Abstract
Objective
Most research on irritability and child psychopathology has focused on depressive disorders, bipolar disorder, and/or oppositional defiant disorder (ODD). Less is known about relationships between child anxiety and irritability and moderators of such associations.
Method
Structural equation modeling (SEM) examined associations between anxiety severity and irritability in a large sample of treatment-seeking youth with anxiety disorders (N=663, ages 7–19 years, M=12.25), after accounting for comorbid depressive disorders and ODD. Additional analyses examined whether associations were moderated by child gender, age, and generalized anxiety disorder (GAD) status.
Results
There was a direct link between child anxiety and irritability even after accounting for comorbid depressive disorders and ODD. Links between child anxiety and irritability were robust across child gender and age. Further, relationships between child anxiety and irritability were comparable across youth with and without GAD, suggesting that the anxiety–irritability link is relevant across child anxiety disorders and not circumscribed to youth with GAD.
Conclusion
Findings add to an increasing body of evidence linking child irritability to a range of internalizing and externalizing psychopathologies, and suggest that child anxiety assessment should systematically incorporate irritability evaluations. Further, youth in clinical settings displaying irritability should be assessed for the presence of anxiety. Moreover, treatments for childhood anxiety may do well to incorporate new treatment modules as needed that specifically target problems of irritability.
Keywords: anxiety, irritability, child, SEM, tantrums
INTRODUCTION
Serious irritability—characterized by increased reactivity to negative emotional stimuli, commonly accompanied by anger and temper outbursts1—affects roughly 3-5% of the general population.2-4 Empirical advances in recent years have clarified the very heavy burdens associated with chronic irritability, which include prospective and cross-sectional links with both externalizing and internalizing psychopathologies and elevated risk for a range of functional impairments.3,5-8 Research has linked irritability with the affective disorders, impulse control and conduct disorders, and the most recent DSM iteration added a new depressive disorder category—disruptive mood dysregulation disorder (DMDD)9,10—that places chronic irritability and developmentally inappropriate temper outbursts at the core of its definition. Longitudinal work shows that even after controlling for psychiatric disorders, irritability prospectively predicts lower income, less educational attainment8 and suicidality,11 underscoring the need to better understand irritability and its links with psychopathology in affected clinical populations.
The majority of research on irritability and child psychopathology has focused on depression, bipolar disorder, and/or oppositional defiant disorder (ODD),12-15 although a small but growing body of research is finding that irritability may also be linked with anxiety disorders. Stringaris and Goodman16 found irritability to prospectively predict internalizing disorders broadly beyond just depression, although they did not further break down their analyses to examine irritability associations with anxiety disorders specifically. Irritability is included in the DSM-5 as a qualifying associated symptom of generalized anxiety disorder (GAD), and a recent study found roughly 90% of a sample of treatment-seeking youth with GAD showed persistent irritability.17 Although irritability is specifically mentioned in the definition of GAD and research has most commonly found irritability to be predictive of GAD diagnosis among youth with anxiety,17-20 research on adult populations and emerging research on child populations have found irritability may be associated with a range of anxiety disorders.21,22
In community samples, episodic irritability has been prospectively linked with GAD and specific phobias.7 In a more recent analysis, Stoddard et al21 found irritability to be greater among a heterogeneous group of youth with anxiety than among healthy controls. Further, across the anxiety disorders, social anxiety disorder and separation anxiety disorder (but not GAD) uniquely predicted parent-reported irritability. In contrast, the reverse was true with regard to child-reported irritability.
Importantly, child anxiety disorders are highly comorbid with depressive disorders23,24 and with ODD,25,26 which in turn are classes of disorder shown to be robustly linked with irritability themselves.12,14 As such, the extent to which irritability is directly related to anxiety, or whether significant anxiety–irritability associations are simply artifacts of anxiety co-presentations with depression and ODD, remains unclear. Research considering links between anxiety and irritability must control for the co-occurring depression and ODD symptoms. Moreover, much of the limited work specifically examining the link between anxiety disorders and irritability21 has focused on between-group comparisons of anxious versus healthy controls. Between-group comparison cannot inform the extent to which linear relationships exist between anxiety and irritability, such that increased anxiety severity is associated with greater irritability. Examinations of such relationships are critical for identifying children at greatest risk and for optimally informing treatment.
Moreover, the limited work examining irritability in relation to child anxiety has not sufficiently considered potential age and gender effects. Indeed, both anxiety and irritability show differential presentation patterns across age and gender. For example, among the anxiety disorders, GAD (which has been most commonly linked with irritability) shows the latest age of onset, whereas specific phobias and separation anxiety disorder typically show much earlier onsets,27 and girls show higher rates of anxiety than boys.28 As such, if irritability shows a greater association with GAD than with other anxiety disorders, it might follow that associations between anxiety severity and irritability become stronger with age. Regarding irritability, population-based research shows onset seems to occur on average in the early preschool years,5 and rates of episodic irritability increase with child age.7 Person-centered research evaluating intra-individual irritability trajectories between ages 3 and 9 find the most common trajectories are associated with low or moderate irritability at age 3 that declines through age 9.29 In contrast, 11% of youth follow trajectories associated with high irritability at age 3 that remains steady through age 9, and another 2% show high irritability at age 3 that significantly increases through age 9.29 Analyses of individual trajectories among adolescents suggests that irritability is relatively stable in later childhood, although a considerable proportion of children with moderate chronic irritability show declines with age through adolescence and young adulthood.7, 30
As with anxiety, girls show higher rates of irritability than boys.7 Given population-based research showing irritability to be intricately linked with negative affect,12 and given higher rates of negative affect in females, it is possible that the anxiety–irritability link is stronger in females than in males. Accordingly, given these developmental and gender-based variations in anxiety and in irritability, links between anxiety and irritability may be more complex than previous research has identified.
Much remains to be learned about the relationships between anxiety and irritability, including: (a) the extent to which increased anxiety severity is linked with increased irritability (going beyond simple between-group differences of controls with and without anxiety); (b) the extent to which anxiety–irritability links are simply artifacts of anxiety co-presentations with depression and ODD; (c) the extent to which anxiety–irritability links are just concentrated among youth with GAD; and (d) the extent to which anxiety–irritability links are robust across age and gender, or whether such demographic factors moderate associations.
Moreover, research to date examining anxiety–irritability links has relied exclusively on single indicators to capture child anxiety (most commonly structured diagnostic interviews) or has examined parent and child reports in separate models. Given the limitations and measurement error inherent in relying on a single indicator to measure child anxiety,31 continued work in this area would be best served by analyses that incorporate multiple observed indicators of child anxiety that can collectively isolate measurement error from the latent construct of child anxiety severity when modeling associations with irritability. Theoretically, such an approach would offer a more accurate assessment of the structural relationships between anxiety and irritability among youth with anxiety disorders, after accounting for comorbid depressive disorders and ODD. Additional analyses examined whether associations between anxiety severity and irritability were moderated by child gender, age, and GAD status.
METHOD
Participants
Participants were 663 consecutive children between the ages of 7 and 19 (M=12.25 SD=3.11; 54.1% female; 82.2% self-identified as non-Hispanic White or Caucasian) and their parents presenting between 2004 and 2013 for child assessment and/or treatment services at a large, university-affiliated outpatient clinic for anxiety disorders in New England. All youth met diagnostic criteria for a DSM-IV-TR anxiety disorder as determined by structured diagnostic interview. Most participants’ parents were married (78.1%). Families ranged in resources: 19.6% were at or below 300% of the national poverty line for their year (e.g., in 2007 $63,609 for a family of four; $75,240 for a family of five) whereas 11.3% of households earned at least 600% of the national poverty line at their year of assessment (e.g., in 2007 $127,218 for a family of four; $150,480 for a family of five).
Regarding diagnosis, 19.3% of youth had a principal diagnosis of GAD, 13.2% had a principal diagnosis of social phobia, 10.2% had a principal diagnosis of obsessive-compulsive disorder (OCD), 10.3% had a principal diagnosis of separation anxiety disorder, 9.6% had a principal diagnosis of specific phobia, 8.7% had a principal diagnosis of anxiety disorder not-otherwise-specified, and 7.4% had a principal diagnosis of panic disorder with agoraphobia.
Overall, youth in the sample met criteria for the following comorbid DSM-IV disorders: GAD (38.5%), social anxiety disorder (32%), specific phobia (25.1%), separation anxiety disorder (19%), OCD (17.3%), anxiety disorder not otherwise specified (14.6%), panic disorder with agoraphobia (10%), attention-deficit/hyperactivity disorder (9.0%), major depressive disorder (MDD; 6.3%), dysthymic disorder (3.3%), depressive disorder not otherwise specified (3.2%), agoraphobia without a history of panic disorder (2.7%), trichotillomania (2.3%), enuresis (1.9%), selective mutism (1.4%), panic disorder without agoraphobia (1.4%), posttraumatic stress disorder (.9%), and disruptive behavior disorder not otherwise specified (0.4%). In addition, 12.7% of the sample met criteria for a depressive disorder (MDD, dysthymic disorder, or depressive disorder not otherwise specified) and 3.3% of children met criteria for ODD. The mean number of diagnoses youth met criteria for is 3.36 (SD =1.63).
Measures/Model Indicators
Child diagnoses
The Anxiety Disorders Interview Schedule, Child and Parent Version (ADIS-IV-C/P)32 is a semi-structured diagnostic interview administered to parents and children to assess present-state internalizing and externalizing problems according to DSM-IV-TR criteria, with time frames for assessing current symptoms varying across diagnoses in accordance with the DSM-IV-TR. The ADIS-C/P is the most widely used interview for the assessment of child anxiety disorders and has demonstrated strong reliability, validity, and sensitivity to change.33,34 Symptom reports inform diagnoses in strict accordance with the DSM-IV-TR, and diagnoses are assigned a clinical severity rating (CSR) ranging from 0 (no symptoms) to 8 (extremely severe symptoms); CSRs >4 indicate that diagnostic criteria for the particular disorder has been met, and CSRs <3 indicate subthreshold diagnostic presentation. DSM-IVTR diagnoses are determined using child and parent reports; parent and child diagnostic profiles are integrated into a composite diagnostic profile using the “or” rule.31
Child anxiety severity
Anxiety severity was assessed via two indicators that included (1) an expert evaluator rating and (2) a child report. The first indicator was the ADIS-IV CSR (described above) assigned by the expert evaluator to characterize the severity of the child's principal anxiety disorder. The second indicator of anxiety severity was the total score from the Multidimensional Anxiety Scale for Children (MASC),35 a 39-item self-report measure administered to children to assess symptoms of anxiety occurring “recently.” The MASC has demonstrated very strong psychometric properties across samples (α=.88 in present sample).34-37
Child irritability
Consistent with previous research examining child irritability,29,38,39,40 we used three strategic items from the Child Behavior Checklist (CBCL), an established and well-supported parent-report of behavioral and emotional problems in children 6–18.41 Parents rate each of 120 items from 0 (not true) to 2 (very true or often true) about their child across the past 6 months. The three items (CBCL Irritability Item 1: “stubborn, sullen or irritable”; CBCL Irritability Item 2: “sudden changes in mood or feelings”; and CBCL Irritability Item 3: “temper tantrums or hot temper”) comprise an irritability scale that has been psychometrically supported in previous literature examining these three items with exploratory factor analysis.40 Several studies in recent literature have used these items to measure irritability in youth.29,38,39,40 Internal consistency across these items was acceptable in the present sample (α=.74).
Procedure
Families first completed a standardized phone screen as part of clinic procedures; youth were excluded who had current psychotic symptoms, suicidal or homicidal risk requiring crisis intervention, two or more hospitalizations for severe psychopathology (e.g., psychosis) within the previous 5 years, or moderate to severe intellectual impairments. Youth on psychotropic medications were required to be stabilized on their current dosages for at least 1 month. After obtaining informed consent/assent, participating youth and their families were assessed via the ADIS-IV-C/P; youth and their mothers also completed the MASC and CBCL, respectively, as part of a prescreening battery for treatment. A diagnostician administered parent and child interviews (ADIS-IV-C/P) separately, and generated a composite diagnostic profile for each child by applying the “or” rule to integrate parent and child reports.31 Diagnostic decisions strictly adhered to DSM-IV-TR criteria. For each participant, the assessment materials for each informant were presented and reviewed at a weekly diagnostic meeting, where symptoms were reviewed and consensus from the diagnostic team was met. Diagnosticians included a team of 22 clinical psychologists, postdoctoral associates, and doctoral candidates specializing in the assessment and treatment of pediatric anxiety disorders. Diagnosticians met internal training and reliability criteria: participating in didactics (including training from one of the developers of the ADIS-IV-C/P), observing 3 completed interviews, collaboratively administering 3 interviews with a trained diagnostician, and conducting supervised interviews until achieving full diagnostic profile agreement on 3 of 5 consecutively supervised assessments. These criteria were developed in collaboration with an author of the ADIS-IV-C/P.
Data Analysis
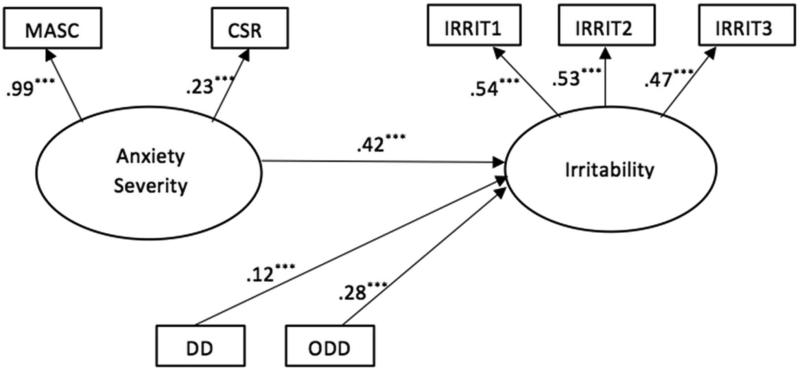
Structural equation modeling was used to examine relationships between the latent variables of anxiety severity and irritability. The ADIS-IV-C/P CSR of the child's principal anxiety disorder and the child-report MASC total score were used as indicators of anxiety severity. The three CBCL items detailed above were used as indicators of irritability. The highest depressive disorder (MDD, dysthymic disorder, or depressive disorder not otherwise specified) CSR and the ODD CSR, as assessed by the ADIS-IV-C/P, were added to the model as covariates (see Figure 1). As the use of a variety of model fit indices is recommended,42 model fit was evaluated using standard guidelines for the root mean square error of approximation (RMSEA), standardized root mean square residual (SRMR), and comparative fit index (CFI). To examine the robustness of observed associations between anxiety severity and irritability, structural relations were examined across categorical moderating subgroups based on age, gender, and GAD status using the multi-group structural equation modeling approach. Specifically, we compared older (≥12 years; n=333) and younger (<12 years; n=330) children (12 was selected as the age cutoff based on research showing relatively stable trajectories of irritability after age 1230 and varying trajectories of irritability in early to middle childhood29), males (n=303) and females (n=359), and youth with (GAD CSR >4; n=255) and without GAD (GAD CSR ≤3; n=408) using multi-group or stacked models. This approach estimates an unconstrained model—in which all parameters are estimated separately for each group—as well as a constrained model in which specific paths (here, the relationship between the anxiety latent factor and the irritability latent factor) are required to be equal across groups; subsequently, the constrained and unconstrained models were compared using procedures set forth by Satorra and Bentler.43 All analyses were conducted in MPlus 6.1244 and used robust standard error estimates.
Figure 1.
Parameter estimates for base model. Note: Endogenous variables are correlated, although these correlations are omitted from this figure for ease of interpretation. CSR = Clinical severity rating of principal DSM-IV-TR anxiety diagnosis, as determined by the Anxiety Disorders Interview Schedule for Children (ADIS-IV-C/P); DD = Depressive disorder CSR; IRRIT1, IRRIT2, IRRIT3 = Child Behavior Checklist items 86, 87, and 95 (respectively); MASC = Multidimensional Anxiety Scale for Children (Child Report) Total Score; ODD = Oppositional defiant disorder CSR. *** p < .001
Missing values analysis
All models were estimated using full information maximum likelihood (FIML). To examine patterns of missing data, a missing values analysis45 evaluated whether individuals included in the main analyses differed from excluded individuals (i.e., cases with missing data from any study variable). Child age was lower among those with missing MASC values (9.7% missing), CBCL Irritability Item 1 (14% missing), CBCL Irritability Item 2 (14% missing), and CBCL Irritability Item 3 (14% missing). Accordingly, age was included as an auxiliary variable in all models to account for missing values.46 Age was not associated with missing CSR values (1% missing), and no other study variables were associated with missing data.
RESULTS
Table 1 presents the means, standard deviations, medians, and bivariate correlations across all study variables. Pairwise associations among the child irritability indicators were medium to large in magnitude, and pairwise associations among the child anxiety severity indicators were small to medium in magnitude.
Table 1.
Correlations Between Variables
| M (SD) | median | 1. | 2. | 3. | 4. | 5. | 6. | |
|---|---|---|---|---|---|---|---|---|
| 1. Child-reported anxiety severitya | 48.7 (18.4) | 48 | - | |||||
| 2. Clinician-rated anxiety severityb | 5.5 (.9) | 5.0 | .15*** | - | ||||
| 3. Irritability item 1c | 0.9 (0.7) | 1 | .07 | .19*** | - | |||
| 4. Irritability Item 2d | 0.8 (0.7) | 1 | .11** | .10* | .55*** | - | ||
| 5. Irritability Item 3e | 0.6 (0.8) | 0 | .04 | .07 | .49*** | .44*** | - | |
| 6. Depressive disorder severityf | .74 (1.7) | 0 | .12** | .30*** | .19*** | .19*** | .07 | - |
| 7. ODD severityg | .25 (.98) | 0 | −.06 | .10* | .19*** | .18** | .22*** | .00 |
Multidimensional Anxiety Scale for Children Total Score.
Principal anxiety diagnosis clinical severity rating (CSR) assessed via the Anxiety Disorders Interview Schedule for Children.
Item 86 on the Child Behavior Checklist (CBCL; “stubborn, sullen, or irritable”).
Item 87 on the CBCL (“sudden changes in mood or feelings”).
Item 95 on the CBCL (“temper tantrums or hot temper”).
Depressive disorder CSR.
Oppositional defiant disorder (ODD) CSR.
p<.05
p<.01
p<.001
Structural relationship between anxiety severity and irritability
The fit of the overall model in the full sample (see Figure 1) was statistically over-identified, allowing us to evaluate fit of the model. Collectively, fit indices indicated that this model provided a good fit to the data (χ2[12] = 25.42, p < .05; RMSEA = .04 [90% CI .02–.06], p > .05; CFI = .98, SRMR = .04). Residuals for each of the observed measures were generally low, suggesting that these measures were reasonable indicators of the latent anxiety severity and irritability constructs. Figure 1 presents the parameter estimates for the model. The standardized coefficient between the Anxiety Severity and Irritability latent variables was .42 after controlling for depressive disorder and ODD severity, indicating that increased anxiety was indeed directly associated with greater child irritability. The model collectively accounted for roughly 29% of the variance in child irritability (R2 = 0.29, SE = 0.09, p < .01), with anxiety severity specifically accounting for roughly 16% of the variance in child irritability.
Evaluating the potential moderating roles of age, gender, and GAD status
To evaluate the potential moderating roles of age, gender, and GAD, multi-group structural equation modeling was used to compare males and females, older and younger youth, and youth with and without GAD. Chi-square statistics compared a model in which all parameters were allowed to be unequal across groups and a model with the anxiety to irritability path constrained to be equal across groups, using the scaling correction for robust standard errors.43 A non-significant test indicates that the anxiety to irritability relationship is not different across the groups, i.e., the group variable does not moderate the effect. The model with all parameters freely estimated in male and female youth was not significantly different from the model with the anxiety to irritability path equal (Χ2[1] = .03, p > .05). The model with all parameters freely estimated in older and younger youth was not significantly different from the model with the anxiety to irritability path equal (Χ2[1] = 2.56, p > .05). The model with all parameters freely estimated in youth with and without GAD was not significantly different from the model with the anxiety to irritability path equal (Χ2[1] = .16, p > .05).
Further, subsequent analyses examined the relationship between anxiety and irritability as moderated by the presence of separation anxiety disorder, social anxiety disorder, and specific phobia. As with GAD, none of these anxiety disorders moderated the relationship (all p's>.05) (data not shown).
DISCUSSION
The present findings add to an increasing body of evidence in recent years linking child irritability to a range of internalizing and externalizing psychopathologies12-15 by documenting a unique link between anxiety severity and irritability among youth with anxiety disorders. Whereas a small number of studies have begun exploring anxiety–irritability associations,7,17,21 the present study is the first to go beyond between-group differences of controls with and without anxiety to consider anxiety severity continuously and to examine the extent to which anxiety–irritability links are not simply artifacts of anxiety co-presentations with depressive disorders and ODD. Given the very serious clinical correlates of irritability across the lifespan,8,11 the present findings suggest that child anxiety assessment practices should systematically incorporate evaluations of irritability. Moreover, given the very negative life course associated with the anxiety disorders,23,47-50 youth displaying irritability should be assessed for the presence of anxiety. Indeed, child anxiety symptoms often go unnoticed,51,52 whereas problems of irritability may be more easily observable to the adults in children's lives. Given the robust association presently observed between irritability and anxiety, child irritability may prove to be a useful indicator that anxiety should also be assessed.
Importantly, we found the link between anxiety and irritability was not simply concentrated among youth with GAD, but rather presented across the full range of child anxiety disorders. At present, GAD is the only anxiety disorder for which irritability is formally included as part of its diagnostic criteria. The present finding that the anxiety–irritability link is not specific to GAD is consistent with previous research showing that social anxiety disorder, separation anxiety disorder, and specific phobias are also associated with irritability,7,21-22 and suggests that future iterations of the diagnostic nomenclature may do well to more broadly incorporate irritability across anxiety disorder definitions.
Future work is needed to examine prospective links between irritability and anxiety to examine issues of temporal precedence. The present design does not inform whether irritability plays a causal role in the development of anxiety, or whether anxiety has a causal role in the development of irritability. It is possible that early irritability is linked with broader temperamental characteristics and general negative affectivity that place children at risk for the development of anxiety disorders. It is also possible that anxiety symptoms and associated negative affect and distress intolerance increase the risk of irritable responding among affected youth. Interestingly, recent longitudinal work has found that irritability is more predictive of subsequent anxious/depressed symptoms than anxious/depressed symptoms are predictive of subsequent irritability.39 Future longitudinal research is needed in order to examine these potential trajectories further, as well as potential dynamic transactional pathways in which anxiety and irritability mutually influence one another across time.
Genetically informed research suggests that irritability is a heritable characteristic, and one strongly linked genetically with depression.38,39 Further, both genetic and (to a lesser extent) environmental factors appear to play a role in cross-sectional and longitudinal associations between irritability and internalizing symptoms more broadly.38,39 In addition to continuing to examine genetic influences associated with the co-variation of irritability and anxiety, research is needed to consider environmental influences—such as family factors and parenting experiences—that may affect the expression of concomitant irritability and anxiety among genetically vulnerable youth. For example, parents with depression are known to show elevated hostility and less warmth relative to parents without depression. Given that the offspring of the former are more likely to show child anxiety, and given that child anxiety disorders are associated with considerable family dysfunction,48,53-55 research would do well to examine whether family environment experiences, such as parental hostility and low warmth, influence trajectories of irritability and child anxiety among children of parents with depression.
The observed links between irritability and anxiety may help to explain, in part, the increasingly prominent role that second-generation antipsychotic medications have assumed in the management of anxiety disorders across the lifespan.56 Despite the absence of controlled trials establishing the safety and efficacy of antipsychotic medications for treating anxiety disorders, between 1996 and 2007, there was a roughly twofold increase among psychiatrists in the rate of antipsychotic prescribing for anxiety disorders, with the proportion of anxiety disorder visits in which an antipsychotic medication was prescribed increasing from one in every ten visits to one in every five visits.56 Although off-label prescribing is not inherently cause for concern, the serious metabolic, endocrine, and cerebrovascular risks associated with second-generation antipsychotic medications,57 as well as the concerning absence of supporting evidence for their role in reducing anxiety disorders, have raised increasing concerns over quality of anxiety disorder care in practice settings. Given the present findings linking irritability with anxiety, and given controlled evaluations supporting the use of antipsychotic medications to treat irritability in youth with autism spectrum disorders,58,59 it is possible that some of the rising antipsychotic prescribing practices for patients with anxiety reflect practitioners targeting irritability associated with anxiety rather than core anxiety symptoms themselves. Although epidemiologic research documents rising trends in the antipsychotic management of anxiety disorders, such work offers no insight into clinical decision making at the individual level. Future work is needed to examine the extent to which practitioners prescribing antipsychotic medications to treat anxiety disorders may be specifically targeting irritability associated with anxiety, and the extent to which such practices are yielding clinical benefit with regard to irritability associated with anxiety.
To date, no treatments directly target irritability presenting within anxious youth. Although selective serotonin reuptake inhibitors (SSRIs) can be effective in reducing irritability in adults,62 the literature is mixed regarding the performance of SSRIs for treating youth with irritability.4,63-65 Cognitive-behavioral therapy (CBT) can be an effective psychotherapeutic approach to treating severe irritability and associated mood dysregulation,66 but established CBT for child anxiety does not directly target irritability.67 Accordingly, much remains to be learned about the pharmacologic and psychotherapeutic management of irritability in youth with anxiety.
Several study limitations warrant comment. First, this study was conducted in a university-based, urban clinic specializing in anxiety disorders in a predominantly Caucasian New England sample. Findings may not generalize to youth in other clinical settings or to the general population of youth with anxiety. Second, the assessments used did not permit examination of different types of child irritability. Given research documenting the usefulness of distinguishing chronic from episodic irritability,4,7 future work incorporating alternative assessment methods would do well to test whether anxiety–irritability relationships differ as a function of chronic versus episodic irritability. Third, as noted, the present analyses were cross-sectional. Future work incorporating longitudinal designs is needed to examine issues of temporal precedence in the links between anxiety and irritability, and to inform pathways of influence between anxiety and irritability across development. In addition, although all of the measures included assess current symptoms, the specific time frames vary somewhat across measures. For example, the CBCL assesses symptoms “now or within the past 6 months,” whereas the MASC assesses how the child has been feeling “recently.” It is thus possible that observed associations do not reflect contemporaneous relations. Finally, although a multi-informant approach was utilized—including collecting reports from children, mothers, and clinicians—and although SEM used multiple indicators of study variables to collectively isolate measurement error from the latent constructs, future work incorporating psychophysiological and other biological data is critical for considering neurodevelopmental mechanisms that may underlie associations between child anxiety and irritability.
Despite these limitations, the present study offers a rare statistical portrait of the unique association between irritability and anxiety severity among children with anxiety disorders, and adds to a growing body of research linking child irritability to a range of internalizing and externalizing psychopathologies. Given the robust association between irritability and child anxiety presently observed, child anxiety assessment practices would do well to incorporate evaluations of child irritability. As there are several evidence-based treatment options for childhood anxiety disorders67 research is needed to examine whether irritability moderates treatment outcomes such that the presence of irritability indicates some treatment options are preferable over others. Moreover, treatments for childhood anxiety disorders may do well to incorporate new treatment modules as needed that specifically target problems of irritability.
Acknowledgments
This work was supported by the National Institutes of Health (K23 MH090247, R01 MH068277).
Dr. Coxe served as the statistical expert for this research.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosure: Drs. Coxe, Pincus, and Comer and Mss. Cornacchio and Crum report no biomedical financial interests or potential conflicts of interest.
Contributor Information
Ms. Danielle Cornacchio, Mental Health Interventions and Technology (MINT) Program, Center for Children and Families, Florida International University, Miami..
Ms. Kathleen I. Crum, Mental Health Interventions and Technology (MINT) Program, Center for Children and Families, Florida International University, Miami..
Dr Stefany Coxe, Mental Health Interventions and Technology (MINT) Program, Center for Children and Families, Florida International University, Miami..
Dr. Donna B. Pincus, Center for Anxiety and Related Disorders (CARD), Boston University, Boston..
Dr Jonathan S. Comer, Mental Health Interventions and Technology (MINT) Program, Center for Children and Families, Florida International University, Miami..
REFERENCES
- 1.Stringaris A. Irritability in children and adolescents: A challenge for DSM-5. Eur Child Adolesc Psychiatry. 2011;20:61–6. doi: 10.1007/s00787-010-0150-4. [DOI] [PubMed] [Google Scholar]
- 2.Althoff RR, Verhulst FC, Rettew DC, Hudziak JJ, van der Ende J. Adult outcomes of childhood dysregulation: A 14-year follow-up study. J Am Acad Child Adolesc Psychiatry. 2010;49:1105–16. doi: 10.1016/j.jaac.2010.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brotman MA, Schmajuk M, Rich BA, et al. Prevalence, clinical correlates, and longitudinal course of severe mood dysregulation in children. Biol Psychiatry. 2006;60:991–7. doi: 10.1016/j.biopsych.2006.08.042. [DOI] [PubMed] [Google Scholar]
- 4.Leibenluft E, Stoddard J. The developmental psychopathology of irritability. Dev Psychopathol. 2013;25:1473–87. doi: 10.1017/S0954579413000722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dougherty LR, Smith VC, Bufferd SJ, et al. Preschool irritability: Longitudinal associations with psychiatric disorders at age 6 and parental psychopathology. J Am Acad Child Adolesc Psychiatry. 2013;52:1304–13. doi: 10.1016/j.jaac.2013.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stringaris A, Goodman R. Mood lability and psychopathology in youth. Psychol Med. 2009;39:1237–45. doi: 10.1017/S0033291708004662. [DOI] [PubMed] [Google Scholar]
- 7.Leibenluft E, Cohen P, Gorrindo T, Brook JS, Pine DS. Chronic versus episodic irritability in youth: A community-based, longitudinal study of clinical and diagnostic associations. J Child Adolesc Psychopharmacol. 2006;16:456–66. doi: 10.1089/cap.2006.16.456. [DOI] [PubMed] [Google Scholar]
- 8.Stringaris A, Cohen P, Pine DS, Leibenluft E. Adult outcomes of youth irritability: A 20-year prospective community-based study. Am J Psychiatry. 2009;166:1048–54. doi: 10.1176/appi.ajp.2009.08121849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 5th ed. American Psychiatric Association; Washington, DC: 2013. [Google Scholar]
- 10.Roy AK, Lopes V, Klein RG. Disruptive mood dysregulation disorder: A new diagnostic approach to chronic irritability in youth. Am J Psychiatry. 2014;171:918–24. doi: 10.1176/appi.ajp.2014.13101301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pickles A, Aglan A, Collishaw S, Messer J, Rutter M, Maughan B. Predictors of suicidality across the life span: The isle of wight study. Psychol Med. 2010;40:1453–66. doi: 10.1017/S0033291709991905. [DOI] [PubMed] [Google Scholar]
- 12.Fava M, Hwang I, Rush AJ, Sampson N, Walters EE, Kessler RC. The importance of irritability as a symptom of major depressive disorder: Results from the national comorbidity survey replication. Mol Psychiatry. 2010;15:856–67. doi: 10.1038/mp.2009.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hunt JI, Case BG, Birmaher B, et al. Irritability and elation in a large bipolar youth sample: Relative symptom severity and clinical outcomes over 4 years. J Clin Psychiatry. 2013;74:e110–e117. doi: 10.4088/JCP.12m07874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Burke JD, Boylan K, Rowe R, et al. Identifying the irritability dimension of ODD: Application of a modified bifactor model across five large community samples of children. J Abnorm Psychol. 2014;123:841–51. doi: 10.1037/a0037898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Burke JD. An affective dimension within oppositional defiant disorder symptoms among boys: Personality and psychopathology outcomes into early adulthood. J Child Psychol Psychiatry. 2012;53:1176–83. doi: 10.1111/j.1469-7610.2012.02598.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Stringaris A, Goodman R. Longitudinal outcome of youth oppositionality: Irritable, headstrong, and hurtful behaviors have distinctive predictions. J Am Acad Child Adolesc Psychiatry. 2009;48:404–12. doi: 10.1097/CHI.0b013e3181984f30. [DOI] [PubMed] [Google Scholar]
- 17.Comer JS, Pincus DB, Hofmann SG. Generalized anxiety disorder and the proposed associated symptoms criterion change for DSM-5 in a treatment-seeking sample of anxious youth. Depress Anxiety. 2012;29:994–1003. doi: 10.1002/da.21999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kendall PC, Pimentel SS. On the physiological symaptom constellation in youth with generalized anxiety disorder (GAD). J Anxiety Disord. 2003;17:211–21. doi: 10.1016/s0887-6185(02)00196-2. [DOI] [PubMed] [Google Scholar]
- 19.Pina AA, Silverman WK, Alfano CA, Saavedra LM. Diagnostic efficiency of symptoms in the diagnosis of DSM-IV: Generalized anxiety disorder in youth. J Child Psychol Psychiatry. 2002;43:959–67. doi: 10.1111/1469-7610.00100. [DOI] [PubMed] [Google Scholar]
- 20.Tracey SA, Chorpita BF, Douban J, Barlow DH. Empirical evaluation of DSM-IV generalized anxiety disorder criteria in children and adolescents. J Clin Child Psychol. 1997;26:404–14. doi: 10.1207/s15374424jccp2604_9. [DOI] [PubMed] [Google Scholar]
- 21.Stoddard J, Stringaris A, Brotman MA, Montville D, Pine DS, Leibenluft E. Irritability in child and adolescent anxiety disorders. Depress Anxiety. 2014;31:566–73. doi: 10.1002/da.22151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Perlis RH, Fava M, Trivedi MH, et al. Irritability is associated with anxiety and greater severity, but not bipolar spectrum features, in major depressive disorder. Acta Psychiatr Scand. 2009;119:282–9. doi: 10.1111/j.1600-0447.2008.01298.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cummings CM, Caporino NE, Kendall PC. Comorbidity of anxiety and depression in children and adolescents: 20 years after. Psychol Bull. 2014;140:816–45. doi: 10.1037/a0034733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Comer JS, Kendall PC. High-end specificity of the children's depression inventory in a sample of anxiety-disordered youth. Depress Anxiety. 2005;22:11–9. doi: 10.1002/da.20059. [DOI] [PubMed] [Google Scholar]
- 25.Drabick DAG, Gadow KD, Loney J. Co-occurring ODD and GAD symptom groups: Source-specific syndromes and cross-informant comorbidity. J Am Acad Child Adolesc Psychiatry. 2008;37:314–26. doi: 10.1080/15374410801955862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fraire MG, Ollendick TH. Anxiety and oppositional defiant disorder: A transdiagnostic conceptualization. Clin Psychol Rev. 2013;33:229–40. doi: 10.1016/j.cpr.2012.11.004. [DOI] [PubMed] [Google Scholar]
- 27.Comer JS, Olfson M. The epidemiology of anxiety disorders. In: Simpson HB, Neria Y, Lewis-Fernández R, Schneier F, editors. Anxiety Disorders: Theory, Research and Clinical Perspectives. Cambridge University Press; New York: 2010. pp. 6–19. [Google Scholar]
- 28.Costello EJ, Mustillo S, Erkanli A, Keeler G, Angold A. Prevalence and development of psychiatric disorders in childhood and adolescence. Arch Gen Psychiatry. 2003;60:837–44. doi: 10.1001/archpsyc.60.8.837. [DOI] [PubMed] [Google Scholar]
- 29.Wiggins JL, Mitchell C, Stringaris A, Leibenluft E. Developmental trajectories of irritability and bidirectional associations with maternal depression. J Am Acad Child Adolesc Psychiatry. 2014;53:1191–1205. doi: 10.1016/j.jaac.2014.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Caprara GV, Paciello M, Gerbino M, Cugini C. Individual differences conducive to aggression and violence: Trajectories and correlates of irritability and hostile rumination through adolescence. Aggressive Behav. 2007;33:359–74. doi: 10.1002/ab.20192. [DOI] [PubMed] [Google Scholar]
- 31.Comer JS, Kendall PC. A symptom-level examination of parent-child agreement in the diagnosis of anxious youths. J Am Acad Child Adolesc Psychiatry. 2004;43:878–86. doi: 10.1097/01.chi.0000125092.35109.c5. [DOI] [PubMed] [Google Scholar]
- 32.Silverman WK, Albano AM. The anxiety disorders interview schedule for children for DSM-IV: Child and parent versions. Psychological Corporation; San Antonio: 1997. [Google Scholar]
- 33.Silverman WK, Ollendick TH. Evidence-based assessment of anxiety and its disorders in children and adolescents. J Clin Child Adolesc Psychol. 2005;34:380–411. doi: 10.1207/s15374424jccp3403_2. [DOI] [PubMed] [Google Scholar]
- 34.Wood JJ, Piacentini JC, Bergman RL, McCracken J, Barrios V. Concurrent validity of the anxiety disorders section of the anxiety disorders interview schedule for DSM-IV: Child and parent versions. J Clin Child Adolesc Psychol. 2002;31:335–42. doi: 10.1207/S15374424JCCP3103_05. [DOI] [PubMed] [Google Scholar]
- 35.March JS, Parker JDA, Sullivan K, Stallings P, Conners CK. The multidimensional anxiety scale for children (MASC): Factor structure, reliability, and validity. J Am Acad Child Adolesc Psychiatry. 1997;36:554–65. doi: 10.1097/00004583-199704000-00019. [DOI] [PubMed] [Google Scholar]
- 36.March JS, Albano AM. New developments in assessing pediatric anxiety disorders. Advances in Clinical Child Psychology. 1998;20:213–41. [Google Scholar]
- 37.March JS, Sullivan K, Parker J. Test–retest reliability of the multidimensional anxiety scale for children. J Anxiety Disord. 1999;13:349–58. doi: 10.1016/s0887-6185(99)00009-2. [DOI] [PubMed] [Google Scholar]
- 38.Stringaris A, Zavos H, Leibenluft E, Maughan B, Eley TC. Adolescent irritability: Phenotypic associations and genetic links with depressed mood. Am J Psychiatry. 2012;169:47–54. doi: 10.1176/appi.ajp.2011.10101549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Savage J, Verhulst B, Copeland W, Althoff RR, Lichtenstein P, Roberson-Nay R. A genetically informed study of the longitudinal relation between irritability and anxious/depressed symptoms. J Am Acad Child Adolesc Psychiatry. 2015;54:377–84. doi: 10.1016/j.jaac.2015.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Roberson-Nay R, Leibenluft E, Brotman MA, et al. Longitudinal stability of genetic and environmental influences on irritability: From childhood to young adulthood. Am J Psychiatry. 2015;172:657–664. doi: 10.1176/appi.ajp.2015.14040509. [DOI] [PubMed] [Google Scholar]
- 41.Achenbach TM RL. Manual for the ASEBA school-age forms and profiles. University of Vermont, Research Center for Children, Youth, and Families; Burlington, VT: 2001. [Google Scholar]
- 42.Jaccard J, Wan CK. LISREL approaches to interaction effects in multiple regression. Sage Publications, Inc.; Thousand Oaks, CA: 1996. pp. 98–vi.pp. 98 [Google Scholar]
- 43.Satorra A, Bentler PM. Latent variables analysis: Applications for developmental research. Sage Publications, Inc.; Thousand Oaks, CA: 1994. Corrections to test statistics and standard errors in covariance structure analysis. pp. 399–419. [Google Scholar]
- 44.Muthén B. New methods for the analysis of change. American Psychological Association; Washington, DC: 2001. Second-generation structural equation modeling with a combination of categorical and continuous latent variables: New opportunities for latent class–latent growth modeling. pp. 291–322. [Google Scholar]
- 45.Little RJ. A test of missing completely at random for multivariate data with missing values. J Am Stat Assoc. 1988;83:1198–1202. [Google Scholar]
- 46.Enders CK. Applied missing data analysis. Guilford Press; New York: 2010. pp. 377–xv.pp. 377 [Google Scholar]
- 47.Benjamin CL, Harrison JP, Settipani CA, Brodman DM, Kendall PC. Anxiety and related outcomes in young adults 7 to 19 years after receiving treatment for child anxiety. J Consult Clin Psychol. 2013;81:865–76. doi: 10.1037/a0033048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Pagani LS, Japel C, Vaillancourt T, Côté S, Tremblay RE. Links between life course trajectories of family dysfunction and anxiety during middle childhood. J Abnorm Child Psychol. 2008;36:41–53. doi: 10.1007/s10802-007-9158-8. [DOI] [PubMed] [Google Scholar]
- 49.Comer JS, Blanco C, Hasin DS, et al. Health-related quality of life across the anxiety disorders: Results from the national epidemiologic survey on alcohol and related conditions (NESARC). J Clin Psychiatry. 2011;72:43–50. doi: 10.4088/JCP.09m05094blu. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Wu P, Goodwin RD, Fuller C, et al. The relationship between anxiety disorders and substance use among adolescents in the community: Specificity and gender differences. J Youth Adolesc. 2010;39:177–88. doi: 10.1007/s10964-008-9385-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Briesch AM, Ferguson TD, Volpe RJ, Briesch JM. Examining teachers’ perceptions of social-emotional and behavioral referral concerns. Remedial Spec Educ. 2013;34:249–56. [Google Scholar]
- 52.Costello EJ, He J, Sampson NA, Kessler RC, Merikangas KR. Services for adolescents with psychiatric disorders: 12-month data from the national comorbidity Survey—Adolescent. Psychiatric Services. 2014;65:359–66. doi: 10.1176/appi.ps.201100518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Bögels SM, Brechman-Toussaint ML. Family issues in child anxiety: Attachment, family functioning, parental rearing and beliefs. Clin Psychol Rev. 2006;26:834–56. doi: 10.1016/j.cpr.2005.08.001. [DOI] [PubMed] [Google Scholar]
- 54.McLeod BD, Wood JJ, Weisz JR. Examining the association between parenting and childhood anxiety: A meta-analysis. Clin Psychol Rev. 2007;27:155–72. doi: 10.1016/j.cpr.2006.09.002. [DOI] [PubMed] [Google Scholar]
- 55.Thompson-Hollands J, Kerns CE, Pincus DB, Comer JS. Parental accommodation of child anxiety and related symptoms: Range, impact, and correlates. J Anxiety Disord. 2014;28:765–73. doi: 10.1016/j.janxdis.2014.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Comer JS, Mojtabai R, Olfson M. National trends in the antipsychotic treatment of psychiatric outpatients with anxiety disorders. Am J Psychiatry. 2011;168:1057–65. doi: 10.1176/appi.ajp.2011.11010087. [DOI] [PubMed] [Google Scholar]
- 57.Olfson M, Marcus SC, Corey-Lisle P, Tuomari AV, Hines P, L'ltalien GJ. Hvperilipidemia following treatment with antipsychotic medications. Am J Psychiatry. 2006;163:1821–5. doi: 10.1176/ajp.2006.163.10.1821. [DOI] [PubMed] [Google Scholar]
- 58.Kirino E. Efficacy and safety of aripiprazole in child and adolescent patients. Eur Child Adolesc Psychiatry. 2012;21:361–8. doi: 10.1007/s00787-012-0270-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Stigler KA, Mullett JE, Erickson CA, Posey DJ, McDougle CJ. Paliperidone for irritability in adolescents and young adults with autistic disorder. Psychopharmacology (Berl ) 2012;223:237–45. doi: 10.1007/s00213-012-2711-3. [DOI] [PubMed] [Google Scholar]
- 60.de la Cruz LF, Simonoff E, McGough JJ, Halperin JM, Arnold LE, Stringaris A. Treatment of children with attention-deficit/hyperactivity disorder (ADHD) and irritability: Results from the multimodal treatment study of children with ADHD (MTA). J Am Acad Child Adolesc Psychiatry. 2015;54:62–70. doi: 10.1016/j.jaac.2014.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Childress AC, Arnold V, Adeyi B, et al. The effects of lisdexamfetamine dimesylate on emotional lability in children 6 to 12 years of age with ADHD in a double-blind placebo-controlled trial. J Atten Disord. 2014;18:123–132. doi: 10.1177/1087054712448252. [DOI] [PubMed] [Google Scholar]
- 62.Andrews W, Parker G, Barrett E. The SSRI antidepressants: Exploring their “other” possible properties. J Affect Disord. 1998;49:141–4. doi: 10.1016/s0165-0327(97)00203-6. [DOI] [PubMed] [Google Scholar]
- 63.Duggal HS, Pathak PC, Coleman CC. Treating selective serotonin reuptake inhibitor-induced behavioral activation with valproate. J Child Adolesc Psychopharmacol. 2003;13:113–4. doi: 10.1089/104454603321666270. [DOI] [PubMed] [Google Scholar]
- 64.Strawn JR, Adler CM, McNamara RK, et al. Antidepressant tolerability in anxious and depressed youth at high risk for bipolar disorder: A prospective naturalistic treatment study. Bipolar Disord. 2014;16:523–30. doi: 10.1111/bdi.12113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Leibenluft E. Severe mood dysregulation, irritability, and the diagnostic boundaries of bipolar disorder in youths. Am J Psychiatry. 2011;168:129–42. doi: 10.1176/appi.ajp.2010.10050766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Leigh E, Smith P, Milavic G, Stringaris A. Mood regulation in youth: Research findings and clinical approaches to irritability and short-lived episodes of mania-like symptoms. Curr Opin in Psychiatry. 2012;25:271–6. doi: 10.1097/YCO.0b013e3283534982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Walkup JT, Albano AM, Piacentini J, et al. Cognitive behavioral therapy, sertraline, or a combination in childhood anxiety. N Engl J Med. 2008;359:2753–66. doi: 10.1056/NEJMoa0804633. [DOI] [PMC free article] [PubMed] [Google Scholar]