Abstract
The flavivirus E glycoprotein, the primary antigen that induces protective immunity, is essential for membrane fusion and mediates binding to cellular receptors. Human flavivirus infections stimulate virus species-specific as well as flavivirus cross-reactive immune responses. Flavivirus cross-reactive antibodies in human sera create a serious problem for serodiagnosis, especially for secondary flavivirus infections, due to the difficulty of differentiating primary from secondary cross-reactive serum antibodies. The presence of subneutralizing levels of flavivirus cross-reactive serum antibodies may result in a dramatic increase in the severity of secondary flavivirus infections via antibody-dependent enhancement. An understanding of flavivirus E-glycoprotein cross-reactive epitopes is therefore critical for improving public health responses to these serious diseases. We identified six E-glycoprotein residues that are incorporated into three distinct flavivirus cross-reactive epitopes. Two of these epitopes which are recognized by distinct monoclonal antibodies contain overlapping continuous residues located within the highly conserved fusion peptide. The third epitope consists of discontinuous residues that are structurally related to the strictly conserved tryptophan at dengue virus serotype 2 E-glycoprotein position 231.
The Flaviviridae are a diverse family of enveloped viruses that infect both arthropods and vertebrates. Members of this family that infect humans frequently cause severe morbidity and mortality, and epidemics of flaviviruses continue to be a major public health concern worldwide. Approximately half of the world's population is at risk of being infected with members of the genus Flavivirus, with 2.5 billion people at risk of infection from the dengue viruses alone (8, 53). This diverse genus includes approximately 70 distinct virus species (8, 33, 49). The medically important flaviviruses include yellow fever virus in Africa and Latin and South America; Japanese encephalitis virus (JEV) in Asia and Australia; West Nile virus in Africa, Central Europe, and most recently, North America; tick-borne encephalitis virus (TBEV) in the temperate regions of Europe, North America, and Asia; and the four serotypes of dengue virus (DENV-1, -2, -3, and -4) in tropical and subtropical regions of the world (36). There are no antiviral drug therapies for any of the flaviviruses, and effective human vaccines are in high demand for many of the medically important species. Human infections by flaviviruses elicit humoral immune responses resulting in the production of virus species-specific as well as flavivirus cross-reactive antibodies (9, 51). The presence of flavivirus cross-reactive antibodies in human sera creates two public health concerns upon secondary infection with heterologous flaviviruses. Firstly, serodiagnosis of secondary flavivirus infections, especially in areas with multiple cocirculating flaviviruses, can be particularly difficult due to the inability to differentiate cross-reactive antibodies elicited by primary infections from those elicited by secondary infections, using the currently available viral antigens. Thus, the identification of the infecting virus either cannot be obtained or is delayed. Additionally, the presence of subneutralizing levels of flavivirus cross-reactive serum antibodies may result in an increase in the severity of secondary flavivirus infections due to antibody-dependent enhancement (ADE), particularly after secondary DENV infection (18, 27, 50, 52). DENV infection typically causes a self-limiting febrile illness known as dengue fever. The incidence of dengue fever epidemics has increased dramatically over the last few decades, with millions of cases occurring annually (22, 53). Moreover, a much more severe form of the disease, dengue hemorrhagic fever (DHF), has emerged during the same time period, causing an estimated 500,000 hospitalizations annually. It is believed that DHF may result from risk associated with sequential infections by heterologous DENV serotypes via ADE (13, 26, 27).
Flaviviruses have a positive-sense single-stranded RNA genome of 10.7 kb that is transcribed into a single polyprotein precursor encoding three structural proteins, the capsid (C), premembrane (prM), and envelope (E) proteins, and seven nonstructural proteins (36, 45). The flavivirus E glycoprotein, the primary antigen that induces protective immunity, is essential for membrane fusion and mediates binding to cellular receptors (4, 14, 44). The flavivirus E glycoprotein therefore directly affects the host range, tissue tropism, and virulence of these viruses. The crystal structures of the ectodomains of the TBEV E glycoprotein and the DENV-2 E glycoprotein have been determined at high resolutions (40, 44). In mature virus particles, the E glycoprotein forms head-to-tail homodimers that lie flat and form a dense lattice on the viral surface (32). The flavivirus E glycoprotein contains three structural and functional domains. Domain I (DI) is an eight-stranded β-barrel containing two large insertion loops that form the elongated finger-like domain II (DII) (44). DII is involved in stabilizing the E-glycoprotein dimer and contains the internal fusion peptide (4). Domain III (DIII) forms a 10-stranded β-barrel with an immunoglobulin-like fold and contains the cellular receptor-binding motifs (14, 40). DI, DII, and DIII have been shown to correlate well with previously identified antigenic regions C, A, and B, respectively (40, 44). DI and DIII (C and B) contain predominately subcomplex- and type-specific epitopes, whereas DII (A) contains the major flavivirus group and subgroup cross-reactive epitopes which are sensitive to reduction and denaturation and are formed from discontinuous amino acid sequences (38, 44, 46).
For this study, we used a DENV-2 prM/M and E-glycoprotein expression plasmid (11) to map flavivirus cross-reactive epitopes. We identified and initially characterized amino acids involved in three discrete flavivirus E-glycoprotein cross-reactive epitopes by using a structure-based rational mutagenesis approach. Two of these cross-reactive epitopes are recognized by distinct monoclonal antibodies (MAbs) yet were previously grouped into the same flavivirus group-reactive epitope A1. Here we show that epitope A1 actually contains at least two independent yet overlapping group-reactive epitopes, incorporating two or three of the highly conserved fusion peptide residues Gly104, Gly106, and Leu107. The third flavivirus cross-reactive epitope (A5) is structurally less discrete but centers on the strictly conserved Trp231 residue and its structurally related neighbors Glu126 and Thr226. The identification and characterization of amino acids that are incorporated into these flavivirus cross-reactive epitopes demonstrate that the application of this approach extends our understanding of the structure-function relationships which are important for flavivirus E-glycoprotein biology and immunopathology. These findings provide important tools and insights for improving flavivirus serodiagnosis, understanding the pathogenesis of ADE, and advancing the development of safe and effective flavivirus vaccines, all of which are essential for improving public health responses to continued emerging flavivirus epidemics worldwide.
MATERIALS AND METHODS
Cell culture, virus strain, and recombinant plasmid.
COS-1 cells (ATCC CRL 1650; American Type Culture Collection, Manassas, Va.) were grown at 37°C with 5% CO2 in Dulbecco's modified Eagle's minimal essential medium (DMEM; Gibco, Grand Island, N.Y.) supplemented with 10% heat-inactivated fetal bovine serum (HyClone Laboratories, Inc., Logan, Utah), 110 mg of sodium pyruvate/liter, 0.1 mM nonessential amino acids, 2 mM l-glutamine, 20 ml of 7.5% NaHCO3/liter, 100 U of penicillin/ml, and 100 μg of streptomycin/ml. CHO cells (ATCC CCL 61) were grown under the same conditions as COS-1 cells with a DMEM-F12 nutrient mixture.
We used the recombinant expression plasmid pCB8D2-2J-2-9-1 as a template DNA for both site-directed mutagenesis and transient expression of the DENV-2 recombinant antigen (see below). This plasmid includes the human cytomegalovirus early gene promoter, the JEV signal sequence, the DENV-2 prM and envelope (E) gene region (amino-terminal 80%), the carboxyl-terminal 20% of the JEV E gene region, and a bovine growth hormone poly(A) signal. This recombinant expression plasmid was recently characterized and described in detail (11). The replacement of the terminal 20% of DENV-2 E with JEV E gene sequences dramatically increases the secretion of extracellular virus-like particles (VLPs) into the culture medium without altering the native DENV-2 E-glycoprotein conformation (11).
Site-directed mutagenesis.
Site-specific mutations were introduced into the DENV-2 E gene by use of a Quick Change multisite-directed mutagenesis kit (Stratagene, La Jolla, Calif.), with pCB8D2-2J-2-9-1 as a DNA template, according to the manufacturer's recommended protocols. The sequences of the mutagenic primers used for all constructs are listed in Table 1. Four or five colonies from each mutagenic PCR transformation were selected and grown in 5-ml Luria-Bertani broth cultures, mini-prepped, and sequenced. Structural gene regions and regulatory elements of all purified plasmids were sequenced entirely upon identification of the correct mutation. Automated DNA sequencing was performed with a CEQ 8000 genetic analysis system (Beckman Coulter, Fullerton, Calif.), and sequences were analyzed with Beckman Coulter CEQ 8000 and Lasergene software (DNASTAR, Madison, Wis.).
TABLE 1.
Nucleotide sequences of primers used for mutagenesis
| Primer | Mutagenic primer sequence (5′-3′)a | Nucleotide mutation | Amino acid substitution |
|---|---|---|---|
| K64N | TGTTGTTGTGTTGGTTAGGTTTGCCTCTATACAG | AAG-AAC | Lys-Asn |
| T76M | TGGGTTCCCCTTGCATTGGGCAGCGAGATTCTGTTGTTG | ACA-ATG | Thr-Asn |
| Q77R | TTCATTTAGGCTGGGTTCCCCTCGTGTTGGGCAG | CAA-CGA | Gln-Arg |
| G104H | CCCTTTCCAAATAGTCCACAGTGATTTCCCCATCCTCTGTCTACC | GGA-CAC | Gly-His |
| G106Q | GCCTCCCTTTCCAAATAGTTGACATCCATTTCCCCA | GGA-CAA | Gly-Gln |
| L107K | GGTCACAATGCCTCCCTTTCCAAATTTTCCACATCCATTTCCCC | CTA-AAA | Leu-Lys |
| E126A | AGTTTTCTGGTTGCACAACTTTTCCTGCCATGTTCTTTTTGC | GAA-GCA | Glu-Ala |
| T226N | GTATCCAATTTGACCCTTGATTGTCCGCTCCGGGCAACC | ACA-AAT | Thr-Asn |
| W231F | GTCTCTTTCTGTATGAAATTTGACCCTTGTGTGTC | TGG-TTC | Trp-Phe |
| W231L | AATGTCTCTTTCTGTATCAGATTTGACCCTTGTGTGTCCGCTCC | TGG-CTG | Trp-Leu |
| H244R | TCCTGTTTCTTCGCACGGGGATTTTTGAAAGTGACC | CAT-CGT | His-Arg |
| K247R | ACAACAACATCCTGTCGCTTCGCATGGGGATTTTTG | AAA-CGA | Lys-Arg |
The mismatched nucleotides causing the desired substitutions are shown in bold.
Transient expression of DENV-2 recombinant antigens in COS-1 or CHO cells by electroporation.
COS-1 and CHO cells were electroporated with pCB8D2-2J-2-9-1 according to a previously described protocol (10). Electroporated cells were recovered in 50 ml of DMEM, seeded into 150-cm2 culture flasks for VLP expression and into 96-well tissue culture plates for immunofluorescence assays (IFAs), and incubated at 37°C with 5% CO2. Six to 8 h after electroporation, the growth medium in the 150-cm2 culture flasks was replaced with DMEM containing 2% fetal bovine serum. Cells in 96-well plates for IFAs were fixed at 14 to 18 h postelectroporation. The tissue culture medium and cells were harvested at 48 and 96 h postelectroporation for antigen characterization.
Characterization of mutant pCB8D2-J2-2-9-1-infected cells and secreted antigen.
Fourteen to 18 h after electroporation, 96-well tissue culture plates (Costar #3603; Corning, Inc., Corning, N.Y.) containing cells transformed with the mutated pCB8D2-2J-2-9-1 clones were washed twice with phosphate-buffered saline, fixed with 3:1 (vol/vol) acetone-phosphate-buffered saline for 10 min, and air dried. E-glycoprotein-specific MAbs recognizing each of the three E-glycoprotein domains were used to determine affinity reductions in DII cross-reactive epitopes by indirect IFAs as described previously (10).
The tissue culture medium was harvested 48 and 96 h after electroporation. Cell debris was removed from the tissue culture medium by centrifugation for 30 min at 10,000 rpm in a Sorvall SS-34 rotor at 4°C. An antigen-capture enzyme-linked immunosorbent assay (Ag-ELISA) was used to detect secreted antigens from the mutagenized pCB8D2-2J-2-9-1-transformed COS-1 cells. Secreted antigens were captured with polyclonal rabbit anti-DENV-2 sera (46) used at a 1:10,000 dilution. Murine hyperimmune ascitic fluid (MHIAF) specific for DENV-2 was used at a 1:3,000 dilution to detect the captured antigen, and this MHIAF was detected with horseradish peroxidase-conjugated goat anti-mouse HIAF used at a 1:5,000 dilution.
Secreted antigens were concentrated from positive tissue culture media by centrifugation overnight at 19,000 rpm in a Beckman type 19 19,000 rpm rotor at 4°C and were resuspended in TNE buffer (50 mM Tris, 100 mM NaCl, 10 mM EDTA, pH 7.5) to 1/200th the original volume. The concentrated antigen was analyzed with our panel of anti-DENV-2 MAbs in an Ag-ELISA to determine MAb end-point reactivities of the mutated antigens according to the protocol of Roehrig et al. (46). This Ag-ELISA protocol was the same as that used above to detect secreted antigens, with the exception of using the specified MAbs (see Table 3) instead of polyclonal MHIAF.
TABLE 3.
MAb reactivities for wild-type and mutant plasmid-transfected cells and for secreted VLP antigens
| Strain or assaya | Epitope, MAb, PRNT, SA, specificityb
|
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Polyclonal, D2HIAE, +, NA | A1a, 4G2, +, +, group | A1b, 6B6C-1, ±, +, group | A2, 4E5, +, −, subcomplex | A3, 1A5D-1, −, ±, type | A5, 1B7-5, +, +, subgroup | A/C?, 10A1D-2, −, ±, complex | C1, 1B4C-2, −, +, subcomplex | C4, 9A4D-1, −, −, type | B1, 3H5, +, +, type | B2, 9A3D-8, +, +, type | B3, 10A4D-2, +, +, subcomplex | B4, 9D12, +, +, type | |
| Wild Type | |||||||||||||
| IFA | 4.1 | 3.8 | 3.8 | 2.6 | 4.4 | 4.1 | ≥2.9 | 4.4 | ≥2.9 | >4.4 | 3.5 | 4.1 | >4.4 |
| Ag-ELISA | >6.0 | >6.0 | ≥6.0 | ≥2.9 | 4.2 | 5.7 | >3.8 | >5.3 | 2.9 | >6.0 | >6.0 | >6.0 | >6.0 |
| T76M | |||||||||||||
| IFA | ND | ND | |||||||||||
| Ag-ELISA | ≤5 | 0.8 | |||||||||||
| G104H | |||||||||||||
| IFA | <3 | 6 | <0.8 | 3 | ND | ND | |||||||
| Ag-ELISA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| G106Q | |||||||||||||
| IFA | <3 | <3 | <0.8 | ND | 6 | ND | |||||||
| Ag-ELISA | <0.1 | <0.1 | <6 | 13 | ≤0.1 | ||||||||
| L107K | |||||||||||||
| IFA | <3 | <25 | 6 | ND | ND | ||||||||
| Ag-ELISA | <0.1 | 5 | 6 | 0.2 | |||||||||
| E126A | |||||||||||||
| IFA | 6 | ND | ND | ||||||||||
| Ag-ELISA | 10 | 13 | |||||||||||
| E126A/T226N | |||||||||||||
| IFA | 3 | 3 | <25 | ND | ND | ||||||||
| Ag-ELISA | 5 | 13 | |||||||||||
| W231F/L | |||||||||||||
| IFA | <3 | <3 | <2 | 6 | |||||||||
| Ag-ELISA | NA | NA | NA | NA | NA | NA | |||||||
Reciprocal end-point titers (log10) for plasmid-transfected cells (IFA) and for secreted VLPs (Ag-ELISA) are shown for the wild-type non-mutated plasmid. MAb end-point values for mutant plasmids and mutant VLP antigen that differed more than fourfold from those of the non-mutated wild-type plasmid are shown as percentages of the remaining wild-type antigen reactivity and shown in bold. MAb end-point values that did not differ from the wild-type by four-fold or more were left blank. NA, not applicable (these constructs did not secrete VLP antigen and thus could not be examined by Ag-ELISA); ND, not determined.
PRNT, plaque reduction neutralization titer at a 1:100 dilution of ascitic fluid (46); SA, epitope surface accessibility from antigen-capture log10 ELISA end-point titers. −, ≤3.0; ±, 3.0 to 5.0; +, ≥5.0.
Identification of DII cross-reactive epitope residues.
To localize the epitopes responsible for inducing flavivirus cross-reactive antibodies, we developed the following procedural algorithm. We initially identified strictly conserved flavivirus residues. These residues were mapped onto the 2.0-Å-resolution E-glycoprotein structure for TBEV (44) and onto a computer-predicted homology model structure for the DENV-2 E glycoprotein by the use of Swiss-Pdb Viewer 3.7 structure analysis software (24; http://www.expasy.org/spdbv/) (the high-resolution DENV-2 E-glycoprotein structure [40] had not yet been published when this work began). A literature review of high-resolution structures for protein antigen-antibody complexes found that typically 10 to 20 residues are involved in making direct contacts between the antigen epitope and the antibody paratope. These contacts result in 20 to 30 residues that are “buried” by the typical antibody footprint, which measures approximately 20 by 30 Å. On average, however, only 25% of the buried side chains, or four to six residues, account for most of the MAb binding energy (5, 7, 15, 17, 19, 34, 37, 41). Based upon this review of the literature, we developed the following criteria to select the most probable flavivirus cross-reactive epitope residues: (i) amino acids must be located in DII (amino acids 52 to 135 and 195 to 285 of the TBEV E protein [44] and amino acids 52 to 132 and 193 to 280 of the DENV-2 E protein [39]) and conserved among the flaviviruses, (ii) amino acids must be on the outer or lateral surface of the E-glycoprotein dimer, (iii) amino acids should have at least a 35% surface accessibility potential, (iv) side chain projections must be accessible to antibody paratopes, and (v) residues with high-temperature (β) factors should be favored, as these residues tend to be flexible and are able to conform to the antibody paratope, increasing the antibody-antigen affinity.
Using this structure-based design approach, we narrowed the number of candidate flavivirus cross-reactive epitope residues from a total of 53 conserved amino acids in DII (38 invariant and 15 almost completely conserved) to fewer than 10 probable DII cross-reactive epitope residues. We modeled amino acid substitutions at these probable cross-reactive epitope residues, selecting substitutions that should disrupt or eliminate antibody recognition without altering the E-glycoprotein structural conformation, disrupting dimer interactions, or impairing particle formation, maturation, or secretion. For this reason, cysteine residues that satisfied our cross-reactive epitope criteria were not considered for mutagenesis because of their involvement in disulfide bridging, which is necessary for proper E-glycoprotein structure and function (40, 44). Stability calculations were performed for all possible amino acid substitutions of candidate residues by using the Prediction of Proteins Mutations Stability Changes server (http://babylone.ulb.ac.be/popmusic/index.html) (26) and the TBEV E-glycoprotein Protein Data Bank file coordinates (44). Amino acid substitutions modeled in the TBEV E-glycoprotein structure causing free energies of folding that were equal to or less than that of the nonmutated wild-type E glycoprotein were reexamined with Swiss-Pdb Viewer software to identify those substitutions that minimized local structural disturbances while maintaining structurally relevant biochemical interactions such as hydrogen bonding and/or charge interactions with neighboring amino acids. Because the outer surfaces of mature flavivirus particles are covered with a dense network of E and prM/M proteins, any conformational changes in the E glycoprotein are likely to induce concerted reorganization across the surface of the virion (32, 40). A comparison of a priori stability calculations based on the TBEV E-glycoprotein structure and a posteriori stability calculations from the DENV-2 atomic structure is shown in Table 2.
TABLE 2.
Stability free energy (ddG) calculations for putative domain II cross-reactive epitope substitutions based upon the published PDB coordinates for the DENV-2 (40) and TBEV (44) E-glycoprotein structures
| DENV-2 substitution | ddG (kcal/mol) | TBEV substitution | ddG (kcal/mol) |
|---|---|---|---|
| K64N | −0.45 | K64N | −0.15 |
| T76M | −0.54 | T76M | −0.02 |
| Q77R | 0.45 | M77R | −0.10 |
| G104H | −0.16 | H104H | NA |
| G106Q | 0.87 | G106Q | −0.03 |
| L107K | 0.19 | L107K | 0.12 |
| E126A | 2.16 | K126A | 0.85 |
| T226N | 0.33 | Q233N | 0.03 |
| E126A/T226N | 2.49 | K126A/Q233N | 0.88 |
| W231F | 1.54 | W235F | 1.34 |
| W231L | 1.84 | W235L | 2.26 |
| H244R | 4.18 | H248R | 0.00 |
| K247R | −0.30 | K251R | −0.19 |
Upon the successful identification of cross-reactive epitope residues, we conducted a nearest neighbor search of the surface of the E-glycoprotein structure to look for additional residues located within 10 to 15 Å of the identified residues. This distance is within the binding footprint of a single antibody paratope (17). In this second iteration of cross-reactive epitope residue identification, we used the same five optimality criteria as described above, with one change. We relaxed the criterion of strict conservation among the flaviviruses to now include variable residues. In this way, we could identify residues that were conserved in their physicochemical nature and/or conserved only within a particular flavivirus complex, such as the four DENV serotypes.
RESULTS
We chose to focus on two previously identified epitopes, A1 and A5, defined by MAbs 4G2 (A1a), 6B6C-1 (A1b), and 1B7-5 (A5) from our panel of anti-DENV-2 antibodies. These two epitopes share several characteristics: they are surface accessible and located in DII, they are flavivirus group or subgroup reactive, they are reduction-denaturation sensitive, they are involved in blocking virus-mediated cell membrane fusion and virus neutralization, and tryptic fragment mapping indicates that they are formed by two discontinuous DENV-2 E-glycoprotein peptide fragments, amino acids (aa) 1 to 120 and aa 158 to 400 (1, 28, 39, 46). We assessed prospective cross-reactive epitope residues by looking for decreases in the reactivities of these three DII cross-reactive MAbs with mutant plasmid-transfected cells by IFA and with mutant VLPs by Ag-ELISA. Proper E-glycoprotein folding and structural conformation were assessed with a panel of E-protein-reactive DENV complex-, subcomplex-, and type-specific MAbs.
Amino acids Gly106, Trp231, His244, and Lys247.
We focused initially on four potential flavivirus cross-reactive epitope residues, identified by the procedural algorithm described in Materials and Methods. The following single amino acid substitutions were introduced into the DENV-2 prM/E expression plasmid: Gly106 to Glu (G106Q), Trp231 to Phe (W231F), His244 to Arg (H244R), and Lys247 to Arg (K247R) (Table 1). Substitutions at Gly106 and Trp231 strongly interfered with the binding of flavivirus cross-reactive MAbs (Table 3). However, substitutions at His244 and Lys247 did not have an effect on the binding of these same cross-reactive MAbs or of any other MAbs from our panel (data not shown).
Gly106 is located within the fusion peptide (3) at the very tip of DII in the E-glycoprotein monomer (Fig. 1 and 2). As with the other fusion peptide residues, Gly106 is strongly conserved among the flaviviruses, with the one exception being Modoc virus, which has an alanine at this position (Table 4). Gly106 is located at the distal end of each E monomer along the upper and outer lateral surfaces of the dimer. This residue has a moderately high surface accessibility, and its relatively high temperature (β) factor suggests its potential flexibility. We modeled the substitution of a large, bulky, polar glutamine residue for glycine at this position. The glutamine substitution fit well into the surrounding region, did not appear to disrupt the local hydrogen bonding network, and produced acceptable stability calculations with the TBEV E-glycoprotein structure coordinates (Table 2). Trp231 is located in a long intervening loop sequence between DII β-strands h and i (40) (Fig. 1). Trp231 lies in a trough on the upper and outer surfaces of DII (Fig. 2). It is structurally close to the glycan on Asn67 and lies laterally exterior to the disulfide bridge between Cys60 and Cys121. The large hydrophobic side chain lies parallel to the dimer surface within this trough. This residue is only moderately surface accessible, yet its high temperature (β) factor and the lack of hydrogen bonding from surrounding residues to the side chain suggest its potential flexibility. Although all of the substitutions that we modeled at Trp231 were predicted to induce substantially high energetic costs based on our stability analyses (data not shown), the phenylalanine substitution was the least costly substitution at this position (Table 2). The phenylalanine side chain fit well into the surrounding molecular region with limited disruption of the local hydrogen bonding network.
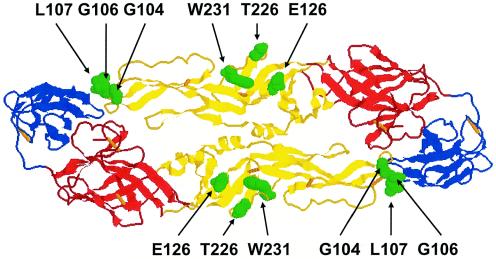
FIG. 1.
DENV-2 envelope glycoprotein homodimer. The image shows a top view looking down towards the viral surface and depicts the locations of flavivirus cross-reactive epitope residues, which are highlighted by green space-filling representations. The structural and functional domains I, II, and III are shown in red, yellow, and blue, respectively, and disulfide bridges are shown as orange bars.
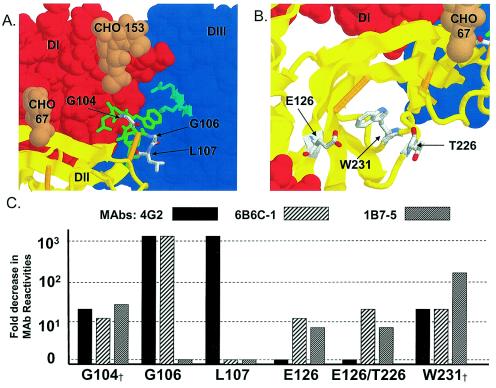
FIG. 2.
Structural locations of cross-reactive epitope residues for flavivirus cross-reactive MAbs in the atomic structure of the DENV-2 E-glycoprotein dimer and bar graphs indicating reductions in MAb reactivities as assayed by IFA and/or Ag-ELISA for mutations at these E-glycoprotein positions. (A) Flavivirus group-reactive A1 epitope residues (MAbs 4G2 and 6B6C-1) from the fusion peptide region of DII. This view is looking downward toward the viral membrane surface at an angle of ∼45° while looking in toward the fusion peptide region about 45° off of parallel to the dimer's longitudinal axis. DI, DII, and DIII are shown in red, yellow, and blue, respectively. DI and DIII from the alternate subunit are depicted as space-filling Van der Waals surfaces to highlight the close fitting of the fusion peptide into this region. Fusion peptide residues 100 to 108 are depicted in green, with the participating amino acids colored by atom and labeled. Glycan moieties attached to Asn153 and Asn67 are depicted with tan space-filling models (labeled CHO153 and CHO67, respectively), and disulfide bridges are shown as orange bars. Lys310 and Arg323 from DIII are depicted as light cyan blue sticks to emphasize that along with the glycan on residue 153, these moieties cover and protect fusion peptide residues Trp101 and Gly102. (B) Flavivirus subgroup-reactive epitope residues (MAb 1B7-5). The angle of this view and the coloring and labeling scheme are the same as those for panel A. The residues identified in this study are depicted as sticks and are labeled as colored individual atoms. (C) Bar graph showing decreases in cross-reactive MAb reactivities in Ag-ELISA for DENV-2 VLPs with substitutions at the listed residues. The fold decreases in MAb reactivities were determined by dividing the wild-type antigen end-point MAb titers by the mutant antigen end-point titers. Anti-A1 reactive MAbs 4G2 and 6B6C-1 are flavivirus group-reactive antibodies, and the anti-A5 MAb 1B7-5 is a flavivirus subgroup-reactive antibody. †, substitutions at G104 and W231 produced plasmids which were unable to secrete measurable VLP antigen into the tissue culture medium. Therefore, fold decreases in MAb reactivities for these two constructs are from IFA data. MAb reactivities with a wild-type unmutated plasmid did not have end points extending nearly as far in the less sensitive immunofluorescence assay as they did in Ag-ELISA (Table 3), and therefore the reductions for substitutions at G104 and W231 were not as large as those for other constructs that were measured by Ag-ELISA, even though the substitutions at these two positions appeared to completely abolish MAb reactivity.
TABLE 4.
Amino acid sequence variability for proposed cross-reactive epitope residues in domain II of the flavivirus E protein
| Virusa | Residue at indicated positionb
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| K64N | T76M | Q77R | G104H | G106Q | L107K | E126A | T226N | W231F/L | H244R | K247R | |
| DENV-2 | K | T | Q | G | G | L | E | T | W | H | K |
| DENV-4 | S | T | Q | G | G | L | T | T | W | H | R |
| DENV-3 | K | T | Q | G | G | L | E | T | W | H | K |
| DENV-1 | K | T | Q | G | G | L | E | T | W | H | K |
| Japanese encephalitis | S | T | T | G | G | L | I | T | W | H | K |
| Murray Valley encephaltitis | T | T | T | G | G | L | A | T | W | H | K |
| West Nile | T | T | M | G | G | L | I | T | W | H | K |
| St. Louis encephalitis | T | T | T | G | G | L | T | T | W | H | K |
| Ilhéus | T | T | M | G | G | L | T | E | W | H | R |
| Rocio | T | T | M | G | G | L | M | D | W | H | R |
| Bagaza | K | T | M | G | G | L | E | G | W | H | K |
| Iguape | E | Q | M | G | G | L | P | G | W | H | K |
| Bussuquara | K | A | V | G | G | L | A | S | W | H | K |
| Kokobera | Q | T | M | G | G | L | E | G | W | H | K |
| Kédougou | T | T | Q | G | G | L | K | A | W | H | K |
| Zika | S | T | Q | G | G | L | T | T | W | H | R |
| Yellow fever | V | S | T | G | G | L | S | G | W | H | T |
| Sepik | S | T | M | G | G | L | E | G | W | H | T |
| Entebbe Bat | N | T | T | G | G | L | Q | D | W | H | S |
| Tick-borne encephalitis | K | T | M | H | G | L | T | Q | W | H | K |
| Louping ill | K | T | M | H | G | L | T | P | W | H | K |
| Omske hemorrhagic fever | K | A | M | H | G | L | T | V | W | H | K |
| Langat | K | T | M | H | G | L | T | E | W | H | K |
| Alkhurma | K | A | M | H | G | L | T | H | W | H | K |
| Deer tick | K | T | T | H | G | F | V | Q | W | H | K |
| Powassan | K | T | T | H | G | F | V | Q | W | H | K |
| Montana myotis leukoencephalitis | D | T | L | G | G | L | A | H | W | H | K |
| Rio Bravo | S | T | Q | G | G | L | I | S | W | H | K |
| Modoc | E | T | Q | G | A | L | M | P | W | Y | K |
| Apoi | A | T | Q | G | G | L | I | K | W | H | K |
Sequences for viruses in italics have not yet been published (Kuno and Chang, personal communication).
DENV-2 strains containing variable amino acid sequences at these positions are indicated as follows with their Genbank accession numbers: 64R, AF359579; 77L, M24449; X15434, and X15214; 107F, M24446; 126K, L10053, D00346, M29095, AF204178, M24450, M24451, AF410348, AF410361, AF410362, AF410365, AF204177, and D10514; 226K, AB111452 and AY158337; 247R, AF231718, AF231719, and AF231720.
We were unable to detect any binding of the G106Q mutant to either of the anti-A1 (flavivirus group-reactive) MAbs (4G2 and 6B6C-1) (Table 3). Anti-A3 and -C1 reactive MAbs (DENV-2 type specific for DII and DI, respectively) exhibited reduced affinities for G106Q mutant-transfected cells and secreted VLPs. The dengue virus complex-specific MAb 10A1D-2 (epitope as yet unidentified) also exhibited a moderately reduced reactivity for the G106Q VLP antigen (Table 3). However, the reactivity of the G106Q mutant was unchanged from that of the wild-type pCB8D2-2J-2-9-1 antigen with polyclonal anti-DENV-2 MHIAF and subgroup cross-reactive MAb 1B7-5 (A5 epitope) as well as with MAbs recognizing the remaining subcomplex- and type-specific epitopes, i.e., A2, B1, B2, B3, B4, and C4 (Table 3 and data not shown).
The W231F substitution also appeared to abolish the binding of all three MAbs that recognized the flavivirus cross-reactive epitopes A1 and A5 (Table 3). This substitution additionally interfered with binding of the type-specific anti-C1 MAb 1B4C-2, but binding of the remaining subcomplex- and type-specific DI, DII, and DIII MAbs and of a polyclonal DENV-2 MHIAF was unchanged (Table 3). In three separate experiments, we were unable to detect any VLP secretion of the W231F mutant antigen into the tissue culture medium from transiently transfected COS-1 or CHO cells. We were therefore only able to analyze the effects of this substitution by an IFA of plasmid-transfected cells. The H244R and K247R substitutions did not have any effect on the binding of any MAbs in either IFAs with transfected cells or Ag-ELISAs with the secreted VLP antigen (data not shown).
Amino acids Lys64, Thr76, Gln77, Gly104, Leu107, Glu126, and Thr226.
With the identification of the cross-reactive epitope residues G106 and W231, we returned to the E-glycoprotein atomic structure to search for additional flavivirus cross-reactive epitope residues. The nearest neighbor search described in Materials and Methods yielded another seven potential epitope residues. Amino acid substitutions at these positions were modeled into the TBEV E-protein structure as previously described, and mutagenic PCR primers were synthesized (Table 1) and used to introduce mutations into the wild-type DENV-2 prM/E expression plasmid. Plasmids were transiently transfected into CHO cells, and transfected cells and secreted VLP antigen were analyzed with the MAb panel (Table 3). The substitutions introduced at these positions were as follows: Lys64 to Asn (K64N), Thr76 to Met (T76M), Gln77 to Arg (Q77R), Gly104 to His (G104H), Leu107 to Lys (L107K), Glu126 to Ala (E126A), and Thr226 to Asn (T226N) (Table 2). We also examined a double mutant with combined substitutions at positions 126 and 226 (E126A/T226N). Since the initial W231F substitution interfered with antigen secretion, we also examined the effects of an alternative substitution, Trp231 to Leu (W231L), at this position.
The G104H, L107K, and W231L substitutions had the largest effects on the reactivities of the flavivirus cross-reactive anti-A1 and -A5 MAbs (Table 3). Gly104 is located on the upper surface of the dimer at the tip of the tight loop structure which the fusion peptide adopts in the E-glycoprotein dimer (40) (Fig. 2). The residue has a moderately high surface accessibility and a relatively high temperature (β) factor. We modeled the replacement of this small aliphatic glycine with a large polar histidine at this position. The histidine residue fit well into this pocket and was predicted not to alter the hydrogen bond network in the region. Moreover, because the tick-borne flaviviruses have a histidine at this position (Table 4), it seemed probable that this substitution would not disrupt the structure in this localized region or elsewhere within DII. In fact, a posteriori stability calculations based upon the DENV-2 E-glycoprotein atomic structure (40) indicated that the G104H substitution is energetically favorable (Table 2). Leu107 sits directly below Gly106 on the outer lateral surface of the E-glycoprotein dimer. This residue has relatively high surface accessibility and temperature (β) factors, and its hydrophobic side chain is directed laterally away from the dimer. This residue is also strongly conserved among the flaviviruses, with the exceptions being the tick-borne deer tick and Powassan viruses, JEV strain SA-14-14-2, and DENV-2 strain PUO-280 (Table 4). All of these viruses have a phenylalanine instead of a leucine at this position. We substituted a large basic lysine residue for the leucine at this position. Modeling of this L107K substitution indicated that it, too, was unlikely to alter the localized hydrogen bonding network. This observation and the low thermodynamic free energy (ddG) stability calculation (Table 2) suggested that this substitution was unlikely to induce localized or domain-associated conformational changes.
The G104H substitution, like both substitutions examined at Trp231, produced a plasmid which was unable to secrete measurable VLP antigen into the tissue culture medium upon transfection into either COS-1 or CHO cells. We were therefore only able to analyze the G104H and W231L mutants by IFAs with transiently transfected cells as described above for the W231F mutant. The G104H substitution eliminated the reactivities of all of the anti-A1 and -A5 reactive MAbs (Table 3). The type-specific anti-A3 MAb 1A5D-1 also showed a strongly reduced reactivity for cells that were transiently transfected with this plasmid (Table 3). The W231L mutant, not surprisingly, showed reductions in MAb reactivities that were very similar to those of the W231F mutant, knocking out any discernible recognition of both anti-A1 and anti-A5 MAbs (Table 3). The reactivity of an anti-C1 MAb was also reduced by this mutation, but there were no discernible changes in the reactivities of the remaining subcomplex- and type-specific MAbs or of the anti-DENV-2 MHIAF for either the G104H or W231L plasmid construct (Table 3).
The L107K substitution exhibited a pattern of reduced reactivities for flavivirus cross-reactive MAbs that was unlike that of any of the other substitutions. The anti-A1 MAb 4G2 showed no discernible reactivity for this construct in either an IFA with plasmid-transfected cells or an Ag-ELISA with secreted VLP antigen. However, the reactivities of the other anti-A1 MAb, 6B6C-1, and of the anti-A5 1B7-5 MAb were unchanged for this antigen relative to those for the nonmutated wild-type antigen (Table 3). L107K plasmid-transfected cells and secreted VLP antigen also showed moderately reduced reactivities for anti-A3 and -C1 MAbs as well as for MAb 10A1D-2, whose epitope identity is still undefined (Table 3). All other MAb reactivities and the polyclonal MHIAF reactivity were not significantly different from those for the wild-type antigen (Table 3).
Unlike Leu107, Glu126 appears to be incorporated into epitopes that are recognized by the anti-A1 MAb 6B6C-1 and the anti-A5 MAb 1B7-5, but this residue is not incorporated into the epitope of the flavivirus group-reactive anti-A1 MAb 4G2. Glu126 is located 10 to 12 Å from Trp231 in the same trough on the upper and outer surfaces of DII (Fig. 2). The bulky side chain projects from the α-carbon backbone up into this trough, producing a moderately high surface accessibility and a high β-factor. We modeled the replacement of this large negatively charged acidic glutamine with a small hydrophobic alanine at this position. This substitution was predicted to induce a moderately high but acceptable energetic folding cost by our free energy stability analysis based on the TBEV E-glycoprotein structure coordinates (in TBEV, the residue is Lys126) (Table 2).
The E126A substitution reduced the reactivity of the group-reactive anti-A1 MAb 6B6C-1 and moderately reduced the reactivity of the anti-A5 reactive MAb 1B7-5 (Table 3). However, the anti-A1 MAb 6B6C-1 exhibited a reduced reactivity only by IFA with mutant plasmid-transfected cells, and 1B7-5 only showed reactivity reductions for this construct by Ag-ELISA (Table 3). Similarly, the type-specific anti-A3 MAb exhibited a moderately reduced reactivity for the E126A mutant by Ag-ELISA, but there was no detectable reduction in its reactivity by IFA (Table 3). Since the single T226N substitution did not alter the reactivity of any of our cross-reactive MAbs relative to that for the nonmutated wild-type plasmid (data not shown), it was not surprising that the E126A/T226N double mutant antigen exhibited a pattern of reduction in MAb reactivities that was similar to that of the E126A substitution. The two exceptions to this similarity were the reactivities of the anti-A5 and 10A1D-2 MAbs. The E126A/T226N mutant exhibited the same moderate 87% reduction in Ag-ELISA reactivity with the anti-A5 MAb 1B7-5 as that for the E126A mutant. However, the double mutant additionally exhibited a strong 97% reduction in reactivity with this same MAb by IFA which was not observed for either single mutant (Table 3). The DENV complex-specific MAb 10A1D-2 also exhibited moderate reactivity decreases by IFA for this double mutant (Table 3). The K64N, T76M, and Q77R mutants were all unchanged in their reactivities with the flavivirus cross-reactive MAbs (data not shown). The T76M VLP antigen did, however, show reduced reactivities for the anti-A3 and -C1 MAbs by Ag-ELISA (Table 3).
DISCUSSION
Flavivirus group-reactive epitope A1.
The six residues identified as participating in the flavivirus cross-reactive epitopes are spatially arranged on the DENV-2 E-glycoprotein surface in two clusters (Fig. 1). The most prominent grouping of these residues is the clustering of three A1 epitope residues in the highly conserved fusion peptide region of DII (4). These residues, Gly104, Gly106, and Leu107, are almost completely conserved among the flaviviruses (Table 4). The A1 epitope is located in structural DII and is flavivirus group reactive, highly surface accessible, reduction-denaturation sensitive, and involved in virus neutralization and virus-mediated cell membrane fusion (46). Tryptic fragment mapping with MAbs suggested that this epitope is formed from two discontinuous E-glycoprotein peptide fragments consisting of aa 1 to 120 and 158 to 142 (1, 28, 39, 46).
We identified substitutions at four amino acid positions, Gly104, Gly106, Leu107, and Trp231, that significantly reduced or eliminated the ability of anti-A1 MAbs to bind to the DENV-2 E glycoprotein (Table 3). The first three of these residues are located within the highly conserved hydrophobic fusion peptide region of DII (Fig. 1 and 2). The fusion peptide is located at the end of the extended finger-like structure of DII in the E-glycoprotein monomer (40). In the native dimer structure the tightly folded fusion peptide loop at the tip of one monomer is packed against the other subunit near the DI-DIII interface (Fig. 1 and 2). This close packing of the fusion peptide against its subunit partner and the glycan on the upper surface at DI residue Asn153 are believed to protect the fusion peptide from irreversible pH-induced conformational changes during maturation and secretion.
The cross-reactive MAbs that were most strongly consistently affected by substitutions in this region were 4G2 and 6B6C-1. These two MAbs are considered to be quite similar; both are flavivirus group reactive and have been grouped into the A1 epitope of the E glycoprotein (20, 28, 38, 46). We demonstrated here that although the epitopes of these two MAbs overlap spatially, they do not contain exactly the same residues. A substitution at Gly104, Gly106, or Leu107 knocked out the ability of MAb 4G2 to bind to the E glycoprotein. However, only substitutions at Gly104 and Gly106 interfered with the binding ability of MAb 6B6C-1. Leu107 is therefore not a component of the flavivirus group-reactive epitope that is recognized by MAb 6B6C-1 (Fig. 2).
The G104H substitution dramatically reduced the reactivities of all three of our flavivirus cross-reactive MAbs for this antigen (Table 3). It is unlikely that a glycine residue, with no side chain, would directly participate in the binding energetics of an antibody-antigen (Ab-Ag) interaction. However, if a glycine residue were included in the buried surface area of this antibody epitope, the introduction of a large bulky hydrophobic side chain would likely disrupt the Ab-Ag shape complementarity and hence increase the dissociation rate constant (Kd) of the Ab-Ag interaction (35). In fact, a preliminary kinetic analysis of the G106Q antigen and MAb 4G2 indicated that an increased Kd was responsible for the affinity reductions of this Ab-Ag interaction. The G104H mutant also reduced the recognition of the type-specific anti-A3 MAb 1A5D-1 (Table 3). The A3 epitope is nonneutralizing, reduction sensitive, and moderately surface accessible (46). All of the fusion peptide substitutions that we introduced into this region reduced the reactivity of this A3 reactive MAb, consistent with the interpretation that the buried surface area footprint of this MAb not only includes DENV-2 serotype-specific residues, but also includes these strongly conserved residues. A comparison of the DENV-2 atomic structure with flavivirus E-glycoprotein alignments identified at least two unique DII surface-accessible residues (Glu71 and Asn83) and a third residue that is variable within DENV-2 but distinct from the other DENV serotypes (Thr81). All of these residues are within 10 to 22 Å of Gly104, a distance well within the buried surface area of a typical Ab-Ag interface (37). Alternatively, less surface-accessible type-specific residues nearby may participate in MAb 1A5D-1 binding since this epitope itself is only moderately surface accessible (46). Since this MAb is DENV-2 specific, these type-specific residues would be expected to provide the majority of the binding energy for this epitope.
The G106Q substitution also knocked out all discernible reactivities for both anti-A1 reactive MAbs, 4G2 and 6B6C-1, although it did not affect the binding of the anti-A5 reactive MAb 1B7-5 (Table 3; Fig. 2). Type-specific anti-A3 and -C1 reactive MAbs lost all measurable reactivity to the G106Q construct. The A3 epitope footprint appears to include conserved fusion peptide residues in addition to DENV-2 serotype-specific residues as discussed above. The reduced reactivity of the C1 reactive MAb for the G106Q construct is difficult to explain. Because of the lack of biological activity of DI (C epitopes), epitope assignments in this domain can be problematic (46). The apparent incorporation of Gly106 and Leu107 (see below) into this C1 epitope is consistent with the possibility that either the previous DI assignment was incorrect or the C1 epitope includes residues from both DI and DII. However, if this anti-C1 reactive MAb recognized such an interdomain epitope, then this high-affinity MAb would be expected to interfere with the E-glycoprotein dimer-to-trimer reorganization (2) that occurs during virus-mediated membrane fusion, which it does not.
Leu107 is the third residue that we identified in the fusion peptide region of DII that is incorporated into the A1 epitope. Unlike the substitutions at Gly104 and Gly106, the L107K substitution knocked out the reactivity of the anti-A1 reactive MAb 4G2, but it did not interfere with the reactivity of the other anti-A1 reactive MAb, 6B6C-1 (Table 3; Fig. 2). Beyond this major discrepancy, the reactivity patterns of the rest of the MAbs for this construct were similar to that observed for the other fusion peptide substitutions (Table 3).
Previous studies have examined the effects of mutagenesis in this fusion peptide region. Pletnev et al. (42) performed mutagenesis of fusion peptide residues 104 and 107 in a chimeric infectious clone containing the TBEV structural genes and DENV-4 nonstructural genes. TBEV has a histidine at position 104, as do all of the tick-borne flaviviruses (Table 4). Pletnev et al. constructed the opposite substitution from the one that we constructed, H104G, replacing the tick-associated histidine with the mosquito-associated glycine, but they were unable to recover live virus from this construct. They also constructed a H104G/L107F double mutant from which they were able to recover virus; however, they were unable to detect any effect of these mutations on mouse neurovirulence. Allison et al. (4) also performed mutagenesis at Leu107 to examine the role of this residue in virus-mediated membrane fusion by using TBEV VLPs. They replaced Leu107 with phenylalanine, threonine, or aspartic acid. They found that all of these mutations reduced the rate of fusion. Moreover, consistent with the results presented here, they found that the L107D substitution appeared to completely abolish the binding of their DII flavivirus group-reactive MAb, which was also assigned to the A1 epitope.
The fourth residue that we identified as having a major effect on the anti-A1 and -A5 reactive MAbs was Trp231, an invariant residue across the flaviviruses (Table 4). Both substitutions that we introduced at Trp231 dramatically reduced the reactivities of both anti-A1 MAbs and the anti-A5 MAb. This residue is structurally distant from the fusion peptide region (Fig. 1 and 2). It is somewhat surprising that substitutions at this residue affect the binding of MAbs that also recognize the distant fusion peptide residues. The strict conservation of tryptophan (Table 4) and the predicted high energetic costs of substitutions at this position (Table 2) suggest that this residue is important for proper DI-DII conformational structure and function. If this is the case, then the loss of reactivity of these mutants with MAbs recognizing fusion peptide residues may occur from the induction of localized structural disturbances across DII occurring at a distance from Trp231. However, the Trp231 substitutions did not significantly affect the binding of anti-A2 and -A3 epitopes or that of 10A1D-2, whereas anti-A2, -A3, and 10A1D-2 MAb reactivities were reduced or eliminated by all three of the fusion peptide substitutions. Anti-A2 MAbs do not recognize native virus, yet they block virus-mediated cell membrane fusion, presumably by recognizing an epitope that is exposed only during or after low-pH-catalyzed conformational changes (2, 46). If substitutions at Trp231 induced domain-wide structural alterations, we would expect a loss of reactivity for the anti-A3 reactive MAb 1A5D-1 and a possible exposure of the non-surface-accessible A2 epitope, resulting in an increase, or at least a change, in the reactivity of the anti-A2 reactive MAb 4E5 by IFA for these constructs. Moreover, the reactivities of polyclonal MHIAF and of all of our DIII MAbs (B epitopes) were no different for these constructs than they were for the nonmutated wild-type plasmid-transfected cells (Table 3). DIII, however, is reduction-denaturation stable and folds into its native IgC-like conformation even when it is expressed alone without the remainder of the E glycoprotein (6).
The apparent inclusion of Trp231 in these epitopes is therefore somewhat surprising. In the context of a single E-glycoprotein dimer, it appears that the location of Trp231 is too far removed from the identified fusion peptide residues to be bound by a single immunoglobulin molecule. There is a distance of approximately 35 to 45 Å from Trp231 to Gly104, Gly106, and Leu107 in the same dimer subunit and of 50 to 60 Å from Trp231 to these residues in the alternate dimer subunit. However, the distance from Trp231 in one dimer to Gly104, Gly106, and Leu107 in its nearest neighbor dimer on the viral E-glycoprotein lattice surface is only 25 to 30 Å, a distance that can be spanned by a single IgG molecule. Such a potential interdimer epitope would span a relatively large gap (10 to 15 Å) between the two dimers and would therefore probably require the incorporation of many close-packed water molecules to insure complementarity and to provide the typically observed polar interactions that occur between antibody paratopes and antigen epitopes (7, 37). The anti-A1 reactive MAb 4G2 has a high affinity, and if epitope A1 did in fact span across dimers and include Trp231, then we would expect that this MAb would also interfere with virus-mediated membrane fusion by disrupting the dimer-to-trimer E-glycoprotein reorganization (2). Unfortunately, it is not known if this MAb interferes with virus-mediated membrane fusion or not. The other anti-A1 reactive MAb, 6B6C-1, does interfere with fusion (46). Given the shared overlapping nature of the residues identified in these two A1 epitopes, it seems reasonable to assume that MAb 4G2, like 6B6C-1, does block virus-mediated membrane fusion. It is therefore possible that the fusion-blocking activity of 6B6C-1 and, by extension, that of 4G2 arise from their recognition of an interdimer epitope and thus their disruption of the dimer-to-trimer conformational change that is essential for initiating virus-mediated membrane fusion. Glu126 is a structural neighbor of Trp231 and is apparently incorporated into the anti-A1 reactive MAb 6B6C-1 epitope. Like W231, this residue might be incorporated in an interdimer epitope. However, since substitutions at this position only reduced 6B6C-1 binding by IFA and not by Ag-ELISA, it is possible that the apparent involvement of Glu126 in this epitope is an artifact, possibly resulting from a nonnative protein conformation in acetone-fixed cells in the IFA.
Flavivirus subgroup cross-reactive epitope A5.
The A5 epitope shares all of the physical and biochemical attributes of the A1 epitope, with the exception of it being flavivirus subgroup reactive instead of flavivirus group reactive (46). We identified at least three residues that appear to be involved in the A5 epitope, Gly104, Trp231, and Glu126, with the possible addition of Thr226. The high level of amino acid conservation at Gly104 and Trp231 (Table 4) and their participation in other flavivirus cross-reactive epitopes (discussed above) are consistent with the interpretation that these residues are incorporated into distinct yet overlapping cross-reactive epitopes.
We observed reductions in the reactivity of the anti-A5 reactive MAb 1B7-5 for the E126A/T226N double mutant by both IFA and Ag-ELISA, whereas the E126A mutant alone reduced the reactivity of this MAb to similar levels in Ag-ELISA, but not in IFA, and the T226N substitution had no effect on the reactivity of this MAb in either assay (Table 3). The larger decrease in the reactivity of 1B7-5 for the double mutant than for either single mutant is interesting. It is possible that the effects of substitutions at these two residues on anti-A5 MAb reactivity are additive or synergistic. Either the positions of these residues in the A5 epitope footprint or the nature of the specific substitutions that we introduced may disrupt the binding of the anti-A5 MAb to the observed magnitude only when they are present together, and the effect of either of these substitutions alone does not interfere as dramatically with anti-A5 MAb binding energetics.
W231F, W231L, and G104H plasmid-transfected cells failed to secrete measurable VLP antigen into the tissue culture medium. The inability of cells transfected with these plasmids to secrete VLP antigen into the tissue culture medium may have resulted from the disruption of a variety of protein maturation processes. Interference with particle maturation may have occurred via a disruption of E-prM/M intermolecular interactions or E-glycoprotein dimer interactions or via a disruption of dimer organization into the surface lattice covering the mature particles. Although the two processes are interdependent, these substitutions may not interfere with particle formation per se, but instead may directly interfere with particle secretion itself. The IFA staining pattern of DENV-2 G104H- and W231F/L-transfected cells was highly punctate and appeared to be localized within inclusion bodies (data not shown). We previously observed similar IFA staining patterns with nonsecreting constructs of dengue virus and other flaviviruses (11, 16, 29). Studies with TBEV VLPs have shown that interactions between prM and E are involved in the prM-mediated intracellular transport of prM-E heterodimers (3). The location of Gly104 near the interior lateral edge of DII puts it very close to the E-dimer “hole” where the prM/M proteins are located in the heterodimer (32) (Fig. 1). Therefore, it seems likely that the G104H mutant interferes with VLP secretion via disruption of the prM-E interactions that are necessary for intracellular transport and secretion. The mosquito-born flaviviruses have a glycine at this position, whereas the tick-borne flaviviruses have a histidine. Interestingly, Pletnev et al. (42) introduced the reverse substitution, H104G, into the TBEV E glycoprotein in a TBEV/DENV-4 chimeric infectious clone, and they were unable to recover virus from this mutant. The inability of G104H mutant-transfected cells to secrete VLP antigen similarly suggests that this too is a lethal substitution in DENV-2. Taken together, these two results are consistent with the idea that vector-specific selection has produced strong epistasis between this residue and another unidentified residue(s) elsewhere in the E or prM/M glycoprotein.
Flavivirus infections elicit virus species-specific as well as flavivirus group cross-reactive immune responses. Preexisting antibodies to flaviviruses that are detectable by in vitro neutralization tests can protect laboratory animals from a challenge with a second, closely related flavivirus, reducing morbidity and mortality in the animals (21, 43, 51). Dengue viruses consist of four antigenically related viruses. This concept of cross-reactive immune protection was hypothesized to explain the absence of dengue hemorrhagic fever/dengue shock syndrome (DHF/DSS) cases during a DENV-2 outbreak among Peruvians who were previously infected with DENV-1 (31). However, Sabin (48) previously demonstrated that volunteers challenged with a secondary DENV serotype were fully cross-protected for only 2 months, partially protected for up to 9 months after the initial infection, and showed no protection thereafter. In contrast to this potential protective role of cross-reactive antibodies, their paradoxical role in the antibody-dependent enhancement (ADE) of secondary DENV infections, resulting in DHF/DSS, has been suggested by many prospective, population-based, cohort, and clinical studies (26, 27).
Current concepts of DENV vaccine development have focused on developing and deploying tetravalent live attenuated or chimeric attenuated vaccines in a single application. This approach theorizes that an effective tetravalent vaccine can provide long-lasting immunity against any future DENV serotype infection, thus decreasing the probability of ADE in areas where DENV is endemic. However, there are potential problems when immunogens are introduced simultaneously, as in the administration of a multivalent DENV vaccine. Although immunological interference has not been very apparent in laboratory animals, the suppression of an antibody response to one or more immunogens and/or unbalanced antibody responses have been found more frequently in humans, even when immunogen doses were adjusted in an attempt to equalize humoral immune responses (12, 25, 30, 47).
We have constructed eukaryotic expression plasmids that express DENV-1, −2, −3, and −4 prM/M and E glycoproteins in the form of VLPs (11; D. Holmes, D. Purdy, and G.-J. Chang, unpublished results). The identification and initial characterization of residues that are incorporated into flavivirus cross-reactive epitopes A1 and A5 and the reduction of MAb recognition of these cross-reactive E-glycoprotein epitopes create an opportunity to investigate and understand the mechanistic basis and pathogenic ramifications of ADE. We hypothesize that the flavivirus group- and subgroup-reactive epitopes A1 and A5 and probable additional shared-antigen epitopes induce flavivirus cross-reactive antibodies that may cause ADE and increase the risk of developing DHF/DSS. We are continuing this structure-based rational mutagenesis approach to identify additional cross-reactive epitopes in the DENV-2 E glycoprotein, extending this epitope mapping to the other DENV serotypes and generalizing this epitope mapping approach to the encephalitic flaviviruses by using St. Louis encephalitis virus as a model. The E glycoproteins expressed by mutated plasmids in these VLPs with reduced cross-reactivities maintained an overall wild-type antigenic structure. Most importantly, many critical type-specific neutralizing antibody binding sites remained unaltered. Mutated plasmid DNAs and/or expressed VLPs will be used to immunize outbred mice and to assess their ability to stimulate type-specific neutralizing antibodies. These VLP antigens with reduced cross-reactivities will then be investigated for their effectiveness as DENV serotype-specific serodiagnostic reagents. Moreover, these immunogens, whether prM/E expression plasmids, VLP antigens, or live attenuated chimeric viruses, will provide both the theoretical foundation and the microbiological tools that are necessary for investigating and developing safer DENV candidate vaccines.
Acknowledgments
We thank Brent Davis and David Purdy for technical assistance and John Roehrig for critical comments on the manuscript.
This work was supported in part by the appointment of W.D.C. to the visiting fellowship program administered and funded by the Centers for Disease Control and Prevention.
REFERENCES
- 1.Aaskov, J. G., H. M. Geysen, and T. J. Mason. 1989. Serologically defined linear epitopes in the envelope protein of DEN 2 (Jamaica strain 1409). Arch. Virol. 105:209-221. [DOI] [PubMed] [Google Scholar]
- 2.Allison, S. L., J. Schalich, K. Staisny, C. W. Mandl, C. Kunz, and F. X. Heinz. 1995. Oligomeric rearrangement of tick-borne encephalitis virus envelope proteins induced by an acidic pH. J. Virol. 69:695-700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Allison, S. L., K. Staisny, K. Stadler, C. W. Mandl, C. Kunz, and F. X. Heinz. 1999. Mapping of functional elements in the stem-anchor region of tick-borne encephalitis virus envelope protein E. J. Virol. 73:5605-5612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Allison, S. L., J. Schalich, K. Staisny, C. W. Mandl, and F. X. Heinz. 2001. Mutational evidence for an internal fusion peptide in the flavivirus envelope protein. J. Virol. 75:4268-4275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Arevalo, J. H., M. J. Taussig, and I. A. Wilson. 1993. Molecular basis of cross-reactivity and the limits of antibody-antigen complementarity. Nature 356:859-863. [DOI] [PubMed] [Google Scholar]
- 6.Bhardwaj, S., M. Holbrook, R. E. Shope, A. D. T. Barrett, and S. J. Watowich. 2001. Biophysical characterization and vector-specific antagonist activity of domain III of the tick-borne flavivirus envelope protein. J. Virol. 75:4002-4007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bhat, T. N., G. A. Bentley, G. Boulot, M. I. Greene, D. Tello, W. Dall'Acqua, H. Souchon, F. P. Schwarz, R. A. Mariuzza, and R. J. Poljak. 1994. Bound water molecules and conformational stabilization help mediate an antigen-antibody association. Proc. Natl. Acad. Sci. USA 91:1089-1093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Burke, D. S., and T. P. Monath. 2001. Flaviviruses, p. 1043-1125. In D. M. Knipe et al. (ed.), Fields virology, 4th ed. Lippincott Williams & Wilkins, Philadelphia, Pa.
- 9.Calisher, C. H., N. Karabatsos, J. M. Dalrymple, R. E. Shope, J. S. Porterfied, E. G. Westaway, and W. E. Brandt. 1989. Antigenic relationships between flaviviruses as determined by cross-neutralization tests with polyclonal antisera. J. Gen. Virol. 70:37-43. [DOI] [PubMed] [Google Scholar]
- 10.Chang, G. J., A. R. Hunt, and B. S. Davis. 2000. A single intramuscular injection of recombinant plasmid DNA induces protective immunity and prevents Japanese encephalitis in mice. J. Virol. 74:4244-4252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chang, G. J., A. R. Hunt, D. A. Holmes, T. Springfield, T. Chiueh, J. T. Roehrig, and D. J. Gubler. 2003. Enhancing biosynthesis and secretion of premembrane and envelope proteins by the chimeric plasmid of DEN virus type 2 and Japanese encephalitis virus. Virology 306:170-180. [DOI] [PubMed] [Google Scholar]
- 12.Chang, G. J., G. Kuno, D. E. Purdy, and B. S. Davis. 2004. Recent advancement in flavivirus vaccine development. Exp. Rev. Vaccines 3:199-220. [DOI] [PubMed] [Google Scholar]
- 13.Chevillon, C., and A. Failloux. 2003. Questions on viral population biology to complete DEN puzzle. Trends Microbiol. 11:415-421. [DOI] [PubMed] [Google Scholar]
- 14.Crill, W. D., and J. T. Roehrig. 2001. Monoclonal antibodies that bind to domain III of DEN virus E glycoprotein are the most efficient blockers of virus adsorption to Vero cells. J. Virol. 75:7769-7773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Davies, D. R., and G. H. Cohen. 1996. Interactions of protein antigens with antibodies. Proc. Natl. Acad. Sci. USA 93:7-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Davis, B. S., G. J. Chang, B. Cropp, J. T. Roehrig, D. A. Martin, C. J. Mitchell, R. Bowen, and M. L. Bunning. 2001. West Nile recombinant DNA vaccine protects mouse and horse from virus challenge and expresses in vitro a noninfectious recombinant antigen that can be used in enzyme-linked immunosorbent assays. J. Virol. 75:4040-4047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Faebler, K., D. Kirchhofer, L. Presta, R. F. Kelley, and Y. A. Muller. 2001. The 1.85 Å resolution crystal structures of tissue factor in complex with humanized Fab D3h44 and of free humanized Fab D3h44: revisiting the salvation of antigen combining sites. J. Mol. Biol. 313:83-97. [DOI] [PubMed] [Google Scholar]
- 18.Ferguson, N., R. Anderson, and S. Gupta. 1999. The effect of antibody-dependent enhancement on the transmission dynamics and persistence of multiple-strain pathogens. Proc. Natl. Acad. Sci. USA 96:790-794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fleury, D., B. Barrere, T. Bizebard, R. S. Daniels, J. J. Skehel, and M. Knossow. 1999. A complex of influenza hemagglutinin with a neutralizing antibody that binds outside the virus receptor binding site. Nat. Struct. Biol. 6:530-534. [DOI] [PubMed] [Google Scholar]
- 20.Gentry, M. K., E. A. Henchal, J. M. McCown, W. E. Brandt, and J. M. Dalrymple. 1982. Identification of distinct antigenic determinants on DEN-2 virus using monoclonal antibodies. Am. J. Trop. Med. Hyg. 31:548-555. [DOI] [PubMed] [Google Scholar]
- 21.Goverdhan, M. K., A. B. Kulkarni, A. K. Gupta, C. D. Tupe, and J. J. Rodrigues. 1992. Two-way cross protection between West Nile and Japanese encephalitis viruses in bonnet macaques. Acta Virol. 36:277-283. [PubMed] [Google Scholar]
- 22.Gubler, D. J. 2002. Epidemic DEN/DEN hemorrhagic fever as a public health, social, and economic problem in the 21st century. Trends Microbiol. 10:100-103. [DOI] [PubMed] [Google Scholar]
- 23.Guerois, R., J. E. Nielsen, and L. Serrano. 2002. Predicting changes in the stability of proteins and protein complexes: a study of more than 1000 mutations. J. Mol. Biol. 320:369-387. [DOI] [PubMed] [Google Scholar]
- 24.Guex, N., and M. C. Peitsch. 1997. SWISS-MODEL and the Swiss-PdbViewer: an environment for comparative protein modeling. Electrophoresis 18:2714-2723. [DOI] [PubMed] [Google Scholar]
- 25.Guirakhoo, F., K. Pugachev, J. Arroyo, C. Miller, Z. X. Zhang, R. Weltzin, K. Georgakopoulos, J. Catalan, S. Ocran, K. Draper, and T. P. Monath. 2002. Viremia and immunogenicity in non-human primates of tetravalent yellow fever-dengue chimeric vaccine: genetic reconstructions, dose adjustment, and antibody response against wild-type dengue virus isolates. Virology 298:146-159. [DOI] [PubMed] [Google Scholar]
- 26.Halstead, S. B. 1988. Pathogenesis of dengue: challenges to molecular biology. Science 239:476-481. [DOI] [PubMed] [Google Scholar]
- 27.Halstead, S. B. 1989. Antibody, macrophages, dengue virus infection, shock and hemorrhage: a pathogenic cascade. Rev. Infect. Dis. 11:830-839. [DOI] [PubMed] [Google Scholar]
- 28.Henchal, E. A., J. M. McCown, D. S. Burke, M. C. Seguin, and W. E. Brandt. 1985. Epitopic analysis of antigenic determinants on the surface of DEN-2 virions using monoclonal antibodies. Am. J. Trop. Med. Hyg. 34:162-169. [DOI] [PubMed] [Google Scholar]
- 29.Hunt, A. R., C. B. Cropp, and G. J. Chang. 2001. A recombinant particulate antigen of Japanese encephalitis virus produced in stably transformed cells is an effective noninfectious antigen and subunit immunogen. J. Virol. Methods 97:133-149. [DOI] [PubMed] [Google Scholar]
- 30.Kanesa-thasan, N., W. Sun, G. Kim-Ahn, S. Van Albert, J. R. Putnak, A. King, B. Raengsakulsrach, H. Christ-Schmidt, K. Gilson, J. M. Zahradnik, D. W. Vaughn, B. L. Innis, J. Saluzzo, and C. H. Hohe. 2001. Safety and immunogenicity of attenuated dengue virus vaccines (Aventis Pasteur) in human volunteers. Vaccine 19:3179-3188. [DOI] [PubMed] [Google Scholar]
- 31.Kochel, T. J., D. M. Watts, S. B. Halstead, C. G. Hayes, A. Espinoza, V. Felices, R. Caceda, C. T. Bautista, Y. Montoya, S. Douglas, and K. L. Russell. 2002. Effect of dengue-1 antibodies on American dengue-2 viral infection and haemorrhagic fever. Lancet 360:310-312. [DOI] [PubMed] [Google Scholar]
- 32.Kuhn, R. J., W. Zhang, M. G. Rossmann, S. V. Pletnev, J. Corver, E. Lenches, C. T. Jones, S. Mukhopadhyay, P. R. Chipman, E. G. Strauss, T. S. Baker, and J. H. Strauss. 2002. Structure of DEN virus: implications for flavivirus organization, maturation, and fusion. Cell 108:717-725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kuno, G., G.-J. J. Chang, K. R. Tsuchiya, N. Karabatsos, and C. B. Cropp. 1998. Phylogeny of the genus Flavivirus. J. Virol. 72:73-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Li, Y., H. Li, S. J. Smith-Gill, and R. A. Mariuzza. 2000. Three-dimensional structures of the free and antigen-bound Fab from monoclonal antilysozyme antibody HyHEL-63. Biochemistry 39:6296-6309. [DOI] [PubMed] [Google Scholar]
- 35.Li, Y., H. Li, F. Yang, S. J. Smith-Gill, and R. A. Mariuzza. 2003. X-ray snapshots of the maturation of an antibody response to a protein antigen. Nat. Struct. Biol. 10:482-488. [DOI] [PubMed] [Google Scholar]
- 36.Lindenbach, B. D., and C. M. Rice. 2001. Flaviviridae: the viruses and their replication, p. 991-1041. In D. M. Knipe et al. (ed.), Fields virology, 4th ed. Lippincott Williams & Wilkins, Philadelphia, Pa.
- 37.Lo Conte, L., C. Chothia, and J. Janin. 1999. The atomic structure of protein-protein recognition sites. J. Mol. Biol. 285:2177-2198. [DOI] [PubMed] [Google Scholar]
- 38.Mandl, C. W., F. Guirakhoo, H. Holzmann, F. X. Heinz, and C. Kunz. 1989. Antigenic structure of the flavivirus envelope protein E at the molecular level, using tick-borne encephalitis virus as a model. J. Virol. 63:564-571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Megret, F., J. P. Hugnot, A. Falconar, M. K. Gentry, D. M. Morens, J. M. Murray, J. J. Schlesinger, P. J. Wright, P. Young, M. H. V. Van Regenmortel, and V. Deubel. 1992. Use of recombinant fusion proteins and monoclonal antibodies to define linear and discontinuous antigenic sites on the DEN virus envelope glycoprotein. Virology 187:480-491. [DOI] [PubMed] [Google Scholar]
- 40.Modis, Y., S. Ogata, D. Clements, and S. C. Harrison. 2003. A ligand-binding pocket in the DEN virus envelope glycoprotein. Proc. Natl. Acad. Sci. USA 100:6986-6991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mylvaganam, S. E., Y. Paterson, and E. D. Getzoff. 1998. Structural basis for the binding of an anti-cytochrome c antibody to its antigen: crystal structures of FabE8-cytochrome c complex to 1.8 Å resolution and FabE8 to 2.26 Å resolution. J. Mol. Biol. 281:301-322. [DOI] [PubMed] [Google Scholar]
- 42.Pletnev, A. G., M. Bray, and C. Lai. 1993. Chimeric tick-borne encephalitis and DEN type 4 viruses: effects of mutations on neurovirulence in mice. J. Virol. 67:4956-4963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Price, W. H., and I. S. Thind. 1971. Protection against West Nile virus induced by a previous injection with dengue virus. Am. J. Epidemiol. 94:596-607. [DOI] [PubMed] [Google Scholar]
- 44.Rey, F. A., F. X. Heinz, C. Mandl, K. Kunz, and S. C. Harrison. 1995. The envelope glycoprotein from tick-borne encephalitis virus at 2Å resolution. Nature 375:291-298. [DOI] [PubMed] [Google Scholar]
- 45.Rice, C. M., E. M. Lenches, S. R. Eddy, S. J. Shin, R. L. Sheets, and J. H. Strauss. 1985. Nucleotide sequence of yellow fever virus: implications for flavivirus gene expression and evolution. Science 229:726-733. [DOI] [PubMed] [Google Scholar]
- 46.Roehrig, J. T., R. A. Bolin, and R. G. Kelly. 1998. Monoclonal antibody mapping of the envelope glycoprotein of the DEN 2 virus, Jamaica. Virology 246:317-328. [DOI] [PubMed] [Google Scholar]
- 47.Sabchareon, A., J. Lang, P. Chanthavanich, S. Yoksan, R. Forrat, P. Attanath, C. Sirivichayakul, K. Pengsaa, C. Pojjaroen-Anant, W. Chokejindachai, A. Jagsudee, J. F. Saluzzo, and N. Bhamarapravati. 2002. Safety and immunogenicity of tetravalent live-attenuated dengue vaccines in Thai adult volunteers: role of serotype concentration, ratio, and multiple doses. Am. J. Trop. Med. Hyg. 66:264-272. [DOI] [PubMed] [Google Scholar]
- 48.Sabin, A. B. 1952. Research on dengue during World War II. Am. J. Trop. Med. Hyg. 1:30-50. [DOI] [PubMed] [Google Scholar]
- 49.Solomon, T., and M. Mallewa. 2001. DEN and other emerging flaviviruses. J. Infect. 42:104-115. [DOI] [PubMed] [Google Scholar]
- 50.Takada, A., and Y. Kawaoka. 2003. Antibody-dependent enhancement of viral infection: molecular mechanisms and in vivo implications. Rev. Med. Virol. 13:387-398. [DOI] [PubMed] [Google Scholar]
- 51.Tesh, R. B., P. A. A. Travassos de Rosa, H. Guzman, T. P. Araujo, and S.-Y. Xiao. 2002. Immunization with heterologous flaviviruses protective against fatal West Nile encephalitis. Emerg. Infect. Dis. 8:245-251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Wallace, M. J., D. W. Smith, A. K. Broom, J. S. Mackenzie, R. A. Hall, G. R. Shellam, and P. C. McMinn. 2003. Antibody-dependent enhancement of Murray Valley encephalitis virus virulence in mice. J. Gen. Virol. 84:1723-1728. [DOI] [PubMed] [Google Scholar]
- 53.World Health Organization. 2002. DEN and DEN hemorrhagic fever. Fact sheet no. 117. World Health Organization, Geneva, Switzerland.