Abstract
With a population in which 70% of the patients were overweight or obese, we reviewed retrospectively 135 breasts of 70 consecutive patients who underwent implant-based immediate breast reconstruction using freeze-dried AlloDerm as the acellular dermal matrix. Several obesity-related parameters were evaluated to determine their possible correlation to early postoperative complications. We found that breast width and surface area of AlloDerm usage correlated with the development of infection and mastectomy skin flap necrosis. Increased breast width and size of AlloDerm matrix implanted were correlated with higher rates of both minor and significant skin necrosis and of cellulitis. Body mass index was correlated with the development of cellulitis and minor and major skin necrosis but not with seroma or reconstruction failure. Preexisting breast cup size correlated with the development of seroma but not the other complications. We observed no statistically significant association between reconstruction failure and any of the parameters reviewed, but this is likely due to the small number of failures in our data set (n = 10).
After mastectomy, the most common type of reconstruction utilizes tissue expanders, which are commonly placed immediately after the mastectomy. Since the early 2000s, acellular dermal matrix (ADM) has been employed concomitantly in breast reconstruction as support at the lower pole of the neobreast mound.1 The expander is exchanged for a permanent implants during a second surgery once the patient’s tissue has had time to adapt to a specific volume of expansion.2 Reconstruction with tissue expanders has many benefits, such as decreased morbidity, shorter operative time, and quicker recovery when compared with autologous reconstruction.2 In addition, tissue expanders allow patients to have more control over their ultimate cup size, which ideally leads to increased patient satisfaction. Although there are benefits to expander use, breast reconstruction overall has its risks. The associated risk factors have been well studied and include radiation, active smoking, obesity, diabetes, and bilateral reconstruction.2–12
Obesity is a growing issue in the United States with at least one third of the country falling into this category.13 Multiple studies have proven that increasing body mass index (BMI) leads to increased perioperative morbidity.2–7,9–12 Nguyen et al.4 reported that a unit increase in BMI predicted a 5.9% increase in the odds of a complication occurring in addition to a 7.9% increase in the odds of reconstruction failure. Although BMI has been a great tool for analyzing the surgical risk of obese patients, there are other factors related to obesity that have not been as well studied, such as cup size, breast width, and ADM surface area. Incidental to a high prevalence of obesity in this study’s patient population, the authors will have the opportunity to evaluate these secondary potential risk factors to determine their significance in association with surgical site infection, seroma formation, and loss of reconstruction.
PATIENTS AND METHODS
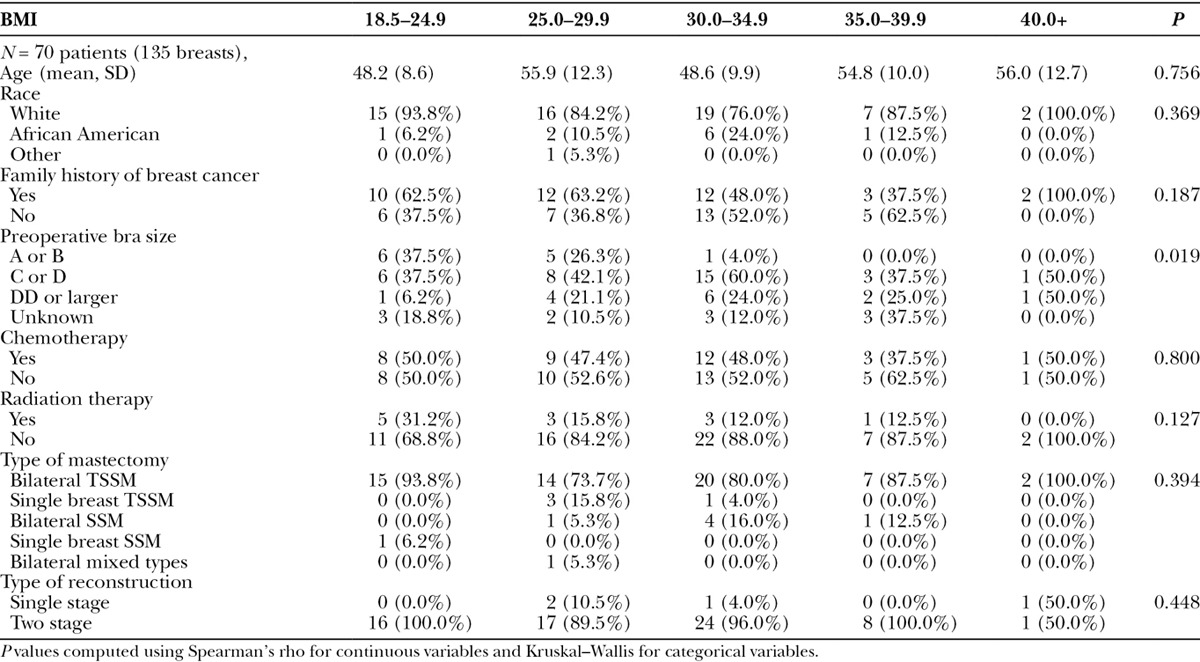
An institutional review board–approved retrospective chart review was conducted on 70 consecutive patients who underwent breast reconstruction performed by a single surgeon at a single institution between June 2011 and October 2013. A review of the electronic health record yielded all information regarding preoperative BMI, cup size, breast width, smoking status, chemotherapy, and radiation history. Outcome data, such as seroma formation, cellulitis, skin necrosis, and explantation, were collected with follow-up of 1 year for each patient. Patient characteristics can be found in Table 1.
Table 1.
Patient Characteristics
Operative Technique
The surgical oncologist performing the mastectomies varied (3 surgeons) in this study, but a single plastic surgeon completed all reconstructions. The mastectomies performed were either simple skin sparing (SSM) or total skin sparing (TSSM), also referred to as nipple sparing. For SSM, the lollipop-shaped incision was used, whereas in TSSM, the vertical incision at the meridian of the lower pole was the standard approach. The senior author performed the reconstruction immediately after the mastectomy after reprepping.
The majority of our cases were done in 2 stages using tissue expanders, but a few patients underwent direct-to-implant reconstruction. The expanders and implants used were Mentor products (Ethicon, Inc.; Somerville, N.J.). In every operation, freeze-dried AlloDerm (LifeCell Corp.; Branchburg, N.J.) was used along with the pectoralis major muscle to create a pocket for the implant. Usually, 1 piece of AlloDerm is sutured to the chest wall along the inframammary crease at the caudal end and to the pectoralis major at the cephalad end. A second piece of AlloDerm is usually employed with the lateral edge folded inward medially and secured to the serratus anterior. The cephalad edge of this second piece is also sutured to the pectoralis major border, and its medial edge is sutured to the first piece of AlloDerm, all with polydioxanone—PDS (Ethicon, Inc.; Somerville, N.J.). The total square centimeters of ADM employed were denoted in the operative report. At the end of each case, closed suction drains were placed and were ultimately discontinued when output was <30 ml/d. Perioperative antibiotic therapy was converted to an oral prescription for 10 days after the patient’s short-stay hospitalization.
For the patients who underwent 2-stage reconstruction, the tissue expanders were gradually filled postoperatively by the surgeon or the advance nurse practitioner in outpatient clinic. The port site was prepped with alcohol or povidone–iodine solution and the expander filled based on patient comfort. Full expansion usually took 3 to 4 months depending on the patient and their postoperative radiation or chemotherapy schedule. Once the patient was pleased with her breast size, she was scheduled for the second surgery in which permanent implants would be placed. The retrospective chart review evaluated early perioperative complications: infection, skin necrosis, seroma formation, and explantation. Long-term results, such as aesthetic outcome and capsular contracture, were not within the scope of this study.
RESULTS
From June 2011 to October 2013, 70 patients underwent immediate reconstruction with implants in 135 breasts total. Average BMI for these patients was 29.41 kg/m2, and according to the World Health Organization classification system, 27% of our patient population was overweight (BMI, 25.0–24.9) and 50% obese (BMI, ≥30). As shown in Table 1, there were no statistically significant differences (P > 0.05) between BMI groups with respect to age, race, family history of breast cancer, preoperative chemotherapy, preoperative radiation therapy, mastectomy procedure, or staging of reconstruction, whereas preoperative breast cup size did vary between groups (P = 0.019).
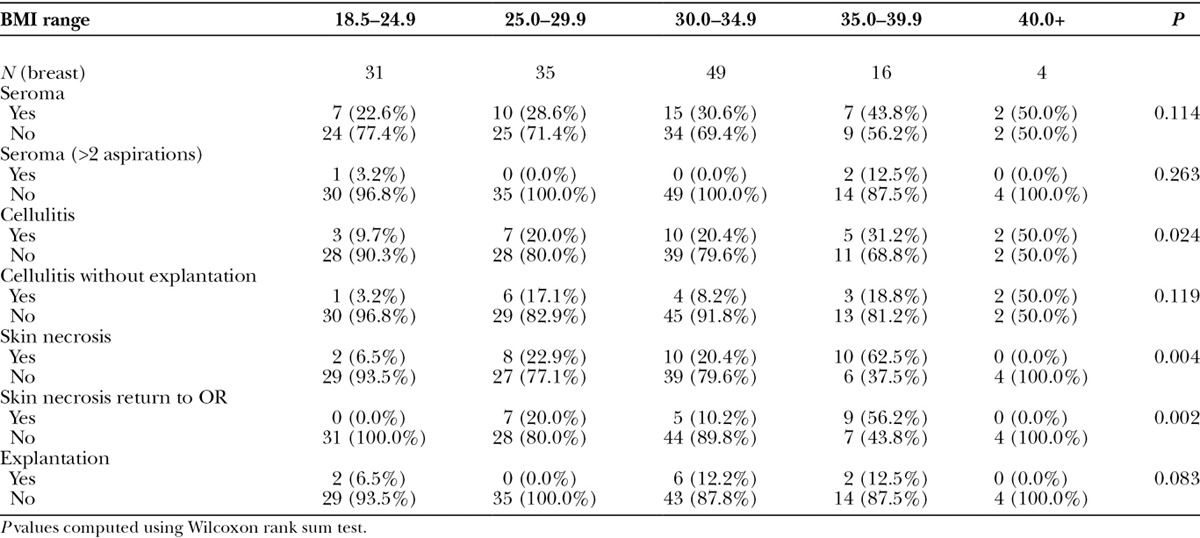
Per-breast complication rates are presented in Table 2 and demonstrate a significantly different rate of cellulitis, skin necrosis, and skin necrosis necessitating return to the operating room (OR) between BMI groups. For example, the rate of cellulitis increased from 9.7% in the normal weight group (BMI, 18.5–24.9) up to 50% in the class III obesity group (BMI, ≥40; P = 0.024). Similarly, rates of skin necrosis and skin necrosis with return to OR increased with BMI (P = 0.004 and 0.002, respectively). A similar pattern, although not statistically significant, was observed for seroma formation.
Table 2.
Rates of Complications by BMI
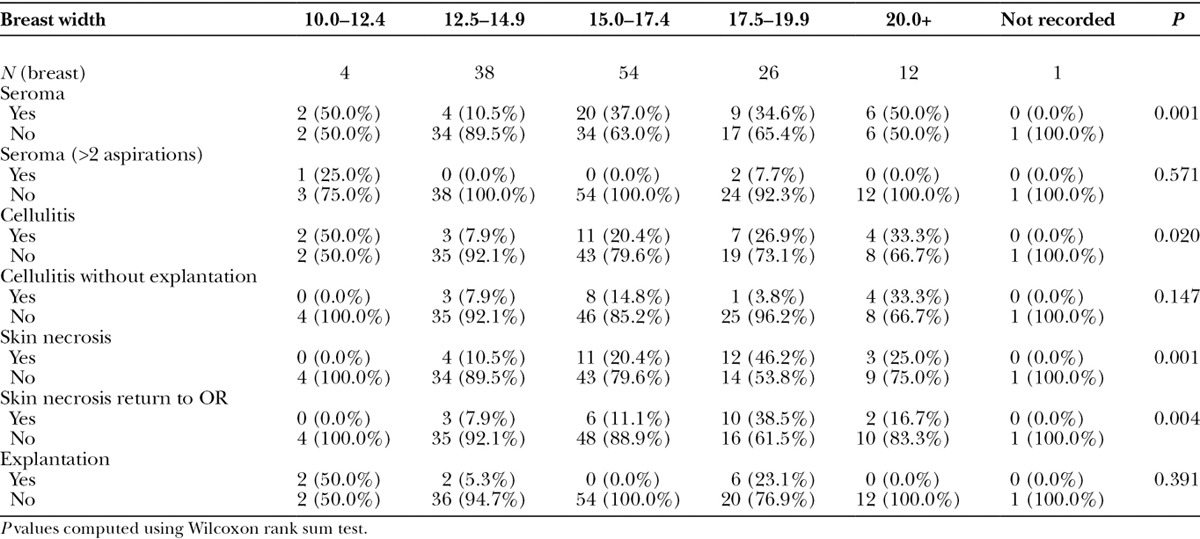
Similar associations were observed between complication rates and breast width, which are presented in Table 3 in 5 categories (10–12.4, 12.5–14.9, 15–17.4, and >20 cm). Greater breast width was significantly associated with higher rates of seroma, cellulitis, skin necrosis, and skin necrosis necessitating return to the OR (P < 0.05). There was not, however, a significant association between breast width and explantation.
Table 3.
Rates of Complications by Breast Width
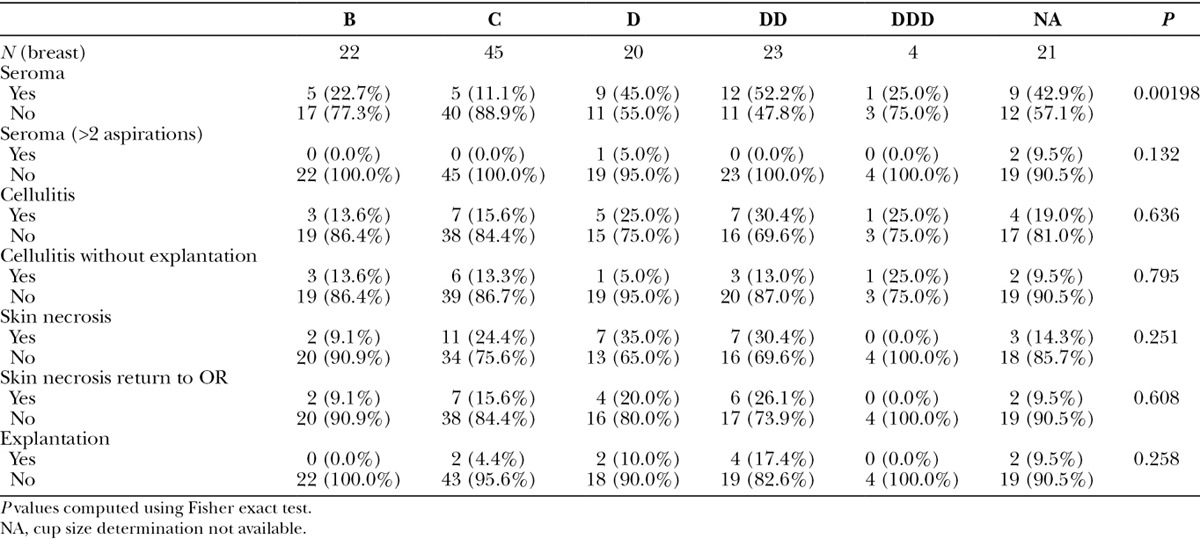
The rate of complications based on cup size showed the least significant results and can be seen in Table 4. Cup size was also divided into 5 categories (B to DDD), with 21 patients of unknown cup size as it was not recorded in their patient chart. We did observe a higher rate of seroma among patients with cup size D and larger (22 out of 47 breasts, 47%) than with cup sizes B and C (10 out of 67, 15%; P = 0.002).
Table 4.
Rates of Complications by Cup Size
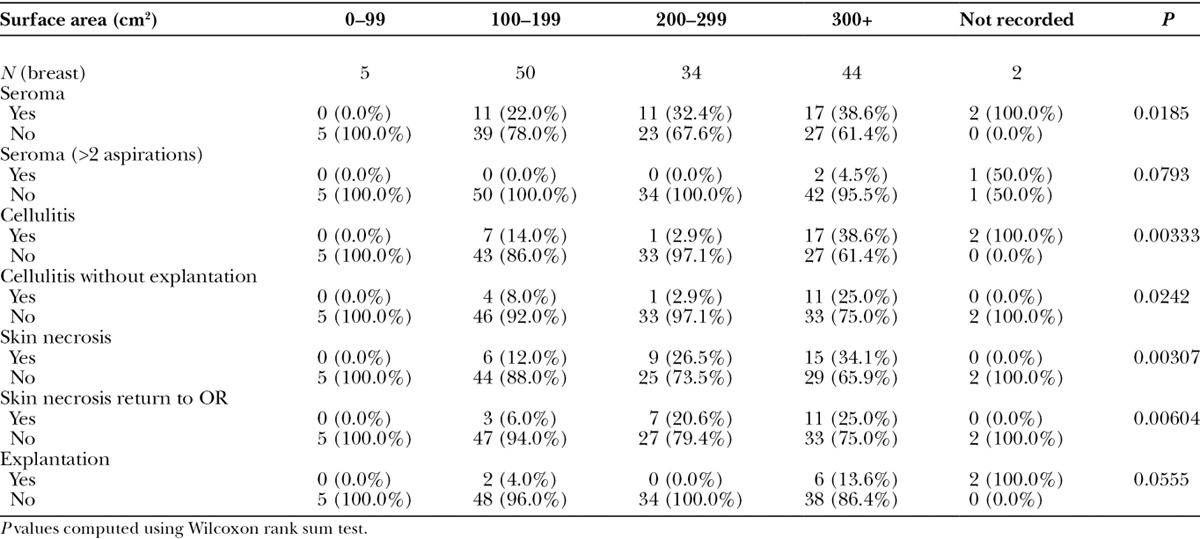
Finally, we analyzed the surface area of AlloDerm used in each breast and results can be seen in Table 5. Results paralleled those for breast width, with significant positive associations observed for the rate of seroma formation, cellulitis, skin necrosis, and skin necrosis return to OR. As with breast width, there was no significant association observed between AlloDerm surface area and the rate of explantation.
Table 5.
Rates of Complications by AlloDerm Surface Area
DISCUSSION
Obesity is a growing problem in the United States and, with more of the population falling into this category, it poses a unique challenge to physicians.13 This study was carried out at an Arkansas teaching hospital. Arkansas has the distinction of being ranked by stateofobesity.org as the state with the highest percentage of obesity among adults (35.9 in 2014).14 According to the Center for Disease Control and Prevention in 2013, 69.9% of adults in Arkansas were overweight or obese, with an obesity rate of 34.6%.15 In our series, 77% of the patients were at least overweight and 50% were obese. Therefore, our catchment area offered a concentrated overweight and obese population for studying the potential secondary risk markers in implant-based breast reconstruction.
Numerous studies have shown that increasing BMI is strongly correlated to an increase in postoperative complications for breast reconstruction.2–12 One study found that obese patients can have as much as an 11.8-fold increase in the odds of experiencing a complication.3 Furthermore, a 1-unit increase in BMI can add 5.9% to a patient’s overall complication risk.4 In our study, we observed a greater than 3-fold increase in the per-breast rate of cellulitis between patients with BMI <25 (3 out of 31, 9.7%) and patients with BMI ≥35 (7 out of 20, 35%).
Francis et al.2 and Khansa et al.11 went beyond BMI and discovered that women with a cup size larger than a C had an increased risk for infection. Our study confirms this correlation between cup size and postoperative complications. Among women with cup size B or C, for example, the rate of seroma formation was 14.9% (10/67), whereas for patients with size D, the rate increased to 45% (9/10), and for patients with DD and greater, the rate increased to 54% (13/27; P = 0.002). We observed a similar trend, although not statistically significant, with cellulitis, as the rate of cellulitis was 14.9%, 25%, and 29.6% for patients with cup sizes B/C, D, and DD/DDD, respectively.
We also observed significant associations between breast width and rates of seroma, cellulitis, skin necrosis, and skin necrosis necessitating return to OR. For example, compared with breast widths from 10 to 14.9 cm, which developed cellulitis in 11.9% of the cases (5/42), patients with each of the 3 subsequent size increments developed a higher incidence of infection in increasing percentages: 20.4% (11/54), 26.9% (7/26), and 33.3% (4/12). To our knowledge, no previous studies have evaluated the risk factor of increase breast width.
Similarly, the surface area of AlloDerm usage in relationship to postoperative complications has not been previously elucidated. The technique performed by the senior author entailed complete coverage of the expander in all areas where the pectoralis major would not cover. This usually required more than one 8 × 12 cm piece of AlloDerm for the average-sized breast because the lateral fold of the expander is also supported. In this series of patients, the AlloDerm, pectoralis major, and the chest wall itself provided a complete pocket for the tissue expander or implant. This technique of complete and precise expander coverage with AlloDerm utilizes more surface area of the matrix compared with the partial expander coverage, single-piece sling approach. With breasts requiring more than 300 cm2, the incidence of seroma and cellulitis was 38.6% (17/44) and 40.9% (18/44), respectively (P = 0.003). For surface area 100 to 199 cm2, the explantation (loss of reconstruction) rate was 4% (2/50), whereas the same complication for surface area of AlloDerm usage of over 300 cm2 was 13.6% (6/38), although this trend did not reach statistical significance (P = 0.055). The increased incidence of skin necrosis relative to the increasing size of surface area in AlloDerm usage was statistically significant.
There are several explanations for why obesity is related to an increased incidence of infection, seroma formation, and skin necrosis. Francis et al. describe longer operative times for obese patients, which increase the risk for contamination of the breast pocket. In addition, the size of the breast pocket is larger, which also increases the chance of contamination and the potential for ischemia and necrosis.2 The high incidence of seroma formation in obese patients could potentially be explained by increased dead space secondary to the mastectomy. The dead space leads to friction between the mastectomy flap and the pectoralis muscle, which could contribute to a seroma.4,16,17 Another possible explanation for why obese patients are at higher risk for complications is that they have more breast surface area, and thus, the possibility for poor perfusion ultimately resulting in necrosis and infection is higher. In addition, the surgeries for obese patients are often longer, which increases the potential for contamination.
It is not a complete surprise that increasing the surface area of AlloDerm usage and increasing the width size of the breast would increase the tendency for postoperative complications with seroma, infection, and skin necrosis. There is already reasonable evidence that the use of ADM increases complications; a recent meta-analysis of 6 studies comparing ADM to submuscular coverage showed increased total complications, seroma, infection, and explantation associated with the use of ADM.18 Under the premise that obesity leads to a higher rate of complication, the larger the patient, the larger would be the width of the breast and the larger amount of AlloDerm required the complete expander coverage technique. It is interesting, though, that the cup size in our study did not reach any statistical significance in association with infection, seroma, or skin necrosis. Cup size may not be as strong of a risk factor indicator when compared with BMI because of the variable breast sizes in the general population. A nonobese patient may have oversized breasts, whereas an obese patient may have disproportionally smaller breasts.
CONCLUSIONS
The obesity epidemic adversely affects the outcome of implant-based breast reconstruction using ADM with tissue expander or direct implant. The extraordinary prevalence of obesity and overweight patients in our patient population afforded a concentrated review of the potential secondary risk parameters related to obesity: bra cup size, breast width, and size of ADM usage. Although this study is retrospective and relatively small, some correlation between these hypothesized secondary risk factors and postoperative complications with seroma, infection, and skin necrosis can be inferred. The larger the surface area of AlloDerm employment, the higher the rate of seroma and cellulitis is observed. Higher breast width is associated with a higher incidence of seroma formation, skin necrosis, and cellulitis. Such outcome data should provide more insight about the patient’s risk of developing early postoperative complications when consulting her preoperatively. Moreover, the possible tendency for an elevated rate of complications with increasing size of AlloDerm usage should provide the surgeon with valuable product performance measure when deciding to use this ADM in implant-based breast reconstruction.
Footnotes
Disclosure: The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by James C. Yuen.
REFERENCES
- 1.Hochberg J, Marseilles AG, Yuen JC, et al. Alloderm (Acellular Human Dermis) in breast reconstruction with tissue expander. Plast Reconstr Surg. (Abstract Supplement) 2005;116:126–127. [Google Scholar]
- 2.Francis SH, Ruberg RL, Stevenson KB, et al. Independent risk factors for infection in tissue expander breast reconstruction. Plast Reconstr Surg. 2009;124:1790–1796. [DOI] [PubMed] [Google Scholar]
- 3.Chen CL, Shore AD, Johns R, et al. The impact of obesity on breast surgery complications. Plast Reconstr Surg. 2011;128:395e–402e. [DOI] [PubMed] [Google Scholar]
- 4.Nguyen KT, Hanwright PJ, Smetona JT, et al. Body mass index as a continuous predictor of outcomes after expander-implant breast reconstruction. Ann Plast Surg. 2014;73:19–24. [DOI] [PubMed] [Google Scholar]
- 5.Fischer JP, Nelson JA, Kovach SJ, et al. Impact of obesity on outcomes in breast reconstruction: analysis of 15,937 patients from the ACS-NSQIP datasets. J Am Coll Surg. 2013;217:656–664. [DOI] [PubMed] [Google Scholar]
- 6.Fischer JP, Cleveland EC, Nelson JA, et al. Breast reconstruction in the morbidly obese patient: assessment of 30-day complications using the 2005 to 2010 National Surgical Quality Improvement Program data sets. Plast Reconstr Surg. 2013;132:750–761. [DOI] [PubMed] [Google Scholar]
- 7.McCarthy CM, Mehrara BJ, Riedel E, et al. Predicting complications following expander/implant breast reconstruction: an outcomes analysis based on preoperative clinical risk. Plast Reconstr Surg. 2008;121:1886–1892. [DOI] [PubMed] [Google Scholar]
- 8.Nelson JA, Fischer JP, Chung C, et al. Risk of readmission following immediate breast reconstruction: results from the 2011 American College of Surgeons National Surgical Quality Improvement Program data sets. Plast Reconstr Surg. 2014;134:193e–201e. [DOI] [PubMed] [Google Scholar]
- 9.Albornoz CR, Cordeiro PG, Farias-Eisner G, et al. Diminishing relative contraindications for immediate breast reconstruction. Plast Reconstr Surg. 2014;134:363e–369e. [DOI] [PubMed] [Google Scholar]
- 10.Lin KY, Johns FR, Gibson J, et al. An outcome study of breast reconstruction: presurgical identification of risk factors for complications. Ann Surg Oncol. 2001;8:586–591. [DOI] [PubMed] [Google Scholar]
- 11.Khansa I, Hendrick RG, Jr, Shore A, et al. Breast reconstruction with tissue expanders: implementation of a standardized best-practices protocol to reduce infection rates. Plast Reconstr Surg. 2014;134:11–18. [DOI] [PubMed] [Google Scholar]
- 12.Fischer JP, Wes AM, Tuggle CT, III, et al. Risk analysis of early implant loss after immediate breast reconstruction: a review of 14,585 patients. J Am Coll Surg. 2013;217:983–990. [DOI] [PubMed] [Google Scholar]
- 13.Flegal KM, Carroll MD, Kit BK, et al. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999-2010. JAMA 2012;307:491–497. [DOI] [PubMed] [Google Scholar]
- 14.The State of Obesity. The State of Obesity in Arkansas. Available at: http://stateofobesity.org/states/ar/. Accessed June 7, 2016.
- 15.Disease Control and Prevention. Arkansas State Nutrition, Physical Activity, and Obesity Profile. Available at: http://www.cdc.gov/nccdphp/dnpao/state-local-programs/profiles/arkansas.html. Accessed June 7, 2016.
- 16.Kim JY, Connor CM.Focus on technique: two-stage implant-based breast reconstruction. Plast Reconstr Surg. 2012;130:104S–115S. [DOI] [PubMed] [Google Scholar]
- 17.Nahas FX, Ferreira LM, Ghelfond C.Does quilting suture prevent seroma in abdominoplasty? Plast Reconstr Surg. 2007;119:1060–1064; discussion 1065–1066. [DOI] [PubMed] [Google Scholar]
- 18.Chun YS, Verma K, Rosen H, et al. Implant-based breast reconstruction using acellular dermal matrix and the risk of postoperative complications. Plast Reconstr Surg. 2010;125:429–436. [DOI] [PubMed] [Google Scholar]


