Policy Points:
Effectively addressing low‐value care calls for engaging the public, including the one‐third of Americans who currently cannot envision benefits from avoiding low‐value care.
Public awareness of and response to low‐value care can be enhanced through revised media messaging. These efforts are more effective if they emphasize health risks rather than the financial costs associated with unnecessary tests and treatments.
Long‐term robust public support for addressing low‐value care may require shifting the focus from particular tests and treatments to emphasize, instead, the potential for better communication and more personalized attention if clinicians spend more time talking and less time testing.
Context
As much as 30% of US health care spending may be unnecessary. The Choosing Wisely campaign, now active in a dozen countries, addresses this problem in part through public education campaigns. This article explores Americans’ understanding of low‐value care in 2015, assesses the impact of media messaging, and tests alternative message framing.
Methods
We use a mixed‐methods design incorporating (1) 8 focus groups exploring Americans’ understanding of and language for low‐value care, (2) 48 intensive interviews with patients on their interactions with physicians regarding questions of cost and value, (3) a national survey of 920 respondents examining their awareness of low‐value care, and (4) a survey experiment with 785 participants, testing the impact of media messages on attitudes about low‐value care, treatment choices, and selection of a primary care clinician.
Findings
One‐third of Americans have difficulty envisioning benefits from avoiding low‐value care, a figure that increases to half for less educated and minority respondents. Most Americans who anticipate benefits hope that less testing and treatment will be replaced by more interactive and personalized care. Even without media priming, many Americans would avoid common forms of low‐value care like unnecessary antibiotics or excess imaging for lower back pain, but few favor clinicians who avoid these practices. Although the public's awareness and actions are increased and disparities are reduced by media messaging, conventional messages also exacerbate the blame placed on providers. Avoiding low‐value care is enhanced, blaming providers is reduced, and disparities are further diminished if messages put more emphasis on the health risks of these tests and treatments.
Conclusions
The public's awareness of low‐value care is incomplete, with substantial disparities related to race, ethnicity, and socioeconomic status. Media messaging can help fill these gaps but, in the short run, would be enhanced by fine‐tuning how low‐value care is characterized. In the longer run, building robust public support for reducing low‐value care may require refocusing attention away from specific tests and treatments and toward the relational benefits for patients if clinicians spent less time on testing and more time on personalized care.
The institute of medicine estimates that 30% of health care spending in the United States—approximately $750 billion per year—is unnecessary.1 This is not a new discovery. For more than a quarter century, research has documented the extensive prevalence of low‐value tests and treatment, in both the United States and other countries.2 Yet it has proven difficult for US policymakers to reduce this seemingly wasteful spending, in large part because the American public remains deeply skeptical about government interventions into their medical care.3
Enter the Choosing Wisely campaign, stage right. This initiative, launched in 2012 by the American Board of Internal Medicine (ABIM) Foundation, represents an effort to reduce low‐value care without government action,4 leveraging professional norms to induce this change. By enhancing physicians’ commitment to stewardship over collective resources, it encourages medical societies to create evidence‐based lists of those tests and procedures most often overused.5
Once lists of low‐value tests and treatments are endorsed by medical societies, reductions in their use are expected to diffuse into clinical practice. Echoing Kahneman's Thinking, Fast and Slow, proponents of Choosing Wisely postulate that many low‐value tests and treatments are ordered by clinicians in a routinized way. Therefore, if clinicians become less hasty and more mindful, the prevalence of these practices could decline substantially.6, 7
Choosing Wisely has successfully induced a widespread response from the medical profession. More than 80 medical societies in the United States have joined the campaign, generating and promoting their own lists of unnecessary tests and procedures. In addition, 21 state‐level initiatives have been launched, including several that sponsor quality report cards on clinicians that now incorporate metrics of low‐value tests and treatment.5 Comparable initiatives have also been established in a dozen countries, with distinct names like “Smarter Medicine” (Switzerland) or “Slow Medicine” (Italy).8
To date, however, the impact on clinical practice has been far less impressive. Although clinicians do appear to respond to targeted education involving Choosing Wisely metrics,9 broader trends in the prevalence of tests and procedures identified in the Choosing Wisely lists have been inconsistent: some have declined, some have increased, and others have remained unchanged.10, 11 Even the positive trends have been very modest in magnitude.
To be sure, these interventions are still new, and changes in clinical practice often take many years to diffuse fully.12 Nonetheless, there are reasons to suspect that a crucial ingredient for slower medicine to take hold may as yet lack sufficient dosage: revised patient expectations, which can either constrain or facilitate clinicians’ ability to reduce low‐value care. Many patients now seek specific tests or procedures or insist on quick interventions because they feel the pressure of work and home responsibilities. Clinicians find such requests difficult to refuse,13 even when they recognize that acquiescing will have little clinical benefit.14
The architects of Choosing Wisely recognized that the public's understanding and acceptance were linchpins of the campaign: “Patients and the public also hold the view that ‘more is better’ in medical care and a Choosing Wisely campaign can only be effective with significant patient and public engagement.”8 At the campaign's inception, the ABIM Foundation partnered with Consumer Reports to enhance its capacity to understand and communicate with the public. By 2014, proponents estimated that media coverage had reached roughly 100 million Americans. Complementary outreach efforts by national mass membership groups and state‐level quality‐improvement coalitions targeted additional messages to between 15 and 20 million people.
Nonetheless, 5 years after Choosing Wisely was launched, we still have very little sense of the public's basic understanding of low‐value care, the perceived salience of low‐value tests or treatments for their own medical care and health care–related choices, or the potential impact of the campaign's messaging on the public's awareness or attitudes. After interviewing 14 experts in the field during the spring of 2016, Consumers Union (the advocacy arm of Consumer Reports) described “the absence of data on how to communicate information about high‐ and low‐value treatments to patients…as a critical, foundational research gap.”15
The study reported here was designed to begin filling this gap. We started by integrating the conceptual literature on message framing with empirical research on consumers’ understanding of cost and value and used this integrated review to examine the specific strategies for attitude change that Choosing Wisely pursued. This review revealed some specific gaps in the existing evidence, which we address in the second section of this article, drawing on findings from the first 3 stages of our study: (1) focus groups, (2) intensive interviews with patients, and (3) a nationally representative survey of the American public. Based on these exploratory analyses, we identified patterns and disparities in how Americans think and talk about low‐value care, which in turn suggested some hypotheses regarding how Choosing Wisely's approach might be refined to enhance the public's understanding and to mitigate disparities. In the third section of this article, we test these hypotheses using a subset of plausible new frames incorporated into a survey experiment with a nationally representative sample. The article concludes with some reflections on the implications of our findings for consumer education, delivery system reform, and health policy.
Conceptual Foundations: Consumer Messaging and Framing
Experts agree that “value” in health care is a complicated concept with many different aspects and that it is understood in different ways by clinicians, scholars, and the general public.15 The efficacy of any intervention designed to alter how people think about and respond to value in health care therefore depends significantly on “framing,” that is, calling attention to particular facets of the concept in order to influence subsequent perceptions, attitudes, and choices.16 Past research demonstrates that framing effects can substantially alter the public's attitudes toward illness, health care, and health policies.17, 18 For example, different descriptions of policies have been shown to alter public support for policies addressing low‐value care.3 Yet no comparable research to date has examined how framing low‐value care itself might influence patients’ attitudes or choices regarding their own health needs or interactions with clinicians.
Choosing Wisely's core strategy involved persuading clinicians to become more mindful and judicious in prescribing tests and treatment.5, 7 The campaign found routinized interactions with patients—and the hurried encounters often seen as their cause—as a primary source of wasted medical resources.7, 19 Routinized care is not inherently “bad” because it generally fits the needs of the typical patient. But relying on practices suitable for the modal patient often fails to adequately account for a patient's particular circumstances, experiences, or preferences.20
Choosing Wisely's messaging targeted to patients initially centered on encouraging them to engage their clinicians in conversations about treatment choices.5 This early emphasis reflected the researchers’ belief that shared decision making could disrupt routinized clinical practices, reducing both excessive testing and aggressive treatment.21, 22 But this initial strategy did not prove to be consistently effective, because a substantial number of patients advocated for the very tests and treatments that Choosing Wisely sought to reduce.13, 14, 23
Over time, the Choosing Wisely campaign adapted its strategies and began encouraging consumers to actively question prescribed tests and treatments. The campaign disseminated a 5‐question script to help patients “talk to your doctor about which tests, treatments, and procedures you need—and which you don't need.”24 Beginning in 2014, a third strategy emerged as a handful of state quality‐improvement coalitions incorporated new measures, which were based on Choosing Wisely's recommendations, into physicians’ report cards. These were intended to encourage consumers to consider the metrics of low‐value care as one way to assess clinicians’ practices, inducing consumers to select clinicians with more conservative practice styles.25
Strategies for conveying Choosing Wisely's messages to the public have varied, with different approaches emerging from the ABIM Foundation nationally, from each of the nationwide membership groups, and from the state‐level Choosing Wisely coalitions. Our comprehensive review of the campaign's media coverage between 2012 and 2014 (described in more detail later), as well as our analysis of the campaign's own print and web‐based materials, revealed 4 distinct messages that were incorporated (albeit with varying degrees of consistency) into print or televised coverage.
The first 2 were intended to increase the public's concern about low‐value care, identifying it as (1) wasteful for society (the most common framing) and/or (2) potentially harmful to patients8: “Some medical tests, treatments, and procedures provide little benefit. And in some cases, they may even cause harm.”5 The third theme characterized physicians as activated to reduce low‐value care as reflected in the actions of individual clinicians and medical societies: “With governments and insurers bemoaning the soaring costs of health care, the medical profession is increasingly offering its own solutions.”26 A fourth theme appears in coverage more sporadically: a call for patients to question their doctors’ recommendations, echoing a major component of Consumer Reports’ public education campaign, which encouraged patients to “Just Say Whoa” to their clinician for some common tests and procedures.24
There is little published research on the impact of the Choosing Wisely campaign on public perceptions, although a smattering of evidence suggests that many Americans are now aware that particular tests or treatments may be unnecessary.27, 28 Research on the public's understanding and preferences regarding the role of cost in clinical decisions,29, 30 however, suggests that changing consumers’ attitudes and behaviors with respect to low‐value care may not be easy. Findings from this research on cost highlight several specific challenges for changing attitudes and expectations with respect to low‐value care.
First, most Americans remain poorly informed about the costs and benefits of particular treatments.24 Second, many patients still seek tests or treatment even when informed that they are unlikely to yield much benefit, because they have been conditioned to fear rare, life‐threatening events.31 Furthermore, many patients proceed with low‐value treatment either because they distrust the evidence of its low value presented to them or because they suspect that the resources saved will only bolster insurer's/provider's profit margins rather than benefit the public.29, 32, 33
In short, because Americans do not appear easily willing to trade the perceived quality or the unfettered quantity of care for lower costs,34 embracing Choosing Wisely's foundational assumptions and core media messages may require a “culture shift” in the public's expectations.14 The campaign's founders recognized this challenge early on, but it remains unclear whether their dominant focus on “waste” to motivate change is compatible with Americans’ individualistic conceptions of value in health care settings. To date, however, the import of these potential impediments remains unclear and the potential for alternative framing has yet to be explored.
First‐Stage Empirical Research: Qualitative Explorations
Research Methods
The exploratory stage of our research combined 3 different methods of data collection: focus groups, intensive interviews, and a national survey incorporating open‐ended questions regarding low‐value care.
Focus Groups
The focus groups were designed to test ways to describe, measure, or frame the concept that not all tests or treatments are necessary or beneficial. In the winter of 2014/2015, we convened 8 groups, with 82 participants, in the Midwest, South, Mid‐Atlantic, and New England (the last in conjunction with Connecticut's Choosing Wisely Coalition). In order to facilitate communication, each group was relatively homogeneous in sociodemographics and health experiences. As a complete set, the focus groups varied in attributes identified in the literature as potentially influencing their acceptance of conservative practice styles: race/ethnicity, socioeconomic status, health status, and geographic region.
Intensive Interviews
Drawing on insights about the value of personalized care evident from our focus groups, we interviewed a representative sample of 48 patients to get a deeper understanding of whether and how patients discuss low‐value care and costs with their own clinicians. The low‐value care questions piggybacked on an existing study of experiences with medical care, interviewing 48 respondents who had visited their clinician in the past year, drawn from a nationally representative internet panel.35 The sample was then stratified into (1) panelists who had a chronic condition requiring regular medical attention, (2) panelists who had had a serious or life‐threatening illness/injury in the past 12 months, and (3) “healthy” respondents who met neither criterion. We asked the interviewees if their clinicians had talked with them about tests or treatments being potentially excessive, unnecessary, or unduly expensive. Approximately 50% of the respondents reported such interactions, and we encouraged them to provide details.
National Survey
We collected data in April 2015 from a standing internet panel of more than 60,000 households recruited and maintained by the research firm GfK (formerly Knowledge Networks). This panel is generally representative of the American public in sociodemographics, internet usage, and health status.36 As evident from Table 1, our sample was slightly older and therefore more likely to be white and to report worse‐than‐average self‐rated health. But the sample contained a sufficient number of nonwhite (28%) and healthy (43%) respondents to allow us to stratify our subsequent analyses according to these attributes.
Table 1.
Characteristics of Low‐Value Care Study Sample Compared With US Population
| Characteristic | Study Sample (%) n = 784 | US Population (%) |
|---|---|---|
| Sociodemographics | ||
| Age | ||
| <30 | 17.0 | 21.5a |
| 30–44 | 21.6 | 25.5 |
| 45–60 | 28.1 | 27.1 |
| >60 | 33.4 | 25.8 |
| Race/Ethnicity | ||
| White | 72.4 | 66.0 |
| African American | 9.7 | 11.6 |
| Latino | 9.6 | 15.0 |
| Other | 8.3 | 7.5 |
| Education | ||
| High school or less | 38.9 | 42.2 |
| Some college | 29.7 | 28.9 |
| College graduate | 31.4 | 28.9 |
| Health status and utilization | ||
| Chronic health problems | ||
| Yes | 41.1 | 49.8b |
| Self‐reported health | ||
| Fair/poor | 15.2 | 12.9c |
| Good | 37.4 | 26.7 |
| Very good/excellent | 47.3 | 60.3 |
US Census, Statistical Abstract of the United States: 2012. Washington DC: U.S. Department of Commerce.
Ward BW, Schiller JS, Goodman RA. Multiple chronic conditions among US adults: a 2012 update. Prev Chronic Dis. 2014;11:E62.
Blackwell DL, Lucas JW, Clarke TC. Summary health statistics for U.S. adults: national health interview survey, 2012. Vital Health Stat 10. 2014(260):1‐161.
A total of 920 panelists joined the study (a participation rate of 76%). They completed an 11‐question initial survey on health status, medical consumerism, and attributes they valued in a clinician. For exploratory purposes, the respondents were asked 1 open‐ended question about their expectations of clinicians who avoided low‐value care. The wording drew on language used by the participants in our interviews and focus groups:
People will sometimes talk about doctors being especially good at avoiding tests and treatments that are likely to have more risk than benefit. If you were to hear or read that a particular doctor was good at this, what—if anything—would you expect them to do differently from most other doctors?
Following conventional grounded‐theory methods, we developed a coding scheme based on an iterative analysis of the responses. Two graduate students, supervised by the project's research coordinator, then independently used this scheme and double‐coded all the responses. We then adjudicated any inconsistencies in their coding.
Findings From the Exploratory Research
We present our findings here in 4 stages, each of which incorporates the data generated using all 3 research methods. We begin by (1) describing how the public perceives and describes what researchers characterize as “low‐value” care (and what Choosing Wisely labels as “waste”8). We then examine (2) what Americans perceive as the primary benefits yielded by avoiding these unnecessary tests and treatments, and (3) their comfort with various interventions intended to reduce the prevalence of such tests and treatments. We conclude by identifying (4) some notable sociodemographic disparities in these attitudes, perceptions, and expectations.
Public Perceptions of and Lexicon for Low‐Value Care
Although Choosing Wisely conveys in its public messaging that low‐value care is either wasteful, harmful, or both, few respondents in either the focus groups or the intensive interviews used terminology consistent with this framing. Consistent with previous studies,8, 23, 27, 29, 33 we found that the mention of cost considerations was generally viewed unfavorably, even by those respondents who had the greatest difficulty paying for medical care. The intensive interviews, which probed explicitly on patient‐clinician interactions regarding appropriate testing, found that cost rarely entered into these conversations in an explicit manner, even when patients were interacting with trusted clinicians. Indeed, only about 15% of all the respondents mentioned cost as part of their clinical interactions.
Most of the healthy respondents had difficulty envisioning how health care, particularly testing, could be harmful to patients. This possibility was more readily understood by respondents with a history of serious illness, many of whom reported personal exposure to duplicated tests and iatrogenic health problems. More commonly, patients were concerned about the opportunity costs (such as loss of time at work) of tests or treatments that had little clinical value. Concerns about the burdens of low‐value or duplicative testing were expressed most strongly by lower‐income respondents, whose life circumstances often make it challenging to find time for needed medical care. Consistent with previous research, we found that the participants in our research described personal burdens as far more salient than general notions of “waste” or the encumbrances of health care spending for society as a whole.8, 29, 33
The concept of “clinical practice style” highlighted a particularly striking discordance between the presumptions embodied in Choosing Wisely and public perceptions. The campaign is predicated on evidence that many clinicians, particularly specialists, are predisposed to test or treat aggressively.37 Messages directed to the public (rather than to specialty societies) emphasize that this predisposition ought to be challenged by patients either through repeated questioning of clinicians or by selecting clinicians who abjure low‐value care. However, we found that the term “practice style” had little meaning for most focus group participants. In fact, many found the notion alienating either because it implies their clinician may be “practicing” on them in an experimental manner, or because it suggests their clinician might have a generic “style” for all patients rather than the important capacity to personalize care for each patient.
These findings were reinforced by analyzing the responses to the open‐ended national survey question (Figure 1). By asking the respondents to envision and describe doctors who avoid low‐value care, we were able to elicit specific expectations about what such care would involve. Roughly two‐thirds of respondents had some sense of what low‐value care might entail, though many were uncertain about the specifics (see the left‐hand bars in Figure 1). Many who did volunteer a description of what low‐value care might entail characterized it exclusively in terms of testing rather than treatment. Perhaps as a result, few respondents (5.6%) anticipated that excessive medical care might harm patients. More surprising, very few respondents (roughly 1%) volunteered a response that linked low‐value care to medical costs, either personal or societal.
Figure 1.
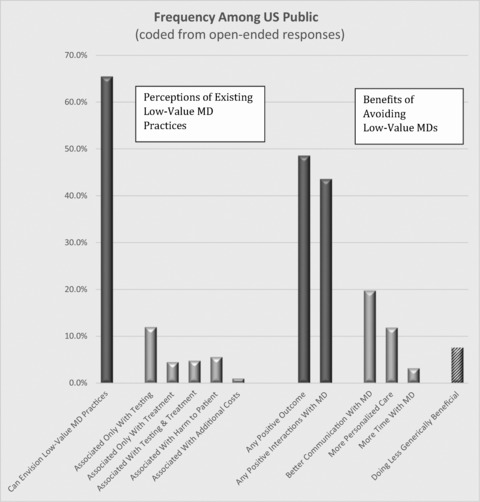
American Public's Perceptions of Low‐Value Care, Spring 2015
Roughly a third (34.5%) of respondents were unable to articulate anything meaningful about low‐value practices. Their limited understanding poses challenges for any public‐facing campaign like Choosing Wisely. We will return to this group when evaluating the survey experiments.
Anticipated Benefits from Avoiding Low‐Value Care
Three‐quarters of those who had some understanding of low‐value care anticipated some concrete benefits from reducing its prevalence (74% of those who offered an explanation, and 48.6% of all participants; see the right‐hand bars in Figure 1).
A small proportion (7.6% of the sample) anticipated that just doing less could be beneficial in itself. But most of the respondents expected that if clinicians were doing less testing and treatment, they might turn their attention to something else more valuable—and the majority anticipated that this would involve more extensive or responsive interactions with patients.
Improved communication was cited most frequently as a beneficial aspect of avoiding low‐value care (19.8% of all respondents). More specifically, the respondents anticipated 2 distinct changes. First, they expected that spending less time ordering and reading tests would allow clinicians more time to talk with their patients. Second, they projected that taking a more mindful, less routinized approach to testing would encourage discussion of the benefits and limitations of each approach and greater acknowledgment of clinical uncertainty (Table 2).
Table 2.
Survey Respondents’ Verbatim Descriptions of Expected Benefits From Avoiding Excess Testing and Treatment
| Theme | Illustrative Examples |
|---|---|
| Better Communication With Doctor | |
| Talking in lieu of testing | |
| Listen very well and recommend a separate opinion. Take additional time in the visit with you to truly listen to your complaints. Ask me more questions and listen to the answers. Listen to the patient to really understand what is going wrong with them. | |
| Acknowledging clinical uncertainty | |
| Carefully explain the tests and tell why/why not he/she would recommend that specific test. I would expect to get an honest answer to the question, “If you were in my situation, what would you do?” | |
| I would expect them to take time to explain the tests, the risks, perhaps recommend a second opinion. Talk about the research studies about the reliability of the test. And I would like for them to let me know if they would recommend it to their own family member. | |
| I would expect them to explain their rationale for recommending (or not recommending) tests and treatments. I also expect them to be always skeptical that they have all the answers, since my personal experience has shown conventional medical protocols are always changing. | |
| Check benefits and risk. Give me his honest opinion on what he would do if this was his wife. Answer any questions I have honestly. | |
| More Personalized Care | |
| Shared decision making | |
| Be less aggressive, inform of risks associated with tests and help me evaluate pros and cons of tests. | |
| Explain it in detail so I would be able to make the final decision. | |
| They would weigh the pros and cons about applying a certain treatments and tests, and would explain them to you, so you both could decide what would be the best way to go about it. | |
| Try and explain the pros and cons so I can make an educated decision. | |
| More active watchfulness (while waiting) | Explain all the alternatives and set time line of when the testing may be ordered based on symptoms. |
| Follow up frequently with me until the need for the tests and treatment can out way the risks. | |
| Watch the problem in question by closely monitoring and having follow‐up appointments or a call‐in follow‐up more often to evaluate progress. | |
| I would hope that the doctor could provide me with instructions on how I could monitor my own health at home with a clear sense of when tests/treatments could become necessary. | |
| Staged Testing/Treatment | |
| Conduct simpler tests/treatments first | Talk to patients one on one. Try some light prescription that he has had satisfactory results with, that have minor or no side effects. |
| I would expect my doctor to do only the medical tests absolutely necessary. I would be trusting him to know what my problem is w/o having to rely completely on medical tests to give him clues. I want him/her to use his head. | |
| I expect him/her to only order test that they feel fit the things that I came to them complaining about. Start with the least expenses and invasive procedures and then go up. To me this would be different than seeing me 15 minutes and then start ordering everything under the sun. | |
| They would offer up different ideas and more moderate treatments first to see if they make any difference. Only after those don't work would they then consider more risky treatments. | |
A second source of improved interactions, anticipated by 11.9% of the respondents, involved more personalized medical care. Doing less and being less routinized was expected to allow clinicians to think more and to engage patients in shared decision making. A number of respondents expected these interactions to transform “watchful waiting” into more active forms of watchfulness, with clinicians and staff reaching out to proactively monitor patients’ well‐being in between visits and/or to assist patients to be more effective at self‐monitoring (see Table 2).
Choosing Wisely was constructed and framed for clinicians as a careful, evidence‐based accounting of the value of particular tests and procedures. Our results suggest, however, that the transition in focus from professional to public legitimacy may call for a shift away from the specificity of the renowned Choosing Wisely lists to address instead the broader context of clinician‐patient relationships within which testing and treatment decisions are made. The potential benefits of this shift in focus were reinforced by our intensive interviews: those patients who described being comfortable in conversations with clinicians who were attentive to low‐value care were those who had the most established, trusting relationships with their clinicians.
Acceptance of Approaches to Reducing Low‐Value Care
About half of the 48 interview respondents reported some interaction with their doctors about the value of particular tests or treatments. Many described being most receptive to avoiding low‐value care when their clinicians suggested a “staging” strategy, beginning with a less complex option (eg, an X‐ray) and proceeding to a more elaborate stage (eg, a CAT scan or MRI) only if necessary. Even though some clinicians were clearly triaging care in ways that their patients perceived as cost saving, they rarely justified staging to patients in those terms. Rather, physicians emphasized efficacy in initial diagnosis/treatment, avoiding a test that was “useless” or “trying this option first” before something more invasive or intensive.
This staging predisposed patients to less intensive interventions, at least as a first option. All depended on thoughtful communication with a trusted physician. Although our respondents were generally averse to factoring cost directly into care decisions, those few whose physicians mentioned cost as part of a staged approach were amenable to figuring cost into the equation as long as there was a clear clinical rationale and assurances that more costly procedures would be deployed if or when necessary. In the words of one respondent, “And so, he'll run the cheaper things and do the cheaper things first and see if that helps before pursuing anything else.”
Disparities in Understanding and Perception of Low‐Value Care
During their initial implementation, health education and health promotion campaigns often exacerbate socioeconomic disparities in public awareness,38, 39 because better‐educated members of the public monitor media coverage of health issues more closely and learn more quickly about and from emerging initiatives.40 Given the recent emergence of concerns about low‐value care into public discourse, we thus expected comparable disparities in this context, and they were in fact evident in our survey data.
Disparities with respect to education follow a predictable pattern: respondents with more education were more aware of low‐value care in clinical practice and were more positive, overall, about avoiding excess testing and treatment. Differences across educational strata were substantial: respondents who had not completed high school were two and a half times as likely as college graduates to not offer a description of what it would mean for a clinician to avoid low‐value care (Table 3, top row). Strikingly, this least‐educated strata of respondents were only half as likely as college graduates to anticipate any benefits from clinicians who avoided low‐value care (Table 3, bottom row).
Table 3.
Sociodemographic Disparities in Perceptions of Potential Benefits of Reducing Low‐Value Care
| By Subpopulation* | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Educational Attainment | Race/Ethnicity | ||||||||
| Perception | Overall Prevalence (%) | Some High School (%) | High School Grad (%) | Some College (%) | College Grad (%) | White (%) | Black (%) | Latino (%) | Other (%) |
| Limited knowledge | |||||||||
| Unable to describe impact of low‐value care | 36.9 | 52.8 | 49.0 | 32.6 | 17.9 | 32.0 | 44.1 | 48.0 | 45.6 |
| Interactional benefits of reduced low‐value care | |||||||||
| Better communication | 19.0 | 16.4 | 9.9 | 22.3 | 26.0 | 17.8 | 27.8 | 17.5 | 19.2 |
| More personalized care | 10.1 | 3.1 | 4.7 | 14.0 | 14.5 | 11.5 | 9.8 | 4.7 | 8.3 |
| More cautious treatment | 7.2 | 8.2 | 3.2 | 5.5 | 12.4 | 7.3 | 13.8 | 2.8 | 4.4 |
| More time with doctor | 2.8 | 0.4 | 2.9 | 1.4 | 5.0 | 2.5 | 3.3 | 2.0 | 5.8 |
| Any anticipated benefit | 47.6 | 31.5 | 40.0 | 53.9 | 55.6 | 48.3 | 42.6 | 46.0 | 52.1 |
*Weighted to account for uneven survey participation rates.
Disparities in perceptions of low‐value care related to race and ethnicity also were notable. Respondents from all minority groups were less likely than whites to be able to describe what avoiding low‐value care might entail. Of those who understood what low‐value care entailed, we found no statistically significant differences between minority and white respondents in who could identify at least one positive benefit, though the nature of these anticipated benefits varied somewhat across subgroups.
Additional insights can be gleaned from multivariate regression analysis. We estimated two models, the first predicting the respondents’ understanding of low‐value care and the second whether the respondents identified any anticipated benefits from avoiding excess testing and treatment. Education, racial and ethnic background, age, gender, and health status (whether the respondent had a chronic condition requiring medical monitoring or a critical health crisis in the previous 12 months) were the explanatory variables.
The regression analyses revealed that after accounting for differences in educational attainment and health status, both blacks and Latinos expressed less understanding of low‐value care (this was only borderline statistical significance, given the small sample sizes, but a fairly large substantive difference). Controlling for other sociodemographic differences, the education gradient in understanding low‐value care persisted, but statistically significant differences emerged only for respondents with at least some college, compared with those with less education.
By contrast, racial and ethnic differences in overall anticipated benefits largely vanished after controlling for other sociodemographics, though African Americans appeared less likely to anticipate a benefit of stronger relationships with doctors who avoided low‐value tests and treatment. A strong educational gradient persisted in perceived benefits, particularly for respondents who had completed college. It was this subset of respondents who most anticipated that avoiding excess testing and treatment would lead to more personalized care, anticipating this benefit twice as frequently as did the respondents with limited education.
Hypotheses Derived From the Exploratory Research
We derived from these findings several more concrete hypotheses regarding the potential impact of reframing Choosing Wisely messages for the public.
First, the proponents of Choosing Wisely anticipated that “framing unnecessary care as waste” would also imply to patients that they were “unduly at risk for harm.”5 However, because most Americans think about waste largely in terms of testing and few see tests as potentially harmful, this inference seems unlikely. Instead, effective behavior change may require more direct framing strategies that emphasize harm to patients in order to convey this threat.
Second, for many Americans, proposals to reduce “waste” raise the specter of rationing care, thereby alienating them from these initiatives even if they can envision benefits from less testing and treatment. To avoid inducing this countervailing reaction, it may be important to articulate an alternative vision more consistent with the staged testing and treatment that emerged as a theme from our focus groups.
Third, because of disparities in the public's understanding of low‐value care and in the perceived benefits of reducing such testing and treatment, the conventional Choosing Wisely approach may exacerbate socioeconomic and racial/ethnic differences in public support. By contrast, alternative approaches to framing may mitigate this problem. Messaging that makes explicit the potential harms of excessive testing and treatment might galvanize action among minorities already less trusting of medical care. Approaches that emphasize staged testing or treatment may also feel safer to minority patients who fear being excluded from needed medical care.
The Survey Experiment
We constructed our survey experiment to test these hypotheses. In the process, we also hoped to generate insight about Americans’ willingness to avoid tests and treatments of questionable value, their propensity to use metrics of low‐value practices in selecting a clinician, and the impact of media messages regarding low‐value care on all these outcomes. To minimize any potential bias that our preliminary survey might create for subsequent experimental results, the participants were invited back to complete the experiment one week after the preliminary survey. In all, 784 participants reengaged, an 85% follow‐up rate with no evident biases related to sociodemographics or consumer activation.
Survey Experiment Methods
Experimental Priming
To test the impact of media messaging, we randomly assigned the participants in the experiment to read 1 of 4 newspaper stories. The baseline story was a shortened (305 words) version of actual coverage of the Choosing Wisely initiative, published in April 2012 (see the exact wording in Appendix A, online). The control group was presented with a story of equal length and similar tone, but written to convey the virtues of having clinicians pay more attention to the emotional aspects of patient‐physician interactions (see the specific wording in Appendix B, online).
To test plausible alternative frames for addressing low‐value care, we randomly assigned the participants from the 2 other arms modified versions of the original Choosing Wisely coverage. We based these alternatives on insights from our exploratory research, just described. We constructed each alternative framing by making modest changes in the wording of the base‐line Choosing Wisely coverage (see the wording in Appendices C and D, online, with the modifications in italics).
The first alternative framing emphasized the possible health threats posed by excessive testing and treatment—a minor theme in conventional coverage that was moderately emphasized in the revised coverage. (These revisions changed less than 10% of the text of the original article; see Appendix C.) We hypothesized that this alternative would induce a larger behavioral response than the response to the conventional coverage, for two reasons. First, it balanced the anxiety caused by forgone tests and treatment with an equally emotional threat from too much treatment. Second, it underscored the salience of a personal threat to health, rather than the more diffuse concern about wasting societal resources on unnecessary medical care.
The second alternative story emphasized the potential for staged deployment of tests and treatment, starting with simpler, lower‐cost interventions and incorporating more elaborate interventions only if needed. This framing was designed (1) to be consistent with the more watchful waiting and careful testing described by the respondents in our focus groups, interviews, and national survey (Table 3, lower portion) and (2) to replicate the triaging process that was described positively in a good number of the intensive interviews. This version altered roughly 15% of the text of the original media coverage (see Appendix D).
After the respondents had read the media story to which they were randomly assigned, they were asked to recount in writing the key elements of the story as if they were summarizing it for family and friends. These summaries become our primary evidence for identifying which key messages and potentially unintended connotations were conveyed through different framings of low‐value care. Again, following the methods of grounded theory, we created a coding scheme that identified the key contents of these responses.
Our primary coding focused on discerning whether the respondent perceived in the story each of Choosing Wisely's 4 core messages: waste, harm, clinicians are activated to avoid unnecessary tests and treatments, and whether patients should question the value of suggested tests and treatment. As the coders applied the scheme to the data, they refined it in order to identify other responses that emerged more inductively. These included the participants’ emotional responses to reading about low‐value care, as well as the extent to which they blamed particular actors (clinicians, drug companies) for excessive testing and treatment. Here again, the responses were independently double‐coded by a team of graduate students.
Postexposure Assessment
To assess the impact of priming on consumers’ behaviors, we directed the participants to a physician‐choice website (SelectMD), successfully deployed in previous experiments using online panels of participants.41 The participants were given star‐rated performance metrics on each of 12 clinicians regarding their patient survey scores, clinical performance, and avoidance of low‐value care, and then they were asked to choose among the doctors. The low‐value care measure incorporated the 4 metrics that our focus groups found most meaningful: (1) avoiding excessive antibiotics, (2) reduced screening for back pain using radiation, (3) palliative rather than aggressive treatment at end of life, and (4) substituting generic drugs for branded pharmaceuticals. (The first 2 measures are already in use on websites maintained by several states’ quality‐improvement coalitions.)
The physician‐choice set was designed so that trade‐offs were unavoidable: selecting a clinician top‐rated for avoiding low‐value care meant sacrificing a top rating for either patient surveys or clinical performance. Because past research suggests that the avoidance of low‐value care is correlated with other metrics of clinical performance, the star ratings for pursuing Choosing Wisely objectives are positively correlated (r = 0.50) with The Healthcare Effectiveness Data and Information Set (HEDIS) star ratings. However, both HEDIS and Choosing Wisely star ratings are uncorrelated with ratings from the patient‐experience surveys, consistent with previous findings from the literature.42 After choosing a clinician, all the participants completed a 17‐question survey, which contained both open‐ and close‐ended questions about their choice process, the attributes they most valued in clinicians listed on the website, and what sorts of information they would seek in making real‐world choices of clinicians in the future.
Among these additional questions, respondents were presented with several clinical choice scenarios, in which they were asked to choose between aggressive treatment and watchful waiting for each of 4 conditions and to choose between clinicians who practiced in a more aggressive or a more conservative manner for 5 different conditions. We report here on the 2 conditions for which we asked the respondents about both treatment choice and clinician choice: (1) cancer screening and (2) use of antibiotics for a persistent cough.
In the treatment‐choice scenarios, the respondents read about a particular health care circumstance and then were asked to express their preference for 2 courses of testing or treatment. The scale used in the questions allowed them to indicate a strong preference for either of the options, a weak preference for either, or a neutral stance between the two. The 2 treatment scenarios were described as follows:
A new way of screening has just been developed for a particular type of cancer. Your family has no history of this type of cancer. The doctors of some of your friends have recommended getting screened every year, but your doctor suggests being screened once every 3 years, since each screening exposes you to radiation that might be bad for your health. Would you choose to be screened once a year or once every 3 years?
You had some sort of flu about 10 days ago, but the coughing has persisted and you're worried about getting pneumonia. Your friends have gotten antibiotics from their doctor when their cough won't go away. But your doctor says that you should wait for another week or two to see if you recover on your own (but call if you feel worse in the meantime). The reasons: antibiotics don't help with a virus and getting too many antibiotics may cause later infections that are resistant to treatment. Would you wait or ask for antibiotics now?
In the 2 clinician‐choice scenarios, the respondents read about different approaches to particular health concerns, the first embodying a more conservative practice style, the second a more aggressive one. In this case, the respondents were asked how much their ideal clinician would differ in these practices compared with the average clinician. The 2 scenarios were described as follows:
Some doctors think that frequent screening for health problems is an important way to catch medical problems before they become too serious, leading to better treatment, that is often cheaper. Other doctors think that frequent screening identifies things in people's bodies that are not normal, but which do not actually lead to health problems, wasting medical resources and producing harmful side‐effects when people are treated for abnormalities that never would have made them sick. If you were choosing a new primary care doctor, would you prefer a doctor who screens patients more frequently than most doctors, one who screens less frequently, or one who is about average?
When their patients have symptoms of the flu that just won't go away (coughing, congestion, low fever) some doctors prefer to treat immediately with antibiotics just in case it might head off bacterial pneumonia. Other doctors prefer to wait and see if the symptoms go away, because antibiotics don't work for viral infections and increase the risk of antibiotic resistant infections in the future. On average, doctors ask patients to wait 4 days before prescribing an antibiotic. If you were choosing a new primary care doctor, would you favor the doctor who asks patients to wait more days than average before getting antibiotics, fewer days than average, or about average?
Statistical Methods
At the heart of the survey experiment is the randomized assignment of respondents to different media primes (news stories). Findings across experimental arms can be compared without statistically controlling for other respondent characteristics. However, we also examine here the impact of particular messages that individual respondents identified from the stories. Unlike exposure, which was randomized, message recognition may be shaped by a variety of respondent characteristics, which then need to be controlled for in multivariate regression models in order to parse out the impact of message recognition (separate from the impact of attributes that make message recognition more likely) on attitudes and behaviors.
In our final analyses, we examined 2 types of interactions. In the first, we stratified the sample based on prior beliefs (assessed from the pre‐experiment survey) about the value of avoiding low‐value care. In the second, we stratified by racial and ethnic subgroups to test for the impact of alternative messaging strategies on disparities in the avoidance of low‐value clinical practices or clinicians who have more aggressive treatment styles.
Primary Findings From the Survey Experiment
Current Consumer Engagement
As of spring 2015, relatively few Americans had been exposed to low‐value care metrics or were asking Choosing Wisely's questions during routine interactions with clinicians. Even fewer Americans had regularly engaged in the sort of choices that Choosing Wisely aspires to promote. Although one‐third of the respondents had seen comparative performance data on physicians in the past 12 months, only 4.3% had seen information about low‐value care. Fewer than a third (31%) reported that when prescribed a diagnostic test, they regularly “ask[ed] how it might help me and my doctor make better choices later on.”
Our baseline for consumer preferences regarding treatment and the selection of clinicians came from respondents randomized into the experiment's control group. When confronted with the preceding scenarios, even without exposure to the Choosing Wisely coverage, a majority favored more conservative practices, even after being informed that some clinicians saw benefits in testing or treating more aggressively (Figure 2). But few translated these treatment preferences into their choice of clinicians, even after selecting a physician on a website that contained low‐value care metrics. Only about 10% of the respondents in the control group were willing to choose a clinician whose testing or treatment rates were well below average, and less than a third were willing to pick a doctor who was below average at all.
Figure 2.
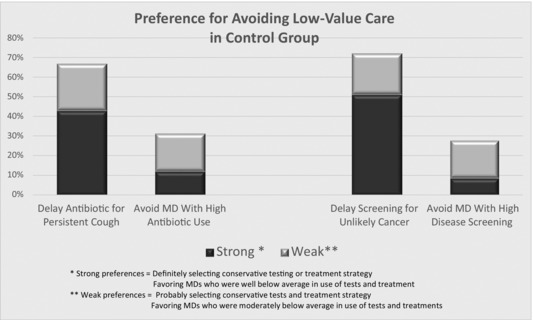
The Public's Preferences for Avoiding Low‐Value Care, Spring 2015
Interpreting Media Messages
The potential for Choosing Wisely or comparable initiatives to reinforce public preferences for avoiding low‐value care depends crucially on what messages the public extracts from the media coverage to which it is exposed. We focused our analyses first on the extent to which Choosing Wisely's 4 core messages were recognized by readers and second on some additional connotations that might have been inadvertently conveyed through the framing of this issue in media coverage.
The assessment by those respondents exposed to actual media coverage is presented in the top row of Table 5. When asked to summarize this article for family or friends, 62% identified waste as a key theme, but only 16% reported low‐value care to be potentially harmful, even though the story used for priming explicitly and repeatedly indicates that excessive tests and treatment put patients “at risk.” The 2 other themes were only partly received: roughly a quarter of all respondents got the message that patients ought to be actively questioning their providers about tests and treatment, but fewer than 10% noted that clinicians had been galvanized to take action on this issue.
Table 5.
Perception of Core Messages and Prevalence of Impressions in Media Framing
| Recognition of Core Messages | Additional Impressions | |||||
|---|---|---|---|---|---|---|
| Media Frames | Wasteful Care Is a Concern (%) | Harmful Care Is a Concern (%) | Clinicians Activated to Respond (%) | Patients Should Question Doctors (%) | Low‐Value Care Limited to Testing (%) | Providers Are to Blame (%) |
| Conventional coverage | ||||||
| Full sample | 61.8 | 15.5 | 9.2 | 27.0 | 70.3 | 20.4 |
| Heightened‐threat story | ||||||
| Full sample | 50.0b | 44.8b | 9.1 | 16.2b | 64.3 | 12.3a |
| Staged‐care story | ||||||
| Full sample | 57.2 | 9.2a | 8.6 | 11.8b | 76.3 | 17.1 |
Difference from conventional coverage statistically significant at P < 0.10.
Difference from conventional coverage statistically significant at P < 0.05.
Each of our 2 alternative media frames induced changes in message receptivity. The heightened‐threat story (Table 5, middle row) substantially increased the perception that low‐value care could harm health, tripling the perception of harm compared with the conventional coverage. But this outcome was associated with less awareness of the other core messages; in this framing the respondents were less likely to identify wastefulness or questioning of clinicians as key elements of the story. The staged‐treatment story (Table 5, bottom row) induced fewer changes from conventional coverage, but it significantly lowered the perception that patients ought to question their doctors.
Past research has demonstrated that media framing can also shape perceptions in unintended ways, altering how the public understands the nature of the problem in question or whom they blame for its emergence.43, 44, 45 Choosing Wisely's emphasis on patients’ questioning of clinicians’ recommendations may create 2 such unintended “side effects”: first, decreasing patients’ trust in their clinicians’ judgment and, second, focusing the public's attention on testing rather than treatment, since patients are typically in a better position to raise questions about testing.
The conventional coverage of Choosing Wisely does both (Table 5, top rows, right‐hand columns). Almost 20% of those who read the conventional coverage attributed some blame to providers for low‐value care. Seventy percent of those who read the conventional news coverage attributed low‐value care entirely to testing (recall that in the pre‐survey [Figure 1], roughly 60% of those who understood low‐value care identified it exclusively with testing).
The staged‐testing frame had only modest impact on these media‐induced side effects. The heightened‐threat frame, however, had more influence on these unintended implications. It significantly reduced the blame on providers, cutting it in half compared with the conventional coverage. It also lowered the extent to which the readers assumed that low‐value care was limited to testing, perhaps because they most often associated iatrogenic harms with treatment.
Impact of Exposure to Specific Media Frames
We assessed the impact of media messaging on 2 sets of clinician‐choice outcomes: the respondents’ use of metrics for low‐value care to assess clinicians and the respondents’ choices of clinicians, weighing low‐value metrics against other aspects of clinician performance. In each case, we had measures of how choices were actually made on the SelectMD website, as well as how the respondents expected to make real‐life choices of clinicians in the future. To assess the impact of media framing, we compared the choices and expectations of the respondents who were randomly assigned to the control arm with those exposed to the 3 different media stories just described.
Exposure to conventional coverage of Choosing Wisely increased consumers’ use and valuation of low‐value care metrics compared with those of the control group (Table 6, top 2 rows). But this impact was uneven, with no clear boost to preferring clinicians who were selective about testing and treatment. Nor was there any evident impact on the choice of clinician. By contrast, both the staged‐care (Table 6, fourth row) and the heightened‐threat (third row) frames were associated with changes in the use of low‐value metrics and choice of clinicians, although the impact of staged care for choice of clinician was not statistically significant.
Table 6.
Association of Message Exposure With Perceptions and Behavior
| Using Metrics for Low‐Value Care | Choosing a Clinician | ||||
|---|---|---|---|---|---|
| Among Top Three Criteria for Choosing a Clinician on SelectMD | |||||
| Media Frames | Selective Care (%) | Watchful Waiting (%) | Would Seek Out Low‐Value Metrics for Future Choice of Clinician (%) | Choose Clinician on SelectMD Top Rated for Avoiding Low‐Value Care (%) | Prefer a Clinician Who Avoids Low‐Value Care in Scenarios (%) |
| Control group | |||||
| Full sample | 32.0 | 17.1 | 46.2 | 18.3 | 35.1 |
| Conventional coverage | |||||
| Full sample | 32.6 | 27.6b | 51.5a | 17.1 | 39.0 |
| Heightened‐threat story | |||||
| Full sample | 37.0 | 17.5 | 58.2b | 18.8 | 45.8b |
| Staged‐care story | |||||
| Full sample | 37.5 | 23.7a | 51.0 | 24.3 | 41.1 |
Difference from control group statistically significant at P < 0.10.
Difference from control group statistically significant at P < 0.05.
Impact of Specific Media Messages
To better understand how alternative frames shape patients’ expectations and consumers’ behavior, we examined which specific messages that readers drew from the media coverage had the strongest associations with different attitudes, preferences, or actions. As we noted earlier, although the exposure to the media stories was randomized, the respondents’ recognition of those messages in the media coverage was not because it is shaped by respondents’ prior health care experiences, educational attainment, and prior understanding of low‐value care. So we need to control statistically for these potentially confounding individual attributes.
To match the results shown in Table 6, we presented the findings on message recognition also in terms of average prevalence. Even though we present here simple comparisons of frequencies, all the patterns evident in Table 7 persisted in multivariate models that controlled statistically for these other potential influences (see Appendix E, online). We focus here on the 3 core Choosing Wisely messages most commonly perceived by the public: the threat of waste, the threat of harm, and the need for consumers to question clinicians’ recommendations (see Table 7). We compared those respondents who identified these messages in the media coverage to which they were exposed with those in the control group (who were not exposed to these messages) for the same outcomes that we previously compared across the experimental arms.
Table 7.
Association of Message Recognition With Perceptions and Behavior
| Using Metrics for Low‐Value Care | Choosing a Clinician | ||||
|---|---|---|---|---|---|
| Among Top Three Criteria for Choosing a Clinician on SelectMD | |||||
| Core Messages | Selective Care (%) | Watchful Waiting (%) | Would Seek Out Low‐Value Metrics for Future Choice of Clinician (%) | Choose Clinician on SelectMD Top Rated for Avoiding Low‐Value Care (%) | Prefer a Clinician Who Avoids Low‐Value Care in Scenarios (%) |
| Control group | |||||
| Full sample | 32.0 | 17.1 | 45.2 | 18.3 | 35.1 |
| Message: harmful exists | |||||
| Full sample | 43.1b | 22.3 | 58.5b | 20.7 | 53.1b |
| Message: wasteful exists | |||||
| Full sample | 35.2 | 25.0a | 54.6b | 21.6 | 42.9a |
| Message: question clinicians | |||||
| Full sample | 40.4b | 19.2 | 57.9b | 15.5 | 43.2b |
Difference from control group statistically significant at P < 0.10.
Difference from control group statistically significant at P < 0.05.
Perceiving any of the 3 messages in the assigned news story (the risk of waste, the threat of harm, the need to question clinical recommendations) was associated with more greatly valuing metrics of low‐value care and more frequently selecting clinicians who avoided such care. But with the exception of valuing watchful waiting, both the threat of harm and the need to question clinicians were associated with far larger shifts in preferences and behavior than was the wastefulness theme. This difference was most pronounced for the threat of harm. For the full sample, averaging across all 5 outcome measures, the harm message was associated with a 50% larger change than was the waste message.
Choices Regarding Specific Tests and Treatment
Our specific choice scenarios involving the use of antibiotics and disease screening suggests that the impact of particular messages depends in part on the type of medical care in question (Figure 3). For antibiotics, having identified the threat of harm or waste in itself had relatively little impact on the respondents’ preferences regarding antibiotics or selection of clinicians who avoided this specific form of low‐value care (Figure 3, left‐side clusters of bars). But when people identified both messages in the media coverage, they were far more likely to favor the delayed application of antibiotics and to seek clinicians who avoided above‐average use. Indeed, our regression analyses suggest that when controlling for sociodemographic characteristics, health status, and prior knowledge of low‐value care, those who perceived the dual message of waste and harm in media coverage were 50% more likely to avoid using antibiotics in their own care and twice as likely to select a clinician with a consistently low use of antibiotics in their practice (see Appendix F, online).
Figure 3.
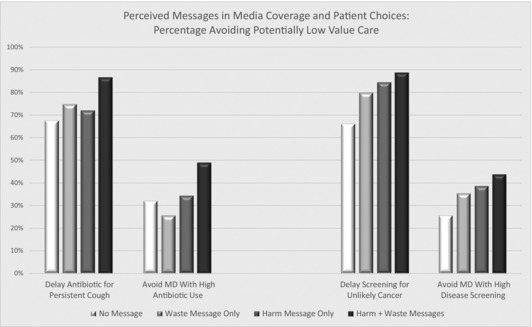
Perceived Messages in Media Coverage and Patient Choices: Percentage Avoiding Potentially Low‐Value Care
By contrast, it appears that for disease screening, concerns about both harm and waste had an additive impact on consumers’ behavior. Here, too, these messages were most strongly associated with avoiding low‐value care when combined in ways that allowed readers to identify both. The combined effects were quite large. Our regression models suggest that those who perceived both messages in the media coverage were more than twice as likely to delay their own screening and to avoid clinicians who screened frequently, compared with otherwise similar respondents who identified neither of these messages in media coverage.
Impact of Framing and Messaging on Disparities
As we observed in Table 3, before any experimental priming, respondents from minority households and those who had less education were significantly less likely to report understanding the concept of low‐value care. Our starting point for assessing the impact of messaging on disparities was therefore to compare the effect of exposure to and recognition of messages based on the extent of prior knowledge regarding low‐value care.
We began by examining what respondents with different levels of prior knowledge drew from the 3 different frames for media coverage of Choosing Wisely (compare Table 8 with Table 5). In some ways, both those with some and those with no prior knowledge read the alternatively framed stories similarly. For example, both groups drew from the heightened‐threat story greater potential harm from excess testing and treatment, and both groups were less likely to see the need for patients to question their providers in this framing.
Table 8.
Perceived Messages and Impressions by Level of Prior Understanding of Low‐Value Care
| Recognition of Core Messages | Additional Impressions | |||||
|---|---|---|---|---|---|---|
| Media Frames (by Level of Prior Understanding) | Wasteful Care Is a Concern (%) | Harmful Care Is a Concern (%) | Clinicians Activated to Respond (%) | Patients Should Question Doctors (%) | Low‐Value Care Limited to Testing (%) | Providers Are to Blame (%) |
| Conventional coverage | ||||||
| Able to describe low‐value care | 70.3 | 19.5 | 11.2 | 29.3 | 66.0 | 18.5 |
| Unable to describe low‐value care | 44.4 | 7.1 | 5.1 | 22.2 | 85.4 | 24.2 |
| Heightened‐threat story | ||||||
| Able to describe low‐value care | 51.9a | 50.0a | 12.5 | 18.3a | 71.0 | 12.5 |
| Unable to describe low‐value care | 46.0 | 34.0a | 2.0 | 12.0a | 48.3a | 12.0a |
| Staged‐care story | ||||||
| Able to describe low‐value care | 63.2 | 12.2 | 12.2 | 13.3a | 79.0a | 16.3 |
| Unable to describe low‐value care | 46.3 | 3.7 | 1.9 | 9.3a | 69.6a | 18.5 |
Difference with conventional coverage statistically significant at P < 0.05.
However, as one might expect, respondents previously familiar with low‐value care were better able than those with no prior knowledge to identify many of the Choosing Wisely core themes in the coverage; this was true for every framing used. The most striking differences emerged in the unplanned connotations: the alternative frames were far less likely to lead previously low‐knowledge respondents to attribute low‐value care exclusively to testing or to blame providers for this care.
We found more striking differences when we compared the impact of message exposure or recognition across these 2 strata of respondents (Table 9). When comparing the attitudes and behaviors of those with no prior understanding of low‐value care across our experimental arms (Table 9, rows 2, 4, and 6), we observed that those with no prior understanding appeared more responsive than did the other respondents to alternative framings. The heightened‐threat coverage induced them to seek low‐value care metrics and to choose a clinician on the SelectMD site who rated well in avoiding low‐value care, but to be less likely to choose a clinician based on their attention to watchful waiting than was true for conventional coverage.
Table 9.
Association of Message Exposure
| Using Metrics for Low‐Value Care | Choosing a Clinician | ||||
|---|---|---|---|---|---|
| Among Top 3 Criteria for Choosing a Clinician on SelectMD | |||||
| Media Frames (by Level of Prior Understanding) | Selective Care (%) | Watchful Waiting (%) | Would Seek Out Low‐Value Metrics in Future Choice of Clinician (%) | Choose a Clinician on SelectMD Top Rated for Avoiding Low‐Value Care (%) | Prefer a Clinician Who Avoids Low‐Value Care in Scenarios (%) |
| Control group | |||||
| Able to describe LVC | 37.4 | 19.6 | 46.2 | 20.6 | 39.6 |
| Unable to describe LVC | 23.5 | 13.2 | 46.3 | 14.7 | 27.9 |
| Message exposure | |||||
| Conventional coverage | |||||
| Able to describe LVC | 34.6 | 30.7b | 54.9a | 19.5 | 44.8 |
| Unable to describe LVC | 28.3 | 21.2b | 44.4 | 12.4 | 26.8 |
| Heightened‐threat story | |||||
| Able to describe LVC | 40.4 | 19.2 | 55.3a | 13.5 | 54.8b |
| Unable to describe LVC | 30.0a | 14.0 | 64.0b | 30.0b | 26.5 |
Abbreviation: LVC, low‐value care
Difference from control group statistically significant at P < 0.10.
Difference from control group statistically significant at P < 0.05.
Differences in message recognition were even more pronounced (Table 10). For those with no prior knowledge of low‐value care, recognizing the harm message was associated with far larger shifts in attitudes and behavior than for those identifying the waste message in media coverage, for 4 of our 5 outcome measures. Only for the fifth outcome measure (selecting doctors in the choice scenarios) was the impact of message more pronounced among those who had prior knowledge of low‐value care.
Table 10.
Association of Message Recognition with Perceptions and Behavior, by Prior Understanding of Low‐Value Care
| Using Metrics for Low‐Value Care | Choosing a Clinician | ||||
|---|---|---|---|---|---|
| Among Top 3 Criteria for Choosing a Clinician on SelectMD | |||||
| Media Frames (by Level of Prior Understanding) | Selective Care (%) | Watchful Waiting (%) | Would Seek Out Low‐Value Metrics in Future Choice of Clinician (%) | Choose a Clinician on SelectMD Top Rated for Avoiding Low‐Value Care (%) | Prefer a Clinician Who Avoids Low‐Value Care in Scenarios (%) |
| Message recognition | |||||
| Low‐Value care causes harm | |||||
| Able to describe LVC | 42.3 | 20.2 | 53.9a | 19.2 | 59.2b |
| Unable to describe LVC | 46.2b | 30.8b | 76.9b | 26.9b | 28.0 |
| Low‐value care causes waste | |||||
| Able to describe LVC | 36.9 | 27.3a | 53.5a | 22.7 | 47.3a |
| Unable to describe LVC | 30.4a | 18.5 | 57.6a | 18.5 | 30.4 |
Abbreviation: LVC, low‐value care
Difference from control group statistically significant at P < 0.10.
Difference from control group statistically significant at P < 0.05.
These patterns suggest that framing and message recognition could substantially affect disparities in response to low‐value care. This is evident in Figure 4 for our concrete‐choice scenarios (we omitted the outcomes for selecting a clinician based on their prior use of antibiotics because there were no statistically significant disparities in the control group).
Figure 4.
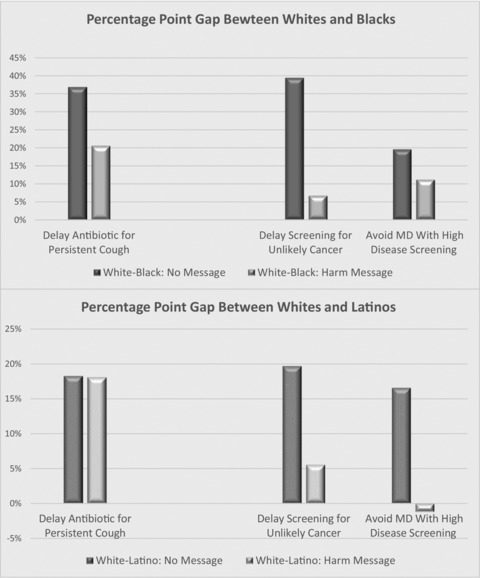
Disparities With and Without Perception of Harm From Low‐Value Care: Percentage Point Gap in Avoiding Low‐Value Tests and Treatment
For example, of those who recognized no messages in the media coverage regarding waste or harm, whites were 36.9% more likely than blacks and 18.6% more likely than Latinos to favor the delayed use of antibiotics for a persistent cough. The racial/ethnic gaps were even larger for screening for low‐probability cancer risks.
Associating low‐value care with harm appears to be a particularly effective strategy for reducing ethnic and racial disparities, even after controlling for other sociodemographic and health status influences in multivariate regression models. For example, the disparity between white and black respondents in accepting a delayed use of antibiotics declined from 36.9% to 20.3% when the respondents recognized the threat of harm, and the disparity in accepting longer periods between cancer screenings fell from 39.8% to 5.6%. A similar decline was evident for differences between Latinos and whites related to cancer screening, but not for antibiotic use.
By contrast, the largest reductions in disparities related to education were for those respondents who perceived the wastefulness theme in media coverage (results not shown). Since respondents with higher education were more responsive to harm messages, these tended to expand disparities related to education. Additional research with larger samples of respondents will be needed to verify these preliminary findings, as well as to understand why certain messages appear to have larger effects than others on particular disparities.
Discussion and Conclusion
This study offers fresh insight into how Americans think about “value” in health care—and how their conceptions might be enriched. Our findings belie the often‐stated presumption that every American demands every test and treatment available, as quickly as possible.46, 47 Notably, two‐thirds of the public favored the more conservative option in our treatment scenarios. Roughly half the respondents gave priority to selective treatment and watchful waiting when choosing a clinician, and 35% to 40% favored clinicians in real life who were below average in ordering frequently overused tests and treatment. To be sure, a portion of the public—our findings suggest about 1 in 5—continues to seek aggressive treatment and practitioners; their demands may be particularly memorable for practitioners.13 Yet there is now a substantial reservoir of public support for more mindful approaches to testing and treatment.
Public campaigns, such as Choosing Wisely, can plausibly claim some of the credit. Exposure to media coverage typical for this campaign did encourage more consumers to avoid low‐value care, most markedly in the form of watchful waiting (see Table 5). But this change was modest in magnitude (5% to 10% of the public) and had little impact on consumer choice, particularly among less‐informed segments of the public. This was largely because 3 of the 4 core Choosing Wisely messages were recognized by only, at most, a quarter of those exposed to this conventional media coverage (see Table 4).
Table 4.
Predictors of Understanding of and Perceived Benefits From Avoiding Low‐Value Care (Logistic Regression Models)
| Anticipates Benefits From Avoiding | |||||
|---|---|---|---|---|---|
| Can't Envision What | Low‐Value Care for Improved | ||||
| Low‐Value Care Means | Relationship With Doctors | ||||
| Respondent Characteristic | Comparison | Odds Ratio | P value | Odds Ratio | P value |
| Black | White | 1.60 | 0.07 | 0.64 | 0.09 |
| Latino | White | 1.63 | 0.07 | 1.14 | NS |
| Other | White | 1.08 | NS | 1.19 | NS |
| High school grad | Some high school | 0.96 | NS | 1.28 | NS |
| Some college | Some high school | 0.52 | 0.03 | 1.65 | NS |
| College grad | Some high school | 0.33 | 0.01 | 2.07 | 0.02 |
Abbreviation: NS = not statistically significant at a P < 0.10 confidence level.
Regression model also controls for gender, age, income, and health status (whether respondent has chronic health condition requiring medical monitoring or has had a serious acute health problem in past year).
Moreover, Choosing Wisely's conventional coverage did not always work as its proponents hoped. By focusing attention on wasted resources, it failed to connect with much of the public. Waste suggests that the problem with low‐value care is primarily the sociotropic burden caused by aggregate medical spending,5, 8 a message with limited appeal because most Americans view health in more individualist terms.27, 29, 32 Few people are motivated to save aggregate resources, which, they assume, will primarily increase profits for insurers and providers.32
Even more problematic, the conventional media coverage of Choosing Wisely placed a surprising amount of blame on health care providers, despite the campaign's efforts to maintain “the centrality of the physician‐patient relationship to help patients make the right decisions.”8 In part, this reflects the failure of conventional coverage to convey to its audience that clinicians are taking on the task of addressing low‐value care. But it is also an unexpected side effect of messaging that emphasizes waste, often in the language of “waste, fraud and abuse.” Respondents who associated low‐value care with waste were 3 times as likely to blame providers as were those who associated low‐value care with health risks. Why this is the case remains unclear, but perhaps the public associates notions of waste with profiteering by health care providers.48, 49
Our findings suggest that public education campaigns can do better. By reframing the ways in which low‐value care is understood by the public, these initiatives can motivate broader consumer activism and likely diminish ethnic and racial disparities in recognition of this issue. The combined threats of waste and health risk elicited the greatest consumer response.
Our qualitative findings (see Table 2) suggest that the popular appeal of efforts to curb low‐value care could be substantially enhanced if they explicitly emphasized the potent promise of linking more person‐centered, relationally engaged care to the avoidance of low‐value tests and treatments—for example, by replacing excessive tests with time for clinicians to talk, listen, and personalize. Our findings document this quite powerfully.
Patients who in interviews and focus groups positively described their interactions with clinicians regarding conservative treatment and watchful waiting did so almost entirely in the context of a trusted relationship with their physician. The vast majority of Americans who currently view reducing low‐value care in a positive light do so because they see it as a means to improve communication with their clinicians (see Figure 1). The framing effects of the story emphasizing staged testing and treatment further reinforced this finding. Respondents who were not already knowledgeable about low‐value care and were exposed to this frame indicated significantly more support for selective testing and treatment by clinicians than did either the control group or those exposed to conventional media coverage of Choosing Wisely (see Table 4).
Our findings must be considered in light of some methodological limitations. Although the GfK panel includes a representative proportion of respondents with limited education, we could not determine how well the Choosing Wisely message resonated with those who are illiterate or who are not fluent in English, since they were not a part of the panel. In addition, our categorization of the current perceptions of benefits that respondents associated with reductions in low‐value care should be seen as an approximation. Although virtually all the perceived benefits clearly involved some aspect of clinician‐patient relationships, the subcategories are somewhat overlapping, making the distinctions between enhanced communication and more personalized clinical practices (including shared decision making) a little fuzzy.
Because of resource constraints, our survey experiment could test only a handful of alternative framing strategies that might be deployed to enrich the public's understanding of low‐value care or to encourage them to act on this knowledge. Additional approaches might concentrate more explicitly on treatment than on testing. Or they might more directly play up the enhanced potential for humane interactions with patients if clinicians spent less time looking at test results on their computer screens.
Finally, although the story used to prime the conventional Choosing Wisely arm in the experiment was representative of the campaign's media coverage, another story worded somewhat differently might have changed the effect on the readers. Furthermore, a one‐time exposure to any message cannot replicate the longer‐term learning potential of an extended public education campaign. Choosing Wisely also aspires to alter the ways in which physicians and patients share in decisions regarding testing and treatment;5 this experiment did not directly test consumers’ openness to those sorts of interactions.
If efforts to further inform the public about low‐value care are to have the greatest and most equitable impact, the core messages (and resultant media coverage) must be adapted to resonate as strongly as possible with the public's values, perceptions, and preferences about medical care. Our findings suggest that what is needed is a message campaign that has the capacity to reach, and mobilize, the majority of Americans who currently see no advantage in reducing low‐value care, particularly the third of the population that has little current understanding of what that concept even means or why it matters. Most crucially, our study highlighted the fact that Americans want relationships with clinicians that are more relational than mechanical and that are deeply humane, personalized, and interactive.50 Partnerships between patients and clinicians to “choose wisely” with respect to tests and treatments seem most likely to thrive when associated with these key values.
Supporting information
Appendix A. Original Wording of Representative Media Coverage of Choosing Wisely
Appendix B. Wording of Media Story for Control Group
Appendix C. Wording of Revised Media Story: Alternative Frame Emphasizing Health Threats
Appendix D. Wording of Revised Media Story: Alternative Frame Emphasizing Staged Testing/Treatment
Appendix E. Association of Perceived Messages With Changes in Attitudes and Behaviors, Results From Logistic Regression Models: Full Sample
Appendix F. Association of Perceived Messages With Changes in Attitudes and Behaviors, Interactions of Messages on Harm and Waste
Funding/Support
The research on which this paper is based was supported by a grant from the Robert Wood Johnson Foundation, funded under its Pioneer program.
Conflict of Interest Disclosures: Both authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Both authors report a grant (1R21HS021858) and a Cooperative Agreement (1U18HS016978) from the Agency for Healthcare Research and Quality outside the submitted work.
Acknowledgments: The project benefited from the assistance and insights of Lacey Rose Barre, serving as project coordinator, and the work of Chaz Felix and Lane Hanson, coding qualitative survey responses. The original design of the study was enhanced by input from Professors Meg Gaines and Sarah Davis from the Center for Patient Partnerships at the University of Wisconsin– Madison. The focus groups were greatly facilitated by assistance from the Center for Patient Partnerships, the CARDS program at the University of Wisconsin, the Cancer Support Community, and the Connecticut Choosing Wisely Collaborative. We also acknowledge the helpful feedback received when elements of this research were presented in seminars at Rutgers University, the Connecticut Choosing Wisely Collaborative, a seminar for health advocates organized by Consumer Reports in Washington DC, and a webinar that Consumer Reports hosted as part of its technical assistance for state‐level Choosing Wisely initiatives.
References
- 1. Institute of Medicine . Roundtable on evidence‐based medicine. In: Yong PL, Saunders RS, Olsen LA, eds. The Healthcare Imperative: Lowering Costs and Improving Outcomes: Workshop Series Summary. Washington, DC: National Academies Press; 2010. [PubMed] [Google Scholar]
- 2. Schuster MA, McGlynn EA, Brook RH. How good is the quality of health care in the United States? Milbank Q. 1998;76(4):517‐563, 509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Gerber A, Patashnik E, Doherty D, Dowling C. The public wants information, not broad mandates, from comparative effectiveness research. Health Aff. 2011;29(10):1872‐1881. [DOI] [PubMed] [Google Scholar]
- 4. Cassel C, Guest J. Choosing wisely: helping physicians and patients make smart decisions about their care. JAMA. 2012;307(17):1801‐1802. [DOI] [PubMed] [Google Scholar]
- 5. Wolfson D, Santa J, Slass L. Engaging physicians and consumers in conversations about treatment overuse and waste: a short history of the Choosing Wisely campaign. Acad Med. 2014; 89(7):990‐995. [DOI] [PubMed] [Google Scholar]
- 6. Kahneman D. Thinking, Fast and Slow. New York, NY: Farrar, Straus and Giroux; 2011. [Google Scholar]
- 7. Blumenthal‐Barby JS. “Choosing Wisely” to reduce low‐value care: a conceptual and ethical analysis. J Med Philos. 2013;38:559‐580. [DOI] [PubMed] [Google Scholar]
- 8. Levinson W, Kallewaard M, Bhatia RS, Wolfson D, Shortt S, Kerr EA. Choosing Wisely: a growing international campaign. BMJ Qual Safety. December 31, 2014. doi:10.1136/bmjqs-2014-003821. [DOI] [PubMed] [Google Scholar]
- 9. Kost A, Genao I, Lee JW, Smith SR. Clinical decisions made in primary care clinics before and after Choosing Wisely. J Am Board Fam Med. 2015;28(4):471‐474. [DOI] [PubMed] [Google Scholar]
- 10. Rosenberg A, Agiro A, Gottlieb M, et al. Early trends among seven recommendations from the Choosing Wisely campaign. JAMA Intern Med. 2015;175(12):1913‐1920. [DOI] [PubMed] [Google Scholar]
- 11. Schwartz AL, Chernew ME, Landon BE, McWilliams JM. Changes in low‐value services in year 1 of the Medicare Pioneer Accountable Care Organization program. JAMA Intern Med. 2015;175(11):1815‐1825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Balas EA; Elkin PL. Technology transfer from biomedical research to clinical practice: measuring innovation performance. Eval & Health Professions. 2013;36(4):505‐517. [DOI] [PubMed] [Google Scholar]
- 13. Fenton JJ, Franks P, Feldman MD, et al. Impact of patient requests on provider‐perceived visit difficulty in primary care. J Gen Intern Med. 2015;30(2):214‐220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Mason DL. Choosing Wisely: changing clinicians, patients, or policies? JAMA. 2015;313(7):657‐658. [DOI] [PubMed] [Google Scholar]
- 15. Quincy L. A Call to Action: Addressing Research Gaps to Provide Better Healthcare Value for Consumers. Research Brief No. 13. Washington, DC: Consumers Union; June 2016. [Google Scholar]
- 16. Druckman JN, Hennessy CL, St. Charles K, Webber J. Competing rhetoric over time: frames versus cues. J Polit. 2010;72(1):136‐148. [Google Scholar]
- 17. Gollust SE, Lantz PM, Ubel PA. The polarizing effect of news media messages about the social determinants of health. Am J Public Health. 2009;99(12):2160‐2167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Barry C, Brescoll V, Gollust S. Framing childhood obesity: how individualizing the problem affects public support for prevention. Poll Psych. 2013;34(3):327‐349. [Google Scholar]
- 19. Corson AH, Fan VS, White T, et al. A multifaceted hospitalist quality improvement intervention: decreased frequency of common labs. J Hosp Med (online). 2015;10(6):390‐395. [DOI] [PubMed] [Google Scholar]
- 20. Wen L, Kosowsky J. When Doctors Don't Listen: How to Avoid Misdiagnoses and Unnecessary Tests. New York, NY: St. Martin's Press / Thomas Dunne Books, 2013. [Google Scholar]
- 21. Wennberg JE, O'Connor AM, Collins ED, Weinstein JN. Extending the P4P agenda, part 1: how Medicare can improve patient decision making and reduce unnecessary care. Health Aff. 2007;26(6):1564‐1574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Bodenheimer T, Fernandez A. High and rising health care costs, part 4: can costs be controlled while preserving quality? Ann Intern Med. 2005;143(1):26‐31. [DOI] [PubMed] [Google Scholar]
- 23. Kanzaria HK, Brook RH, Probst MA, Harris D, Berry SH, Hoffman JR. Emergency physician perceptions of shared decision‐making. Acad Emerg Med. 2015;22(4):399‐405. [DOI] [PubMed] [Google Scholar]
- 24. Consumer Reports Health . Five questions to ask your doctor. 2015. http://consumerhealthchoices.org/catalog/choosing-wisely-questions-poster-small/. Accessed November 7, 2015.
- 25. ABIM Foundation . Promoting healthy choices. Choosing Wisely Monthly Newsletter. March 2016. http://www.choosingwisely.org/resources/updates-from-the-field/. Accessed July 20, 2016. [Google Scholar]
- 26. Avril T. Medical group takes up the fight against unnecessary tests. Philadelphia Inquirer. April 4, 2012:A01. [Google Scholar]
- 27. Consumers Union . Consumer attitudes toward health care costs, value and system reforms: a review of the literature. Yonkers, NY: Consumers Union; 2014. [Google Scholar]
- 28. Wasson JH. A patient‐reported spectrum of adverse health care experiences: harms, unnecessary care, medication illness, and low health confidence. J Ambient Care Manage. 2013;36(3):245‐250. [DOI] [PubMed] [Google Scholar]
- 29. Danis M, Sommers R, Logan J, et al. Exploring public attitudes towards approaches to discussing costs in the clinical encounter. J Gen Intern Med. 2013;29(1):223‐229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Meluch AL, Oglesby WH. Physician‐patient communication regarding patients’ healthcare costs in the US: a systematic review of the literature. J Comm Healthcare. 2015;8(2):151‐160. [Google Scholar]
- 31. Kőszegi B. Health, anxiety and patient behavior. J Health Econ. 2003;22(6):1073‐1084. [DOI] [PubMed] [Google Scholar]
- 32. Goold S, Klipp G. Managed care members talk about trust. Soc Sci Med. 2002;54(6):879‐888. [DOI] [PubMed] [Google Scholar]
- 33. Sommers R, Goold S, McGlynn E, Pearson S, Danis M. Focus groups highlight that many patients object to clinicians’ focusing on costs. Health Aff. 2013;32(2):338‐346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Tompson J, Benz J, Willcoxon N, et al. Finding quality doctors: how Americans evaluate provider quality in the United States. The Associated Press‐NORC Center for Public Affairs Research. http://www.apnorc .org/projects/Pages/finding-quality-doctors-how-americans-evaluate-provider-quality-in-the-united-states.aspx. July 2014. Accessed November 9, 2015.
- 35. Grob, R , Schlesinger M, Shaller D, et al. Breaking narrative ground: innovative methods for rigorously eliciting and assessing patient narratives. Health Serv Res. 2016;51(3):1248‐1272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Chang L, Krosnick JA. National surveys via RDD telephone interviewing versus the internet: comparing sample representativeness and response quality. Public Opinion Q. 2009;73:641‐678. [Google Scholar]
- 37. Consumer Reports . When to Say “Whoa!” to Doctors . June 2012. http://www.consumerreports.org/cro/magazine/2012/06/many-common-medical-tests-and-treatments-are-unnecessary/index.htm. Accessed July 24, 2016.
- 38. Mechanic D. Policy challenges in addressing racial disparities and improving population health. Health Aff. 2005;24(2):335‐338. [DOI] [PubMed] [Google Scholar]
- 39. Green JE, Brown AG, Ohri‐Vachaspati P. Sociodemographic disparities among fast‐food restaurant customers who notice and use calorie menu labels. J Acad Nutr Diet. 2015;115(7):1093‐1101. [DOI] [PubMed] [Google Scholar]
- 40. Brodie M, Hamel E, Altman D, Blendon R, Benson J. Health news and the American public, 1996‐2002. J Health Pol, Policy Law. 2003;28(5):927‐950. [DOI] [PubMed] [Google Scholar]
- 41. Schlesinger M, Kanouse DE, Martino SC, Shaller D, Rybowski L. Complexity, public reporting, and choice of doctors: a look inside the blackest box of consumer behavior. Med Care Res Rev. 2014;71:38S‐64S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Anhang Price R, Elliott MN, Zaslavsky AM, et al. Examining the role of patient experience surveys in measuring health care quality. Med Care Res Rev. 2014;71(5):522‐554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Saguy A, Almeling R. Fat in the fire? Science, the news media, and the “obesity epidemic.” Soc Forum. 2008;23(1):53‐83. [Google Scholar]
- 44. Shepherd MA, Gerend MA. The blame game: cervical cancer, knowledge of its link to human papillomavirus and stigma. Psych Health. 2013;29(1):94‐109. [DOI] [PubMed] [Google Scholar]
- 45. Kvaale EP, Haslam N, Gottdiener WH. The “side effects” of medicalization: a meta‐analytic review of how biogenetic explanations affect stigma. Clin Psych Rev. 2013;33(6):782‐794. [DOI] [PubMed] [Google Scholar]
- 46. Sorenson C, Gusmano M, Oliver A. The politics of comparative effectiveness research. J Health Pol, Policy Law. 2014;39(1):139‐169. [DOI] [PubMed] [Google Scholar]
- 47. Kim M, Blendon R, Benson J. How interested are Americans in new medical technologies? Health Aff. 2001;20(5):194‐201. [DOI] [PubMed] [Google Scholar]
- 48. Vayreda A, Antaki C. To vaccinate or not? The disqualification of commercial sources of health advice in an online forum. Comm Med. 2011;8(3):273‐282. [DOI] [PubMed] [Google Scholar]
- 49. Schoenthal AR, Getzen TE. Bariatric surgery and the financial reimbursement cycle. J Health Care Finance. 2005;31(3):1‐9. [PubMed] [Google Scholar]
- 50. Kelley M, James C, Alessi Kraft S, et al. Patient perspectives on the learning health system: the importance of trust and shared decision making. Am J Bioethics. 2015;15(9):4‐17. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix A. Original Wording of Representative Media Coverage of Choosing Wisely
Appendix B. Wording of Media Story for Control Group
Appendix C. Wording of Revised Media Story: Alternative Frame Emphasizing Health Threats
Appendix D. Wording of Revised Media Story: Alternative Frame Emphasizing Staged Testing/Treatment
Appendix E. Association of Perceived Messages With Changes in Attitudes and Behaviors, Results From Logistic Regression Models: Full Sample
Appendix F. Association of Perceived Messages With Changes in Attitudes and Behaviors, Interactions of Messages on Harm and Waste


