Abstract
Background
Few publications have dealt exclusively with the use of flow diverter stents for the treatment of aneurysms of the anterior cerebral artery (ACA).
Objective
To determine the efficacy of flow-diverting stents in the treatment of small, unruptured aneurysms of the ACA.
Methods
We retrospectively reviewed our database of prospectively collected information for all patients treated with flow diversion for an unruptured saccular aneurysm of the ACA between September 2009 and July 2016. The aneurysm fundus size, neck size, number and type of flow-diverting stent (FDS), complications, and follow-up data were recorded.
Results
In total 26 patients, with 27 aneurysms were identified that matched our inclusion criteria (11 male and 15 female). The average age of the patients was 59.3 years (range 27–77 years). All patients, except one, had a single aneurysm affecting the ACA. Fourteen aneurysms were located on the left (51.9%). The average aneurysm fundus size was 2.9 mm (range 2–6 mm). Twenty patients had follow-up angiographic studies. In total, 16 aneurysms were completely excluded, 1 aneurysm showed a very small remnant, and no follow-up angiographic data are available for the remaining patients. One patient had a treatment-related complication.
Conclusions
Treatment of aneurysms arising from the ACA with flow diverters is technically feasible and carries a high degree of success with low complication rate.
Keywords: Aneurysm, Stent
Introduction
The introduction of flow-diverting technology represented a monumental advancement in our ability to exclude aneurysms from the circulation and also to reconstruct the parent vessel. These new stents were originally tested in previously untreatable aneurysms or those in which previous endovascular treatments had failed.1 The mechanism of action of aneurysm exclusion is slowly being elucidated and probably involves reduced intra-aneurysmal flow, stasis, and thrombosis, with neo-endothelialization of the stent to finally reconstruct the parent vessel.2 This process occurs slowly and usually spares covered perforator branches, such as the anterior choroidal artery or the lenticulostriate arteries.3–5 These devices have an increased metal coverage compared with conventional stents with an optimal porosity of between 60% and 76% according to some studies.6 7
A variety of different flow-diverting stents (FDS) are available, including the Pipeline Embolization Device (PED; Covidien, Irvine, California), Silk (Balt Extrusion, Montmercy, France), Surpass (Stryker Neurovascular, Fremont, California), p64 (phenox, Bochum, Germany), and the Flow Re-direction Endoluminal Device (FRED; Microvention, Tustin, California). Newer derivations of these devices, such as the Pipeline FLEX have also entered the market and offer added advantages such as near complete resheathability.
The PED is one of the most widely studied devices and is made of 25% platinum and 75% nickel–cobalt chromium alloy with a porosity of 65–70%. It is available in a variety of different sizes and diameters and multiple telescoped PEDs can be used to alter the porosity.8 The Pipeline for Uncoilable or Failed aneurysms Study (PUFS)1 showed an aneurysm occlusion rate of 73.6% at 6 months and major ipsilateral stroke or neurological death rate of 5.5%, whereas the PED for the Intracranial Treatment of Aneurysms (PITA) showed a 6 months’ aneurysm occlusion rate of 93.3% and ischemic stroke risk of 6.5%.8 More recently, Griessenauer et al9 published their multicenter results on the use of the PED for small (≤7 mm) aneurysms and showed a complete occlusion rate of 87% and symptomatic procedural complication rate of 6%.
The Silk flow diverter has a porosity of 45–60% and can be resheathed even up to 90% deployment. The Silk is made up of 48 braided nitinol strands and was the first device to enter clinical use for the treatment of intracranial pathologies. In the recent systematic review performed by Murthy et al10 a 12 months’ aneurysm occlusion rate of 81.8% was seen with ischemic complications occurring in 10% of patients and a cumulative mortality of 4.9%. Similarly, the recently published results of a Canadian registry showed that 83.1% of aneurysms treated with the Silk flow diverter were either completely or nearly completely occluded at last follow-up with a perioperative morbidity of 8.7% and mortality of 2.2%.11
The Surpass flow diverter employs a different design in order to maintain pore density at close to 70% across different device diameters. The device has a varying number of metal struts, increasing in number from 48 (2 mm diameter devices) to 96 (5 mm diameter devices) at larger diameters. It is made of a cobalt–chromium alloy and contains 12 platinum wires to aid radio-opacity. Wakhloo et al12 recently reported the preliminary angiographic and clinical results from a multicenter study. They showed complete occlusion in 75% of patients who had follow-up angiography (158 of 186 aneurysms). Ischemic stroke was seen in 3.7% of patients in ≤30 days with intra-parenchymal hemorrhage and subarachnoid hemorrhage (≤7 days) seen in 2.5% and a mortality of 1.6% for aneurysms in the anterior circulation.
The FRED flow diverter has a unique dual layer design that consists of a low porosity inner mesh and higher porosity outer mesh. The device is composed of 48 braided nitinol inner strands and 16 outer struts with 4 interwoven marker strands as well as proximal and distal markers. The dual layer is restricted to the mid-section and covers approximately 80% of the device length with the aim of increasing coverage across the aneurysmal neck. Kocer et al13 published their initial experience of the FRED flow diverter and showed progressive occlusion of aneurysms up to 12 months with low rates of morbidity and mortality. Similarly, Möhlenbruch et al14 showed progressive aneurysmal occlusion with 73% of aneurysms completely occluded at the 6 months’ follow-up while Briganti et al15 had occlusion rates of 83%. The safety profile also seems comparable to the other devices with no deaths seen in the studies and morbidity seen in 10% of cases in the series by Möhlenbruch and 8% in that of Briganti et al.15
The p64 is a braided FDS composed of 64 nitinol wires. Two platinum wires wrapped around the shaft assist in radio-opacity. The 64 wires are grouped into eight bundles proximally, with each bundle consisting of eight wires. A radio-opaque marker is attached to end of each of these bundles. The porosity of the device is 51–60%. The p64 is unique among flow diverters in that it is mechanically detached and can be resheathed even after complete deployment. Fischer et al16 published their initial experience and showed, similar to other flow diverters, a progressive occlusion with an overall occlusion rate of 85.7% at last follow-up and a good safety profile (permanent morbidity 1.7%, and mortality 0.8%). Briganti et al17 have also reported their experience with the p64 and showed occlusion rates of 88% and 2.5% permanent morbidity with no mortality.
With the introduction of flow diversion into clinical practice, previously untreatable or difficult to treat aneurysms are now amenable to endovascular treatment approaches. Until recently, little has been published on the use of flow diverters above the level of the circle of Willis and especially their use in the anterior cerebral artery (ACA).18 The purpose of our study is to report our experience with flow diverters in the management of aneurysms of the ACA, excluding the anterior communicating artery (AcomA), including the safety and effectiveness of this strategy.
Materials and methods
Patient population
Between September 2009 and February 2016, 26 patients with unruptured ACA aneurysms were admitted to our institution for endovascular treatment. For each patient we recorded demographic data, clinical presentation, location of the aneurysm, therapeutic intervention, immediate angiographic and clinical result, and clinical and radiological follow-up information. The data were entered into our prospectively collected computer database.
Classification of ACA segment aneurysms
All aneurysms were evaluated and anatomically located based in the position of the aneurysmal neck. The A1 segment was classified as the segment extending from the termination of the internal carotid artery (ICA) to the AcomA. The A2 segment was defined as the segment of the vessel extending from the AcomA to the region between the rostrum and the genu of the corpus callosum. The A3 portion of the vessel was defined as that portion of the vessel lying anterior to, and curving around, the genu of the corpus callosum. There were no documented aneurysms arising from the A4 segment or distal. We purposefully excluded aneurysms of the AcomA itself as we feel these aneurysms warrant separate attention and alternative treatment strategies.
Endovascular treatment
All treatments were performed under general anesthesia. Two commercially available FDS were used: PED (Medtronic) and p64 (phenox, Bochum, Germany). Patient informed consent was obtained before the procedure in all cases. The selection of FDS was dependent upon the operators' judgment. A single FDS was placed in all patients.
All patients received dual antiplatelet therapy (aspirin 100 mg daily and clopidogrel 75 mg) before the treatment. The effectiveness of the antiplatelet regimen was tested using the Multiplate analyzer (Roche). Patients found to be resistant to clopidogrel received 2×90 mg ticagrelor daily. The postprocedural antiplatelet regimen consisted of clopidogrel continued for 12 months after treatment and aspirin continued for life.
All procedures were performed via the right common femoral route using a 6 Fr access system as standard and either a Marksman (Covidien) catheter or XT27 (Stryker Neurovascular) catheter to deploy the FDS. All procedures were performed under heparin anticoagulation with a 5000 IU bolus dose at the start of the procedure and subsequent 1000 IU bolus doses every hour to maintain the activated clotting time between 2 and 2.5 times the baseline level.
Procedural assessment and follow-up
Patency and flow characteristics within the ACA and any cortical branches were assessed angiographically immediately after placement of the FDS and during follow-up. Procedural follow-up (digital subtraction angiography (DSA)) was performed initially at 3–6 months, again at 9–12 months and then once a year. Standard angiographic projections were used to assess the patency of the vessels and the aneurysms in addition to angiographic projections that repeated those used during the treatment. Aneurysm occlusion was graded as either completely excluded, minor remnant, major remnant, or unchanged (patent).
Neurological examinations were performed to evaluate potential ischemic or hemorrhagic complications in the postoperative period (<24 hours after the procedure) and at each subsequent follow-up.
Results
Patient population
We identified 26 patients with 27 aneurysms. Eleven patients were male and the average of the patients was 59.3 years old (range 27–77 years). Fourteen patients had left-sided aneurysms. Nine aneurysms were located on the A1 segment, 15 at the A1/A2 junction, 2 on the A2 segment, and 1 aneurysm was located at the A2/A3 junction. The average aneurysm fundus size was 2.9 mm (range 2–6 mm). The results are summarized in table 1.
Table 1.
The anatomical and radiological data of the treated aneurysms
| Patient No | Location | Number of aneurysms on the ACA | Laterality | Aneurysm neck (mm) | Aneurysm dome (mm) | Other treatment | Flow diverter | First F/U (months) | Occluded at F/U | Covered branch patent? | mRS before intervention | mRS after intervention |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | A1 | 1 | l | 2 | 2 | 0 | 2×PED | 3 | Y | Y | 0 | 0 |
| 2 | A1/A2 | 1 | r | 2.5 | 2.5 | 0 | 1×p64 | 2 | Y | Y | 0 | 0 |
| 3 | A1 | 1 | r | 2 | 2 | 0 | 1×p64 | 3 | Y | Y | 0 | 0 |
| 4 | A1/A2 | 1 | r | 2 | 3 | 0 | 1×p64 | 3 | Y | Y | 0 | 0 |
| 5 | A1/A2 | 1 | l | 2 | 3 | 0 | 1×p64 | 3 | Y | Y | 0 | 0 |
| 6 | A1/A2 | 1 | r | 3 | 3 | 0 | 2×PED | 4 | Y | Y | 1 | 1 |
| 7 | A1 | 1 | l | 2 | 4 | Coils | 2×p64 telescoped | 4 | Y | Y | 0 | 0 |
| A1/A2 | 1 | l | 2 | 2 | 0 | 5 | Y | Y | 0 | 0 | ||
| 8 | A1 | 1 | l | 2 | 4 | 0 | 1×p64 | 4 | N/A | Y | 1 | 1 |
| 9 | A1/A2 | 1 | l | 2 | 2 | 0 | 1×p64 | 1 | Y | Y | 1 | 1 |
| 10 | A1 | 1 | r | 1 | 2.5 | 0 | 1×p64 | 3 | Y | Y | 0 | 0 |
| 11 | A1 | 1 | l | 2 | 2 | 0 | 1×p64 | 1 | Y | Y | 0 | 0 |
| 12 | A1/A2 | 1 | l | 3 | 6 | Solitaire stent | 1×PED | N/A | N/A | Y | 0 | 3 |
| 13 | A1 | 1 | r | 4 | 2 | 0 | 1×p64 | 3 | Y | Y | 0 | 0 |
| 14 | A1/A2 | 1 | r | 2 | 2 | 0 | 1×p64 | 3 | N/A | Y | 0 | 0 |
| 15 | A1/A2 | 1 | l | 0 | 0 | 0 | 1×p64 | 3 | N | Y | 0 | 0 |
| 16 | A1 | 1 | l | 2 | 4 | Coils | 1×p64 | N/A | N/A | Y | 0 | 0 |
| 17 | A1 | 1 | r | 2 | 4 | 0 | 1×p64 | 3 | N | Y | 0 | 0 |
| 18 | A1/A2 | 1 | l | 3 | 4 | Coils | 1×p64 | 3 | N/A | Y | 1 | 1 |
| 19 | A1/A2 | 1 | l | 2 | 5 | 0 | 1×p64 | N/A | N/A | Y | 0 | 0 |
| 20 | A2/3 | 1 | l | 4 | 2.5 | Coils | 1×PED | 5 | Y | Y | 0 | 0 |
| 21 | A2 | 1 | l | 1 | 2 | 0 | 1×p64 | 3 | Y | Y | 1 | 1 |
| 22 | A1/A2 | 1 | r | 2 | 2 | 0 | 1×p64 | N/A | N/A | Y | 0 | 0 |
| 23 | A1/A2 | 1 | l | 3 | 2 | Enterprise stent | 1×p64 | 3 | Y | Y | 0 | 0 |
| 24 | A1/A2 | 1 | r | 2 | 2 | 0 | 1×p64 | N/A | N/A | Y | 0 | 0 |
| 25 | A1/A2 | 1 | r | 3 | 6 | 0 | 1×p64 | N/A | N/A | Y | 0 | 0 |
| 26 | A2 | 1 | r | 2 | 2 | 0 | 1×PED | 4 | Y | Y | 1 | 1 |
ACA, anterior cerebral artery; F/U, follow-up; mRS, modified Rankin Scale; PED, Pipeline Embolization Device.
Feasibility
Delivery of the flow diverter was possible in all cases. Adjunctive devices were used for six aneurysms—four had coils and two patients had stents. A single type of flow diverter—for example, either a p64 or PED, was used in 23 patients and two telescoped stents were used in 1 patient. Delivery of the flow diverter was possible in all cases.
Angiographic follow-up
At least one follow-up angiogram was available in 20 patients at an average of 3.1 months (range 1–5 months). Delayed follow-up was available in 13 patients at an average of 27.3 months (range 7–66 months). Of all patients with at least one follow-up angiogram 16 aneurysms were completely occluded (80% occlusion) and one patient had a minor remnant (5%). All covered branches remained patent at follow-up.
Complication rate
A single death was seen in our series (patient 12). In this patient a left A1/A2 aneurysm had previously been coiled after a subarachnoid hemorrhage. Follow-up DSA showed a progressive reperfusion of the aneurysm. Catheterization of, and flow diverter deployment, into the left ACA were straightforward. DSA thereafter revealed a wire dissection of the left pericallosal artery, with a minor leakage. The perforated vessel was occluded with glue, with an instantaneous interruption of the extravasation. During the following night, the patient deteriorated clinically and CT showed a massive intracranial hemorrhage (ICH), which eventually caused the death of this patient.
Discussion
Flow diverters are a new generation of stents that cause disruption of intra-aneurysmal blood flow and changes in the transmural pressure gradient. Progressive intra-aneurysmal stasis and thrombosis occurs as does neo-endothelialization of the stent to finally exclude the aneurysm from the circulation and reconstruct the parent artery.2 Even though these devices have only recently entered the interventional sphere, a large body of evidence about their effectiveness, safety profile, and technical limitations has already been amassed, with several systematic reviews available. The review by Briganti et al19 included 18 studies with a total of 1704 aneurysms in 1483 patients. Unruptured aneurysms accounted for 90% of aneurysms treated and 87.5% of aneurysms were located in the anterior circulation, the majority being located on the ICA up to the bifurcation (1368 aneurysms) with only 135 located on either the ACA or middle cerebral artery (MCA). This group reported an overall rate of occlusion at final follow-up of 81.5% (range 69–100%). This study also showed progressive occlusion of the aneurysm, with occlusion of 74.5% of aneurysms at the 6-month follow-up (nine studies) and 89.6% occluded at 12 months (eight studies). The overall rate of ischemic complications was 4.1%, hemorrhagic complications 2.9%, and mortality was reported to be 3.4%.
Lv et al20 published the results of their meta-analysis and systematic review, which included 1524 patients with 1732 aneurysms, 87.5% unruptured and 85.3% located in the anterior circulation below the level of the ICA bifurcation. This group focused principally on complication rates, morbidity, and mortality. They showed that the overall technical failure rate and complication rate was 9.3%, with incomplete deployment of the stents accounting for most of the technical complications (5.2%), and vessel perforation, misplacement dissection, wire fracture, and stent migration all accounting for less than 1% of the technical complications. In this study the overall favorable clinical outcome was reported as 88.2% (modified Rankin Scale <2) and complete or near-complete aneurysmal occlusion rate of 84.4%. They reported morbidity and mortality of 6.6% and these results are comparable with those of other analyses performed by Brinjikji et al,21 who reported aneurysmal occlusion rates of 76%, morbidity of 5%, and mortality of 4% in the 29 studies they evaluated. Similarly Arrese et al22 (15 studies, 897 patients with 1018 aneurysms) reported early mortality of 2.8% and late mortality of 1.3%, with early morbidity 7.3%, late morbidity 2.6%, and overall occlusion rates of 76.2%. Interestingly, they showed a difference in the occlusion rate between the Silk flow diverter and the PED (68% occlusion vs 88%, respectively) but no increase in the rate of hemorrhagic complications between the devices. The rates of occlusion, morbidity, and mortality from the major series using individual flow diverters (PED, Silk, Surpass, p64, and FRED) are summarized in table 2.
Table 2.
Review of the published Flow Diverter data for individual stent type
| Flow diverter | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Study | Year of publication | No. of Patients | No. of aneurysms | PED | Silk | Surpass | p64 | FRED | Morbidity (%) | Mortality (%) | Occlusion rate at last F/U (%) |
| Berge et al23 | 2012 | 65 | 77 | 73 | 7.80 | 3 | 84.50 | ||||
| Wagner et al24 | 2012 | 22 | 26 | 23 | 5 | 5 | 86 | ||||
| Maimon et al25 | 2012 | 28 | 32 | 31 | 7.20 | 3.60 | 83.30 | ||||
| Lubicz et al26 | 2015 | 58 | 70 | 54 | 5.50 | 0 | 73 | ||||
| Strauss et al27 | 2016 | 60 | 67 | 62 | 10 | 6.67 | 88 | ||||
| Mpotsaris et al28 | 2015 | 25 | 28 | 28 | 8 | 4 | 59 | ||||
| Shankar et al11 | 2016 | 92 | 92 | 92 | 8.70 | 2.20 | 83.10 | ||||
| Briganti et al29 | 2012 | 273 | 295 | 182 | 151 | 3.70 | 5.90 | 85 | |||
| Yu et al30 | 2012 | 143 | 178 | 213 | 3.50 | 3.50 | 84 | ||||
| O’Kelly et al31 | 2013 | 97 | 97 | 156 | 4.30 | 6.40 | 90 | ||||
| Saatci et al32 | 2012 | 191 | 251 | 324 | 1 | 0.50 | 94.60 | ||||
| Fischer et al33 | 2012 | 88 | 101 | 235 | 5.60 | 1.10 | 52 | ||||
| Wakhloo et al12 | 2015 | 165 | 186 | 165 | 4.20 | 2.40 | 75 | ||||
| De Vries et al34 | 2013 | 37 | 49 | 38 | 13.5 | 0 | 94 | ||||
| Fischer et al16 | 2015 | 121 | 130 | 127 | 1.70 | 0.80 | 85.70 | ||||
| Möhlenbruch et al14 | 2015 | 29 | 34 | 35 | 10.30 | 0 | 73 | ||||
| Poncyljusz et al35 | 2013 | 6 | 8 | 8 | 0 | 0 | 100 | ||||
| Briganti et al15 | 2016 | 20 | 24 | 24 | 0 | 0 | 83 | ||||
| Kocer et al13 | 2014 | 35 | 37 | 35 | 2.80 | 0 | 100 (at 12 months) | ||||
| Average | 5.41 | 2 | 81.8 | ||||||||
FRED, Flow Re-direction Endoluminal Device; PED, Pipeline Embolization Device.
The ACA is an extremely important artery that supplies eloquent brain territories with numerous small perorating branches.36 37 Some of these arteries can be derived from the AcomA when this vessel is present. Damage to these small vessels can result in devastating effects, including hemiparesis, anosmia, amnesic syndromes, and psychiatric conditions.38 39 Therefore, it is perhaps not entirely unexpected that the treatment of aneurysms arising from this vessel has followed standard endovascular and neurosurgical approaches. The patency of covered branches has naturally been of major concern when considering the use of flow diverters despite evidence from animal models suggesting that even multiple telescoped flow diverters do not result in occlusion of perforating vessels.40 Neki et al3 recently published the results of their study evaluating the patency of the anterior choroidal artery following coverage by a flow diverter and they showed that in all cases with angiographic follow-up the artery remained patent; this is something we have also seen in our department (unpublished results).
However, infarction after placement of a flow diverter in the distal anterior circulation has been seen. Nelson et al8 reported a left basal ganglia infarction secondary to two PEDs placed in the M1 segment of the left MCA with a pre-existing stent. Van Rooij and Sluzewski41 reported a further case of left basal ganglia infarction after two telescoped PEDs were placed in the A1 segment of the ACA. Recently, larger series have been published. Zanaty et al42 described 10 patients with MCA aneurysms treated with flow diversion and showed an occlusion rate of 77.7% (mean follow-up of 7.55 months) with one periprocedural stroke (10%). One branch occlusion and one parent vessel occlusion, both of which were asymptomatic, were also seen in this group. Similarly, Yavuz et al4 used the PED to treat 25 aneurysms of the MCA with a complete occlusion rate of 84%, no deaths, and only one morbidity, which was deemed to be secondary to vasospasm. In this series, of the nine cortical branches that were covered and showed either reduced filling or complete occlusion, all were clinically asymptomatic. Caroff et al43 performed a retrospective analysis of 14 patients with 15 aneurysms of the MCA bifurcation, all treated with flow diversion and in this series although there were no deaths, morbidity was 21% at follow-up and 43% of patients showed ischemic lesions on MRI that was deemed secondary to the treatment. Similarly, Briganti et al44 in their series showed a high rate of ischemic complications (27%) with permanent neurological deficit in 21%. Pistocchi et al45 published their series of 30 aneurysms treated with either the Silk or PED. Of these 30 aneurysms, 21 were located in the ACAs. At mean follow-up of 13 months, 79% of aneurysms were occluded, with neurological complications seen in 11.1% (3.7% permanent). Lin et al46 recently published their series of 28 patients with 28 aneurysms distal to the ICA bifurcation, all of which were treated with the PED. In this study, of the 27 patients with angiographic follow-up, 21 had complete aneurysm occlusion. The periprocedural complication rate was 10.7% with good outcome (modified Rankin Scale ≤2) in 96.4%. Gawlitza et al47 published their series of 17 patients with 18 aneurysms, 13 of which were present on the MCA. In total 19 cortical branches were covered. Of these ‘jailed’ branches, three were immediately occluded with a further three showing reduced blood flow (15.8% each). However, at the latest follow-up only two branches were completely occluded, although 47.4% of the covered branches were of reduced caliber. This demonstrates that changes in the flow pattern can occur rapidly and can adjust over time to changes in flow demand. There were no deaths or permanent morbidity but two patients had symptomatic perforator territory infarctions and asymptomatic lacunar infarctions were seen in 29.4% of patients. It is also worth noting that in the recent meta-analysis performed by Lv et al,20 only posterior circulation aneurysms and peripheral location had a statistically significant increased odds ratio for morbidity and mortality. However, this was not seen in the multivariate analysis conducted by Brinjikji et al.48 In our series none of the covered branches were occluded at follow-up.
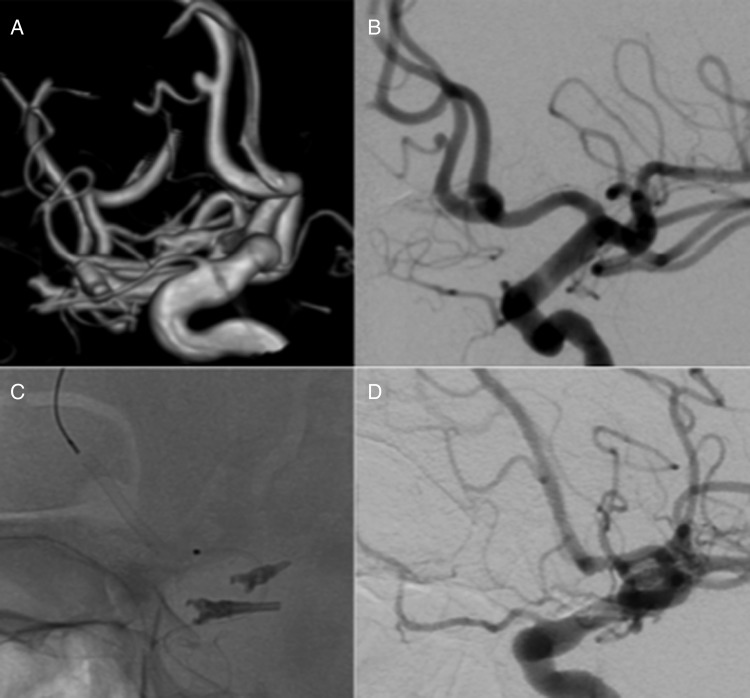
Figure 1.
A patient in their twenties presented with an unruptured aneurysm of the A2 segment that was treated with a single Pipeline Embolization Device (PED). Catheter angiography performed at 3 months showed complete exclusion of the aneurysm from the circulation and patency of the fronto-polar branch.
Figure 2.
A patient in their early teens was treated with a single p64 flow diverter for an unruptured aneurysm arising from the proximal A1 segment of the right anterior cerebral artery. An angiogram performed at 3 months after treatment showed complete exclusion of the aneurysm from the circulation.
Several reports have recently been published that deal specifically with flow diversion in the ACA territory. Clarençon et al49 recently reported their results of treating ACA aneurysms with flow diverters. In their study of seven patients with eight aneurysms, three were located on the A1 segment and two on the A2/A3 segment with the remainder located on the AcomA. Three of the treated aneurysms showed complete occlusion at follow-up (grade A on the Raymond–Roy classification) and two showed grade B occlusion on the Raymond–Roy classification at follow-up. There were no acute or delayed clinical complications and they noted that treatment with flow-diverting stents was feasible in all patients. Dabus et al50 published the largest series to date of aneurysms in the ACA territory treated with the PED. In their series of 20 patients with 20 aneurysms they showed an aneurysm occlusion rate of 68.7% (11/16 patients with angiographic follow-up data at a mean of 10 months). There was one death, secondary to early postoperative hemorrhage that the authors could not easily explain and one minor infarction (5% morbidity and 5% mortality). Taken together these results suggest that flow diverters can be used in the distal circulation with high success rates for aneurysm occlusion. However, the risk of perforator infarction is present and although it does not often lead to permanent morbidity, there is a definite risk of this occurring. The predisposing factors for perforator infarction—for example, fusiform aneurysm, stent type etc, are yet to be elucidated and larger studies are required.
In our series one death occurred after hemorrhage that occurred secondary to wire perforation of a vessel during deployment of the flow diverter. Even though the vessel was glued intraoperatively and the hemorrhage controlled, a repeat hemorrhage occurred during the night and the patient died. It is difficult for us to explain this. Vessel perforation has been noted when balloon inflation is used to remodel implanted flow diverters and during wire manipulation.8 34 Delayed hemorrhage is generally considered to be one of two different types—either subarachnoid or intraparenchymal, and each occurs with a risk of 3%21 but the underlying mechanism is still to be elucidated. Distant hemorrhages may be caused by hemorrhagic transformation of infarctions that occurred during the procedure,51 52 whereas subarachnoid hemorrhage is thought to occur secondary to degradation of the aneurysm wall by enzymes triggered during thrombosis.53 54
In addition to flow diversion, alternative endovascular treatment strategies are available. Cavalcanti et al55 published their single-center experience of 22 consecutive patients with distal ACA aneurysms. They achieved initial occlusion in all aneurysms of ≥95%, including in the 13 patients who presented with subarachnoid hemorrhage. Of the 13 patients who had radiographic follow-up, complete occlusion was seen in 11 and re-coiling was required in two cases. Before this Menovsky et al56 presented their series of coiled distal ACA aneurysms, in which they achieved initial complete occlusion in 91.7% of patients with 66.7% of aneurysms remaining completely occluded at last follow-up. Similarly, Yamazaki et al57 achieved complete occlusion in 19 of 27 coiled pericallosal aneurysms, with a neck remnant in six aneurysms. Overall, using coiling as the primary treatment of ACA aneurysms, both ruptured and unruptured, the mean morbidity stands at 8.8% (range 0–17.2%) with a mean mortality of 8.8% (range 0–20.7%).56 58–62 Neurosurgical treatment is also an option and de Sousa et al63 reported a 100% rate of complete occlusion on routine postoperative angiography after the treatment of 74 distal ACA aneurysms. Lehecka et al64 reported an occlusion rate of 95% in 362 patients undergoing microneurosurgical treatment.
This paper is one of the first to exclusively deal with aneurysms arising from the ACA. Our results suggest that this treatment option is technically feasible and has a low risk of transient and/or permanent clinical complications.
Our study has several limitations. First, it is a retrospective analysis of data prospectively collected from a single center. The relatively small population and lack of long-term follow-up are further limitations.
Conclusion
Our series suggests that the treatment of ACA aneurysms with flow diverters is technically feasible, has a good safety profile, and can result in exclusion of the aneurysms arising from these vessels.
Footnotes
Twitter: Follow Marta Perez at @MartaAguilarPe2
Contributors: MAP, PB, RMM data gathering, manuscript preparation; OG, HB: review, editing; HH: guarantor, overall review, study design.
Competing interests: MAP, PB, and RMM are proctors and consultants for phenox GmbH, and receive moderate financial compensation. HH is a co-founder and shareholder of phenox GmbH.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Becske T, Kallmes DF, Saatci I, et al. . Pipeline for uncoilable or failed aneurysms: results from a multicenter clinical trial. Radiology 2013;267:858–68. 10.1148/radiol.13120099 [DOI] [PubMed] [Google Scholar]
- 2.Kadirvel R, Ding YH, Dai D, et al. . Cellular mechanisms of aneurysm occlusion after treatment with a flow diverter. Radiology 2014;270:394–9. 10.1148/radiol.13130796 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Neki H, Caroff J, Jittapiromsak P, et al. . Patency of the anterior choroidal artery covered with a flow-diverter stent. J Neurosurg 2015;123:1540–5. 10.3171/2014.11.JNS141603 [DOI] [PubMed] [Google Scholar]
- 4.Yavuz K, Geyik S, Saatci I, et al. . Endovascular treatment of middle cerebral artery aneurysms with flow modification with the use of the pipeline embolization device. AJNR Am J Neuroradiol 2014;35:529–35. 10.3174/ajnr.A3692 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kallmes DF, Ding YH, Dai D, et al. . A new endoluminal, flow-disrupting device for treatment of saccular aneurysms. Stroke J Cereb Circ 2007;38:2346–52. 10.1161/STROKEAHA.106.479576 [DOI] [PubMed] [Google Scholar]
- 6.Augsburger L, Farhat M, Reymond P, et al. . Effect of flow diverter porosity on intraaneurysmal blood flow. Klin Neuroradiol 2009;19:204–14. 10.1007/s00062-009-9005-0 [DOI] [PubMed] [Google Scholar]
- 7.Lieber BB, Stancampiano AP, Wakhloo AK. Alteration of hemodynamics in aneurysm models by stenting: influence of stent porosity. Ann Biomed Eng 1997;25:460–9. 10.1007/BF02684187 [DOI] [PubMed] [Google Scholar]
- 8.Nelson PK, Lylyk P, Szikora I, et al. . The pipeline embolization device for the intracranial treatment of aneurysms trial. AJNR Am J Neuroradiol 2011;32:34–40. 10.3174/ajnr.A2421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Griessenauer CJ, Loukas M, Scott JA, et al. . The artery of Davidoff and Schechter: an anatomical study with neurosurgical case correlates. Br J Neurosurg 2013;27:815–18. 10.3109/02688697.2013.798856 [DOI] [PubMed] [Google Scholar]
- 10.Murthy SB, Shah S, Shastri A, et al. . The SILK flow diverter in the treatment of intracranial aneurysms. J Clin Neurosci 2014;21:203–6. 10.1016/j.jocn.2013.07.006 [DOI] [PubMed] [Google Scholar]
- 11.Shankar JJS, Tampieri D, Iancu D, et al. . SILK flow diverter for complex intracranial aneurysms: a Canadian registry. J Neurointerv Surg 2016;8:273–8. 10.1136/neurintsurg-2015-011708 [DOI] [PubMed] [Google Scholar]
- 12.Wakhloo AK, Lylyk P, de Vries J, et al. . Surpass flow diverter in the treatment of intracranial aneurysms: a prospective multicenter study. AJNR Am J Neuroradiol 2015;36:98–107. 10.3174/ajnr.A4078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kocer N, Islak C, Kizilkilic O, et al. . Flow Re-direction Endoluminal Device in treatment of cerebral aneurysms: initial experience with short-term follow-up results. J Neurosurg 2014;120:1158–71. 10.3171/2014.1.JNS131442 [DOI] [PubMed] [Google Scholar]
- 14.Möhlenbruch MA, Herweh C, Jestaedt L, et al. . The FRED flow-diverter stent for intracranial aneurysms: clinical study to assess safety and efficacy. AJNR Am J Neuroradiol 2015;36:1155–61. 10.3174/ajnr.A4251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Briganti F, Leone G, Ugga L, et al. . Safety and efficacy of flow re-direction endoluminal device (FRED) in the treatment of cerebral aneurysms: a single center experience. Acta Neurochir (Wien) 2016;158:1745–55. 10.1007/s00701-016-2875-4 [DOI] [PubMed] [Google Scholar]
- 16.Fischer S, Aguilar-Pérez M, Henkes E, et al. . Initial experience with p64: a novel mechanically detachable flow diverter for the treatment of intracranial saccular sidewall aneurysms. AJNR Am J Neuroradiol 2015;36:2082–9. 10.3174/ajnr.A4420 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Briganti F, Leone G, Ugga L, et al. . Mid-term and long-term follow-up of intracranial aneurysms treated by the p64 Flow Modulation Device: a multicenter experience. J Neurointerv Surg 2017;9:70–6.. 10.1136/neurintsurg-2016-012502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rouchaud A, Saleme S, Gory B, et al. . Endovascular exclusion of the anterior communicating artery with flow-diverter stents as an emergency treatment for blister-like intracranial aneurysms. Interv Neuroradiol 2013;19:471–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Briganti F, Leone G, Marseglia M, et al. . Endovascular treatment of cerebral aneurysms using flow-diverter devices: a systematic review. Neuroradiol J 2015;28:365–75. 10.1177/1971400915602803 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lv X, Yang H, Liu P, et al. . Flow-diverter devices in the treatment of intracranial aneurysms: a meta-analysis and systematic review. Neuroradiol J 2016;29:66–71. 10.1177/1971400915621321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Brinjikji W, Murad MH, Lanzino G, et al. . Endovascular treatment of intracranial aneurysms with flow diverters a meta-analysis. Stroke 2013;44:442–7. 10.1161/STROKEAHA.112.678151 [DOI] [PubMed] [Google Scholar]
- 22.Arrese I, Sarabia R, Pintado R, et al. . Flow-diverter devices for intracranial aneurysms: systematic review and meta-analysis. Neurosurgery 2013;73:193–9; discussion 199–200 10.1227/01.neu.0000430297.17961.f1 [DOI] [PubMed] [Google Scholar]
- 23.Berge J, Biondi A, Machi P, et al. . Flow-diverter silk stent for the treatment of intracranial aneurysms: 1-year follow-up in a multicenter study. AJNR Am J Neuroradiol 2012;33:1150–5. 10.3174/ajnr.A2907 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wagner A, Cortsen M, Hauerberg J, et al. . Treatment of intracranial aneurysms. Reconstruction of the parent artery with flow-diverting (Silk) stent. Neuroradiology 2012;54:709–18. 10.1007/s00234-011-0949-9 [DOI] [PubMed] [Google Scholar]
- 25.Maimon S, Gonen L, Nossek E, et al. . Treatment of intra-cranial aneurysms with the SILK flow diverter: 2 years’ experience with 28 patients at a single center. Acta Neurochir (Wien) 2012;154:979–87. 10.1007/s00701-012-1316-2 [DOI] [PubMed] [Google Scholar]
- 26.Lubicz B, Van der Elst O, Collignon L, et al. . Silk flow-diverter stent for the treatment of intracranial aneurysms: a series of 58 patients with emphasis on long-term results. AJNR Am J Neuroradiol 2015;36:542–6. 10.3174/ajnr.A4143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Strauss I, Maimon S. Silk flow diverter in the treatment of complex intracranial aneurysms: a single-center experience with 60 patients. Acta Neurochir (Wien) 2016;158:247–54. 10.1007/s00701-015-2644-9 [DOI] [PubMed] [Google Scholar]
- 28.Mpotsaris A, Skalej M, Beuing O, et al. . Long-term occlusion results with SILK flow diversion in 28 aneurysms: do recanalizations occur during follow-up? Interv Neuroradiol 2015;21:300–10. 10.1177/1591019915583119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Briganti F, Napoli M, Tortora F, et al. . Italian multicenter experience with flow-diverter devices for intracranial unruptured aneurysm treatment with periprocedural complications--a retrospective data analysis. Neuroradiology 2012;54:1145–52. 10.1007/s00234-012-1047-3 [DOI] [PubMed] [Google Scholar]
- 30.Yu SCH, Kwok CK, Cheng PW, et al. . Intracranial aneurysms: midterm outcome of pipeline embolization device—a prospective study in 143 patients with 178 aneurysms. Radiology 2012;265:893–901. 10.1148/radiol.12120422 [DOI] [PubMed] [Google Scholar]
- 31.O'Kelly CJ, Spears J, Chow M, et al. . Canadian experience with the pipeline embolization device for repair of unruptured intracranial aneurysms. AJNR Am J Neuroradiol 2013;34:381–7. 10.3174/ajnr.A3224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Saatci I, Yavuz K, Ozer C, et al. . Treatment of intracranial aneurysms using the pipeline flow-diverter embolization device: a single-center experience with long-term follow-up results. AJNR Am J Neuroradiol 2012;33:1436–46. 10.3174/ajnr.A3246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fischer S, Vajda Z, Aguilar Perez M, et al. . Pipeline embolization device (PED) for neurovascular reconstruction: initial experience in the treatment of 101 intracranial aneurysms and dissections. Neuroradiology 2012;54:369–82. 10.1007/s00234-011-0948-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.De Vries J, Boogaarts J, Van Norden A, et al. . New generation of flow diverter (Surpass) for unruptured intracranial aneurysms: a prospective single-center study in 37 patients. Stroke 2013;44:1567–77. 10.1161/STROKEAHA.111.000434 [DOI] [PubMed] [Google Scholar]
- 35.Poncyljusz W, Sagan L, Safranow K, et al. . Initial experience with implantation of novel dual layer flow-diverter device FRED. Wideochir Inne Tech Maloinwazyjne 2013;8:258–64. 10.5114/wiitm.2011.35794 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Perlmutter D, Rhoton AL. Microsurgical anatomy of the anterior cerebral-anterior communicating-recurrent artery complex. J Neurosurg 1976;45:259–72. 10.3171/jns.1976.45.3.0259 [DOI] [PubMed] [Google Scholar]
- 37.Perlmutter D, Rhoton AL. Microsurgical anatomy of the distal anterior cerebral artery. J Neurosurg 1978;49:204–28. 10.3171/jns.1978.49.2.0204 [DOI] [PubMed] [Google Scholar]
- 38.Marinković S, Milisavljević M, Marinković Z. Branches of the anterior communicating artery. Microsurgical anatomy. Acta Neurochir (Wien) 1990;106:78–85. 10.1007/BF01809337 [DOI] [PubMed] [Google Scholar]
- 39.Ostrowski AZ, Webster JE, Gurdjian ES. The proximal anterior cerebral artery: an anatomic study. Arch Neurol 1960;3:661–4. 10.1001/archneur.1960.00450060049005 [DOI] [PubMed] [Google Scholar]
- 40.Dai D, Ding YH, Kadirvel R, et al. . Patency of branches after coverage with multiple telescoping flow-diverter devices: an in vivo study in rabbits. AJNR Am J Neuroradiol 2012;33:171–4. 10.3174/ajnr.A2879 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.van Rooij WJ, Sluzewski M. Perforator infarction after placement of a pipeline flow-diverting stent for an unruptured A1 aneurysm. AJNR Am J Neuroradiol 2010;31:E43–4. 10.3174/ajnr.A2034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zanaty M, Chalouhi N, Tjoumakaris SI, et al. . Flow diversion for complex middle cerebral artery aneurysms. Neuroradiology 2014;56:381–7. 10.1007/s00234-014-1339-x [DOI] [PubMed] [Google Scholar]
- 43.Caroff J, Neki H, Mihalea C, et al. . Flow-diverter stents for the treatment of saccular middle cerebral artery bifurcation aneurysms. AJNR Am J Neuroradiol 2016;37:279–84. 10.3174/ajnr.A4540 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Briganti F, Delehaye L, Leone G, et al. . Flow diverter device for the treatment of small middle cerebral artery aneurysms. J Neurointerv Surg 2016;8:287–94. 10.1136/neurintsurg-2014-011460 [DOI] [PubMed] [Google Scholar]
- 45.Pistocchi S, Blanc R, Bartolini B, et al. . Flow diverters at and beyond the level of the circle of willis for the treatment of intracranial aneurysms. Stroke 2012;43:1032–8. 10.1161/STROKEAHA.111.636019 [DOI] [PubMed] [Google Scholar]
- 46.Lin N, Lanzino G, Lopes DK, et al. . Treatment of Distal Anterior Circulation Aneurysms With the Pipeline Embolization Device: A US Multicenter Experience. Neurosurgery 2016;79:14–22. 10.1227/01.neu.0000317307.16332.03 [DOI] [PubMed] [Google Scholar]
- 47.Gawlitza M, Januel A-C, Tall P, et al. . Flow diversion treatment of complex bifurcation aneurysms beyond the circle of Willis: a single-center series with special emphasis on covered cortical branches and perforating arteries. J Neurointerv Surg 2016;8:481–7. 10.1136/neurintsurg-2015-011682 [DOI] [PubMed] [Google Scholar]
- 48.Brinjikji W, Lanzino G, Cloft HJ, et al. . Risk factors for ischemic complications following pipeline embolization device treatment of intracranial aneurysms: results from the IntrePED study. AJNR Am J Neuroradiol. Published Online First: 21 April 2016. doi:10.3174/ajnr.A4807 10.3174/ajnr.A4807 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Clarençon F, Di Maria F, Gabrieli J, et al. . Flow diverter stents for the treatment of anterior cerebral artery aneurysms: safety and effectiveness. Clin Neuroradiol. Published Online First: 7 August 2015. doi:10.1007/s00062-015-0441-8 10.1007/s00062-015-0441-8 [DOI] [PubMed] [Google Scholar]
- 50.Dabus G, Grossberg JA, Cawley CM, et al. . Treatment of complex anterior cerebral artery aneurysms with Pipeline flow diversion: mid-term results. J Neurointerv Surg 2017;9:147–51.. [DOI] [PubMed] [Google Scholar]
- 51.Cruz JP, Chow M, O'Kelly C, et al. . Delayed ipsilateral parenchymal hemorrhage following flow diversion for the treatment of anterior circulation aneurysms. AJNR Am J Neuroradiol 2012;33:603–8. 10.3174/ajnr.A3065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Colby GP, Lin LM, Coon AL. Revisiting the risk of intraparenchymal hemorrhage following aneurysm treatment by flow diversion. AJNR Am J Neuroradiol 2012;33:E107; author reply E108 10.3174/ajnr.A3201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Turowski B, Macht S, Kulcsár Z, et al. . Early fatal hemorrhage after endovascular cerebral aneurysm treatment with a flow diverter (SILK-Stent): do we need to rethink our concepts? Neuroradiology 2011;53:37–41. 10.1007/s00234-010-0676-7 [DOI] [PubMed] [Google Scholar]
- 54.Kulcsár Z, Houdart E, Bonafé A, et al. . Intra-aneurysmal thrombosis as a possible cause of delayed aneurysm rupture after flow-diversion treatment. AJNR Am J Neuroradiol 2011;32:20–5. 10.3174/ajnr.A2370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Cavalcanti DD, Abla AA, Martirosyan NL, et al. . Endovascular management of distal ACA aneurysms: single-institution clinical experience in 22 consecutive patients and literature review. AJNR Am J Neuroradiol 2013;34:1593–9. 10.3174/ajnr.A3408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Menovsky T, van Rooij WJJ, Sluzewski M, et al. . Coiling of ruptured pericallosal artery aneurysms. Neurosurgery 2002;50:11–14; discussion 14–15. [DOI] [PubMed] [Google Scholar]
- 57.Yamazaki T, Sonobe M, Kato N, et al. . Endovascular coiling as the first treatment strategy for ruptured pericallosal artery aneurysms: results, complications, and follow up. Neurol Med Chir (Tokyo) 2013;53:409–17. 10.2176/nmc.53.409 [DOI] [PubMed] [Google Scholar]
- 58.Keston P, White PM, Horribine L, et al. . The endovascular management of pericallosal artery aneurysms. J Neuroradiol 2004;31:384–90. 10.1016/S0150-9861(04)97021-6 [DOI] [PubMed] [Google Scholar]
- 59.Waldenberger P, Petersen J, Chemelli A, et al. . Endovascular therapy of distal anterior cerebral artery aneurysms—an effective treatment option. Surg Neurol 2008;70:368–77. 10.1016/j.surneu.2007.07.058 [DOI] [PubMed] [Google Scholar]
- 60.Pandey A, Rosenwasser RH, Veznedaroglu E. Management of distal anterior cerebral artery aneurysms: a single institution retrospective analysis (1997–2005). Neurosurgery 2007;61:909–16; discussion 916–7 10.1227/01.neu.0000303186.26684.81 [DOI] [PubMed] [Google Scholar]
- 61.Nguyen TN, Raymond J, Roy D, et al. . Endovascular treatment of pericallosal aneurysms. J Neurosurg 2007;107:973–6. 10.3171/JNS-07/11/0973 [DOI] [PubMed] [Google Scholar]
- 62.Vora N, Thomas AJ, Gupta R, et al. . Endovascular treatment of distal anterior cerebral artery aneurysms: technical results and review of the literature. J Neuroimaging 2010;20:70–3. 10.1111/j.1552-6569.2008.00324.x [DOI] [PubMed] [Google Scholar]
- 63.de Sousa AA, Dantas FL, de Cardoso GT, et al. . Distal anterior cerebral artery aneurysms. Surg Neurol 1999;52:128–35; discussion 135–6 10.1227/01.neu.0000317307.16332.03 [DOI] [PubMed] [Google Scholar]
- 64.Lehecka M, Lehto H, Niemelä M, et al. . Distal anterior cerebral artery aneurysms: treatment and outcome analysis of 501 patients. Neurosurgery 2008;62:590–601; discussion 590–601 10.1227/01.neu.0000317307.16332.03 [DOI] [PubMed] [Google Scholar]