Policy Points:
Congress has expressed concern about electronic health record (EHR) vendors and health care providers knowingly interfering with the electronic exchange of patient health information. These “information blocking” practices would privately benefit vendors and providers but limit the societal quality and efficiency benefits from EHR adoption.
We found that information blocking is reported to frequently occur among EHR vendors as well as hospitals and health systems, and that it is perceived to be motivated by opportunities for revenue gain.
Because information blocking is largely legal today, the most effective policy response likely involves a combination of direct enforcement and the altering of market conditions that promote information blocking.
Context
Congress has raised concerns about providers and electronic health record (EHR) vendors knowingly engaging in business practices that interfere with electronic health information exchange (HIE). Such “information blocking” is presumed to occur because providers and vendors reap financial benefits, but these practices harm public good and substantially limit the value to be gained from EHR adoption. Crafting a policy response has been difficult because, beyond anecdotes, there is no data that captures the extent of information blocking.
Methods
We conducted a national survey of leaders of HIE efforts who work to enable HIE across provider organizations. We asked them about the frequency of information blocking, its specific forms, and the effectiveness of various policy strategies to address it. We received responses from 60 individuals (57% response rate). We calculated descriptive statistics across responses.
Findings
Half of respondents reported that EHR vendors routinely engage in information blocking, and 25% of respondents reported that hospitals and health systems routinely do so. Among EHR vendors, the most common form of information blocking was deploying products with limited interoperability. Among hospitals and health systems, the most common form was coercing providers to adopt particular EHR or HIE technology. Increasing transparency of EHR vendor business practices and product performance, stronger financial incentives for providers to share information, and making information blocking illegal were perceived as the most effective policy remedies.
Conclusions
Information blocking appears to be real and fairly widespread. Policymakers have some existing levers that can be used to curb information blocking and help information flow to where it is needed to improve patient care. However, because information blocking is largely legal today, a strong response will involve new legislation and associated enforcement actions.
Electronic health information exchange (hie) is 1 of 3 goals specified by Congress in the 2009 Health Information Technology for Economic and Clinical Health (HITECH) Act to ensure that the $30 billion federal investment in electronic health records (EHRs) results in higher‐quality, lower‐cost care.1 However, HIE progress has been slow,2 and one of the key challenges is ensuring that both providers and EHR vendors have financial incentives that promote engagement in and support of HIE. Providers have expressed concern about the loss of patients and associated revenue that could result from sharing data with competitor organizations and more generally express uncertainty about the return on investment from prioritizing HIE ahead of other investments.3 EHR vendors can improve their bottom‐line by charging high fees for HIE and may also benefit if they make cross‐vendor connectivity difficult because it may increase the likelihood that providers select their product.
However, there is little empirical data that elucidates the extent to which incentives for providers and vendors to pursue HIE are perverse, or simply weak. If incentives are weak, providers and vendors see value in pursuing HIE and should work to achieve it, albeit slowly. If incentives are perverse, providers and vendors are better off when HIE does not occur and would actively work to interfere with it. Concerns about perverse incentives have received substantial attention recently, following a congressional request for the Office of the National Coordinator for Health IT (ONC) to produce a report on information blocking. Information blocking occurs when providers or vendors knowingly and unreasonably interfere with the exchange or use of electronic health information in ways that harm policy goals.4 Since the April 2015 report, which formally defined information blocking and contained several examples of known information blocking, 2 congressional committees proposed legislation that would give the federal government tools to curb information blocking, which is largely legal today.5, 6
Before concerted action is taken in response to information blocking, it is critical to assess the extent to which information blocking occurs and the specific forms that it takes, as well as to better understand the effectiveness of policy responses. Because information blocking is a relatively new concept and also because it occurs in the form of provider and vendor business practices, there is no existing data that speaks to these open questions. Therefore, in this study, we sought to collect data that could help guide an effective policy response to information blocking. We surveyed third‐party HIE organizations because they routinely observe the business practices of providers and vendors as part of their mission to enable HIE among providers in a geographic region that use diverse EHR systems. We sought to answer the following specific research questions: (1) To what extent do EHR vendors and providers engage in information blocking? (2) When information blocking occurs, what are the most common forms that it takes? (3) What policy strategies are perceived as most effective in curbing information blocking? Our results offer the first systematic, national data on information blocking and directly inform a policy response that fosters an environment that promotes broad‐based electronic health information exchange.
Methods
Definition and Identification of Sampling Frame of Those Leading HIE Efforts
We sought to survey individuals currently leading HIE efforts and to target the subset who would report on information blocking with the least possible bias. We therefore limited our sample along 2 dimensions. First, we excluded efforts that only enable exchange within a single provider enterprise (ie, all exchange partners are under the same ownership) as well as those led by single, or a consortium of, electronic health record vendors (eg, Epic's CareEverywhere platform or the CommonWell Health Alliance). We made this decision because these HIE efforts are led by the types of organizations that are believed to engage in information blocking and, therefore, do not represent the more neutral “third‐party” perspective on information blocking that we sought. Second, we excluded defunct HIE efforts because leaders of these efforts may be more prone to perceive certain behaviors by providers or EHR vendors as information blocking when they are not. Even with these exclusions, it is likely that some degree of bias remains in our sample, which may be related to the possibility that HIE efforts themselves are a contributor to information blocking. This key limitation of our sample is further addressed in the limitations section.
Our sampling frame included 141 individuals who led a HIE effort that met our inclusion criteria as of early 2015. We had access to this list as part of a longitudinal national survey of HIE efforts that we conducted over the past 10 years, most recently in early 2015.7, 8, 9, 10 Our lead for each HIE effort is the person who completed prior surveys that asked about organizational demographics (eg, participants involved in data exchange, types of data exchanged, governance, geographic coverage), ability to support meaningful use criteria, engagement in delivery and payment reform, funding sources, and barriers to development. Respondents therefore had detailed knowledge of HIE and were almost always the CEO or other senior leader of the effort.
Survey Instrument Development
We developed a new survey instrument focused specifically on information blocking, as opposed to broader barriers to HIE and interoperability. The survey included 4 sections. The first section defined information blocking using the definition from the ONC report4 to help ensure that respondents shared a common understanding of the phenomenon. The first section then asked about respondents’ familiarity with information blocking and about the extent to which they had direct or indirect contact with EHR vendors and providers, assuming that such contact provided the opportunity to observe information blocking practices. Respondents had to indicate that they had direct or indirect contact with EHR vendors in order to be shown questions about vendor engagement in information blocking, and similarly had to indicate contact with providers in order to be shown questions about provider information blocking.
The second section of the survey asked respondents to identify the frequency with which EHR vendors and providers engage in information blocking. Response choices were “routine,” “occasional,” or “rare.” Because we expected that different types of provider organizations might engage in information blocking to different degrees, we asked about the frequency of information blocking separately for large hospital or health systems; independent urban hospitals; independent rural hospitals, including critical access hospitals and federally qualified health centers; independent practices (primary care); and independent practices (specialty care).
The third section asked about the frequency with which EHR vendors engage in 8 specific forms of information blocking. For hospitals and health systems, we asked about the frequency with which they engage in 3 specific forms of information blocking. We focused on this type of provider organization because they are largely the focus of concerns about information blocking practices. This section of the survey also asked about the perceived motivations for each stakeholder group to engage in information blocking, and these questions included a “don't know” option because respondents may not have interacted with vendors and providers in a way that allowed them to form an opinion on vendor or provider motivations. We developed our list of specific forms of information blocking and motivations from the ONC information‐blocking report and the ONC expert who wrote the report.
The fourth and final section of the survey asked about the effectiveness of policy responses to address information blocking. The list of policy solutions differed for EHR vendors (7 options) and for hospitals and health systems (6 options). Response choices were “very effective,” “moderately effective,” and “not effective.”
We pilot tested the survey with 3 leaders of HIE efforts and modified questions in response to feedback.
Survey Administration
The survey was administered between October 2015 and January 2016. We sent a link to the Qualtrics online survey to all respondents on our list, and nonrespondents received a minimum of 3 emails and 2 phone calls. There were no financial incentives offered to participate. We removed 32 names from our original sampling frame of 141 because the contact had left the HIE effort, and we removed an additional 4 names from the list because the contact told us that they had organizational constraints that prevented them from responding to the survey. This left us with 105 leaders of HIE efforts, with 60 responding to the survey (a 57% response rate).
Analysis
We first assessed the extent to which respondents reported familiarity with information blocking. Given that all respondents indicated at least some familiarity with information blocking, we did not restrict results based on degree of familiarity. To answer our first research question regarding frequency of information blocking, for EHR vendors and hospitals/health systems separately, we calculated the proportion of respondents who indicated that information blocking was routine, occasional, and rare. To answer our second research question, for each form of information blocking for each stakeholder group, we calculated the proportion of respondents who indicated “routinely/often,” “sometimes,” and “rarely/never.” We similarly calculated the frequency of response choices for each perceived information‐blocking motivation for each stakeholder group, including the “don't know” option. To answer our third research question, we calculated the proportion of respondents who indicated that each policy strategy was likely to be very effective, moderately effective, and not effective, again separately for EHR vendors and for hospitals/health systems.
Results
Familiarity With Information Blocking and Breadth of Engagement With Vendors and Providers
Overall, 83% of respondents indicated strong familiarity with information blocking, 12% reported some familiarity, and 5% reported minimal familiarity. Of the 60 respondents, 59 worked with both EHR vendors and providers, and the remaining respondent worked with EHR vendors and not providers (and therefore was not asked to respond to questions about provider engagement in information blocking). On average, respondents had worked with 18 EHR vendors (range of 2–138) and with 31 hospitals or health systems (range of 1–140).
Frequency of Information Blocking
Fifty percent of respondents reported that EHR vendors routinely engage in information blocking, with an additional 33% reporting that EHR vendors engage in information blocking occasionally (Figure 1). The remaining 17% of respondents indicated that EHR vendors rarely engage in information blocking. Frequency of information blocking by hospitals and health systems was lower. Twenty‐five percent of respondents indicated that these providers routinely engage in information blocking, with an additional 34% reporting that they do so occasionally and 41% saying that information blocking was rare (see Figure 1).
Figure 1.
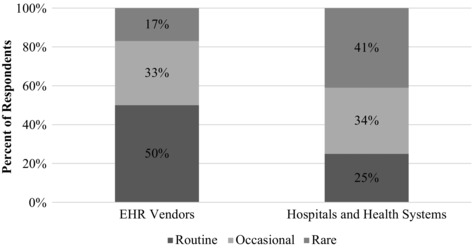
Frequency of Information Blocking
Forms of Information Blocking
Among the 8 specific forms of information blocking in which EHR vendors may engage, 49% of respondents reported that vendors routinely or often deploy products with limited interoperability. Forty‐seven percent of respondents reported that vendors routinely or often charge high fees for HIE unrelated to cost, followed by 42% that reported that vendors routinely or often make third‐party access to standardized data difficult (Table 1).
Table 1.
Specific Forms of Information Blocking
| Often/Routinely | Sometimes | Rarely/Never | |
|---|---|---|---|
| EHR Vendors | |||
| Deployment of products with limited interoperability | 49% | 31% | 20% |
| High fees for HIE unrelated to cost | 47% | 40% | 13% |
| Making third‐party access to standardized data difficult | 42% | 41% | 17% |
| Refusing to support HIE with specific vendors or HIEs | 31% | 37% | 32% |
| Making data export difficult | 28% | 40% | 32% |
| Changing HIE contract terms postimplementation | 19% | 21% | 60% |
| Unfavorable contract terms for HIE | 17% | 35% | 48% |
| Gag clauses on providers speaking out about information‐blocking practices | 12% | 18% | 70% |
| Hospitals and Health Systems | |||
| Coercing providers to adopt particular EHR or HIE technology | 28% | 24% | 48% |
| Controlling patient flow by selectively sharing patient health information | 22% | 24% | 54% |
| Using HIPAA as a barrier to patient health information sharing when it is not | 15% | 35% | 50% |
Among the 3 specific forms of information blocking in which hospitals and health systems may engage, 28% of respondents reported that they routinely or often coerce providers to adopt particular EHR or HIE technology, followed by 22% that reported that hospitals/health systems routinely or often control patient flow by selectively sharing patient information (see Table 1).
Perceived Motivations for Information Blocking
For EHR vendors, respondents perceived that information‐blocking practices were motivated by a desire to maximize short‐term revenue (41% indicated that this was a routine motivation and an additional 28% indicated that this was an occasional motivation) (Figure 2). Another frequent perceived motivation was to increase the likelihood that providers will select their EHR instead of a competitor's EHR (44% routine and 11% occasional). Among hospitals and health systems, the most frequent perceived motivation was also related to improving revenue, namely to strengthen their competitive position in the market (47% routine and 30% occasional), followed by accommodating more important internal priorities than HIE (29% routine and 31% occasional) (see Figure 2).
Figure 2.
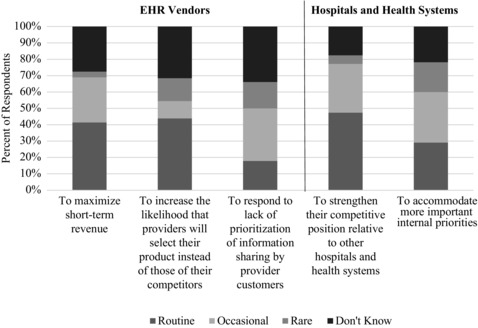
Perceived Motivations for Engaging in Information Blocking
Policy Recommendations to Curb Information Blocking
To curb information blocking by EHR vendors, 3 strategies were roughly equal in the extent to which they were deemed to be either very or moderately effective: prohibiting gag clauses and encouraging public reporting and comparisons of vendors and products (93%); stronger demonstrations of product interoperability “in the field” (92%); and establishing stronger state and/or national infrastructures, policies, and standards for core aspects of information exchange (91%) (Figure 3). Focusing exclusively on the proportion of respondents who reported that a policy strategy would be “very effective,” making information blocking illegal was the most frequent choice (67%).
Figure 3.
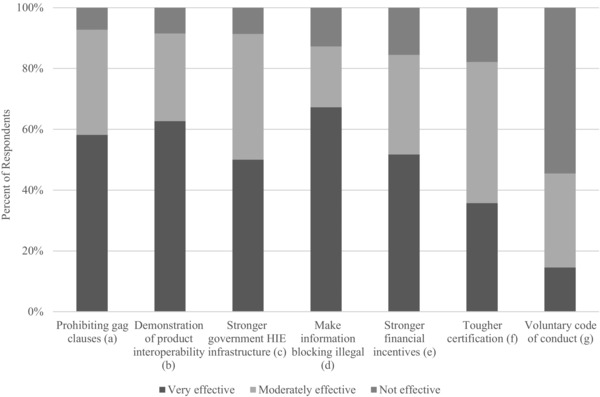
Policy Strategies to Address Information Blocking by EHR Vendors
Note: Full text of each policy option is as follows:
aProhibit “gag clauses” and encourage public reporting and comparisons of vendors and products.
bRequire vendors to demonstrate that their products interoperate with other vendors’ products “in the field.”
cEstablish stronger state and/or national infrastructures, policies, and standards for core aspects of information exchange.
dMake information blocking “illegal” and prosecute those who engage in it.
eCreate stronger financial incentives for supporting providers in engaging in interoperable information exchange.
fCreate stronger interoperability EHR certification requirements.
gFacilitate voluntary adherence to vendor “code of conduct” that prohibits information‐blocking business practices.
For hospitals and health systems, the top 2 policy strategies were stronger Centers for Medicare & Medicaid Services (CMS) incentives for care coordination and/or risk‐based contracts (97%) and public reporting or other efforts to increase transparency of provider business practices (93%) (Figure 4). Limited to strategies deemed “very effective,” making information blocking illegal was the most frequent choice (71%).
Figure 4.
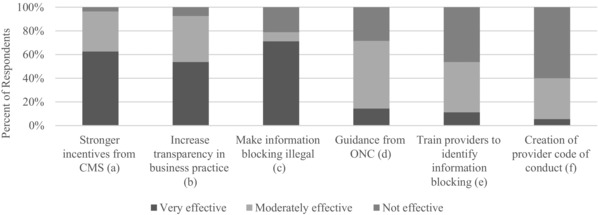
Policy Strategies to Address Information Blocking by Hospitals and Health Systems
Notes: Full‐text of each policy option is as follows:
aEstablish stronger CMS incentives for care coordination and/or risk‐based contracts.
bIncrease public reporting or other efforts to increase transparency of provider business practices.
cMake information blocking illegal and prosecute those who engage in it.
dProvide education and guidance from the Office for Civil Rights and ONC on privacy and security laws governing electronic health information exchange.
eProvide education and outreach from ONC to encourage providers to identify and stop information‐blocking business practices.
fCreate voluntary provider “code of conduct” that prohibits information‐blocking business practices.
Discussion
Information blocking has been a hotly debated policy issue since the Senate Committee on Health, Education, Labor, and Pensions began investigating it in 2016. However, we lack data to shed light on the frequency of information blocking or on effective policy responses. We therefore collected national data specifically on this topic by surveying individuals leading HIE efforts; we chose these respondents because they are in a position to observe information blocking and, as compared to vendors and providers, to provide a less biased assessment. We found that half of respondents reported that EHR vendors routinely engage in information blocking, and one‐quarter of respondents reported that hospitals and health systems routinely do so. The most common forms of, and perceived motivations for, information blocking suggest that it is perceived to confer a competitive advantage. Popular policy responses among our respondents were to promote transparency and address misaligned incentives, as well as to directly combat information blocking by making it illegal. For policymakers, our results offer the first systematic data on information blocking and suggest that some existing policy tools can be leveraged to curb information‐blocking behaviors, but that a strong response will involve new legislation.
We were not surprised to find that more respondents reported that EHR vendors routinely engage in information blocking than do hospitals and health systems. EHR vendors are, with very few exceptions, for‐profit companies and consistently make decisions intended to maximize revenue. In contrast, most hospitals and health systems are not‐for‐profit and routinely balance “mission versus margin” decisions. In addition, not all hospitals and health systems are in competitive markets, and payers are increasingly pursuing risk‐based contracts11 that create incentives for hospitals and health systems to engage in HIE with other providers in their market that they may have previously considered competitors. Nonetheless, given that one‐quarter of respondents reported that hospitals and health systems routinely engage in information blocking, a comprehensive policy response must target EHR vendors as well as these providers.
The specific forms of and perceived motivations for information blocking were harder to predict a priori. What we found in relation to specific forms is that EHR vendors appear to most often engage in information‐blocking behaviors that directly maximize short‐term revenue. Our respondents reported that EHR vendors deploy products with limited interoperability and charge providers high fees unrelated to the actual cost to deliver those capabilities or refuse to support information exchange with specific EHRs and HIEs. These practices may increase the likelihood that providers will select a vendor's EHR instead of a competitor's EHR (the most frequent specific perceived “routine” motivation in our results), which increases short‐term revenue (the second‐most frequent “routine” motivation) as well as long‐term revenue.
In our results, the most commonly reported forms of information blocking among hospitals and health systems point to their interest in strengthening their competitive position in the market by controlling patient flow, which has been reported in other studies.3, 12 Coercing other provider organizations to adopt a specific EHR technology, the most frequent form of information blocking in our results, ties those providers to the given hospital or health system, thereby increasing referrals. By selectively sharing patient information and using HIPAA as a reason not to share information, the second and third most frequent forms of information blocking in our results, hospitals and health systems create barriers that make it less likely that patients will seek care elsewhere.3 Together, these actions may increase patient flow into the organization and then make it difficult for patients to go elsewhere for care.
While not directly informed by our results, vendor and provider motivations may reinforce each other. A hospital or health system seeking to control market share would not be unhappy with an EHR vendor that charges high prices for HIE with other vendors because both stakeholders benefit from the resulting scenario where affiliated providers choose to adopt the vendor's product. This dynamic may also help explain why providers purchase EHRs that do not readily enable HIE. Vendors are incentivized to claim that their products readily enable HIE when they do not, and providers are not incentivized to perform due diligence to assess the true information‐sharing capabilities of the system and negotiate acceptable HIE‐related fees before purchase. If true, it will be critical to pursue a policy response that targets vendors and providers.
Limitations
Our study has several limitations. First, our data reflect the experiences of one type of stakeholder—HIE efforts—whose leaders are working to enable HIE in various regions throughout the country. We chose leaders of specific types of HIE efforts as our target respondents because they are most likely to have observed information blocking if it occurs, are willing to share their experiences, and represent the group most likely to report on information blocking in an unbiased way. However, they are not wholly unbiased; because they seek to enable HIE, it is possible that they are particularly prone to label EHR vendor and provider business practices as information blocking when they are not. It is also possible that some or all HIE efforts intentionally or unintentionally contribute to information blocking, and this could bias our results (though it is unclear in which direction the bias would go). Nonetheless, we believe that our sample offers the least‐biased group of viable respondents and is therefore the best group with which to conduct the first large‐scale survey on information blocking. A related limitation is that our respondents do not observe some forms of information blocking (eg, obstructing electronic patient access to their own health information) and we therefore did not ask about these forms on the survey. In addition, information blocking is still an emerging concept and the ONC definition includes some ambiguity. Thus, there were likely some differences in how our respondents understood our questions. Finally, we achieved a response rate of 57%, and nonrespondents could differ in important ways from respondents. However, given the sensitivity of the topic, this is a strong response rate that is likely sufficient to capture the first national snapshot of experiences with information blocking. Future work, involving different types of respondents, will be required in order to capture a robust and complete understanding of information blocking. It will also be important to assess how information blocking relates to the broader set of challenges impeding health information exchange.13
Policy Implications
Our results have direct policy implications. First, they suggest that policymaker concerns about information blocking are founded and that efforts to pursue policy actions to curb information blocking are warranted. However, given that many respondents did not indicate that information blocking is routine among vendors and providers, actions may be most effective if targeted, though it will be challenging to ascertain exactly when and where information blocking occurs. These dynamics likely explain why the popular policy responses among our respondents included a mix of strategies that foster an environment with incentives that discourage information blocking and direct enforcement by making information blocking illegal. Enforcement is a near‐term strategy that could be used in a narrow way to target egregious offenders and help overcome inertia that is impeding the uptake of policies aimed at realigning economic incentives. In the long run, transparency and value‐based payment should create market dynamics that foster broad‐based information sharing.
The key challenge to pursuing this mix of strategies is that they are not included in our current regulatory framework. Because there is no federal law that directly prohibits information blocking, federal enforcement agencies can only take action against information blocking in very limited circumstances.4, 14 For example, the Office for Civil Rights cannot impose penalties on entities that engage in information blocking unless their actions also violate a specific requirement under HIPAA, such as the requirement to provide patients with a copy of their protected health information upon request.15 Similarly, the Health and Human Services Office of Inspector General (OIG) can only take action against information blocking if it involves kickbacks, fraud, or other illegal practices, as described in a recent policy reminder.16
In the absence of a federal prohibition against information blocking, the tools that are within the authority of the ONC and CMS are fairly weak. For example, the ONC can (and does) collect complaints about occurrences of information blocking and can share these with state and federal authorities, but they cannot respond with direct enforcement action. A somewhat stronger response involves altering the conditions that providers and vendors must meet to participate in (or be certified under) specific programs, such as meaningful use and certification of EHR technologies.4 One approach that the ONC has focused on, and which was popular among respondents in our study, is to increase transparency about the costs and limitations of certified EHRs and the business practices of vendors. The ONC recently finalized new rules that require vendors to disclose detailed information about limitations and the types of costs that could affect the use of certified EHR capabilities.17 However, information is limited to what is relevant to certification, and the ONC therefore cannot require vendors to disclose many of the details needed to determine whether information blocking has occurred.14 For example, many pricing decisions, contractual provisions, and other business policies and practices that interfere with HIE may have no direct relationship to whether a vendor's product possesses certified functionalities.
To address information blocking by providers, a popular option among our respondents was to increase incentives for care coordination and risk‐based contracts. With expansion of accountable care organizations and new value‐based physician payment in the Medicare Access and CHIP Reauthorization Act, it appears that these efforts are under way, but it remains an open question as to whether they will create incentives for broad‐based HIE or simply for larger islands of exchange with information blocking between them.
Given the limitations of current policies, an array of efforts seeks to create new tools to curb information blocking. In its annual appropriations request, the ONC proposed “a coordinated approach to administration and enforcement that builds on and strengthens the existing roles and competencies of the ONC and the OIG. The proposal would explicitly prohibit information blocking by health IT vendors and by health care providers and suppliers. Further, it would authorize the [HHS] secretary to adopt related conditions and requirements for vendors of health IT certified under ONC programs and to require vendors to periodically attest to compliance.”14 In addition, 2 recent bills are circulating in Congress that contain provisions to address information blocking.5, 6 Both propose giving the OIG the authority to investigate and establish deterrents (including financial penalties) to information blocking, similar to what the ONC is proposing, although one bill targets EHR vendors and providers while the other only targets EHR vendors. Beyond federal efforts, 2 states have chosen to take action on their own.18, 19 Most notable is Connecticut, which passed a law that makes information blocking an unfair trade practice and authorizes the state attorney general to bring civil enforcement actions for penalties and punitive damages.18 Against this backdrop, our results serve as a guide to effectively target and tailor these policy responses.
Regardless of which policy strategies are pursued, information blocking should remain high on policymakers’ priority list. When information is not able to flow across provider organizations, there are direct implications for the quality of patient care: missing information impairs clinical decision making in ways that result in care that is unsafe, is duplicative, and fails to meet evidence‐based guidelines. More broadly, when information cannot be shared across the care continuum, it impedes current reform efforts to move toward a person‐centered, high‐performing health care system.4 Relatedly, patients are less able to switch providers and are therefore limited in their choice of providers, which in turn serves to decrease competition among health care providers. Finally, information blocking prevents advances in biomedical and public health research, which require the ability to access information from many sources in order to identify public health risks, develop new treatments, and enable precision medicine.4
Conclusion
In summary, we undertook the first national study to investigate the frequency and forms of and perceived motivations for information blocking among EHR vendors and health care providers. We found that EHR vendors were more often reported to routinely engage in information blocking as compared to hospitals and health systems. For both stakeholders, the perceived motivation was to improve revenue. Policy actions that our respondents considered most effective at curbing information blocking focused on increasing transparency, strengthening incentives, and direct enforcement. Current ONC efforts and bills in Congress pursue enforcement by authorizing the OIG to investigate and establish deterrents to information blocking. If successful, reducing information blocking will help ensure that data follow patients across provider organizations, which is essential to improving the quality and efficiency of care.
Funding/Support
None.
Conflict of Interest Disclosures: All authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Dr. Adler‐Milstein reports financial support from QPID Health outside of this work.
Acknowledgments: We would like to acknowledge Karson Mahler for his invaluable feedback on the survey and manuscript.
References
- 1. Blumenthal D. Stimulating the adoption of health information technology. N Engl J Med. 2009;360(15):1477‐1479. [DOI] [PubMed] [Google Scholar]
- 2. Adler‐Milstein J, DesRoches CM, Kralovec P, et al. Electronic health record adoption in US hospitals: progress continues, but challenges persist. Health Aff (Millwood). 2015;34(12):2174‐2180. [DOI] [PubMed] [Google Scholar]
- 3. Grossman JM, Kushner KL, November EA. Creating sustainable local health information exchanges: can barriers to stakeholder participation be overcome? Res Brief. 2008;(2):1‐12. [PubMed] [Google Scholar]
- 4. Office of the National Coordinator for Health Information Technology . Report to Congress: Report on Health Information Blocking. Washington, DC: Department of Health and Human Services; April 2015. https://www.healthit.gov/sites/default/files/reports/info_blocking_040915.pdf. Accessed October 28, 2016. [Google Scholar]
- 5. TRUST IT Act, S 2141, 114th Cong (2015) . https://www.congress.gov/bill/114th‐congress/senate‐bill/2141?q=%7B%22search%22%3A%5B%22Health+trust%22%5D%7D&resultIndex=2. Accessed October 28, 2016.
- 6. 21st Century Cures Act, HR 6, 114th Cong (2015). https://www.congress.gov/bill/114th‐congress/house‐bill/6. Accessed October 28, 2016.
- 7. Adler‐Milstein J, Bates DW, Jha AK. A survey of health information exchange organizations in the United States: implications for meaningful use. Ann Intern Med. 2011;154(10):666‐671. [DOI] [PubMed] [Google Scholar]
- 8. Adler‐Milstein J, Bates DW, Jha AK. US regional health information organizations: progress and challenges. Health Aff (Milwood). 2009;28(2):483‐492. [DOI] [PubMed] [Google Scholar]
- 9. Adler‐Milstein J, McAfee AP, Bates DW, Jha AK. The state of regional health information organizations: current activities and financing. Health Aff (Milwood). 2008;27(1):w60‐w69. [DOI] [PubMed] [Google Scholar]
- 10. Adler‐Milstein J, Bates DW, Jha AK. Operational health information exchanges show substantial growth, but long‐term funding remains a concern. Health Aff (Milwood). 2013;32(8):1486‐1492. [DOI] [PubMed] [Google Scholar]
- 11. Epstein AM, Jha AK, Orav EJ, et al. Analysis of early accountable care organizations defines patient, structural, cost, and quality‐of‐care characteristics. Health Aff (Milwood). 2014;33(1):95‐102. [DOI] [PubMed] [Google Scholar]
- 12. Grossman JM, Bodenheimer TS, McKenzie K. Hospital‐physician portals: the role of competition in driving clinical data exchange. Health Aff (Milwood). 2006;25(6):1629‐1636. [DOI] [PubMed] [Google Scholar]
- 13. Office of the National Coordinator for Health IT, Health IT Policy Committee . Report to Congress: Challenges and Barriers to Interoperability. Washington, DC: Department of Health and Human Services; December 2015. https://www.healthit.gov/facas/sites/faca/files/HITPC_Final_ITF_Report_2015‐12‐16%20v3.pdf. Accessed October 28, 2016. [Google Scholar]
- 14. Office of the National Coordinator for Health IT . Fiscal Year 2017: Justification of Estimates for Appropriations Committee. Washington, DC: Department of Health and Human Services; 2016. https://www.healthit.gov/sites/default/files/final_onc_cj_fy_2017_clean.pdf. Accessed October 28, 2016. [Google Scholar]
- 15. US Department of Health and Human Services . Access of individuals to protected health information. 45 CFR §164.524. https://www.law.cornell.edu/cfr/text/45/164.524. Accessed October 28, 2016.
- 16. Office of Inspector General . OIG Policy Reminder: Information Blocking and the Federal Anti‐Kickback Statute. Washington, DC: US Department of Health and Human Services; October 6, 2015. http://oig.hhs.gov/compliance/alerts/guidance/policy‐reminder‐100615.pdf. Accessed October 28, 2016. [Google Scholar]
- 17. US Department of Health and Human Services . 2015 Edition Health Information Technology (Health IT) Certification Criteria, 2015 Edition Base Electronic Health Record (EHR) Definition, and ONC Health IT Certification Program Modifications. https://www.federalregister.gov/articles/2015/10/16/2015‐25597/2015‐edition‐health‐information‐technology‐health‐it‐certification‐criteria‐2015‐edition‐base#p‐1537. Published October 16, 2015. Accessed October 28, 2016.
- 18. An Act Concering Hospitals, Insurers, and Health Care Consumers. SB 811, Public Act 15‐146 (Conn 2015) . https://www.cga.ct.gov/2015/ACT/PA/2015PA‐00146‐R00SB‐00811‐PA.htm. Effective October 1, 2015. Accessed October 28, 2016.
- 19. HB 2609, 98th General Assembly, 2nd Sess (Mo 2016) . http://www.house.mo.gov/billtracking/bills161/billpdf/intro/hb2609i.pdf. Introduced February 23, 2016. Accessed October 28, 2016.


