Abstract
Purpose:
To compare the anterior segment indices measured by two Scheimpflug camera machines; Galilei and Pentacam.
Methods:
In this observational case series, the anterior segment indices of myopic healthy subjects seeking for refractive surgery were measured by Pentacam and Galilei on the same day. Analyzed parameters were anterior and posterior best fit spheres (BFS), axial curvature, true corneal power, central corneal thickness (CCT), anterior chamber (AC) depth, AC volume, AC angle, and pupil diameter.
Results:
This study included 176 eyes of 88 participants. Mean radius of the anterior BFS was 7.79 ± 0.34 mm versus 7.75 ± 0.39 mm measured by Pentacam and Galilei, respectively (r = 0.877, P < 0.001). Corresponding values for the mean radius of posterior BFS were 6.42 ± 0.32 and 6.47 ± 0.38 mm, respectively (r = 0.879, P < 0.001). Anterior corneal mean power was 43.8 ± 1.9 diopters (D) with Pentacam and 43.8 ± 2.4 D with Galilei (r = 0.905,P < 0.001). Posterior corneal mean power was measured − 6.3 ± 0.3 and − 6.3 ± 0.4 D using Pentacam and Galilei, respectively (r = 0.873, P < 0.001). True corneal power was 43.9 ± 1.9 D with Pentacam and 43.5 ± 2.3 D with Galilei (r = 0.909, P < 0.001). CCT was 537 ± 44 and 553 ± 51 μm measured by Pentacam and Galilei, respectively (r = 0.796, P < 0.001). AC depth measurements using Pentacam and Galilei were 3.29 ± 0.4 and 3.3 ± 0.38 mm (P < 0.001), respectively; AC volume was 207 ± 50 and 129 ± 39 mm3≥ (P = 0.004), and AC angle was 39.7 ± 9.2 and 54.2 ± 5.2 degrees (P = 0.051), respectively. Average pupil diameter was measured 3.91 ± 1.77 mm by Pentacam and 3.34 ± 0.89 mm by Galilei (P = 0.018).
Conclusions:
There was a significant correlation between the Pentacam and Galilei in all measured parameters except AC angle, AC volume, and average pupil diameter.
Keywords: Scheimpflug Analyzer, Corneal Imaging, Galilei, Pentacam
INTRODUCTION
During the past two decades, incredible advances were made in refractive surgery to improve the results and reduce the complications of this procedure. Determining the exact topographic and pachymetric maps of the cornea is a fundamental diagnostic step for refractive surgery. Additionally, accurate corneal elevation measurements are helpful in diagnosis of corneal ectatic disorders, avoiding the complications of refractive surgery, and monitoring the postoperative recovery of the cornea.[1] Refractive surgeons use some defined criteria to diagnose the keratoconus suspects, who should not be considered as candidates for refractive surgery.
Many types of instruments are available to measure the anterior segment parameters. Recently, Scheimpflug imaging devices have become commercially available for anterior segment measurements. The Pentacam Scheimpflug analyzer (Oculus Optikgerate GmbH, Wetzlar, Germany) uses a single Scheimpflug camera to acquire multiple photographs of the anterior segment of the eye.[2,3,4,5,6] The Galilei dual-Scheimpflug analyzer (V4.01 Ziemer, Port, Switzerland) uses dual Scheimpflug cameras and a Placido disk to improve the accuracy of corneal power and pachymetric measurements. There is no gold standard for corneal topography to check the accuracy of in vivo measurements. It seems that the Scheimpflug technology is superior to the Placido-based corneal topography because it can measure parameters beyond the anterior corneal surface including corneal thickness and posterior curvature with high precision. In addition, Scheimpflug tomography may provide more precise anterior and posterior corneal measurements, compared with the first commercially available tomography scanning slit systems (Orbscan).[7]
Both Pentacam and Galilei use Scheimpflug imaging technology; however they have significant differences in regards to hardware and software. There are few papers comparing these two Scheimpflug systems. The aim of this study was to investigate the agreement between the measurements obtained by the Pentacam and Galilei analyzers in a large number of normal eyes.
METHODS
This observational case series included consecutive subjects with compound myopic astigmatism who were evaluated for refractive surgery. The study was conducted at Labbafinejad Medical Center affiliated to Shahid Beheshti University of Medical Sciences, Tehran, Iran. Subjects with myopia between −1.0 to −8.0 diopters (D) and maximum astigmatism of −3.0 D with a stable refractive error for at least one year were enrolled. Complete ophthalmic examinations were performed in all participants. The subjects had neither contraindications for corneal refractive surgery nor a history of previous ocular surgery.
The Pentacam and Galilei analyzers were used to obtain the measurements in all subjects. The order of the examination by each device was randomly chosen according to a random number sequence (dichotomy sequence, 0 and 1). The maximum test interval was one hour. All tests were performed in the refractive surgery clinic of the hospital by an experienced technician between 8:00 to 12:00 A.M. A signed informed consent was obtained after the purposes of the study were clearly explained to the participants. The study adhered to the tenets of the Declaration of Helsinki.
The systems take images of all anterior segment structures (cornea, iris, pupil, anterior chamber, and lens) to evaluate and analyze the corneal curvature, thickness and elevation, pupil size, and anterior chamber parameters (depth, volume, and angle). The Pentacam system uses a rotating Scheimpflug camera and a monochromatic slit-light source (blue light-emitting diode [LED] at 475 nm). The camera rotates around the optical axis of the eye to calculate a 3-dimensional (3D) model of the anterior segment. Overall, 138,000 true elevation points are recorded.[8] The Galilei uses a dual rotating Scheimpflug camera integrated with a Placido topographer. The flash illumination is emitted from a 475 nm wavelength blue ultraviolet free LED and it measures more than 122,000 data points per scan.
The following parameters were evaluated:
Anterior and Posterior Elevation (Best-Fit Sphere [BFS])
Our measurements were conducted over an analyzed area of 8.0 mm. Schiempflug technology allows for the acquisition of the spatial coordinates of multiple points from both the anterior and posterior corneal surfaces. The colors on the elevation map represent the height of the analyzed corneal surface with respect to a references surface (BFS).[9] The corresponding radius of the BFS was evaluated in the present study.
Corneal Curvature
Corneal curvature was measured at both anterior and posterior surfaces over the central 3.0 and 4.0-mm zones by the Pentacam and Galilei devices, respectively. In our study, mean values were measured from limbus to limbus and are automatically reported in concentric rings of 1.0 mm increments. Curvature can be reported in millimeters or diopters. Dioptric power maps are produced by converting the radius of the curvature into diopter using various refractive indices. Axial power is clinically useful because it relates the corneal power to the corneal shape.[5]
True Corneal Net Power
The total corneal power displayed on the Galilei is calculated by ray tracing through the anterior and posterior corneal surfaces using the Snell law with real refraction index numbers (1 for air, 1.376 for cornea, and 1.336 for aqueous humour). Total corneal power at the central zone (0.0 to 4.0 mm) was evaluated. This parameter is termed as “total corneal refractive power” by the Pentacam device and as “total corneal power” by the OCT. The unit of measurement is the prism diopter.[10]
Central Corneal Thickness (CCT)
Corneal thickness is available for the entire cornea, limbus to limbus; although data are often not available for the full surface. The default standard is to report pachymetry using the pupil center as the reference point. Central corneal thickness is reported for the pupil center and the corneal vertex.[5]
Anterior Chamber Volume
Integral calculus is used to calculate anterior chamber volume as a solid bounded by the posterior surface of the cornea (12.0 mm around the corneal vertex) and the iris and the lens.[5]
Anterior Chamber Depth
Anterior chamber depth is calculated from the corneal endothelium in line with the corneal vertex to the anterior surface of the lens. Anterior chamber depth can also be calculated from the corneal epithelium by changing the settings of the machine.[5] In the present study, the anterior chamber depth was measured from the endothelium.
Anterior Chamber Angle
As a default, the angle of anterior chamber is considered as a less than two angle horizontal size in the topographic corneal maps. Machine settings can be changed to display the superior, inferior, temporal, or nasal angle measurements.[5]
Pupil Diameter
Pupil diameter is averaged over the duration of the scan, and the value that appears in the output is the mean diameter of the pupil. The x and y Cartesian coordinates give the horizontal and vertical positions of the pupil center in relation to the corneal vertex.
Statistical Analysis
To describe data, we used frequency (percent), mean ± SD, median, range, and 95% confidence interval (95% CI). To evaluate the difference between the two sets, we used 95% CI of difference and paired t-test. Pearson correlation was utilized to evaluate the correlation between two sets. The Bland-Altman graphs were used to determine 95% limits of agreement (95% LOA) between the measurements by Pentacam and Galilei analyzers. All statistical analyses were performed by SPSS software (Version 17.0, SPSS Inc., Chicago, IL, USA) and P-value less than 0.05 was considered as statistically significant.
RESULTS
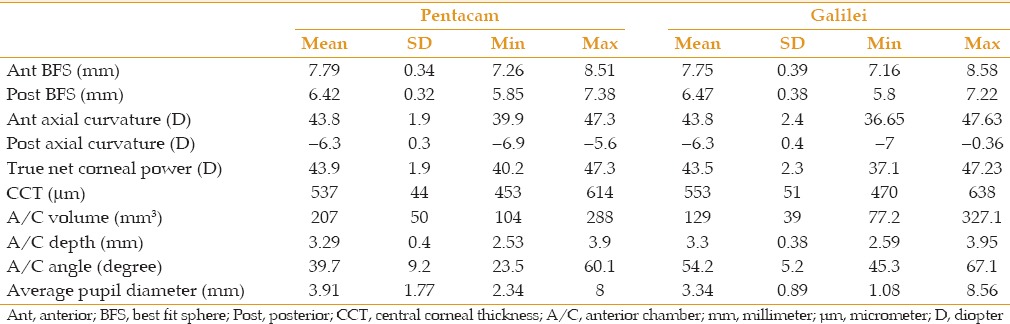
One hundred and seventy-six eyes of 88 subjects (38 male and 50 female subjects) were included. Mean age of the participants was 35 (range, 30–40) years. The measurements by the Pentacam and Galilei analyzers are presented in Table 1.
Table 1.
Corneal and anterior segment parameters measured by the Pentacam and Galilei
Anterior BFS
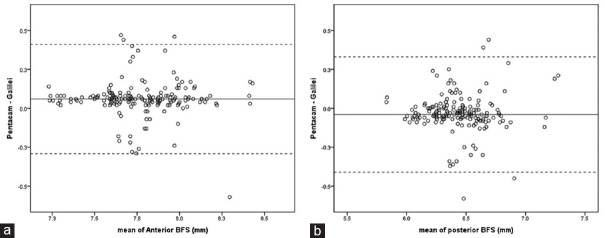
The difference between the two systems in anterior BFS was shown in Table 2. The correlation was significant and it seems that we can use two devices interchangeably with respect to the range of 95% LOA (−0.29 to 0.41 mm). Bland–Altman plot shows a good level of agreement between Pentacam and Galilei [Figure 1a].
Table 2.
Comparisons of corneal and anterior segment parameters measured by the Pentacam versus Galilei parameters

Figure 1.
Bland-Altman plots of anterior and posterior BFS. (a) The dotted lines enclose differences of Ant- BFS from the upper and the lower 95% LOA. The middle line represents mean differences between the results of Pentacam and Galilei values. (b) The dotted lines enclose differences of Post-BFS from the upper and the lower 95% LOA (±1.96 SD). The middle line represents mean differences between the results of Pentacam and Galilei values. BFS, Best-fit sphere; Ant, Anterior; Post, Posterior; LOA, limit of agreement; SD, standard deviation.
Posterior BFS
There was a significant correlation between Pentacam and Galilei measurements in posterior BFS. The 95% LOA was − 0.41 to 0.33 mm, indicating a good agreement between two devices. Bland–Altman plot shows the same result [Figure 1b].
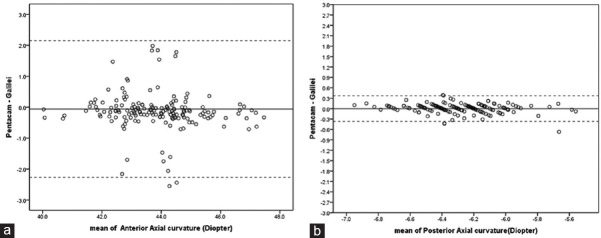
Axial Curvatures
Difference between Pentacam and Galilei in anterior corneal curvature measurements was statistically significant. Despite a significant correlation between the two devices, the range of 95% LOA was wide (−2.27 to 2.15 D); therefore the two devices could not be used interchangeably. There was no significant difference in posterior axial curvature measurements. There was a strong correlation between Pentacam and Galilei in posterior axial curvature measurements with a narrow range of 95% LOA (−0.37 to 0.37 D) [Figure 2a and b].
Figure 2.
Bland-Altman plots of anterior and posterior axial curvature. (a) The dotted lines enclose differences of anterior axial curvature from the upper and the lower 95% LOA (±1.96 SD). The middle line represents mean differences between the results of Pentacam and Galilei values. (b) The dotted lines enclose differences of posterior axial curvature from the upper and the lower 95% LOA (±1.96 SD). The middle line represents mean differences between the results of Pentacam and Galilei values. LoA, limit of agreement; SD, standard deviation.
True Net Corneal Power
Mean difference of true net corneal power was significant between Pentacam and Galilei. The 95% LOA varied from −1.45 to 2.27 D. Due to the importance of this parameter, it seems that this difference cannot be accepted for total corneal power [Figure 3].
Figure 3.

Bland-Altman plots of net corneal power. The dotted lines enclose differences from the upper and the lower 95% LOA (±1.96 SD). The middle line represents mean differences between the results of Pentacam and Galilei values. LOA, limit of agreement; SD, standard deviation.
Central Corneal Thickness (CCT)
Mean CCT measured by the Galilei was significantly thicker than that measured by the Pentacam. There was a strong correlation between the Pentacam and Galilei CCT measurements; however the range of 95% LOA was relatively wide(−62 to 31 µm) [Figure 4].
Figure 4.
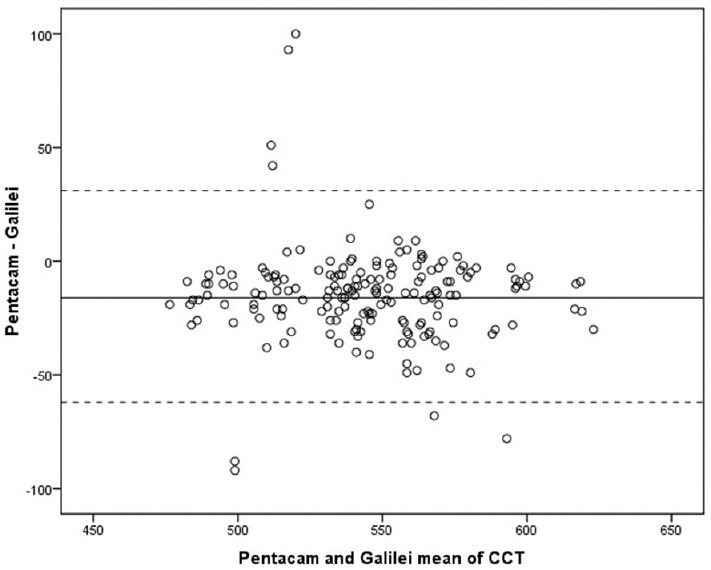
Bland-Altman plots of central corneal thickness. The dotted lines enclose differences from the upper and the lower 95% LOA (±1.96 SD). The middle line represents mean differences between the results of Pentacam and Galilei values. LOA, limit of agreement; SD, standard deviation.
Anterior Chamber Volume
Mean difference of anterior chamber volume between Pentacam and Galilei was significant (P < 0.001). Additionally, the correlation between the two systems was weak in terms of anterior chamber volume (95% LOA, −31.2 to 187.5 mm3).
Anterior Chamber Depth
There was no significant difference between Pentacam and Galilei measurements in terms of the anterior chamber depth. There was a significant correlation between the two sets with an acceptable range of 95% LOA (−0.44 to 0.42 mm).
Anterior Chamber Angle
Mean difference of anterior chamber angle was significant between the two devices. There was a weak correlation between Pentacam and Galilei measurement with respect to anterior chamber angle. The range of 95% LOA was −34.5 to 5.5 degrees.
Average Pupil Diameter
Pupil diameter values measured by the Pentacam and Galilei were comparable. The correlation between the two measurements was also weak and the 95% LOA was between −2.97 and 4.01 mm.
DISCUSSION
In the present study, we demonstrated that there was a strong agreement between Pentacam and Galilei systems in anterior and posterior BFS. We found a good agreement between the two systems in posterior corneal curvature measurements but not in anterior corneal curvature. Only two studies compared the elevation data of Pentacam with those by Galilei.[8,10] They found a good agreement between the single and dual Scheimpflug systems in central but not peripheral elevation data.[8] Aramberri et al found a better agreement for most of the parameters in anterior corneal surface than posterior corneal surface between these two devices.[10] However, they reported a significant difference in anterior, posterior, and total corneal curvature repeatability and reproducibility between the two systems. They mentioned that single camera device was approximately two times more precise than the dual camera device for all curvature parameters.[10]
Measurement of the exact corneal power is very valuable in calculation of the intraocular lens (IOL) power, especially after refractive surgery. Regarding the 95% LOA, our results showed that these systems cannot be used interchangeably to determine the net corneal power. Aramberri et al found a significant difference (1.58 D) between the total corneal refractive power measured by single and dual camera Scheimpflug devices.[10] Kawamorita et al reported moderate agreement between rotating Scheimpflug tomographer and scanning-slit topography for total corneal power.[7] Our findings demonstrated that there was a significant correlation between the two devices in terms of the total corneal power, but the level of agreement was not acceptable. Anayol et al noticed that simK measurements from Galilei, Pentacam and Sirius devices produced significantly different mean values. They also showed that Galilei and Sirius systems demonstrated better agreement with each other than with Pentacam.[11] Thus, although the names and definitions in the software of the two devices are similar, they have different parameters in reality, which is necessary to pay attention while applying them. The difference observed among different studies can be attributed to the various software versions used in each study. In new version of the Galilei analyzer, the optical reference plane for the definition of total corneal power was changed to the anterior corneal surface which can reduce the values calculated using the previous software versions by approximately 3%.[10,11]
Accurate measurement of CCT is of importance for diagnosis of different corneal pathologies and accurate evaluation of the intraocular pressure. Anayol et al compared the central corneal thickness and the thinnest corneal measurement among Galilei, Pentacam and Sirius devices and observed that pachymetry measurements obtained by different devices cannot be used interchangeably.[11] They found that the measurements by the Galilei were significantly higher than those obtained by either the Sirius or the Pentacam systems and showed that Pentacam and Sirius systems demonstrated better agreement with each other than with the Galilei, comparable to the findings reported by Huang et al.[11,12] Jahadi Hosseini et al found a good correlation and agreement amongst Galilei, Pentacam and ultrasound pachymetry in corneal thickness measurement. Measured corneal thickness by Pentacam was less than that by Galilei.[13] Aramberri et al showed that central and thinnest point measurements by a dual-camera device were more precise than that by a single-camera device. Compared with other technologies, the precision of Scheimpflug tomographers seems similar to or slightly better than that of ultrasound and scanning-slit tomography.[10] We found that Galilei always recorded higher amounts of central corneal thickness than Pentacam. Despite the high correlation, the range of 95% LOA (−62 to 31 µm) is wide. Since CCT is very important for decision making for refractive surgery, these two systems cannot be used interchangeably.
In addition to the data obtained regarding the cornea, these two systems provide important data about the anterior chamber. Salouti et al compared AC depth values measured by Galilei, Pentacam, and Orbscan II in healthy individuals. They found that Orbscan overestimated AC depth compared to Galilei and Pentacam. However, the results by the Pentacam and Galilei systems were comparable and could be used interchangeably.[14] Aramberi et al and Wang et al also showed a good level of agreement between the two Scheimpflug devices in AC depth measurements.[10,15] The results of the current study similarly showed a significant correlation between Pentacam and Galilei with respect to the AC depth. In contrast with our findings, Anayol et al found a significant difference in AC depth values obtained by the Galilei, Pentacam, and Sirius. They concluded that Galilei yielded greater values for AC depth in comparison with other two devices and suggested that these three devices cannot be used interchangeably.[11] Domínguez-Vicent et al found that Galilei produced significantly lower AC depth measurements than Pentacam; however this range is not clinically relevant to the IOL power calculation. Therefore, they believed that these devices can be used interchangeably to calculate IOL power, but not to predict the IOL vault.[16]
Domínguez-Vicent et al reported that Pentacam measured significantly higher pupil diameter values than Galilei. Furthermore, their results revealed that Pentacam produced significantly greater C angle values than Galilei and concluded that these two devices could not be used interchangeably.[16] In a study by Shankar et al, pupil measurements by Pentacam had poor repeatability.[5] In our study, there was not any correlation between the two systems regarding the AC angle, the AC volume and the mean pupil diameter. Another significant finding of the current study is that Galilei system always yields smaller AC volumes despite greater AC angle values and comparable AC depth values as compared with Pentacam.
In summary, the two systems had a high level of correlation and agreement with respect to the anterior and posterior BFS, posterior axial curvature and AC depth. Regarding the 95% LOA calculated for central corneal thickness and net corneal power, considering 95% LOA, the two systems should not be used interchangeably. AC angle, AC volume, and average pupil diameter measured by the two devices had no significant correlations. This discrepancy may be due to different software used by each device. Despite significant differences, some parameters measured by the Pentacam were significantly correlated with those measured by the Galilei. This finding indicates that there is a systematic error between Pentacam and Galilei, it may be due to the mechanism of image capturing. This means that the measurements by Pentacam can be changed into those by Galilei using coefficients. Future studies are warranted to determine these correction factors.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Ciolino JB, Khachikian SS, Cortese MJ, Belin MW. Long-term stability of the posterior cornea after laser in situ keratomileusis. J Cataract Refract Surg. 2007;33:1366–1370. doi: 10.1016/j.jcrs.2007.04.016. [DOI] [PubMed] [Google Scholar]
- 2.Barkana Y, Gerber Y, Elbaz U, Schwartz S, Ken-Dror G, Avni I, et al. Central corneal thickness measurement with the Pentacam Scheimpflug system, optical low-coherence reflectometry pachymeter, and ultrasound pachymetry. J Cataract Refract Surg. 2005;31:1729–1735. doi: 10.1016/j.jcrs.2005.03.058. [DOI] [PubMed] [Google Scholar]
- 3.O’Donnell C, Maldonado-Codina C. Agreement and repeatability of central thickness measurement in normal corneas using ultrasound pachymetry and the OCULUS Pentacam. Cornea. 2005;24:920–924. doi: 10.1097/01.ico.0000157422.01146.e9. [DOI] [PubMed] [Google Scholar]
- 4.Amano S, Honda N, Amano Y, Yamagami S, Miyai T, Samejima T, et al. Comparison of central corneal thickness measurements by rotating Scheimpflug camera, ultrasonic pachymetry, and scanning-slit corneal topography. Ophthalmology. 2006;113:937–941. doi: 10.1016/j.ophtha.2006.01.063. [DOI] [PubMed] [Google Scholar]
- 5.Shankar H, Taranath D, Santhirathelagan CT, Pesudovs K. Anterior segment biometry with the Pentacam: Comprehensive assessment of repeatability of automated measurements. J Cataract Refract Surg. 2008;34:103–113. doi: 10.1016/j.jcrs.2007.09.013. [DOI] [PubMed] [Google Scholar]
- 6.Shankar H, Taranath D, Santhirathelagan CT, Pesudovs K. Repeatability of corneal first-surface wavefront aberrations measured with Pentacam corneal topography. J Cataract Refract Surg. 2008;34:727–734. doi: 10.1016/j.jcrs.2007.11.056. [DOI] [PubMed] [Google Scholar]
- 7.Kawamorita T, Uozato H, Kamiya K, Bax L, Tsutsui K, Aizawa D, et al. Repeatability, reproducibility, and agreement characteristics of rotating Scheimpflug photography and scanning-slit corneal topography for corneal power measurement. J Cataract Refract Surg. 2009;35:127–133. doi: 10.1016/j.jcrs.2008.10.019. [DOI] [PubMed] [Google Scholar]
- 8.Salouti R NM, Zamani M, Hafrkonandeh Fard A, Niknam S. Comparison of anterior and posterior elevation map measurements between 2 Scheimpflug imaging systems. J Cataract Refract Surg. 2009;35:856–862. doi: 10.1016/j.jcrs.2009.01.008. [DOI] [PubMed] [Google Scholar]
- 9.Carins G, McGhee CN. orbscan computerized topography: Attributes, application, and limitation. J Cataract Refract Surg. 2005;31:205–220. doi: 10.1016/j.jcrs.2004.09.047. [DOI] [PubMed] [Google Scholar]
- 10.Aramberri J, Araiz L, Garcia A, Illarramendi I, Olmos J, Oyanarte I, et al. Dual versus single Scheimpflug camera for anterior segment analysis: Precision and agreement. J Cataract Refract Surg. 2012;38:1934–1949. doi: 10.1016/j.jcrs.2012.06.049. [DOI] [PubMed] [Google Scholar]
- 11.Anayol M, Güler E, Yagci R, Şekeroğlu MA, Ylmazoğlu M, Trhş H, et al. Comparison of Central Corneal Thickness, Thinnest Corneal Thickness, Anterior Chamber Depth, and Simulated Keratometry Using Galilei, Pentacam, and Sirius Devices. Cornea. 2014;33:582–586. doi: 10.1097/ICO.0000000000000119. [DOI] [PubMed] [Google Scholar]
- 12.Huang J, Ding X, Savini G, Pan C, Feng Y, Cheng D, et al. A comparison between Scheimpflug imaging and optical coherence tomography in measuring corneal thickness. Ophthalmology. 2013;120:1951–1958. doi: 10.1016/j.ophtha.2013.02.022. [DOI] [PubMed] [Google Scholar]
- 13.Jahadi Hosseini HR, Katbab A, Khalili MR, Abtahi MB. Comparison of corneal thickness measurements using Galilei, HR Pentacam, and ultrasound. Cornea. 2010;29:1091–1095. doi: 10.1097/ICO.0b013e3181cf98e5. [DOI] [PubMed] [Google Scholar]
- 14.Salouti R, Nowroozzadeh MH, Zamani M, Ghoreyshi M. Comparison of anterior chamber depth measurements using Galilei, HR Pentacam, and Orbscan II. Optometry. 2010;81:35–39. doi: 10.1016/j.optm.2009.04.100. [DOI] [PubMed] [Google Scholar]
- 15.Wang Q, Ding X, Savini G, Chen H, Feng Y, Pan C, et al. Anterior chamber depth measurements using Scheimpflug imaging and optical coherence tomography: Repeatability, reproducibility, and agreement. J Cataract Refract Surg. 2015;41:178–185. doi: 10.1016/j.jcrs.2014.04.038. [DOI] [PubMed] [Google Scholar]
- 16.Domínguez-Vicent A, MonsálVez-romín D, Aguila-Carrasco AJ, García-Lázaro S, Montés-Micó R. Measurements of anterior chamber depth, white-to-white distance, anterior chamber angle, and pupil diameter using two Scheimpflug imaging devices. Arq Bras Oftalmol. 2014;77:233–237. doi: 10.5935/0004-2749.20140060. [DOI] [PubMed] [Google Scholar]