Abstract
Supplemental Digital Content is available in the text.
There are a variety of techniques described to reconstruct a breast.1 Among adipofascial free flaps, the deep inferior epigastric flap is the most popular option.2 However, abdominal-based flaps are sometimes contraindicated. Allen et al recently described the profunda artery perforator (PAP) flap for breast reconstruction using a transverse skin paddle, which is designed just below the gluteal crease.3, 4 We present a case of bilateral breast reconstruction using bilateral PAP flaps designed with longitudinal skin paddles.
A 60-year-old woman presented for bilateral delayed breast reconstruction after undergoing right nipple sparing mastectomy and left modified radical mastectomy, axillary lymph node dissection and radiation, and suboptimal implant-based reconstruction (see figure, Supplemental Digital Content 1, http://links.lww.com/PRSGO/A351). Abdominal-based autologous reconstruction was contraindicated due to multiple previous abdominal scars including liposuction. On physical examination, we noticed abundant inner thigh tissues suitable for transfer (Fig. 1). Bilateral longitudinal pattern PAP flaps were harvested. Each flap measured 8 × 25 cm, weighed 350 g, and had a pedicle of 10 cm in length (Fig. 2). Both flaps were successfully transferred to reconstruct the contralateral breast using the left internal mammary vessels and right thoracodorsal system as recipients.
Fig. 1.
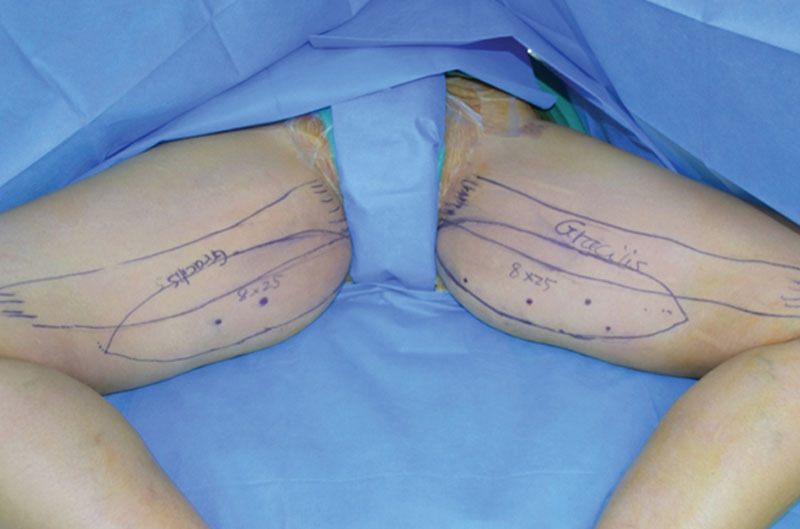
Preoperative marking of the flap.
Fig. 2.
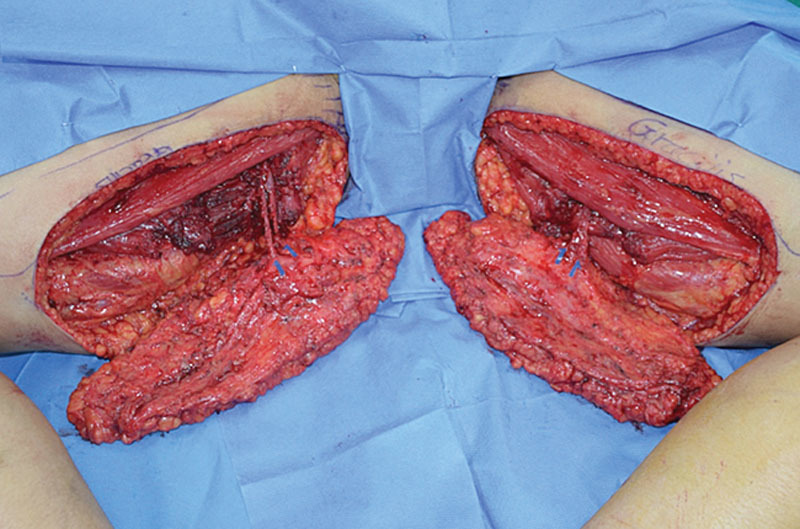
Harvested bilateral PAP flap.
Briefly, we start our harvesting by mapping the perforators posterior to the gracillis muscle. After marking the proposed incision lines, the anterior incision is made first and carried down to the muscle; dissection proceeds subfascially. The gracilis muscle is retracted anterolaterally, exposing the fascia covering the adductor magnus muscle where perforators can be identified and retrograde dissection of the perforator is performed. Because the left axillary contracture required soft tissue coverage, the PAP flap was advanced into the axilla, which required the addition of an implant for the volume augmentation. At 6-month follow-up, the patient was satisfied and pleased with the outcome (see figures, Supplemental Digital Content 2–4, http://links.lww.com/PRSGO/A352, http://links.lww.com/PRSGO/A353, http://links.lww.com/PRSGO/A354).
The description of the PAP flap for breast reconstruction was made with a transverse skin paddle. Although Allen et al described the use of proximal perforator; our skin paddle design gives us the flexibility in utilizing more distal and larger perforators, ideally the most robust in a relatively centric position in relation to the skin paddle. Therefore, most of the time, we do not use the most proximal perforators.
This breast reconstruction technique is novel because we used a vertically oriented skin paddle and a different set of perforators, which to the best of our knowledge has not been described before in the literature. The longitudinally oriented skin paddle takes advantage of redundant inner thigh tissues, which makes it a good choice for patients seeking inner thigh reduction while the abdominal tissue is not an option. The donor site is well hidden and resembles the scar of a vertical inner thighplasty. An inverted “fleur-de-lis” skin paddle combining our described technique and the previously described technique by Allen et al may be also designed to take advantage of additional volume. Our technique yielded a flap of a much larger volume than the largest published series using a transverse design (range 100–260 g).5
Supplementary Material
Footnotes
Presented at the Canadian Society of Plastic Surgeons, June 15, 2016, Ottawa, Canada.
Disclosure: The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by the authors.
Supplemental digital content is available for this article. Clickable URL citations appear in the text.
REFERENCES
- 1.Serletti JM, Fosnot J, Nelson JA, et al. Breast reconstruction after breast cancer. Plast Reconstr Surg. 2011;127:124e–135e. [DOI] [PubMed] [Google Scholar]
- 2.Healy C, Allen RJ., Sr.The evolution of perforator flap breast reconstruction: twenty years after the first DIEP flap. J Reconstr Microsurg. 2014;30:121–125. [DOI] [PubMed] [Google Scholar]
- 3.Allen RJ, Haddock NT, Ahn CY, et al. Breast reconstruction with the profunda artery perforator flap. Plast Reconstr Surg. 2012;129:16e–23e. [DOI] [PubMed] [Google Scholar]
- 4.Haddock NT, Greaney P, Otterburn D, et al. Predicting perforator location on preoperative imaging for the profunda artery perforator flap. Microsurgery. 2012;32:507–511. [DOI] [PubMed] [Google Scholar]
- 5.Saad A, Sadeghi A, Allen RJ.The anatomic basis of the profunda femoris artery perforator flap: a new option for autologous breast reconstruction—a cadaveric and computer tomography angiogram study. J Reconstr Microsurg. 2012;28:381–386. [DOI] [PubMed] [Google Scholar]


