Abstract
Background
Urban adolescent and young adult women often require adult support throughout their transition to adulthood particularly regarding seeking healthcare. While confidentiality is crucial feature of care delivery, successful adherence to treatment can be multi-factorial. The purpose of this study is to determine factors associated with parental notification and engagement in self-care of young women diagnosed with Pelvic Inflammatory Disease (PID).
Methods
This study utilizes data from 187 participants in the Technology Enhanced Community Health Nursing (TECH-N) study, a randomized controlled trial of an intervention to prevent recurrent STIs after a diagnosis of mild-moderate PID. Participants were recruited from pediatric ambulatory settings provided baseline demographic, reproductive history, and perceived social support using an audio computerized self-interview at baseline and parental notification collected during a two-week follow-up interview, served as the primary outcome.
Results
Sixty-five percent of participants informed a parent of their PID diagnosis, 74% of whom reported receiving supportive care. Participants who reported a higher sense of responsibility to others were 17% less likely to inform a parent of their diagnosis.
Conclusion
Most urban young women with PID notify parents of their diagnosis and obtain support for self-management in the outpatient setting. While autonomy is a critical milestone for transition to young adulthood, these data suggest that proactive youth-managed parental engagement may be an underutilized resource for young women diagnosed with PID.
Keywords: PID, adolescent, young adult, parental notification, parental engagement
Short Summary
Nearly 70% of young women diagnosed with PID notified a parent. Women reporting greater responsibility to others on the social provisions scale were significantly less likely to involve a parent. Clinician support for patient-initiated parental engagement respectful of confidentiality could potentially provide affected patients additional supports for PID self-management in the outpatient setting.
INTRODUCTION
Urban adolescent and young adult women often require adult support for successful self-management of reproductive health conditions throughout their transition to adulthood. While studies have evaluated the associations between adolescent confidentiality-seeking behavior and fear of parental retribution or disapproval,1 few have considered the factors associated with adolescent initiated parental notification of sexually transmitted infections (STIs) or reproductive health decisions. Confidentiality remains the legal and ethical cornerstone of adolescent and young adult clinical service delivery. Because successful outpatient adherence to treatment for complicated STIs, such as pelvic inflammatory disease (PID), involves complex self-management, adult support is often required to achieve optimal treatment outcomes. As such, the scope of confidentiality between patients and parents should be considered relative to variations in adolescent age, psychosocial status, economic autonomy,1 and status of their parental relationship.
Prior research suggests that urban young women often engage parents around reproductive health decisions.2 However, clinical providers are least likely to consider parental knowledge of the adolescent or young adult’s PID diagnosis when prescribing self-care dispositions for complicated STIs or PID.3 Yet parental or other adult social support, defined as advice, comfort, medication reminders, is a well-established protective factor against adolescent risk taking behavior4 and may enhance the adherence to the complex self-care regimen prescribed for treatment of PID. Prior data indicate that many adolescents treated for PID may not receive adequate self-care discharge instructions in pediatric ambulatory settings3,4 and engagement of adult social support may enhance adherence to the Centers for Disease Control and Prevention (CDC) recommended treatment regimen.5 The purpose of this study was to evaluate the factors associated with participant-initiated parental notification and parental engagement with self-care activities (e.g. medication reminders, advice, or comfort) of young women diagnosed with PID.
MATERIALS AND METHODS
This study utilized preliminary analysis of data from the Technology Enhanced Community Health Nursing (TECH-N) trial (NCT01640379). The methods for the TECH-N study have been previously described in the literature,6, 7 but will be briefly reviewed here. The study is a single-blind randomized control trial (RCT) designed to evaluate a community health nursing (CHN) intervention using one-on-one home counseling visits supplemented with text message communications to the patients aged 13–25 years for improved clinical self-management and adherence. The goal of the intervention was to achieve short-term reduction in adverse outcomes after a PID diagnosis. Only those participants randomized into the CHN intervention group received one-on-one counseling and text message reminders to take PID medication. Young women in the control arm did not receive any of the interventions. Participants were recruited from two outpatient clinics and adult and pediatric emergency departments of a large urban academic center in Baltimore, MD. All eligible women completed a baseline audio-computerized assisted self-interview (ACASI) through which participants provided data on demographics, reproductive and sexual history, parental notification behavior and perceived social support. The Johns Hopkins Medical Institutional Review Board approved the study.
Social support was measured using the validated 24-item Social Provision Questionnaire (SPQ).8 The SPQ was derived from the conceptual framework of Robert Weiss and identified six domains to describe relationships: guidance (advice and information), reassurance of worth (respect for abilities and personal qualities), social integration (mutual interests and concerns and belonging to a group of similar others), attachment (expressions of caring and love), opportunity to provide nurturance (serving as support to others), and reliable alliance (tangible aid). The SPQ measure includes four questions for each of the six domains. Each item was scored using a four-point Likert scale (strongly disagree, disagree, agree or strongly agree) ranging from a score of 1, indicating “strongly disagree,” to 4, indicating “strongly agree.” Both the total score and social support subscale scores for each of the six social provisions were calculated from the four questions specific to each domain for a range in score from 24–96. Higher scores indicated higher perceived social support.5 Cronbach’s alpha was calculated for internal consistency reliability of each subscale domain.
Parental notification and engagement (parental assistance with care) during the 2 week PID treatment period were ascertained during an in-person interview at a 2-week follow-up visit during which participants were asked about parental notification and engagement in treatment. The item included “Did you notify your parent or legal guardian about your PID diagnosis?” Parental notification was coded as Yes or No and this dichotomous variable served as the primary outcome. Participant age was dichotomized into adolescent (14–17 years) or young adult (18–25 years). Logistic regression models used to determine the factors associated with parental notification and included evaluation of participant’s age, perceived social support (SPQ), number of current and lifetime sexual partners. Participant’s group status (intervention versus standard of care control) was controlled for in regression analyses due to potential confounding role of this variable.
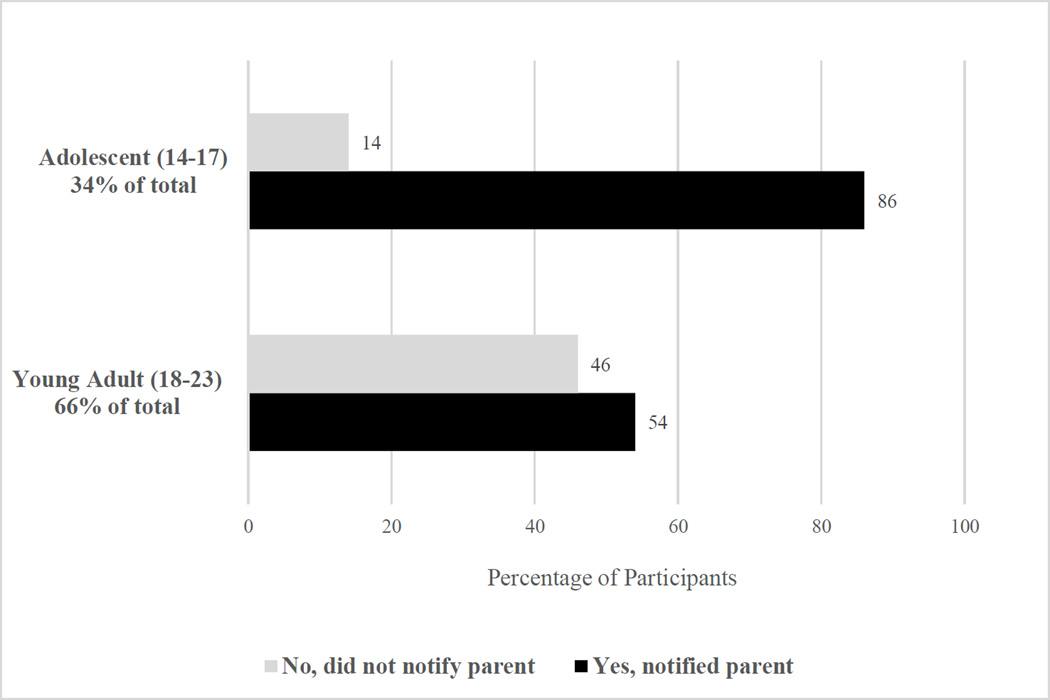
RESULTS
A total of 187 participants were in the sample. Most participants were African American (94%), Medicaid insured (80%), and resided in single female-headed households (66%) with most parents (80%) reporting high school or less as their level of education (Table 1). Mean age of all participants was 18.4 years [SD 2.2], although nearly one-third (34%) were adolescents between age 14–17 years and 66% were young adults between 18–23 years of age. Mean age of participants sexual debut (mean age 14.8 years, [SD 1.7]) and average lifetime sexual partners was 5.8 [SD 6.1]. Fifty-three percent of participants reported a previous STI diagnosis and 55% reported a previous diagnosis of pregnancy. Most participants (65%, N=121) notified a parent of their PID diagnosis with significantly more notification among younger women (adolescent: 85.9%; young adult: 53.7%; p<0.001) (Figure 1). Among participants reporting parental notification of their PID diagnosis, almost three-quarters (74%) reported concurrent parental engagement in care of their PID diagnosis. Group assignment was not associated with parental notification (CHN intervention vs. control, p=0.499). Of the six Social Provision sub-scales, the nurturance, reassurance and alliance subscales (Cronbach’s alpha results were 0.44, 0.41, 0.73 respectively) were significantly associated with parental notification (Table 2). In the final logistic regression model, participants who reported an increased sense of responsibility for the wellbeing of others (an increase of one point in the Nurturance subscale) were almost 20% less likely to notify a parent about their diagnosis [OR 0.829 (95% CI: 0.707, 0.973; p=0.022)], controlling for participants’ age and intervention group status. Participants who reported a higher sense of recognition of competence, respect for abilities and personal qualities (Reassurance subscale) were 20% more likely to notify a parent about their diagnosis [OR 1.197 (95% CI: 1.008, 1.422; p=0.040)]. Finally, participants who reported a higher sense that they can count on others (Alliance subscale) were 16% more likely to notify a parent about their diagnosis [OR 1.160 (95% CI: 1.023, 1.317; p=0.021)], controlling for participants’ age and intervention group status.
TABLE 1.
Sociodemographic & Sexual Health Characteristics, N=187
| Age (mean, sd) years | 18.4, 2.2 |
| African American race (%) | 94 |
| Medicaid Insured (%) | 80 |
| Highest Level of Parental Education High School or Less (%) | 80 |
| Head of participant’s household | |
| Mother/grandmother/aunt/sister (%) | 66 |
| Father/grandfather/uncle/brother (%) | 9 |
| Foster parent (%) | 4 |
| Other relative/Legal guardian (%) | 8 |
| Sexual Debut (mean age, sd) | 14.8, 1.7 |
| Lifetime Number of Sexual Partners (mean, sd) | 5.8, 6.1 |
| Previously diagnosed with STI (%) | 53 |
| Previously diagnosed with pregnancy (%) | 55 |
| Intervention/Control Study Arm (%) | 54/46 |
FIGURE 1.
Parental Notification by Age, p<0.001
TABLE 2.
Logistic Regression Analysis Results Social Support Subscales by Parental Notification, N=187
| Social Provision Subscales | Mean (sd) |
Mean (Parent not notified) |
Mean (Parent notified) |
OR (95% CI) | P-value | Cronbach’s alpha |
|---|---|---|---|---|---|---|
| Guidance (Advice or information) |
12.4 (2.3) | 11.9 (2.3) | 12.7 (2.3) | 1.143 (1.000, 1.308) |
0.050 | 0.71 |
| Reassurance* (Recognition of competence) |
11.8 (1.9) | 11.4 (1.7) | 12.0 (1.9) | 1.197 (1.008, 1.422) |
0.040* | 0.41* |
| Integration (Sense of belonging) |
11.9 (2.0) | 11.8 (2.1) | 12.0 (2.0) | 1.047 (0.898, 1.222) |
0.557 | 0.56 |
| Attachment (Emotional closeness) |
11.9 (2.0) | 11.7 (2.0) | 12.1 (2.0) | 1.091 (0.935, 1.273) |
0.266 | 0.50 |
| Nurturance* (Assisting others) |
11.6 (2.0) | 12.0 (2.2) | 11.3 (1.8) | 0.829 (0.707, 0.973) |
0.022* | 0.44* |
| Alliance* (Others can be counted on) |
12.3 (2.5) | 11.7 (2.6) | 12.6 (2.4) | 1.160 (1.023, 1.317) |
0.021* | 0.73* |
Note: An odds ratio greater than one indicates a higher likelihood that a parent will be notified when the subscale score is higher. An odds ratio less than one indicates that an individual will be less likely to notify a parent when their subscale score is higher.
Indicates p value < 0.05
DISCUSSION
Our data indicate that most urban young women with PID notify a parent regarding their PID diagnosis and nearly 75% of these patients reported parental support during the treatment period. While parental notification was common when adolescents were hospitalized for PID as standard practice, there are no published reports on social support or parental engagement in the care for PID since treatment for mild to moderate disease has since shifted the outpatient setting.5 Notably, patient age was a significant determinant of parental notification. Young women who perceived greater responsibility to nurture others were more likely to undertake self-management alone while young women who perceived greater competency and ability to rely on others were more likely to notify a parent. Nurse and physician provider awareness of the patient’s sense of nurturance or responsibility to others (such as whether the patient is a parent or caretaker herself) could serve as an indicator to further inquire about the need for additional parental clinical support. Additionally, provider inquiry about perceived competence (reassurance) and ability to count on others (alliance) could indicate sources of strength and support in treatment and management of PID. This information could serve as an initiation point for the providers to further assess and discuss the potential value parental engagement in PID treatment or referral for additional health care services including home health for community nursing support.
Prior reports indicate that health providers who care for adolescents were least likely to consider parental involvement when making clinical disposition decisions for adolescents diagnosed with PID in the outpatient setting.9 This lack of acknowledgment of the importance of parental involvement by providers may actually undermine effective engagement of supports for self-management. While autonomy is a critical milestone for transition to young adulthood,1 these data suggest that support from a caring adult, including a parent, is important for most young women across ages who are managing care a diagnosis of PID in the outpatient setting. Clinician and nursing assessments of social supports during the patient interview and/or at the time of disposition may lead to identification of key social supports for self-care in the outpatient setting. Further, clinicians and discharging nurses may miss an opportunity to assist the adolescent with parental engagement when the parent is present with them in the outpatient clinic and/or emergency department where most participants were recruited in this sample.
The findings from this study should be considered in the context of several general limitations. Generalizability may be limited due to a fairly homogenous demographic population recruited from a single city and academic medical center located in a community with high STI rates. However, we purposely target this population because of the significant risks for reproductive morbidity and youth-parent relationship dynamics that facilitate communication about STIs and reproductive health that have been previously observed.10 Additionally, we have limited information about the context of parental notification such as difficulty or challenges with revealing their diagnosis, context surrounding notification, and the true level of responsibility and independence for adolescents who self report a higher sense of nurturance, reassurance, and alliance.8
In conclusion, our findings support the notion that adolescents perceive PID as a serious medical problem as evidenced by parental notification and engagement behaviors. These findings are consistent with prior research indicating that adolescents generally indicated a preference for more help with PID care and parental preferences to support their daughters to ensure adequate follow-up for PID and other reproductive health issues.10,11 Future research to actively explore the potential role of adolescent-controlled parental notification and engagement as a strategy to increase outpatient support and adherence is warranted. Helping adolescents to voluntarily capitalize on positive relationships with their parents and/or other supportive adults in their lives during the acute management phase may be an important public health strategy to reduce the adverse health outcomes associated with PID. Future work in this area should rely on perceived support and proceed with caution given the data on foregone care by adolescents without confidentiality.12
Supplementary Material
Acknowledgments
This work was funded by a grant from the National Institute of Nursing Research [5R01NR013507] with additional support from the National Institute of Biomedical Imaging and Bioengineering [U-54EB007958]. We also acknowledge the contributions from the young women who participated in this study as well as the work of the TECH-N research team.
Conflicts of Interest:
The authors report no conflicts of interest and there was no pharmaceutical or industry support for this work.
REFERENCES
- 1.Confidential Health Care for Adolescents: Position Paper of the Society for Adolescent Medicine. Journal of Adolescent Health. 1997;21:408–415. doi: 10.1016/s1054-139x(97)00171-7. [DOI] [PubMed] [Google Scholar]
- 2.Trent M, Tomaszewski K. Family Planning Appointment Attendance Among Urban Youth: Results from the DepoText Trial. Journal of Adolescent Health. 2013;52(2):S88. [Google Scholar]
- 3.Trent M, Lehmann H, Butz A, Qian Q, Frick K. Clinician Perspectives on Management of Adolescents With Pelvic Inflammatory Disease Using Standardized Patient Scenarios. Sexually Transmitted Diseases. 2013;40(6):496–498. doi: 10.1097/OLQ.0b013e318284e3b5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Trent M, Ellen JM, Walker A. Pelvic Inflammatory Disease in Adolescents: Care Delivery in Pediatric Ambulatory Settings. Pediatric Emergency Care. 2005;21(7):431–436. doi: 10.1097/01.pec.0000169432.14067.eb. [DOI] [PubMed] [Google Scholar]
- 5.Workowski KA, Berman S. Center for Disease Control Morbidity and Mortality Weekly Report, Sexually Transmitted Diseases Treatment Guidelines. [Accessed 2016 October 7];2010 59(RR-12) Available at: https://www.cdc.gov/std/treatment/2010/ [PubMed] [Google Scholar]
- 6.Butz A, Gaydos C, Toppins J, Johnson B, Huettner S, Trent M. Clinical Pediatrics, Care Seeking Behavior after Notification among Young Women with Recurrent Sexually Transmitted Infections (STIs) after Pelvic Inflammatory Disease (PID), Clinical Pediatrics. 2016;55(12):1107–1112. doi: 10.1177/0009922816662863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Trent M, Chung S, Gaydos C, Frick K, Anders J, Huettner S, Rothman R, Butz A. Recruitment of Minority Adolescents and Young Adults into Randomized Clinical Trials: Testing the Design of the Technology Enhanced Community Health Nursing (TECH-N) Pelvic Inflammatory Disease Trial. EMJ Repro Health. 2016;2(1):44–51. [PMC free article] [PubMed] [Google Scholar]
- 8.Cutrona CE, Russell D. The Provisions of Social Relationships and Adaptation to Stress. Advances in Personal Relationships. 1984;(1):37–67. [Google Scholar]
- 9.Trent M, Lehmann H, Butz A, Qian Q, Frick K. Clinician Perspectives on Management of Adolescents with Pelvic Inflammatory Disease Using Standardized Patient Scenarios. Médecine de la Repoduction Gynecologie Endcrinologie. 2013;15(3):234–238. doi: 10.1097/OLQ.0b013e318284e3b5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Trent M, Lehmann HP, Qian Q, Thompson CB, Ellen JM, Frick KD. Adolescent and Parental Utilities for the Health States Associated with Pelvic Inflammatory Disease. Sexually Transmitted Infections. 2011;87(7):583–587. doi: 10.1136/sextrans-2011-050187. [DOI] [PubMed] [Google Scholar]
- 11.Trent M, Thompson C, Tomaszewski K. Text Messaging Support for Urban Adolescent and Young Adults Using Injectable Contraception: Outcomes of the DepoText Pilot Trial. The Journal of Adolescent Health. 2015;57(1):100–106. doi: 10.1016/j.jadohealth.2015.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McKee D, Fletcher J. Primary Care for Urban Adolescent Girls from Ethnically Diverse Populations: Foregone Care and Access to Confidential Care. J Health Care Poor Underserved. 2006;17(4):759–774. doi: 10.1353/hpu.2006.0131. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.