Abstract
Background
The conditional process model (CPM) of mindfulness and emotion regulation posits that specific mediators and moderators link these constructs to mental health outcomes. The current study empirically examined the central tenets of the CPM, which posit that nonreactivity moderates the indirect effect of observation on symptoms of emotional disorders through cognitive emotion regulation strategies.
Methods
A clinical sample (n=1667) of individuals from Japan completed a battery of self-report instruments. Several path analyses were conducted to determine whether cognitive emotion regulation strategies mediate the relationship between observation and symptoms of individual emotional disorders, and to determine whether nonreactivity moderated these indirect effects.
Results
Results provided support the CPM. Specifically, nonreactivity moderated the indirect effect of observation on symptoms through reappraisal, but it did not moderate the indirect effect of observation on symptoms through suppression.
Limitations
Causal interpretations are limited, and cultural considerations must be acknowledged given the Japanese sample
Conclusions
These results underscore the potential importance of nonreactivity and emotion regulation as targets for interventions.
1. Introduction
Recent years have witnessed novel conceptualizations of anxiety and depression, which consider contextual and mechanistic factors that maintain clinical levels of psychopathology (Hofmann, 2014; Kashdan et al., 2014). Of note, there has been increasing interest in comprehending emotional disorders in the context of mindfulness and emotion regulation (Desrosiers, Vine, Klemanski, & Nolen-Hoeksema, 2013; Desrosiers, Vine, Curtiss, & Klemanski, 2014). Mindfulness refers to the ‘the act of paying attention, on purpose, in the present moment, non-judgmentally’ (Kabat-Zinn, 1990, p. 4). Derived from several Buddhist traditions, mindfulness entails the cultivation of greater levels of present moment awareness by engaging in exercises that facilitate focused attention and open monitoring (Lutz, Slagter, Dunne, & Davidson, 2008). These traditional conceptualizations of mindfulness are consistent with the two-component definition of mindfulness, which involves attending to one’s immediate experience and adopting a present-moment orientation characterized by acceptance and openness (Bishop et al., 2004). The canonical definition of emotion regulation emphasizes the ‘processes by which individuals influence which emotions they have, when they have them, and how they experience and express them’ (Gross, 1998, p. 275). Adaptive forms of emotion regulation promote appropriate behavioral responses to environmental demands by modulating rather than eliminating affective experiences (Roemer, Williams, & Rollins, 2015).
Research on these two constructs has been developing in parallel, which has prompted recent efforts to formulate integrated accounts of mindfulness and emotion regulation (cf. Roemer, Williams, & Rollins, 2015; Chambers, Gullone, & Allen, 2009). Specifically, Roemer et al. (2015) postulate an association between mindfulness and adaptive emotion regulation, and note that mindfulness practice might precede healthy emotion regulation abilities. Likewise, Chambers and colleagues (2009) theorize that mindfulness and emotion regulation are robustly related, and regard mindfulness as a specific type of cognitive reappraisal. Although extant theories of mindfulness and emotion regulation underscore the fact that they are in some way associated (Chiesa, Serretti, & Jakobsen, 2013; Teper, Segal, & Inzlicht, 2013; Garland, Farb, Goldin, & Fredrickson, 2015; Hayes & Feldman, 2004; Roemer, Williams, & Rollins, 2015; Chambers, Gullone, & Allen, 2009), very little research has been devoted to both the mechanisms and contextual factors that account for their relationship to mental health outcomes. Mechanisms specific to mindfulness interventions have been examined, including emotion regulation strategies (i.e., worry and rumination), compassion, and trait mindfulness (Gu, Strauss, Bond, & Kavanagh, 2015; Kuyken et al., 2010). Indeed, some integrative theories posit that processes such as executive control or cognitive reappraisal constitute possible mechanisms underlying the relationship between these two constructs (Teper, Segal, & Inzlicht, 2013; Garland, Farb, Goldin, & Fredrickson, 2015), yet very little attention is given to the potential moderators that influence mechanistic processes.
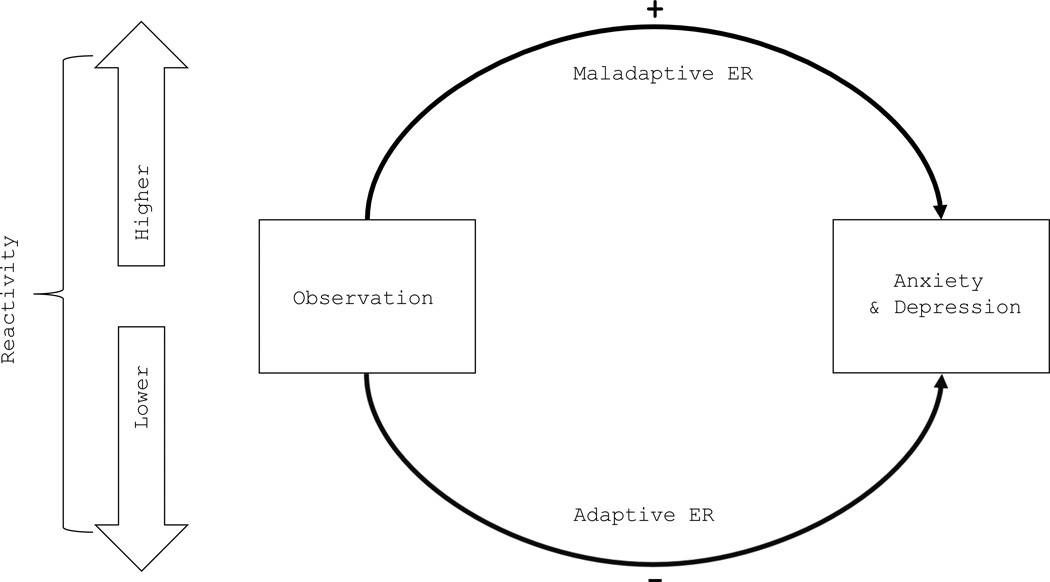
One such model that does consider both mediators and moderators simultaneously is the conditional process model (CPM) of mindfulness and emotion regulation (Klemanski & Curtiss, 2016; Desrosiers et al., 2014) (Figure 1). A distinctive feature of the CPM is that it appreciates the nuanced complexity of the relationship between these multifactorial constructs and mental health outcomes. Although treatment outcome research generally suggests that mindfulness based interventions contribute to symptom remission (Hofmann, Sawyer, Witt, & Oh, 2010), psychometric research has revealed conflicting results as to whether all aspects of mindfulness are associated with lower levels of psychopathology (Harnett, Reid, Loxton, & Lee, 2016). Specifically, the role of observation (i.e., an individual component of mindfulness that reflects basic attentional processes) has undergone much controversy, as divergent results indicate that it predicts both decreases and increases in symptoms of emotional disorders (Curtiss & Klemanski, 2014a; Neale-Lorello & Haga, 2015). The CPM was proposed in an effort to reconcile this ostensible discrepancy in the literature. Contemporary theories of mindfulness regard observation as one of the most fundamental processes that influence emotion awareness, generation, and regulation (Klemanski & Curtiss, 2016; Kabat-Zinn, 1990). Consistent with prior research and other prominent models (Roemer et al., 2015; Chambers et al., 2009), the CPM hypothesizes that observation conveys its effect on emotional distress by way of cognitive emotion regulation mechanisms. Additionally, it stipulates that nonreactivity (i.e., refraining from responding to emotions or thoughts in a reactive manner) constitutes an important contextual factor that determines whether observation will be conducive to emotional wellbeing. Specifically, the CPM predicts that nonreactivity influences the indirect effect of observation on symptoms by augmenting adaptive emotion regulation strategies (e.g., reappraisal) and dampening maladaptive strategies (e.g., suppression), which accords with prior research (Desrosiers et al., 2014). Thus, the principle objective of the CPM is to elucidate the conditions under which mindfulness exerts a salutary influence on mental health, as well as the processes by which it does so.
Figure 1.
Conditional Process Model.
Note: The conditional process model posits that observation leads to either increased or decreased symptoms of emotional disorders depending on one’s level of reactivity to emotions. Specifically, observation should predict greater use of adaptive emototion regulation and fewer symptoms with lower levels of reactivity, whereas observation should result in greater use of maladaptive emotion regulation and elevated symptom with higher levels of reactivity.
ER = emotion regulation.
Although one previous study provided empirical support for the CPM of mindfulness and emotion regulation (Desrosiers et al., 2014), it confined its investigation to broad pathological constructs (i.e., overall anxiety and depression) and did not consider the mechanistic role of suppression. Findings from Desrosiers and colleagues (2014) indicated that observation was associated with high levels of reappraisal and lower levels of rumination and worry among individuals with higher levels of nonreactivity. Furthermore, nonreactivity moderated the indirect effect of observation on depression through rumination and reappraisal, whereas it moderated the indirect effect of observation on anxiety through worry and rumination. These results provide evidence that nonreactive observation is associated with reduced worry and rumination, which both reflect forms of repetitive negative thinking (McEvoy, Mahoney, & Moulds, 2011). However, it remains unknown whether nonreactivity would moderate the association between observation and suppression, which involves attempts to inhibit unwanted thoughts or outward displays of affect (Nixon et al., 2008). Therefore, the current study expands on these findings by (i) examining both suppression and reappraisal as mediators, and (ii) determining whether the conditional indirect effect of observation is robust enough to predict domain specific symptoms of several disorders rather than broad psychopathology constructs. It was predicted that observation will convey a conditional indirect effect on symptoms of generalized anxiety disorder, obsessive compulsive disorder, social anxiety disorder, and major depressive disorder. These particular outcome variables were selected because they represent domain specific symptoms of different emotional disorders (Brown & Barlow, 2009), which is the primary mental health outcome of the CPM. Because the CPM purports to be a transdiagnostic model that explains symptoms of individual anxiety and depressive disorders, it will be of theoretical importance to determine whether nonreactivity moderates the indirect effect of observation on several disparate symptom domains. Such evidence would afford further support for this trandiagnostic hypothesis.
In accordance with a model building approach, the current study utilized path analyses to examine each of the principle hypotheses that were motivated by the aforementioned literature. The first hypothesis (1) predicted that observation will convey an indirect effect on symptoms of each disorder by way of cognitive emotion regulation strategies. Specifically, it was hypothesized that (1a) increases in observation will predict increases in reappraisal which will, in turn, predict decreases in symptoms of each disorder. Conversely, it was expected that (1b) increases in observation will predict increases in suppression which will predict increases in symptoms of each disorder. This would be consistent with prior literature that suggests that symptoms of emotional disorders are inversely associated with reappraisal (i.e., developing alternative or benign interpretations of a stressful situation to reduce distress) and positively associated with suppression (i.e., rigid attempts to prohibit the expression of unwanted thoughts or emotions; Aldao, Nolen-Hoeksema, & Schweizer, 2010). Consistent with Desrosiers and colleagues (2014), the second hypothesis (2) of the CPM posits that these indirect effects will be moderated by nonreactivity. It was predicted that lower levels of nonreactivity would lead to a positive indirect effect of observation on symptom measures through reductions in reappraisal (2a) and increases in suppression (2b).
2. Methods
2.1. Participants and Procedures
Participants in the current study were recruited from panelists registered on Macromill Incorporation, which is a large internet marketing research company in Japan. The panelist pool of Macromill has been used in prior studies (e.g., Sawada et al., 2012), and more details about the current sample are described by Ito et al. (2015). Of the 1,095,443 registered panelists, 389,265 are registered as “disease panelists”. Disease panelists are defined by the monitor's self-report of a current diagnosis of a disorder that was provided by a medical practitioner. Participants were asked whether they were currently diagnosed and were using medical services for treatment. For instance, the item related to panic disorder was “Are you currently diagnosed as having Panic Disorder and being treated for the problem in a medical setting?” We asked the same questions for SAD, OCD, MDD, and “other mental disorders”. Briefly, the current sample comprised 2830 Japanese participants who were extracted randomly from the panelist pool based on age, gender, and living area in each group. Of the participants, 1547 were female, and the mean age was 42.44 (SD = 10.39). These anonymous participants completed a variety of self-report instruments, including those emphasized in the current study. According to participants’ prior medical history, they were divided into non-clinical (n = 1163) and clinical participants (total n = 1667; PD n = 193; SAD n = 116; OCD n = 66; MDD n = 406; comorbid MDD and any anxiety disorder n = 636; comorbid anxiety disorders n = 99; other mental disorders n = 146). In the clinical sample, the mean age was 42.41 (SD = 9.49), and 775 were female. All analyses were conducted using the clinical sample.
2.2. Measures
2.2.1. Five facet mindfulness questionnaire (FFMQ)
This 39-item instrument comprises five subscales measuring different aspects of mindfulness: observation, describing, acting with awareness, nonreactivity, and nonjudgment. Versions of this instrument have been validated in both non-clinical and clinical samples (Baer, Smith, Hopkins, Krietemeyer, & Toney, 2006; Curtiss & Klemanski, 2014a). The FFMQ was also validated in a Japanese sample and exhibited good psychometric properties (Sugiura, Sato, Ito, & Murakami, 2012). In the current sample, good reliability was obtained for both the observation (α = 0.82) and nonreaction (α = 0.79) subscales.
2.2.2. Emotion regulation questionnaire (ERQ)
This 10-item scale assesses two aspects of emotion regulation: reappraisal and suppression (Gross & John, 2003). Its reliability and validity have been widely demonstrated (Gross & John, 2003). The Japanese version exhibited good reliability and validity (Yoshizu, Sekiguchi, & Amemiya, 2013). In the current sample, good reliability was obtained for both the reappraisal (α = 0.81) and suppression (α = 0.76) subscales.
2.2.3. Generalized anxiety disorder 7-item scale (GAD-7)
This 7-item instrument assesses the symptom of generalized anxiety during two weeks (Muramatsu, Seiryou, Muramatsu, & Miyaoka, 2009; Spitzer et al., 2006). Reliability and construct criterion validity have been reported to be good for clinical populations (Spitzer et al., 2006). The GAD-7 was also validated in a Japanese sample (Muramatsu et al., 2009). Reliability was excellent in the current sample (α = 0.93).
2.2.4. Brief version of fear of negative evaluation scale (FNE)
This 12-item scale assesses the tendency to feel threats to be negatively evaluated by others, which is a core feature of social anxiety disorder (Leary, 1983; Sasagawa et al., 2004). The Japanese version demonstrated good reliability (Sasagawa et al., 2004). Reliability was excellent in the current sample (α = 0.93).
2.2.5. Short version of obsessive-compulsive inventory (OCI)
This 18-item instrument assesses obsessive compulsive symptoms among non-clinical and clinical populations (Foa et al., 2002). The reliability and validity of the Japanese has been demonstrated in both clinical and nonclinical samples (Ishikawa, Kobori, & Shimizu, 2014). Reliability was excellent in the current sample (α = 0.93).
2.2.6. Patient health questionnaire (PHQ-9)
This 9-item questionnaire assesses depression severity by asking the frequency of depressive symptoms during the prior two weeks (Kroenke & Spitzer, 2002). The PHQ-9, widely used in clinical settings, has been validated as a measure of depression among clinical and general populations (Kroenke & Spitzer, 2002), and the Japanese version has demonstrated good psychometric properties in terms of reliability (Muramatsu et al., 2007). Reliability was excellent in the current sample (α = 0.93).
2.3. Data Analytic Strategy
The conditional process model was estimated using path analyses in R with the latent variable program Lavaan (Rosseel, 2012). Path analytic techniques confer the advantage of permitting simultaneous estimation of all direct and indirect effects. Full-information maximum likelihood was utilized. To test the direct and indirect effects, nonparametric bootstrapping statistical analyses were used (Preacher & Hayes, 2008). Through this method, data was randomly resampled with replacement from the original sample (Preacher & Hayes, 2008). Data was re-sampled 10,000 times to test direct and indirect effects based on standard errors. Bootstrapped confidence intervals (BCI) of the indirect effect were set at 95%, with an α level of 0.05. All interaction terms were mean centered to facilitate interpretation and to mitigate undue collinearity. Although Type 1 error inflation can be an issue in structural equation models in which numerous parameters are specified (Cribbie, 2007), widely accepted remedial strategies have yet to be validated. Thus, to complement traditional significance tests, effect sizes will be reported for salient indirect effects, which is consistent with prior literature (Brown & Naragon-Gainey, 2013). Specifically, the kappa squared (κ2) was computed to ascertain the proportion of maximum possible indirect effect that could have occurred (Preacher & Kelly, 2011). Because generalizations of κ2 have not been extended to moderated mediation, this effect size will be reported for the indirect effects of the primary process model. Consistent with established precedent, Preacher and Kelly (2011) define small, medium, and large effect sizes as values close to 0.01, 0.09, and 0.25, respectively.
To evaluate each of the hypotheses assumed by the conditional process model, individual path models were estimated in a model building fashion. First, a process model was estimated, which specified mediation pathways of observation on symptom measures through cognitive emotion regulation strategies. Alternative mediation models were estimated, in which cognitive emotion regulation strategies mediated the effect of symptom measures on observation. This competing model is informed by literature suggesting that anxiety and depression symptoms prospectively predict emotion regulation use and that emotion regulation strategies prospectively predict mindfulness (Garland et al., 2016; Calvete, Orue, & Hankin, 2015). Second, a conditional model was examined, which estimated the direct and interactive effects of observation and nonreactivity on each mediator and on each symptom domain, controlling for reappraisal and suppression. Significant interaction coefficients were retained in the final model. Third, the synthesized conditional process model was estimated, which specified moderated mediation effects.
3. Results
3.1. Descriptive Statistics
Correlations and descriptive statistics are depicted in Table 1. All symptom measures were positively associated with each other. As regards mindfulness, observation was positively associated with all symptom measures, whereas nonreactivity was inversely associated with them. Although reappraisal was inversely associated with all symptom measures, suppression was not robustly correlated with any symptom measure.
Table 1.
Correlations and descriptive statistics.
| Mean | SD | 1. | 2. | 3. | 4. | 5. | 6. | 7. | |
|---|---|---|---|---|---|---|---|---|---|
| 1. Observation | 20.53 | 6.06 | |||||||
| 2. Nonreaction | 17.60 | 4.86 | 0.34** | ||||||
| 3. Reappraisal | 23.35 | 7.08 | 0.09** | 0.45** | |||||
| 4. Suppression | 15.50 | 5.02 | 0.10** | 0.21** | 0.46** | ||||
| 5. MDD Sx | 10.42 | 7.74 | 0.30** | −0.21** | −0.32** | 0.01 | |||
| 6. GAD Sx | 7.97 | 6.32 | 0.32** | −0.24** | −0.35** | −0.05** | 0.84** | ||
| 7. OCD Sx | 40.18 | 14.95 | 0.38** | −0.11** | −0.20** | 0.03 | 0.58** | 0.63** | |
| 8. SAD Sx | 39.28 | 10.93 | 0.17** | −0.29** | −0.25** | 0.01 | 0.43** | 0.46** | 0.35** |
Note: All p-values were submitted to false discovery rate correction. Values are for the entire sample. SD = Standard Deviation; Sx = symptoms;
p < 0.05;
p<0.01.
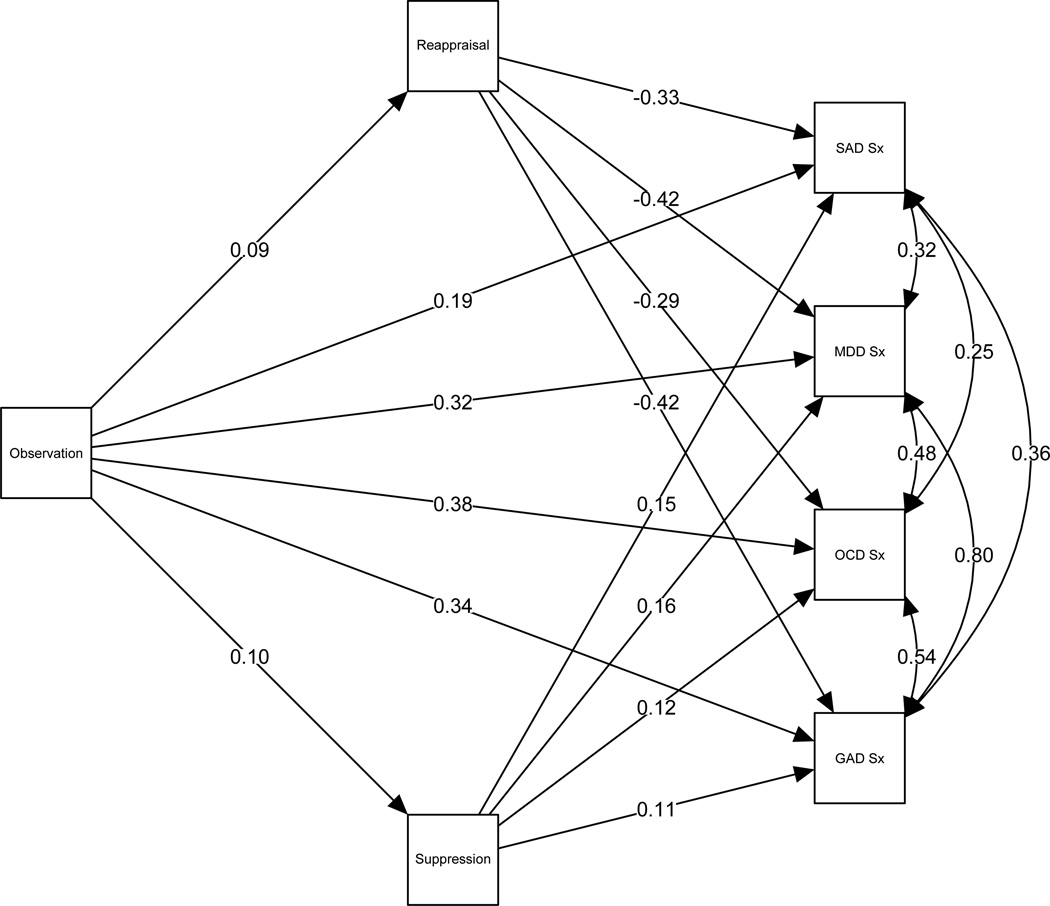
3.2. Results of Process Model
Parameter coefficients of the mediation analyses are displayed in Table 2, and the path diagram is depicted in Figure 2. All of the indirect effects were statistically significant. Consistent with the hypotheses, observation contributed a negative indirect effect on each symptom domain through reappraisal, as well as a positive indirect effect through suppression. Results of the alternative mediation model indicate that none of the indirect effects were significantly different from zero (Table 3).
Table 2.
Parameter estimates of process model.
| Estimate | S.E. | Lower BCI | Upper BCI | κ2 | ||
|---|---|---|---|---|---|---|
| Outcome Variable | Predictor Variable | |||||
| GAD Sx | ||||||
| Observation | 0.36** | 0.02 | 0.33 | 0.39 | ||
| Reappraisal | −0.38** | 0.02 | −0.41 | −0.35 | ||
| Suppression | 0.14** | 0.02 | 0.10 | 0.18 | ||
| OCD Sx | ||||||
| Observation | 0.96** | 0.04 | 0.88 | 1.04 | ||
| Reappraisal | −0.62** | 0.04 | −0.69 | −0.55 | ||
| Suppression | 0.38** | 0.05 | 0.28 | 0.47 | ||
| MDD Sx | ||||||
| Observation | 0.42** | 0.02 | 0.38 | 0.46 | ||
| Reappraisal | −0.47** | 0.02 | −0.51 | −0.44 | ||
| Suppression | 0.26** | 0.03 | 0.21 | 0.31 | ||
| SAD Sx | ||||||
| Observation | 0.34** | 0.03 | 0.28 | 0.41 | ||
| Reappraisal | −0.52** | 0.03 | −0.57 | −0.46 | ||
| Suppression | 0.32** | 0.04 | 0.25 | 0.40 | ||
| Reappraisal | ||||||
| Observation | 0.11** | 0.02 | 0.06 | 0.15 | ||
| Suppression | ||||||
| Observation | 0.08** | 0.02 | 0.05 | 0.11 | ||
| Indirect Effect via Reappraisal | ||||||
| O→R→GAD | −0.04** | 0.01 | −0.06 | −0.02 | 0.05 | |
| O→R→OCD | −0.06** | 0.01 | −0.09 | −0.04 | 0.03 | |
| O→R→MDD | −0.05** | 0.01 | −0.07 | −0.03 | 0.04 | |
| O→R→SAD | −0.05** | 0.01 | −0.08 | −0.03 | 0.03 | |
| Indirect Effect via Suppression | ||||||
| O→S→GAD | 0.01** | 0.00 | 0.01 | 0.02 | 0.01 | |
| O→S→OCD | 0.03** | 0.01 | 0.02 | 0.05 | 0.01 | |
| O→S→MDD | 0.02** | 0.00 | 0.01 | 0.03 | 0.01 | |
| O→S→SAD | 0.03** | 0.01 | 0.02 | 0.04 | 0.005 | |
Note: S.E. = Standard Error; BCI = Bootstrapped Confidence Intervals; O = Observation; R = Reappraisal; S = Suppression; Sx = symptoms; κ2= kappa squared;
p < 0.05;
p<0.01.
Figure 2.
Process Model.
Note: Error terms were omitted to simplify presentation. All coefficients are standardized.
Table 3.
Indirect effects of alternative mediation model.
| Estimate | S.E. | Lower BCI | Upper BCI | ||
|---|---|---|---|---|---|
| Indirect Effect via Reappraisal | |||||
| GAD→R→O | −0.04 | 0.01 | −0.06 | 0.01 | |
| OCD→R→O | 0.01 | 0.003 | −0.01 | 0.01 | |
| MDD→R→O | −0.01 | 0.01 | −0.02 | 0.01 | |
| SAD→R→O | −0.01 | 0.003 | −0.01 | 0.01 | |
| Indirect Effect via Suppression | |||||
| GAD→S→O | −0.01 | 0.01 | −0.02 | 0.01 | |
| OCD→S→O | 0.002 | 0.002 | −0.002 | 0.01 | |
| MDD→S→O | 0.002 | 0.002 | −0.003 | 0.01 | |
| SAD→S→O | 0.001 | 0.001 | −0.001 | 0.002 | |
Note: S.E. = Standard Error; BCI = Bootstrapped Confidence Intervals; O = Observation; R = Reappraisal; S = Suppression; Sx = symptoms;
p < 0.05;
p<0.01.
3.3. Results of Conditional Model
Parameter coefficients of the direct and interaction effects are depicted in Table 4. Although the interaction effect between observation and nonreactivity on reappraisal was significant (B = 0.01, 95% BCI [0.002, 0.02]), the interaction effect on suppression was not statistically significant (B = 0.00, 95% BCI [−0.01, 0.01]).1 Furthermore, none of the direct effects of observation on symptom domains were statistically significant. Because nonreactivity only moderated the relationship between observation and reappraisal, this interaction term was preserved in the final model.
Table 4.
Parameter estimates of conditional model.
| Estimate | S.E. | Lower BCI | Upper BCI | ||
|---|---|---|---|---|---|
| Outcome Variable | Predictor Variable | ||||
| GAD Sx | |||||
| Observation | 0.45** | 0.02 | 0.41 | 0.49 | |
| Int. | 0.01 | 0.00 | 0.00 | 0.01 | |
| Reappraisal | −0.28** | 0.02 | −0.31 | −0.25 | |
| Nonreaction | −0.35** | 0.03 | −0.40 | −0.30 | |
| Suppression | 0.13** | 0.02 | 0.09 | 0.18 | |
| OCD Sx | |||||
| Observation | 1.12** | 0.05 | 1.02 | 1.21 | |
| Int. | 0.01 | 0.01 | −0.01 | 0.03 | |
| Reappraisal | −0.44** | 0.05 | −0.53 | −0.35 | |
| Nonreaction | −0.61** | 0.07 | −0.75 | −0.48 | |
| Suppression | 0.37** | 0.06 | 0.25 | 0.48 | |
| MDD Sx | |||||
| Observation | 0.51** | 0.02 | 0.46 | 0.55 | |
| Int. | 0.00 | 0.00 | −0.01 | 0.01 | |
| Reappraisal | −0.36** | 0.02 | −0.41 | −0.32 | |
| Nonreaction | −0.37** | 0.03 | −0.44 | −0.30 | |
| Suppression | 0.25** | 0.03 | 0.19 | 0.30 | |
| SAD Sx | |||||
| Observation | 0.52** | 0.04 | 0.45 | 0.59 | |
| Int. | −0.01 | 0.01 | −0.02 | 0.00 | |
| Reappraisal | −0.30** | 0.04 | −0.37 | −0.22 | |
| Nonreaction | −0.74** | 0.05 | −0.84 | −0.65 | |
| Suppression | 0.31** | 0.05 | 0.22 | 0.41 | |
| Reappraisal | |||||
| Observation | −0.07** | 0.03 | −0.12 | −0.02 | |
| Int. | 0.01** | 0.00 | 0.002 | 0.02 | |
| Nonreaction | 0.69** | 0.03 | 0.64 | 0.75 | |
| Suppression | |||||
| Observation | 0.03 | 0.02 | −0.01 | 0.07 | |
| Int. | 0.00 | 0.00 | −0.01 | 0.01 | |
| Nonreaction | 0.20** | 0.02 | 0.16 | 0.25 | |
Note: S.E. = Standard Error; BCI = Bootstrapped Confidence Intervals; Int. = Interaction between observation and nonreaction; Sx = symptoms;
p < 0.05;
p<0.01.
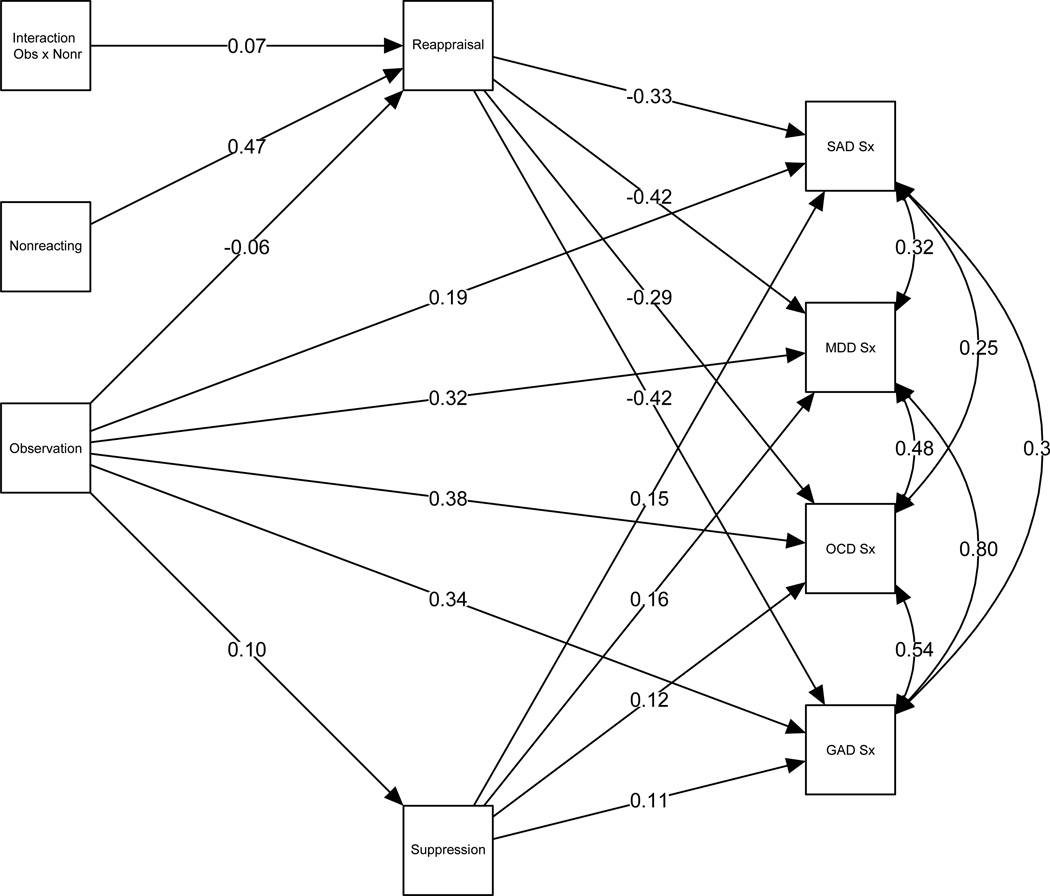
3.4. Results of Synthesized Conditional Process Model
All of the parameter coefficients of the final conditional process model are displayed in Table 5. The path diagram is depicted in Figure 3. Overall, the results indicated that nonreactivity significantly moderated the indirect effects of observation on each symptom domain through reappraisal (B = 0.01, 95% BCI [0.002, 0.02]). To probe the interaction effects, each indirect effect was estimated at −1, 0, and +1 standard deviations of nonreactivity. Inspection of these estimates in Table 5 reveals that the indirect effect on each symptom domain becomes stronger and positive as nonreactivity diminishes. Finally, all the indirect effects of observation on each symptom domain through suppression were positive and statistically significant, which is consistent with the results of the process model in Table 3.
Table 5.
Parameter estimates of conditional process model.
| Estimate | S.E. | Lower BCI | Upper BCI | ||
|---|---|---|---|---|---|
| Outcome Variable | Predictor Variable | ||||
| GAD Sx | |||||
| Observation | 0.36** | 0.02 | 0.32 | 0.40 | |
| Reappraisal | −0.38** | 0.02 | −0.41 | −0.35 | |
| Suppression | 0.14** | 0.02 | 0.09 | 0.18 | |
| OCD Sx | |||||
| Observation | 0.96** | 0.05 | 0.87 | 1.05 | |
| Reappraisal | −0.62** | 0.04 | −0.70 | −0.53 | |
| Suppression | 0.38** | 0.06 | 0.25 | 0.48 | |
| MDD Sx | |||||
| Observation | 0.42** | 0.02 | 0.37 | 0.46 | |
| Reappraisal | −0.47** | 0.02 | −0.51 | −0.43 | |
| Suppression | 0.26** | 0.03 | 0.19 | 0.31 | |
| SAD Sx | |||||
| Observation | 0.34** | 0.03 | 0.28 | 0.41 | |
| Reappraisal | −0.52** | 0.04 | −0.59 | −0.45 | |
| Suppression | 0.32** | 0.05 | 0.22 | 0.42 | |
| Reappraisal | |||||
| Observation | −0.07** | 0.03 | −0.12 | −0.02 | |
| Int. | 0.01** | 0.00 | 0.00 | 0.02 | |
| Nonreaction | 0.69** | 0.03 | 0.63 | 0.75 | |
| Suppression | |||||
| Observation | 0.08** | 0.02 | 0.05 | 0.12 | |
| Conditional Indirect Effects via Reappraisal | |||||
| O→R→GADHigh NR | 0.01 | 0.01 | −0.02 | 0.04 | |
| O→R→GADModerate NR | 0.03** | 0.01 | 0.01 | 0.05 | |
| O→R→GADLow NR | 0.05** | 0.01 | 0.03 | 0.07 | |
| O→R→OCDHigh NR | 0.01 | 0.02 | −0.03 | 0.06 | |
| O→R→OCDModerate NR | 0.05** | 0.02 | 0.01 | 0.08 | |
| O→R→OCDLow NR | 0.08** | 0.02 | 0.04 | 0.12 | |
| O→R→MDDHigh NR | 0.01 | 0.02 | −0.03 | 0.04 | |
| O→R→MDDModerate NR | 0.04** | 0.01 | 0.01 | 0.06 | |
| O→R→MDDLow NR | 0.06** | 0.01 | 0.03 | 0.09 | |
| O→R→SADHigh NR | 0.01 | 0.02 | −0.03 | 0.05 | |
| O→R→SADModerate NR | 0.04** | 0.01 | 0.01 | 0.07 | |
| O→R→SADLow NR | 0.07** | 0.02 | 0.04 | 0.10 | |
| Indirect Effects via Suppression | |||||
| O→S→GAD | 0.01** | 0.00 | 0.01 | 0.02 | |
| O→S→OCD | 0.03** | 0.01 | 0.02 | 0.05 | |
| O→S→MDD | 0.02** | 0.01 | 0.01 | 0.03 | |
| O→S→SAD | 0.03** | 0.01 | 0.01 | 0.04 | |
Note: Conditional indirect effects are displayed for low (−1 SD), moderate (0 SD), and high (+1 SD) levels of nonreactivity. S.E. = Standard Error; BCI = Bootstrapped Confidence Intervals; Int. = Interaction between observation and nonreaction; O = Observation; R = Reappraisal; S = Suppression; NR = Nonreaction; Sx = symptoms;
p < 0.05;
p<0.01.
Figure 3.
Synthesized Conditional Process Model.
Note: Error terms were omitted to simplify presentation. All coefficients are standardized.
4. Discussion
This study represents the first attempt to systematically evaluate the CPM of mindfulness and emotion regulation in the context of individual emotional disorders (i.e., generalized anxiety disorder, social anxiety disorder, obsessive compulsive disorder, and major depressive disorder). Although prior research has corroborated several tenets of the CPM (Desrosiers et al., 2014), it confined its investigation to broad psychopathological constructs and did not consider the role of suppression. The results of the current study provided empirical support for the CPM. Specifically, our first hypothesis was confirmed, as cognitive emotion regulation strategies mediated the relationship between observation and symptoms of each disorder. Both of the ancillary hypotheses were also supported. That is, increases in observation were associated with higher levels of both reappraisal and suppression. Whereas reappraisal predicted less symptoms of each disorder (hypothesis 1a), suppression predicted more symptoms (hypothesis 1b). Most of the effect sizes ranged from medium-small to small in magnitude. Results corroborated the second hypothesis, as nonreactivity moderated the indirect effects of observation on symptoms through a cognitive emotion regulation strategy. However, nonreactivity moderated only the indirect effect involving reappraisal (hypothesis 2a), as the interaction term predicting suppression was not significant (hypothesis 3a).
These findings accord well with prior literature. Research has demonstrated that observation of unwanted emotions often elicits more regulatory attempts using both adaptive and maladaptive strategies (Gruber, Harvey, & Gross, 2013). A study by Aldao and Nolen-Hoeksema (2013) revealed that individuals tended to respond to disgust eliciting stimuli by deploying multiple emotion regulation strategies regardless of each strategy’s adaptive utility. Whereas reactive observation of negative experiences can promote heightened symptoms (e.g., interoceptive awareness exacerbating panic disorder symptoms; Dunn et al., 2010), nonreactive observation of emotions may facilitate adaptive emotion regulation (Garland et al., 2015; Sauer & Baer, 2012). Our study is consistent with this research, as observation was positively associated with reappraisal and suppression. However, reappraisal was the only mediator that predicted decreased symptoms of each disorder. As for the moderated mediation effects, our results agreed with those of Desrosier et al. (2014), which indicated that nonreactivity moderated the indirect effect involving reappraisal. Specifically, the interaction was such that individuals with lower levels of nonreactivity used reappraisal less after observing their emotions, which predicted poorer health outcomes across each disorder.
The lack of an interaction effect on suppression contradicted one of the initial hypotheses in the CPM; however, a number of explanations could account for this discrepancy. One potential reason may pertain to the extreme rigidity of suppression. Because suppression paradoxically results in emotions of greater intensity and is characterized by inordinate inflexibility (Campbell-Sills, Barlow, Brown, & Hofmann, 2006; Gross & John, 2003), contextual factors such as nonreactivity may not be able to influence the extent to which one employs this strategy. In fact, most of the correlations between suppression and other constructs were either trivial or non-significant, indicating that several psychological processes may not robustly influence suppression use. Alternatively, these results could be a consequence of cultural factors. Research suggests that the effects of suppression differ across Asian and European cultures (Butler, Lee, & Gross, 2007). Butler et al. (2007) demonstrated that the habitual use of suppression was related to negative emotional experiences among individuals with European values, whereas these relationships were reversed among those with Asian values. One explanation for this cultural difference might pertain to differential capacities to use suppression in a flexible manner. Extant literature indicates that individuals from European cultures tend to use suppression rigidly, whereas individuals from Asian cultures are more sensitive to social context and environmental demands, which enables them to use suppression more flexibly (Butler et al., 2007; Morling, Kitayama, & Miyamoto, 2002). Perhaps nonreactivity did not moderate suppression use in the current sample beacause individuals from Japan already have a better capacity to employ suppression in a less rigid manner. Future research should carefully consider the role of cultural factors in the expression of emotion regulation and mindfulness.
When considering the results of the current study, certain limitations warrant mention. First, the cross-sectional design of this study precludes causal interpretations. It would be beneficial for future research to examine the temporal dynamics of the processes involved in the CPM. Second, using a clinical sample could limit the amount of variability needed to identify subtle interaction effects. However, the same pattern of results emerged even after re-conducting the analyses in the combined clinical and non-clinical sample. Third, certain methodological considerations may attenuate confidence in the results (e.g., self-report, etc.). In particular, the fact that certain constructs were assessed by the same scale (e.g., reappraisal and suppression) may produce shared method variance issues. Fourth, diagnoses for the current sample were obtained through self-report as to whether an individual received certain psychiatric diagnoses. Future studies should use formal diagnostic interviewing to confirm diagnoses. Fifth, interpretation of the results requires consideration of cultural factors involving the Japanese sample. Additional replication of the current results in diverse samples will be necessary to license generalization of the CPM. Sixth, mindfulness experience was not assessed, which may prevent generalization of the CPM to individuals who regularly engage in meditation and mind-body practices.
Nonetheless, a number of conclusions can be derived from the current study. Namely, the results suggest that the CPM is relevant to a variety of individual emotional disorders (i.e., generalized anxiety disorder, social anxiety disorder, obsessive compulsive disorder, and major depressive disorder). Given the excessive comorbidity and overlap among emotional disorders (Kessler, Chiu, Demler, & Walters, 2005; Curtiss & Klemanski, 2016), the CPM may afford a reasonable framework for understanding their co-occurrence. The core processes underlying the CPM (i.e., cognitive emotion regulation strategies and mindful nonreactivity) might contribute to the maintenance of emotional disorders. This would be in accordance with prior research indicating that nonreactivity contributes to the expression of emotional disorders (Curtiss & Klemanski, 2014b). Future research should consider these processes as potential treatment targets. Furthering our understanding of mindfulness and emotion regulation can inform both the conceptualization and treatment of emotional disorders.
Footnotes
When analyzed with the both clinical and non-clinical samples, the pattern of results remained the same. The interaction effect on reappraisal was significant (B = 0.01, 95% BCI [0.005, 2.02]), yet the interaction effect on suppression was not statistically significant (B = 0.00, 95% BCI [−0.05, 0.004]). Thus, we elected to proceed with the clinical sample, which is more relevant to our central aim.
References
- Aldao A, Nolen-Hoeksema S. One versus many: Capturing the use of multiple emotion regulation strategies in response to an emotion-eliciting stimulus. Cognition & Emotion. 2013;27:753–760. doi: 10.1080/02699931.2012.739998. [DOI] [PubMed] [Google Scholar]
- Aldao A, Nolen-Hoeksema S, Schweizer S. Emotion-regulation strategies across psychopathology: A meta-analytic review. Clinical Psychology Review. 2010;30:217–237. doi: 10.1016/j.cpr.2009.11.004. [DOI] [PubMed] [Google Scholar]
- Baer RA, Smith GT, Hopkins J, Krietemeyer J, Toney L. Using self-report assessment methods to explore facets of mindfulness. Assessment. 2006;13:27–45. doi: 10.1177/1073191105283504. [DOI] [PubMed] [Google Scholar]
- Bishop SR, Lau M, Shapiro S, Carlson L, Anderson ND, Carmody J, Devins G. Mindfulness: A proposed operational definition. Clinical Psychology: Science and Practice. 2004;11:230–241. [Google Scholar]
- Brown TA, Barlow DH. A proposal for a dimensional classification system based on the shared features of the DSM-IV anxiety and mood disorders: implications for assessment and treatment. Psychological Assessment. 2009;21:256–271. doi: 10.1037/a0016608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown TA, Naragon-Gainey K. Evaluation of the unique and specific contributions of dimensions of the triple vulnerability model to the prediction of DSM-IV anxiety and mood disorder constructs. Behavior Therapy. 2013;44:277–292. doi: 10.1016/j.beth.2012.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butler EA, Lee TL, Gross JJ. Emotion regulation and culture: are the social consequences of emotion suppression culture-specific? Emotion. 2007;7:30–48. doi: 10.1037/1528-3542.7.1.30. [DOI] [PubMed] [Google Scholar]
- Calvete E, Orue I, Hankin BL. Cross-Lagged Associations Among Ruminative Response Style, Stressors, and Depressive Symptoms in Adolescents. Journal of Social and Clinical Psychology. 2015;34:203–220. [Google Scholar]
- Campbell-Sills L, Barlow DH, Brown TA, Hofmann SG. Acceptability and Suppression of Negative Emotion in Anxiety and Mood Disorders. Emotion. 2006;6:587–595. doi: 10.1037/1528-3542.6.4.587. [DOI] [PubMed] [Google Scholar]
- Chambers R, Gullone E, Allen NB. Mindful emotion regulation: An integrative review. Clinical Psychology Review. 2009;29:560–572. doi: 10.1016/j.cpr.2009.06.005. [DOI] [PubMed] [Google Scholar]
- Chiesa A, Serretti A, Jakobsen JC. Mindfulness: Top–down or bottom–up emotion regulation strategy? Clinical Psychology Review. 2013;33:82–96. doi: 10.1016/j.cpr.2012.10.006. [DOI] [PubMed] [Google Scholar]
- Cribbie RA. Multiplicity control in structural equation modeling. Structural Equation Modeling. 2007;14:98–112. [Google Scholar]
- Curtiss J, Klemanski DH. Factor analysis of the five facet mindfulness questionnaire in a heterogeneous clinical sample. Journal of Psychopathology and Behavioral Assessment. 2014a;36:683–694. [Google Scholar]
- Curtiss J, Klemanski DH. Teasing apart low mindfulness: Differentiating deficits in mindfulness and in psychological flexibility in predicting symptoms of generalized anxiety disorder and depression. Journal of Affective Disorders. 2014b;166:41–47. doi: 10.1016/j.jad.2014.04.062. [DOI] [PubMed] [Google Scholar]
- Curtiss J, Klemanski DH. Taxonicity and network structure of generalized anxiety disorder and major depressive disorder: An admixture analysis and complex network analysis. Journal of Affective Disorders. 2016;199:99–105. doi: 10.1016/j.jad.2016.04.007. [DOI] [PubMed] [Google Scholar]
- Desrosiers A, Vine V, Curtiss J, Klemanski DH. Observing nonreactively: A conditional process model linking mindfulness facets, cognitive emotion regulation strategies, and depression and anxiety symptoms. Journal of Affective Disorders. 2014;165:31–37. doi: 10.1016/j.jad.2014.04.024. [DOI] [PubMed] [Google Scholar]
- Desrosiers A, Vine V, Klemanski DH, Nolen-Hoeksema S. Mindfulness and emotion regulation in depression and anxiety: common and distinct mechanisms of action. Depression and Anxiety. 2013;30:654–661. doi: 10.1002/da.22124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunn BD, Stefanovitch I, Evans D, Oliver C, Hawkins A, Dalgleish T. Can you feel the beat? Interoceptive awareness is an interactive function of anxiety-and depression-specific symptom dimensions. Behaviour Research and Therapy. 2010;48:1133–1138. doi: 10.1016/j.brat.2010.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feldman G, Hayes A, Kumar S, Greeson J, Laurenceau JP. Mindfulness and emotion regulation: The development and initial validation of the Cognitive and Affective Mindfulness Scale-Revised (CAMS-R) Journal of Psychopathology and Behavioral Assessment. 2007;29:177–190. [Google Scholar]
- Foa EB, Huppert JD, Leiberg S, Langner R, Kichic R, Hajcak G, Salkovskis PM. The Obsessive-Compulsive Inventory: development and validation of a short version. Psychological Assessment. 2002;14:485–496. [PubMed] [Google Scholar]
- Garland EL, Farb NA, Goldin PR, Fredrickson BL. The Mindfulness-to-Meaning Theory: Extensions, applications, and challenges at the attention–appraisal–emotion interface. Psychological Inquiry. 2015;26:377–387. [Google Scholar]
- Garland EL, Kiken LG, Faurot K, Palsson O, Gaylord SA. Upward Spirals of Mindfulness and Reappraisal: Testing the Mindfulness-to-Meaning Theory with Autoregressive Latent Trajectory Modeling. Cognitive Therapy and Research. 2016:1–12. [Google Scholar]
- Gross JJ. The emerging field of emotion regulation: an integrative review. Review of General Psychology. 1998;2:271–299. [Google Scholar]
- Gross JJ, John OP. Individual differences in two emotion regulation processes: Implications for affect, relationships, and well-being. Journal of Personality and Social Psychology. 2003;85:348–362. doi: 10.1037/0022-3514.85.2.348. [DOI] [PubMed] [Google Scholar]
- Gruber J, Harvey AG, Gross JJ. When trying is not enough: Emotion regulation and the effort–success gap in bipolar disorder. Emotion. 2012;12:997–1003. doi: 10.1037/a0026822. [DOI] [PubMed] [Google Scholar]
- Gu J, Strauss C, Bond R, Cavanagh K. How do mindfulness-based cognitive therapy and mindfulness-based stress reduction improve mental health and wellbeing? A systematic review and meta-analysis of mediation studies. Clinical Psychology Review. 2015;37:1–12. doi: 10.1016/j.cpr.2015.01.006. [DOI] [PubMed] [Google Scholar]
- Harnett PH, Reid N, Loxton NJ, Lee N. The relationship between trait mindfulness, personality and psychological distress: A revised reinforcement sensitivity theory perspective. Personality and Individual Differences. 2016;99:100–105. [Google Scholar]
- Hayes AM, Feldman G. Clarifying the construct of mindfulness in the context of emotion regulation and the process of change in therapy. Clinical Psychology: Science and Practice. 2004;11:255–262. [Google Scholar]
- Hofmann SG. Toward a cognitive-behavioral classification system for mental disorders. Behavior Therapy. 2014;45:576–587. doi: 10.1016/j.beth.2014.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofmann SG, Sawyer AT, Witt AA, Oh D. The effect of mindfulness-based therapy on anxiety and depression: A meta-analytic review. Journal of Consulting and Clinical Psychology. 2010;78:169–183. doi: 10.1037/a0018555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ishikawa R, Kobori O, Shimizu E. Development and validation of the Japanese version of the obsessive-compulsive inventory. BMC Research Notes. 2014;7:1–10. doi: 10.1186/1756-0500-7-306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ito M, Oe Y, Kato N, Nakajima S, Fujisato H, Miyamae M, Norman SB. Validity and clinical interpretability of Overall Anxiety Severity and Impairment Scale (OASIS) Journal of Affective Disorders. 2015;170:217–224. doi: 10.1016/j.jad.2014.08.045. [DOI] [PubMed] [Google Scholar]
- Kabat-Zinn J. Full catastrophe living: Using the wisdom of your body and mind to face stress, pain and illness. New York, NY: Delacorte; 1990. [Google Scholar]
- Kashdan TB, Goodman FR, Machell KA, Kleiman EM, Monfort SS, Ciarrochi J, Nezlek JB. A contextual approach to experiential avoidance and social anxiety: Evidence from an experimental interaction and daily interactions of people with social anxiety disorder. Emotion. 2014;14:769–781. doi: 10.1037/a0035935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demler O, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62:617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klemanski DH, Curtiss JE. Don't let your anxiety run your life: Using the science of emotion regulation and mindfulness to overcome fear and worry. Oakland, CA: New Harbinger Publications; 2016. [Google Scholar]
- Kroenke K, Spitzer RL. The PHQ-9: a new depression diagnostic and severity measure. Psychiatric Annals. 2002;32:509–515. [Google Scholar]
- Kuyken W, Watkins E, Holden E, White K, Taylor RS, Byford S, Dalgleish T. How does mindfulness-based cognitive therapy work? Behaviour Research and Therapy. 2010;48:1105–1112. doi: 10.1016/j.brat.2010.08.003. [DOI] [PubMed] [Google Scholar]
- Leary MR. A brief version of the Fear of Negative Evaluation Scale. Personality and Social Psychology Bulletin. 1983;9:371–375. [Google Scholar]
- Lutz A, Slagter HA, Dunne JD, Davidson RJ. Attention regulation and monitoring in meditation. Trends in Cognitive Sciences. 2008;12:163–169. doi: 10.1016/j.tics.2008.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McEvoy PM, Mahoney AE, Moulds ML. Are worry, rumination, and post-event processing one and the same?: Development of the Repetitive Thinking Questionnaire. Journal of Anxiety Disorders. 2010;24:509–519. doi: 10.1016/j.janxdis.2010.03.008. [DOI] [PubMed] [Google Scholar]
- Morling B, Kitayama S, Miyamoto Y. Cultural practices emphasize influence in the United States and adjustment in Japan. Personality and Social Psychology Bulletin. 2002;28:311–323. [Google Scholar]
- Muramatsu K, Kamijima K, Yoshida M, Otsubo T, Miyaoka H, Muramatsu Y, Gejyo F. The Patient Health Questionnaire, Japanese Version: Validity According to the Mini-International Neuropsychiatric Interview–Plus. Psychological Reports. 2007;101:952–960. doi: 10.2466/pr0.101.3.952-960. [DOI] [PubMed] [Google Scholar]
- Muramatsu K, Seiryou N, Muramatsu Y, Miyaoka H. Validation and utility of a Japanese version of the GAD-7. Panminerva Medica. 2009;51:79. [Google Scholar]
- Neale-Lorello D, Haaga DA. The “observing” facet of mindfulness moderates stress/symptom relations only among meditators. Mindfulness. 2015;6:1286–1291. [Google Scholar]
- Nixon R, Menne A, Kling L, Steele A, Barnes J, Dohnt H, Tyler H. Metacognition, working memory, and thought suppression in acute stress disorder. Australian Journal of Psychology. 2008;60:168–174. [Google Scholar]
- Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods. 2008;40:879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Kelley K. Effect Size Measures for Mediation Models: Quantitative Strategies for Communicating Indirect Effects. Psychological Methods. 2011;16:93–115. doi: 10.1037/a0022658. [DOI] [PubMed] [Google Scholar]
- Roemer L, Williston SK, Rollins LG. Mindfulness and emotion regulation. Current Opinion in Psychology. 2015;3:52–57. [Google Scholar]
- Rosseel Y. lavaan: An R package for structural equation modeling. Journal of Statistical Software. 2012;48:1–36. [Google Scholar]
- Sasagawa S, Kanai Y, Muranaka Y, Suzuki S, Shimada H, Sakano Y. Development of a Short Fear of Negative Evaluation Scale for Japanese using item response theory. Japanese Journal of Behavioral Therapy. 2004;30:87–98. [Google Scholar]
- Sauer SE, Baer RA. Ruminative and mindful self-focused attention in borderline personality disorder. Personality Disorders. 2012;3:433–441. doi: 10.1037/a0025465. [DOI] [PubMed] [Google Scholar]
- Sawada N, Uchida H, Watanabe K, Kikuchi T, Suzuki T, Kashima H, Mimura M. How successful are physicians in eliciting the truth from their patients? A large-scale Internet survey from patients' perspectives. The Journal of Clinical Psychiatry. 2012;73:311–317. doi: 10.4088/JCP.11m07078. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Archives of Internal Medicine. 2006;166:1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Sugiura Y, Sato A, Ito Y, Murakami H. Development and validation of the Japanese version of the Five Facet Mindfulness Questionnaire. Mindfulness. 2012;3:85–94. [Google Scholar]
- Teper R, Segal ZV, Inzlicht M. Inside the mindful mind how mindfulness enhances emotion regulation through improvements in executive control. Current Directions in Psychological Science. 2013;22:449–454. [Google Scholar]
- Yoshizu J, Sekiguchi R, Amemiya T. Development of a Japanese version ofemotion regulation questionnaire. Japanese Journal of Research on Emotions. 2013;20:56–62. [Google Scholar]