Abstract
Rabies virus (RV) has recently been developed as a novel vaccine candidate for human immunodeficiency virus type 1 (HIV-1). The RV glycoprotein (G) can be functionally replaced by HIV-1 envelope glycoprotein (Env) if the gp160 cytoplasmic domain (CD) of HIV-1 Env is replaced by that of RV G. Here, we describe a pilot study of the in vivo replication and immunogenicity of an RV with a deletion of G (ΔG) expressing a simian/human immunodeficiency virus SHIV89.6P Env ectodomain and transmembrane domain fused to the RV G CD (ΔG-89.6P-RVG) in a rhesus macaque. An animal vaccinated with ΔG-89.6P-RVG developed SHIV89.6P virus-neutralizing antibodies and SHIV89.6P-specific cellular immune responses after challenge with SHIV89.6P. There was no evidence of CD4+ T-cell loss, and plasma viremia was controlled to undetectable levels by 6 weeks postchallenge and has remained suppressed out to 22 weeks postchallenge.
Protective immune responses to rhabdoviruses are directed against the single-membrane glycoprotein (G), which elicits potent virus-neutralizing antibodies (VNA) (9, 20). Therefore, when rhabdoviruses are used as vectors, antibodies generated by the initial inoculation limit the effectiveness of subsequent administrations of the same virus (15). However, a unique feature of rhabdovirus vectors is that the single G can be functionally replaced by a foreign glycoprotein expressing the cytoplasmic domain (CD) of G (8, 11). Replacement of the vesicular stomatitis virus (VSV) G with the human immunodeficiency virus type 1 (HIV-1) receptor CD4 and the coreceptor CXCR4 resulted in a VSV strain with G deleted (ΔG VSV) that was capable of infecting and specifically killing cells previously infected with HIV-1 that were expressing HIV-1 gp160 on their surfaces (17). ΔG versions of VSV and rabies virus (RV) expressing HIV-1 gp160 fused to the RV or VSV G CD preferentially infect human CD4+/HIV-1 chemokine receptor-positive cells in a pH-independent manner and are capable of infecting human dendritic cells (6, 8). Thus far, the immunogenicity of replication-competent ΔG rhabdoviruses has only been studied in the mouse model with VSV constructs expressing influenza virus A hemagglutinin (HA). A ΔG VSV expressing influenza virus A HA (VSV ΔG-HA) was shown to be apathogenic in mice but showed reduced protection from lethal influenza challenge when compared to a G-containing VSV vector expressing HA (VSV-HA) (15). The replication capacity, both in vitro and in vivo, of the VSV ΔG-HA vector was likely due to residual VSV G contained on the virion from the VSV G-expressing cell line in which the vector was prepared. In vitro the virus was neutralized by anti-G, but not anti-HA, antibodies (15).
Members of our laboratory previously demonstrated that the infectivity of ΔG RV expressing HIV-1 Env is mediated by functional HIV-1 gp160 (8). These ΔG RV are recovered and propagated on T-cell lines in the complete absence of RV G. Here, we report the preliminary analysis of the replication and immunogenicity of a ΔG RV expressing the simian/human immunodeficiency virus SHIV89.6P Env ectodomain (ΔG-89.6P-RVG) in a rhesus macaque. An animal vaccinated with ΔG-89.6P-RVG seroconverted to both HIV-1 Env and RV nucleoprotein (N). Upon challenge with pathogenic SHIV89.6P, this animal controlled viral replication, likely through high-titer virus-neutralizing antibodies and Env-specific cellular immune responses. Although these are preliminary results, the data suggest that first-generation ΔG RV are replication competent in vivo and can elicit beneficial immune responses in nonhuman primates.
MATERIALS AND METHODS
The construction and recovery of ΔG RV vectors expressing HIV-1 Env proteins containing the CD of RV G have been described previously (8). For the present study, the sequences for the gp120 and gp41 ecto- and transmembrane domains of SHIV89.6P Env were amplified by PCR from plasmid pKB9SHIV (89.6P; Aids Research and Reference Reagent Program) and cloned in frame with the RV G CD. The resulting plasmid was entitled pΔG-89.6P-RVG, and the virus recovered from pΔG-89.6P-RVG was designated ΔG-89.6P-RVG.
The enzyme-linked immunosorbent assay (ELISA) methods used for this study have been described previously (10). For RV ribonucleoprotein (RNP) ELISA, purified RV RNP was used at 100 ng/well. To determine seroconversion to SHIV89.6P Env, oligomeric gp140 (strain HIV-189.6) was prepared from vaccinia virus-infected BSC-1 cells as previously described (14). For Western blot analysis, cell lysates were prepared from BSR (a BHK clone) cells infected with an empty RV vector (BNSP), an RV vector expressing SHIV89.6P Env containing the CD of RV G (BNSP-89.6P-RVG), or an RV vector expressing wild-type SHIV89.6P Env (BNSP-89.6P, full length). The proteins were separated by sodium dodecyl sulfate-polyacrylamide gel electrophoresis, transferred to a polyvinylidene difluoride membrane, and probed with serum collected at week 8 after initial immunization.
The ELISPOT assay for Env-specific cellular immune responses was performed as previously described (12, 18). Briefly, peripheral blood mononuclear cells (PBMC) were isolated from whole blood and added to a microtiter plate. Cells were either mock infected (media control), infected with vaccinia virus strain WR194 (vaccinia control), or infected with vaccinia virus expressing Env of strain 89.6 (HIV-189.6) overnight at 37°C. Cells were transferred to an ELISPOT plate coated with a monoclonal antibody specific for rhesus IFN-γ for a 5-h incubation at 37°C. The plate was developed, and the spots were counted and adjusted to spot-forming cells (number of spot-forming cells per 106 PBMC).
Virus-neutralizing antibody titers against SHIV89.6P were determined in an MT-2 cell-killing assay, as described elsewhere (7), and postchallenge plasma viremia was determined for specific time points by a branched DNA assay (Bayer Reference Testing Laboratory) (21). The assay limit of detection was 125 copies of viral RNA/ml.
All flow cytometry-based assays for peripheral blood cell counts were performed at Tulane National Primate Research Center by the immunology core group. Whole blood and antibodies for CD3, CD4, or CD8 conjugated to appropriate fluorochromes (BD Pharmingen) were incubated for 30 min at room temperature. Erythrocytes were lysed, and the stained cells were fixed using the Multi-Q-Prep instrument (Beckman-Coulter). Acquisition was done on a FACSCalibur (Becton Dickinson), and the results were analyzed using Cellquest software.
RESULTS
Since this was a pilot experiment designed to determine whether surrogate RV with an HIV-1-like tropism were replication competent in vivo, we chose to vaccinate via three routes. The animal was given 1-ml doses (9 × 105 50% tissue culture infective doses of ΔG-89.6P-RVG each) via intramuscular, intravenous (i.v.), and subcutaneous routes at day 0 and week 7 and an additional i.v.-only booster at week 19. At week 25, the monkey was challenged i.v. with 30 monkey infectious doses of pathogenic SHIV89.6P. The animal was observed for clinical signs of infection, and sequential blood samples were obtained to monitor lymphocyte counts, plasma viremia, and the postchallenge immune response as described below.
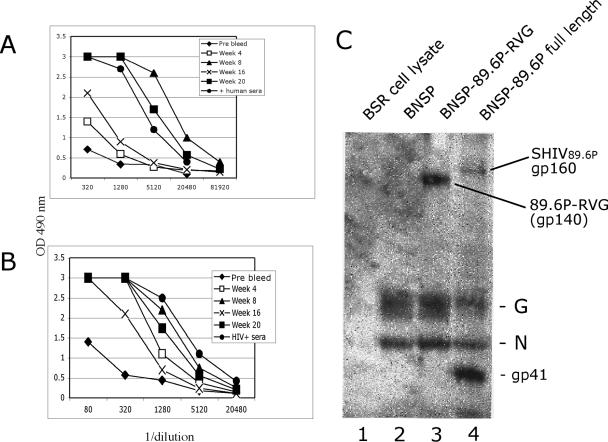
To assess the anti-RV and anti-SHIV89.6P Env response in the rhesus macaque following vaccination, ELISAs designed to detect antibody responses to RV RNP and oligomeric gp140 were performed. As shown in Fig. 1, the animal seroconverted to both RV N (Fig. 1A) and HIV-1 Env (Fig. 1B). The anti-RNP response peaked at week 8, with the signal decreasing by 9 weeks after the booster was given (week 16) and then rebounding significantly following administration of the week 19 booster (Fig. 1A). Similarly, reactivity to oligomeric gp140 peaked at week 8, moderated by week 16, and rebounded after the week 19 booster was given (1B). The boosting response at weeks 8 and 20 suggests that ΔG RV, such as ΔG-89.6P-RVG, are reusable vectors in that vector-directed antibodies are not preventing multiple vaccinations.
FIG. 1.
Immune responses after vaccination. (A) Anti-RV RNP response after vaccination with ΔG-89.6P-RVG. The animal received intramuscular, i.v., and subcutaneous inoculations at day 0 and week 7 and an additional i.v. booster on week 19. The positive control is human serum from an RV-vaccinated individual. OD 490 nm, optical density at 490 nm. (B) Anti-HIV-189.6 Env response in a vaccinated animal. Oligomeric HIV-189.6 gp140 was coated onto a microtiter plate and reacted with serial dilutions of rhesus serum from the indicated time points as indicated. Serum from an individual chronically infected with HIV-1 served as a positive control. (C) Western blot analysis of week 8 serum from an immunized macaque. Cell lysates were prepared from uninfected BSR cells (lane 1), cells infected with an empty RV vector (lane 2), an RV vector expressing SHIV89.6P Env containing the cytoplasmic domain of RV G (lane 3), or RV vector expressing SHIV89.6P Env containing the entire gp160 coding region (lane 4).
Seroconversion to SHIV89.6P Env and RV N was also confirmed by Western blotting (Fig. 1C). Week 8 serum reacted with chimeric SHIV89.6P RV G Env (89.6P-RVG) contained in the vaccine (Fig. 1C, lane 3) and also recognized proteins representing gp41 and gp160 from a lysate prepared from cells infected with an RV expressing full-length SHIV89.6P Env (lane 4). This serum also detects proteins of the expected size of RV G and N proteins. The anti-RV G reactivity was initially a concern given that the vaccine did not encode the ectodomain of RV G protein. However, the vaccine did contain the RV G CD, which indicates that this animal generates antibodies directed against the G CD portion of the chimeric envelope. The detection of SHIV89.6P Env, shown in Fig. 1C, lane 4, confirmed that the detected antibodies are also directed against the SHIV89.6P Env portion of the chimeric protein. Preimmunization serum from this animal did not detect any RV- or SHIV89.6P-specific proteins in a similar Western blot carried out in parallel (data not shown). Based on the observed reactivity to SHIV89.6P Env, the animal was challenged with SHIV89.6P, and the postchallenge immune response was monitored.
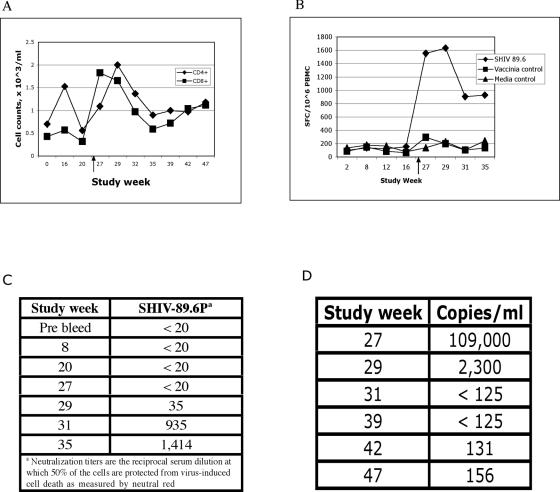
An initial concern in using a live-attenuated vaccine targeted to CD4+ T cells was that cytopathology induced by SHIV89.6P Env could result in measurable CD4+ T-cell death. As Fig. 2A reveals, there was no evidence of CD4+ T-cell decline at any time point pre- or postchallenge. Neither the vaccinations nor the challenge induced detectable loss of CD4+ T cells. One previous study utilizing DNA and recombinant modified vaccinia virus Ankara vectors also reported no evidence of postchallenge CD4+ T-cell loss (1). However, other reports showed vaccinated animals having an acute drop in CD4+ T cells followed by a rebound to near baseline levels (5, 16). Since the course of infection in unvaccinated rhesus macaques is characterized by a rapid and profound loss of CD4+ T cells (13), generally within the first 2 to 4 weeks following challenge, the data shown in Fig. 2A suggest that the ΔG-89.6P-RVG vaccination afforded protection from CD4+ T-cell loss in this animal.
FIG. 2.
Time course of immune cells, viral loads, and anti-SHIV89.6P neutralizing antibodies during immunization and challenge. (A) CD4+ and CD8+ T-cell counts. Whole blood was incubated with antibodies specific for CD3, CD4, or CD8. Data were generated by gating on lymphocytes and CD3 and then through CD4 or CD8. The black arrow indicates SHIV89.6P challenge at week 25. (B) IFN-γ ELISPOT results on pre- and postchallenge time points. PBMC were isolated from whole blood and infected overnight with vaccinia virus expressing the envelope protein of SHIV89.6P, then transferred to an ELISPOT plate for a 5-h incubation. Env-specific responses were determined by comparison to mock-infected cells. A vaccinia virus vector expressing no transgene served as an additional control. SFC, spot-forming cells. The black arrow depicts SHIV89.6P challenge at week 25. (C) SHIV89.6P virus-neutralizing antibody results. The rhesus macaque was challenged with SHIV89.6P at week 25. (D) Viral loads following SHIV89.6P challenge. Postchallenge plasma viremia was determined on plasma samples from the indicated weeks postchallenge in an ultrasensitive branched DNA assay (Bayer Reference Testing Laboratory). Probes specific for SIV239 Gag were used to detect SHIV89.6P RNA in plasma. The assay limit of detection was 125 copies of viral RNA/ml.
To examine the envelope-specific cellular immune response to both the vaccine (ΔG-89.6P-RVG) and the SHIV89.6P challenge, ELISPOT assays were performed for the detection of gamma interferon (IFN-γ)-secreting cells. PBMC were isolated for each time point and infected with recombinant vaccinia viruses overnight and then analyzed in an ELISPOT assay. As demonstrated by Fig. 2B, only background levels of IFN-γ-secreting cells were detected prior to challenge. By 2 weeks postchallenge, however, a robust anti-Env specific response was observed, which peaked 4 weeks postchallenge when more than 1,600 spot-forming cells/106 PBMC were detected. This result corresponds well with the increase in CD8+ T cells observed between 2 and 4 weeks postchallenge (Fig. 2A). The magnitude and time course of the response are in line with previously reported results for HIV-1 or SHIV Env-specific IFN-γ-secreting cells (16).
To determine whether any of the anti-Env antibodies detected in the ELISA assay (Fig. 1B) had neutralizing capabilities, plasma samples from weeks 8 and 20 were submitted for VNA testing. Further, to see whether the monkey generated postchallenge VNA, samples from weeks 27, 29, 31, and 35 were also analyzed. The results are summarized in Fig. 2C. ΔG-89.6P-RVG did not elicit prechallenge VNA at either time point tested. This is consistent with a previous report that also failed to generate prechallenge VNA with an SHIV89.6P Env-based immunogen (3). This animal does generate VNA by 4 weeks postchallenge, with the titers increasing out to week 10 postchallenge. The appearance of postchallenge VNA coincides with the cellular immune response to Env illustrated in Fig. 2B.
We next sought to determine what effect these responses had on the replication of the challenge virus. As Fig. 2D shows, peak viremia occurred 2 weeks postchallenge with 1.1 × 105 copies of RNA/ml. The animal subsequently suppressed the infection to undetectable levels by week 6 postchallenge. The suppression has been maintained at the limit of detection out to 22 weeks postchallenge. This level of control of SHIV89.6P challenge, both in terms of peak viremia observed and days postchallenge when viral loads are at undetectable levels, is unmatched in any previous study. Historically, in this model, peak viremia occurs 2 weeks following challenge, with vaccinated monkeys having between 106 and 107 genome copies/ml and control animals having in excess of 108 genome copies/ml (1, 5, 16, 19). We realize that without concurrent control animals the responses seen here cannot be directly validated. However, previous control animals inoculated with the same stock of SHIV89.6P challenge virus given at the same dose and route of administration displayed the expected outcome from SHIV89.6P infection in naïve animals, as seen by acute CD4+ T-cell loss and peak plasma viremia of more than 107 genome copies/ml within 3 weeks of challenge (16). Further, there are well-documented studies using this challenge model with Env-based immunogens as part of the vaccination regimen that provide additional comparisons for the response observed in this animal (1, 5). It is clear, however, that this ΔG-89.6P-RVG-vaccinated animal has strongly suppressed the challenge infection and remained healthy with no signs of disease throughout the initial follow-up.
DISCUSSION
Preliminary results from this proof-of-principle study show that an SHIV89.6P Env-only immunogen, based on a live-attenuated chimeric rhabdovirus construct, is capable of providing protection from disease in the SHIV89.6P model. Seroconversion to both envelope and RV proteins was seen following immunization, which shows this RV-based vector to be replication competent in vivo. The data further show that this animal had strong cellular and humoral responses to the SHIV89.6P challenge, which resulted in impressive suppression of plasma viremia. This control of viral replication has been maintained to 22 weeks postchallenge. To date, there has been no evidence of CD4+ T-cell loss, and no adverse effects for this animal from either the vaccination or SHIV89.6P infection have been observed.
Only prolonged follow-up will determine whether the suppression of plasma viremia observed in this animal is maintained or whether viral escape from immune control will occur as has been reported previously (2, 4). The initial response in this animal is encouraging given that SHIV89.6P Env was the only vaccine antigen common to the challenge virus used in this study. In previous studies in this nonhuman primate model, HIV or SHIV Env was either excluded (19) or included as part of a multiprotein vaccine (1, 3, 16).
These results provide the foundation, and indicate the need, for future experiments with chimeric viruses expressing additional HIV/simian immunodeficiency virus genes. A larger-scale study with the inclusion of concurrent control animals will serve to give statistical significance to the response observed here and determine whether this level of protective effect can be improved upon or reproduced using a ΔG RV vaccine vector expressing an envelope protein other than SHIV89.6P. Additionally, this study demonstrates that recombinant viral vectors with altered cell tropisms can be targeted to specific cell types, which could have potentially powerful applications beyond HIV-1 vaccine development.
Acknowledgments
We gratefully acknowledge Eileen D. deHaro for her assistance with the ELISPOT assays and M. R. Crab for excellent technical assistance. Numerous reagents were obtained through the AIDS Research and Reference Reagent Program (ARRRP), Division of AIDS, NIAID, NIH.
This study was supported in part by NIH grants AI49153 (to M.J.S.), DK50550P (to A.L.), AI30034 (to D.C.M.), and RR00164 (to the Tulane National Primate Research Center). P.M.M. was supported in part by training grant 5T32AI07523 from the NIH Training Program in AIDS Research.
REFERENCES
- 1.Amara, R. R., F. Villinger, J. D. Altman, S. L. Lydy, S. P. O'Neil, S. I. Staprans, D. C. Montefiori, Y. Xu, J. G. Herndon, L. S. Wyatt, M. A. Candido, N. L. Kozyr, P. L. Earl, J. M. Smith, H.-L. Ma, B. D. Grimm, M. L. Hulsey, J. Miller, H. M. McClure, J. M. McNicholl, B. Moss, and H. L. Robinson. 2001. Control of a mucosal challenge and prevention of AIDS by a multiprotein DNA/MVA vaccine. Science 292:69-74. [DOI] [PubMed] [Google Scholar]
- 2.Barouch, D., J. Kunstman, M. Kuroda, J. Schmitz, S. Santra, F. Peyerl, G. Krivulka, K. Beaudry, M. Lifton, D. Gorgone, D. Montefiori, M. Lewis, S. Wolinsky, and N. Letvin. 2002. Eventual AIDS vaccine failure in a rhesus monkey by viral escape from cytotoxic T lymphocytes. Nature 415:335-339. [DOI] [PubMed] [Google Scholar]
- 3.Barouch, D. H., T. M. Fu, D. C. Montefiori, M. G. Lewis, J. W. Shiver, and N. L. Letvin. 2001. Vaccine-elicited immune responses prevent clinical AIDS in SHIV(89.6P)-infected rhesus monkeys. Immunol. Lett. 79:57-61. [DOI] [PubMed] [Google Scholar]
- 4.Barouch, D. H., J. Kunstman, J. Glowczwskie, K. J. Kunstman, M. A. Egan, F. W. Peyerl, S. Santra, M. J. Kuroda, J. E. Schmitz, K. Beaudry, G. R. Krivulka, M. A. Lifton, D. A. Gorgone, S. M. Wolinsky, and N. L. Letvin. 2003. Viral escape from dominant simian immunodeficiency virus epitope-specific cytotoxic T lymphocytes in DNA-vaccinated rhesus monkeys. J. Virol. 77:7367-7375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Barouch, D. H., S. Santra, J. E. Schmitz, M. J. Kuroda, T.-M. Fu, W. Wagner, M. Bilska, A. Craiu, X. X. Zheng, G. R. Krivulka, K. Beaudry, M. A. Liftom, C. E. Nickerson, W. L. Trigona, K. Punt, D. C. Freed, L. Guan, S. Dubey, D. Casimoro, A. Simon, M.-E. Davies, M. Chastain, T. B. Strom, R. S. Gelman, D. C. Montefiori, M. G. Lewis, E. A. Emini, J. W. Shiver, and N. L. Letvin. 2000. Control of viremia and prevention of clinical AIDS in rhesus monkeys by cytokine-augmented DNA vaccination. Science 290:486-492. [DOI] [PubMed] [Google Scholar]
- 6.Boritz, E., J. Gerlach, J. E. Johnson, and J. K. Rose. 1999. Replication-competent rhabdoviruses with human immunodeficiency virus type 1 coats and green fluorescent protein: entry by a pH-independent pathway. J. Virol. 73:6937-6945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Crawford, J. M., P. Earl, B. Moss, R. C. Reichman, M. Wyand, K. Manson, M. Bilska, J. Zhou, C. D. Pauza, P. W. Parren, D. R. Burton, J. Sodroski, N. Letvin, and D. Montefiori. 1999. Characterization of primary isolate-like variants of simian immunodeficiency virus. J. Virol. 73:10199-10207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Foley, H. D., M. Otero, J. M. Orenstein, R. J. Pomerantz, and M. J. Schnell. 2002. Rhabdovirus-based vectors with human immunodeficiency virus type 1 (HIV-1) envelopes display HIV-1-like tropism and target human dendritic cells. J. Virol. 76:19-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kelley, J. M., S. U. Emerson, and R. R. Wagner. 1972. The glycoprotein of vesicular stomatitis virus is the antigen that gives rise to and reacts with neutralizing antibody. J. Virol. 10:1231-1235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McKenna, P. M., R. J. Pomerantz, B. Dietzschold, J. P. McGettigan, and M. J. Schnell. 2003. Covalently linked human immunodeficiency virus type 1 gp120/gp41 is stably anchored in rhabdovirus particles and exposes critical neutralizing epitopes. J. Virol. 77:12782-12794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mebatsion, T., S. Finke, F. Weiland, and K.-K. Conzelmann. 1997. A CXCR4/CD4 pseudotype rhabdovirus that selectively infects HIV-1 envelope protein-expressing cells. Cell 90:841-847. [DOI] [PubMed] [Google Scholar]
- 12.Moretto, W. J., L. A. Drohan, and D. F. Nixon. 2000. Rapid quantification of SIV-specific CD8 T cell responses with recombinant vaccinia virus ELISPOT. AIDS 14:2625-2627. [DOI] [PubMed] [Google Scholar]
- 13.Reimann, K. A., J. T. Li, R. Veazey, M. Halloran, I.-W. Park, G. B. Karlsson, J. Sodroski, and N. L. Letvin. 1996. A chimeric simian/human immunodeficiency virus expressing a primary patient human immunodeficiency virus type 1 isolate env causes an AIDS-like disease after in vivo passage in rhesus monkeys. J. Virol. 70:6922-6928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Richardson, T. M., Jr., B. L. Stryjewski, C. C. Broder, J. A. Hoxie, J. R. Mascola, P. L. Earl, and R. W. Doms. 1996. Humoral response to oligomeric human immunodeficiency virus type 1 envelope protein. J. Virol. 70:753-762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Roberts, A., L. Buonocore, R. Price, J. Forman, and J. K. Rose. 1999. Attenuated vesicular stomatitis viruses as vaccine vectors. J. Virol. 73:3723-3732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rose, N. F., P. A. Marx, A. Luckay, D. F. Nixon, W. J. Moretto, S. M. Donahoe, D. Montefiori, A. Roberts, L. Buonocore, and J. K. Rose. 2001. An effective AIDS vaccine based on live attenuated vesicular stomatitis virus recombinants. Cell 106:539-549. [DOI] [PubMed] [Google Scholar]
- 17.Schnell, M. J., J. E. Johnson, L. Buonocore, and J. K. Rose. 1997. Construction of a novel virus that targets HIV-1-infected cells and controls HIV-1 infection. Cell 90:849-857. [DOI] [PubMed] [Google Scholar]
- 18.Shacklett, B. L., B. Ling, R. S. Veazey, A. Luckay, W. J. Moretto, D. T. Wilkens, J. Hu, Z. R. Israel, D. F. Nixon, and P. A. Marx. 2002. Boosting of SIV-specific T cell responses in rhesus macaques that resist repeated intravaginal challenge with SIVmac251. AIDS Res. Hum. Retrovir. 18:1081-1088. [DOI] [PubMed] [Google Scholar]
- 19.Shiver, J., T. Fu, L. Chen, D. Casimiro, M. Davies, R. Evans, Z. Zhang, A. Simon, W. Trigona, S. Dubey, L. Huang, V. Harris, R. Long, X. Liang, L. Handt, W. Schleif, L. Zhu, D. Freed, N. Persaud, L. Guan, K. Punt, A. Tang, M. Chen, K. Wilson, K. Collins, G. Heidecker, V. Fernandez, H. Perry, J. Joyce, K. Grimm, J. Cook, P. Keller, D. Kresock, H. Mach, R. Troutman, L. Isopi, D. Williams, Z. Xu, K. Bohannon, D. Volkin, D. Montefiori, A. Miura, G. Krivulka, M. Lifton, M. Kuroda, J. Schmitz, N. Letvin, M. Caulfield, A. Bett, R. Youil, D. Kaslow, and E. Emini. 2002. Replication-incompetent adenoviral vaccine vector elicits effective anti-immunodeficiency-virus immunity. Nature 415:331-335. [DOI] [PubMed] [Google Scholar]
- 20.Wiktor, T. J., E. Gyorgy, D. Schlumberger, F. Sokol, and H. Koprowski. 1973. Antigenic properties of rabies virus components. J. Immunol. 110:269-276. [PubMed] [Google Scholar]
- 21.Yeghiazarian, T., Y. Zhao, S. E. Read, W. Kabat, X. Li, S. J. Hamren, P. J. Sheridan, J. C. Wilber, D. N. Chernoff, and R. Yogev. 1998. Quantification of human immunodeficiency virus type 1 RNA levels in plasma by using small-volume-format branched-DNA assays. J. Clin. Microbiol. 36:2096-2098. [DOI] [PMC free article] [PubMed] [Google Scholar]