Abstract
Purpose:
To evaluate the correlation between visual field index (VFI) and both structural and functional measures of the optic disc in primary open angle glaucoma patients and suspects.
Methods:
In this retrospective study, 162 glaucoma patients and suspects underwent standard automated perimetry (SAP), retinography, and retinal nerve fiber layer (RNFL) measurement. The optic disc was stratified according to the vertical cup/disc ratio (C/D) and sorted by the disc damage likelihood scale (DDLS). RNFL was measured with the optical coherence tomography. The VFI perimetry was correlated with the mean deviation (MD) and pattern standard deviation (PSD) obtained by SAP, and structural parameters by Pearson's correlation coefficients.
Results:
VFI displayed strong correlation with MD (R = 0.959) and PSD (R = −0.744). The linear correlations between VFI and structural measures including C/D (R = −0.179, P = 0.012), DDLS (R = −0.214, P = 0.006), and RNFL (R = 0.416, P < 0.001) were weak but statistically significant.
Conclusion:
VFI showed a strong correlation with MD and PSD but demonstrated a weak correlation with structural measures. It can possibly be used as a marker for functional impairment severity in patients with glaucoma.
Keywords: Glaucoma, Perimetry, Visual Field, Optic Disc, Disease Progression
INTRODUCTION
Glaucoma is characterized by progressive optic neuropathy with slowly progressive degeneration of retinal ganglion cells and their axons resulting in a distinct appearance of the optic disc and a concomitant pattern of visual loss.[1] On clinical grounds, evaluation of the optic disc and retinal nerve fiber layer (RNFL) (structural assessment) and the visual field testing (functional assessment) are employed for diagnosis and staging of the disease.
The mean deviation from standard automated perimetry is generally used to evaluate glaucoma progression. Since it can be affected by media opacity, a new functional index has been developed. The visual field index (VFI) is a new global metric that represents the entire visual field as a single number. It is estimated by calculating age corrected defect depth at the test points identified as significantly depressed in pattern deviation probability maps. The valid operating range for pattern deviation analysis is estimated. When exceeding this range, the total deviation probability maps are used for identification of significantly depressed points. VFI is expressed in percentage, where 100% represents a normal visual field and 0% represents a perimetrically blind field, and is plotted versus patient age.[2] Using a linear regression model of consecutive automated perimetry exams, one can appreciate the trend of visual field loss over time and assess the glaucoma functional progression.
The correlation between structure and function in glaucoma is controversial. The weight of evidence points to a linear relationship between the number of retinal cells and retinal sensitivity outside the central 15°.[3] The spatial relationship between the measurements, the variables tested, and the study selection bias may account for the differences.
The relationship between VFI and other structural/functional measures has not been studied extensively.[4,5] Hence, the purpose of this study was to evaluate the correlation between VFI with both structural – clinical subjective measures of the optic disc and the RNFL thickness – and functional variables – mean deviation (MD) and pattern standard deviation (PSD) from automated perimetry.
METHODS
Study population
This retrospective, observational, cross-sectional study included patients with primary open angle glaucoma (POAG) and glaucoma suspects older than 40 years of age of both genders, with 20/20 best corrected visual acuity, and any ethnicity from the clinical practice of one of the authors (NK). Subjects with cataracts or any other ocular diseases and previous incision or laser surgery for glaucoma were not included in the study. The Institution Ethics Committee approved the study and the procedures adhered to the principles of the Declaration of Helsinki in 1964 (amended by the 59th WMA General Assembly, Seoul, Korea, October 2008). The charts of all eligible subjects were reviewed in order to make sure they fulfilled the inclusion criteria. All data for the study were extracted by two of the authors (NAI and RAG). In order to be included in the study, POAG patients had to have typical optic disc damage (diffuse or localized rim thinning, enlarged cupping, disc hemorrhage, asymmetry in cup-to-disc (C/D) ratio of 0.2 or greater between eyes) with corresponding visual field loss on a reliable perimetry exam (at least 3 adjacent points in an expected location of the central 24° field that had P value <5% on the pattern deviation plot, one of which with P <1%; glaucoma hemifield test “outside normal limits”; PSD with a P value <5%), and open angles on gonioscopy. Perimetry was considered reliable if fixation loss was less than 20%, and both false negatives and false positives were less than 15%. Glaucoma suspects comprised subjects with glaucomatous appearance of optic discs and normal visual fields as well as ocular hypertensive patients (IOP greater than 21 mmHg without any hypotensive medication). Each subject provided data from only one random eye for the study.
Proceedings
Optic disc photography was previously done with a retinal camera (TRC-NW7SF Mark I, Topcon Corporation, Tokyo, Japan) for each patient after pupil dilation by a trained technician. The images were digitalized and analyzed by two examiners (NK and NAI) who stratified the optic disc into a subjective fashion according to the C/D as proposed by Armaly and the disc damage likelihood scale (DDLS).[6,7,8,9]
The RNFL-OCT images were retrieved from the optical coherence tomography (OCT) hard drive (Spectralis®, Heidelberg Engineering GmbH, Heidelberg, Germany). The Spectralis OCT uses spectral domain coherence tomography technology. The image was acquired on a scan rate of 40 kHz with 1.8 mm depth and 512 pixel size, providing a tissue axial resolution of 7 μm optical (3.5 μm/pixel digital) and 14 μm optical lateral resolution.
The acquisition of images was done by a technician according to a standard procedure. After pharmacologic pupillary dilation, the RNFL thickness was measured around the optic disc with approximately 16 consecutive circular B-scans (diameter of 3.5 mm, 768 A-scans). Involuntary eye movements were compensated with an online tracking system and the RNFL thickness was automatically segmented (software version 4.0.0.0).
Visual fields were assessed using the central 24-2 program, Swedish interactive threshold algorithm (SITA) standard strategy with the Humphrey Field Analyzer II, model 750 (Zeiss Humphrey Systems, Dublin, CA, USA) with the appropriate correction of refractive errors. A trained technician performed all visual field testings. Only the charts of patients with reliable tests were included.
Statistical Analysis
Differences between glaucoma patients and suspects were analyzed with one-way analysis of variance (ANOVA) or Chi-square test when appropriate. Glaucoma patients were stratified into early, moderate and advanced disease according to the MD for comparison.
The relationship between VFI and the other two functional measures, MD and PSD, was assessed using a linear model of regression analysis (y = a + bx). The correlation between the VFI and structural variables, C/D, DDLS and RNFL thickness was evaluated using both linear and logarithm regression analysis (log(y) = a + bx), as dB values being a logarithmic transformation of differential light sensitivity. The VFI recorded in percentage (%) was treated as the dependent variable and the structural measures and the other two functional measures, MD and PSD recorded in dB, were considered as the independent variables. Pearson's product moment correlation coefficients with 95% confidence intervals (95% CI) were calculated to measure the degree of association between VFI and structural parameters and between VFI and two automated perimetry measures. Statistical significance was set at P < 0.05 and all analyses were done with MedCalc® software, version 9.3.7.0 (MedCalc Software bvba, Belgium).
RESULTS
Detailed information of participants and differences among groups are presented in Table 1. One hundred and sixty-two patients with POAG or glaucoma suspects, and subjects with ocular hypertension were included comprising of 92 (56.8%) males and 70 (43.2%) females. Mean age was 54.0 ± 14.9 years. Regarding the ethnicity, 120 (74%) cases were white, 12 (7.4%) were African-Brazilian, 15 (9.3%) were Asian, and 15 (9.3%) were of mixed ethnicity.
Table 1.
Sample demographic characteristics
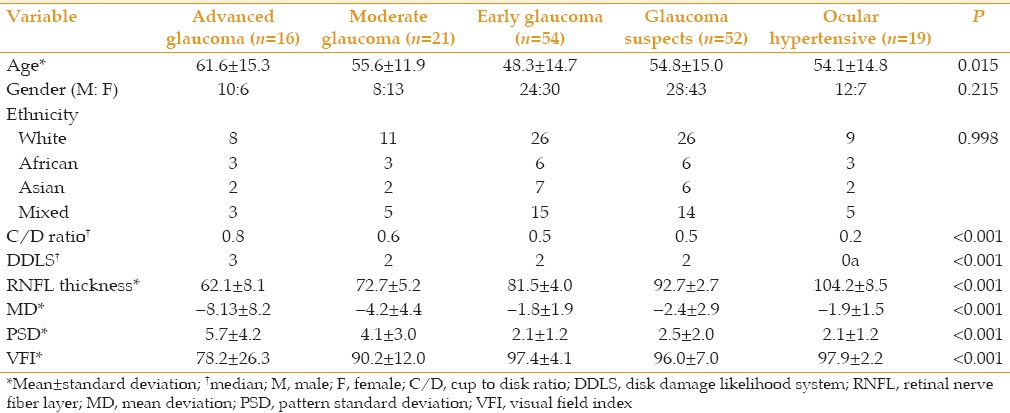
The median C/D ratio was 0.4 (range, 0.1 to 0.9) and the median DDLS was 1 (range, 0a to 7a). Mean VFI was 94.0 ± 11.9%, mean MD value was −3.0 ± 4.1, and mean PSD value was 2.8 ± 2.4.
A subset of 118 subjects with available OCT RNFL data were assessed for the correlation between VFI and an objective structural measure. They were 74 female and 44 male subjects with the mean age of 54.8 ± 14.9 years. Mean VFI was 88.4 ± 16.7 (range, 5 to 100), and mean MD was −3.4 ± 5.5; most patients had early glaucoma (median MD −2.11).
Figures 1 and 2 display the scatterplot matrix and the Pearson correlation coefficient (R) for each correlation. All correlations between VFI and functional/structural measures showed statistical significance (P < 0.05), except for VFI and C/D with logarithmic transformation (P = 0.068).
Figure 1.
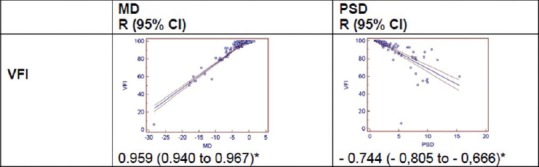
Scatterplot matrix of the correlation between the Visual Field Index and functional measures (MD and PSD). VFI: visual field index; MD: mean deviation; PSD: pattern standard deviation; R: Pearson correlation coefficient; 95% CI: 95% confidence interval; *P < 0.001.
Figure 2.
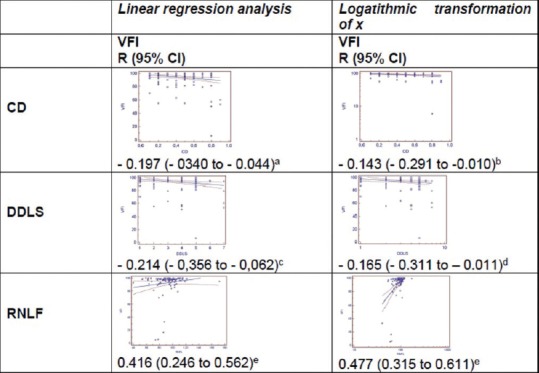
Scatterplot matrix of the correlation between the Visual Field Index and structural measures (C/D, DDLS and RNFL thickness). VFI: visual field index; CD: cup to disc ratio; DDLS: disc damage likelihood scale; RNFL: retinal nerve fiber layer; R: Pearson correlation coefficient; 95% CI: 95% confidence interval.aP = 0.012;bP = 0.068;cP = 0.006;dP = 0.035;eP < 0.001.
DISCUSSION
The results of this study revealed that VFI displayed a strong positive correlation with MD and a weak negative correlation with PSD. The VFI ranged from zero (perimetrically blind eye) to 100% (normal visual field). The correlation between VFI and both MD and PSD was linear. This correlation was expected since VFI, MD and PSD are all parameters assessed by the same equipment (Humphrey Field Analyzer) using decibels. The MD value of automated perimetry is a weighted average decibel deviation from age normal database; the lower the MD value, the more damaged the visual function. The strong positive correlation found in the study (R = 0.956) means that the worse the MD, the lower the VFI value. On the other hand, the PSD value is the standard deviation of the difference between the threshold value at each test location and the expected value and, as an indicator of localized defects, it reflects the roughness of the visual field. It is calculated by summing the absolute value of the difference between the threshold value for each point and the average visual field sensitivity at each point. The correlation between PSD and VFI was negative (R = −0.744), i.e., the higher the PSD value, the lower the VFI. In other words, patients with localized defects on the visual field have correspondently lower values of VFI.
Kimura et al examined the correlation between the VFI and MD, as well as the correlation on VFI slope and MD slope on 105 eyes of 60 patients according to visual field patterns (paracentral, peripheral, mixed and normal defect type).[4] A significant correlation was shown between the VFI and MD, as well as VFI slope and MD slope in all eyes. However, they found no correlation between the VFI slope and MD slope in the paracentral area.[4] This might be due to the fact that VFI weighs central points more than peripheral ones. In the current study, we did not analyze the correlation stratified by visual field defect patterns.
The correlation between the VFI and the structural measures of the optic disc and the RNFL were weak but statistically significant. The C/D ratio describes the disc using cup diameter as a percentage of overall disc diameter in both the vertical and the horizontal aspects. In this study, we used only the vertical C/D, since in glaucoma, the cup enlarges preferentially in this meridian as a result of greater susceptibility of the superior and inferior poles.[10] The ratio can vary from 0.1 (normal cupping) to 1.0 (totally cupped disc). The larger the C/D ratio, the smaller the amount of neural rim and the more advanced the disease. The correlation between VFI and C/D (R = −0.197) revealed that the smaller the VFI, the greater the C/D. The C/D ratio was a significant advance in quantifying glaucomatous optic neuropathy; it was easy to use in clinical practice and clinical trials. However, the two principal limitations of the C/D ratio staging system are the fact that the system does not account for disc size and also that focal narrowing of the neuroretinal rim is not adequately highlighted.[8]
The DDLS is based on the appearance of the neuroretinal rim of the optic disc corrected for disc diameter. First, the optic disc is classified as small (<1.5 mm), average (1.5–2 mm) or large (>2.0 mm). Then, the circumferential extent of rim absence (0 rim/disc ratio) is measured in degrees. The eight stages, extending from no damage to far advanced damage, are 0a (1), 0b (2), 1 (3), 2 (4), 3 (5), 4 (6), 5 (7), 6 (8), 7a (9) and 7b (10).[7] In this study, we have used a 1 to 10 scale to facilitate statistical calculations. The correlation between VFI and DDLS was weak and negative (R = −0.214), i.e., the smaller the VFI value, the larger the DDLS.
In the present study, we found a positive correlation between VFI and RNFL thickness; the higher the VFI, the thicker the RNFL. In fact, the correlation was even stronger than the correlation between VFI and both C/D and DDLS. Optical coherence tomography provides an objective measurement of the RNFL whereas both C/D and the DDLS are subjective and examiner dependent methods; they give a qualitative evaluation of the optic disc. Besides, the optic nerve head in glaucoma patients has features that are not related to nerve fiber loss, such as the posterior bowing of the lamina cribrosa, peripapillary atrophy, and pallor of the neuroretinal rim. The RNFL thickness is more closely related to the nerve fiber loss in glaucoma. These differences may explain the different correlation indexes.
The sample in this study comprised mostly of patients with early glaucoma and glaucoma suspects (126 patients), whereas subjects with moderate and advanced glaucoma were fewer (36 patients). To some extent, this observation may account for the weak correlation between VFI and structural measures in the current study.
Recently, Marvasti et al evaluated the relationship between VFI and the estimated number of retinal ganglion cells (RGCs) in glaucoma in a cohort of 1,245 healthy, glaucomatous and suspected glaucomatous subjects.[5] Estimates of RGC count and percentage of RGCs remaining, compared to the age matched healthy eyes, were calculated from time domain OCT using the Harwerth formula.[11] The authors concluded that the relationship between VFI and estimated RGC counts was nonlinear and the index might substantially underestimate the amount of neural loss early in the disease.[5] In our study, we used clinical measures to estimate structural damage (C/D ratio and DDSL) and the RGCs number was not calculated, although the RNFL thickness was available for some patients.
The correlation between structural and functional variables is controversial. Both the diagnosis and assessment of glaucoma progression are often based on a method of ophthalmic testing to identify and quantify the pattern of visual defects (functional defects) or the thinning of the RNFL (structural damage). Because of the unitary cause, structural and functional events should be correlated to the loss of RGCs.[11] Although most studies report a non-linear relationship (exponential or logarithmic) between structural measures relating to the number of RGCs and the retinal sensitivity (in decibels), others have noted a linear correlation.[12,13,14,15,16,17,18] In this study, the correlation between VFI and structural measures was linear using both clinical measures (C/D and DDLS) and an objective measure (RNFL thickness). Our sample was made mostly of subjects with early glaucoma and suspects. This may account for this observation to some extent.[19]
This study has some obvious shortcomings. First, it was retrospective in design. By using records that were not designed for the study, the available data may be of poor quality. Besides, there can frequently be an absence of data on potential confounding factors when the data was recorded in the past. In this regard, not all subjects had RNFL data from the OCT and the sample size for this analysis was limited. We have tried to minimize some of these drawbacks by reviewing all optic disc photos for the study before assigning a C/D ratio and DDLS. Another caveat is that the type of visual field defect can affect the correlation between MD and VFI. Visual field defects were defined by Anderson's criteria regardless of the type of defect. In fact, if we had a larger sample and enough cases for each type of visual field defect, we could have presented a sub-analysis for each subgroup. Since this was a correlation study, only the values of MD, PSD and VFI were used to both depict visual field status and to analyze the correlation between variables.
In summary, this study has confirmed that VFI correlates with both structural and functional measures of the glaucoma optic neuropathy. Although initially developed to assess functional progression of glaucoma, we believe that VFI can be used to stage the disease severity in clinical practice.
Financial Support and Sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Weinreb RN, Khaw PT. Primary open-angle glaucoma. Lancet. 2004;363:1711–1720. doi: 10.1016/S0140-6736(04)16257-0. [DOI] [PubMed] [Google Scholar]
- 2.Bengtsson B, Heijl A. A visual field index for calculation of glaucoma rate of progression. Am J Ophthalmol. 2008;145:343–353. doi: 10.1016/j.ajo.2007.09.038. [DOI] [PubMed] [Google Scholar]
- 3.Garway-Heath DF. Comparison of structural and functional methods – I. In: Weinreb RN, Greve EL, editors. Glaucoma Diagnosis. Structure and Function. The Hague, Netherlands: Kluger Publications; 2004. pp. 135–143. [Google Scholar]
- 4.Kimura S, Kimura T, Ono K, Murakami A. Correlation between visual field index values and mean deviation values of Humphrey field analyzer. Nippon Ganka Gakkai Zasshi. 2011;115:686–692. [PubMed] [Google Scholar]
- 5.Marvasti AH, Tatham AJ, Zangwill LM, Girkin CA, Liebmann JM, Weinreb RN, et al. The relationship between Visual Field Index and estimated number of retinal ganglion cells in glaucoma. PLoS One. 2013;8:e76590. doi: 10.1371/journal.pone.0076590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Armaly M, Sayegh R. The cup/disc ratio. Arch Ophthalmol. 1969;82:191–196. doi: 10.1001/archopht.1969.00990020193008. [DOI] [PubMed] [Google Scholar]
- 7.Spaeth GL, Henderer J, Liu C, Kensen M, Altangerel U, Bayer A, et al. The disc damage likelihood scale: Reproducibility of a new method of estimating the amount of optic nerve damage caused by glaucoma. Trans Am Ophthalmol Soc. 2002;100:181–186. [PMC free article] [PubMed] [Google Scholar]
- 8.Henderer JD. Disc damage likelihood scale. Br J Ophthalmol. 2006;90:395–396. doi: 10.1136/bjo.2005.083360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bayer A, Harasymowycz P, Henderer JD, Steinmann WG, Spaeth GL. Validity of a new disc grading scale for estimating glaucomatous damage: Correlation with visual field damage. Am J Ophthalmol. 2002;133:758–763. doi: 10.1016/s0002-9394(02)01422-8. [DOI] [PubMed] [Google Scholar]
- 10.Quigley HA, Addicks EM. Regional differences in the structure of the lamina cribrosa and their relation to glaucomatous optic nerve damage. Arch Ophthalmol. 1981;99:137–143. doi: 10.1001/archopht.1981.03930010139020. [DOI] [PubMed] [Google Scholar]
- 11.Harwerth RS, Wheat JL, Fredette MJ, Anderson DR. Linking structure and function in glaucoma. Prog Retin Eye Res. 2010;29:249–271. doi: 10.1016/j.preteyeres.2010.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Oliveira AC, Oliveira FC, Albers MBV, Cohen R, Kasahara N. Clinical correlation between structural and functional assessment in glaucoma: Armaly cup to disk ratio and Brusini glaucoma staging system. Arq Bras Oftalmol. 2008;71:242–245. doi: 10.1590/s0004-27492008000200020. [DOI] [PubMed] [Google Scholar]
- 13.Hood DC, Greenstein VC. Multifocal VEP and ganglion cell damage: Applications and limitations for the study of glaucoma. Prog Retin Eye Res. 2003;22:201–251. doi: 10.1016/s1350-9462(02)00061-7. [DOI] [PubMed] [Google Scholar]
- 14.Danesh-Meyer HV, Ku JY, Papchenko TL, Jayasundera T, Hsiang JC, Gamble GD. Regional correlation of structure and function in glaucoma, using the Disc Damage Likelihood Scale, Heidelberg Retina Tomograph, and visual fields. Ophthalmol. 2006;113:603–611. doi: 10.1016/j.ophtha.2005.10.055. [DOI] [PubMed] [Google Scholar]
- 15.Airaksinen PJ, Drance SM. Neuroretinal rim area and retinal nerve fiber layer in glaucoma. Arch Ophthalmol. 1985;103:203–204. doi: 10.1001/archopht.1985.01050020055018. [DOI] [PubMed] [Google Scholar]
- 16.Jonas JB, Gründler AE. Correlation between mean visual field loss and morphometric optic disk variables in the open-angle glaucomas. Am J Ophthalmol. 1997;124:488–497. doi: 10.1016/s0002-9394(14)70864-5. [DOI] [PubMed] [Google Scholar]
- 17.Garway-Heath DF, Viswanathan A, Westcott M, Kamal D, Fritzke FW, Hitchings RA. Relationship between perimetric light sensitivity and optic disc neuroretinal rim area. In: Wall M, Wild JM, editors. Perimetry update 1998/1999. The Hague, Netherlands: Kugler Publications; 1999. pp. 381–389. [Google Scholar]
- 18.Bartz-Schmidt KU, Thumann G, Jonescu-Cuypers CP, Krieglstein GK. Quantitative morphologic and functional evaluation of the optic nerve head in chronic open-angle glaucoma. Surv Ophthalmol. 1999;44(Suppl 1):S41–53. doi: 10.1016/s0039-6257(99)00076-4. [DOI] [PubMed] [Google Scholar]
- 19.Garway-Heath DF, Hitchings RA. Sources of bias in studies of optic disc and retinal nerve fiber layer in glaucoma. Br J Ophthalmol. 1998;82:986. doi: 10.1136/bjo.82.9.986. [DOI] [PMC free article] [PubMed] [Google Scholar]


