might communicate using secure messaging in their preferred language, thus facilitating dialogue between office visits. Language concordance might be a proxy for a mutual cultural affinity, facilitating rapport and communication.27 Finally, patients often resist initiating insulin when recommended, and better communication with Spanish-speaking providers might ease the concerns of LEP patients.28
Similar to LEP patients who changed from discordant to concordant providers, those who changed from concordant to discordant providers experienced improvements in LDL control. The effect sizes in both groups were of the same order of magnitude with overlapping 95% confidence intervals. While the results in the discordant to concordant group support our hypothesis that improved communication leads to better clinical outcomes, it is difficult to apply this logic to the concordant to discordant group. Rather, we suspect that some other closely linked but unmeasured aspect of care improved (e.g, patient satisfaction or trust in provider) despite switching to a language discordant provider. KPNC, a setting with uniform access to professional translation services and an EMR which integrates pharmacy, laboratory, specialty and primary care services, provides good continuity of care following a provider switch; even among Spanish speaking LEP patients switching to discordant providers.
Our quasi-experimental, differences-in-differences study design provides stronger evidence of causality than previous cross sectional studies and minimizes potential confounding from measured and unmeasured risk factors because it uses each individual as his/her own control. We ran sensitivity analyses among patients whose provider switch was initiated administratively. This restricted the analysis to patients who were less vulnerable to self-selection bias because they did not initiate the provider switch on their own, resembling a “natural experiment”. In this sensitivity analysis, we found qualitatively similar effect sizes. Some of the estimates were no longer statistically significant due to the reduced sample size and loss of power. These consistent findings assuage concerns about observational self-selection bias.
Some limitations should be mentioned. These results may underestimate the effect of language barriers in populations with fewer bilingual providers or less comprehensive interpreter services. While professional interpreter services were available at all KPNC facilities, we cannot verify the extent of their use. Underuse has been documented in other settings with uniform availability of such services.29-31 We could not determine Spanish language proficiency for 30% of KPNC providers; these providers and their patient panels were excluded from the study. Although excluded providers were more likely to be non-Hispanic, and excluded patients were more likely female, excluded and included patients were similar with respect to age, neighborhood level socio-economic status, baseline risk factor control and pre-post changes in glycemic, lipid and systolic blood pressure. Thus, we believe that the exclusions introduced no systematic bias. We could not verify that LEP patients with concordant providers were communicating with their providers in Spanish. Latinos preferring to speak Spanish, but proficient in English may have been misclassified as LEP. We compared our administrative measure to self-report of LEP on the DISTANCE survey6,12,32 and estimated this misclassification rate to be about 20%. However, this misclassification is likely non-differential with respect to the direction of switch and provider concordance, thus biasing the findings toward the null and making the estimates conservative. Lacking an objective measure of provider Spanish language fluency, we relied on physician self-report or utilization data recording bilingual care delivery and misclassification is possible. The majority of the literature concurs that self-report at the high end of the scale is an acceptable proxy in the absence of formal testing15,17,33 and therefore we only categorized physicians who self-reported “high” fluency as Spanish-speaking. There are limitations to using utilization data to categorize providers’ Spanish language ability as these do not directly measure proficiency level. However, the utilization data clearly state that the provider is bilingual and these data are used for HEDIS reporting purposes. The high sensitivity (93%) and specificity (91%) of this measure provide reassurance that misclassification is minimal. Moreover, misclassifying providers would likely bias our results toward the null.
Conclusions
We found improvements in the prevalence of glycemic control among LEP Latinos with diabetes who switched from language discordant to concordant providers after accounting for expected background changes. There was no evidence of harm after switching from concordant to discordant providers, and in the case of LDL control, these switches also resulted in improvement. There are several compelling non-clinical reasons for providing language concordant care when possible, including increased patient satisfaction and facilitating communication. Our study suggests that health systems caring for LEP Latinos with diabetes may also improve glycemic control by facilitating language concordant care, even if it means switching providers.
Acknowledgments
Source of Support: Funds were provided by a Kaiser Permanente Community Benefit Grant and the National Institute of Diabetes, Digestive and Kidney Diseases: R01 DK090272, R01 DK099108 and K24 DK102057.
REFERENCES
- 1.U.S. Census Bureau ACS-YE Languages Spoken at Home By Ability to Speak English for the Population 5 Years and Over (Hispanic or Latino) 2014 http://factfinder.census.gov/faces/tableservices/jsf/pages/productview.xhtml?pid=ACS_14_1YR_B16006&prodType=table. Accessed November 20, 2015.
- 2.Sentell T, Braun K. Low Health Literacy, Limited English Proficiency, and Health Status in Asians, Latinos, and Other Racial/Ethnic Groups in California. J Health Commun. 2012;17(Suppl 3):82–99. doi: 10.1080/10810730.2012.712621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Perez-Stable EJ, Napoles-Springer A, Miramontes JM. The effects of ethnicity and language on medical outcomes of patients with hypertension or diabetes. Med Care. 1997;35(12):1212–1219. doi: 10.1097/00005650-199712000-00005. [DOI] [PubMed] [Google Scholar]
- 4.Ngo-Metzger Q, Sorkin DH, Phillips RS, et al. Providing high-quality care for limited English proficient patients: the importance of language concordance and interpreter use. J Gen Intern Med. 2007;22(Suppl 2):324–330. doi: 10.1007/s11606-007-0340-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.(IOM) IoM . Race, Ethnicity and Language Data: Standardization for Health Care Quality Improvement. The National Academies Press; Washington, D.C.: 2009. [PubMed] [Google Scholar]
- 6.Schenker Y, Karter AJ, Schillinger D, et al. The impact of limited English proficiency and physician language concordance on reports of clinical interactions among patients with diabetes: the DISTANCE study. Patient education and counseling. 2010;81(2):222–228. doi: 10.1016/j.pec.2010.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gonzalez HM, Vega WA, Tarraf W. Health care quality perceptions among foreign-born Latinos and the importance of speaking the same language. J Am Board Fam Med. 2010;23(6):745–752. doi: 10.3122/jabfm.2010.06.090264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fernandez A, Schillinger D, Grumbach K, et al. Physician language ability and cultural competence. An exploratory study of communication with Spanish-speaking patients. J Gen Intern Med. 2004;19(2):167–174. doi: 10.1111/j.1525-1497.2004.30266.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Detz A, Mangione CM, Nunez de Jaimes F, et al. Language concordance, interpersonal care, and diabetes self-care in rural Latino patients. J Gen Intern Med. 2014;29(12):1650–1656. doi: 10.1007/s11606-014-3006-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sudore RL, Landefeld CS, Perez-Stable EJ, Bibbins-Domingo K, Williams BA, Schillinger D. Unraveling the relationship between literacy, language proficiency, and patient-physician communication. Patient Educ Couns. 2009;75(3):398–402. doi: 10.1016/j.pec.2009.02.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wilson E, Chen AH, Grumbach K, Wang F, Fernandez A. Effects of limited English proficiency and physician language on health care comprehension. J Gen Intern Med. 2005;20(9):800–806. doi: 10.1111/j.1525-1497.2005.0174.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fernandez A, Schillinger D, Warton EM, et al. Language barriers, physician-patient language concordance, and glycemic control among insured Latinos with diabetes: the Diabetes Study of Northern California (DISTANCE) Journal of general internal medicine. 2011;26(2):170–176. doi: 10.1007/s11606-010-1507-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Traylor AH, Schmittdiel JA, Uratsu CS, Mangione CM, Subramanian U. Adherence to cardiovascular disease medications: does patient-provider race/ethnicity and language concordance matter? J Gen Intern Med. 2010;25(11):1172–1177. doi: 10.1007/s11606-010-1424-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Karter AJ, Schillinger D, Adams AS, et al. Elevated rates of diabetes in Pacific Islanders and Asian subgroups: The Diabetes Study of Northern California (DISTANCE) Diabetes Care. 2013;36(3):574–579. doi: 10.2337/dc12-0722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rosenthal A, Wang F, Schillinger D, Perez Stable EJ, Fernandez A. Accuracy of physician self-report of Spanish language proficiency. J Immigr Minor Health. 2011;13(2):239–243. doi: 10.1007/s10903-010-9320-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Reuland DS, Frasier PY, Olson MD, Slatt LM, Aleman MA, Fernandez A. Accuracy of self-assessed Spanish fluency in medical students. Teach Learn Med. 2009;21(4):305–309. doi: 10.1080/10401330903228489. [DOI] [PubMed] [Google Scholar]
- 17.Chaufan C, Karter AJ, Moffet HH, Quan J, Parker MM, Kruger J, Schillinger D, Fernandez A. Identifying Spanish Language Competent Physicians: The Diabetes Study of Northern California (DISTANCE) Ethn Dis. 2016;26(4):8. doi: 10.18865/ed.26.4.537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Standards of Medical Care in Diabetes—2016: Summary of Revisions. Diabetes Care. 2016;39(Supplement 1):S4–S5. doi: 10.2337/dc16-S003. [DOI] [PubMed] [Google Scholar]
- 19.Health O 2016 HEDIS Measures. 2016 http://public.optimahealth.com/lists/optimaformslibrary/qi-hedis-definitions.pdf. Accessed June 22, 2016.
- 20.Messer LC, Laraia BA, Kaufman JS, et al. The development of a standardized neighborhood deprivation index. J.Urban.Health. 2006;83(6):1041–1062. doi: 10.1007/s11524-006-9094-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Meyer BD. Natural and Quasi-Experiments in Economics. Journal of Business & Economic Statistics. 1995;13(2):151–161. [Google Scholar]
- 22.Campbell DT, Stanley JC. Experimental and Quasi-Experimental Designs for Research. Houghton Mifflin Co.; Boston: 1963. [Google Scholar]
- 23.Palau-Collazo MM, Rose P, Sikes K, et al. Effectiveness of a spanish language clinic for Hispanic youth with type 1 diabetes. Endocr Pract. 2013;19(5):800–804. doi: 10.4158/EP13004.OR. [DOI] [PubMed] [Google Scholar]
- 24.Mehler PS, Lundgren RA, Pines I, Doll K. A community study of language concordance in Russian patients with diabetes. Ethn Dis. 2004;14(4):584–588. [PubMed] [Google Scholar]
- 25.Meyers K, Tang G, Fernandez A. Responding to the Language Challenge: Kaiser Permanente's Approach. Perm J. 2009;13(3):77–83. doi: 10.7812/tpp/08-103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Eamranond PP, Davis RB, Phillips RS, Wee CC. Patient-physician language concordance and lifestyle counseling among Spanish-speaking patients. J Immigr Minor Health. 2009;11(6):494–498. doi: 10.1007/s10903-008-9222-7. [DOI] [PubMed] [Google Scholar]
- 27.Moreno G, Walker KO, Morales LS, Grumbach K. Do physicians with self-reported non-English fluency practice in linguistically disadvantaged communities? J Gen Intern Med. 2011;26(5):512–517. doi: 10.1007/s11606-010-1584-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Caballero AE. Building cultural bridges: understanding ethnicity to improve acceptance of insulin therapy in patients with type 2 diabetes. Ethn Dis. 2006;16(2):559–568. [PubMed] [Google Scholar]
- 29.Schenker Y, Wang F, Selig SJ, Ng R, Fernandez A. The impact of language barriers on documentation of informed consent at a hospital with on-site interpreter services. J Gen Intern Med. 2007;22(Suppl 2):294–299. doi: 10.1007/s11606-007-0359-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Diamond LC, Schenker Y, Curry L, Bradley EH, Fernandez A. Getting by: underuse of interpreters by resident physicians. J Gen Intern Med. 2009;24(2):256–262. doi: 10.1007/s11606-008-0875-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tang AS, Kruger JF, Quan J, Fernandez A. From admission to discharge: patterns of interpreter use among resident physicians caring for hospitalized patients with limited english proficiency. J Health Care Poor Underserved. 2014;25(4):1784–1798. doi: 10.1353/hpu.2014.0160. [DOI] [PubMed] [Google Scholar]
- 32.Moffet HH, Adler N, Schillinger D, et al. Cohort Profile: The Diabetes Study of Northern California (DISTANCE)--objectives and design of a survey follow-up study of social health disparities in a managed care population. International journal of epidemiology. 2009;38(1):38–47. doi: 10.1093/ije/dyn040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Diamond L, Chung S, Ferguson W, Gonzalez J, Jacobs EA, Gany F. Relationship between self-assessed and tested non-English-language proficiency among primary care providers. Med Care. 2014;52(5):435–438. doi: 10.1097/MLR.0000000000000102. [DOI] [PMC free article] [PubMed] [Google Scholar]