Abstract
Background:
Recurrence rate of rotator cuff tears is still high despite the improvements of surgical techniques, materials used and a better knowledge of the healing process of the rotator cuff tendons. Large to massive rotator cuff tears are particularly associated with a high failure rate, especially in elderly.
Augmentation of rotator cuff repairs with extracellular matrix or synthetic patches has gained popularity in recent years with the aim of reducing failure. The aim of this study was to investigate the outcome of rotator cuff repairs augmented with denatured extracellular matrix in a series of patients who underwent arthroscopic rotator cuff repair for large to massive tears.
Methods:
Ten consecutive patients, undergoing arthroscopic rotator cuff repair with extracellular matrix augment for large and massive tears, were prospectively enrolled into this single surgeon study. All repairs were performed arthroscopically with a double row technique augmented with extracellular matrix.
Oxford Shoulder Score, Constant Score and pain visual analogue scale (VAS) were used to monitor the shoulder function and outcome pre-operatively and at three, six and 12-month follow-up. Minimum follow up was three months. Mean follow up was 7 months.
Results:
Mean Constant score improved from 53 (SD=4) pre-operatively to 75 (SD=11) at final follow up. Mean Oxford score also increased from 30 (SD=8) pre-operatively to 47 (SD=10) at the final follow up. The visual analogue scale (VAS) improved from seven out of 10 (SD=2) preoperatively to 0.6 (SD=0.8) at final follow up. Additionally, there was significant improvement at three months mark in Constant score.
Conclusion:
Arthroscopic repair and augmentation of large and massive rotator cuff tears with extracellular matrix patch has good early outcome.
Keywords: Augmentation, Double-row technique, Extracellular matrix, Owl technique, Patch, Rotator cuff repair, Rotator cuff tear, Scaffold, Tendinopathy
Introduction
Rotator cuff tears are very common particularly in elderly population. Although a proportion of these tears are asymptomatic, many patients suffer with pain, reduced function and quality of life and are therefore candidates for surgical repairs. In the last 15 years, advances in surgical techniques and equipment have revolutionized arthroscopic rotator cuff repairs (1,2). Despite these developments, large and massive rotator cuff tear repairs are still associated with a high failure rate ranging from 25% to in excess of 70% in older age group (1,3).
The sites of failure of the rotator cuff repairs are reported to be at the bone-tendon interface and at the junction suture-tendon (4-6). The biology of the healing process between tendons and bone is complex because it involves healing between two dissimilar tissues and a successful repair is dependent on establishment of collagen fibers continuity between tendon and bone (5).
Additionally, large-massive rotator cuff repairs are often performed in chronic tears of elderly population who often have poor quality tendon and fragile tissue. As a consequence, at the tendon-suture interface there is a higher risk of failure particularly in presence of a high tension repair. An optimal repair is one that establishes a fine tuned balance where tension of the repair is spread as uniformly as possible with preserved blood supply to the area (7).
Several different techniques have been used to try to minimize the re-tear rate following rotator cuff (RC) tears. Double row repair is one strategy that has gained huge popularity. There are a number of biomechanical studies that clearly indicate double row repairs are stronger construct with increased load to failure and better restoration of the tendon footprint (7,8). Furthermore, recent radiology studies are indicating that double row technique can reduce the re-tear rate of rotator cuff repairs (RCR) (9). However, despite these biomechanical and radiological studies, there does not appear to be a significant clinical differences in the overall shoulder function when comparing single with double row techniques (10).
Another strategy is addition of platelet rich plasma (PRP) at the time of RCR. Although further research is required on PRP’s role for RCR, so far there does not appear to be any convincing evidence for the positive role of PRP in overall outcome of shoulder function nor re-tear rate of rotator cuff tears (RCT) (1,3,11-13).
The persistently high RCR re-tear rates have drawn attention of the investigators into the use of patch augmentation. There are a number of patches in the market including augmentation with cellular components (either allogenic or autogenic), and extracellular matrix (xenograft, allograft, and synthetic). The aim here to decrease re-tear rates by evenly spreading the mechanical load across the repair site and strengthening the repair construct as well as enhancing the biological environment required for healing by providing different growth factors and structural protein (14). There are a number of biomechanical studies that demonstrate a mechanical advantage with augmentation of the graft (15-17). Clinically there are some studies which show better outcome whereas others which do not (18,19).
The aim of this study was to study the early outcome of arthroscopic rotator cuff repair of large and massive rotator cuff tears performed where the repair was additionally augmented with extracellular matrix augmentation.
Materials and Methods
Ten consecutive patients undergoing arthroscopic rotator cuff repair with extracellular matrix augment for large and massive tears were prospectively enrolled into this single surgeon study. All the patients were assessed pre-operatively in clinic, by the consultant or the upper limb clinical fellow, with shoulder X-rays (antero-posterior, axillary and outlet view) and magnetic resonance imaging (MRI). Oxford Shoulder Score, Constant Score and pain visual analogue scale (VAS) were used to score shoulder function. All were reviewed three weeks post surgery and again at three, six months and 12 months. Oxford Shoulder Score, Constant Score and pain visual analogue scale (VAS) were used to score shoulders function on each occasion accept at three weeks post surgery.
Only patients with large or massive repairable rotator cuff tears were included in the study (20,21) [Table 1]. We did not use the augment to bridge the gap in irreparable RCT.
Table 1.
Inclusion and Exclusion Criteria
| Inclusion Criteria | Exclusion Criteria |
|---|---|
| • Large (> 3cm) RC tears | • Small (< 1cm) RC tears |
| • Massive (i.e. > 2 tendons) RC tears | • Medium (1 < 3cm)RC tears |
| • Repairable RC tears | • Irreparable RC tears |
| • Poor tissue quality | • Good tissue quality |
| • Patient goals of pain relief and improved shoulder function | • Non achievable patient objectives |
| • No evidence of cuff arthropathy | • Evidence of cuff arthropathy |
| • No signs of OA of the GHJ | • OA of the GHJ |
| • Muscular atrophy of Goutallier stage I – III (26) | • Muscular atrophy of Goutallier stage IV (27) |
| • Systemically well | • Active Infections |
HH: humeral head; OA: osteoarthritis; GHJ: gleno humeral joint.
Our exact technique has been previously described (22). All the procedures were performed under general anesthesia (GA) and inter-scalene block. Teicoplanin 400mg and Gentamycin 120mg were given as prophylaxis to all the patients at induction.
With the patient in the lateral position, an arthroscopic diagnostic assessment was performed through a standard posterior port. The size and shape of the tear, the quality of the tendons and the amount of retraction of the cuff was evaluated. At this stage, when necessary, extensive release of adhesions was performed in order to mobilize the rotator cuff. In presence of subscapularis tears, arthroscopic subscapularis repair was concomitantly performed. Similarly, in those patient with clinical features of long head of biceps (LHB) pathology and arthroscopic evidence LHB abnormality, either LHB tenotomy or tenodesis was performed. Additionally, arthroscopic sub-acromial decompression was performed in all the patients and acromio-clavicular (ACJ) excision was performed in those with ACJ tenderness.
All the rotator cuff repairs were performed by the same surgeon (AN). A double row technique was used. A cannula was positioned in the lateral portal (Passport 10mm x 4/5cm – Anthrex, Naple, FL). One or two medial row anchors (Helicoil 5.5 PK, Smith & Nephews) were used depending on the dimensions of the tear. There were four or eight passes into the tendon (four with one medial row anchor and eight with two medial row anchors) as in a knotted mattress technique. Following this the repair was augmented using extra-cellular matrix (ECM) (Arthrex DX, Naples, FL) using the “Owl” technique as previously described.
The suture limbs of the medial row anchors were passed through holes of the augment which was then inserted into the subacromial space. The augment was then stabilized by inserting two lateral anchors (Swivelock 5.5 biocomposite – Arthrex, Naples,FL) with the medial row suture limbs (similar to “transosseous equivalent” with the exceptions of medial anchor suture limbs going over the augment before being inserted laterally with the lateral row anchors) [Figure 1].
Figure 1.
Intraoperative picture of the augmentation patch secured to the RC with a double row repair. Scope is introduced through the lateral port.
Shoulders were immobilized in a shoulder abduction wedge at the end of the procedure and patients were instructed to wear this for six weeks. Physiotherapy as per large-massive rotator cuff repair protocols is organized before discharge.
Differences between Constant and Oxford scores as well as visual analogue scores and abduction range recorded preoperatively and postoperatively were evaluated by use of Mann Whitney U test.
Results
The mean age of the patients was 74 (range, 65-82). There were six females and four males. Minimum follow up was three months with an average follow up period of seven months (range 3-12 months) [Table 2].
Table 2.
Follow up scores at the final visit
| Patient Number | Follow Up Period | Pre-Op Oxford Scores | Final Follow up Oxford Scores | Pre-Op Constant Scores | Final Follow up Constant Scores |
|---|---|---|---|---|---|
| 1 | 12 months | 19 | 42 | 50 | 59 |
| 2 | 12 months | 35 | 55 | 51 | 80 |
| 3 | 6 months | 17 | 63 | 57 | 78 |
| 4 | 6 months | 35 | 48 | 57 | 88 |
| 5 | 6 months | 34 | 48 | 51 | 73 |
| 6 | 6 months | 34 | 48 | 55 | 89 |
| 7 | 6 months | 35 | 41 | 54 | 56 |
| 8 | 6 months | 18 | 31 | 57 | 70 |
| 9 | 3 months | 35 | 58 | 44 | 76 |
| 10 | 3 months | 33 | 39 | 55 | 80 |
Five patients underwent concomitant ACJ excision whereas LHB tenotomy was performed in three patients. Concomitant subscapularis repair was also performed in two of the patients. Five patients had large supraspinatus tears and five had massive tears. The tear also involved the infraspinatous in 4 patients. We did not have any infections.
Mean Constant score improved from 53 (SD=4) pre-operatively to 75 (SD=11) at final follow up (P<0.05). Mean Constant score at the three months mark (mean=65, SD=12) was also significantly improved compared to pre-op score (P<0.05) [Table 2, Figure 2].
Figure 2.
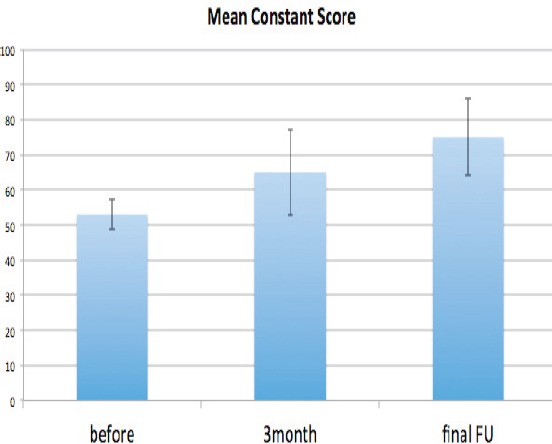
Constant shoulder score pre-surgery, at 3 months post surgery and at 6 months post surgery.
Similarly mean Oxford score also increased from 30 (SD=8) pre-operatively to 47 (SD=10) at the final follow up (P<0.05). Although there was also an increase in Oxford score at three months (mean=38.7, SD=12.7), this improvement was not significant (P>0.05) [Table 2, Figure 3].
Figure 3.
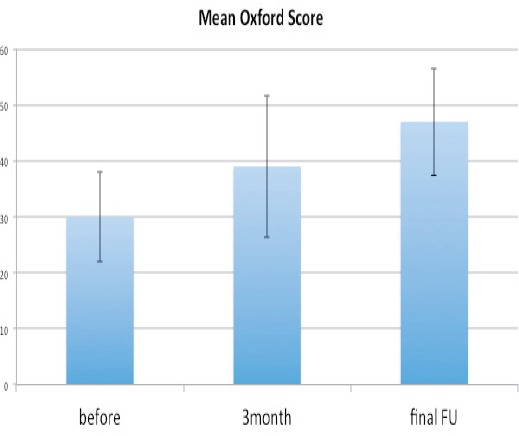
Oxford shoulder score pre-surgery, at 3 months post surgery and at 6 months post surgery.
The visual analogue scale (VAS) improved from seven out of 10 (SD=2) preoperatively to 0.6 (SD=0.8) at final follow up (P<0.05). Mean VAS at three months mark (mean=0.83, SD=0.8) was also significantly improved compared to pre-op score (P<0.05) [Figure 4].
Figure 4.
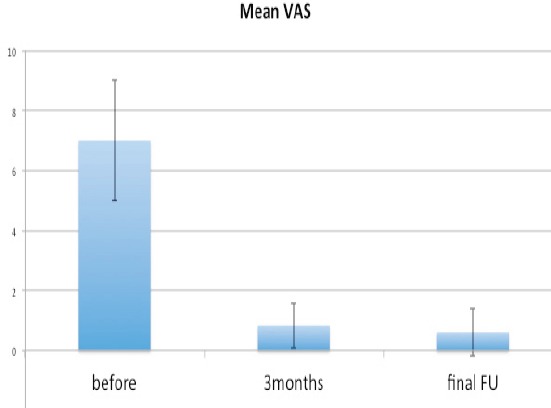
Visual analogue scores (VAS) pre-surgery, at 3 months post surgery and at 6 months post surgery.
Mean abduction also improved from 93 (SD=27) pre-operatively to 153 (SD=24) at the final follow up (P<0.05). Mean abduction at the three months mark (141, SD=31) was also significantly improved compared to pre-op score (P<0.05) [Figure 5].
Figure 5.
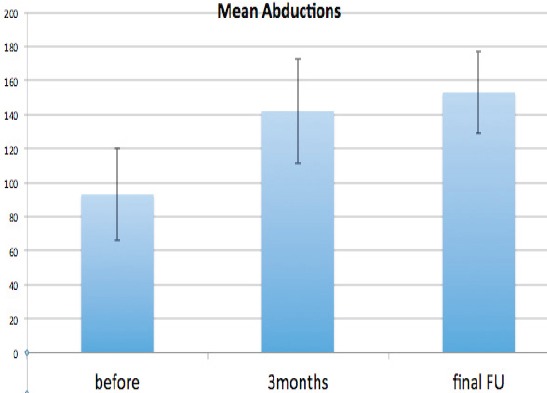
Mean abduction pre-surgery, at 3 months post surgery and at 6 months post surgery.
Discussion
Despite the huge advances in arthroscopic techniques and instrumentation, re-tears following arthroscopic repairs are common and in elderly population with cuff repairs for massive and large tears can be in excess of 70% (23). This is a comparable re-tear rate to that reported by Zumstein et al (57%), Miller et al (41%), Kim et al (42.4%), and Park et al (25%) (24-27). It is therefore not surprising that in recent years there has been a focus of attention into ways of reducing this significant re-tear rate.
Augment patches have acquired popularity in the last 10 years as yet another strategy to optimize healing and reduce re-tear rates. The increased load to failure of a rotator cuff repair augmented with a patch is demonstrated by a biomechanical cadaveric study of Shea et al. (15). Non augmented RCR had a rate failure of 33%, while all the augmented repairs remained intact with the loading cyclic protocol. It is also reported that the gap at the interface tendon-bone is decreased by 40% when an augmentation is performed. As most of the rotator cuff repair failures occur in the interface tendon-bone, an increased contact at this level can make the difference in the natural history of the repair (4,20).
Recent literature reports suggest that good outcomes and reduced re-tear rates may be achieved when augmentation patches are utilised. Wong et al. (2010) published a study using graftjacket allograft a-cellular human dermal matrix to repair large to massive RCT, reporting good results at two-year follow-up (18). Similarly, Barber at al. reported encouraging results using acellular human dermal matrix graft (28). Intact repairs were found in 85% of the augmented group and 40% of the non augmented group (gadolinium-enhanced MRI at 14 months). The shoulder functions were also better in the augmented group, at 2-year follow-up (28).
In 2013, Gupta AK. at al. used a porcine xenograft to repair large to massive RCT. They reported that the overall shoulder function improved (two-year follow-up) and 73% of the patients had a fully intact tendon-graft reconstruction showed by the shoulder ultrasound (US), performed two years post-operatively; 22% had a partially intact reconstruction, 5% (1 patient) had a complete tear at the graft-bone interface caused by suture anchor pullout as a result of a fall (29). The same year, an Italian group published good long term results using a porcine dermal collagen repair patch. Better shoulder outcome achieved and no re-tears observed at two and half years follow-up (30).
A poly-l-lactic acid synthetic patch was used as a reinforcement device by Proctor et al. In their study, 83% of patients at 12 months after surgery and 78% of patients at 42 months after surgery had an intact RC with substantial functional improvement of the shoulder function (31).
In another study, polypropylene patch augmentation was demonstrated to significantly improve the 36-month outcome in terms of function, strength, and re-tear rate if compared with a control group of patients who had a simple RCR and a third group who had the RC repaired with a collagen patch. The group treated with a collagen patch had a higher re-tear rate if compared with the other two groups (19).
Our data also provides evidence for positive short-term outcome following arthroscopic RC repair with extracellular matrix augmentation for large and massive RC tears. There were significant improvements in shoulder function outcome scores, visual analogue scores and abduction at the final follow up (minimum follow up was three months and average follow up was over seven months). It is also interesting to note that there were also significant improvements in Constant scores, visual analogue scores and shoulder abduction at the three months mark. Although Oxford shoulder score also improved at three months, this improvement was not significant at P<0.05 level. This is in contrast to Hughes et al study where there was only a significant improvement in Constant scores at the six months mark and not the three months with arthroscopic cuff repair without augmentation (25). The improved function and pain observed with our patients at the three months mark may be due to the augment reducing the tension of the repair in the early rehabilitation phase and therefore minimizing pain and optimizing the healing environment.
There are a number of limitations with our study. First of all, the number of patients is small and we have a short follow up period. Secondly, this is not a randomized controlled study therefore it may be the case that if we have compared the series to a group patients having rotator cuff repairs without augmentation, there may have not been a difference between the two groups and the patients with RC repair without augmentation may have done as well as those with augmentation. Thirdly, we did not perform imaging in all the patients post surgery to confirm that the rotator cuff has indeed healed without any evidence of re-tears. Nevertheless, we feel that our series demonstrate that good outcomes may be achieved following arthroscopic RC repair with augmentation and highlight the need for randomized controlled studies with long term follow ups to investigate whether this good outcome is better than that observed with RCR without augmentation. Our series also suggest that cuff repairs with augmentation may lead to significant function improvement as early as three months post repair which has been has not been the case with previous literature on standard RC repair. We did not do any magnetic resonance imaging (MRI) in our patient before the 12 months mark as we felt it was important to wait at least for a year before any meaningful conclusions could be drawn as to whether the RC has healed on the MRI images. We did do MRI imaging in two patients who had past one year mark and the repair was intact in both patients [Figure 6a, b].
Figure 6.
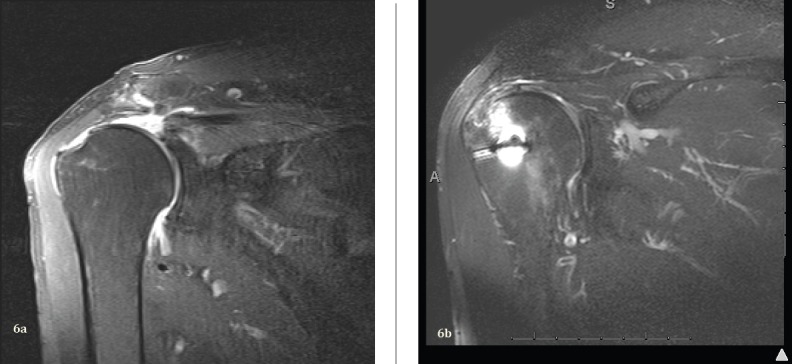
MRI of tear pre-op (6a) and one year post op (6b) in the same patient.
Biomechanically, augmentation of the RCR makes sense (15-17). Furthermore, it might optimize the healing environment by distributing the load and reducing the tendon repair tension in the early rehabilitation period. There may also be some additional biological advantages too when augmenting the repair with extracellular augment. Clinically, our series suggest that good short term outcomes may be observed with RC repair and augmentation. Augmentation, therefore may prove to be the tool to decrease the re-tear rates in large and massive tears in elderly.
Arthroscopic repair and augmentation of large and massive rotator cuff tears with extracellular matrix patch has good early outcome.
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
References
- 1.Ruiz-Moneo P, Molano-Muñoz J, Prieto E, Algora J. Plasma rich in growth factors in arthroscopic rotator cuff repair: A randomized, double-blind, controlled clinical trial. Arthroscopy. 2013;29(1):2–9. doi: 10.1016/j.arthro.2012.08.014. [DOI] [PubMed] [Google Scholar]
- 2.Derwin KA, Badylak SF, Steinmann SP, Iannotti JP. Extracellular matrix scaffold devices for rotator cuff repair. J Shoulder Elbow Surg. 2010;19(3):467–476. doi: 10.1016/j.jse.2009.10.020. [DOI] [PubMed] [Google Scholar]
- 3.Neyton L, Godeneche A, Nove-Josserand L, et al. Arthroscopic suture-bridge repair for small to medium size supraspinatus tear: Healing rate and retear, pattern. Arthroscopy. 2013;29(1):10–17. doi: 10.1016/j.arthro.2012.06.020. [DOI] [PubMed] [Google Scholar]
- 4.Rodeo SA, Arnoczky SP, Torzilli PA, et al. Tendon-healing in a bone tunnel. A biomechanical and histological study in the dog. J Bone Joint Surg Am. 1993;75(12):1795–1803. doi: 10.2106/00004623-199312000-00009. [DOI] [PubMed] [Google Scholar]
- 5.Gilot GJ, Attia AK, Alvarez AM. Arthroscopic Repair of Rotator Cuff Tears Using Extracellular Matrix Graft. Arthroscopy Techniques. 2014;43(4):e487–9. doi: 10.1016/j.eats.2014.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Omae H, Yamamoto S, Mochizuki Y, Ochi M. An Augmentation Suture Technique for Arthroscopic Rotator Cuff Repair. Arthroscopy Techniques. 2014;53(3):e313–5. doi: 10.1016/j.eats.2014.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mazzocca AD, Millett PJ, Guanche CA, Santangelo SA, Arciero RA. Arthroscopic single-row versus double-row suture anchor rotator cuff repair. Am J Sports Med. 2005;33(12):1861–8. doi: 10.1177/0363546505279575. [DOI] [PubMed] [Google Scholar]
- 8.Millett PJ, Mazzocca A, Guanche CA. Mattress double anchor footprint repair: a novel, arthroscopic rotator cuff repair technique. Arthroscopy. 2004;20(8):875–9. doi: 10.1016/j.arthro.2004.07.015. [DOI] [PubMed] [Google Scholar]
- 9.Hein J, Reilly JM, Chae J, Maerz T, Anderson K. Re-tear Rates After Arthroscopic Single-Row, Double-Row, and Suture Bridge Rotator Cuff Repair at a Minimum of 1 Year of Imaging Follow-up: A Systematic Review. Arthroscopy. 2015;31(11):2274–8. doi: 10.1016/j.arthro.2015.06.004. [DOI] [PubMed] [Google Scholar]
- 10.Barber FA. Triple-Loaded Single-Row Versus Suture-Bridge Double-Row Rotator Cuff Tendon Repair With Platelet-Rich Plasma Fibrin Membrane: A Randomized Controlled Trial. Arthroscopy. 2016;32(5):753–61. doi: 10.1016/j.arthro.2015.11.020. [DOI] [PubMed] [Google Scholar]
- 11.Bergeson AG, Tashjian RZ, Greis PE, Crim J, Stoddard GJ, Burks RT. Effects of Platelet-Rich Fibrin Matrix on Repair Integrity of At-Risk Rotator Cuff Tears. Am J Sports Med. 2012;40(2):286–93. doi: 10.1177/0363546511424402. [DOI] [PubMed] [Google Scholar]
- 12.Weber SC, Kauffman JI, Parise C, Weber SJ, Katz SD. Platelet-Rich Fibrin Matrix in the Management of Arthroscopic Repair of the Rotator Cuff: A Prospective, Randomized, Double-Blinded Study. Am J Sports Med. 2013;41(2):263–70. doi: 10.1177/0363546512467621. [DOI] [PubMed] [Google Scholar]
- 13.Castricini R, Longo UG, De Benedetto M, Panfoli N, Pirani P, Zini R, et al. Platelet-rich plasma augmentation for arthroscopic rotator cuff repair: A randomized controlled trial. Am J Sports Med. 2011;39(2):258–265. doi: 10.1177/0363546510390780. [DOI] [PubMed] [Google Scholar]
- 14.Greenspoon J.A, Petri M, Warth R.J, Millett P.J. Massive rotator cuff tears: pathomechanics, current treatment options, and clinical outcomes. J Shoulder Elbow Surg. 2015;24(9):1493–505. doi: 10.1016/j.jse.2015.04.005. [DOI] [PubMed] [Google Scholar]
- 15.Shea KP, Obopilwe E, Sperling JW, Iannotti JP. A biomechanical analysis of gap formation and failure mechanics of a xenograft- reinforced rotator cuff repair in a cadaveric model. J Shoulder Elbow Surg. 2012;21(8):1072–9. doi: 10.1016/j.jse.2011.07.024. [DOI] [PubMed] [Google Scholar]
- 16.Ely EE, Figueroa NM, Gilot GJ. Biomechanical Analysis of Rotator Cuff Repairs With Extracellular Matrix Graft Augmentation. Orthopedics, the cutting edge. 2014;37(9):608–14. doi: 10.3928/01477447-20140825-05. [DOI] [PubMed] [Google Scholar]
- 17.Omae H, Steinmann SP, Zhao C, Zobitz ME, Wongtriratanachai P, Sperling JW, et al. An Biomechanical effect of rotator cuff augmentation with an acellular dermal matrix graft: A cadaver study. Clinical Biomechanics. 2012;27(8):789–92. doi: 10.1016/j.clinbiomech.2012.05.001. [DOI] [PubMed] [Google Scholar]
- 18.Wong I, Burns J, Snyder S. Arthroscopic GraftJacket repair of rotator cuff tears. J Shoulder Elbow Surg. 2010;19(2 Suppl):104–9. doi: 10.1016/j.jse.2009.12.017. [DOI] [PubMed] [Google Scholar]
- 19.Ciampi P, Scotti C, Nonis A, Vitali M, Di Serio C, Peretti GM, et al. The benefit of synthetic versus biological patch augmentation in the repair of posterosuperior massive rotator cuff tears: a 3-year follow-up study. Am J Sports Med. 2014;42(5):1169–75. doi: 10.1177/0363546514525592. [DOI] [PubMed] [Google Scholar]
- 20.Burkhart SS, Barth JR, Richards DP, Zlatkin MB, Larsen M. Arthroscopic repair of massive rotator cuff tears with stage 3 and 4 fatty degeneration. Arthroscopy. 2007;23(4):347–54. doi: 10.1016/j.arthro.2006.12.012. [DOI] [PubMed] [Google Scholar]
- 21.Goutallier D, Postel JM, Bernageau J, Lavau L, Voisin MC. Fatty muscle degeneration in cuff ruptures. Pre- and postoperative evaluation by CT scan. Clin Orthop. 1994;304:78–83. [PubMed] [Google Scholar]
- 22.Narvani A, Consigliere P, Polyzois I, Sarkhel T, Gupta R, Levy O. “Owl” Technique for All-Arthroscopic Augmentation of a Massive or Large Rotator Cuff Tear With Extracellular Matrix Graft. Arthroscopy. 2016. In press. [DOI] [PMC free article] [PubMed]
- 23.Chung SW, Kim JY, Kim MH, Kim SH, Oh JH. Arthroscopic repair of massive rotator cuff tears: outcome and analysis of factors. Am J Sports Med. 2013;41(7):1674–83. doi: 10.1177/0363546513485719. [DOI] [PubMed] [Google Scholar]
- 24.Zumstein MA, Jost B, Hempel J, Hodler J, Gerber C. The clinical and structural long term results of open repair of massive tears of the rotator cuff. J Bone Joint Surg Am. 90(11):2423–31. doi: 10.2106/JBJS.G.00677. [DOI] [PubMed] [Google Scholar]
- 25.Miller BS, Downie BK, Kohen RB, Kijek T, Lesniak B, Jacobson JA, et al. When do rotator cuff repairs fail? Serial ultrasound examination after arthroscopic repair of large and massive rotator cuff tears. Am J Sports Med. 2011;39(10):2064–70. doi: 10.1177/0363546511413372. [DOI] [PubMed] [Google Scholar]
- 26.Kim JR, Cho YS, Ryu KJ, Kim JH. Clinical and radiographic outcomes after arthroscopic repair of massive rotator cuff tears using a suture bridge technique: assessment of repair integrity on magnetic resonance imaging. Am J Sports Med. 2012;40(4):786–93. doi: 10.1177/0363546511434546. [DOI] [PubMed] [Google Scholar]
- 27.Park JY, Lhee SH, Oh KS, Moon SG, Hwang JT. Clinical and ultrasonographic outcomes of arthroscopic suture bridge repair for massive rotator cuff tear. Arthroscopy. 2013;29(2):280–9. doi: 10.1016/j.arthro.2012.09.008. [DOI] [PubMed] [Google Scholar]
- 28.Barber FA, Burns JP, Deutsch A, Labbé MR, Litchfield RB. A prospective, randomized evaluation of acellular human dermal matrix augmentation for arthroscopic rotator cuff repair. Arthroscopy. 2012;28(1):8–15. doi: 10.1016/j.arthro.2011.06.038. [DOI] [PubMed] [Google Scholar]
- 29.Gupta AK, Hug K, Boggess B, Gavigan M, Toth AP. Massive or 2-tendon rotator cuff tears in active patients with minimal glenohumeral arthritis: clinical and radiographic outcomes of reconstruction using dermal tissue matrix xenograft. Am J Sports Med. 2013;41(4):872–9. doi: 10.1177/0363546512475204. [DOI] [PubMed] [Google Scholar]
- 30.Giannotti S, Ghilardi M, Dell’osso G, Magistrelli L, Bugelli G, Di Rollo F, et al. Study of the porcine dermal collagen repair patch in morpho-functional recovery of the rotator cuff after minimum follow-up of 2.5 years. Surg Technol Int. 2014;24:348–52. [PubMed] [Google Scholar]
- 31.Proctor CS. Long-term successful arthroscopic repair of large and massive rotator cuff tears with a functional and degradable reinforcement device. J Shoulder Elbow Surg. 2014;23(10):1508–13. doi: 10.1016/j.jse.2014.01.010. [DOI] [PubMed] [Google Scholar]


