Abstract
Background
While there are reviews reporting on the prevalence of acute use of alcohol (AUA) prior to suicide attempts, no review has used a meta-analytic approach to estimate common odds ratios (OR) of the effect of AUA on suicide attempts. We aim to report the results of the first meta-analysis of controlled epidemiological studies on acute alcohol use and suicide attempt.
Methods
The English language literature on Medline, PsychInfo, Google Scholar, and public-use databases was searched for original articles and critical review reports on acute alcohol use and suicide attempt for the period ranging from 1996–2015. Studies had to report an OR estimate for this association. Common odds ratios and 95% Confidence Intervals (95%CI) from random effects in meta-analyses for any acute alcohol use and 2 levels of alcohol use on suicide attempt were calculated.
Results
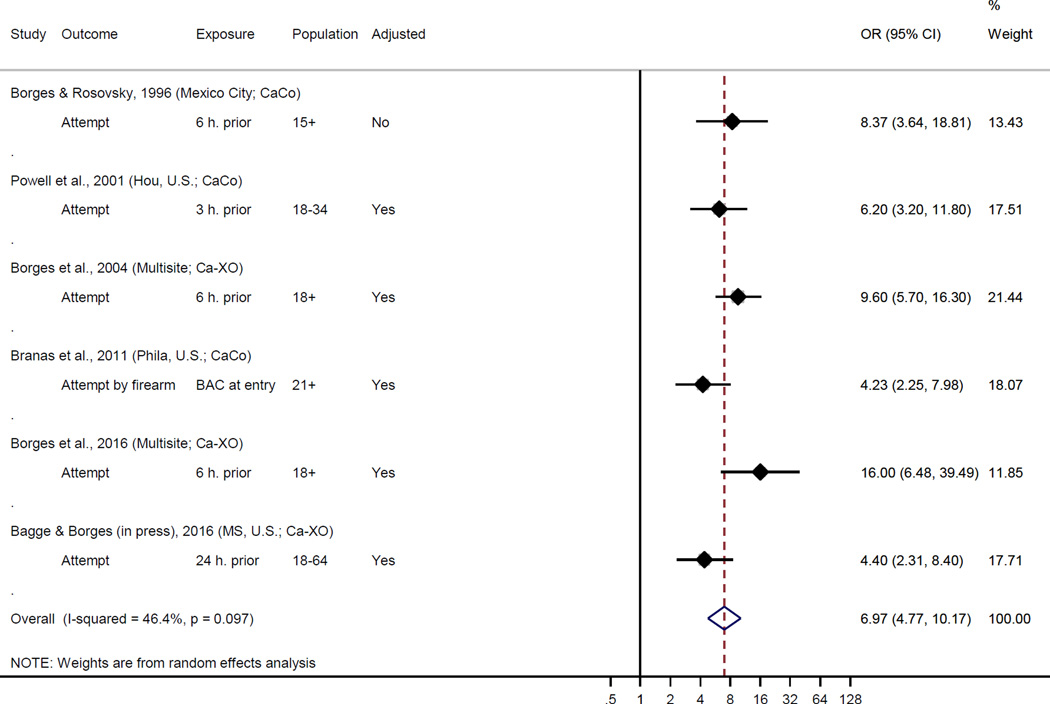
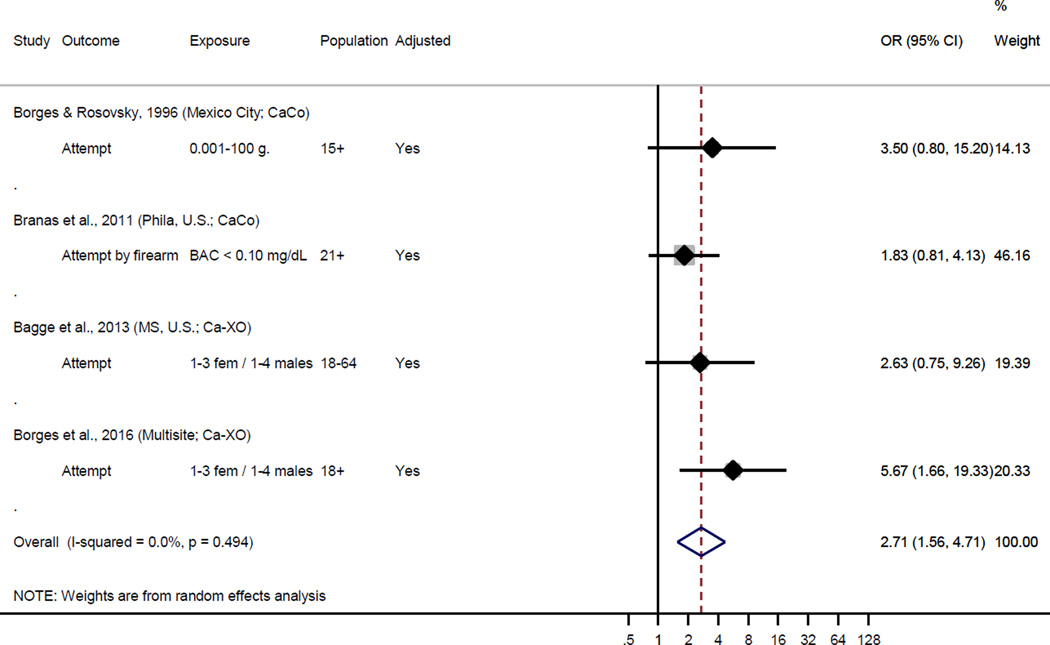
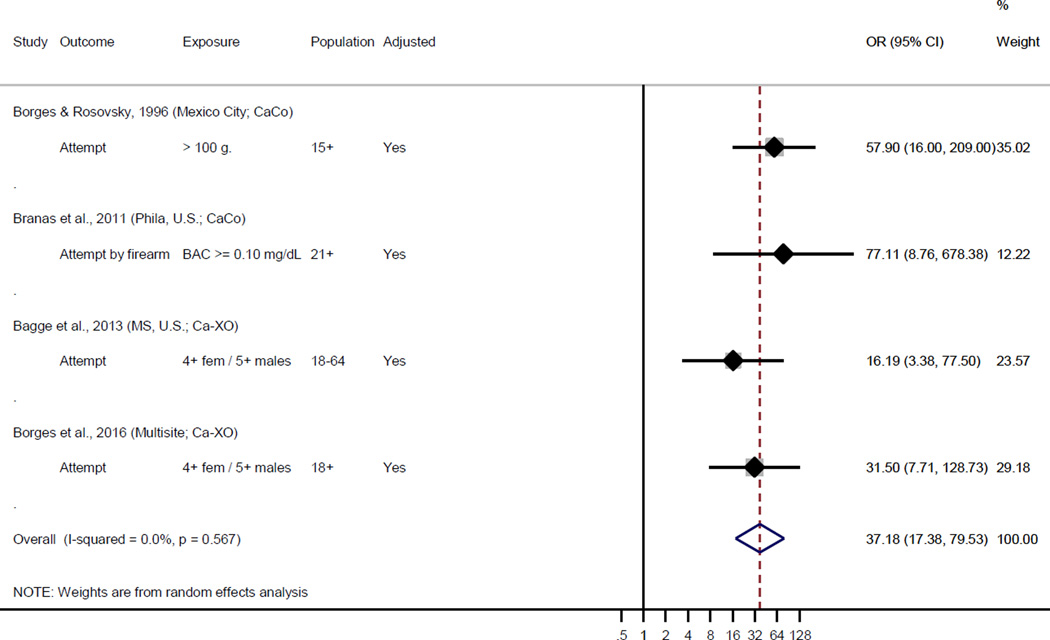
We gathered 7 studies that provided OR estimates for the likelihood of suicide attempt by acute alcohol use, compared to those who did not drink alcohol. Studies used case-control (3) and case-crossover design (4). All studies found increased ORs for acute alcohol use on suicide attempt. Meta-analysis revealed a common OR of 6.97 (95%CI=4.77, 10.17) for any acute alcohol use. Evidence from 4 studies suggests that «low levels of acute drinking» resulted in an OR of 2.71 (95%CI=1.56, 4.71) and «high levels» had much greater odds of suicide attempt, OR of 37.18 (95%CI=17.38, 79.53).
Conclusions
Acute use of alcohol is associated with increased likelihood of a suicide attempt, particularly at high doses. Such data should be incorporated into estimates of the burden of disease associated with alcohol use, which are currently limited by a consideration of only alcohol’s chronic effects. Future research should focus on the mechanisms through which acute use of alcohol confers risk for attempt.
Keywords: suicide attempt, meta-analyses, acute alcohol use, case-control, case-crossover
INTRODUCTION
In 2012, worldwide, over 800,000 deaths resulted from suicide and suicide accounted for 1.4% of all deaths, making it the 15th leading cause of death and the second leading cause of death in 15-29-year-olds (World Health Organization, 2014b). Harmful use of alcohol and alcohol use disorders (World Health Organization, 2014a) are one of the main risk factors for suicidal behavior (i.e., death by suicide and suicide attempts). Of the suicide disability-adjusted life year (DALY) that is attributable to mental and substance use disorders in 2010, alcohol dependence was responsible for the second largest proportion (13.25%), only behind major depressive disorder (Ferrari et al., 2014). The attributable fraction for alcohol on suicide in 2012 was estimated to be 20% of all DALYS ((World Health Organization, 2014a), figure 14).
Two dimensions of alcohol use including 1) acute use of alcohol (AUA) shortly prior to a behavior/event and 2) chronic alcohol use disorders (AUD), are associated with suicide fatalities (heretofore referred to simply as suicide) and nonlethal suicide attempt (heretofore referred to simply as suicide attempt) (Norström and Rossow, 2016). The extent of research on AUA and AUD in relation to suicide and suicide attempt (suicidal behavior) has not been uniform. The vast majority of research on alcohol-related risk for suicidal behavior has focused on the role of AUD (as reviewed by (Berglund and Ojehagen, 1998; Conner et al., 2008; Norström and Rossow, 2016)) and recent meta-analyses have shown elevated risk for these outcomes by AUD (Darvishi et al., 2015; Roerecke and Rehm, 2014). Notably, although correlated, AUA and AUD are distinct constructs (see (Conner et al., 2014)). For example studies have shown that AUA increases risk for suicidal behavior after adjusting for drinking pattern or AUD (Borges and Loera, 2010) and among those with a history of AUD, many instances of suicidal behavior occur outside windows of acute intoxication (Simon et al., 2002; Wojnar et al., 2008). Further, there are different proposed mechanisms underlying relations between AUA and AUD and suicidal behavior (Conner and Duberstein, 2004) (see also (Bagge and Sher, 2008) and (Conner et al., 2014) for a discussion).
As the focus of this study is on AUA and suicidal behavior, we will here briefly address possible underlying mechanisms for this association. First, consistent with the diathesis-stress model and related approaches (Mann et al., 1999), AUA may trigger suicide attempt in vulnerable individuals. Due to alcohol's acute effect on neurotransmittors and cognitive functions, AUA may propel suicide attempts through various mechanisms: by increasing dysphoria, aggressiveness and impulsivity (Oquendo and Mann, 2000); by weakening or removing barriers to self-harm; and by narrowing the ability to find alternative solution strategies (Bagge and Sher, 2008; Cherpitel et al., 2004; Hufford, 2001). From a sociological point of view, Durkheim's theory and concepts (1897/1951) offer a parallel line of thought. Here, anomie is defined as the social condition of unregulated persons and according to Durkheim, anomic suicide results from man's activity lacking regulation by society and his consequent sufferings (Durkheim, 1897). AUA, or a state of alcohol intoxication, can be regarded as representing a 'time-out' from the set of social norms regulating and controlling behaviour (Room, 2001). Within this framework, AUA may therefore be considered as a form of anomie, that is, a condition in which normal control mechanisms are weakened or eliminated (Cherpitel et al., 2004; Skog, 1991). Thus, the destructive consequences of AUA for social regulation ('anomic intoxication') is one way to explain why AUA may trigger suicidal behaviour (Skog, 1991). Although most studies of alcohol-related suicidal behaviour pertain to the role of AUD, controlled evidence on the role of AUA in death by suicide (e.g., (Branas et al., 2011; Kaplan et al., 2016) and suicide attempt (e.g., (Bagge et al., 2013; Borges et al., 2006) has been accumulating.
While there are reviews reporting on the prevalence of acute alcohol use prior to suicide attempts (Cherpitel et al., 2004) and two reviews reporting on AUA as a risk factor for suicidal behavior (Borges and Loera, 2010; Conner, 2015), no review has used a meta-analytic approach to estimate common odds ratios (OR) of the effect of AUA on suicide attempts (Norström and Rossow, 2016). Such estimates are essential for quantifying the causal effect of AUA on suicide attempts and for estimating the disease burden attributable to alcohol consumption. While it is well accepted that AUD affects the risk of suicide and these risks have been used in calculations of the burden of alcohol, the dimension of AUA has not been fully incorporated in these calculations. The aim of the current study is therefore to report a meta-analysis of epidemiological studies on the effect of AUA on suicide attempt. We report here only on acute alcohol use and suicide attempt because so far, to the best of our knowledge, only two studies have provided OR estimates for acute alcohol use and suicide (Branas et al., 2011; Kaplan et al., 2016).
MATERIALS AND METHODS
A prior review by one of us (Conner, 2015) listed the results of six published studies reporting estimates of the odds ratios (OR) of AUA on suicide attempts (Bagge et al., 2013; Borges et al., 2004; Borges et al., 2006; Borges and Rosovsky, 1996; Branas et al., 2011; Powell et al., 2001). For the current analysis we included these studies and also added the results of one recent study (Borges et al., 2016). Also available after Conner (Conner, 2015) is a new report from Bagge (Bagge and Borges, 2016) that is an extension of her prior work (Bagge et al., 2013) that includes now 363 suicide attempts (representing an increase of 171 cases). The report from Borges and colleagues (Borges et al., 2016), is also an extension of a prior work (Borges et al., 2006) (based on 152 cases of suicide attempt) that includes now 272 cases of suicide attempt (representing an increase of 120 cases). For completeness, we performed additional searches for the English language literature on Medline, PsychInfo, Google Scholar, and public-use databases for other original articles and critical review reports on AUA and suicide attempt, which reported odds ratio (OR) estimates for the period ranging from 1996–2015.
While new reports are available on cross-sectional samples of patients seeking treatment for a suicide attempt, that usually report exclusively on the presence of alcohol use prior to an attempt (for example, as in (Boenisch et al., 2010)), we focused here on controlled studies with non-suicide attempters serving as the control group (in case-control studies) or another time window serving as a within-subject control period (in case-crossover studies). We concentrated on studies where the ORs are interpretable as the risk of suicide attempt if drink prior to the attempt compared to not drinking prior to the attempt. Drinking prior to a suicide attempt was mostly defined by patients self-reported alcohol use within 3–24 hours prior to the attempt and in one study by positive blood alcohol level. Definitions of suicide attempt varied depending on the particular report, but most were cases of attempts that lead to a medical consultation, usually in emergency settings, and are somehow serious attempts. A new report from Iran on 305 cases of suicide attempt (Ghanbari et al., 2015) which did report an OR (OR=21.9, CI= 8.0–59.8) associated with acute use of alcohol, was not included in our meta-analyses because specific information regarding the control period was not included.
Common Odds ratios (OR) and 95% Confidence Intervals using random effects in meta-analyses for any AUA and varying levels of AUA were calculated using STATA software. We pooled the effect size for suicide attempt after alcohol use across studies using the DerSimonian and Laird random- effects method implemented in the “metan” command (Harris et al., 2008; Stata Statistical Sofware, 2013). Publication bias was assessed by visual inspection of funnel plots depicting the standard normal deviate of the estimates (the odds ratio divided by its standard error) against their precision (inverse of the S.E.): it is expected that symmetrical funnel plots will depict studies scatter around a line running through the origin (at standard normal deviate equal to zero), with a slope that indicates the size and direction of the effect. This was supported using Egger’s regression-based test, where asymmetry was assessed, due to the small number of studies included, with an intercept's p<0.10 (Egger et al., 1997). Between-study heterogeneity was quantified by I2 and Cochran’s Q (Higgins et al., 2003). I2 can be interpreted as the percentage of the total variance due to between-study heterogeneity.
RESULTS
Table 1 presents the main data and characteristics from the 7 studies that estimated the association for AUA and suicide attempt. The studies analyzed data from trauma hospitals/emergency room admissions in 19 countries. Three studies used a case-control design and the remaining four used the case-crossover strategy. The reference period for AUA prior to suicide attempt varied across studies; from three hours to 24 hours. Two studies (Bagge et al., 2013) (Bagge and Borges, 2016) are not independent samples. In 2013 Bagge and colleagues (Bagge et al., 2013) reported on a reduced sample that included levels of drinking; in 2016 Bagge and Borges (Bagge and Borges, 2016) reported on a larger sample of any AUA, but did not report on levels of drinking. We thereby used her work from 2016 (Bagge and Borges, 2016) for the estimate of “any alcohol use” in meta-analyses for Figure 1 and her work from 20013 (Bagge et al., 2013) for estimating levels of drinking for meta-analyses in Figures 2 and 3. Similarly, Borges et al reported first in 2004 on 102 suicide attempts and provided now in 2016 data on 272 attempts (including the 102 reported before) from a larger set of EDs. Prevalence of any AUA in those 7 studies ranged from 26.5% to a high 44.4% (mean prevalence= 33%) and ORs ranged from a low 4.2 to a high16.0. The number of variables and the substantive relevance of control variables in case-control studies varied widely. In case-crossover studies, by design all time-constant variables (such as age and sex) are kept constant and thus are controlled by design. Trait variables, such as impulsivity, are also constant and other psychiatric variables (such as mood disorders) are also kept constant, to the extent that they are not acute episodes. Four out of these 7 studies provide estimates for 3 alcohol consumption levels (no acute consumption being the first level). Definitions of “low” and “high” consumption varied across studies, as seen in Table 1. Across studies “low drinking” levels varied from 0.001–100grs to BAC < 0.10 mg/dL and 1–3 drinks for females / 1–4 drinks for males; “heavy drinking” levels varied from >100grs to BAC >= 0.10 mg/dL and 4+ drinks for females / 5+ drinks for males.
Table 1.
Studies with Odds Ratio (ORs) estimates for acute alcohol use and suicide attempt. Any acute alcohol use, low and heavy drinking.
| Author/year | Study type | Number of cases |
Prevalence of exposure |
ORs (95% CI) | Description of cases // controls (or control period) |
Control variables |
|---|---|---|---|---|---|---|
|
Borges & Rosovsky, 1996 (any alcohol use recalculated) |
Case-control | 36 | 6 hours before the attempt / 44.4% |
Any alcohol 8.37 (3.64, 18.81) Low drinking 3.50 (0.80, 15.20) Heavy drinking 57.90 (16.00, 209.00) |
Suicide attempts from eight emergency room (ER) hospitals in Mexico City // The control group comprised patients (N = 372) admitted to ER because of workplace accidents, animal bites and recreational accidents except drowning). |
Sex, age, day of event, education, employment status, marital status. |
| Powell et al., 2001 | Case-control | 153 | 3 hour prior / 26.5% |
Any alcohol 6.20 (3.20, 11.80) |
Suicide attempt at the emergency departments // 513 control-subjects from the same geographic area were enrolled during the same time period using a random-digit-dialed telephone survey of three major hospitals in central Houston. |
Symptoms of depression, migration, body mass index, upsetting end to a relationship, having a “nonsuicide death exposure” exposure to suicidal behavior, sex, age group, race/ethnicity, marital status, years of education completed, employment, and total household income. |
| Borges et al., 2004 | Case- crossover- usual frequency |
102 | 6 hours before the attempt / 35% |
Any alcohol 9.60 (5.70, 16.30) |
Suicide attempts from seven ER studies carried out in the United States, Canada, Mexico and Australia // Usual alcohol consumption during the past 12 months served as the control period. |
All fixed-time variables are controlled by design |
| Branas et al., 2011 | Case-control | 149 | Blood alcohol concentrations from emergency departments and the morgue / 31% |
Any alcohol 4.23 (2.25, 7.98) Low drinking 1.83 (0.81, 4.13) Heavy drinking 77.11 (8.76, 678.38) |
Self-inflicted gun injury cases residents of Philadelphia identified at the Philadelphia Police Department // 302 population-based controls were sampled from all of Philadelphia using random digit dialing was conducted from 2003 to 2006. |
Age, race, gender, ethnicity, unemployment, education, and marital status. Situational characteristics being outdoors, the neighborhood within which the shooting occurred: its alcohol outlet availability, racial and ethnic makeup, unemployment and income levels, and education. |
| Bagge et al., 2013 | Case- crossover- pair matching |
192 | 6 hours before the attempt / 24.5% |
Any alcohol 6.30 (2.10, 19.30) Low drinking 2.63 (0.75, 9.26) Heavy drinking 16.19 (3.38, 77.50) |
Suicide attempters presenting to a Level 1 trauma hospital in the state of Mississippi // control period was the matching 6 hours the day before. |
All fixed-time variables are controlled by design. Plus other drug use and negative life events prior to the attempt within the case period. |
| Bagge and Borges (in press), 2016 | Case- crossover- pair matching |
336 | 24 hours prior to the attempt / 33.1% |
Any alcohol 4.40 (2.31, 8.40) |
Recent suicide attempters presenting to a Level 1 trauma hospital in the State of Mississippi// control period was the matching 24 hours the day before. |
All fixed-time variables are controlled by design. Plus other drug use and negative life events prior to the attempt within the case period. |
| Borges et al., 2016 | Case- crossover- pair matching |
272 | 6 hours before the attempt / 37.1% |
Any alcohol 16.00 (6.48, 39.49) Low drinking 5.67 (1.66, 19.33) Heavy drinking 31.50 (7.71, 128.73) |
Suicide attempts from seven ER studies carried out in Argentina, Belarus, Brazil, Canada, China, Costa Rica, Dominican Republic, Guatemala, Guyana, India, Ireland, Korea, Mexico, Nicaragua, Panama, Sweden and Taiwan // alcohol during the same 6 hours time-period on the same day in the previous week. |
All fixed-time variables are controlled by design |
| Cut-points: | "low drinking" | "heavy drinking" |
|---|---|---|
| Borges & Rosovsky, 1996 | 0.001–100 g. | > 100 g. |
| Branas et al., 2011 | BAC < 0.10 mg/dL | BAC >= 0.10 mg/dL |
| Bagge et al., 2013 | 1–3 fem / 1–4 males | 4+ fem / 5+ males |
| Borges et al., 2016 | 1–3 fem / 1–4 males | 4+ fem / 5+ males |
Figure 1.
Forest plot showing effect sizes for suicide attempt according to any acute alcohol use in individual studies
Heterogeneity Q = 9.32 (5 df); p = 0.097
Egger's test for small-study effects p = 0.251
Ca-XO: Case-Crossover, CaCo:Case-Control, fem:Female, BAC: Blood Alcohol Concentration
Hou: Houston, Phila: Philadelphia, MS: Mississippi
2004 Multisite (4 countries): US, CA, MX & AU
2016 Multisite (17 countries): AR, BY, BR, CA, CN, CR, DO, GT, GY, IN, IE, KR, MX, NI, PA, SE & TW
Figure 2.
Forest plot showing effect sizes for suicide attempt according to 'low acute alcohol use' in individual studies
Heterogeneity Q = 2.4 (3 df); p = 0.494
Egger's test for small-study effects p = 0.251
Ca-XO: Case-Crossover, CaCo:Case-Control, fem:Female, BAC: Blood Alcohol Concentration
Phila: Philadelphia, MS: Mississippi
2016 Multisite (17 countries): AR, BY, BR, CA, CN, CR, DO, GT, GY, IN, IE, KR, MX, NI, PA, SE & TW
Figure 3.
Forest plot showing effect sizes for suicide attempt according to 'heavy acute alcohol use' in individual studies
Heterogeneity Q = 2.02 (3 df); p = 0.567
Egger's test for small-study effects p = 0.879
Ca-XO: Case-Crossover, CaCo:Case-Control, fem:Female, BAC: Blood Alcohol Concentration
Phila: Philadelphia, MS: Mississippi
2016 Multisite (17 countries): AR, BY, BR, CA, CN, CR, DO, GT, GY, IN, IE, KR, MX, NI, PA, SE & TW
Figure 1 shows the forest plot odds ratios (ORs) and 95% confidence intervals (CIs) for any AUA in individual studies and the pooled OR from random effect models, while Figures 2 and 3 shows these ORs for “low” and “high” acute alcohol levels. Although there was no evidence for heterogeneity or publication bias within any of the 3 figures, nonetheless we used random effect estimates in order to be conservative. Examination of all studies included in Figure 1 revealed increased ORs of suicide attempt after any AUA. The common OR from meta-analysis was 6.97 (95% CI=4.77, 10.17). Evidence from 4 studies, presented in Figures 2 and 3, suggests that a lower level of consumption increased acute risk for suicide attempt, with a common OR from meta-analysis of 2.71 (95% CI=1.56, 4.71). High levels of AUA resulted in even greater odds of suicide attempt (common OR from meta-analysis was 37.18 (95% CI=17.38, 79.53)).
DISCUSSION
This is the first study to use meta-analytic techniques to determine the magnitude of the effect of AUA on suicide attempt. Any AUA was associated with increased risk of a suicide attempt, with a common OR from meta-analysis of 6.97 (95% CI=4.77, 10.17). Furthermore, dose-response results indicated that the higher the amount of AUA consumed the greater the risk, with «low levels of acute drinking» resulting in an OR of 2.71 (95% CI=1.56, 4.71) and «high levels» had much greater odds of suicide attempt, showing an OR of 37.18 (95% CI=17.38, 79.53). The obtained prevalence of AUA preceding a suicide attempt is in line with previous reviews on this topic (e.g., (Cherpitel et al., 2004). However, since the mere presence (prevalence) of AUA does not inform the magnitude of AUA-related risk for suicide attempts, the current review greatly adds to the literature by solely focusing on prior studies, which include a control group or a within-subject control period.
The estimates of AUA on suicide attempt derived from case-crossover studies are above and beyond the effects of chronic alcohol use (such as alcohol use disorders), which suggest that there are specific mechanisms by which AUA poses risk for suicide attempt. Theoretically, these may be of several kinds, as noted above, and the primary studies included in this meta-analytic study did not have the capacity to address this issue. However, AUA’s role in suicidal behavior by increasing dysphoria was illustrated in a recent study by (Bagge et al., 2014). This study demonstrated that across the 24 hours prior to a suicide attempt, the AUA within a specific hour led to increased intensity of suicidal ideation in the subsequent hour, controlling for the prior hour level of suicidal ideation. Further, some individuals use alcohol prior to an attempt to facilitate the attempt (e.g., numb fears about attempting)(see (Bagge et al., 2015). This research demonstrates that a “one size fits all” model cannot be used to understand the role of AUA on suicide attempts.
The observed dose-response relationship between AUA and suicidal behaviour may be explained by an immediate dose dependent effect of AUA on the central nervous system. There are indications of a dose-response relationship between blood alcohol concentration (intoxication level) and acute effects on - aggressiveness and impulsivity (Caswell et al., 2013; Dougherty et al., 2008; Gustafson, 1993); - on feelings of sadness (or mood) (Heinz et al., 2001); and on cognitive functions (Peterson et al., 1990; Popke et al., 2000). Thus, high alcohol doses, as compared to lower doses, seem to produce stronger effects on mood and cognitive states that play a causal role in suicidal behaviour.
More empirical research on mechanisms that may underlie the AUA–suicide attempt relation is needed. However, there are ethical concerns to conducting laboratory mechanistic experiments focused on providing alcohol/inducing distress to currently suicidal patients. Further, the low incidence of suicide attempts makes it impractical to conduct prospective analysis (such as ecological momentary assessment) to study drinking and other factors occurring within the hours of a suicide attempt. Moreover, asking a participant to continue to document his/her experience within an acute suicidal crisis would mandate intervention that would alter the course of the acute factors being studied. Therefore, an expanded timeline followback design may be an option for helping to pinpoint potential mechanisms (e.g., increased levels of distress) underlying the relation between AUA and suicide attempts (as developed in (Bagge et al., 2013).
In addition, future research using much larger samples are needed to determine specially for what subgroups (e.g., combination of distal risk factors), AUA poses increased risk for suicide attempt. Integration and simultaneous analysis of both vulnerability/distal and acute factors would provide critical information for comprehensive and integrated suicide models and ultimately inform suicide prevention efforts.
Limitations
There are a number of limitations to this study that deserve comment and suggest future areas of research. This study uses data from reports of patients from different countries, and given the low number of studies available to meta-analyses we were not able to determine how effects differ by individual characteristics (e.g. age, gender, social class) or at the country level or by cultural context. Prior studies conducted by Cherpitel (Cherpitel et al., 2015) on possible effects of a country-level drinking pattern determined by the World Health Organization (WHO) country’s detrimental drinking pattern (DDP) (Rehm et al., 2001) shows that countries with the most detrimental drinking patterns may have increased alcohol attributable fractions for injuries than countries with a lower DDP. Others (Norström and Rossow, 2016) also showed that the relation between alcohol abuse and suicide may vary at the population level across cultures with different drinking patterns. Whether such variations could be present on the relation between acute alcohol use and suicide attempt remains a matter of future inquiry.
In the 3 obtained case-control studies the list of control variables varied widely, only one study reported to control for symptoms of depression (Powell et al., 2001), and 0/3 studies controlled for habitual alcohol consumption. However, in terms of the latter, it is important to note that research on suicidal behaviours broadly shows that alcohol-related death is due to alcohol’s acute effects, and not its chronic effects (such as disease progression; see (Conner, 2015). Further, habitual alcohol use is controlled by design in case-crossover studies. In case-crossover studies, variables that do not vary day-to-day (e.g., sex, history of mood and substance use disorders, chronic drinking patterns, childhood abuse, personality traits) are controlled for by study design (because subjects act as their own control). Thus, obtained results are not an artifact of chronic drinking or other fixed factors. However it is possible that other variables that can fluctuate day-to-day (such as episodes of anger, mood swings, use of other substances and acute stressful events) may account for obtained results. Only the case-crossover studies conducted by Dr. Bagge’s research group (Bagge et al., 2013) and (Bagge and Borges, 2016) adjusted for other acute exposures. The study in Mississippi ruled out the presence of confounding for 2 main acute time-varying confounding variables (other acute substances and negative events).
This meta-analysis is provided by authors with extensive experience examining acute use of alcohol and suicide attempts and in updating this literature in published reviews and, to our knowledge, it includes all of the published reports that met our inclusion criteria, but we did not conduct a formal literature search to confirm that our analysis is comprehensive. While this report uses data from different reports that included patients from different countries, we still have but a few primary studies from a few countries, and the generalizability of these findings beyond the ‘cultural contexts’ of those populations studied here are beyond our possibilities.
CONCLUSION
The current study found that any AUA is associated with increased likelihood of a suicide attempt, particularly at high doses. Such data should be incorporated into estimates of the burden of disease associated with alcohol use which currently only incorporates alcohol’s chronic effects on both acute and chronic conditions. We conclude that AUA plays an important role in suicide attempts and should be considered strongly in theory and clinical practice.
Acknowledgments
This work was done while Guilherme Borges was on a consultancy for the Management of Substance Abuse (MSB), Department of Mental Health and Substance Abuse (MSD)-World Health Organization (Geneva- Switzerland)-
Partially supported by a grant from the U.S. Institute of Alcohol Abuse and Alcoholism (5 R01 AA013750) (CJC)
Footnotes
A presentation of an initial version of this manuscript was done at the World Health Organization (WHO) SUBSTANCE USE AND SUICIDE IN THE INTERNATIONAL CONTEXT, GENEVA, SWITZERLAND, WHO HEADQUARTERS, 19–21 October 2015
Declarations of interest
All authors declare that they have no conflict of interest.
References
- Bagge CL, Borges G. Acute substance use as a warning sign for suicide attempts: A Case-crossover examination of the 48 hours prior to a recent suicide attempt. J Clin Psychiatry. 2016 doi: 10.4088/JCP.15m10541. Ref Type: In Press. [DOI] [PubMed] [Google Scholar]
- Bagge CL, Conner KR, Reed L, Dawkins M, Murray K. Alcohol use to facilitate a suicide attempt: An event-based examination. J Stud Alcohol Drugs. 2015;76:481. doi: 10.15288/jsad.2015.76.474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bagge CL, Lee HJ, Schumacher J, Gratz K, Krull J, Holloman G. Alcohol as an acute risk factor for recent suicide attempts: A case-crossover analysis. J Stud Alcohol Drugs. 2013;74:552–558. doi: 10.15288/jsad.2013.74.552. [DOI] [PubMed] [Google Scholar]
- Bagge CL, Littefield AK, Conner KR, Schumacher J, Lee HJ. Near-term predictors of the intensity of suicidal ideation: An examination of the 24 hours prior to a recent suicide attempt. J Affect Disord. 2014;165:53–58. doi: 10.1016/j.jad.2014.04.010. [DOI] [PubMed] [Google Scholar]
- Bagge CL, Sher KJ. Adolescent alcohol involvement and suicide attempts: Toward the development of a conceptual framework. Clin Psychol Rev. 2008;28:1283–1296. doi: 10.1016/j.cpr.2008.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berglund M, Ojehagen A. The influence of alcohol drinking and alcohol use disorders on psychiatric disorders and suicidal behavior. Alcohol Clin Exp Res. 1998;22:333S–345S. doi: 10.1097/00000374-199807001-00010. [DOI] [PubMed] [Google Scholar]
- Boenisch S, Bramesfeld A, Mergl R, Havers I, Althaus D, Lehfeld H, Niklewski G, Hegerl U. The role of alcohol use disorder and alcohol consumption in suicide attempts–A secondary analysis of 1921 suicide attempts. Eur Psychiatry. 2010;25:414–420. doi: 10.1016/j.eurpsy.2009.11.007. [DOI] [PubMed] [Google Scholar]
- Borges G, Cherpitel C, MacDonald S, Giesbrecht N, Stockwell T, Wilcox HC. A case-crossover study of acute alcohol use and suicide attempt. J Stud Alcohol Drugs. 2004;65:708–714. doi: 10.15288/jsa.2004.65.708. [DOI] [PubMed] [Google Scholar]
- Borges G, Cherpitel C, Orozco R, Bond J, Ye Y, MacDonald S, Rehm J, Poznyak V. Multicentre study of acute alcohol use and non-fatal injuries: Data from the WHO collaborative study on alcohol and injuries. Bull World Health Organ. 2006;84:453–460. doi: 10.2471/blt.05.027466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borges G, Loera CR. Alcohol and drug use in suicidal behaviour. Curr Opin Psychiatry. 2010;23:195–204. doi: 10.1097/YCO.0b013e3283386322. [DOI] [PubMed] [Google Scholar]
- Borges G, Cherpitel C, Orozco R, Ye Y, Monteiro M, Hao W, Benegal V. A dose-response estimate for acute alcohol use and risk of suicide attempt. Addict Biol. 2016 doi: 10.1111/adb.12439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borges G, Rosovsky H. Suicide attempts and alcohol consumption in an emergency room sample. J Stud Alcohol Drugs. 1996;57:543–548. doi: 10.15288/jsa.1996.57.543. [DOI] [PubMed] [Google Scholar]
- Branas CC, Richmond TS, Ten Have TR, Wiebe DJ. Acute alcohol consumption, alcohol outlets, and gun suicide. Subst Use Misuse. 2011;46:1592–1603. doi: 10.3109/10826084.2011.604371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caswell AJ, Morgan MJ, Duka T. Acute alcohol effects on subtypes of impulsivity and the role of alcohol-outcome expectancies. Psychopharmacology (Berl) 2013;229:21–30. doi: 10.1007/s00213-013-3079-8. [DOI] [PubMed] [Google Scholar]
- Cherpitel C, Borges G, Wilcox HC. Acute alcohol use and suicidal behavior: A review of the literature. Alcohol Clin Exp Res. 2004;28:18S–28S. doi: 10.1097/01.alc.0000127411.61634.14. [DOI] [PubMed] [Google Scholar]
- Cherpitel C, Ye Y, Bond J, Borges G, Monteiro M. Relative risk of injury from acute alcohol consumption: modeling the dose–response relationship in emergency department data from 18 countries. Addiction. 2015;110:279–288. doi: 10.1111/add.12755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conner KR. Commentary on "The modal suicide decedent did not consume alcohol just prior to the time of death: An analysis with implications for understanding suicidal behavior". J Abnorm Psychol. 2015;124:457–459. doi: 10.1037/abn0000047. [DOI] [PubMed] [Google Scholar]
- Conner KR, Bagge CL, Goldston DB, Ilgen MA. Alcohol and suicidal behavior: What is known and what can be done. Am J Prev Med. 2014;47:S204–S208. doi: 10.1016/j.amepre.2014.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conner KR, Duberstein PR. Predisposing and precipitating factors for suicide among alcoholics: Empirial review and conceptual integration. Alcohol Clin Exp Res. 2004;28:6S–17S. doi: 10.1097/01.alc.0000127410.84505.2a. [DOI] [PubMed] [Google Scholar]
- Conner KR, McCloskey MS, Duberstein PR. Psychiatric risk factors for suicide in the alcohol-dependent patient. Psychiat Ann. 2008;38:742–748. [Google Scholar]
- Darvishi N, Farhadi M, Haghtalab T, Poorolajal J. Alcohol-related risk of suicidal ideation, suicide attempt, and completed suicide: a meta-analysis. PloS one. 2015;10:e0126870. doi: 10.1371/journal.pone.0126870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dougherty DM, Marsh-Richard DM, Hatzis ES, Nouvion SO, Mathias CW. A test of alcohol dose effects on multiple behavioral measures of impulsivity. Drug Alcohol Depend. 2008;96:111–120. doi: 10.1016/j.drugalcdep.2008.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Durkheim E. Suicide. 1951. New York: Free Press; 1897. [Google Scholar]
- Egger M, Davey S, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrari AJ, Norman RE, Freedman GD, Baxter AJ, Pirkis J, Harris MG, Page A, Carnahan E, Degenhardt L, Vos T, Whiteford H. The burden attributable to mental and substance use disorders as risk factors for suicide: findings from the Global Burden of Disease Study 2010. PloS one. 2014;9:e91936. doi: 10.1371/journal.pone.0091936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghanbari B, Malakouti SK, Nojomi M, De Leo D, Saeed K. Alcohol abuse and suicide attempt in Iran: A case-crossover study. Glob J Health Sci. 2015;8:53092. doi: 10.5539/gjhs.v8n7p58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gustafson R. What do experimental paradigms tell us about alcohol-related aggressive responding? J Stud Alcohol Supplement. 1993:20–29. doi: 10.15288/jsas.1993.s11.20. [DOI] [PubMed] [Google Scholar]
- Harris RJ, Bradburn MJ, Deeks JJ, Harbord RM, Altman DG, Sterne JAC. metan: fixed- and random-effects meta-analysis. Stata J. 2008;8:3–28. [Google Scholar]
- Heinz A, Mann K, Weinberger DR, Goldman D. Serotonergic dysfunction, negative mood states, and response to alcohol. Alcohol Clin Exp Res. 2001;25:487–495. [PubMed] [Google Scholar]
- Higgins J, Deeks JJ, Thompson S, Deeks, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hufford MR. Alcohol and suicidal behavior. Clin Psychol Rev. 2001;21:797–811. doi: 10.1016/s0272-7358(00)00070-2. [DOI] [PubMed] [Google Scholar]
- Kaplan MS, Huguet N, McFarland BH, Caetano R, Conner KR, Nolte KB, Giesbrecht N. Heavy alcohol use among suicide decedents and a population-based living comparison sample: Differences in risk across racial/etnic groups. Psychiatr Serv. 2016;67:258. doi: 10.1176/appi.ps.201500494. [DOI] [PubMed] [Google Scholar]
- Mann JJ, Waternaux C, Haas GL, Malone KM. Toward a clinical model of suicidal behavior ir psychiatric patients. Am J Psychiatry. 1999;156:181–189. doi: 10.1176/ajp.156.2.181. [DOI] [PubMed] [Google Scholar]
- Norström T, Rossow I. Alcohol consumption as a risk factor for suicidal behaviour: a systematic review of associations at the individual and at the population level. Arch Suicide Res. 2016 doi: 10.1080/13811118.2016.1158678. [DOI] [PubMed] [Google Scholar]
- Oquendo MA, Mann JJ. The biology of impulsivity and suicidality. Psychiatr Clin North Am. 2000;23:11–25. doi: 10.1016/s0193-953x(05)70140-4. [DOI] [PubMed] [Google Scholar]
- Peterson JB, Rothfleisch JM, Zelazo PD, Pihl RO. Acute alcohol intoxication and cognitive functioning. J Stud Alcohol. 1990;51:114–122. doi: 10.15288/jsa.1990.51.114. [DOI] [PubMed] [Google Scholar]
- Popke EJ, Allen SR, aule MG. Effects of acute ethanol on indices of cognitive-behavioral performance in rats. Alcohol. 2000;20:187–192. doi: 10.1016/s0741-8329(99)00081-6. [DOI] [PubMed] [Google Scholar]
- Powell KE, Kresnow M, Mercy JA, Potter LB, Swann AC, Frankowski RF, Lee RK, Bayer TL. Alcohol consumption and nearly lethal suicide attempts. Suicide Life Threat Behav. 2001;32:30–41. doi: 10.1521/suli.32.1.5.30.24208. [DOI] [PubMed] [Google Scholar]
- Rehm J, Monteiro M, Room R, Gmel G, Jernigan D, Frick U, Graham K. Steps towards constructing a global comparative risk analysis for alcohol consumption: determining indicators and empirical weights for patterns of drinking, deciding about theoretical minimum, and dealing with different consequences. Eur Addict Res. 2001;7:138–147. doi: 10.1159/000050731. [DOI] [PubMed] [Google Scholar]
- Roerecke M, Rehm J. Cause-specific mortality risk in alcohol use disorder treatment patients: a systematic review and meta-analysis. Int J Epidemiol. 2014;43:906–919. doi: 10.1093/ije/dyu018. [DOI] [PubMed] [Google Scholar]
- Room R. Intoxication and bad behaviour: understanding cultural differences in the link. Soc Sci Med. 2001;53:189–198. doi: 10.1016/s0277-9536(00)00330-0. [DOI] [PubMed] [Google Scholar]
- Simon TR, Swann AC, Powell KE, Potter LB, Kresnow M, O´Carroll PW. Characteristics of impulsive suicide attempts and attempters. Suicide Life Threat Behav. 2002;32:49–59. doi: 10.1521/suli.32.1.5.49.24212. [DOI] [PubMed] [Google Scholar]
- Skog O. Alcohol and suicide- Durkheim revisited. Acta Sociol. 1991;34:193–206. [Google Scholar]
- Stata Statistical Sofware. Release 13. College Station, TX: StataCorp LP; 2013. [Google Scholar]
- Wojnar M, Ilgen MA, Jakubczyk A, Wnorowskaa A, Klimkiewicz A, Brower KJ. Impulsive suicide attempts predict post-treatment relapse in alcohol-dependent patients. Drug Alcohol Depend. 2008;97:268–275. doi: 10.1016/j.drugalcdep.2008.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. Global status report on alcohol and health 2014. Geneva, Switzerland: World Health Organization; 2014a. [Google Scholar]
- World Health Organization. Preventing suicide: A global imperative. Geneva, Switzerland: World Health Organization; 2014b. [Google Scholar]