Abstract
Background:
Endotracheal intubation and prolonged immobilization of patients receiving mechanical ventilation may reduce expectoration function. High-frequency chest wall oscillation (HFCWO) may ameliorate airway secretion movement; however, the instantaneous changes in patients’ cardiopulmonary responses are unknown. Moreover, HFCWO may influence ventilator settings by the vigorous oscillation. The aim of this study was to investigate these issues.
Methods:
Seventy-three patients (52 men) aged 71.5 ± 13.4 years who were intubated with mechanical ventilation for pneumonic respiratory failure were recruited and randomly classified into 2 groups (HFCWO group, n = 36; and control group who received conventional chest physical therapy (CCPT, n = 37). HFCWO was applied with a fixed protocol, whereas CCPT was conducted using standard protocols. Both groups received sputum suction after the procedure. Changes in ventilator settings and the subjects’ responses were measured at preset intervals and compared within groups and between groups.
Results:
Oscillation did not affect the ventilator settings (all P > 0.05). The mean airway pressure, breathing frequency, and rapid shallow breathing index increased, and the tidal volume and SpO2 decreased (all P < 0.05). After sputum suction, the peak airway pressure (Ppeak) and minute ventilation decreased (all P < 0.05). The HFCWO group had a lower tidal volume and SpO2 at the end of oscillation, and lower Ppeak and tidal volume after sputum suction than the CCPT group.
Conclusions:
HFCWO affects breathing pattern and SpO2 but not ventilator settings, whereas CCPT maintains a steadier condition. After sputum suction, HFCWO slightly improved Ppeak compared to CCPT, suggesting that the study extends the indications of HFCWO for these patients in intensive care unit. (ClinicalTrials.gov number NCT02758106, retrospectively registered.)
Keywords: acute respiratory failure, chest physiotherapy, high-frequency chest wall oscillation, mechanical ventilatory support
1. Introduction
Pneumonia may increase bronchial secretion and decrease mucociliary function, thereby causing lung atelectasis.[1] Cough function is paramount for expectoration; however, coughing is not practical for acute pneumonic patients with respiratory failure receiving endotracheal intubation, mechanical ventilation, and sedation.[1] These patients may therefore have a large amount of pulmonary secretions,[2–5] thereby worsening bronchial hygiene, oxyhemoglobin saturation, ventilation-perfusion match, and lung atelectasis or collapse.[1,6,7] Although pneumonia is not currently an indication for chest physical therapy,[8] acute pneumonic patients with respiratory failure receiving mechanical ventilation and sedation may have the risk to develop atelectasis or lobar collapse, thereby potentially having the indication.
Conventional chest physical therapy (CCPT) may dislodge airway secretions.[9] High-frequency chest wall oscillation (HFCWO), mimicking a “mini-cough” by compressing and relaxing the chest wall to generate an oscillated volume from the lungs, can dislodge airway secretions as efficiently as CCPT[4,9,10] and can therefore save manpower to conduct CCPT.[11] However, most studies that have reported no significant effects of HFCWO, as these outcome measurements focusing on mortality, hospital stay,[4] lung function[12,13] or BODE score (a multidimensional 10-point scale for evaluation of chronic obstructive pulmonary disease)[12] are not associated with the immediate effects of chest physical therapy and may be seriously affected by other factors such as disease severity.[14] Using the amount of sputum as the outcome measurement of HFCWO is not strongly recommended.[15–17]
Although measurement of immediate cardiopulmonary changes in patients receiving HFCWO is more explicit and practical than lung function and BODE score, the measurement has not been studied in patients receiving mechanical ventilation. Additionally, changes in ventilator settings caused by HFCWO are a concern when the patients receive both treatments simultaneously. The aim of this study was to investigate the effect of HFCWO on pneumonic subjects with acute respiratory failure receiving mechanical ventilation by evaluating immediate cardiopulmonary changes and changes in the initial ventilator settings caused by oscillation.
2. Methods
We conducted this randomized controlled single-blinded study at a university hospital between January 1, 2014 and February 28, 2016. The participants were randomly allocated to the study group or the control group on a 1:1 ratio using a computer-generated randomization schedule. Adult subjects with pneumonia complicated with acute respiratory failure requiring endotracheal intubation and mechanical ventilation were consecutively recruited from a medical intensive care unit (ICU) (20-bed capacity). Pneumonia was defined as the presence of new or progressive pulmonary infiltrates and 2 of the following: body temperature >38.3°C or <36°C; white blood cell count >12,000 cells/mL or <4000 cells/mL; purulent tracheal secretions without other signs of infection requiring antimicrobial treatment. Acute respiratory failure was defined as a sudden decrease in PaO2 <60 mmHg (or arterial oxyhemoglobin saturation <90%) with or without PaCO2 >45 mmHg.[18–20] All of the patients had sufficient sputum production to require the physician to order airway secretion clearance. Disease severity was assessed by Acute Physiology and Chronic Health Evaluation II score at admission to the ICU.[21] Adverse events were evaluated by the investigators and reported to the institutional review board. The exclusion criteria were pregnancy, pneumothorax, manifest hemoptysis, unstable hemodynamics (i.e., despite aggressive fluid resuscitation, systolic blood pressure <90 mmHg or drop >40 mmHg, or mean arterial blood pressure <60 mmHg), increased intracranial pressure, and the status following major thoracotomy or abdominal surgery.
All of the eligible patients had acute pneumonic respiratory failure and received endotracheal intubation and mechanical ventilation, and their surrogates signed informed consent forms as the subjects had been intubated before each experiment started. The indications of endotracheal intubation and institution of mechanical ventilation are when, despite “optimal” medical therapy and oxygen administration there is moderate-to-severe acidosis (pH <7.36) and hypercapnia (arterial carbon dioxide tension, PaCO2 >45–60 mmHg) and breathing frequency ≥30 breaths/min. The patients were randomly allocated to the study group (HFCWO) or the control group (CCPT), as the efficacy of bronchial hygiene for both HFCWO and CCPT is comparable.[4] The primary investigators (MLC and CYL) were blinded to which procedure the patients received. The local institutional review board of Chung Shan Medical University Hospital approved this study (No. CS13004). This study is registered at ClinicalTrials.gov (NCT02758106). The experimental research was conducted in compliance with the Helsinki Declaration.
To prevent vomiting during or after chest care, all of the subjects underwent the procedure 1 hour before or 2 hours after feeding via a nasogastric tube.[1] Inhalation therapy was performed with an aerosolized solution of 6 mL of half saline via the ventilator before HFCWO or CCPT.[1]
HFCWO was performed using a Vest Airway Clearance System Model 105 (Hill-Rom, St. Paul, MN) connected to a vest via 2 flexible tubes by trained nurses who were blinded to the purpose of the study. All of the nurses had been well trained in how to perform both HFCWO and CCPT before the study, as these procedures are routinely performed by nurses at our institution. HFCWO was applied to each subject at a frequency of 10 to 12 Hz and a pulse pressure setting of 1 to 2 selected from a scale ranging from 1 to 10 (arbitrary units) for 15 minutes.[2] The patients receiving HFCWO were placed in a semiupright sitting position, and the patients undergoing CCPT received cup-hand percussion with the hands positioned 3 inches from the chest, striking the chest with a waving movement while they were placed in right and left decubitus positions for 5 to 10 minutes each.[1] Following HFCWO or CCPT, suction was performed immediately via an endotracheal tube.[15]
For detecting the instantaneous effects of both techniques, the measurements were undertaken during a single session, usually at the first time use of HFCWO or CCPT. Changes to the initial ventilator settings during HFCWO were recorded by the trained nurses by checking the ventilator panel before and at 5, 10, and 15 minutes during HFCWO. The variables included peak airway pressure (Ppeak), positive-end expiratory pressure, respiratory rate, fraction of inspired oxygen, inspiratory time, and sensitivity settings.
Changes in the patients’ cardiopulmonary responses were measured before and at 5, 10, and 15 minutes during oscillation and at 15 minutes after sputum suction. The measurement protocol for the CCPT group was the same as for the HFCWO group, except no measurements were taken at 5 or 10 minutes during percussion because it was not possible for a single nurse to perform percussion and record measurements at the same time.
Rapid shallow breathing index (RSBI) was calculated as follows:
RSBI = breathing frequency (breaths/minute)/tidal volume (liters)[22] (1)
Oxyhemoglobin saturation was measured using a pulse oximeter (SpO2) and validated with SaO2 of arterial blood measured with a blood gas analyzer.
The predetermined primary outcome measure was differences in the Ppeak between baseline and 15 minutes after suction. The predetermined secondary outcome measures were differences in the other cardiopulmonary variables between baseline and 15 minutes after suction.
Randomization was conducted using a computer-generated randomization schedule. As both techniques are equally efficacious in dislodging airway secretions,[4,9,10] it is not our intention to detect which is better than the other. Rather, the change of Ppeak between baseline and 15 minutes after sputum suction in either group is our primary outcome. Therefore, sample size of either group with an expected dropout rate of 10% was estimated on the assumption of mean change of Ppeak between the 2 time points being 1 mmHg and standard deviation (SD) being 2 mmHg. Sample size was 37 with an α level of 0.05 and a power of 0.8.
Intent-to-treat analysis was used between the HFCWO group and the CCPT group in this study. Data were presented as mean ± SD or median (interquartile range). For each outcome variable, comparisons were planned a priori. A paired t or unpaired t test was used for within-group or between-group comparisons. For non-normal data, the Mann–Whitney U test was used. The χ2 test or Fisher exact test was used to compare proportions of categorical variables between the 2 groups. A P value <0.05 was considered to be statistically significant. All statistical analyses were performed using SAS software version 9.3 (SAS Institute Inc, Cary, NC) and Microcal Origin version 4.0 (Northampton, MA).
3. Results
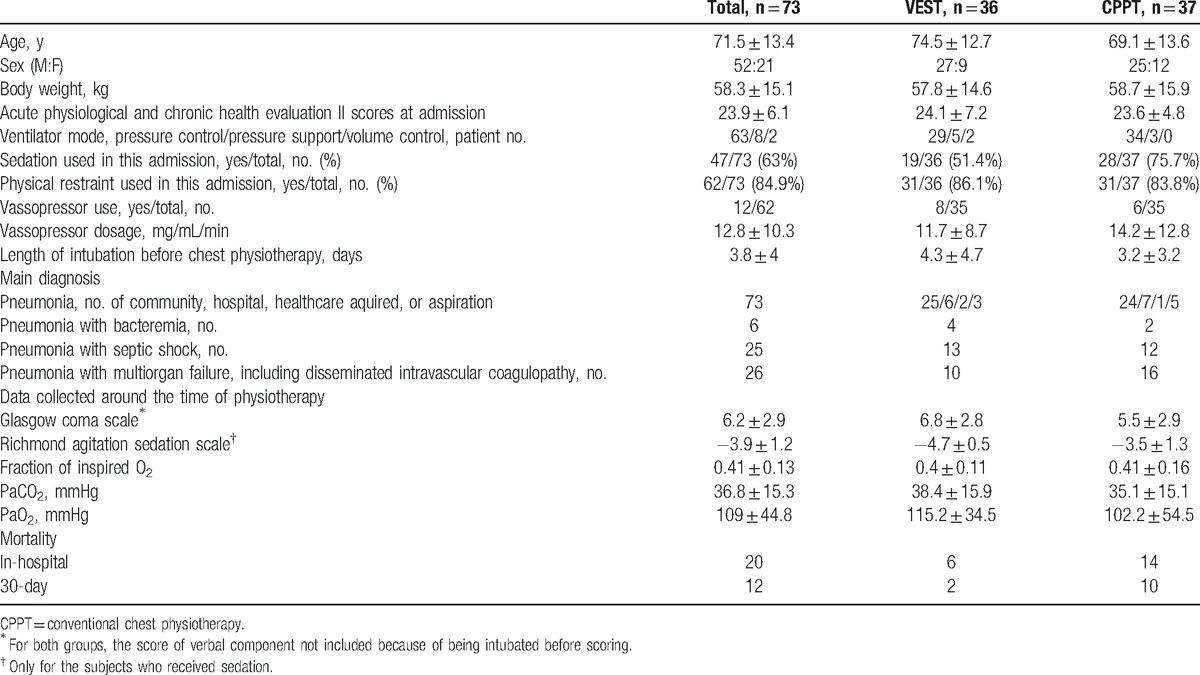
Of the 118 patients screened (Fig. 1), 73 patients (52 men), aged 71.5 ± 13.4 years with pneumonic respiratory failure were randomized in this study (Table 1), with 36 in the HFCWO group and 37 in the CCPT group. No subject dropped out from either the HFCWO group or the CCPT group.
Figure 1.
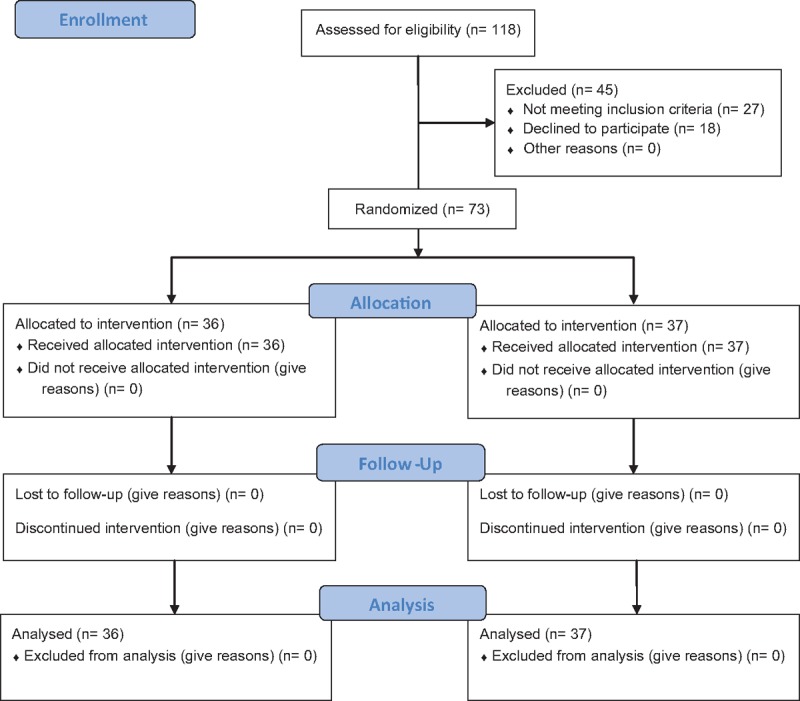
Flow diagram. A total of 118 patients with acute pneumonic respiratory failure receiving mechanical ventilatory support were screened. Forty-five patients were excluded, and 73 subjects were randomly allocated to the high-frequency chest wall oscillation group or conventional chest physiotherapy group with a 1:1 ratio.
Table 1.
Demographic data and disease entities of pneumonic patients complicated with sepsis and acute respiratory failure.
There were no significant changes in ventilator settings during HFCWO (Table 2, all P > 0.05). During oscillation, there were no significant changes in Ppeak, minute ventilation, systolic blood pressure, or heart rate compared to the baseline values (Figs. 2 and 3, all P > 0.05); however, there were significant increase in Pmean, breathing frequency, and RSBI at the 5th and 10th minutes (Fig. 4, all P < 0.001) and diastolic blood pressure at 10th minute (Fig. 3, P < 0.05). At the 15th minute, Pmean, breathing frequency and diastolic blood pressure returned to baseline levels (Figs. 3 and 4); however, RSBI remained higher than the baseline level (Fig. 4, P < 0.05). The tidal volume and SpO2 were significantly lower during the procedure, respectively (Fig. 5, baseline vs. at the 5th, 10th, and 15th minute, all P < 0.05–0.001, and baseline vs. at the 10th and the 15th minute, both P < 0.05, respectively). At the 15th minute after sputum suction, Ppeak and minute ventilation were significantly lower than the baseline levels (Fig. 2, both P < 0.05), whereas the other variables returned to baseline levels (Figs. 2–5, all P > 0.05).
Table 2.
Ventilator setting changes in response to high-frequency chest wall oscillating (n = 36).
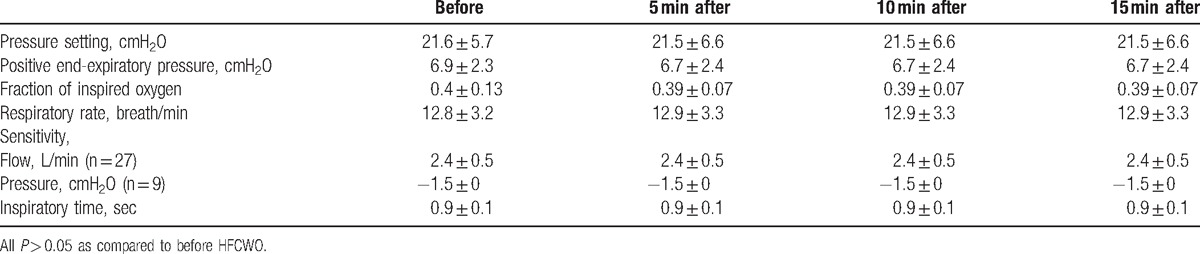
Figure 2.
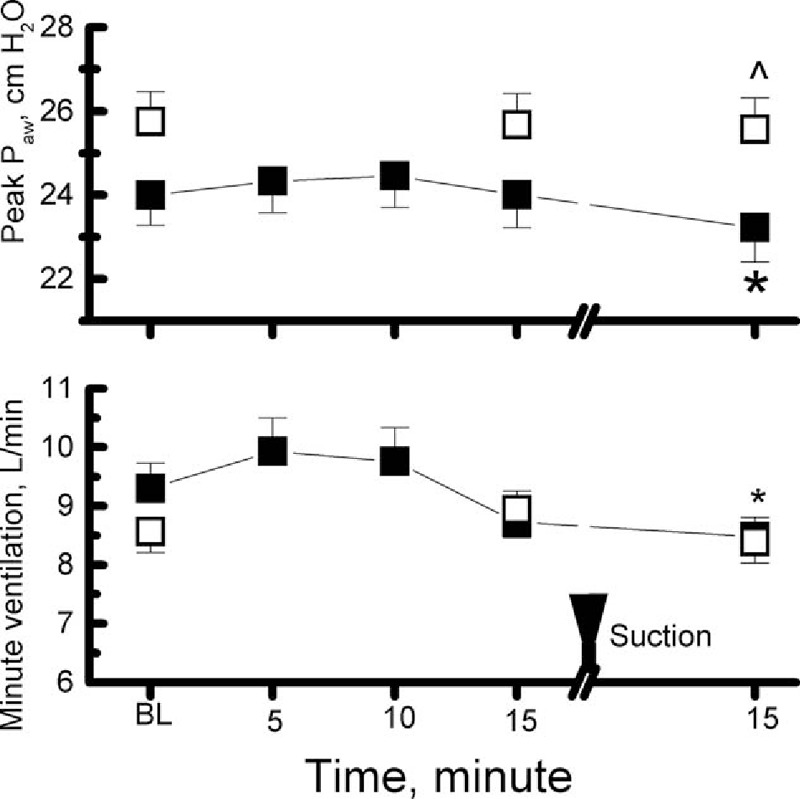
Changes in pulmonary physiology during high-frequency chest wall oscillation (HFCWO) for 5, 10, and 15 minutes and 15 minutes after sputum suction and during conventional chest physiotherapy (CCPT) for 15 minutes and 15 minutes after sputum suction. Each solid symbol indicates the mean of each variable at each time point of the HFCWO group; each open symbol indicates the mean of each variable at each time point of the CCPT group; bars indicate standard error (SE); within-group comparisons to the baseline: ∗P < 0.05, between-group comparisons: ^P < 0.05; BL = baseline, Paw = airway pressure. Upside-down triangle indicates sputum suction.
Figure 3.
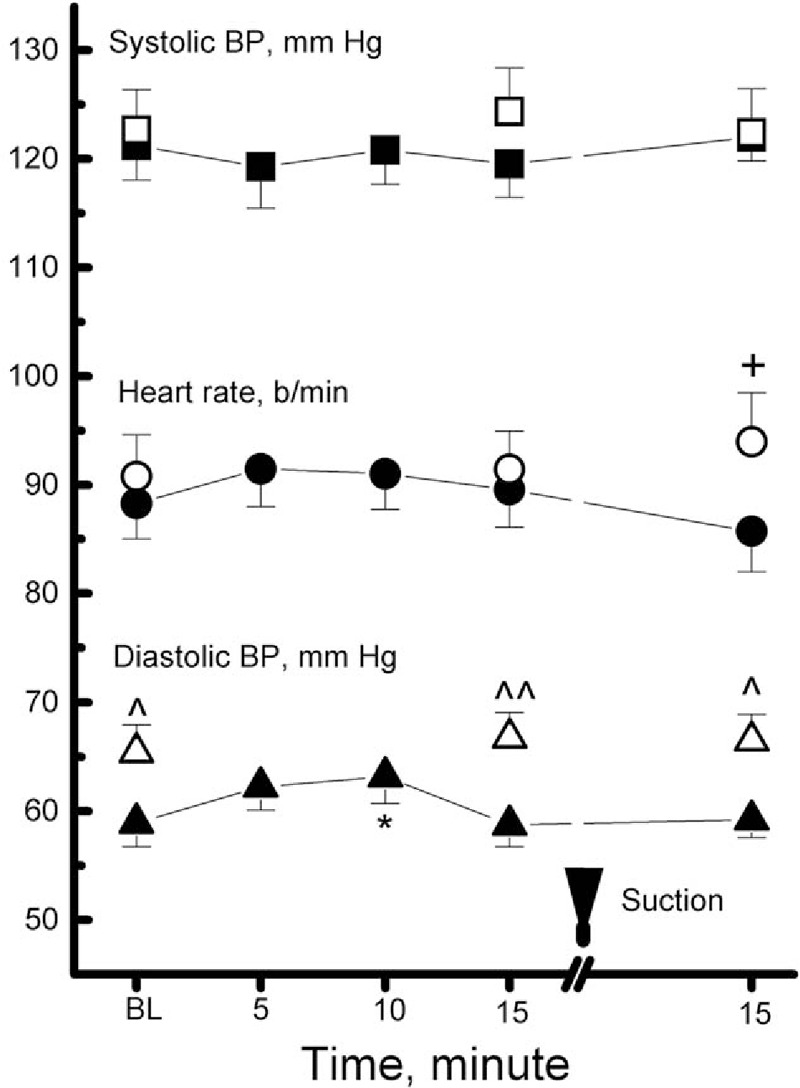
Changes in cardiovascular physiology during high frequency chest wall oscillation (HFCWO) for 5, 10, and 15 minutes and 15 minutes after sputum suction and during conventional chest physiotherapy (CCPT) for 15 minutes and 15 minutes after sputum suction. Each solid symbol indicates the mean of each variable at each time point of the HFCWO group; each open symbol indicates the mean of each variable at each time point of the CCPT group; bars indicate standard error (SE); within-group comparisons to the baseline: all P > 0.05 except ∗P < 0.05, between-group comparisons: ^P < 0.05, ^^P < 0.01, +P = 0.06; BL = baseline, BP = blood pressure, upside down triangle indicates sputum suction.
Figure 4.
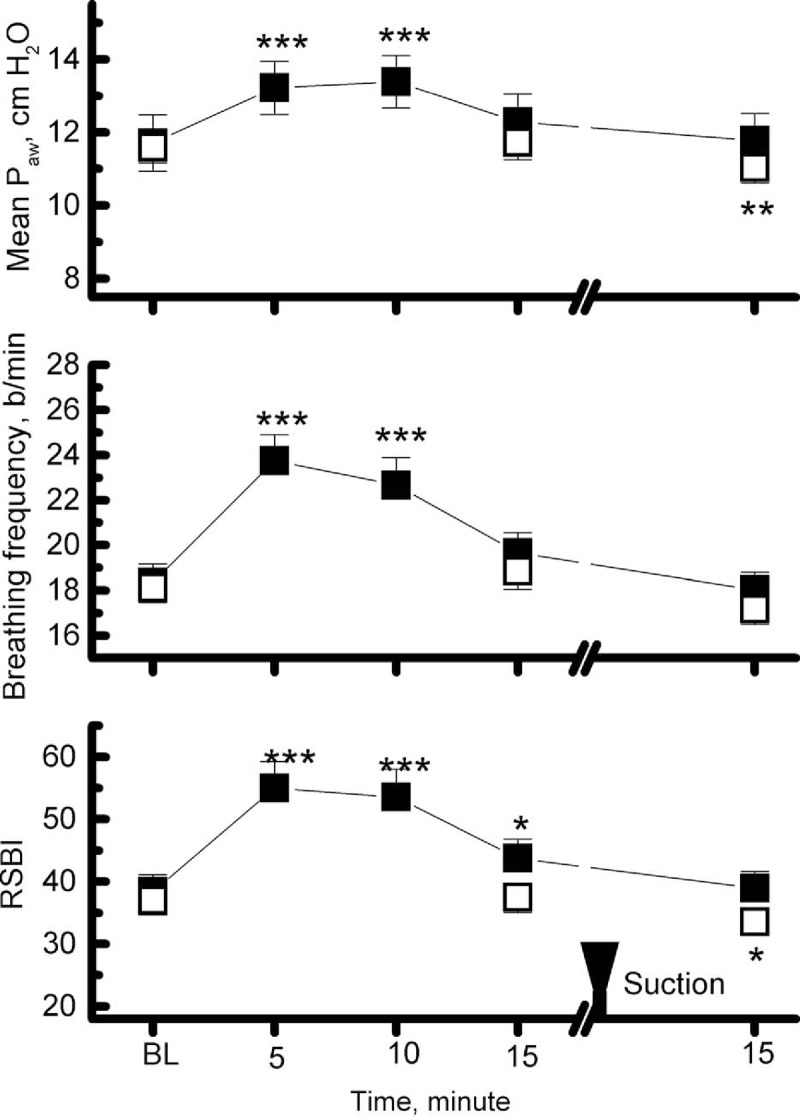
Changes in pulmonary physiology during high-frequency chest wall oscillation (HFCWO) for 5, 10, and 15 minutes and 15 minutes after sputum suction and during conventional chest physiotherapy (CCPT) for 15 minutes and 15 minutes after sputum suction. Each solid symbol indicates the mean of each variable at each time point of the HFCWO group; each open symbol indicates the mean of each variable at each time point of the CCPT group; bars indicate standard error (SE); within-group comparisons to the baseline: ∗P < 0.05, ∗∗∗P < 0.001, between-group comparisons: all P > 0.05;.BL = baseline, Paw = airway pressure, RSBI = rapid shallow breathing index, upside-down triangle indicates sputum suction.
Figure 5.
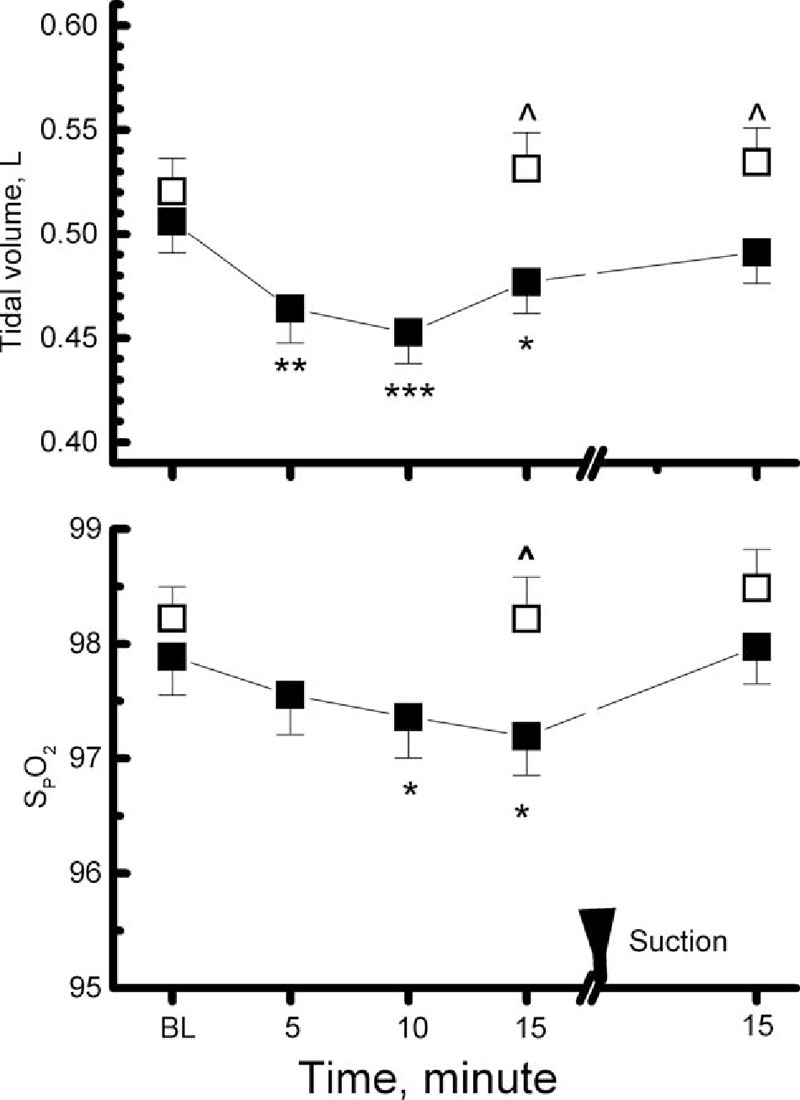
Changes in pulmonary physiology during high-frequency chest wall oscillation (HFCWO) for 5, 10, and 15 minutes and 15 minutes after sputum suction and during conventional chest physiotherapy (CCPT) for 15 minutes and 15 minutes after sputum suction. Each solid symbol indicates the mean of each variable at each time point of the HFCWO group; each open symbol indicates the mean of each variable at each time point of the CCPT group; bars indicate standard error (SE); within-group comparisons to the baseline: ∗P < 0.05, ∗∗P < 0.01, ∗∗∗P < 0.001, between-group comparisons: ^P < 0.05. BL = baseline, SpO2 = oxyhemoglobin saturation measured with a pulse oximeter, upside-down triangle indicates sputum suction.
During CCPT, there were no significant differences in any of the measured variables between the baseline level and the 15th minute of the procedure (Figs. 2–5, all P > 0.05). At the 15th minute after sputum suction, Pmean and RSBI were significantly lower compared to baseline levels (Figs. 2 and 4, all P < 0.05–0.01).
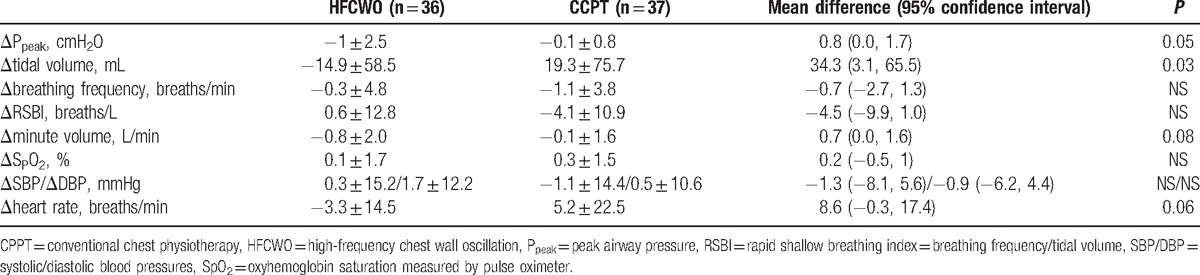
Compared to the CCPT group, tidal volume and SpO2 were significantly lower in the HFCWO group at the end of oscillation or hand percussion (Fig. 5, both P < 0.05). The tidal volume and Ppeak were mildly but significantly lower (Figs. 2 and 5, both P ≤ 0.05, and Table 3) and a trend of a lower heart rate (Fig. 3 and Table 3, P = 0.06) in the HFCWO group than in the CCPT group at the 15th minute after sputum suction. Diastolic blood pressure was significantly higher in the CCPT group at baseline, at the 15th minute of hand percussion or oscillation, and after sputum suction compared to the HFCW group (Fig. 3, all P < 0.05).
Table 3.
Differences between groups in changes (Δ) of variables between baseline and recovery from sputum suction for 15 minutes.
4. Discussion
The key findings of this study are that HFCWO does not interfere with ventilator settings, but that during the procedure, oscillation causes gradual decreases in tidal volume and SpO2, and gradual increases in mean airway pressure, breathing frequency, and RSBI, whereas none of these variables change in patients undergoing CCPT. However, comparing the measurements after sputum suction to the baseline, the HFCWO group had significantly lower Ppeak and minute ventilation (both P < 0.05), whereas the CCPT group had significantly lower Pmean and RSBI (all P < 0.05–0.01). To the best of our knowledge, this is the first study to report the immediate effects of HFCWO on ventilator settings and cardiopulmonary responses of intubated subjects undergoing mechanical ventilation. Compared to the CCPT group, the HFCWO group had significant decreases in Ppeak and tidal volume (both P ≤ 0.05) and a trend of a lower heart rate (P = 0.06) between baseline and 15 minutes after sputum suction (Table 3). Both HFCWO and CCPT may decrease airway pressure by dislodging sputum, and HFCWO seemed to have a better effect.
4.1. The effects of HFCWO on ventilator settings
It has been reported that HFCWO may interfere with ventilator performance.[4,23] Chatburn[15] reported that HFCWO may trigger a ventilator because the sensitivity of triggering a ventilator is usually set at very low pressure or flow (i.e., −2 cm H2O or 3 L/min), and because VEST changes the background pressure or inspired flow by more than -2 cm H2O or 3 L/min.[15] However, we did not observe any significant changes with regards to the ventilator settings (Table 2, all P > 0.05). This finding is consistent with the study of Fink et al,[24] who reported an airway pressure change of only 0.5 to 0.75 cm H2O.
4.2. The effects of HFCWO and CCPT on cardiopulmonary responses
There were no significant changes in Ppeak, minute ventilation, systolic blood pressure, or heart rate during oscillation (Figs. 2 and 3, all P > 0.05) in this study. This may have been because of sputum remaining inside the airway before sputum suction. The decreases in tidal volume and SpO2 and the increases in Pmean, breathing frequency, and RSBI might be because of compression of the chest wall resulting in a decrease in functional residual capacity or end-expiratory lung volume[25,26] with a compensatory increase in breathing frequency. It is speculated that increase in diastolic blood pressure could be because of compression of the chest wall resulting in a decrease in cardiovascular relaxation in thorax. Compression of the chest wall may also have caused elevated alveolar pressure, as Pmean increased with oscillation. An inflated vest without oscillation has been reported to decrease vital capacity and peak flow rate.[27] Although the tidal volume and SpO2 gradually decreased during oscillation, both decrease were very small (Fig. 5, the former <50 mL, the latter <1%). Both values returned to baseline levels after sputum suction. Although Pmean, breathing frequency and RSBI increased during oscillation, they also returned to baseline levels after sputum suction. This suggests that HFCWO immediately followed by sputum suction is safe for both nonintubated[13] and intubated patients as seen in this study. Another concern is that after sputum suction, the greater decreases in Ppeak and in tidal volumes were noted in the HFCWO group than in the CPPT group, suggesting that oscillation did not instantaneously change the respiratory system compliance, but might dislodge sputum in the airway.
Bott et al[28] recommended sputum suction after chest physiotherapy. We also noted the benefits of sputum suction after HFCWO for 15 minutes (Fig. 2), in that it reduced Ppeak and minute ventilation (both P < 0.05), thereby reducing the work of breathing. Compared to the CCPT group, oscillation further reduced Ppeak (Table 3, P = 0.05). Although Pmean and RSBI were lower after sputum suction than at baseline in the CCPT group, there were no significant differences in these variables compared to the HFCWO group. These results suggest that a combination of HFCWO and sputum suction is modestly superior to CCPT with regards to dislodging sputum in intubated patients with mechanical ventilation.
Previous studies have reported that HFCWO is not superior to CCPT for other parameters such as the length of hospital stay, mortality rate, nosocomial pneumonia frequency,[4] and lung function.[12,13] We speculate that these variables may not directly indicate the efficacy of oscillation,[29,30] but may be more related to other factors such as disease severity[14] or quality of care. Further longitudinal controlled large-scale studies are warranted to elucidate this issue.
4.3. Study limitations
Although this is a randomized controlled study, there was still enrollment bias. Despite more subjects receiving sedation in the CCPT group than in the HFCWO group, the CCPT group was sedated to a more shallow level. However, the entire CCPT group had poorer consciousness because some of them had lower levels of consciousness because of underlying illness despite receiving less sedation. The poorer consciousness might be the main cause of a steadier cardiopulmonary response during the procedures in the CCPT group than in the HFCWO group. However, Ppeak was lower in the HFCWO group than in the CCPT group after sputum suction, suggesting that sedation use or consciousness level did not affect the main results of the study. Patients were intended to use ventilator on pressure control mode. However, 2 patients of the HFCWO group were used volume control mode. Intent-to-treat analysis was used in this study. Therefore, the 2 patients were not excluded from analysis. This study shows that HFCWO can be safe, but CCPT seems more efficacious for tidal volume before and after sputum suction. However, the changes (Δ) in tidal volume between baseline and after sputum suction for 15 minutes were not significant in either group (Fig. 5), suggesting a larger scale of patient population for this regard is warranted. Another selection bias was a concern that Ppeak was higher at baseline so that Ppeak might be higher at 15 minutes after sputum suction in the CCPT group than the HFCWO group (Fig. 2). However, the difference between groups in ΔPpeak between baseline and recovery from sputum suction for 15 minutes was larger in HFCWO group than in CCPT group (Table 3). Mortality rate was higher in the CCPT group than the HFCWO. This might also be attributed to selection bias as the incidence of multiorgan failure tended to be higher in the CCPT group than in the HFCWO group, although insignificantly. The hospital stay, lung function, or BODE score was not reported, as these were not the foci of the study. Lastly, as this is an observational study exploring many variables, there is a potential risk of finding statistically significant association because of chance.
5. Conclusions
During oscillation, HFCWO did not affect the ventilator settings, but did significantly change breathing pattern and increase mean airway pressure, and diastolic blood pressure and modestly decreased SpO2. With subsequent sputum suction, HFCWO significantly lowered Ppeak and tended to lower the heart rate as compared to CCPT, suggesting that the study extends the indications of HFCWO for patients with acute pneumonic respiratory failure in ICU.
Acknowledgments
The authors thank Professor I-Feng Lin of National Yang Ming University, Taipei, Taiwan, ROC for statistical consultation and comments on the manuscript preparation.
Footnotes
Abbreviations: APACHE = Acute Physiology and Chronic Health Evaluation, BODE score = a multidimensional 10-point scale for evaluation of chronic obstructive pulmonary disease, CCPT = conventional chest physical therapy, HFCWO = high-frequency chest wall oscillation, ICU = intensive care unit, Pmean = mean airway pressure, Ppeak = peak airway pressure, RSBI = rapid shallow breathing index, SPO2 = oxyhemoglobin saturation was measured using a pulse oximeter.
Registered at this site: Chung Shan Medical University Hospital, Taichung, Taiwan
Registration number: CS13004
The name of the institution(s) review board: The Institutional Review Board of Chung Shan Medical University Hospital
Trial Registration: ClinicalTrials.gov number NCT02758106
Contributions: MLC initiated and designed the study, analyzed and interpreted the data, wrote the manuscript, and approved the version to be published; YLC collected and reviewed the data, revised the manuscript critically for important intellectual content, and approved the version to be published; CYL prepared for IRB approval, collected and reviewed the data, revised the manuscript critically for important intellectual content, and approved the version to be published; SFH collected and reviewed the data, revised the manuscript critically for important intellectual content, and approved the version to be published.
Equal contribution to the first author: Y-LC.
The authors declare that they have no competing interests.
References
- [1].Myslinski MJ, Scanlan CL. Wilkins RL, Sytoller JK. Bronchial hygiene therapy. Egan's Fundamentals of Respiratory Care. St. Louis: Mosby; 2003. 883–910. [Google Scholar]
- [2].Allan JS, Garrity JM, Donahue DM. High-frequency chest-wall compression during the 48 hours following thoracic surgery. Respir Care 2009;54:340–3. [PubMed] [Google Scholar]
- [3].Chaisson KM, Walsh S, Simmons Z, et al. A clinical pilot study: high frequency chest wall oscillation airway clearance in patients with amyotrophic lateral sclerosis. Amyotroph Lateral Scler 2006;7:107–11. [DOI] [PubMed] [Google Scholar]
- [4].Clinkscale D, Spihlman K, Watts P, et al. A randomized trial of conventional chest physical therapy versus high frequency chest wall compressions in intubated and non-intubated adults. Respir Care 2012;57:221–8. [DOI] [PubMed] [Google Scholar]
- [5].Plioplys AV, Lewis S, Kasnicka I. Pulmonary vest therapy in pediatric long-term care. J Am Med Dir Assoc 2002;3:318–21. [DOI] [PubMed] [Google Scholar]
- [6].Longworth DL, Schmitt SK. Wilkins RL, Sytoller JK. Pulmonary infections. Egan's Fundamentals of Respiratory Care. St. Louis: Mosby; 2003. 451–68. [Google Scholar]
- [7].O’Donovan PB, Stoller JK. Wilkins RL, Sytoller JK. A synosis of thoracic imaging. Egan's Fundamentals of Respiratory Care. St. Louis: Mosby; 2003. 427–47. [Google Scholar]
- [8].Jones AP, Rowe BH. Bronchopulmonary hygiene physical therapy for chronic obstructive pulmonary disease and bronchiectasis. Cochrane Database Syst Rev 2000. CD000045. [DOI] [PubMed] [Google Scholar]
- [9].McCool FD, Rosen MJ. Nonpharmacologic airway clearance therapies: ACCP evidence-based clinical practice guidelines. Chest 2006;129:250S–9S. [DOI] [PubMed] [Google Scholar]
- [10].Whitman J, Van Beusekom R, Olson S, et al. Preliminary evaluation of high-frequency chest compression for secretion clearance in mechanically ventilated patients. Respir Care 1993;38:1081–7. [PubMed] [Google Scholar]
- [11].Langenderfer B. Alternatives to percussion and postural drainage. A review of mucus clearance therapies: percussion and postural drainage, autogenic drainage, positive expiratory pressure, flutter valve, intrapulmonary percussive ventilation, and high-frequency chest compression with the ThAIRapy Vest. J Cardiopulm Rehabil 1998;18:283–9. [DOI] [PubMed] [Google Scholar]
- [12].Goktalay T, Akdemir SE, Alpaydin AO, et al. Does high-frequency chest wall oscillation therapy have any impact on the infective exacerbations of chronic obstructive pulmonary disease? A randomized controlled single-blind study. Clin Rehabil 2013;27:710–8. [DOI] [PubMed] [Google Scholar]
- [13].Park H, Park J, Woo SY, et al. Effect of high-frequency chest wall oscillation on pulmonary function after pulmonary lobectomy for non-small cell lung cancer. Crit Care Med 2012;40:2583–9. [DOI] [PubMed] [Google Scholar]
- [14].Chuang ML, Lee CY, Chen YF, et al. Revisiting Unplanned Endotracheal Extubation and Disease Severity in Intensive Care Units. PLoS One 2015;10:e0139864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Chatburn RL. High-frequency assisted airway clearance. Respir Care 2007;52:1224–35. discussion 1235–1227. [PubMed] [Google Scholar]
- [16].Dosman CF, Jones RL. High-frequency chest compression: a summary of the literature. Can Respir J 2005;12:37–41. [DOI] [PubMed] [Google Scholar]
- [17].King M, Phillips DM, Gross D, et al. Enhanced tracheal mucus clearance with high frequency chest wall compression. Am Rev Respir Dis 1983;128:511–5. [DOI] [PubMed] [Google Scholar]
- [18].Cherniack R, Cherniack L. Pathophysiology of respiratory failure. Respiration in health and disease. Philadelphia: WB Saunders; 1983. [Google Scholar]
- [19].Shelledy D, Peters J. Wilkins RL, Stoller JK, Scanlan CL. Initiating and adjusting ventilatory support. Egan's Fundamentals of Respiratory Care. St. Louis: Mosby; 2003. 1003–57. [Google Scholar]
- [20].West JB. West JB. Acute respiratory failure. Lippincott, Williams & Wilkins, Pulmonary Physiology and Pathophysiology: an Integrated, Case-based Approach. Philadelphia:2001. [Google Scholar]
- [21].Knaus WA, Draper EA, Wagner DP, et al. APACHE II: a severity of disease classification system. Crit Care Med 1985;13:818–29. [PubMed] [Google Scholar]
- [22].Yang KL, Tobin MJ. A prospective study of indexes predicting the outcome of trials of weaning from mechanical ventilation. N Engl J Med 1991;324:1445–50. [DOI] [PubMed] [Google Scholar]
- [23].Ntoumenopoulos G. High-frequency chest wall compressions: good for the patient? Good for the clinician? Respir Care 2012;57:323–5. [DOI] [PubMed] [Google Scholar]
- [24].Fink JB, Mahlmeister MJ. High-frequency oscillation of the airway and chest wall. Respir Care 2002;47:797–807. [PubMed] [Google Scholar]
- [25].Darbee JC, Kanga JF, Ohtake PJ. Physiologic evidence for high-frequency chest wall oscillation and positive expiratory pressure breathing in hospitalized subjects with cystic fibrosis. Phys Ther 2005;85:1278–89. [PubMed] [Google Scholar]
- [26].Jones R, Lester, Brown N. Effects of high-frequency chest compression on respiratory system mechanics in normal subjects and cystic fibrosis patients. Can Respir J 1995;2:40–6. [Google Scholar]
- [27].Laurikka JO, Toivio I, Tarkka MR. Effects of a novel pneumatic vest on postoperative pain and lung function after coronary artery bypass grafting. Scand Cardiovasc J 1998;32:141–4. [DOI] [PubMed] [Google Scholar]
- [28].Bott J, Blumenthal S, Buxton M, et al. Guidelines for the physiotherapy management of the adult, medical, spontaneously breathing patient. Thorax 2009;64(suppl 1):i1–51. [DOI] [PubMed] [Google Scholar]
- [29].Esquina AM, Patel B, Pravinkumar E. High-frequency chest wall oscillation in infective exacerbation of COPD: is airway secretion clearance the cornerstone? Clin Rehabil 2014;28:206–7. [DOI] [PubMed] [Google Scholar]
- [30].Ntoumenopoulos G, Presneill JJ, McElholum M, et al. Chest physiotherapy for the prevention of ventilator-associated pneumonia. Intensive Care Med 2002;28:850–6. [DOI] [PubMed] [Google Scholar]


