Abstract
Background:
Stereotactic body radiotherapy (SBRT) is an emerging treatment option for spinal metastases with demonstrated efficacy in the upfront, postoperative, and re-treatment settings, as well as for tumor histologies considered radioresistant. Uncertainty exists regarding the optimal dose and fractionation schedule, with single and multifraction regimens commonly utilized.
Methods:
A literature search of the PubMed and Medline databases was conducted to identify papers specific to spine SBRT and the effect of varying dose/fractionation regimens on outcomes. Bibliographies of relevant papers were searched for further references, and international spine SBRT experts were consulted.
Results:
Local control rates generally exceed 80% at 1 year, while high rates of pain control have been attained. There is insufficient evidence to suggest superiority of either single or multiple fraction regimens with respect to local control and pain control. Low rates of toxicity have been reported, assuming strict dose constraints are respected. Radiation myelopathy may be the most morbid toxicity, although the rates are low. The risk of vertebral compression fracture appears to be associated with higher doses per fraction such as those used in single-fraction regimens. The Spinal Instability Neoplastic Score should be considered when evaluating patients for spine SBRT, and prophylactic stabilisation may be warranted. Pain flare is a relatively common toxicity which may be mediated with prophylactic dexamethasone. Because of the treatment complexity and potentially serious toxicities, strict quality assurance should occur at the organizational, planning, dosimetric, and treatment delivery levels.
Conclusion:
Both single and multifraction regimens are safe and efficacious in spine SBRT for spinal metastases. There may be advantages to hypofractionated treatment over single-fraction regimens with respect to toxicity. Ongoing investigation is underway to define optimal dose and fractionation schedules.
Keywords: Metastases, radiotherapy, SBRT, spine, stereotactic body radiation
INTRODUCTION
Spinal metastases are relatively common, with their incidence projected to increase as modern systemic therapies prolong patients’ overall survival. There is increasing focus on optimizing the rates of local control and pain relief, and the durability of both outcomes in appropriate patients. Spine stereotactic body radiation therapy (SBRT) is an emerging treatment option which may offer significant advantages in these aspects over conventional radiotherapy, with a growing body of evidence demonstrating safety and efficacy.[16]
SBRT utilizes ablative radiation doses in few fractions (typically 1–5) to the target. Intensity-modulated radiation therapy (IMRT)/volumetric modulated arc therapy (VMAT) and image-guidance allow the generation of steep dose gradients millimetres from the target, allowing spinal tumors to be treated with high biologically effective doses (BED) while protecting the adjacent spinal cord.[16,45,60] This is demonstrated in Figure 1.
Figure 1.
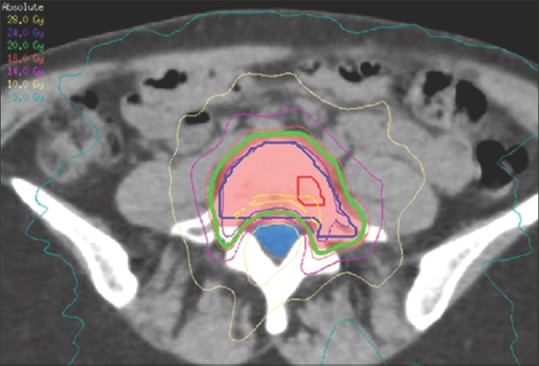
Axial CT scan demonstrating dosimetry for a lumbar spine lesion treated with VMAT, highlighting the steep dose gradient generated between the involved vertebral body and the thecal sac (blue). Adapted with permission[19]
High rates of local control and pain relief are achieved via high BEDs and possibly enhanced antitumor immune response.[6,39] In the upfront setting, its role is to optimize local control and pain relief in patients with reasonable prognoses.[29] In the oligometastatic setting, it can ablate disease nonsurgically with a view to cure or prolong disease-free survival.[12] In the postoperative setting, it improves local control following surgery, particularly if gross disease remains after decompression and/or stabilization. It may allow for de-escalation of surgery to less-invasive/extensive procedures, minimizing morbidity.[51] In the re-treatment setting, SBRT can optimize local and symptom control while limiting dose to previously-irradiated spinal cord/cauda equina.[10,55]
Because of the ablative doses involved, spine SBRT exposes patients to potential toxicities uncommonly observed in conventional radiotherapy such as radiation myelopathy and vertebral compression fracture (VCF), which fortunately occur at a relatively low rate.[34] To optimize treatment quality and safety, the majority of physicians recommend SBRT be offered only in high-volume, experienced centres with a predefined minimum number of patients treated per year. An SBRT-specific team of physicians, therapists, and physicists should be maintained, as well as rigorous protocols and quality assurance processes to ensure treatment quality and consistency.[17,26,60]
With increasing early phase data, spine SBRT has been widely adopted in the developed world. Nonetheless, there is a relative paucity of phase III data,[46] and uncertainty exists regarding the optimal dose and fractionation with respect to local control, symptom control, and risk of adverse effects. This overview of spine SBRT in the current era will focus on how the evolving evidence has guided treatment in the various spine SBRT indications with reference to the impact of dose and fractions on patient outcomes.
PATIENT SELECTION
Predictive scoring systems have been developed to assess which patients benefit most from spine SBRT.[63] Improved overall survival has been associated with female gender, better performance status, previous surgery at the site of spine SBRT, presence of a solitary metastasis in the spine, and a long disease-free interval. Previous radiotherapy and the presence of nonbone metastatic sites negatively affect prognosis. Patients should be able to lie flat and still with appropriate immobilization devices in use for the amount of time required for planning and treatment delivery.[43] Recommendations regarding patient selection for spine SBRT are detailed in Table 1.[36]
Table 1.
Inclusion, relative, and major contraindications for spine SBRT. Adapted with permission[36]
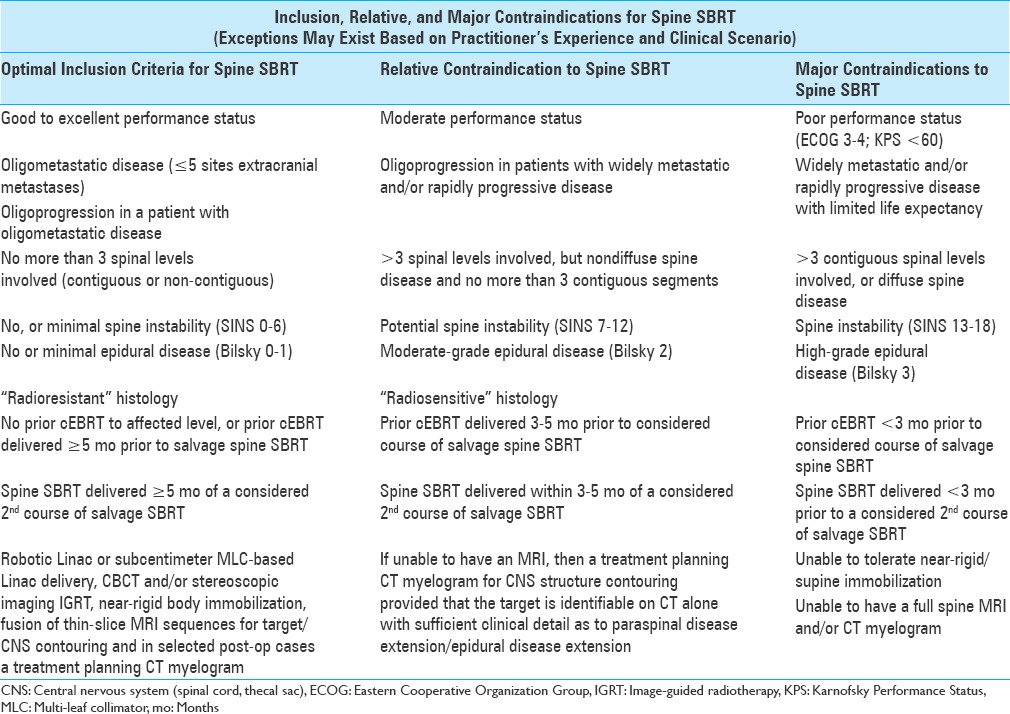
In general terms, disease should be limited to three spinal levels at most, and ideally be at least 2–3 mm from the spinal cord itself to allow for a region of dose drop-off.[45] Bilsky et al. developed a grading system to categorize the extent of epidural disease involvement.[5] Disease compressing the spinal cord but with cerebrospinal fluid still visible is deemed a relative contraindication to spine SBRT, whereas more severe compression is a major contraindication.[36] Patients should have a stable spinal column based on assessment via the Spinal Instability Neoplastic Score (SINS), which risk-stratifies lesions based on location, pain, lesion type, spinal alignment, presence of vertebral body collapse, and posterolateral involvement of spinal elements.[56] In the re-irradiation setting, a period of at least 5 months should have elapsed since previous radiotherapy.[36]
SBRT should not be used for the primary treatment of spinal cord compression outside of a clinical trial setting because of the amount of time required for treatment planning/delivery and risk of under-dosing tumor immediately adjacent to the spinal cord.[45] However, it can be offered as a postoperative treatment after separation surgery.[1,41] In the postoperative setting, patients should be given sufficient time to allow for wound healing, typically one month.
LOCAL CONTROL
The primary rationale for spine SBRT is to deliver a significantly higher BED, thereby improving local control compared with conventional radiotherapy, with published evidence demonstrating efficacy in the upfront, retreatment, and postoperative settings even in radioresistant histologies. Uncertainty exists regarding the optimal dose and fractionation regimen.
Upfront
Both prospective and retrospective data suggest high local control rates for spine SBRT in the upfront setting. Prospective studies reveal local control rates of between 80.5–95% at 12 to 18 months.[3,23,71] These studies included a mixture of patients from each of the three aforementioned treatment settings, though the majority were upfront. Doses were 15–24 Gy in 1 fraction to 27–30 Gy in 3 fractions. Long term follow-up data will be important with increasing long-term cancer survivorship.
A multi-institutional analysis of 301 patients treated upfront with spine SBRT with a variety of dose and fractionation schedules (from 8–60 Gy in 1–20 fractions) found local control at 2 years to be 83.9%, with a highly favorable toxicity profile.[29] Hall et al. reviewed 15 published reports of 1388 patients with 1775 lesions. At median follow-up of 15 months, the combined local control rate was 90%.[31]
Postoperative
Spine SBRT is highly efficacious in the postoperative setting despite the potential for target volume uncertainty following surgical intervention. Tao et al. evaluated the outcomes of 66 patients treated via phase I or II trials, all following laminectomy or vertebrectomy. The 1 and 2-year local control rates were 85% and 79%, respectively.[64] Laufer et al. report a similarly high cumulative 1-year local control rate of 83.6%.[41] Further analysis showed significantly higher local control (96%) with doses ranging from 24–30 Gy in 3 fractions, compared with 18–36 Gy in 5–6 fractions (78%). Redmond et al. summarized outcomes from 12 studies reporting on 426 patients treated postoperatively, demonstrated in Figure 2. The crude local control rate ranged between 70 and 100%, compared with rates of 4 and 79% for conventional radiotherapy, suggesting superiority of SBRT.[51] Of note, high local control rates were reported with both single and multifraction regimens.
Figure 2.
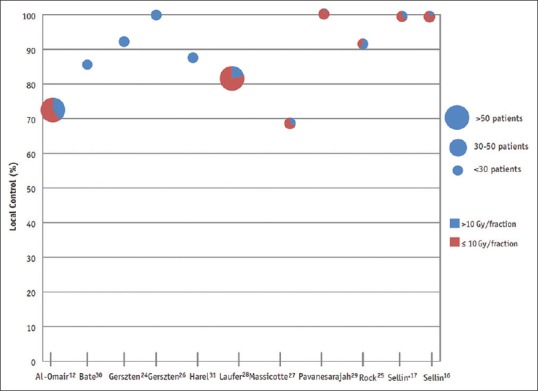
Local control following postoperative spine SBRT, as reviewed by Redmond et al. Dose per fraction is represented via each colour. Adapted with permission[51]
For patients with thecal sac compression, local control after spine SBRT was significantly improved when patients with high grade preoperative epidural disease (Bilsky grade 2 or 3) were downgraded to Bilsky grade 0 or 1, compared with those who had postoperative grade 2 disease.[1] This highlights the benefit of the extent of surgery in clearing epidural disease.
Retreatment
Local failure following conventional radiotherapy is an increasingly common scenario as modern systemic therapies increase patients’ overall survival. The challenge lies in delivering sufficient dose to control recurrent disease while maintaining an acceptable risk of spinal cord myelopathy.
The only multi-institutional study on retreatment is a pooled outcome analysis by Hashmi et al. demonstrating a high degree of efficacy and safety.[32] The median initial conventional radiotherapy dose was 30 Gy in 10 fractions, whereas subsequent median SBRT doses were 16.6 Gy in 1 fraction or 24 Gy in 3 fractions. Local control at 6 and 12 months were 93% and 83%, respectively, while toxicity was limited with a VCF rate of 4.5%; there were no cases of radiation myelopathy. Of note, single fraction treatment was found to predict better local control despite similar equivalent 2-Gy-fraction doses in both regimens. A review of six nonrandomized studies using spine SBRT in the re-irradiation setting showed local control rates at ≥1 year between 66% and 93%.[37] Notably, the studies utilizing lower median prescription doses (20 Gy in 2 fractions and 20 Gy in 5 fractions) demonstrated lower rates of local control.
The number of cases where local failure occurs following spine SBRT is not insignificant and the rationale for conventional radiotherapy in this setting is limited. Retreatment with fractionated spine SBRT safely confers high rates of local control. Thibault et al. reported 40 patients treated with a second course of SBRT with 20–35 Gy in 2–5 fractions; the median dose from initial SBRT was 24 Gy in 2 fractions. Local control at 1 year was 81%, while no cases of vertebral compression fracture nor radiation myelopathy were seen.[66] Median cumulative point-maximum doses to spinal cord PRV were 73.9 Gy in equivalent 2-Gy-fractions (alpha-beta ratio of 2) in patients who had received conventional radiotherapy plus an initial and re-treatment course of SBRT, and 51.3 Gy in patients who had two courses of SBRT. Given the demonstrated safety, these parameters should be respected in the retreatment setting.
Single fraction vs. multifraction
There is no prospective data demonstrating an optimal fractionation schedule for spine SBRT, with both single and multiple fraction regimens commonly utilised. Fractionation exploits intrinsic differences in radiosensitivity between tumour and spinal cord, allowing high tumouricidal doses to be safely delivered to lesions within the epidural space – where up to half of all recurrences occur following conventional radiotherapy.[10]
Conversely, single fraction treatments greater than 15 Gy per fraction are postulated to cause additional cell death via apoptosis. There is no conclusive data demonstrating an advantage in local control with either method – though it is possible that toxicities such as vertebral compression fractures, pain flare, and radiation myelopathy may be reduced with fractionation. Fractionated SBRT may be more appropriate for larger treatment volumes, or in the postoperative and re-irradiation settings.[52]
Published data comparing single to multifraction SBRT is limited to retrospective series. Heron et al. compared single fraction spine SBRT to a mean dose of 16.3 Gy with fractionated SBRT to mean doses of 20.6 Gy to 24.5 Gy in 3–5 fractions.[33] Local control at 2 years was superior for the multifraction group, although note should be made of the relatively conservative doses utilized. For radioresistant histologies, single fraction treatment with 24 Gy in 1 fraction appeared to impart better local control than multifraction SBRT of 27–30 Gy in 3–5 fractions,[21,27] although this may be due to the higher biologically equivalent doses utilized with single-fraction regimens. Further prospective studies are needed to determine the optimal dose and fractionation schedule.
Histology
Tumor histologies such as renal cell carcinoma, melanoma, and sarcoma have traditionally been regarded as radioresistant. Nonetheless, high local control rates have been observed for these tumor types when treated with spine SBRT.
For sarcoma metastases treated with 24–28.5 Gy in 1–3 fractions, the 12-month local control rate was 87.9%, which is significantly higher than historical 1-year local control rates of 50–77% with conventional radiotherapy.[21] In contrast, Tao et al. found a local control rate of only 58% at 1 year in the postoperative setting, although it was suggested that their multifraction regimens delivered insufficient BED to control this radioresistant histology.[64]
For renal cell carcinoma, 1- and 2-year local control rates of 83.5% and 66.2%, respectively, have been reported. The median dose used was 24 Gy in 2 fractions.[65] Ghia et al. found 1- and 2-year local control rates of 82% and 68%, respectively, for renal cell carcinoma metastases. Treatment consisted of either 24 Gy in 1 fraction, 27 Gy in 3 fractions, or 30 Gy in 5 fractions. Sites treated with a single fraction had 1- and 2-year local control rates of 95% and 86%, compared with 71% and 55% for multifraction SBRT.[27] This again suggests that the higher BED regimen can improve local control for radioresistant histologies. A high degree of efficacy is also seen in the postoperative setting for radioresistant tumors. Moulding et al. found 1-year local control rates of 90.5% for patients treated with surgical decompression and single fraction spine SBRT at doses ranging 18–24 Gy.[47]
Gerszten et al. demonstrated efficacy for melanoma spinal metastases using single fraction treatments of 17.5–25 Gy.[25] Of 4 cases treated due to radiological progression, 3 cases achieved long-term tumor control. For patients where the indication for treatment was pain, 96% reported long-term pain improvement.
It can be seen that SBRT provides superior local control compared with conventional radiotherapy for radioresistant histologies. The impact of the number of fractions is unknown, though it is likely that a high BED is required to adequately ablate these metastases. SBRT allows for feasible delivery of such high doses, resulting in the high rates of local control observed.
PAIN CONTROL
Spine SBRT is also efficacious for symptom palliation, an important outcome for patients of reasonable prognosis where the goal is to prolong progression-free survival. Conventional radiotherapy is associated with partial pain relief rates of approximately 60%, with complete pain response rates of 24%.[11]
Reported pain outcomes in 149 prospectively treated patients with a mean baseline pain score of 3.4 on an 11-point Brief Pain Inventory scale fell to 2.1 at 4 weeks post-SBRT. At baseline, 34% of the patients rated pain as moderate to severe, falling to 15% at 2 months. At 6 months, 53.9% of patients reported no pain.[71] The multi-institutional analysis by Guckenberger et al. found that 56.3% of patients suffering mild/moderate pain pre-SBRT were pain free at 11.5 months. Over 80% of patients suffering severe pain at baseline had only mild/moderate pain or were pain free at 11.5 months.[29]
High rates of pain response in the retreatment setting have also been reported, with 84% of the patients experiencing improvement in pain and 74% of patients becoming pain free. Mean pain scores (measured via visual analog scale score of 0–100) were 51 at baseline, and 17.5 at 1 year.[18] There is no data to suggest a difference in pain control based on dose or fractionation schedule.
COMPLICATIONS FROM SPINE SBRT
The available literature suggests low complication rates for spine SBRT, highlighting its utility in the palliative setting. A phase II feasibility study of spine SBRT found no cases of grade 4–5 toxicity, a 2.3% rate of grade 3 toxicity, and a 25% rate of grade 1–2 toxicity among 44 patients.[54] Nonetheless, serious complications have been documented in retrospective studies.[44]
The specific toxicities reported in the literature will be outlined, with the most prominent issues being vertebral compression fracture (VCF) and radiation myelopathy.
Vertebral compression fracture
Radiation-induced tissue necrosis may be the underlying mechanism leading to vertebral instability and subsequent fracture.[15] Rates of VCF following spine SBRT are variable, though are higher than traditional rates of approximately 3% for conventional radiotherapy.[11] The majority of data regarding VCF is in the form of nonrandomized retrospective data, with an evident trend that high doses per fraction result in increased risk. Single fractions of 24 Gy have been associated with VCF rates of 36–39%,[48,53] whereas a series of patients treated with 18 Gy in 1 fraction had a VCF rate of 21%.[24] Fractionated SBRT appears to confer a comparatively lower rate of vertebral compression fracture. In a multi-institutional analysis, only 5.7% of patients received single fraction SBRT, with a low overall VCF rate of 7.8%.[29]
Analyses by Sahgal et al. and Cunha et al. found that 3 components of SINS were risk factors for VCF following spine SBRT, including pre-existing VCF, lytic tumor type, and spinal deformity. Furthermore, the risk of VCF was found to progressively decrease as dose per fraction decreased, suggesting that high doses per fraction are inappropriate for patients with high SINS.[15,56] In high risk cases, there may be a role for pre-SBRT stabilization.[4]
Chang et al. reviewed 24 studies which reported VCF rates and found a crude VCF rate of 13.7%. Where VCF occurred, the rate of salvage intervention was 45%. Of these, 50% were cement augmentation, 2% percutaneous instrumentation, and 48% decompression and reconstruction.[8] However there was a high degree of inconsistency between studies, with some reporting intervention rates as low as 6%. The reasons for intervention can vary considerably, and are affected by surgeon and patient-specific factors. Patients may be of such condition that surgical intervention is not tolerable, or be at a treatment stage where interruption of systemic therapy is undesirable. It is apparent that not all patients with VCF require surgical intervention, though this is difficult to quantify with certainty.
Careful consideration should be given to response assessment posttreatment, as osteoradionecrosis, fibrosis, or VCF can be mistaken for local progression. Thus, biopsy may be required in some cases where local progression is suspected following SBRT.[2,67]
VCF is thus a well-recognized complication of spine SBRT. SINS should always be considered and caution should be taken when considering high-dose single fractions.
Myelopathy
Radiation myelopathy may be the most feared of all potential complications from spine SBRT. Permanent neurological deficit resulting from palliative treatment is a catastrophic outcome, particularly because patients selected for SBRT typically have a reasonable prognosis.
Prospective studies reveal rates of radiation myelopathy between 0% and 3%,[3,23,54] whereas the largest retrospective review to date of 1388 patients revealed a myelopathy rate of 0.4%.[31] However caution should be taken when interpreting these results because myelopathy is a late complication and many patients may have not lived long enough for it to manifest. Furthermore, these rates are based on the utilization of strict dose limitations on spinal cord tolerance.
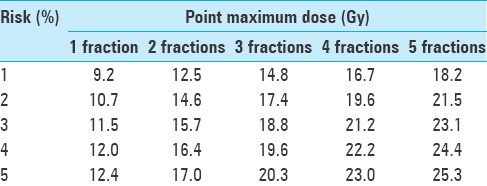
Spinal cord tolerance can be affected by small dose inhomogeneities, and particular attention is paid to the point maximum dose within the spinal cord.[57,58] There is a growing body of evidence regarding safe dose limits. In 2013, Sahgal et al. reported risk estimates for myelopathy following spine SBRT based on 9 reported cases of myelopathy compared with 66 cases without.[61] Using an alpha-beta ratio of 2, spinal cord point maximum doses with estimates of corresponding myelopathy risk are provided in Table 2.
Table 2.
Point maximum doses to spinal cord, categorized by myelopathy risk and fractionation schedule. Adapted with permission[61]
Sahgal et al. analyzed patients re-irradiated with SBRT following conventional external beam treatment.[59] The analysis included 5 patients who had developed radiation myelopathy compared with 14 patients who did not. Following 30–50 Gy of conventional radiotherapy, a cumulative thecal sac point maximum dose of 70 Gy in equivalent 2-Gy-fractions (alpha-beta ratio of 2) was recommended, as long as there were ≥5 months since initial radiotherapy. The point maximum dose for the retreatment course should not exceed 25 Gy in equivalent 2-Gy-fractions.
It is apparent there is a correlation between dose/fractionation and the risk of myelopathy, which needs to be considered when selecting treatment regimens. Treatment and dose constraints applied should be balanced against the likely greater risks of neurological deficit caused by uncontrolled tumor progression.
Pain flare
Acute pain flare occurs more commonly for spine SBRT compared with conventional RT. The onset is typically within days of treatment. Its incidence has been reported as high as 68%, though evidence suggests that the risk of pain flare significantly reduces with increasing fraction number.[9,49]
Standard management for pain flare consists of dexamethasone, with recent evidence suggesting a benefit to prophylactic use. Prophylactic dexamethasone reduces the incidence of pain flare to 19.2% at a dose of 4 mg daily for 5 days, commencing on the day of the first fraction.[38]
Esophageal toxicity
Esophageal toxicity can occur in patients receiving spine SBRT though rates are low, even when target volumes directly abut the eosphagus. Two studies report low rates of esophageal toxicity with 24 Gy single-fraction regimens. Cox et al. found a 1.5% rate of grade 3 or higher acute esophageal toxicity when treating spinal metastases directly abutting the esophagus. The rate of grade 3 late toxicity (stenosis, fistula, or ulcer) was 5%.[13] Gomez et al. found a grade 3 toxicity rate of 1.8% using the same dose/fractionation in the treatment of thoracic structures.[28]
A report of lung and liver SBRT treated to a median dose of 50 Gy in 5 fractions found a grade 3 esophageal toxicity rate of 3.8%. It was postulated that the use of bevazicumab contributed to esophageal toxicity.[62] Of note, the doses used were significantly higher than typically employed in spine SBRT.
Damage to great vessels
Rates of radiotherapy-related complications for the aorta are generally low, and other organ constraints typically take precedence. Xue et al. reported 625 cases treated with SBRT over 1–5 fractions with aorta or major vessel contours. It was not reported how many patients specifically received spine SBRT versus non-spine SBRT sites, though no grade 3 or higher toxicity was observed. The authors’ recommended dose constraints were all higher than typical prescription doses for spine SBRT, suggesting that this complication is unlikely.[72]
QUALITY ASSURANCE
The planning and treatment process for spine SBRT is complex and the potential for serious toxicity has been outlined. A focus on optimizing treatment quality is needed to achieve the favorable rates of local control and toxicity demonstrated in the literature. Multiple factors within each institution need to be considered when assessing its ability to deliver high quality treatment.
Organizational quality
There is international consensus on the need for specialized teams of physicians, physicists, and radiation therapists with SBRT-specific training.[22,40,50,60] In addition, there is multinational expert agreement that spine-specific SBRT credentialing is needed for all involved staff. An in-house supervision program whereby staff are supervised for an initial quota of patients is commonly utilized for credentialing.[26] Institutions should have appropriate guidelines for patient selection, as well as dedicated imaging and image guidance during treatment delivery.[30] The consistency and quality of treatment can be further improved via interinstitutional collaboration, participation in clinical trials, and regular quality assurance peer review rounds.[60]
Planning dosimetric quality
Magnetic resonance imaging (MRI) is a prerequisite. T1 and T2 noncontrast images are recommended, with T2 especially useful for delineating spinal cord/thecal sac and paraspinal disease extension. Slice thickness should be fine at 1–2 millimetres. In the postoperative setting, particular attention should be paid to the preoperative imaging findings, as this is associated with patterns of local recurrence.[7]
Consensus guidelines exist regarding volume definition for upfront and retreatment spine SBRT based on expert recommendations. In general, coverage of the entire vertebral body is recommended unless tumor involves only the lamina, spinous process, or in select cases, the pedicle. This is detailed more comprehensively in the original article by Cox et al.[14]
There is less certainty regarding the target volumes in the postoperative setting, though a recent postoperative review paper recommends image fusion of preoperative scans, utilization of documented operative findings, and direct communication with the surgeon to guide target delineation. CT myelogram can be used where surgical hardware obscures visualization of spinal cord/cauda equina.[51]
Planning Target Volumes (PTV) and Planning organ-at-Risk Volumes (PRV) are required to account for intrafraction movement and setup error, though these can be minimized with appropriate image guidance and correction techniques to approximately 2 mm.[42] An MRI-based intrafraction movement study suggested that a spinal cord PRV of approximately 1.5–2.0 mm may be adequate.[68]
Planning and delivery quality
Near rigid immobilization systems are recommended to minimize intrafraction motion, given the typically steep dose gradients that are generated between the spinal cord and target volume.[44] Treatment machines capable of patient positioning in six degrees of freedom (including translational and rotational) and onboard image guidance systems are needed to accurately deliver dose. Stereoscopic X-rays or three-dimensional volumetric imaging such as cone beam computed tomography (CBCT) should be utilized. Strict tolerance levels for target position are recommended – as low as 1–2 mm of translational variation and 1–2 degrees of rotation – recognizing that the effect of rotational variation may be less significant for small tumor volumes, and more pronounced where multiple vertebral levels are involved.[20,35,70]
Commonly utilized treatment machines include linear accelerators with multileaf collimators and treatment couches capable of fine translational and rotational repositioning, and a linear accelerator mounted on a robotic arm (Cyberknife, Accuray, Sunnyvale, CA, USA). Intensity modulated protons have also been deemed adequate on a dosimetric basis, although these are not widely available.[69]
ONGOING RANDOMIZED TRIALS
Further randomized studies are underway to provide higher quality data for spine SBRT in a variety of treatment scenarios.
To evaluate the role of spine SBRT in the upfront setting, the Canadian Cancer Trials Group (NCIC) are recruiting for a randomized phase 2 study (NCT02512965) comparing spine SBRT with conventional radiotherapy with respect to pain palliation, via regimens of 24 Gy in 2 fractions for SBRT and 20 Gy in 5 fractions for conventional radiotherapy. Along similar lines, the Radiation Therapy Oncology Group (RTOG) are recruiting for a phase III randomized comparison of single-fraction SBRT to single-fraction conventional radiotherapy (NCT00922974, or RTOG 06-31).
For patients deemed at high risk of VCF following spine SBRT, an MD Anderson-based phase 2 study (NCT02387905) is underway to evaluate the efficacy of prophylactic vertebral cement augmentation. If efficacy is demonstrated, this may spare patients from subsequent fracture-related morbidity and additional surgical procedures.
For patients with early spinal cord compression and minor neurological deficits, investigators in Denmark are comparing spine SBRT of 16 Gy in 1 fraction with decompressive surgery and postoperative conventional radiotherapy, with the primary endpoint being the ability to walk at 6 weeks (NCT02167633). If efficacy is demonstrated, some patients may be spared the morbidity of surgery.
To investigate optimal dose and fractionation regimens with respect to local control, the Memorial Sloan Kettering Cancer Center is performing two randomized phase 3 trials comparing single fraction SBRT of 24 Gy with hypofractionated SBRT of 27 Gy in 3 fractions. The first (NCT02320825) is specific to patients in the postoperative spine setting, whereas the second (NCT01223248) includes a variety of metastatic sites including bone, spine, soft tissue, and lymph nodes. With an overall enrolment of 220 patients, spine-specific data will be of interest.
CONCLUSION
Spine SBRT is a highly efficacious and safe treatment in the treatment of spinal tumors in appropriately selected patients, though focus is needed on ensuring treatment quality across a range of domains.
High quality randomized data regarding optimal dose and fractionation is lacking, though the available evidence suggests hypofractionated spine SBRT may have advantages with respect to toxicity when compared with single fraction regimens. This should be considered when evaluating each patient on a case-by-case basis. Ongoing investigation is underway to further guide clinicians’ dose/fractionation decisions.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Footnotes
Contributor Information
Michael Huo, Email: michaelhuo@live.com.au.
Arjun Sahgal, Email: arjun.sahgal@sunnybrook.ca.
David Pryor, Email: david.pryor@health.qld.gov.au.
Kristin Redmond, Email: kjanson3@jhmi.edu.
Simon Lo, Email: simonslo@uw.edu.
Matthew Foote, Email: matthew.foote@health.qld.gov.au.
REFERENCES
- 1.Al-Omair A, Masucci L, Masson-Cote L, Campbell M, Atenafu EG, Parent A, et al. Surgical resection of epidural disease improves local control following postoperative spine stereotactic body radiotherapy. Neurooncology. 2013;15:1413–9. doi: 10.1093/neuonc/not101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Al-Omair A, Smith R, Kiehl TR, Lao L, Yu E, Massicotte EM, et al. Radiation-induced vertebral compression fracture following spine stereotactic radiosurgery: Clinicopathological correlation. J Neurosurg Spine. 2013;18:430–5. doi: 10.3171/2013.2.SPINE12739. [DOI] [PubMed] [Google Scholar]
- 3.Amdur RJ, Bennett J, Olivier K, Wallace A, Morris CG, Liu C, et al. A prospective, phase II study demonstrating the potential value and limitation of radiosurgery for spine metastases. Am J Clin Oncol. 2009;32:515–20. doi: 10.1097/COC.0b013e318194f70f. [DOI] [PubMed] [Google Scholar]
- 4.Anwar M, Barani IJ. Role of stereotactic body radiotherapy in spinal metastasis and subsequent fracture risk: Identifying and treating the at-risk patient. CNS Oncol. 2013;2:437–45. doi: 10.2217/cns.13.31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bilsky MH, Laufer I, Fourney DR, Groff M, Schmidt MH, Varga PP, et al. Reliability analysis of the epidural spinal cord compression scale. J Neurosurg Spine. 2010;13:324–8. doi: 10.3171/2010.3.SPINE09459. [DOI] [PubMed] [Google Scholar]
- 6.Brown JM, Carlson DJ, Brenner DJ. The tumor radiobiology of SRS and SBRT: Are more than the 5 Rs involved? Int J Radiat Oncol Biol Phys. 2014;88(2):254–262. doi: 10.1016/j.ijrobp.2013.07.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chan MW, Thibault I, Atenafu EG, Yu E, John Cho BC, Letourneau D, et al. Patterns of epidural progression following postoperative spine stereotactic body radiotherapy: Implications for clinical target volume delineation. J Neurosurg Spine. 2016;24:652–9. doi: 10.3171/2015.6.SPINE15294. [DOI] [PubMed] [Google Scholar]
- 8.Chang JH, Shin JH, Yamada Y, Mesfin A, Fehlings MG, Rhines LD, et al. Stereotactic Body Radiotherapy for Spinal Metastases: What are the Risks and how do we Minimize Them? Spine. 2016;41(Suppl 20):S238–45. doi: 10.1097/BRS.0000000000001823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chiang A, Zeng L, Zhang L, Lochray F, Korol R, Loblaw A, et al. Pain flare is a common adverse event in steroid-naive patients after spine stereotactic body radiation therapy: A prospective clinical trial. Int J Radiat Oncol Biol Phys. 2013;86:638–42. doi: 10.1016/j.ijrobp.2013.03.022. [DOI] [PubMed] [Google Scholar]
- 10.Choi CY, Adler JR, Gibbs IC, Chang SD, Jackson PS, Minn AY, et al. Stereotactic radiosurgery for treatment of spinal metastases recurring in close proximity to previously irradiated spinal cord. Int J Radiat Oncol Biol Phys. 2010;78:499–506. doi: 10.1016/j.ijrobp.2009.07.1727. [DOI] [PubMed] [Google Scholar]
- 11.Chow E, Harris K, Fan G, Tsao M, Sze WM. Palliative radiotherapy trials for bone metastases: A systematic review. J Clin Oncol. 2007;25:1423–36. doi: 10.1200/JCO.2006.09.5281. [DOI] [PubMed] [Google Scholar]
- 12.Corbin KS, Hellman S, Weichselbaum RR. Extracranial oligometastases: A subset of metastases curable with stereotactic radiotherapy. J Clin Oncol. 2013;31:1384–90. doi: 10.1200/JCO.2012.45.9651. [DOI] [PubMed] [Google Scholar]
- 13.Cox BW, Jackson A, Hunt M, Bilsky M, Yamada Y. Esophageal toxicity from high-dose, single-fraction paraspinal stereotactic radiosurgery. Int J Radiat Oncol Biol Phys. 2012;83:e661–7. doi: 10.1016/j.ijrobp.2012.01.080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cox BW, Spratt DE, Lovelock M, Bilsky MH, Lis E, Ryu S, et al. International Spine Radiosurgery Consortium consensus guidelines for target volume definition in spinal stereotactic radiosurgery. Int J Radiat Oncol Biol Phys. 2012;83:e597–605. doi: 10.1016/j.ijrobp.2012.03.009. [DOI] [PubMed] [Google Scholar]
- 15.Cunha MV, Al-Omair A, Atenafu EG, Masucci GL, Letourneau D, Korol R, et al. Vertebral compression fracture (VCF) after spine stereotactic body radiation therapy (SBRT): Analysis of predictive factors. Int J Radiat Oncol Biol Phys. 2012;84:e343–9. doi: 10.1016/j.ijrobp.2012.04.034. [DOI] [PubMed] [Google Scholar]
- 16.Dahele M, Fehlings MG, Sahgal A. Stereotactic radiotherapy: An emerging treatment for spinal metastases. Can J Neurol Sci. 2011;38:247–50. doi: 10.1017/s0317167100011410. [DOI] [PubMed] [Google Scholar]
- 17.Dahele M, Hatton M, Slotman B, Guckenberger M. Stereotactic body radiotherapy: A survey of contemporary practice in six selected European countries. Acta Oncol. 2015;54:1237–41. doi: 10.3109/0284186X.2014.1003961. [DOI] [PubMed] [Google Scholar]
- 18.Degen JW, Gagnon GJ, Voyadzis JM, McRae DA, Lunsden M, Dieterich S, et al. CyberKnife stereotactic radiosurgical treatment of spinal tumors for pain control and quality of life. J Neurosurg Spine. 2005;2:540–9. doi: 10.3171/spi.2005.2.5.0540. [DOI] [PubMed] [Google Scholar]
- 19.Finnigan R, Burmeister B, Barry T, Jones K, Boyd J, Pullar A, et al. Technique and early clinical outcomes for spinal and paraspinal tumours treated with stereotactic body radiotherapy. J Clin Neurosci. 2015;22:1258–63. doi: 10.1016/j.jocn.2015.01.030. [DOI] [PubMed] [Google Scholar]
- 20.Finnigan R, Lamprecht B, Barry T, Jones K, Boyd J, Pullar A, et al. Inter- and intra-fraction motion in stereotactic body radiotherapy for spinal and paraspinal tumours using cone-beam CT and positional correction in six degrees of freedom. J Med Imaging Radiat Oncol. 2016;60:112–8. doi: 10.1111/1754-9485.12353. [DOI] [PubMed] [Google Scholar]
- 21.Folkert MR, Bilsky MH, Tom AK, Oh JH, Alektiar KM, Laufer I, et al. Outcomes and toxicity for hypofractionated and single-fraction image-guided stereotactic radiosurgery for sarcomas metastasizing to the spine. Int J Radiat Oncol Biol Phys. 2014;88:1085–91. doi: 10.1016/j.ijrobp.2013.12.042. [DOI] [PubMed] [Google Scholar]
- 22.Foote M, Bailey M. Guidelines for safe practice of stereotactic body (ablative) radiation therapy. J Med Imaging Radiat Oncol. 2015;59:646–53. doi: 10.1111/1754-9485.12336. [DOI] [PubMed] [Google Scholar]
- 23.Garg AK, Shiu AS, Yang J, Wang XS, Allen P, Brown BW, et al. Phase 1/2 trial of single-session stereotactic body radiotherapy for previously unirradiated spinal metastases. Cancer. 2012;118:5069–77. doi: 10.1002/cncr.27530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Germano IM, Carai A, Pawha P, Blacksburg S, Lo YC, Green S. Clinical outcome of vertebral compression fracture after single fraction spine radiosurgery for spinal metastases. Clin Exp Metastasis. 2016;33:143–9. doi: 10.1007/s10585-015-9764-8. [DOI] [PubMed] [Google Scholar]
- 25.Gerszten PC, Burton SA, Quinn AE, Agarwala SS, Kirkwood JM. Radiosurgery for the treatment of spinal melanoma metastases. Stereotact Funct Neurosurg. 2005;83:213–21. doi: 10.1159/000091952. [DOI] [PubMed] [Google Scholar]
- 26.Gerszten PC, Sahgal A, Sheehan JP, Kersh R, Chen S, Flickinger JC, et al. A multi-national report on methods for institutional credentialing for spine radiosurgery. Radiat Oncol. 2013;8:158. doi: 10.1186/1748-717X-8-158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ghia AJ, Chang EL, Bishop AJ, Pan HY, Boehling NS, Amini B, et al. Single-fraction versus multifraction spinal stereotactic radiosurgery for spinal metastases from renal cell carcinoma: Secondary analysis of Phase I/II trials. J Neurosurg Spine. 2016;24:829–36. doi: 10.3171/2015.8.SPINE15844. [DOI] [PubMed] [Google Scholar]
- 28.Gomez DR, Hunt MA, Jackson A, O’Meara WP, Bukanova EN, Zelefsky MJ, et al. Low rate of thoracic toxicity in palliative paraspinal single-fraction stereotactic body radiation therapy. Radiother Oncol. 2009;93:414–8. doi: 10.1016/j.radonc.2009.10.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Guckenberger M, Mantel F, Gerszten PC, Flickinger JC, Sahgal A, Letourneau D, et al. Safety and efficacy of stereotactic body radiotherapy as primary treatment for vertebral metastases: A multi-institutional analysis. Radiat Oncol. 2014;9:226. doi: 10.1186/s13014-014-0226-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Guckenberger M, Sweeney RA, Flickinger JC, Gerszten PC, Kersh R, Sheehan J, et al. Clinical practice of image-guided spine radiosurgery-results from an international research consortium. Radiat Oncol. 2011;6:172. doi: 10.1186/1748-717X-6-172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hall WA, Stapleford LJ, Hadjipanayis CG, Curran WJ, Crocker I, Shu HK. Stereotactic body radiosurgery for spinal metastatic disease: An evidence-based review. Int J Surg Oncol 2011. 2011 doi: 10.1155/2011/979214. 979214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hashmi A, Guckenberger M, Kersh R, Gerszten PC, Mantel F, Grills IS, et al. Re-irradiation stereotactic body radiotherapy for spinal metastases: A multi-institutional outcome analysis. J Neurosurg Spine. 2016;25:646–53. doi: 10.3171/2016.4.SPINE151523. [DOI] [PubMed] [Google Scholar]
- 33.Heron DE, Rajagopalan MS, Stone B, Burton S, Gerszten PC, Dong X, et al. Single-session and multisession CyberKnife radiosurgery for spine metastases-University of Pittsburgh and Georgetown University experience. J Neurosurg Spine. 2012;17:11–8. doi: 10.3171/2012.4.SPINE11902. [DOI] [PubMed] [Google Scholar]
- 34.Husain ZA, Thibault I, Letourneau D, Ma L, Keller H, Suh J, et al. Stereotactic body radiotherapy: A new paradigm in the management of spinal metastases. CNS Oncol. 2013;2:259–70. doi: 10.2217/cns.13.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hyde D, Lochray F, Korol R, Davidson M, Wong CS, Ma L, et al. Spine stereotactic body radiotherapy utilizing cone-beam CT image-guidance with a robotic couch: Intrafraction motion analysis accounting for all six degrees of freedom. Int J Radiat Oncol Biol Phys. 2012;82:e555–62. doi: 10.1016/j.ijrobp.2011.06.1980. [DOI] [PubMed] [Google Scholar]
- 36.Jabbari S, Gerszten PC, Ruschin M, Larson DA, Lo SS, Sahgal A. Stereotactic Body Radiotherapy for Spinal Metastases: Practice Guidelines, Outcomes, and Risks. Cancer J. 2016;22:280–9. doi: 10.1097/PPO.0000000000000205. [DOI] [PubMed] [Google Scholar]
- 37.Jain AK, Yamada YJ. The role of stereotactic body radiotherapy and stereotactic radiosurgery in the re-irradiation of metastatic spinal tumors. Exp Rev Anticancer Ther. 2014;14:1141–52. doi: 10.1586/14737140.2014.940326. [DOI] [PubMed] [Google Scholar]
- 38.Khan L, Chiang A, Zhang L, Thibault I, Bedard G, Wong E, et al. Prophylactic dexamethasone effectively reduces the incidence of pain flare following spine stereotactic body radiotherapy (SBRT): A prospective observational study. Support Care Cancer. 2015;23:2937–43. doi: 10.1007/s00520-015-2659-z. [DOI] [PubMed] [Google Scholar]
- 39.Kim MS, Kim W, Park IH, Kim HJ, Lee E, Jung JH, et al. Radiobiological mechanisms of stereotactic body radiation therapy and stereotactic radiation surgery. Radiat Oncol J. 2015;33:265–75. doi: 10.3857/roj.2015.33.4.265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kirkbride P, Burton K, Cassoni A, Cooper T, Eccles C. on behalf of the National SBRT NRIG Subgroup. Stereotactic body radiotherapy, guidelines for commissioners, providers and clinicians in England 2011. National Cancer Action Team, NHS. 2010. [Last accessed on 2016 Jun 12]. Available from: http://www.cancerresearchuk.org/cancer-info/prod_consump/groups/cr_common/@nre/@new/@gen/documents/generalcontent/cr_074729.pdf .
- 41.Laufer I, Iorgulescu JB, Chapman T, Lis E, Shi W, Zhang Z, et al. Local disease control for spinal metastases following “separation surgery” and adjuvant hypofractionated or high-dose single-fraction stereotactic radiosurgery: Outcome analysis in 186 patients. J Neurosurg Spine. 2013;18:207–14. doi: 10.3171/2012.11.SPINE12111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Li W, Sahgal A, Foote M, Millar BA, Jaffray DA, Letourneau D. Impact of immobilization on intrafraction motion for spine stereotactic body radiotherapy using cone beam computed tomography. Int J Radiat Oncol Biol Phys. 2012;84:520–6. doi: 10.1016/j.ijrobp.2011.12.039. [DOI] [PubMed] [Google Scholar]
- 43.Lo SS, Foote M, Siva S, Slotman BJ, Teh BS, Guckenberger M, et al. Technical know-how in stereotactic ablative radiotherapy (SABR) J Med Radiat Sci. 2016;63:5–8. doi: 10.1002/jmrs.163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lo SS, Sahgal A, Chang EL, Mayr NA, Teh BS, Huang Z, et al. Serious complications associated with stereotactic ablative radiotherapy and strategies to mitigate the risk. Clin Oncol. 2013;25:378–87. doi: 10.1016/j.clon.2013.01.003. [DOI] [PubMed] [Google Scholar]
- 45.Lo SS, Sahgal A, Wang JZ, Mayr NA, Sloan A, Mendel E, et al. Stereotactic body radiation therapy for spinal metastases. Discov Med. 2010;9:289–96. [PubMed] [Google Scholar]
- 46.Lo SS, Slotman BJ, Lock M, Nagata Y, Guckenberger M, Siva S, et al. The development of stereotactic body radiotherapy in the past decade: A global perspective. Future Oncol. 2015 doi: 10.2217/fon.15.220. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 47.Moulding HD, Elder JB, Lis E, Lovelock DM, Zhang Z, Yamada Y, et al. Local disease control after decompressive surgery and adjuvant high-dose single-fraction radiosurgery for spine metastases. J Neurosurg Spine. 2010;13:87–93. doi: 10.3171/2010.3.SPINE09639. [DOI] [PubMed] [Google Scholar]
- 48.Moussazadeh N, Lis E, Katsoulakis E, Kahn S, Svoboda M, DiStefano NM, et al. Five-Year Outcomes of High-Dose Single-Fraction Spinal Stereotactic Radiosurgery. Int J Radiat Oncol Biol Phys. 2015;93:361–7. doi: 10.1016/j.ijrobp.2015.05.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Pan HY, Allen PK, Wang XS, Chang EL, Rhines LD, Tatsui CE, et al. Incidence and predictive factors of pain flare after spine stereotactic body radiation therapy: Secondary analysis of phase 1/2 trials. Int J Radiat Oncol Biol Phys. 2014;90:870–6. doi: 10.1016/j.ijrobp.2014.07.037. [DOI] [PubMed] [Google Scholar]
- 50.Potters L, Kavanagh B, Galvin JM, Hevezi JM, Janjan NA, Larson DA, et al. American Society for Therapeutic Radiology and Oncology (ASTRO) and American College of Radiology (ACR) practice guideline for the performance of stereotactic body radiation therapy. Int J Radiat Oncol Biol Phys. 2010;76:326–32. doi: 10.1016/j.ijrobp.2009.09.042. [DOI] [PubMed] [Google Scholar]
- 51.Redmond KJ, Lo SS, Fisher C, Sahgal A. Postoperative Stereotactic Body Radiation Therapy (SBRT) for Spine Metastases: A Critical Review to Guide Practice. Int J Radiat Oncol Biol Phys. 2016;95:1414–28. doi: 10.1016/j.ijrobp.2016.03.027. [DOI] [PubMed] [Google Scholar]
- 52.Redmond KJ, Sahgal A, Foote M, Knisely J, Gerszten PC, Chao ST, et al. Single versus multiple session stereotactic body radiotherapy for spinal metastasis: The risk-benefit ratio. Future Oncol. 2015;11:2405–15. doi: 10.2217/fon.15.160. [DOI] [PubMed] [Google Scholar]
- 53.Rose PS, Laufer I, Boland PJ, Hanover A, Bilsky MH, Yamada J, et al. Risk of fracture after single fraction image-guided intensity-modulated radiation therapy to spinal metastases. J Clin Oncol. 2009;27:5075–9. doi: 10.1200/JCO.2008.19.3508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ryu S, Pugh SL, Gerszten PC, Yin FF, Timmerman RD, Hitchcock YJ, et al. RTOG 0631 phase 2/3 study of image guided stereotactic radiosurgery for localized (1-3) spine metastases: Phase 2 results. Pract Radiat Oncol. 2014;4:76–81. doi: 10.1016/j.prro.2013.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Sahgal A, Ames C, Chou D, Ma L, Huang K, Xu W, et al. Stereotactic body radiotherapy is effective salvage therapy for patients with prior radiation of spinal metastases. Int J Radiat Oncol Biol Phys. 2009;74:723–31. doi: 10.1016/j.ijrobp.2008.09.020. [DOI] [PubMed] [Google Scholar]
- 56.Sahgal A, Atenafu EG, Chao S, Al-Omair A, Boehling N, Balagamwala EH, et al. Vertebral compression fracture after spine stereotactic body radiotherapy: A multi-institutional analysis with a focus on radiation dose and the spinal instability neoplastic score. J Clin Oncol. 2013;31:3426–31. doi: 10.1200/JCO.2013.50.1411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Sahgal A, Ma L, Fowler J, Weinberg V, Gibbs I, Gerszten PC, et al. Impact of dose hot spots on spinal cord tolerance following stereotactic body radiotherapy: A generalized biological effective dose analysis. Technol Cancer Res Treat. 2012;11:35–40. doi: 10.7785/tcrt.2012.500232. [DOI] [PubMed] [Google Scholar]
- 58.Sahgal A, Ma L, Gibbs I, Gerszten PC, Ryu S, Soltys S, et al. Spinal cord tolerance for stereotactic body radiotherapy. International journal of radiation oncology, biology, physics. 2010;77(2):548–553. doi: 10.1016/j.ijrobp.2009.05.023. [DOI] [PubMed] [Google Scholar]
- 59.Sahgal A, Ma L, Weinberg V, Gibbs IC, Chao S, Chang UK, et al. Reirradiation human spinal cord tolerance for stereotactic body radiotherapy. Int J Radiat Oncol Biol Phys. 2012;82:107–16. doi: 10.1016/j.ijrobp.2010.08.021. [DOI] [PubMed] [Google Scholar]
- 60.Sahgal A, Roberge D, Schellenberg D, Purdie TG, Swaminath A, Pantarotto J, et al. The Canadian Association of Radiation Oncology scope of practice guidelines for lung, liver and spine stereotactic body radiotherapy. Clin Oncol. 2012;24:629–39. doi: 10.1016/j.clon.2012.04.006. [DOI] [PubMed] [Google Scholar]
- 61.Sahgal A, Weinberg V, Ma L, Chang E, Chao S, Muacevic A, et al. Probabilities of radiation myelopathy specific to stereotactic body radiation therapy to guide safe practice. Int J Radiat Oncol Biol Phys. 2013;85:341–7. doi: 10.1016/j.ijrobp.2012.05.007. [DOI] [PubMed] [Google Scholar]
- 62.Stephans KL, Djemil T, Diaconu C, Reddy CA, Xia P, Woody NM, et al. Esophageal dose tolerance to hypofractionated stereotactic body radiation therapy: Risk factors for late toxicity. Int J Radiat Oncol Biol Phys. 2014;90:197–202. doi: 10.1016/j.ijrobp.2014.05.011. [DOI] [PubMed] [Google Scholar]
- 63.Tang C, Hess K, Bishop AJ, Pan HY, Christensen EN, Yang JN, et al. Creation of a Prognostic Index for Spine Metastasis to Stratify Survival in Patients Treated With Spinal Stereotactic Radiosurgery: Secondary Analysis of Mature Prospective Trials. Int J Radiat Oncol Biol Phys. 2015;93:118–25. doi: 10.1016/j.ijrobp.2015.04.050. [DOI] [PubMed] [Google Scholar]
- 64.Tao R, Bishop AJ, Brownlee Z, Allen PK, Settle SH, Chang EL, et al. Stereotactic Body Radiation Therapy for Spinal Metastases in the Postoperative Setting: A Secondary Analysis of Mature Phase 1-2 Trials. Int J Radiat Oncol Biol Phys. 2016;95:1405–13. doi: 10.1016/j.ijrobp.2016.03.022. [DOI] [PubMed] [Google Scholar]
- 65.Thibault I, Al-Omair A, Masucci GL, Masson-Cote L, Lochray F, Korol R, et al. Spine stereotactic body radiotherapy for renal cell cancer spinal metastases: Analysis of outcomes and risk of vertebral compression fracture. J Neurosurg Spine. 2014;21:711–8. doi: 10.3171/2014.7.SPINE13895. [DOI] [PubMed] [Google Scholar]
- 66.Thibault I, Campbell M, Tseng CL, Atenafu EG, Letourneau D, Yu E, et al. Salvage Stereotactic Body Radiotherapy (SBRT) Following In-Field Failure of Initial SBRT for Spinal Metastases. Int J Radiat Oncol Biol Phys. 2015;93:353–60. doi: 10.1016/j.ijrobp.2015.03.029. [DOI] [PubMed] [Google Scholar]
- 67.Thibault I, Chang EL, Sheehan J, Ahluwalia MS, Guckenberger M, Sohn MJ, et al. Response assessment after stereotactic body radiotherapy for spinal metastasis: A report from the SPIne response assessment in Neuro-Oncology (SPINO) group. Lancet Oncol. 2015;16:e595–603. doi: 10.1016/S1470-2045(15)00166-7. [DOI] [PubMed] [Google Scholar]
- 68.Tseng CL, Sussman MS, Atenafu EG, Letourneau D, Ma L, Soliman H, et al. Magnetic resonance imaging assessment of spinal cord and cauda equina motion in supine patients with spinal metastases planned for spine stereotactic body radiation therapy. Int J Radiat Oncol Biol Phys. 2015;91:995–1002. doi: 10.1016/j.ijrobp.2014.12.037. [DOI] [PubMed] [Google Scholar]
- 69.van Mourik AM, Elkhuizen PH, Minkema D, Duppen JC, van Vliet-Vroegindeweij C. Multiinstitutional study on target volume delineation variation in breast radiotherapy in the presence of guidelines. Radiother Oncol. 2010;94:286–91. doi: 10.1016/j.radonc.2010.01.009. [DOI] [PubMed] [Google Scholar]
- 70.Wang H, Shiu A, Wang C, O’Daniel J, Mahajan A, Woo S, et al. Dosimetric effect of translational and rotational errors for patients undergoing image-guided stereotactic body radiotherapy for spinal metastases. Int J Radiat Oncol Biol Phys. 2008;71:1261–71. doi: 10.1016/j.ijrobp.2008.02.074. [DOI] [PubMed] [Google Scholar]
- 71.Wang XS, Rhines LD, Shiu AS, Yang JN, Selek U, Gning I, et al. Stereotactic body radiation therapy for management of spinal metastases in patients without spinal cord compression: A phase 1-2 trial. Lancet Oncol. 2012;13:395–402. doi: 10.1016/S1470-2045(11)70384-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Xue J, Kubicek G, Patel A, Goldsmith B, Asbell SO, LaCouture TA. Validity of Current Stereotactic Body Radiation Therapy Dose Constraints for Aorta and Major Vessels. Semin Radiat Oncol. 2016;26:135–9. doi: 10.1016/j.semradonc.2015.11.001. [DOI] [PubMed] [Google Scholar]


