Abstract
Background
Magnetic resonance arthrogram (MRA) with radial cuts is presently the best available preoperative imaging study to evaluate chondrolabral lesions in the setting of femoroacetabular impingement (FAI). Existing followup studies for surgical treatment of FAI have evaluated predictors of treatment failure based on preoperative clinical examination, intraoperative findings, and conventional radiography. However, to our knowledge, no study has examined whether any preoperative findings on MRA images might be associated with failure of surgical treatment of FAI in the long term.
Questions/purposes
The purposes of this study were (1) to identify the preoperative MRA findings that are associated with conversion to THA, any progression of osteoarthritis, and/or a Harris hip score of < 80 points after acetabuloplasty and/or osteochondroplasty of the femoral head-neck junction through a surgical hip dislocation (SHD) for FAI at a minimum 10-year followup; and (2) identify the age of patients with symptomatic FAI when these secondary degenerative findings were detected on preoperative radial MRAs.
Methods
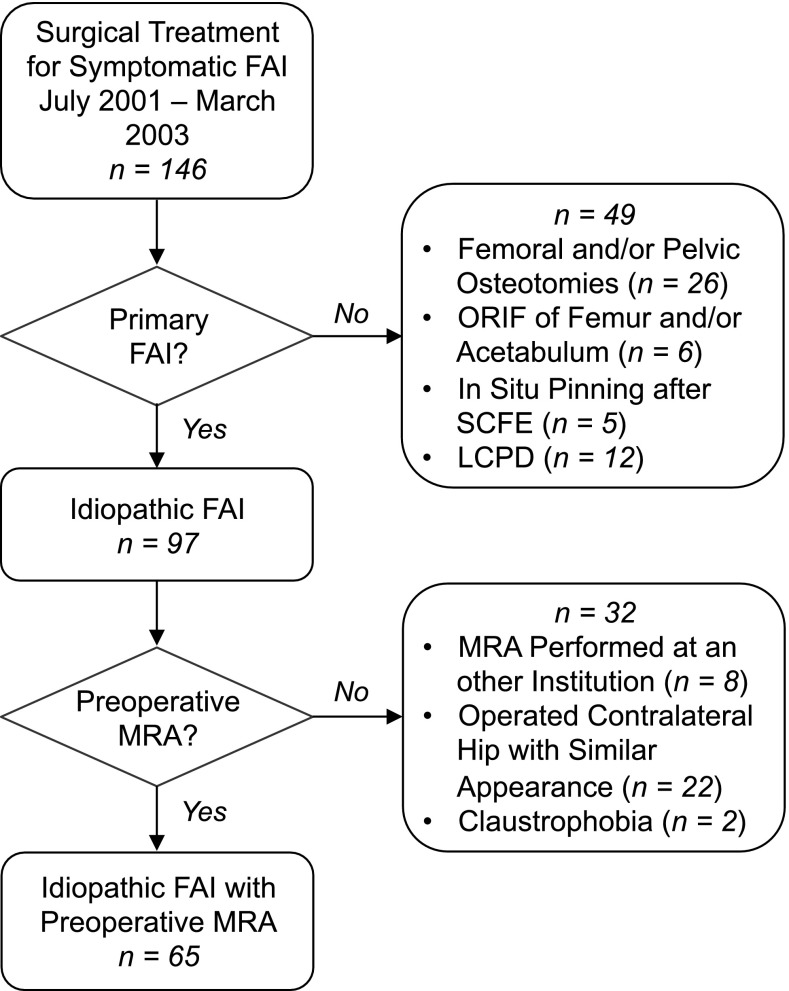
We retrospectively studied 121 patients (146 hips) who underwent acetabuloplasty and/or osteochondroplasty of the femoral head-neck junction through SHD for symptomatic anterior FAI between July 2001 and March 2003. We excluded 35 patients (37 hips) with secondary FAI after previous surgery and 11 patients (12 hips) with Legg-Calvé-Perthes disease. All patients underwent preoperative MRA to further specify chondrolabral lesions except in 19 patients (32 hips) including 17 patients (20 hips) who presented with an MRI from an external institution taken with a different protocol, 10 patients with no preoperative MRA because the patients had already been operated on the contralateral side with a similar appearance, and two patients (two hips) refused MRA because of claustrophobia. This resulted in 56 patients (65 hips) with idiopathic FAI and a preoperative MRA. Of those, three patients (three hips) did not have minimal 10-year followup (one patient died; two hips with followup between 5 and 6 years). The remaining patients were evaluated clinically and radiographically at a mean followup of 11 years (range, 10–13 years). Thirteen pathologic radiographic findings on the preoperative MRA were evaluated for an association with the following endpoints using Cox regression analysis: conversion to THA, radiographic evidence of any progression of osteoarthritis, and/or a Harris hip score of < 80. The age of the patient when each degenerative pattern was found on the preoperative MRA was recorded.
Results
The following MRI findings were associated with one or more of our predefined failure endpoints: cartilage damage exceeding 60° of the circumference had a hazard ratio (HR) of 4.6 (95% confidence interval [CI], 3.6–5.6; p = 0.003) compared with a damage of less than 60°, presence of an acetabular rim cyst had a HR of 4.1 (95% CI, 3.1–5.2; p = 0.008) compared with hips without these cysts, and presence of a sabertooth osteophyte had a HR of 3.2 (95% CI, 2.3–4.2; p = 0.013) compared with hips without a sabertooth osteophyte. The degenerative pattern associated with the youngest patient age when detected on preoperative MRA was the sabertooth osteophyte (lower quartile 27 years) followed by cartilage damage exceeding 60° of the circumference (28 years) and the presence of an acetabular rim bone cyst (31 years).
Conclusions
Preoperative MRAs with radial cuts reveal important findings that may be associated with future failure of surgical treatment for FAI. Most of these factors are not visible on conventional radiographs or standard hip MRIs. Preoperative MRA evaluation is therefore strongly recommended on a routine basis for patients undergoing these procedures. Findings associated with conversion to arthroplasty, radiographic evidence of any progression of osteoarthritis, and/or a Harris hip score of < 80 points should be incorporated into the decision-making process in patients being evaluated for joint-preserving hip surgery.
Level of Evidence
Level III, therapeutic study.
Introduction
Surgical treatment of femoroacetabular impingement (FAI) can result in decreased hip pain, improved hip function, and prevention of progression of osteoarthritis or conversion to THA in mid- and long-term followup [31, 45, 61, 62]. Several factors have been identified that can adversely affect the outcome of acetabuloplasty and/or osteochondroplasty of the femoral head-neck junction by open surgical hip dislocation (SHD) or arthroscopy [31, 45, 59, 61, 62]. These factors have been derived from demographic information, conventional radiography, and intraoperative findings [6, 31, 53, 61, 62]. Interestingly, none of these factors is based on magnetic resonance arthrography (MRA) despite the importance of this imaging modality in the standard imaging workup of patients with FAI [2, 38, 57].
The presence of osteoarthritis, reflected by a decrease in joint space width (Tönnis Grade > 0), is a consistently identified negative predictor for surgical outcome [31, 45, 61, 62]. Often, subtle secondary degenerative findings are present before joint space narrowing or loss of cartilage [42, 60]. These findings, including chondrolabral lesions, paralabral cysts, and subtle osteophytes, are more reliably detected on radial MRI of the hip [28, 34, 60]. These degenerative features have never been evaluated looking for an association with long-term outcomes after surgical treatment of FAI. In addition, it is not known when these degenerative changes can first be seen using MRA. More detailed knowledge about MRA-based degenerative changes in hips designated for surgical correction of FAI would help refine surgical indications, optimize long-term results, and provide guidance to the surgeon when counseling patients about realistic expectations of surgery.
The aims of this study were therefore (1) to identify the preoperative arthro-MRA findings associated with an unfavorable outcome (defined as conversion to THA, radiographic evidence of any progression of osteoarthritis, and/or a Harris hip score of < 80 points) after acetabuloplasty and/or osteochondroplasty of the femoral head-neck junction for FAI using SHD with a minimum followup of 10 years; and (2) to detect the age of the patients when these secondary degenerative alterations were detected on preoperative radial MRAs.
Patients and Methods
We retrospectively studied 121 patients (146 hips) who underwent acetabuloplasty and/or osteochondroplasty of the femoral head-neck junction through SHD for symptomatic anterior FAI between July 2001 and March 2003 (Fig. 1). Of these, we excluded 35 patients (37 hips) with secondary FAI after previous surgery: femoral and/or pelvic osteotomies (26 hips), open reduction and internal fixation of the femur and/or acetabulum (six hips), and in situ pinning after slipped capital femoral epiphysis (five hips). Eleven patients (12 hips) with Legg-Calvé-Perthes disease were also excluded. This left a subset of 75 patients (97 hips) with “idiopathic” FAI. During the period in question, generally all patients underwent preoperative MRA according to our protocol at our institution to further specify chondrolabral lesions. We did not repeat such a standardized MRA in patients who presented with an MRI from an external institution taken with a different protocol (17 patients [20 hips]). In 10 hips no preoperative MRA was done because the patients had already been operated on the contralateral side with a similar appearance. Two patients (two hips) refused the MRI because of claustrophobia. This resulted in a subset of 56 patients (65 hips) with idiopathic FAI and a preoperative MRA. Two patients (two hips) were lost to followup between 5 and 6 years after surgery without any progression of osteoarthritis or conversion to THA. These patients presented with a good clinical result (Harris hip score of 90 for both hips) at the most recent followup. One patient (one hip) died 8 years postoperatively from a cause unrelated to surgery. All three patients (three hips) without a minimal followup of 10 years were included in the statistical analysis to evaluate the association of MRA findings with outcome. The remaining 53 patients (62 hips) had a minimum 10-year followup (average, 11 years; range, 10–13 years).
Fig. 1.
Overview of the study population. ORIF = open reduction and internal fixation; SCFE = slipped capital femoral epiphysis; LCPD = Legg-Calvé-Perthes disease; MRA = magnetic resonance arthrogram.
FAI was diagnosed using established criteria based on a combination of clinical examination findings, conventional radiographic imaging, and MRI [2, 38, 66]. Mean age of the patients was 32 ± 9 years (range, 15–52 years). There were 38 male patients (68%) and 40 right hips (62%). The mean body mass index of the patients was 25 ± 4 kg/m2 (range, 18–35 kg/m2). Four patients (five hips) were diagnosed with isolated cam-type FAI, six patients (six hips) with isolated pincer-type FAI, and 46 patients (54 hips) with mixed-type (combined cam and pincer lesions) FAI. Diagnosis of FAI type was based on the intraoperative dynamic examination of the hip and the following criteria: cam-type FAI was defined by an α angle exceeding 50° [49] on the axial radiograph. Pincer-type FAI was defined by a lateral center-edge angle exceeding 40° [63, 69], a positive crossover sign [56], or persistent, intraoperatively visualized pincer-type impingement after offset correction.
All patients underwent correction of their FAI pathomorphology through a SHD, an intermuscular and internervous surgical approach that allows safe surgical dislocation of the hip without iatrogenic muscle damage [19]. The detailed surgical technique is described elsewhere [17, 65]. Briefly, patients were positioned in the lateral decubitus position. Through a straight lateral incision, the Gibson interval between the gluteus maximus and medius muscle was exposed. After a digastric trochanteric osteotomy, the hip capsule was then exposed in the interval between the piriformis and the gluteus minimus muscles. By cutting the round ligament, the hip can be safely dislocated. Pincer-type FAI was corrected by surgically detaching the labrum along the area of excessive acetabular coverage and resecting the excessive acetabular rim (acetabuloplasty). Cam-type FAI was corrected by addressing the abnormal asphericity on the femoral head-neck junction (osteochondroplasty of the femoral head-neck junction). In the 54 hips with mixed-type FAI, combined acetabuloplasty with osteochondroplasty of the femoral head-neck junction was performed. The six hips with isolated pincer-type FAI underwent acetabuloplasty only and the five hips with isolated cam-type FAI underwent osteochondroplasty of the femoral head-neck junction only. All patients underwent labral refixation using bone anchors with nonabsorbable sutures (G II Titanium Anchor; DePuy, Mitek, Norwood, MA, USA). Once all corrections were completed, impingement-free ROM was verified, aiming for a minimum of 20° of internal rotation in 90° of flexion. After closure of the capsule, the trochanteric fragment was reattached using two to three 3.5-mm cortical screws. Immediate postoperative continuous passive motion (CPM) of the hip was administered daily during the time of hospitalization to prevent intraarticular adhesions. CPM was applied for 1 hour three times a day with flexion limited to 90°. The mean duration of hospitalization was 7 ± 2 days (range, 4–11 days). Patients were maintained on partial weightbearing of 15 to 20 kg until full healing of the trochanteric osteotomy was confirmed radiographically. The mean trochanteric healing time was 62 ± 16 days (range, 43–148 days) with two patients (two hips) needing revision surgery for trochanteric refixation. Once trochanteric osteotomy healing was confirmed, abductor training was initiated.
Clinical examination was performed at 6 weeks, 12 weeks, and 1 year postoperatively and at least every 5 years thereafter. Examination included a full goniometric ROM assessment and evaluation with the anterior impingement test (Table 1).
Table 1.
Clinical results preoperatively and at a minimum of 10-year followup
| Parameters (best-worst score possible) | Subcategories | Preoperative | 10-year followup | p value |
|---|---|---|---|---|
| Anterior impingement test (percent positive) | – | 94 | 39 | < 0.001 |
| ROM | Flexion | 103 ± 11 (85–130) | 98 ± 9 (80–120) | 0.040 |
| Extension | 2 ± 5 (0–20) | 4 ± 3 (0–10) | 0.055 | |
| Internal rotation | 15 ± 10 (0–40) | 18 ± 10 (0–45) | 0.053 | |
| External rotation | 29 ± 11 (5–60) | 29 ± 13 (5–60) | 0.719 | |
| Abduction | 31 ± 9 (10–50) | 42 ± 11 (5–60) | < 0.001 | |
| Adduction | 20 ± 8 (0–35) | 21 ± 7 (3–45) | 0.715 | |
| Harris hip score [20] (0–100) | Total | – | 91 ± 11 (44–100) | – |
| Number of hips (percentage) with excellent result (90–100) | – | 37 (57%) | – | |
| Number of hips (percentage) with good result (80–89) | – | 12 (18%) | – | |
| Number of hips (percentage) with fair result (70–79) | – | 5 (8%) | – | |
| Number of hips (percentage) with poor result (< 70)* | – | 11 (17%) | – | |
| Merle d’Aubigné-Postel score [3] (18–0) | Total | 15.2 ± 1.4 (9–17) | 16.6 ± 1.4 (12–18) | < 0.001 |
| Pain (6–0) | 3.8 ± 0.7 (2–5) | 5.0 ± 0.9 (3–6) | < 0.001 | |
| Mobility (6–0) | 5.8 ± 0.5 (4–6) | 5.8 ± 0.4 (5–6) | 0.625 | |
| Walking ability (6–0) | 5.6 ± 0.7 (2–6) | 5.8 ± 0.4 (4–6) | 0.308 | |
| WOMAC [7] (0–100) | – | 7 ± 13 (0–59) | – | |
| Pain (0–100) | – | 7 ± 12 (0–50) | – | |
| Stiffness (0–100) | – | 10 ± 14 (0–55) | – | |
| Function (0–100) | – | 6 ± 13 (0–63) | – | |
| SF-12 [16, 71] | Physical component scale (100–0) | – | 52 ± 8 (24–61) | – |
| Mental component scale (100–0) | – | 50 ± 10 (20–63) | – | |
| UCLA score [73] (10–0) | – | 8 ± 2 (2–10) | – |
For the following patient-reported outcomes, no preoperative data were available: the Harris hip score, WOMAC, SF-12, and the UCLA score; values of continuous parameters are expressed as mean ± SD with range in parentheses; *including the patients who underwent THA.
Radiographic evaluation consisted of an AP pelvic radiograph taken in a standardized manner and a cross-table lateral view [66]. One of us not involved in the surgical care of the patients (SDS) assessed 13 parameters pre- and postoperatively on the AP pelvis radiograph using Hip2Norm (University of Bern, Bern, Switzerland) [64, 67, 74], validated and reliable software for description of the pathomorphology of the hip (Table 2). All patients underwent previously described standard MRI of the hip with intraarticular contrast agent [33]. The scans were carried out on a Siemens Vision 1.5-T high field scanner (Erlangen, Germany) using a flexible surface coil after fluoroscopic-guided intraarticular injection of saline-diluted gadolinium-DTPA (Dotarem 1:200; Guerbert AG, Paris, France). Standard axial, sagittal, and coronal proton density-weighted (PDW) and T1-weighted sequences were obtained. In addition, to assess the whole joint, a radial PDW sequence was used in which all slices were oriented orthogonal to the femoral neck and head. These slices were based on a sagittal oblique localizer, which was marked on the PDW coronal sequence and runs parallel to the sagittal oblique course of the femoral neck. For every patient these slices were defined individually resulting in a total of 14 radial slices with an interval of 26°.
Table 2.
Pre- and postoperative radiographic data
| Parameters | Preoperative | Postoperative | p value |
|---|---|---|---|
| Tönnis grade of osteoarthritis (number of hips [percent of hips])* [68] | |||
| Grade 0 | 50 (77) | 41 (63) | 0.0217 |
| Grade 1 | 14 (22) | 19 (29) | |
| Grade 2 | 1 (2) | 4 (6) | |
| Grade 3 | 0 (0) | 1 (2) | |
| Lateral center-edge angle (degrees) [72] | 30 ± 7 (18–46) | 25 ± 7 (12–44) | < 0.001 |
| Acetabular index (degrees) [68] | 3 ± 6 (−11–17) | 7 ± 7 (−6–25) | < 0.001 |
| Extrusion index (percent) [44] | 20 ± 6 (6–32) | 25 ± 6 (8–37) | < 0.001 |
| ACM angle (degrees) [9, 24] | 44 ± 4 (33–55) | 43 ± 6 (34–56) | 0.020 |
| Crossover sign (number of hips [percent of hips]) (percent positive) [56] | 31 (48) | 13 (20) | 0.001 |
| Retroversion index [66] (percent of hips with positive crossover sign [56]) | 28 ± 17 (8–52) | 15 ± 8 (6–48) | 0.144 |
| Posterior wall sign (number of hips [percent of hips]) (percent positive) [56] | 54 (83) | 56 (86) | 0.392 |
| Ischial spine sign (number of hips [percent of hips]) (percent) [26] | 26 (40) | 30 (46) | 0.387 |
| Caudocranial coverage (percent) | 81 ± 8 (64–100) | 75 ± 8 (57–91) | < 0.001 |
| Anterior coverage (percent) | 24 ± 6 (11–37) | 18 ± 6 (9–35) | < 0.001 |
| Posterior coverage (percent) | 43 ± 8 (27–64) | 42 ± 9 (25–64) | 0.532 |
| Axial alpha angle (degrees) [49] | 61 ± 12 (37–85) | 46 ± 8 (30–76) | < 0.001 |
Values of continuous parameters are expressed as mean ± SD with range in parentheses; *comparison of preoperative status and most resent followup; ACM = angle of Idelberger and Frank.
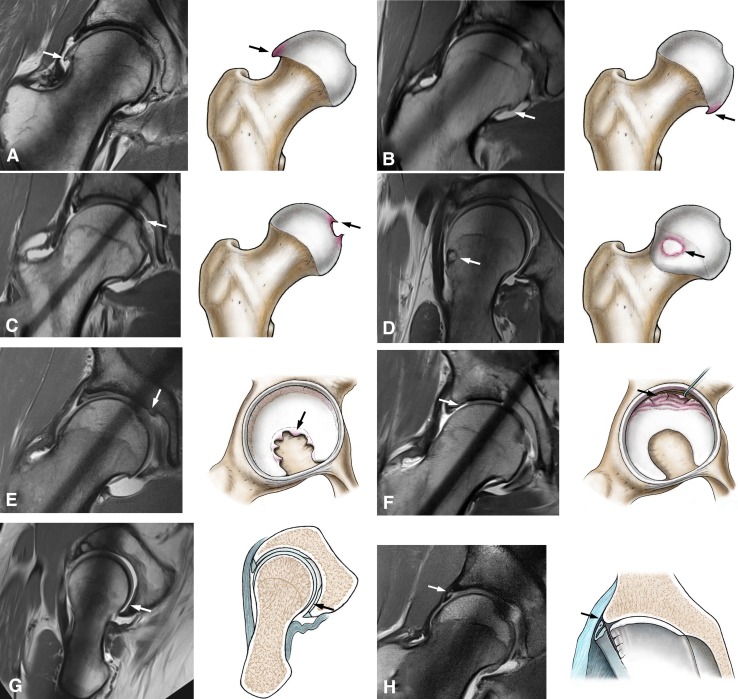
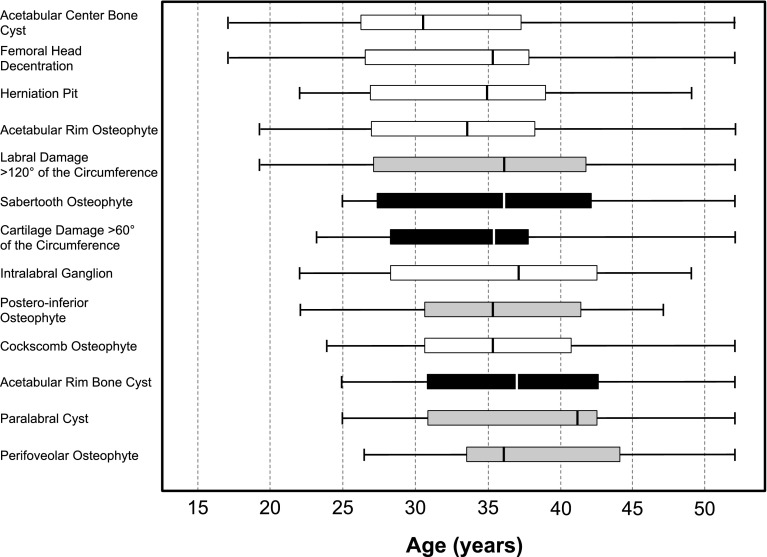
Thirteen study variables were assessed on every MRA (Table 3): labral damage, intralabral/paralabral cyst, acetabular rim/acetabular center bone cyst, osteophytes (cockscomb-type, perifoveolar, posteroinferior, acetabular rim, sabertooth), herniation pits, cartilage damage, and femoral head decentration (Fig. 2). These parameters represent either degenerative signs from the classic literature [11, 14, 21, 25, 32, 35, 42, 47, 70] or known secondary degenerative lesions in patients with MRIs [33, 37, 48, 55, 58, 60]. We included only parameters that seemed readily identifiable. In particular, labral lesions were not further subclassified because it is proven that there is a limited correlation between the MRI classification of labral tears [13] and intraoperative findings [8]. Instead, we assessed the extent of labral tears along the acetabular rim by means of the degrees of the circumference with 360° representing the entire circumference. Similarly, cartilage lesions were assessed dichotomously as present or absent if a clear inflow of the contrast agent between the acetabular and femoral cartilage surfaces was present (Fig. 1).
Table 3.
Description of the evaluated morphological MRA features including the results of reliability and reproducibility analysis
| Parameter | Description | Kappa intraobserver 1 | Kappa intraobserver 2 | Kappa interobserver |
|---|---|---|---|---|
| Cockscomb osteophyte | Beginning, subtle osteophyte formation at the superior to superoposterior femoral head neck junction [21, 25, 47] | 0.91 (0.73–1.0) | 0.90 (0.69–1.0) | 0.90 (0.74–1.0) |
| Posteroinferior osteophyte | Beginning, subtle osteophyte formation at the posteroinferior portion of the femoral head [21, 25, 47] | 0.83 (0.60–1.0) | 0.78 (0.47–1.0) | 0.80 (0.59–1.0) |
| Perifoveolar osteophyte | Beginning, subtle osteophyte formation at the fovea of the femoral head [21, 25] | 0.92 (0.76–1.0) | 0.78 (0.54–1.0) | 0.89 (0.74–1.0) |
| Herniation pit | Cystic formation at the anterosuperior femoral neck [18, 48, 54] | 0.92 (0.76–1.0) | 1 (NA) | 0.77 (0.49–1.0) |
| Sabertooth osteophyte | Beginning, subtle osteophyte formation at the central area of the lunate surface in the acetabular fossa [35, 42, 70] | 0.94 (0.81–1.0) | 0.86 (0.67–1.0) | 0.83 (0.63–1.0) |
| Cartilage damage | Any visible chondral degeneration including contrast material-filled defects or an area of clear cartilage signal intensity alteration [58] | 0.78 (0.57–0.98) | 0.77 (0.56–0.98) | 0.77 (0.57–0.98) |
| Femoral head decentration | Inflow of contrast agent in the posteroinferior joint space as a sign of contact loss between the corresponding femoral and acetabular cartilage [14, 32] | 0.94 (0.83–1.0) | 0.86 (0.66–1.0) | 0.78 (0.57–0.99) |
| Labral damage | Any visible labral degeneration including partial or full-thickness labral tears, fibrillations, flaps or intralabral signal alteration resulting from mucoid degeneration (excluding intralabral or paralabral cysts) [5, 13] | 0.90 (0.76–1.0) | 0.75 (0.54–0.95) | 0.83 (0.66–1.0) |
| Intralabral cyst | Round or oval-shaped cyst formation within the labral substance [55] | 0.90(0.69–1.0) | 0.73 (0.43–1.0) | 0.75 (0.47–1.0) |
| Paralabral cyst | Single- or multiloculated, sometimes septated well-defined fluid-intensity cyst bulging extraosseously at the level of the acetabular recess [36, 37] | 0.89 (0.73–1.0) | 0.89 (0.73–1.0) | 0.77 (0.56–0.98) |
| Acetabular rim bone cyst | Intraosseous, fluid-containing cystic formation at the acetabular rim adjacent to the base of the acetabular labrum [60] | 0.86 (0.67–1.0) | 0.75 (0.49–1.0) | 0.85 (0.65–1.0) |
| Acetabular center bone cyst | Intraosseous, fluid-containing subchondral cystic formation in the weightbearing zone of the acetabulum [55, 60] | 0.88 (0.71–1.0) | 1.0 (NA) | 0.87 (0.70–1.0) |
| Acetabular rim osteophyte | Beginning, subtle osteophyte formation at any portion of the acetabular rim [11, 60] | 0.82 (0.62–1.0) | 0.77 (0.56–0.98) | 0.65 (0.39–0.90) |
Values are expressed as mean with 95% confidence interval; MRA = magnetic resonance arthrogram; ICC = intraclass correlation coefficient; NA = not applicable.
Fig. 2A–M.
A total of 13 degenerative patterns seen in the MRA have been evaluated to find an association with conversion to THA, progression of osteoarthritis, or a HHS of < 80 (the arrows highlight the features): (A) cockscomb osteophyte [21, 25, 47]; (B) posteroinferior osteophyte [21, 25, 47]; (C) perifoveolar osteophyte [21, 25]; (D) herniation pit [18, 48, 54]; (E) sabertooth osteophyte [35, 42, 70]; (F) cartilage damage [58]; (G) femoral head decentration [14, 32]; (H) labral damage [5, 13]; (I) intralabral cyst [55]; (J) paralabral cyst [36, 37]; (K) acetabular rim bone cyst [60]; (L) acetabular center bone cyst [55, 60]; and (M) acetabular rim osteophyte [11, 60]. Figures created by and used with permission from Klaus Oberli.
To detect the reproducibility and reliability of these assessments, 40 MRI slices were randomly chosen from the study patient database. Two independent observers (MSH, SDS; both orthopaedic residents in training and not involved in surgical care of the patients) analyzed the blinded images on two separate occasions at least 1 month apart. Inter- and intraobserver agreement of the 13 study variables was analyzed using the κ value (Table 3). The intraobserver κ values ranged from 0.73 to 1.0 and the interobserver κ values from 0.65 to 0.90 indicating at least a good or very good agreement according to Altman [1].
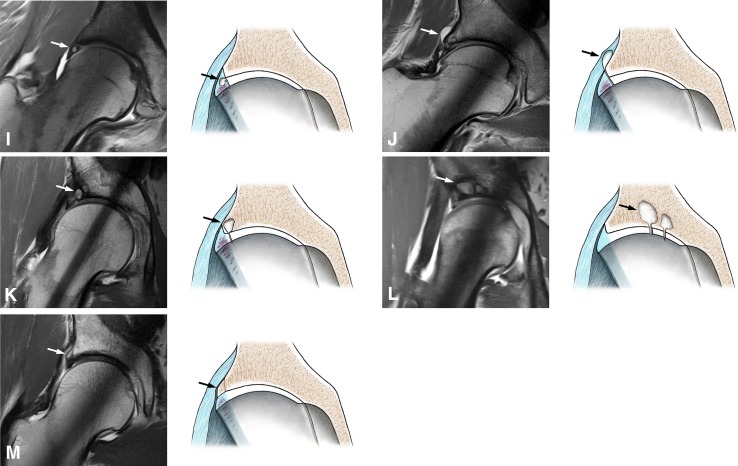
We recorded the age of the patients when each of these 13 factors had been identified on preoperative MRA. The concept behind the second research question was to evaluate whether any of these radiographic findings associated with one of the endpoints would be present at an early patient age. If so, this could help to identify “hips at risk” earlier. In addition, it would offer information on the degenerative cascade in hips with MRI even without a longitudinal study design.
All patients were invited for a clinical and radiographic followup after a minimum of 10 years postoperatively (mean, 11 years; range, 10–13 years). The following patient-reported outcomes were assessed at latest followup: the WOMAC [7], Harris hip score (HHS) [20], UCLA activity scale [73], the SF-12 [16, 71], and the Merle d’Aubigné score [3] (Table 1). Of these, only the Merle d’Aubigné score was available from the preoperative status because the others were not systematically assessed at that time. The conventional radiographs were assessed for the presence or absence of osteoarthritis according to Tönnis [68] by one observer (SDS). A complete data set at the 10-year followup point was available for 48 patients (57 hips). Five patients (five hips) refused radiographic followup because of concerns related to radiation exposure. On all five, we had clinical followup including the clinical scores at a minimum of 10 years with latest radiographic followup between 5 and 7 years postoperatively.
We tested normal distribution with the Kolmogorov-Smirnov test. Because not all parameters were normally distributed, we used the Wilcoxon rank-sum test for comparison of paired data (radiographic parameters, ROM, Merle d’Aubigné score). Categorical data (eg, presence of a crossover sign) were compared with Fisher’s exact test. The Tönnis score [66] was compared with the chi square test. The 13 previously defined MRA-based factors were tested for an association with failure and calculation was performed with the multivariate Cox proportional model with hazard ratios (HRs) [12]. HRs were calculated with 95% confidence intervals (CIs). Failures were defined as: conversion to THA, any radiographic progression of osteoarthritis, and a poor or fair HHS at last followup (defined as HHS < 80 points [40]). Twenty-one of 65 hips (32%) reached an endpoint of failure. Nine hips (14%) were converted to a THA after a mean of 5 ± 2 (range, 3–9 years). Five hips (8%) showed progression of osteoarthritis during the followup period. Seven hips (11%) showed a HHS of < 80 points during the followup period. This resulted in a cumulative 10-year survivorship of 73% (95% CI, 62%-84%). We used box plots to visualize the temporal relationship of the 13 evaluated parameters for all patients. Factors were sorted according to the lower quartile of the age of patients when these factors were detected for the first time on preoperative MRAs.
Results
The following MRA-based findings were associated with one or more of our predefined failure endpoints: cartilage damage exceeding 60° of the circumference (HR, 4.6; 95% CI, 3.6–5.6), presence of an acetabular rim bone cyst (HR, 4.1; 95% CI, 3.1–5.2), and presence of a sabertooth osteophyte (HR, 3.2; 95% CI, 2.3–4.2; Table 4).
Table 4.
Predictive factors for failure* with corresponding hazard ratios
| Parameters | Prevalence of the parameter in all patients that failed (%) | Prevalence of parameter in all patients without failure (%) | p value | Hazard ratio (95% confidence interval) | p value | Adjusted hazard ratio (95% confidence interval) |
p value |
|---|---|---|---|---|---|---|---|
| Cockscomb osteophyte | 33 | 20 | 0.260 | 2.0 (1.1–2.9) | 0.146 | ||
| Posteroinferior osteophyte | 43 | 16 | 0.018 | 3.2 (2.4–4.1) | 0.008 | ||
| Perifoveolar osteophyte | 24 | 5 | 0.019 | 3.9 (2.9–5.0) | 0.010 | ||
| Herniation pit | 29 | 23 | 0.609 | 1.4 (0.4–2.3) | 0.534 | ||
| Sabertooth osteophyte | 43 | 9 | 0.001 | 4.0 (3.1–4.9) | 0.002 | 3.2 (2.3–4.2) | 0.013 |
| Cartilage damage exceeding 60° of the circumference | 38 | 5 | < 0.001 | 4.8 (3.9–5.7) | 0.001 | 4.6 (3.6–5.6) | 0.003 |
| Femoral head decentration | 43 | 20 | 0.059 | 2.3 (1.4–3.2) | 0.061 | ||
| Labral damage exceeding 120° of the circumference | 81 | 41 | 0.002 | 4.3 (3.2–5.4) | 0.009 | ||
| Intralabral cyst | 29 | 20 | 0.468 | 1.1 (0.2–2.1) | 0.795 | ||
| Paralabral cyst | 43 | 14 | 0.009 | 3.4 (2.5–4.2) | 0.007 | ||
| Acetabular rim bone cyst | 48 | 25 | 0.068 | 2.2 (1.4–3.1) | 0.066 | 4.1 (3.1–5.2) | 0.008 |
| Acetabular center bone cyst | 24 | 32 | 0.508 | 0.7 (-0.3–1.7) | 0.557 | ||
| Acetabular rim osteophyte | 67 | 43 | 0.077 | 2.4 (1.5–3.3) | 0.060 |
Values are expressed as mean with 95% confidence interval; *a failure was defined by the following endpoints at 10-year followup: THA, radiographic progression of osteoarthritis, and/or Harris hip score < 80 points.
The multivariate factor associated with one of the endpoints occurring at the youngest patient age was the sabertooth osteophyte (lower quartile 27 years) followed by the cartilage damage exceeding 60° of the circumference (28 years) and the presence of an acetabular rim bone cyst (31 years; Fig. 3).
Fig. 3.
The age of the patient for each of the 13 degenerative patterns found in the preoperative MRA is shown. Factors were sorted according to their chronologic appearance of the lower quartile. Multivariate parameters are represented with a black box, univariate parameters with a gray box, and factors not associated with the endpoints (conversion to THA, any progression of osteoarthritis, HHS < 80) with a white box.
Discussion
Although MRI has become a standard imaging method in the diagnostic workup of patients with FAI, which degenerative findings on MRA are associated with inferior outcomes after surgery for FAI has not been fully explored. The aims of this study were (1) to identify the preoperative MRA findings associated with conversion to arthroplasty, radiographic evidence of any progression of osteoarthritis, and/or a HHS of < 80 points after acetabuloplasty or osteochondroplasty of the femoral head-neck junction for FAI at a minimum followup of 10 years; and (2) identify the age of patients with symptomatic FAI when these secondary degenerative findings were detected on preoperative radial MRAs.
We found that hips with a sabertooth osteophyte, cartilage damage exceeding 60° of the circumference, and an acetabular rim bone cyst will be more likely to have poorer hip scores, progressive arthritis, and conversion to THA.
This study has several limitations. First, we did not have serial MRAs to longitudinally study the degenerative cascade of the hip. We described the age of the patients when the degenerative patterns occurred on the preoperative MRA. This clearly does not represent the first moment when one of these degenerative patterns could be identified on the MRA. However, it may still allow one to detect early occurring degenerative patterns (Fig. 3) and this information allows the surgeon to identify hips at risk. Second, we are unable to specify our results for the different subgroups of FAI. Because the overall study population was already relatively small, the number of patients with isolated pincer- and cam-type FAI in our cohort was simply too small for sufficient statistical power for further analysis. Third, we specifically focused on MRA parameters only and did not examine other variables such as demographic variables in the regression analysis. Nevertheless, the cartilage damage detected on the preoperative MRA remains associated with inferior results even when all potential factors are considered in the analysis [61, 62]. This emphasizes the validity of our results. Fourth, the techniques for diagnosing and treating patients with FAI have changed slightly over the observation period. This includes mainly the use of a step-cut osteotomy, the offset correction with a high-speed burr, the implementation of femoral torsion in the FAI concept, and more restrictive indications for FAI procedures based on the preoperative Tönnis osteoarthritis score on conventional radiographs.
We identified three preoperative MR arthrographic findings associated with poorer long-term prognosis after acetabuloplasty and/or osteochondroplasty of the femoral head-neck junction in hips with FAI (Table 4). Many of the identified degenerative factors often occur together (Table 5). The most commonly found associations were between the sabertooth osteophyte and the labral damage, and between the perifoveolar osteophyte and the labral damage. The provided values (Table 5) can be interpreted as follows: for example, if a sabertooth osteophyte was present, a concomitant labral lesion exceeding 120° was found in 92% of these hips. Comparing our results with those of others, all except three MRI studies [27, 30, 46] evaluating potential findings that are associated with unfavorable outcome after FAI surgery refer only to demographic, intraoperative, or conventional radiographic factors (Table 6). None of these three studies evaluate the predictive value of MRA parameters in long-term followup. Similar to our observations, Larson et al. [30] found an association of an increasing MRI chondral damage grade with poorer clinical scores at a mean followup of 2.3 years. In contrast, Nabavi et al. [46] found no association of chondrolabral damage and lower clinical scores at 1-year followup. Krych et al. [27] found an association of subchondral edema with cystic change and poorer clinical scores at a minimum followup of 2 years. Most of these studies report their initial experience with surgical treatment for FAI, which typically included hips with joint space narrowing or advanced stages of osteoarthritis [6, 30, 31, 53, 59]. Meanwhile, there is now general consensus that radiographic osteoarthritis > Tönnis Grade 1 is a relative contraindication for surgery [61, 62]. We can provide further findings that are associated with an unfavorable outcome in cases without obvious signs of osteoarthritis on conventional radiographs based on radial MRA of the hip. These findings represent the basis for future controlled studies evaluating the outcome of contemporary treatment of patients with FAI.
Table 5.
The prevalence of combinations of two morphological features is shown*
| Numerator | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Parameter | Cockscomb osteophyte | Posteroinferior osteophyte | Perifoveolar osteophyte | Herniation pit | Sabertooth osteophyte | Cartilage damage† | Femoral head decentration | Labral damage‡ | Intralabral cyst | Paralabral cyst | Acetabular rim bone cyst | Acetabular center bone cyst | Acetabular rim osteophyte | |
| Denominator | Cockscomb osteophyte | – | 31% | 14% | 11% | 17% | 17% | 23% | 31% | 11% | 14% | 20% | 20% | 29% |
| Posteroinferior osteophyte | 69% | – | 31% | 38% | 44% | 25% | 50% | 75% | 19% | 44% | 44% | 31% | 69% | |
| Perifoveolar osteophyte | 71% | 71% | – | 29% | 57% | 57% | 71% | 86% | 29% | 71% | 43% | 57% | 57% | |
| Herniation pit | 25% | 38% | 13% | – | 31% | 13% | 44% | 69% | 38% | 13% | 56% | 44% | 69% | |
| Sabertooth osteophyte | 46% | 54% | 31% | 38% | – | 31% | 69% | 92% | 38% | 46% | 46% | 31% | 62% | |
| Cartilage damage† | 60% | 40% | 40% | 20% | 40% | – | 70% | 80% | 40% | 50% | 60% | 50% | 70% | |
| Femoral head decentration | 44% | 44% | 28% | 39% | 50% | 39% | – | 78% | 28% | 33% | 67% | 56% | 56% | |
| Labral damage‡ | 31% | 34% | 17% | 31% | 34% | 23% | 40% | – | 20% | 31% | 46% | 26% | 63% | |
| Intralabral cyst | 27% | 20% | 13% | 40% | 33% | 27% | 33% | 47% | – | 40% | 47% | 27% | 40% | |
| Paralabral cyst | 33% | 47% | 33% | 13% | 40% | 33% | 40% | 73% | 40% | – | 60% | 40% | 53% | |
| Acetabular rim bone cyst | 33% | 33% | 14% | 43% | 29% | 29% | 57% | 76% | 33% | 43% | – | 57% | 71% | |
| Acetabular center bone cyst | 37% | 26% | 21% | 37% | 21% | 26% | 53% | 47% | 21% | 32% | 63% | – | 53% | |
| Acetabular rim osteophyte | 30% | 33% | 12% | 33% | 24% | 21% | 30% | 67% | 18% | 24% | 45% | 30% | – | |
* For example, in all hips presenting with a sabertooth osteophyte (denominator), labral damage exceeding 120° of the circumference (numerator) was present in 92%; †cartilage damage exceeding 60° of the circumference; ‡labral damage exceeding 120° of the circumference.
Table 6.
Overview of the literature with negative predictive factors for FAI surgery
| Author, year | Type of treatment | Negative predictive features | Number of hips (patients) | Followup (years) | Endpoints | Study type |
|---|---|---|---|---|---|---|
| Murphy et al., 2004 [43] | SHD ± intertrochanteric/periacetabular osteotomy | Untreated dysplasia, subluxation caused by osteophytes | 22 | 5.2 (2–12) | THA | Case series |
| Beck et al., 2004 [6] | SHD | Osteoarthritis > Grade 2 [69], extensive articular cartilage damage (intraoperatively) | 19 | 4.7 (4–5) | THA, OA progression | Case series |
| Beaulé et al., 2007 [4] | SHD | No correlation of cartilage damage with clinical outcome | 37 | 3.1 (2–5) | WOMAC, UCLA activity score, SF-12 | Case series |
| Laude et al., 2009 [31] | Miniopen anterior approach + arthroscopy | Age > 40 years, depth of cartilage lesion, full-thickness cartilage defect | 100 | 4.9 (2–9) | THA | Case series |
| Philippon et al., 2009 [53] | Arthroscopy | Preoperative HHS < 47, joint space narrowing < 2 mm, labral débridement | 122 (122) | 2.3 (2–3) | mHHS | Case series |
| Peters et al., 2010 [52] | SHD | Cartilage damage > Outerbridge IV (trend) | 96 (94) | 2.2 (2–8) | OA progression, THA, lower HHS than preoperatively; | Case series |
| Haviv et al., 2010 [22] | Arthroscopy | Older patients with higher grade of cartilage lesions | 170 (166) | 1.8 (1–6) | mHHS, NAHS | Case series |
| Larson et al., 2011 [30] | Arthroscopy | > 50% joint space narrowing or ≤ 2 mm joint space, chondral lesions (MRI), symptom duration | I: 169 (154) II: 58 (56) |
2.3 (1–5) | HHS | Case-control |
| Meftah et al., 2011 [41] | Arthroscopy | Osteoarthritis | 50 (50) | 8.4 (7–14) | HHS | Case series |
| Naal et al., 2012 [45] | SHD | Women, age > 29 years, low BMI, advanced osteoarthritis (trend) | 233 (185) | 5.0 (2–10) | THA, dissatisfaction | Case series |
| Larson et al., 2012 [29] | Arthroscopy | Labral débridement | I: 44 (42) II: 50 (48) | 3.5 (2–6) | HHS < 70, THA, SHD | Case-control |
| Palmer et al., 2012 [50] | Arthroscopy | Advanced osteoarthritis (Grade 4 chondral defect) | 201 (185) | 3.8 | THA | Case series |
| Steppacher et al., 2014 [62] | SHD | Age > 40 years, weight > 90 kg, BMI > 25 kg/m2, anterior femoral coverage < 15%, OA ≥ Grade 1 [69] | 97 (75) | 6.0 (5–7) | THA, OA progression, MdA < 15 | Case series |
| Skendzel et al., 2014 [59] | Arthroscopy | Joint space ≤ 2 mm, women, age | I: (383) II: (63) |
6.1 (5–8) | THA | Cohort study |
| Steppacher et al., 2015 [61] | SHD | Age > 40 years, weight > 100 kg, BMI > 30 kg/m2, anterior femoral coverage < 15%, OA ≥ 1 [69] | 97 (75) | 11.0 (10–13) | THA, OA progression, MdA < 15 | Case series |
| Peters et al., 2015 [51] | SHD | Age | 142 (142) | 3.0 (1–12) | THA, increase of mHHS < 20 points | Case series |
| Nabavi et al., 2015 [46] | Arthroscopy | Elevated BMI, workers’ compensation patient | 280 (253) | 1.0 | Increase of mHHS or NAHS < 20 points | Case series |
| Krych et al., 2016 [27] | Arthroscopy | Subchondral edema with an acetabular cyst on MRI | NA (104) | NA (2–5) | THA, abnormal or severe abnormal HOS-ADL | Case-control |
| Hufeland et al., 2016 [23] | Arthroscopy | Age, advanced osteoarthritis | NA (44) | 5.5 (4–7) | THA | Case series |
FAI = femoroacetabular impingement; SHD = surgical hip dislocation; OA = osteoarthritis; BMI = body mass index; HHS = Harris hip score; mHHS = modified Harris hip score; NAHS = nonarthritis hip score; HOS-ADL = hip outcome score–activities of daily living; MdA = Merle d’Aubigné-Postel score; NA = not applicable.
In young patients, the first multivariate finding that was associated with unfavorable outcome was the sabertooth osteophyte followed by cartilage damage exceeding 60° of the circumference and the presence of an acetabular rim bone cyst (Fig. 3). Hips presenting with these three signs can be considered as “hips at risk”. Routine evaluation of preoperative MRA should therefore include an explicit statement about the presence or absence of these factors. The breakdown of the evaluated degenerative factors according to the patient age at the time of preoperative MRA reflects in some part the suggested osteoarthritis cascade [10]. Generally, soft tissue alterations such as chondrolabral lesions or cysts occur earlier in the cascade (Fig. 2). Once a chondrolabral separation is present, the high joint pressure maintained by the labrum forces synovial fluid through the chondrolabral separation [15]. This can then result in intralabral ganglia or even intraosseous cysts at the acetabular rim. With complete separation of the labrum from the acetabular rim, paralabral cysts can subsequently occur. A loss of the labral attachment reportedly leads to a loss of the protective suction seal [15] resulting in more advanced cartilage damage. Eventually, subtle osteophytes then occur at the femoral neck (cockscomb-type, posteroinferior), medial femoral head (perifoveolar), or the acetabular fossa (sabertooth osteophyte), which are often difficult to detect on conventional radiographs. We found that many of the degenerative factors noted have been present even in patients with Tönnis Grade 0 osteoarthritis on conventional radiographs (Table 7). For example, 44% of all hips with Tönnis Grade 0 presented with an acetabular rim osteophyte, which was not visible on conventional radiographs (Table 7). Thirty percent of hips with Tönnis Grade 0 had an acetabular rim bone cyst, which was identified as a multivariate factor in our analysis.
Table 7.
Prevalence of the evaluated MRA-based degenerative factors based on the Tönnis osteoarthritis score with conventional radiographs
| Parameter | Tönnis Grade 0 | Tönnis Grade > 0 | p value |
|---|---|---|---|
| Cockscomb osteophyte | 18% | 47% | 0.024 |
| Posteroinferior osteophyte | 16% | 53% | 0.006 |
| Perifoveolar osteophyte | 6% | 27% | 0.044 |
| Herniation pit | 20% | 40% | 0.115 |
| Sabertooth osteophyte | 12% | 47% | 0.007 |
| Cartilage damage* | 12% | 26% | 0.167 |
| Femoral head decentration | 22% | 47% | 0.061 |
| Labral damage† | 44% | 87% | 0.003 |
| Intralabral cyst | 20% | 33% | 0.282 |
| Paralabral cyst | 16% | 47% | 0.013 |
| Acetabular rim bone cyst | 30% | 40% | 0.851 |
| Acetabular center bone cyst | 28% | 33% | 0.768 |
| Acetabular rim osteophyte | 44% | 73% | 0.044 |
* Cartilage damage exceeding 60° of the circumference; †labral damage exceeding 120° of the circumference; MRA = magnetic resonance arthrogram.
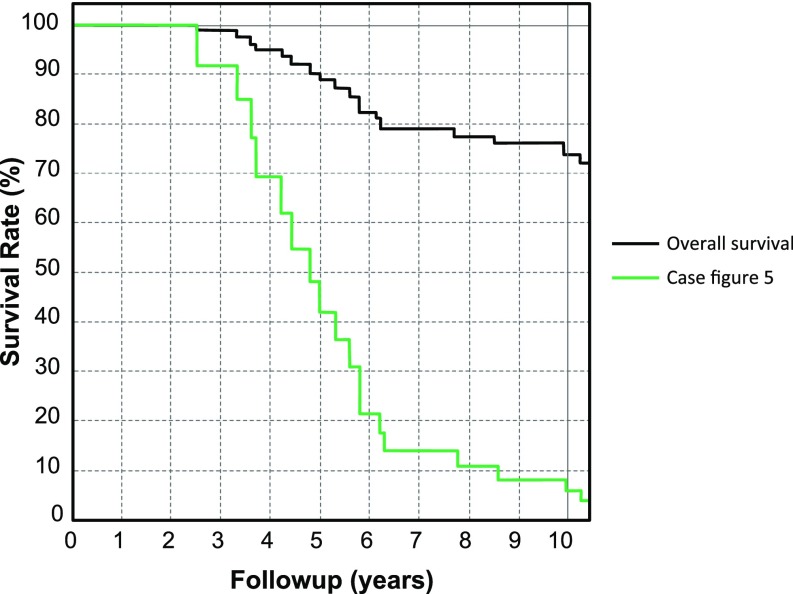
The findings that are associated with unfavorable outcomes from our study can be used in clinical practice as a helpful adjunct for decision-making. The prerequisite for this is the availability of radial MRA sequences [60]. Many of the factors are generally not visible on conventional radiographs or standard hip/pelvis MRIs [34]. Patients with FAI, who are typically very high-functioning [39], should be informed if one or more of the degenerative patterns associated with poor outcome are present because this may negatively influence the result of hip-preserving surgery. The multivariate findings that are associated with unfavorable outcome may help establish a prognosis in patients scheduled for surgical treatment of FAI (Fig. 4). As an illustrative example, a 32-year-old patient with symptomatic mixed-type FAI is presented (Figs. 5, 6). Although the conventional radiographs do not reveal any classic signs of osteoarthritis (Fig. 5A–B), the radial MRI sequences show seven distinct secondary alterations (Fig. 5C), two of them matching our multivariate findings that are associated with an unfavorable outcome. The individual prognostic curve for the patient’s hip (Fig. 6) drops substantially. This correlates with the radiographic and clinical followup 5 years after femoral-neck osteochondroplasty and acetabuloplasty through SHD with superior joint space narrowing on the AP pelvis radiograph, osteophyte formation, and a HHS of < 80 points.
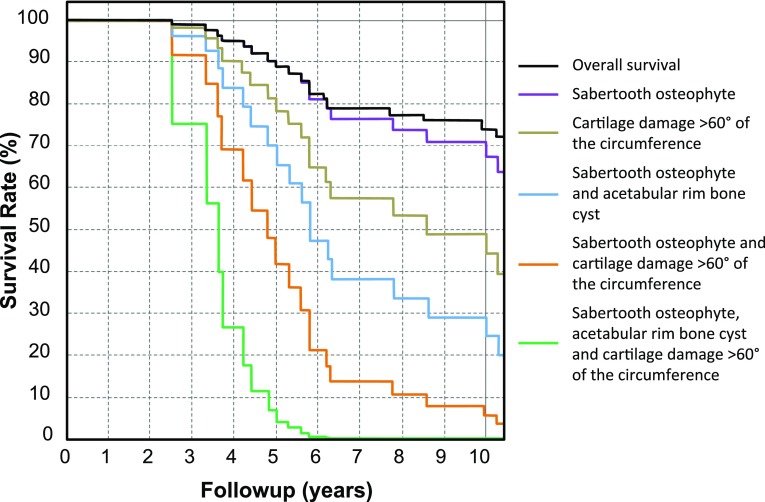
Fig. 4.
Survival of the hip is shown with the endpoints defined as conversion to THA, any progression of osteoarthritis, or a HHS of < 80. Survival is associated with different endpoints or a combination of them: sabertooth osteophyte, a cartilage damage exceeding 60° of the circumference, and an acetabular rim bone cyst.
Fig. 5A–C.
(A) This figure shows the preoperative (left), postoperative (middle), and followup radiographs (right) of a 32-year-old patient with symptomatic mixed-type FAI as a result of a pistol grip deformity (white arrow) and slight acetabular retroversion. There is no evidence of osteoarthritis on the preoperative radiograph (left). The postoperative radiograph (middle) shows a good correction (gray arrow) of the femoral head-neck junction and the acetabular rim with labral refixation. The followup radiographs 5 years after surgery (right) show superolateral joint space narrowing and the new formation of an acetabular rim osteophyte (black arrow) as signs of osteoarthritis progression. Furthermore, the patient presented with a HHS of < 80 points. (B) The corresponding axial radiographs are shown. (C) The preoperative MRI shows a beginning posteroinferior osteophyte (white arrow), cockscomb osteophyte (black arrow), beginning sabertooth osteophyte (gray arrow), perifoveolar osteophyte (white double arrow), cartilage lesion (gray double arrow), a labral lesion (black double arrow), and a femoral head decentration (white triple arrow).
Fig. 6.
Overall survival and specific survival of a patient (Fig. 5) with the following endpoints associated with inferior outcome (conversion to THA, any progression of osteoarthritis, and a HHS < 80): a sabertooth osteophyte and a cartilage lesion exceeding 60° of the circumference.
In summary, preoperative MR arthrography with radial cuts revealed important findings that are associated with unfavorable outcomes in long-term followup of surgical treatment for FAI. Most of these factors are not visible on conventional radiographs. Preoperative MRA evaluation is therefore strongly recommended on a routine basis. The findings that are associated with unfavorable outcome from our study should be incorporated in the decision-making process in patients considering joint-preserving hip surgery: cartilage lesions exceeding 60° of the circumference of the acetabulum and the presence of a sabertooth osteophyte or an acetabular rim bone cyst, especially when occurring at age younger than 30 years.
Acknowledgments
We thank Joseph M. Schwab, Department of Orthopaedic Surgery, Medical College of Wisconsin, for his linguistic help in the preparation of the manuscript and critical reviewing.
Footnotes
One of the authors (MT) has received funding from the Swiss National Science Foundation (SNSF, project number PP00P3_144856).
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research ® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
Each author certifies that his or her institution has approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at the University of Bern, Bern, Switzerland.
A comment to this article is available at http://dx.doi.org/10.1007/s11999-016-5085-8.
An erratum to this article is available at http://dx.doi.org/10.1007/s11999-016-5075-x.
References
- 1.Altman DG. Practical Statistics for Medical Research. London, UK: Chapman & Hall/CRC; 1991. [Google Scholar]
- 2.Anderson SE, Siebenrock KA, Mamisch TC, Tannast M. Femoroacetabular impingement magnetic resonance imaging. Top Magn Reson Imaging. 2009;20:123–128. doi: 10.1097/RMR.0b013e3181d99459. [DOI] [PubMed] [Google Scholar]
- 3.d’Aubigné RM, Postel M. Functional results of hip arthroplasty with acrylic prosthesis. J Bone Joint Surg Am. 1954;36:451–475. [PubMed]
- 4.Beaulé PE, Le Duff MJ, Zaragoza E. Quality of life following femoral head-neck osteochondroplasty for femoroacetabular impingement. J Bone Joint Surg Am. 2007;89:773–779. doi: 10.2106/JBJS.F.00681. [DOI] [PubMed] [Google Scholar]
- 5.Beck M, Kalhor M, Leunig M, Ganz R. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br. 2005;87:1012–1018. doi: 10.1302/0301-620X.87B7.15203. [DOI] [PubMed] [Google Scholar]
- 6.Beck M, Leunig M, Parvizi J, Boutier V, Wyss D, Ganz R. Anterior femoroacetabular impingement: part II. Midterm results of surgical treatment. Clin Orthop Relat Res. 2004;418:67–73. doi: 10.1097/00003086-200401000-00012. [DOI] [PubMed] [Google Scholar]
- 7.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15:1833–1840. [PubMed] [Google Scholar]
- 8.Blankenbaker DG, De Smet AA, Keene JS, Fine JP. Classification and localization of acetabular labral tears. Skeletal Radiol. 2007;36:391–397. doi: 10.1007/s00256-006-0240-z. [DOI] [PubMed] [Google Scholar]
- 9.Brückl L. [Congenital deformity of the hip joint] [in German] In: Jäger M, Wirth CJ, eds. Praxis der Orthopädie. Stuttgart, Germany: Georg Thieme Verlag; 1998.
- 10.Carty F, Crosbie I, Ryan J, Cashman J. Imaging of the acetabular labrum: a review. Hard Tissue. 2013;22:9. [Google Scholar]
- 11.Corten K, Ganz R, Chosa E, Leunig M. Bone apposition of the acetabular rim in deep hips: a distinct finding of global pincer impingement. J Bone Joint Surg Am. 2011;93(Suppl 2):10–16. doi: 10.2106/JBJS.J.01799. [DOI] [PubMed] [Google Scholar]
- 12.Cox R. Regression models and life tables. J R Stat Soc B. 1972;34:187–220. [Google Scholar]
- 13.Czerny C, Hofmann S, Neuhold A, Tschauner C, Engel A, Recht MP, Kramer J. Lesions of the acetabular labrum: accuracy of MR imaging and MR arthrography in detection and staging. Radiology. 1996;200:225–230. doi: 10.1148/radiology.200.1.8657916. [DOI] [PubMed] [Google Scholar]
- 14.Dougados M, Gueguen A, Nguyen M, Berdah L, Lequesne M, Mazieres B, Vignon E. Radiological progression of hip osteoarthritis: definition, risk factors and correlations with clinical status. Ann Rheum Dis. 1996;55:356–362. doi: 10.1136/ard.55.6.356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ferguson SJ, Bryant JT, Ganz R, Ito K. An in vitro investigation of the acetabular labral seal in hip joint mechanics. J Biomech. 2003;36:171–178. doi: 10.1016/S0021-9290(02)00365-2. [DOI] [PubMed] [Google Scholar]
- 16.Gandek B, Ware JE, Aaronson NK, Apolone G, Bjorner JB, Brazier JE, Bullinger M, Kaasa S, Leplege A, Prieto L, Sullivan M. Cross-validation of item selection and scoring for the SF-12 Health Survey in nine countries: results from the IQOLA Project. International Quality of Life Assessment. J Clin Epidemiol. 1998;51:1171–1178. doi: 10.1016/S0895-4356(98)00109-7. [DOI] [PubMed] [Google Scholar]
- 17.Ganz R, Gill TJ, Gautier E, Ganz K, Krügel N, Berlemann U. Surgical dislocation of the adult hip a technique with full access to the femoral head and acetabulum without the risk of avascular necrosis. J Bone Joint Surg Br. 2001;83:1119–1124. doi: 10.1302/0301-620X.83B8.11964. [DOI] [PubMed] [Google Scholar]
- 18.Gao Z, Yin J, Ma L, Wang J, Meng Q. Clinical imaging characteristics of herniation pits of the femoral neck. Orthop Surg. 2009;1:189–195. doi: 10.1111/j.1757-7861.2009.00029.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Glynn AA, Barattiero FY, Albers CE, Hanke MS, Steppacher SD, Tannast M. Surgical hip dislocation does not result in atrophy or fatty infiltration of periarticular hip muscles. J Hip Preserv Surg. 2014;1:82–95. doi: 10.1093/jhps/hnu008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51:737–755. doi: 10.2106/00004623-196951040-00012. [DOI] [PubMed] [Google Scholar]
- 21.Harrison MH, Schajowicz F, Trueta J. Osteoarthritis of the hip: a study of the nature and evolution of the disease. J Bone Joint Surg Br. 1953;35:598–626. doi: 10.1302/0301-620X.35B4.598. [DOI] [PubMed] [Google Scholar]
- 22.Haviv B, Singh PJ, Takla A, O’Donnell J. Arthroscopic femoral osteochondroplasty for cam lesions with isolated acetabular chondral damage. J Bone Joint Surg Br. 2010;92:629–633. doi: 10.1302/0301-620X.92B5.23667. [DOI] [PubMed] [Google Scholar]
- 23.Hufeland M, Krüger D, Haas NP, Perka C, Schröder JH. Arthroscopic treatment of femoroacetabular impingement shows persistent clinical improvement in the mid-term. Arch Orthop Trauma Surg. 2016;136:687–691. doi: 10.1007/s00402-016-2427-7. [DOI] [PubMed] [Google Scholar]
- 24.Idelberger K, Frank A. A new method for determination of the angle of the pelvic acetabulum in child and in adult [in German] Z Für Orthop Ihre Grenzgeb. 1952;82:571–577. [PubMed] [Google Scholar]
- 25.Jeffery AK. Osteophytes and the osteoarthritic femoral head. J Bone Joint Surg Br. 1975;57:314–324. [PubMed] [Google Scholar]
- 26.Kalberer F, Sierra RJ, Madan SS, Ganz R, Leunig M. Ischial spine projection into the pelvis: a new sign for acetabular retroversion. Clin Orthop Relat Res. 2008;466:677–683. doi: 10.1007/s11999-007-0058-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Krych AJ, King AH, Berardelli RL, Sousa PL, Levy BA. Is subchondral acetabular edema or cystic change on MRI a contraindication for hip arthroscopy in patients with femoroacetabular impingement? Am J Sports Med. 2016;44:454–459. doi: 10.1177/0363546515612448. [DOI] [PubMed] [Google Scholar]
- 28.Kubo T, Horii M, Harada Y, Noguchi Y, Yutani Y, Ohashi H, Hachiya Y, Miyaoka H, Naruse S, Hirasawa Y. Radial-sequence magnetic resonance imaging in evaluation of acetabular labrum. J Orthop Sci. 1999;4:328–332. doi: 10.1007/s007760050112. [DOI] [PubMed] [Google Scholar]
- 29.Larson CM, Giveans MR, Stone RM. Arthroscopic débridement versus refixation of the acetabular labrum associated with femoroacetabular impingement: mean 3.5-year follow-up. Am J Sports Med. 2012;40:1015–1021. doi: 10.1177/0363546511434578. [DOI] [PubMed] [Google Scholar]
- 30.Larson CM, Giveans MR, Taylor M. Does arthroscopic FAI correction improve function with radiographic arthritis? Clin Orthop Relat Res. 2011;469:1667–1676. doi: 10.1007/s11999-010-1741-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Laude F, Sariali E, Nogier A. Femoroacetabular impingement treatment using arthroscopy and anterior approach. Clin Orthop Relat Res. 2009;467:747–752. doi: 10.1007/s11999-008-0656-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ledingham J, Dawson S, Preston B, Milligan G, Doherty M. Radiographic progression of hospital referred osteoarthritis of the hip. Ann Rheum Dis. 1993;52:263–267. doi: 10.1136/ard.52.4.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Leunig M, Werlen S, Ungersböck A, Ito K, Ganz R. Evaluation of the acetabular labrum by MR arthrography. J Bone Joint Surg Br. 1997;79:230–234. doi: 10.1302/0301-620X.79B2.7288. [DOI] [PubMed] [Google Scholar]
- 34.Locher S, Werlen S, Leunig M, Ganz R. MR-Arthrography with radial sequences for visualization of early hip pathology not visible on plain radiographs [in German] Z Für Orthop Ihre Grenzgeb. 2002;140:52–57. doi: 10.1055/s-2002-22122. [DOI] [PubMed] [Google Scholar]
- 35.Madadi F, Yazdanshenas H, Madadi F, Bazargan-Hejazi S. Double acetabular wall—a misleading point for hip arthroplasty: an anatomical, radiological, clinical study. Int Orthop. 2013;37:1007–1011. doi: 10.1007/s00264-013-1780-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Magee T, Hinson G. Association of paralabral cysts with acetabular disorders. AJR Am J Roentgenol. 2000;174:1381–1384. doi: 10.2214/ajr.174.5.1741381. [DOI] [PubMed] [Google Scholar]
- 37.Magerkurth O, Jacobson JA, Girish G, Brigido MK, Bedi A, Fessell D. Paralabral cysts in the hip joint: findings at MR arthrography. Skeletal Radiol. 2012;41:1279–1285. doi: 10.1007/s00256-012-1395-4. [DOI] [PubMed] [Google Scholar]
- 38.Mamisch TC, Werlen S, Zilkens C, Trattnig S, Kim Y-J, Siebenrock KA, Bittersohl B. Radiological diagnosis of femoroacetabular impingement [in German] Radiololge. 2009;49:425–433. doi: 10.1007/s00117-009-1833-z. [DOI] [PubMed] [Google Scholar]
- 39.Mannion AF, Impellizzeri FM, Naal FD, Leunig M. Fulfillment of patient-rated expectations predicts the outcome of surgery for femoroacetabular impingement. Osteoarthritis Cartilage. 2013;21:44–50. doi: 10.1016/j.joca.2012.09.013. [DOI] [PubMed] [Google Scholar]
- 40.Marchetti P, Benazir R, Vaccari V, Girolami M, Morici F, Impallomeni C, Commessatti M, Silvello L. Long-term results with cementless Fitek (or Fitmore) cups. J Arthroplasty. 2005;20:730–737. doi: 10.1016/j.arth.2004.11.019. [DOI] [PubMed] [Google Scholar]
- 41.Meftah M, Rodriguez JA, Panagopoulos G, Alexiades MM. Long-term results of arthroscopic labral débridement: predictors of outcomes. Orthopedics. 2011;34:e588–e592. doi: 10.3928/01477447-20110826-04. [DOI] [PubMed] [Google Scholar]
- 42.Mofidi A, Shields JS, Stubbs AJ. Central acetabular osteophyte (saber tooth sign), one of the earliest signs of osteoarthritis of the hip joint. Eur J Orthop Surg Traumatol. 2010;21:71–74. doi: 10.1007/s00590-010-0663-z. [DOI] [Google Scholar]
- 43.Murphy S, Tannast M, Kim Y-J, Buly R, Millis MB. Débridement of the adult hip for femoroacetabular impingement: indications and preliminary clinical results. Clin Orthop Relat Res. 2004;429:178–181. doi: 10.1097/01.blo.0000150307.75238.b9. [DOI] [PubMed] [Google Scholar]
- 44.Murphy SB, Ganz R, Müller ME. The prognosis in untreated dysplasia of the hip. A study of radiographic factors that predict the outcome. J Bone Joint Surg Am. 1995;77:985–989. doi: 10.2106/00004623-199507000-00002. [DOI] [PubMed] [Google Scholar]
- 45.Naal FD, Miozzari HH, Schär M, Hesper T, Nötzli HP. Midterm results of surgical hip dislocation for the treatment of femoroacetabular impingement. Am J Sports Med. 2012;40:1501–1510. doi: 10.1177/0363546512445884. [DOI] [PubMed] [Google Scholar]
- 46.Nabavi A, Olwill CM, Harris IA. Preoperative predictors of outcome in the arthroscopic treatment of femoroacetabular impingement. Hip Int. 2015;25:402–405. doi: 10.5301/hipint.5000261. [DOI] [PubMed] [Google Scholar]
- 47.Neuman P, Hulth A, Lindén B, Johnell O, Dahlberg L. The role of osteophytic growth in hip osteoarthritis. Int Orthop. 2003;27:262–266. doi: 10.1007/s00264-003-0485-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Nokes SR, Vogler JB, Spritzer CE, Martinez S, Herfkens RJ. Herniation pits of the femoral neck: appearance at MR imaging. Radiology. 1989;172:231–234. doi: 10.1148/radiology.172.1.2740509. [DOI] [PubMed] [Google Scholar]
- 49.Nötzli HP, Wyss TF, Stoecklin CH, Schmid MR, Treiber K, Hodler J. The contour of the femoral head-neck junction as a predictor for the risk of anterior impingement. J Bone Joint Surg Br. 2002;84:556–560. doi: 10.1302/0301-620X.84B4.12014. [DOI] [PubMed] [Google Scholar]
- 50.Palmer DH, Ganesh V, Comfort T, Tatman P. Midterm outcomes in patients with cam femoroacetabular impingement treated arthroscopically. Arthroscopy. 2012;28:1671–1681. doi: 10.1016/j.arthro.2012.04.154. [DOI] [PubMed] [Google Scholar]
- 51.Peters CL, Anderson LA, Diaz-Ledezma C, Anderson MB, Parvizi J. Does the nature of chondrolabral injury affect the results of open surgery for femoroacetabular impingement? Clin Orthop Relat Res. 2015;473:1342–1348. doi: 10.1007/s11999-014-4039-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Peters CL, Schabel K, Anderson L, Erickson J. Open treatment of femoroacetabular impingement is associated with clinical improvement and low complication rate at short-term followup. Clin Orthop Relat Res. 2010;468:504–510. doi: 10.1007/s11999-009-1152-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Philippon MJ, Briggs KK, Yen Y-M, Kuppersmith DA. Outcomes following hip arthroscopy for femoroacetabular impingement with associated chondrolabral dysfunction: minimum two-year follow-up. J Bone Joint Surg Br. 2009;91:16–23. doi: 10.1302/0301-620X.91B1.21329. [DOI] [PubMed] [Google Scholar]
- 54.Pitt MJ, Graham AR, Shipman JH, Birkby W. Herniation pit of the femoral neck. AJR Am J Roentgenol. 1982;138:1115–1121. doi: 10.2214/ajr.138.6.1115. [DOI] [PubMed] [Google Scholar]
- 55.Register B, Pennock AT, Ho CP, Strickland CD, Lawand A, Philippon MJ. Prevalence of abnormal hip findings in asymptomatic participants: a prospective, blinded study. Am J Sports Med. 2012;40:2720–2724. doi: 10.1177/0363546512462124. [DOI] [PubMed] [Google Scholar]
- 56.Reynolds D, Lucas J, Klaue K. Retroversion of the acetabulum. A cause of hip pain. J Bone Joint Surg Br. 1999;81:281–288. doi: 10.1302/0301-620X.81B2.8291. [DOI] [PubMed] [Google Scholar]
- 57.Riley GM, McWalter EJ, Stevens KJ, Safran MR, Lattanzi R, Gold GE. MRI of the hip for the evaluation of femoroacetabular impingement; past, present, and future. J Magn Reson. Imaging. 2015;41:558–572. doi: 10.1002/jmri.24725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Schmid MR, Nötzli HP, Zanetti M, Wyss TF, Hodler J. Cartilage lesions in the hip: diagnostic effectiveness of MR arthrography. Radiology. 2003;226:382–386. doi: 10.1148/radiol.2262020019. [DOI] [PubMed] [Google Scholar]
- 59.Skendzel JG, Philippon MJ, Briggs KK, Goljan P. The effect of joint space on midterm outcomes after arthroscopic hip surgery for femoroacetabular impingement. Am J Sports Med. 2014;42:1127–1133. doi: 10.1177/0363546514526357. [DOI] [PubMed] [Google Scholar]
- 60.Stelzeneder D, Mamisch TC, Kress I, Domayer SE, Werlen S, Bixby SD, Millis MB, Kim Y-J. Patterns of joint damage seen on MRI in early hip osteoarthritis due to structural hip deformities. Osteoarthritis Cartilage. 2012;20:661–669. doi: 10.1016/j.joca.2012.03.014. [DOI] [PubMed] [Google Scholar]
- 61.Steppacher SD, Anwander H, Zurmühle CA, Tannast M, Siebenrock KA. Eighty percent of patients with surgical hip dislocation for femoroacetabular impingement have a good clinical result without osteoarthritis progression at 10 years. Clin Orthop Relat Res. 2015;473:1333–1341. doi: 10.1007/s11999-014-4025-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Steppacher SD, Huemmer C, Schwab JM, Tannast M, Siebenrock KA. Surgical hip dislocation for treatment of femoroacetabular impingement: factors predicting 5-year survivorship. Clin Orthop Relat Res. 2014;472:337–348. doi: 10.1007/s11999-013-3268-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Tannast M, Hanke MS, Zheng G, Steppacher SD, Siebenrock KA. What are the radiographic reference values for acetabular under- and overcoverage? Clin Orthop Relat Res. 2015;473:1234–1246. doi: 10.1007/s11999-014-4038-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Tannast M, Mistry S, Steppacher SD, Reichenbach S, Langlotz F, Siebenrock KA, Zheng G. Radiographic analysis of femoroacetabular impingement with Hip2Norm-reliable and validated. J Orthop Res. 2008;26:1199–1205. doi: 10.1002/jor.20653. [DOI] [PubMed] [Google Scholar]
- 65.Tannast M, Siebenrock K-A. Open therapy of femoroacetabular impingement [in German] Oper Orthop Traumatol. 2010;22:3–16. doi: 10.1007/s00064-010-3001-7. [DOI] [PubMed] [Google Scholar]
- 66.Tannast M, Siebenrock KA, Anderson SE. Femoroacetabular impingement: radiographic diagnosis–what the radiologist should know. AJR Am J Roentgenol. 2007;188:1540–1552. doi: 10.2214/AJR.06.0921. [DOI] [PubMed] [Google Scholar]
- 67.Tannast M, Zheng G, Anderegg C, Burckhardt K, Langlotz F, Ganz R, Siebenrock KA. Tilt and rotation correction of acetabular version on pelvic radiographs. Clin Orthop Relat Res. 2005;438:182–190. doi: 10.1097/01.blo.0000167669.26068.c5. [DOI] [PubMed] [Google Scholar]
- 68.Tönnis D. General radiography of the hip joint. In: Tönnis D, editor. Congenital Dysplasia and Dislocation of the Hip. Heidelberg, Germany: Springer-Verlag; 1987. [Google Scholar]
- 69.Tönnis D, Heinecke A. Acetabular and femoral anteversion: relationship with osteoarthritis of the hip. J Bone Joint Surg Am. 1999;81:1747–1770. doi: 10.2106/00004623-199912000-00014. [DOI] [PubMed] [Google Scholar]
- 70.Varich L, Pathria M, Resnick D, Hodler J, Bruser D, Bosch E, Trudell D, Tyson R. Patterns of central acetabular osteophytosis in osteoarthritis of the hip. Invest Radiol. 1993;28:1120–1127. doi: 10.1097/00004424-199312000-00007. [DOI] [PubMed] [Google Scholar]
- 71.Ware J, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 72.Wiberg G. The anatomy and roentgenographic appearance of a normal hip joint. Acta Chir Scand. 1939;83:7–38. [Google Scholar]
- 73.Zahiri CA, Schmalzried TP, Szuszczewicz ES, Amstutz HC. Assessing activity in joint replacement patients. J Arthroplasty. 1998;13:890–895. doi: 10.1016/S0883-5403(98)90195-4. [DOI] [PubMed] [Google Scholar]
- 74.Zheng G, Tannast M, Anderegg C, Siebenrock KA, Langlotz F. Hip2Norm: an object-oriented cross-platform program for 3D analysis of hip joint morphology using 2D pelvic radiographs. Comput Methods Programs Biomed. 2007;87:36–45. doi: 10.1016/j.cmpb.2007.02.010. [DOI] [PubMed] [Google Scholar]