Abstract
To date, the disclosure of a sex chromosome aneuploidy (SCA) diagnosis to an affected individual has not been explored. This study aimed to assess the timing and content revealed to an affected child by his or her parent(s), resources accessed in preparation, parental feelings of preparedness, common parental concerns, and recommendations for disclosure approaches. Two online surveys were created: 1) for parents of a child with a diagnosis and 2) for individuals with a diagnosis. One-hundred thirty-nine parent surveys (XXY n=68, XXX n=21, XYY n=9, other SCAs n=41) and 67 individual surveys (XXY n=58, XXX n=9) were analyzed. Parents most frequently discussed the topics of learning disabilities (47%) and genetics (45%) with their child during the initial disclosure. A significantly greater proportion of parent respondents reported feeling prepared vs. unprepared for disclosure, regardless of their child’s diagnosis (z-test of proportions, all p’s<.001). Both prepared and unprepared parents most frequently accessed resources such as websites, support groups, and discussion with the child’s physician prior to disclosure, with unprepared parents accessing fewer resources (M = 2.0 ± 1.41) than prepared parents [M= 2. ± 1.56; t(101) = −2.02, p<.05]. Common parental concerns included making the conversation age-appropriate, discussing infertility, and possible impact on the child’s self-esteem. Both parent and individual respondents endorsed being honest with the child, disclosing the diagnosis early and before puberty, and discussing the diagnosis gradually over time. These results provide recommendations for parents, and suggest benefits from additional resources and supports to alleviate concerns when approaching diagnosis disclosure.
Keywords: diagnosis disclosure, sex chromosome aneuploidy, Klinefelter syndrome, trisomy X, genetic counseling, XXYY, XYY, XXY
Sex chromosome aneuploidy (SCA) describes a group of conditions in which individuals have an atypical number of sex chromosomes. The most common SCAs in males are Klinefelter syndrome (KS or 47,XXY, hereby noted as XXY) with a prevalence of 1 in 650 male births and 47,XYY, occurring in 1 in 1000 male births (Bojesen et al. 2003; Coffee et al. 2009; Nielsen 1990). More rare male chromosome aneuploidies include 48,XXYY, 48,XXXY, and 49,XXXXY (hereby noted without chromosome number). Shared features of these disorders include tall stature and increased risk for developmental delays, speech-language disorders, social-emotional difficulties, and cognitive impairments. Higher rates of additional medical problems, congenital malformations, and complex psychosocial and intellectual involvement are observed in individuals with tetrasomy and pentasomy conditions. SCA conditions in males in which there are one or more extra X chromosomes are associated with microorchidism, the need for testosterone replacement therapy, and decreased fertility. In contrast, males with 47, XYY (referred from this point as XYY) typically have normal fertility, testicular size, and testosterone levels.
Trisomy X (47,XXX, hereby noted as trisomy X) is the most common SCA condition in females, occurring in approximately 1 in 1000 female births. It is estimated that only 10% of cases are clinically ascertained due to many individuals being asymptomatic or only mildly affected (Nielson 1990). Developmental delays, learning disabilities, mood disorders (anxiety and depression), and other psychological disorders can be associated with trisomy X. Fertility is normal in most women with trisomy X, although cases of premature ovarian failure have been described (Goswami et al. 2003; Jacobs et al. 1959). Turner syndrome (45, X), another SCA condition that occurs among females, was not included in this study due the differences in the medical and neurodevelopmental phenotype compared to supernumerary SCA conditions and because our clinic did not specialize in this population at the time of the study. However, the Turner syndrome population shares many of the same disclosure considerations as the supernumary SCA conditions included in the study, such as those surrounding reduced fertility.
Disclosure and Barriers to disclosure
When a child is diagnosed with an SCA before birth or during childhood, parents often face the decision of how and when to disclose the diagnosis to their child. While some limited studies have characterized the information given to parents at the time of their child’s SCA diagnosis (e.g. Abramsky et al. 2001; Hall, Abramsky and Marteau 2003), the initial disclosure conversation with the child has not been explored to date. In this study we examine parents’ experiences of telling their child about his or her diagnosis for the first time, and we explore the perspectives of individuals diagnosed with SCAs on the experience of discussing their diagnosis.
Research into other types of parent-to-child disclosures, such as the use of an egg/sperm donor for conception, or the risk for other genetic diseases, has revealed multiple barriers to communication of sensitive information (e.g. MacDougall et al. 2007; Metcalfe et al. 2008; Sutton et al. 2006). Barriers identified include parents having difficulty understanding the information, or the information being emotionally upsetting, with parents consequently being more likely to avoid disclosure. In these studies, some parents described feeling uncertainty as to how to explain the information to their child, when to inform their child, or the child’s ability to understand and cope with potentially distressing information (Sullivan and McConkie-Rosell 2010). Sutton et al. (2006) reported that parents of girls with Turner syndrome expressed the primary reasons for nondisclosure were feeling that they were ill-equipped to disclose the diagnosis, and that they wanted to protect their daughter from potential emotional distress related to infertility.
The nature of the physical and cognitive features associated with SCAs, as well as the variability in features among diagnosed individuals, may present additional barriers for parents in disclosing the diagnosis to their child. In cases of prenatal diagnoses of trisomy X or XYY, a child who is unaffected or mildly affected might otherwise never have reason to learn of their diagnosis if not told by a parent. Additionally, the sensitive issues of infertility and hormone replacement therapy may be difficult to broach for parents of boys with extra X chromosomes (Borelli et al. 1984; Isaacs Cover 2012). Further, the name “sex chromosome abnormality/aneuploidy” may in itself pose a barrier, as the term may be conflated with conceptions of gender or sexuality (Linden, Bender and Robinson 2002; Tartaglia et al. 2010).
These and other unidentified barriers may result in some parents choosing nondisclosure, particularly in the case of unaffected or mildly affected individuals who were diagnosed prenatally, or children with intellectual disability who may have reduced awareness of their symptoms. Alternatively, some parents may selectively disclose limited features of the diagnosis and omit features that may be painful or uncomfortable to discuss, confusing to the parent or child, or features the parent believes to be unnecessary for the child’s self knowledge. In the study by Sutton and colleagues (2006), one-third of participating women with Turner syndrome spontaneously mentioned that their parents or health practitioner had withheld part or all of the diagnosis from them. They also reported that they eventually learned in an undesirable manner, such as through health care providers who assumed they already knew, overhearing conversations or messages left on answering machines, or by doing their own research on symptoms they experienced (Sutton et al. 2006). Several of these women addressed the traumatic nature of learning of the diagnosis unexpectedly or from strangers, which resulted in feelings of distress, anger, and betrayal, as well as damaging the sense of trust the women had with family members who elected to withhold the diagnosis. Sullivan and
McConkie-Rosell (2010) noted that a diagnosis, once withheld, may expand into a family secret, which in turn may foster an environment of distrust and strain family relationships. Furthermore, children are often able to sense that something is wrong, and they may assume a more distressing cause for the secret (Linden et al., 2002; Sullivan and McConkie-Rosell 2010; Sutton et al. 2006). An atmosphere of secrecy might also discourage children from asking questions; Metcalfe and colleagues (2011) found that if a parent did not acknowledge the genetic condition in the family, siblings of the affected child felt inhibited from asking questions because they did not want to upset their parents.
Strategies for disclosure
Some limited research has explored strategies used by parents when disclosing their child’s donor conception status or risk to be a genetic disease carrier. Several parallels may be drawn between disclosure of donor conception and disclosure of an SCA diagnosis: both require the child to have some understanding of biological concepts and issues of privacy, and an unaffected or mildly affected individual with an SCA might not even learn of their diagnosis unless revealed by a parent or physician, similar to the scenario of donor conception status. MacDougall et al. (2007) interviewed couples that had conceived a child using donor gametes about how they envisioned and enacted disclosure of the conception status to their children. The researchers identified parents as primarily utilizing one or a combination of two strategies: early disclosure or “seed planting” at 3–4 years of age with subsequent conversations so that the child would always know, or waiting for the “right time” in the child’s development for him or her to receive and comprehend the information. Parents who endorsed the “seed planting” strategy felt that waiting to tell the diagnosis could cause the child to feel distrustful of the parents and perceive the donor conception as something shameful or unusual. Families using the “right time” strategy considered the child’s personality, level of maturity, and concept of discretion; although families anticipated this to be around 10–12 years, most told their children beginning at 6–7 years of age. Notably, parents utilizing the “right-time” strategy reported greater feelings of uncertainty about the disclosure process and outcome, and expressed desire for guidance or advice.
Gallo and colleagues (2005) interviewed parents in families of children with various genetic conditions to examine the way information about the disorder and genetic risk was shared within families. Most parents reported using an open approach towards sharing information, and initially focused on sharing management issues relevant to the condition. Parents reported determining that their children were ready for information when they began asking questions and demonstrated curiosity. The majority of parents were not given any advice from health professionals on how to talk with the affected child or his or her siblings about the genetic condition.
Children’s preferences for information disclosure
Little is known about children’s preferences for the way genetic risk or diagnostic information be conveyed to them. Adolescent girls and young women from families with Fragile X syndrome have reported a preference for genetic risk information to be given in stages and with reassurance and for normalization; they also reported that parents should be truthful, honest, and knowledgeable about the information given (McConkie-Rosell, Heise and Spiridiglozzi 2009). In a study of communication of genetic risk in families affected by various genetic conditions, both affected children and unaffected siblings requested information to be given in small amounts over time to increase their understanding (Metcalfe et al. 2011). Notably, over half of the young people in that study also wanted information directly from health care professionals.
Present Study
This study is the first to consider the disclosure process of an SCA diagnosis from both the parent and the affected individual’s perspective. This study aimed to explore parents’ experiences of discussing their child’s diagnosis with him or her for the first time, to identify common parent concerns, and assess resources accessed and parent feelings of preparedness prior to diagnosis disclosure to the child. Additionally, we sought to explore the experiences and perspectives of individuals with an SCA diagnosis regarding diagnosis disclosure.
Methods
Design and Recruitment
This study was survey-based and utilized both a quantitative and qualitative design. Ethical approval for this study was sought and obtained from the Colorado Multiple Institutional Review Board (COMIRB). An Internet search was performed to identify organizations, support groups, and social media (i.e. Facebook) groups that serve families and individuals affected by SCA conditions. Representatives of these groups were contacted via email and provided a description of the study, along with a request to post a link to the survey on their website or online forum, and/or to distribute the survey to their membership.
An informational paragraph on the first page of the survey provided informed consent. This paragraph stated that the purpose of the survey was to learn about the experience discussing the diagnosis of an X or Y chromosome variation, and that responses would be used to develop printed information for families who are considering discussing the diagnosis with their child. Respondents were informed that completion of the survey was voluntary and all responses would remain anonymous. Neither the group representatives distributing the survey nor survey respondents were compensated for their involvement.
Two surveys were utilized. One survey was designed for parents of a child with a diagnosed SCA (“parent survey”), and a second survey was designed for individuals with a diagnosed SCA (“individual survey”). Both surveys were accessed via the same survey link. The initial survey question assessed whether the participant was a parent or caregiver of a child with a diagnosed X or Y chromosome variation, an individual with an SCA variation, or neither. Respondents who identified as either a parent/caregiver or as an individual with a diagnosis were continued onto questions from either the parent or individual surveys, respectively. Respondents answering as “neither” (n=6) were asked to exit the survey.
Survey content
A combination of multiple choice and free response questions were utilized within a branched framework, with particular responses to some questions prompting or eliminating subsequent questions. Study surveys were created, collected and managed using REDCap (Research Electronic Data Capture), a secure, web-based application hosted at the University of Colorado, Denver.
Parent survey
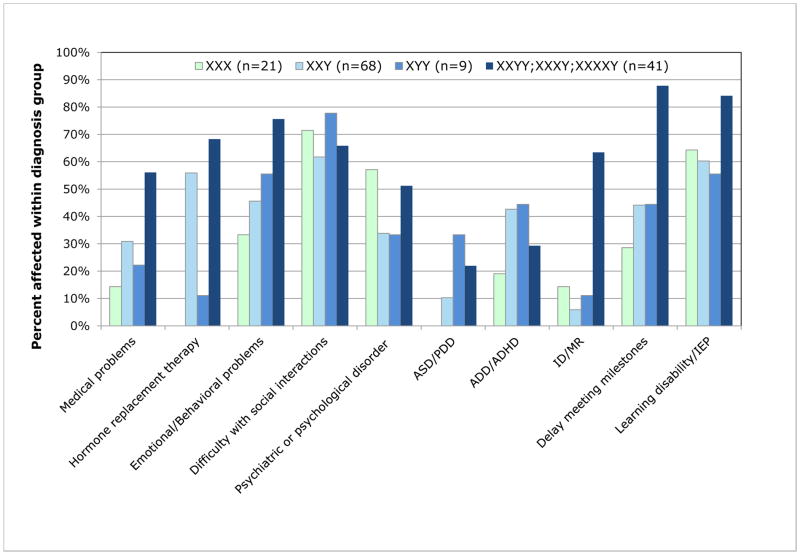
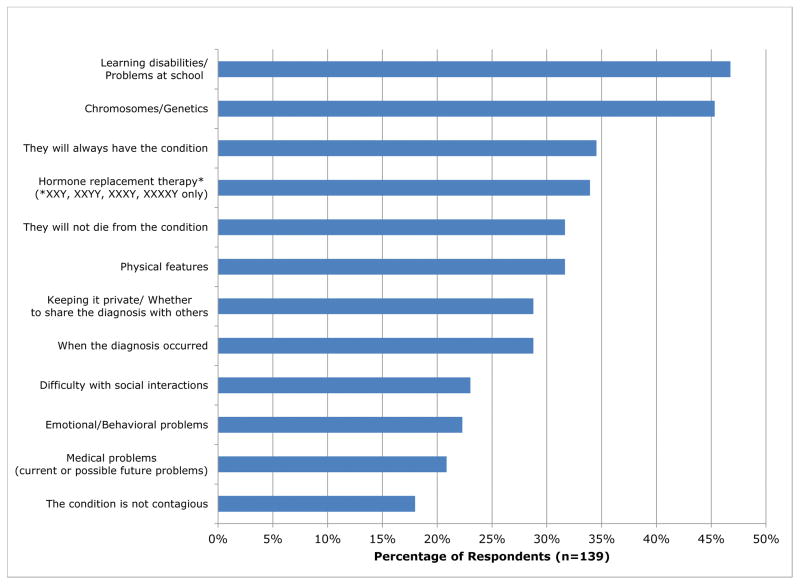
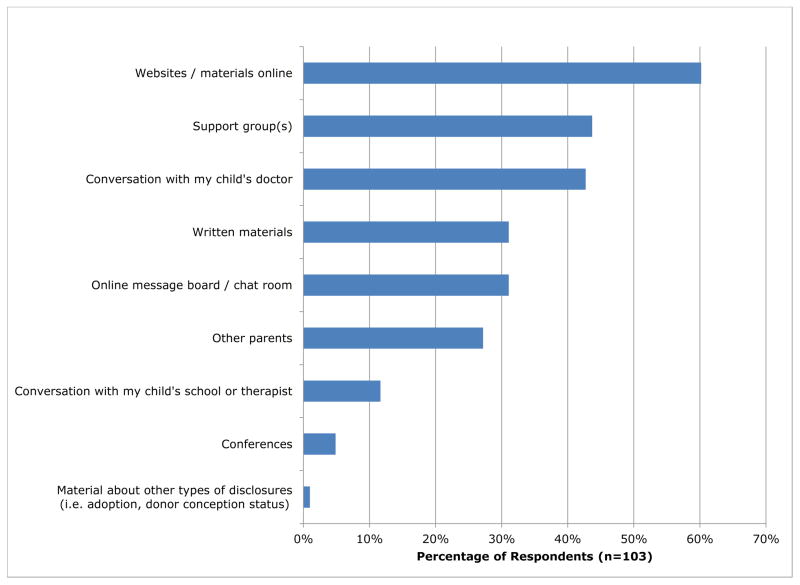
Survey questions for parents were developed to characterize their child’s diagnosis and to describe the first time the child was told of the diagnosis. Questions asked for the child’s current age, diagnosis, age at diagnosis, and indication for diagnosis. Parents were asked to select all problems their child had experienced as a result of the diagnosis from a provided list (as illustrated in Figure 1). Questions assessed the timing of the initial disclosure, who disclosed this information, and topics discussed (as shown in Figure 2). Parents were asked to select from a provided list all resources they had accessed to prepare them for discussing the diagnosis with the child and whether these resources were helpful or not helpful (as shownin Figure 3). Free response questions also inquired as to how the child reacted, most and least challenging aspects of disclosure, what additional information would have been helpful, and advice they would give another parent who is considering discussing the diagnosis with their child for the first time. Demographic questions assessed age, highest level of education received for the parent respondent and for the child’s other caregiver if applicable, and current country of residence.
Fig 1.
Features experienced by children of parent respondents
Fig 2.
Parent report of topics discussed at initial disclosure
Fig 3.
Resources accessed by parents prior to initial disclosure to their child
Individual survey
Questions on the individual survey assessed the respondent’s experience with his or her diagnosis and characterized the first time he or she learned of the diagnosis. Individuals were also asked about the problems they have experienced as a result of their diagnosis and how they felt about their diagnosis (Figure 1). Respondents’ past and current comfort levels discussing their diagnosis with their parents and physician were also assessed. Additionally, respondents were asked what advice they would give to a parent of a child with an SCA about discussing the diagnosis. Demographic questions assessed age, relationship status, highest level of education received, and current country of residence.
Data analysis
Study data were exported from the REDCap application for analysis in SPSS- version 20. Statistical analyses were tailored for each specific research question and data characteristics. The following tests were utilized in this study: t-test, z-test of proportions, chi-square, one-way ANOVA and mixed ANOVA. A conservative method (Bonferroni correction) was used to control for multiple comparisons, when appropriate.
Chi-square tests were used to examine the association between each topic discussed among each of the SCA diagnoses in the parent survey, as well as between comfort levels and SCA diagnosis in the individual survey. Bonferroni corrections were used due to multiple comparisons (for each topic discussed or problem experienced). Due to low cell counts, Fisher’s Exact Test value was reported. Cramer’s V is reported for strength of any significant associations.
Proportions tests (z-tests) (Newcombe 1998a, b) were carried out using the SPSS (v20) Custom Tables Module to determine if there was a significant difference in the percentage of parents who reported feeling prepared versus unprepared within each SCA group, as well as to examine if there was a significant difference in unpreparedness across the SCA groups. Alpha values were adjusted for multiple comparisons using a Bonferroni correction.
Results
Participants (Table 1)
Table 1.
Participant Demographics
| % | n | Mean (SD) | Range | |
|---|---|---|---|---|
| Parents or Caregivers (N = 139) | ||||
| Relationship to child | ||||
| Mother | 88.5% | 123 | ||
| Father | 9.4% | 13 | ||
| Other | 2.2% | 3 | ||
| Respondent's Age (n=106) | 51.3 (10.0) | 26 – 88 | ||
| Child's Current Age (n=137) | 18.5 (11.2) | 1 – 60 | ||
| Child's Diagnosis | ||||
| 47,XYY | 6.5% | 9 | ||
| 47,XXX | 15.1% | 21 | ||
| 47,XXY | 48.9% | 68 | ||
| 48,XXYY | 12.2% | 17 | ||
| 48,XXXY | 7.2% | 10 | ||
| 49,XXXXY | 10.1% | 14 | ||
| Child's Age at Diagnosis | ||||
| Prenatal | 34.5% | 48 | ||
| Younger than 5 years | 23.7% | 33 | ||
| 6 – 12 years old | 16.5% | 23 | ||
| 13– 18 years old | 15.8% | 22 | ||
| After 18 years | 7.9% | 11 | ||
| No response | 1.4% | 2 | ||
| Education level | ||||
| Less than High school/Some High school | 0.0% | 0 | ||
| High School Diploma/GED | 3.6% | 5 | ||
| Some College (less than 2 years) | 7.3% | 10 | ||
| A.A. or Technical 2-year degree | 6.6% | 9 | ||
| Bachelor's Degree (B.A., B.S., etc.) | 30.7% | 42 | ||
| Graduate Degree (M.S., PhD., etc) | 29.2% | 40 | ||
| I choose not to provide this information | 0.7% | 1 | ||
| No Reponse | 23.4% | 32 | ||
| Asia | 1.4% | 2 | ||
| Location (n=106) | ||||
| Australia/New Zealand | 3.6% | 5 | ||
| Canada | 3.6% | 5 | ||
| Europe | 3.6% | 5 | ||
| United States | 63.3% | 88 | ||
| Other | 0.7% | 1 | ||
| No response | 23.7% | 33 | ||
| Individuals (N = 67) | ||||
| Respondent's Age | 40.7 (14.6) | 15 – 74 | ||
| Diagnosis | ||||
| 47,XXX | 13.4% | 9 | ||
| 47,XXY | 86.6% | 58 | ||
| Age at diagnosis | ||||
| Prenatal | 6.0% | 4 | ||
| Younger than 5 years | 6.0% | 4 | ||
| 6 – 12 years old | 9.0% | 6 | ||
| 13– 18 years old | 23.9% | 16 | ||
| After 18 years | 55.2% | 37 | ||
| Education level | ||||
| Less than High school / Some High school | 4.5% | 3 | ||
| High School Diploma/GED | 13.4% | 9 | ||
| Some College (less than 2 years) | 17.9% | 12 | ||
| A.A. or Technical 2-year degree | 16.4% | 11 | ||
| Bachelor's Degree (B.A., B.S., etc.) | 23.9% | 16 | ||
| Graduate degree (M.S., PhD., etc) | 4.5% | 3 | ||
| No Response | 19.4% | 13 | ||
| Relationship status | ||||
| Single | 41.8% | 28 | ||
| In a relationship, not living together | 16.4% | 11 | ||
| Married / living together | 37.3% | 25 | ||
| Divorced / separated | 4.5% | 3 | ||
| Location | ||||
| Africa | 1.5% | 1 | ||
| Australia/New Zealand | 6.0% | 4 | ||
| Canada | 7.5% | 5 | ||
| Europe/UK | 7.5% | 5 | ||
| United States | 58.2% | 39 | ||
| No response | 19.4% | 13 |
Parent survey
A total of 244 parents or caregivers responded to the first question of the survey. Forty-seven respondents were excluded for significantly incomplete surveys; partially completed surveys with responses beyond the initial demographic questions were included in global analysis (n =31). Because the study aimed to explore parents’ experiences of discussing the diagnosis with their child, we excluded from analysis 54 respondents who reported that their child had not been told, or they did not know if the child had been told. An additional 4 respondents were excluded due to the child having a rare SCA for which 3 or less surveys were received. Data analysis included the remaining 139 respondents. All parent respondents denied that they were currently pregnant with a fetus diagnosed with an SCA.
Demographics of the participants are shown in Table 1. The average current age of the affected child was 18.5 years (SD=11.2, range 1–60 years). One-hundred twenty-three (88.4%) parent respondents were mothers, 13 were fathers (9.4%), and 3 (2.2%) identified as an “other” caregiver (sister, adoptive mother, and grandparent). The most common diagnosis was XXY (n=68, 48.9%); followed by trisomy X (n=21, 15.1%); XXYY (n=17, 12.2%); XXXXY (n=14, 10.0%); XXXY (n=10, 7.2%) and XYY (n=9, 6.5%).
Two parent respondents indicated that the child’s other caregiver also took the survey. Additionally, one participant responded to both surveys, as he has a personal diagnosis of an SCA and also has a child with a diagnosis.
Individual survey
Eighty-nine individuals self-reported to have a diagnosis of an SCA responded to the first question of the survey. Seventeen incomplete surveys were excluded. Five respondents were excluded due to diagnoses unique from all other respondents, or who did not disclose their diagnosis. Data analysis was conducted on the remaining 67 respondents.
Respondent’s ages ranged from 15 to 74 years with a mean of 40.7 (SD=14.5). The majority of respondents reported a diagnosis of XXY (n=58, 86.6%), and 9 (13.4%) respondents reported a diagnosis of trisomy X. The survey did not ascertain whether or not respondents received assistance from others (e.g. parents) with their responses to the survey questions.
Parent Survey Results
Features experienced as a result of the child’s diagnosis
All parent respondents answered the question “What has your child experienced as a result of his or her diagnosis?” which provided parents a list of features from which they could select all that apply. When collapsed across diagnoses, the most common features experienced included learning disability/ Individualized Education Plan (IEP) (67.6%), difficulty with social interactions (65.5%), delay meeting milestones (53.2%), and behavioral problems (54.2%) (Figure 1). The diagnosis of an autism spectrum disorder or pervasive developmental disorder was experienced by the fewest children (13.7%). About 9% of respondents noted their child had experienced “other” symptoms, of which speech delay or language disorder was most commonly mentioned.
Age at diagnosis disclosure
The majority (90.6%, n=102) of children diagnosed prenatally were told of the diagnosis during childhood, with the remainder learning during their teenage years. Nearly all children diagnosed before the age of 12 were also told prior to teenage years (97.5%); one child was told between 13 and 18 years of age. When diagnosed in the teens or later years, most (96.6%) were told at or close to the time of diagnosis. Group sizes were too small for comparison of differences among diagnosis groups.
Topics discussed in the first conversation
Parents were asked to select from a list all topics discussed with their child the first time they disclosed the diagnosis to him or her (Figure 2). About 47% of parents reported discussing learning disabilities or problems at school, 45.3% discussed genetics/chromosomes, and 34.5% informed their child that the condition was life-long. Physical features of their child’s condition and the fact that the condition was not fatal were each discussed by 31.6% of the parents. Roughly one-third (28.8%) of parents recalled telling their child when the diagnosis had first been made, and discussing whether to tell others or keeping the diagnosis private. The topic of hormone replacement therapy was discussed by 47.1% of parents of males with XXY and 12.2% of parents of males with XXXY, XXYY and XXXXY. The topics least frequently discussed in the initial disclosure conversation were social difficulties (23.0%), emotional or behavioral problems (22.3%), and medical problems (20.9%). Only 18.0% reported telling their child that the condition is not contagious.
Assessment of the association between which topics were discussed and the different SCA diagnoses revealed significant associations between SCA condition and the topics of when the diagnosis occurred, chromosomes/genetics, whether to tell others/keeping the diagnosis private, and hormone replacement therapy (all p<.05). These specific topics were discussed less frequently with boys with pentasomy and tetrasomy conditions than with children with other diagnoses, with the exception of hormone replacement therapy, which was discussed more frequently with boys with XXY. After corrected for multiple comparisons, the associations for two of the topics remained significant: whether to tell others/keeping the diagnosis private (Fisher’s exact test p<.0042) and hormone replacement therapy (Fisher’s exact test p<.0042). The strength of these associations were moderate (Cramer’s Vprivacy= .369; Cramer’s VHRT= .442).
Free response questions were analyzed for topics discussed in the first and subsequent conversations that parents had with their child about the diagnosis. The most commonly identified topics parents discussed were the challenges the child would experience or that the child was already experiencing as a result of the disorder.
“We told him that he had some extra messages in each cell in his body and needed special help with talking and coloring.” - Mother of son with XXY, prenatal diagnosis
“She was around 10 years old and I told her that she was wired differently but that didn't mean she was not going to get the work presented to her, and that it would be harder for her, but she would learn at her own pace and in her own style.” – Mother of daughter with XXX, diagnosed after age 6
Many parents reported highlighting for their child that everyone has his or her own challenges and differences. One mother of a child with XXY (prenatal diagnosis) reported:
“But I tell him that everyone has to deal with something in their life and this is his. Some kids deal with diabetes, or a parent that dies, etc., but he has to deal with blood tests, doctor appointments, etc., and we are doing this to keep him healthy.”
The genetic cause of the disorder (ranging from specifics of chromosomes and cells to basic reference to the child’s “extra X”), hormone replacement therapy or other medications, learning disabilities, and other medical problems or physical features associated with the disorder were other frequently mentioned topics. Several parents of boys with XXY, XXYY, XXXY, and XXXXY reported discussing the likelihood of future infertility with their child, as well as alternative ways to create a family (i.e. adoption).
“We discussed the positive aspects of adoption and mentioned other ways of overcoming fertility issues.” –Mother of son with XXY, prenatal diagnosis
Other less frequently mentioned topics included that the disorder was not a disease or disability, that the child should not use the disorder as an excuse, that the parents would help the child overcome challenges, that the disorder was not the child’s fault, that the child is special because of the diagnosis, and identifying the child’s strengths. Five parents reported discussing aspects of the diagnosis but not using the specific name of the disorder.
“He doesn't know that it has a name nor the severity of it, but he does know that he has a condition that creates certain challenges for him. We felt, however, that he isn't old enough to know the name of the diagnosis.” –Mother of 7 year-old son with XXY, age at diagnosis not reported
Alternatively, some families used special names for the diagnosis, with the child being referred to as “Xtra special,” “X-man” or “Super X.” Common topics of subsequent conversations included relationships and dating, responsible healthcare practices, and sex and the risk of STDs despite infertility (for XXY, XXYY, XXXY).
How and when the child was told of the diagnosis
Parent free responses were assessed for themes on how they told their child of his or her diagnosis, and when this conversation first occurred. Parents most commonly reported telling their child information about the diagnosis gradually across multiple conversations, instead of all at once.
“There was no one 'big' moment - it was just something we were always open about.” –Mother of son with XYY, prenatal diagnosis
“I felt it was better to start early with a simple explanation and build on details over time.” – Mother of son with XXY, prenatal diagnosis
Several parents reported telling their child about the diagnosis with the assistance of the child’s physician. Multiple parents also reported “keeping it simple,” acting as though the diagnosis was “no big deal,” maintaining a positive demeanor, and remaining open to child questions or thoughts. Other reported methods of discussing the diagnosis included comparing the disorder to other health problems or genetic disorders familiar to the child and calling upon religious beliefs.
The most frequently reported time for telling the child of the diagnosis was when the child began to have multiple appointments related to the diagnosis, or when the child needed to see a specialist for the disorder.
“My son began questioning as he realized we were going to many different doctor appointments and would want to know what this doctor was for, etc.” – Mother of son with XXXXY, diagnosed between ages 6 and 12
Other common circumstances for initial disclosure included when the child began to ask questions, when problems arose related to the diagnosis (i.e. struggling in school), when the child was studying biology or genetics in school, and for males with XXY, when the child was at an age to begin hormone therapy or to assess fertility.
Parent disclosures
When asked to select from a list of who else they had told of their child’s diagnosis, 85.6% of parents reported telling their child’s primary care physician, 77.0% had informed their child’s school or teacher, 76.3% told extended family, 69.1% had told the child’s siblings, and 59.7% had told their own friends.
Parent feelings of preparedness
The majority of parents reported feeling either very prepared (45.6%) or somewhat prepared (35.0%) to discuss the diagnosis with their child for the first time. Z-test of proportions revealed that significantly more parents of children in each diagnosis group reported feeling prepared versus unprepared to discuss the diagnosis with their child (XXX 82.4%, z=-4.95; XXY 84.6%, z=−9.78; XYY 85.7%, z=−3.82; XXYY, XXXY, and XXXXY 70.4%, z=−3.28; all p-values<.001). Though fewer parents of children with XXYY/XXXY/XXXXY reported feeling prepared, this was not statistically significant from the other SCA groups (all p-values>.05).
Resources accessed
Sixty percent of parents reported accessing websites or materials online for information prior to discussing the diagnosis with their child for the first time (Figure 3). Other frequently used resources were support groups (43.6%), and conversations with the child’s doctor (42.3%). Less than one-third of parents utilized other parents or conversations with the child’s school or therapist, and one respondent reported accessing material about other types of disclosures (i.e. adoption or donor conception status). Five respondents spontaneously mentioned attending a conference when asked about additional resources that were accessed; other identified resources included genetic counseling, age-appropriate books about genetics, and talking with adults who have the same diagnosis as their child. Most respondents felt that the resources they accessed were helpful to them. It is unclear whether the 36 respondents who did not report using any resources simply chose not to respond, or if they did not access any resources prior to discussing the diagnosis. There was a significant difference in the number of resources accessed among the prepared (M= 2.77±1.56) and unprepared (M = 2.0±1.41) groups [t(101)= −2.02, p=.046], with unprepared parents accessing fewer resources than prepared parents. The majority of respondents (80.5%) indicated that they would have benefited from written or electronic materials on how to discuss the diagnosis with a child, while 19.5% did not think this would have benefited them.
Common parent concerns
Many parents reported within the free text responses having concerns or fears about discussing the diagnosis with their children (Table 2). The most common fear was that learning of the diagnosis would cause the child to feel “different” and negatively affect the child’s self-esteem.
“I was concerned that it would erode his sense of self and his confidence. I was worried that he would feel bad about who he is.” – Mother of son with XXY, prenatal diagnosis
Table 2.
Parent respondents' common concerns for initial disclosure to their child
| Child will feel different/it will affect his or her self-esteem |
| How the child will react |
| Discussing infertility (parents of boys with XXY, XXYY, XXXXY) |
| What to say, words to use, and making conversation age-appropriate |
| The child will not understand |
| The parent's emotions will interfere with the conversation |
| Privacy concerns/the child will face discrimination |
| The child will use the disorder as an excuse |
| When is the right time for diagnosis disclosure? |
| Discussing medical problems the child has/may have |
Other common concerns included that the child would not understand or would have a negative reaction to the diagnosis, when to disclose, being unsure about what words to use or how to make the discussion age-appropriate, and that the parent would become emotional during the conversation.
“I was concerned about keeping my emotions in check.” – Mother of son with XXY, prenatal diagnosis
“I was nervous, and I was worried about giving him too much info at one time. It was a moment that I had been dreading since the day that I learned. I had to keep in mind that his initial reaction, be it positive or negative, would evolve and that it was a big load for an immature kid.” – Mother of son with XXY, prenatal diagnosis
Several parents of children with XXY, XXYY, XXXY, or XXXXY identified having concerns on how to address the likelihood of their child’s future infertility.
“[The most challenging aspect of disclosure was] telling him that it will be difficult to have children. At 13 year[s] old, he can't even decide what he [wants] to eat for dinner, let alone if he wants to try to freeze his sperm for a child some day.” – Mother of son with XXY, diagnosed between ages 6 and 12
A smaller number of parents identified fears that their child would share the diagnosis inappropriately with others and/or face discrimination, or that their child would use the diagnosis as an excuse.
Perceived child reactions to the diagnosis
Perceived child reactions to the diagnosis were identified from parent responses to the question “How did your child react to learning of the diagnosis?” as well as from the other free response questions. The most common reported reactions were interpreted as being neutral, including that the diagnosis was “no big deal,” disinterest in the diagnosis, or having no apparent reaction.
“He had a few questions but acted like it was no big deal.” Mother of son with XXY, prenatal diagnosis
“She didn't respond too much in any way. She just absorbed the information.” – Mother of daughter with trisomy X, prenatal diagnosis
Many parents reported that their child responded positively with feelings of relief, interest, and acceptance.
“He seemed somewhat relieved. He had begun to feel different, and I think it was initially reassuring to know there was a reason for his differences.” – Mother of son with XXY, prenatal diagnosis
“She was very interested, not frightened or concerned. At that point in her life I think she liked the idea that she had this special 'difference’.” Mother of daughter with trisomy X, prenatal diagnosis
Negative reactions to the diagnosis included the child seeming confused, overwhelmed, not understanding, feeling upset or depressed, expressing anger, feeling anxious or feeling embarrassed.
“She was not very interested and seemed not to really comprehend.” Mother of daughter with trisomy X, prenatal diagnosis
“[He was] somewhat angry, sad, confused.” – Mother of son with XXY, diagnosed between ages 13 and 18
The percentage of positive, negative, and neutral reactions were generally consistent across all diagnoses groups, with 41–50% of parents across diagnosis groups reporting their child had a neutral reaction, 25–33% reported a positive reaction, and 25–30% perceived their child to have a negative reaction.
Recommendations for other parents
Recommendations given by parents for discussing the diagnosis were generally consistent with the timing, content and approach parents reported for the actual conversations they had with their child. The most common recommendations parents gave for how to discuss the diagnosis included discussing the diagnosis gradually over time, being honest with the child, keeping the information simple, and staying positive (Table 3).
“Be honest and give information that is age appropriate and expands as your son/daughter matures. Check in occasionally (but not too often) with them to see if they want to talk about it with a parent or with someone else.” Mother of son with XYY, diagnosed between ages 6 and 12
“Be open, honest and straight forward with your child. Make sure the child is old enough to understand what you are saying. Give lots of examples. Put the diagnosis in a positive light, but still be honest about some of the issues the child may have.” – Mother of child with XXY, diagnosed between ages 6 and 12
Table 3.
Recommendations for parents for disclosing the diagnosis to a child from parents and individuals
Recommendations are listed in each category from most to least frequently mentioned. Bolded recommendations represent those shared by both parents and individuals.
| Parent | Individual | ||
|---|---|---|---|
|
| |||
| How | Discuss the diagnosis gradually, over time | Be honest | |
| Be honest | Do not lie, omit information, or mislead | ||
| Parents should inform themselves first | Be supportive, open, and non-judgmental | ||
| Be positive | Discuss the diagnosis gradually, over time | ||
| Keep it simple | Use pictures | ||
| Be supportive and reassuring | Be calm and casual | ||
| Use pictures | Give the diagnosis with a physician | ||
| Treat it as "no big deal" | |||
| Be direct; use appropriate terms | |||
| Do not treat it as an abnormality | |||
|
| |||
| When | "Early on" | "Early on" | |
| Based upon child's maturity | Before puberty | ||
| When the child starts asking questions | When the child starts asking questions | ||
| Before puberty | When HRT is needed | ||
| At the diagnosis | Teens or 20s | ||
| When the child starts to have problems | When the child starts to have problems | ||
| When the child is studying genetics in school | |||
|
| |||
| What | Everyone has different challenges | It is not a disability, disease, or weird | |
| You will help your child get help | Encourage the child to ask questions | ||
| Identify child's strengths | Advancements/future possibilities | ||
| Privacy considerations | It is not an excuse | ||
| It makes the child special | Everyone has different challenges | ||
| Symptoms of the disorder | It makes the child special/It is a positive thing | ||
| The child is not sick/disorder is not fatal | There are other people with the same diagnosis | ||
| No one caused the disorder to happen | What the child should expect (i.e. hormone treatments) | ||
| Genetics | You will help the child get help | ||
| Encourage the child to ask questions | |||
Eight respondents recommended parents prepare by researching the diagnosis before discussing it with their child.
“Become very informed about the condition. Read as much as you can. Remain current with the literature.” – Mother of daughter with trisomy X, diagnosed between ages 6 and 12
Parents who commented on when to discuss the diagnosis most frequently recommended telling the child when he or she began having appointments or challenges related to the diagnosis, early and before puberty, as well as considering the child’s questions and level of maturity. The most frequent recommendations for what to tell the child included explaining that everyone has unique challenges and differences, that the parent will help the child to receive assistance, and pointing out the child’s strengths. Some parents felt it was important to tell their child to keep the diagnosis private, while others allowed their child to make the decision on whom to share it with.
Individual Survey Results
Learning of the diagnosis
Respondents of the individual survey included males with XXY (n=58, 86.6%), and females with trisomy X (n=9, 13.4%). Most individuals with XXY were diagnosed after age 13, and learned of the diagnosis at or close to the time of diagnosis. Of the 4 women with trisomy X diagnosed prenatally, all were told before age 12. One respondent with trisomy X was diagnosed between the ages of 6 and 12 and told between ages 13 –18; the remainder were told at the same time as their diagnosis in their teens or adulthood.
Two-thirds of women with trisomy X learned of their diagnosis from their parent(s), while the remaining third learned from a physician. The majority of men with XXY were told of the diagnosis by a physician (86.2%), with 12% learning from their parent(s), and one individual learning from an unspecified “other.”
Problems experienced
The most commonly reported symptoms experienced by individuals with XXY included hormone replacement therapy (84.5%), psychiatric or psychological disorder (62.1%), medical problems (57.0%), and difficulty with social interactions (55.2%).
Women with trisomy X most frequently reported experiencing learning disabilities (77.8%), difficulty with social interactions (77.8%), psychiatric or psychological disorder (66.7%), and behavioral problems (55.6%).
Comfort level with discussing the diagnosis
Seventy-seven percent of individuals reported telling their primary care physician about their diagnosis. All women with XXX reported telling their friends about their diagnosis, while 55% of XXY men had told friends. In general, individuals reported a moderate to high level of comfort discussing the diagnosis with their parents and physician, with comfort levels increasing over time. About 71% reported being somewhat or very comfortable discussing their diagnosis with physicians in the past, with 92.9% reporting these levels of comfort at present. Individuals were somewhat less comfortable discussing the diagnosis with their parents than with their physicians; 46.4% were somewhat comfortable or very comfortable in the past, with 69.6% currently feeling comfortable. Fischer’s exact analysis revealed no significant differences between comfort levels of individuals with XXY and trisomy X (all p>.05).
A mixed analysis of variance (ANOVA) was conducted to compare the average comfort rating of participants based on time (present vs. past), person (parent vs. physician) and group (trisomy X vs. XXY). There was a significant main effect of time [F(1,53)=7.867, p=.007], such that participants reported being more comfortable discussing their diagnosis currently compared to the past. There was also a significant main effect of person [F(1,53)=8.501, p=.005], such that participants reported being more comfortable discussing their diagnosis with their doctor compared to their parent. There was no significant main effect of diagnosis, indicating that comfort ratings of the trisomy X and XXY groups were generally similar. There were no significant interaction effects between group, time or person on comfort ratings.
Recommendations from individuals
Respondents were asked the question, “If a parent asked you advice on how to talk to their child about his or her X or Y chromosome variation, what would you say to them?” The most frequently reported advice was to be honest, not to lie or omit information, and not to mislead the child. Individuals suggested that parents remain open, calm and casual, express support, and remain non-judgmental (Table 3).
“Answer questions up front and honestly in age appropriate language. You have (or can get) the info and he/she needs info to understand what he/she is feeling.” – Respondent with XXY, age 68
“I think that a parent should be up-front and honest with their child from the beginning. Just keep it age appropriate. Never lie or mislead the child…” – Respondent with XXY, age 45
“Be ready to give a lot of support to your child – that’s the one thing I think helps me through life – is knowing my family and significant other understands me fully and respects me for who I am with all my strange quirks and knowing that it will take me a lot longer to grasp things.” –Respondent with trisomy X, age 22
Individuals encouraged discussing the diagnosis gradually and using pictures to help explain difficult concepts. Individuals stressed the importance of parents being informed about the diagnosis, and some suggested giving the diagnosis with the help of a physician.
“I would say: Learn more about it prior to telling them” –Respondent with XXY, age 25
“Depending on the age of the child, I would tell the parents to get as much information as possible and educate themselves on KS. I would then tell them to take their child to the doctor’s office and have the conversation there; that way the doctor can also help with the discussion.” –Respondent with XXY, age 38
Of individuals who gave a recommendation on when the diagnosis should be disclosed, 50% specifically endorsed “early” disclosure; other recommended times included before puberty, when the child starts asking questions, when the child starts to have problems, or when hormone replacement therapy is needed (for XXY).
“Start as early as possible. It is not necessary to give all details but it is important to be aware and demonstrate to the child that the child is not strange or weird. It is important for parents to establish for the reality of the child that this is not a life-ending experience but is something to accept.” –Respondent with XXY, age 68
“A parent should tell the child sometime before he is 16 at the very least, and if he is getting hormone treatment then he should know before he starts it.” – Respondent with XXY, age 63
“Wait until they are older to have an understanding on things, maybe in their teens or 20's. Sit down and make sure you have lots of pictures and information when you tell them. Break it down to a child's level of understanding. Keep talking and be open and calm.” – Respondent with trisomy X, age 25
Several individuals identified the importance of telling the child that their SCA is not a disability, disease, or “weird.” While some respondents recommended telling the child that the condition does not make them different, others endorsed telling the child that their SCA makes them special.
“I would just suggest to tell them that this variation makes them who they are and it’s a wonderful thing. Each person whether or not they have a genetic variation might have challenges down the line, but that is just a beautiful part of life. I would also be super supportive with any issues [that] come up.” – Respondent with trisomy X, age 19
Multiple individuals recommended encouraging the child to ask questions and talk about their feelings. Practical topics included what the child might expect to experience because of the disorder and the potential need for hormone treatments for males with XXY. Other recommendations included informing the child that there are many other people with the same diagnosis, that the parent will help the child to receive help needed for challenges the child may face, that everyone has their own unique challenges, and that the diagnosis should not be used as an excuse. No individuals mentioned discussing genetics in recommendations to parents.
Discussion
Little has been known about the way parents disclose the diagnosis of a sex chromosome aneuploidy to their child. Based on surveys completed by 139 parents of children with diagnosed SCAs and 67 individuals with a diagnosed SCA, this study was able to characterize the content and timing of initial disclosure conversations between parents and children with an SCA, examine concerns and feelings of preparedness regarding disclosure, assess the types of resources accessed, and evaluate the experiences of individuals with an SCA condition. It is important to acknowledge that recommendations from individuals with SCA are undoubtedly influenced by their own disclosure experiences. Also, the respondents to the individual survey were on average older (teenagers or adults) at the time of diagnosis in comparison to a younger age of diagnosis for children of the parent respondents.
We found that initial discussions per parent report often included specific aspects of the diagnosis that the child may experience or was currently experiencing, such as learning challenges or medical treatments. The majority of parents reported referencing the genetic etiology of the disorder, ranging from specifics of chromosomes and cells to simple mention of the child’s “extra X.” Parents also frequently reported pointing out to their child that everyone faces challenges and has qualities that make them unique, highlighting the child’s strengths, and explaining they would help the child to overcome any challenges faced. Framing the diagnosis with these aspects may serve to help the child accept and normalize the diagnosis. The reduced frequency with which parents of children with tetrasomy and pentasomy conditions discussed privacy issues, genetics, and when the diagnosis occurred with their children likely speaks to the differences in intellectual involvement and decreased occurrence of prenatal diagnosis for this group.
Common concern expressed by parents in the survey included finding the “right time” and appropriate topics to discuss during disclosure. Parents reported keeping the initial disclosure and subsequent conversations age-appropriate, and providing information gradually over time, with the majority of information addressed prior to early adolescence if the diagnosis was made before that age. The variation in topics discussed at initial disclosure by parents may reflect the differences in ages at which children were told. For example, age-appropriate initial disclosure of an XXY diagnosis to a 7 year-old may not include specifics of needing hormone replacement therapy at puberty, but disclosure to an 11 year-old might incorporate this information. Consistent with the “seed planting” strategy identified by MacDougall et al. (2007) some parents identified talking about the diagnosis from a very young age so that the there was not a formal “reveal” of the diagnosis. Others began the disclosure when it became necessary to provide an explanation for why the child was having medical or therapy appointments, seeing specialists, or experiencing learning, social, or physical problems related to the diagnosis.
In general, advice given by parents on how to discuss the diagnosis was largely consistent with the actual disclosure conversations reported, and did not differ greatly from recommendations given to parents by individuals with a diagnosis. One of the most frequent recommendations from both parents and individuals was to remain honest; notably, individuals further stressed the importance of not misleading the child or omitting information about the diagnosis. Many parents and individuals endorsed normalizing the diagnosis by pointing out to the child that everyone has unique challenges and differences, remaining casual, and explaining that it is not a disease or disability, and that there are many other people with the same diagnosis. In contrast, some individuals and parents advised telling the child that the diagnosis made him or her special, and in some families the child was referred to as “Xtra special” or “Super X.” It may be that the appropriateness of each approach depends on the child’s personality, level of affectedness, and family communication style.
Interestingly, no individuals with an SCA mentioned discussion of genetics in their recommendations for disclosure. It may be that individuals consider the genetic etiology less important compared to other aspects of the disorder, or that the genetic aspect is not distinct from the diagnosis itself to warrant special mention. Because the disorders are not typically inherited or passed on to children, the value of knowing the genetic mechanism may seem secondary to the symptoms, treatment, or other aspects of the disorder. However, it may be important to provide at least a rudimentary explanation of genetics in order for the child to understand that the disorder happened randomly and no one caused it to occur, that it is not contagious, and that the condition is life-long (Linden et al., 2002; Tartaglia et al. 2010).
A strong majority of the individuals with an SCA reported feeling comfortable discussing their diagnosis with their physician or their parent, with comfort levels increasing over time. Although individuals generally reported higher comfort levels with their physicians as compared to their parents, this most likely reflects that most respondents were diagnosed in adulthood, when parents are less likely to be involved in their child’s healthcare. It may be that earlier disclosure conversations in childhood may lead to increased comfort discussing the diagnosis with a parent in adulthood.
We found that most parents felt somewhat prepared or very prepared to talk about the diagnosis for the first time. The majority of parents accessed 2 to 3 resources prior to the initial disclosure conversation, and the majority found these resources helpful. Parents who reported feeling prepared to talk about the diagnosis accessed a greater number of resources on average than parents who felt unprepared, although the average number of resources between these groups differed by less than one. This may imply that greater exposure to resources prior to disclosure helps parents to feel more prepared, or that parents who are more likely to feel prepared are also more inclined to access additional resources. The top resources for both prepared and unprepared parents included websites/online materials and support groups. Of note, the children of some parent respondents were diagnosed as distantly as thirty years ago, such that not all resource options were available to them at the time of diagnosis. While not significantly different in comparison to the trisomy conditions, the fact that only 70% of parents of sons with XXYY, XXXY, and XXXXY reported feeling prepared may reflect concerns of child’s ability to understand due to the higher prevalence of intellectual involvement in these diagnoses, or a more limited amount of resources available for these rarer conditions. Despite their feelings of preparedness, the majority of parents said that they would have found helpful a written or online brochure specifically about how to discuss the diagnosis with their child.
Only 42% had conversations with the child’s doctor about discussing the diagnosis with their child. Although this is higher than the 10% of parents of children who received support from their physician in the study by Gallo et al. (2005), this may suggest that physicians are an under-utilized resource for parents with regard to diagnosis disclosure, or that physicians are not well equipped to assist parents on this topic. Though discussion of disclosure with a genetic counselor was not directly assessed by the survey, several parents spontaneously reported using genetic counselors as a resource. While we would anticipate that the percentage of parents discussing disclosure with a genetic counselor is similar to or less than the figure for physicians due to limited access to genetic counseling services, it may also be that parents are receiving disclosure support from genetic counselors in lieu of the child’s primary care provider. Several individuals as well as parents recommended using a health care professional to help with the diagnosis disclosure. This may also be useful for parents who are concerned about their ability to provide their child with accurate age-appropriate information.
Several common fears about discussing the diagnosis emerged from the parents’ responses. The primary concern was that learning the diagnosis would make the child feel different or affect his or her self-esteem. Notably, however, many parents perceived their child to feel relieved upon learning the diagnosis. Parents attributed this to the child suddenly having a reason for the struggles they were already experiencing or alleviating fears of a more dire family secret. Responses from individuals with SCAs suggest that children with learning disabilities, physical changes, or social difficulties may already feel “different” from peers, and knowing there are others like them with the same diagnosis might be reassuring and exert a positive influence on their self-esteem.
Parents commonly expressed uncertainty of what to say to their child, including what specific words they should use and how to keep the conversation age-appropriate. The topics of infertility (for parents of XXY, XXYY, XXXY, and XXXXY) and potential medical problems were most challenging for parents to discuss. These fears are consistent with barriers to disclosure identified in previous literature (Sullivan and McConkie-Rosell 2010; Sutton et al. 2006). Some of these fears may be allayed by utilizing a healthcare professional to help facilitate age-appropriate disclosure or by accessing literature specifically designed to address these concerns.
While many parents expressed fears about how their child would react to the diagnosis, the actual perceived reactions were more commonly neutral (e.g., unconcern) or positive (e.g., accepting) than negative. Of reactions interpreted as negative, the majority were children who did not understand or were confused by the diagnosis; this may reflect a learning or intellectual disability, and/or that the disclosure conversation occurred in a manner inappropriate for the child’s age or maturity.
Recommendations for parents
Based upon results of this study and suggestions from other professionals and support literature (Linden et al., 2002; Tartaglia et al. 2010; KS&A; Rogers P. & Turner Syndrome Support Society), we recommend the following strategies for parents when disclosing the diagnosis of an SCA to their child:
Recognize that every child is different with regard to his or her needs, comprehension, communication and coping skills. You know your child best.
Become informed about the diagnosis and seek answers to your own questions before you talk with your child.
Start the discussion early, and build on the conversation gradually over time (for those with a prenatal or early diagnosis).
Consider including a trusted health care professional in the disclosure process, such as your child’s primary care provider, a genetic counselor, a medical specialist (geneticist, developmental medicine specialist, or endocrinologist), an advanced practice nurse or physician assistant, or a therapist. These professionals could be utilized either for the initial discussion or as a follow-up to discussion(s) that took place at home.
Use simple and direct language. Avoid ambiguous descriptions or complex terminology. Check that your child understands your main points.
Be open, honest, and calm.
Encourage your child to ask questions and discuss his or her feelings.
Express support. Offer to help your child obtain any help or information he or she may need for the challenges he or she may experience.
Reassure your child that their diagnosis is not a disability or a disease and that it is not contagious or fatal. Inform your child that the condition resulted from a random event that happened before they were born, and no one caused it to happen.
Let your child know there are many other individuals like him or her with the same diagnosis.
Use pictures, books, or other aids to help communicate complex information such as genetics if appropriate.
Be thoughtful about how the terms “sex” or “sex chromosome” are used, and how your child may interpret these terms. Some parents prefer to refer to “X and Y chromosomes” instead to prevent misinterpretations and deemphasize sex. When explaining genetics, consider introducing that everyone (males and females) has one X chromosome, and the second sex chromosome (X or Y) determines female or male. When extra X and/or Y chromosomes are added to this pair, there can be different challenges and medical features (which can be highlighted depending on the SCA condition of your child and their individual case).
Older children or adolescents may require reassurance that their condition does not change their gender or sexuality, or imply sexual incompetence.
-
For diagnoses associated with infertility:
From childhood and when appropriate for your child, actively incorporate into discussions different ways families can be made, such as adoption, fostering, choosing not to have children, or using different advanced reproductive techniques such as sperm donor or in vitro fertilization. This can be discussed when topic arises in books, television programs, or in relation to friends or family members
Address specific questions and concerns regarding infertility as the child matures.
Remain informed about advanced reproductive techniques and ongoing fertility research in XXY and other SCA conditions, since many advances are being made and new recommendations are emerging for strategies associated with sperm retrieval or sperm banking.
We developed written materials for parents of children with XXY, XYY, XXX and XXYY on the topic of diagnosis disclosure informed by the results of this study. These are available through our clinic and can be accessed by sending an e-mail request to extraordinarykidsclinic@childrenscolorado.org.
Study Limitations
There are several limitations to this study that need to be considered. This study only included parents whose child was aware of his or her diagnosis, and therefore may over- or under-represent specific family communication styles. Respondents self-selected into the study from SCA support websites, support groups, and social media communities. Therefore, the study may be biased toward those who are already open to discussing the diagnosis, or more likely to seek outside support and resources. Further, individuals or parents of children who are minimally affected by the diagnosis may be less likely to join support groups or visit organization websites, and may be under-represented by respondents of this study. Parent respondents were predominately mothers, reported high levels of education, and were predominantly from the United States. Consequently findings may not be applicable to other demographics. Survey responses are based only on participant report, and subject to recall bias. Finally, only one researcher was involved in coding of free response questions.
Research Recommendations
Given that less than half of parents in our study discussed disclosure with a physician, further studies may focus directly on provider preparedness to bring up or address the topic of diagnosis disclosure with parents, which may be useful for facilitating provider education or outreach on this topic. Additional research is needed to explore the motivations and barriers for parents who have chosen not to disclose their child’s diagnosis; such studies may benefit the development of interventions or supports to facilitate communication in these families. The majority of children and individuals in this study were to some degree medically or cognitively affected by their SCA, which provided many families an impetus for diagnosis disclosure. Further studies are also necessary to characterize the disclosures or barriers to disclosures to children who are not affected or only mildly affected. This is especially important with the recent advances in non-invasive prenatal genetic testing (NIPT) technology, from which we will likely see an increased number of diagnosed SCAs that may not otherwise present clinically. Although we anticipate that the findings of this research may generally apply to other genetic conditions (Turner syndrome, for example), additional studies with other genetic populations are necessary for building a comprehensive body of disclosure literature.
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000. Informed consent was obtained from all patients for being included in the study.
Acknowledgments
This work was primarily completed by A. Dennis for scholarly project requirements of University of Colorado Genetic Counseling program. The topic for this project was inspired by a exceptional young man with “XYXY” syndrome. Senior author Nicole Tartaglia acknowledges support from NIH/NINDS 1K23NS070337, NIH/NCATS Colorado CTSI Grant Number UL1 TR001082, NIH/NCRR Colorado CTSI Grant Number UL1 RR025780, and University of Colorado IDDRC. Contents are the authors’ sole responsibility and do not necessarily represent official NIH views. The authors would also like to thank Richard Boada for his consultation on statistical analyses, Kali Messer, MS, CGC for survey and recruitment examples, Carol Walton, MS, CGC for her support, the organizations who participated in recruitment (including KS&A, Klinefeltersyndrome.org, KS Global Support Group, and regional support groups), and the study participants for sharing their time and experiences.
A. Dennis, S. Howell, L. Cordeiro and N. Tartaglia declare that they have no conflict of interest.
References
- Abramsky L, Hall S, Levitan J, Marteau TM. What parents are told after prenatal diagnosis of a sex chromosome abnormality: Interview and questionnaire study. BMJ. 2001;322:463–466. doi: 10.1136/bmj.322.7284.463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bojesen A, Juul S, Gravholt CH. Prenatal and Postnatal Prevalence of Klinefelter Syndrome: A National Registry Study. The Journal of Clinical Endocrinology & Metabolism. 2003;88(2):622–626. doi: 10.1210/jc.2002-021491. [DOI] [PubMed] [Google Scholar]
- Borelli JB, Bender BG, Puck MH, Salbenblatt JA, Robinson A. The meaning of early knowledge of a child’s infertility in families with 47, XXY and 45,X children. Child Psychiatry and Human Development. 1984;14(4):215–222. doi: 10.1007/BF00706035. [DOI] [PubMed] [Google Scholar]
- Coffee B, Keith K, Albizua I, Malone T, Mowrey J, Sherman SL, Warren ST. Incidence of fragile X syndrome by newborn screening for methylated FMR1 DNA. American Journal of Human Genetics. 2009;85(4):503–514. doi: 10.1016/j.ajhg.2009.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Isaacs Cover V. Living with Klinefelter Syndrome (47,XXY) Trisomy X (47,XXX) and 47,XYY: A guide for families and individuals affected by X and Y chromosome variations. Canada: Virginia Isaacs Cover; 2012. [Google Scholar]
- Gallo A, Angst D, Knafl KA, Hadley E, Smith C. Parents sharing information with their children about genetic conditions. Journal of Pediatric Health Care. 2005:267–275. doi: 10.1016/j.pedhc.2005.05.008. [DOI] [PubMed] [Google Scholar]
- Gallo A. Information management in families who have a child with a genetic condition. Journal of Pediatric Nursing. 2009;24(3):194–204. doi: 10.1016/j.pedn.2008.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goswami R, Goswami D, Kabra M, Gupta N, Dubey S, Dadhwal V. Prevalence of the triple X syndrome in phenotypically normal women with premature ovarian failure and its association with autoimmune thyroid disorders. Fertility and Sterility. 2003;80(4):1052–1054. doi: 10.1016/s0015-0282(03)01121-x. [DOI] [PubMed] [Google Scholar]
- Hall S, Abramsky L, Marteau TM. Health professionals’ reports of information given to parents following the prenatal diagnosis of sex chromosome anomalies and outcomes of pregnancies: a pilot study. Prenatal Diagnosis. 2003;23:535–538. doi: 10.1002/pd.637. [DOI] [PubMed] [Google Scholar]
- Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap) - A metadata-driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics. 2009;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobs P, Baikie A, Brown W, Macgregor T, Maclean N, Harnden D. Evidence for the existence of the human “super female. Lancet. 1959;2:423–425. doi: 10.1016/s0140-6736(59)90415-5. [DOI] [PubMed] [Google Scholar]
- KS&A. FAQ: When and how should I tell my son that he has 47,XXY/my daughter that she has Trisomy X? 2012 Retrieved March 23, 2014 from http:www.genetic.org.
- Linden MG, Bender BG. Fifty-one prenatally diagnosed children and adolescents with sex chromosome abnormalities. American Journal of Medical Genetics. 2002;110:11–18. doi: 10.1002/ajmg.10394. [DOI] [PubMed] [Google Scholar]
- Linden MG, Bender BG, Robinson A. Genetic counseling for sex chromosome abnormalities. American Journal of Medical Genetics. 2002;110:3–10. doi: 10.1002/ajmg.10391. [DOI] [PubMed] [Google Scholar]
- Mac Dougall K, Becker G, Scheib J, Nachtigall RD. Strategies for Disclosure: How parents approach telling their children that they were conceived with donor gametes. Fertility and Sterility. 2007;87(3):524–533. doi: 10.1016/j.fertnstert.2006.07.1514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McConkie-Rosell A, Del Giorno J, Heise E. Communication of genetic risk information to daughters in families with Fragile X Syndrome: The parent’s perspective. Journal of Genetic Counseling. 2011;20:58–69. doi: 10.1007/s10897-010-9326-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McConkie-Rosell A, Heise E, Spiridiglozzi GA. Genetic risk communication: Experiences of adolescent girls and young women with families with Fragile X Syndrome. Journal of Genetic Counseling. 2009;18:313–325. doi: 10.1007/s10897-009-9215-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Metcalfe A, Coad J, Plumridge GM, Gill P, Farndon P. Family Communication between children and their parents about inherited genetic conditions: A meta-synthesis of the research. European Journal of Human Genetics. 2008;16:1193–1200. doi: 10.1038/ejhg.2008.84. [DOI] [PubMed] [Google Scholar]
- Metcalfe A, Plumridge G, Coad J, Shanks A, Gill P. Parents’ and children’s communication about genetic risk: a qualitative study, learning from families’ experiences. European Journal of Human Genetics. 2011;19:640–646. doi: 10.1038/ejhg.2010.258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newcombe RG. Interval estimation for the difference between independent proportions: comparison of eleven methods. Statistics in Medicine. 1998;17(8):873–90. doi: 10.1002/(sici)1097-0258(19980430)17:8<873::aid-sim779>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- Newcombe RG. Two-sided confidence intervals for the single proportion: comparison of seven methods. Statistics in Medicine. 1998;17(8):857–72. doi: 10.1002/(sici)1097-0258(19980430)17:8<857::aid-sim777>3.0.co;2-e. [DOI] [PubMed] [Google Scholar]
- Nielsen J. Sex chromosome abnormalities found among 34, 910 newborn children: Results from a 13-year incidence study in Arhus, Denmark. Birth Defects Original Article Series. 1990;26(4):209–223. [PubMed] [Google Scholar]
- Rogers P. Fact Sheet Six: Disclosure [Pamphlet] Turner Syndrome Support Society; No date. Available at http://www.tss.org.uk. [Google Scholar]
- Stochholm K, Juul S, Juel K, Weis Naeraa R, Gravholt CH. Prevalence, incidence, diagnostic delay, and mortality in Turner Syndrome. The Journal of Clinical Endocrinology & Metabolism. 2006;91(10):3897–3902. doi: 10.1210/jc.2006-0558. [DOI] [PubMed] [Google Scholar]
- Sullivan J, McConkie-Rosell A. Helping parents talk to their children. In: Gaff CL, Bylund CL, editors. Family communication about genetics: Theory and practice. Oxford: Oxford University Press; 2010. pp. 227–242. [Google Scholar]
- Sutton EJ, Young J, McInerney-Leo A, Bondy CA, Gollust SE, Biesecker B. Truth-telling and Turner Syndrome: The importance of diagnostic disclosure. The Journal of Pediatrics. 2006;148(1):102–107. doi: 10.1016/j.jpeds.2005.08.022. [DOI] [PubMed] [Google Scholar]
- Tartaglia N, Ayari N, Howell S, D’Epagnier C, Zeitler P. 48,XXYY, 48,XXXY and 49,XXXXY syndromes: Not just variants of Klinefelter syndrome. Acta Paediatrica. 2011;100:851–860. doi: 10.1111/j.1651-2227.2011.02235.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tartaglia NR, Howell S, Sutherland A, Wilson R, Wilson L. A review of trisomy X (47,XXX) Orphanet Journal of Rare Diseases. 2010;5(8) doi: 10.1186/1750-1172-5-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Visootsak J, Graham JM. Klinefelter syndrome and other sex chromosomal aneuploidies. Orphanet Journal of Rare Diseases. 2006;1(42) doi: 10.1186/1750-1172-1-42. [DOI] [PMC free article] [PubMed] [Google Scholar]