Abstract
The evidence base for psychopharmacologic interventions in youth with depressive and anxiety disorders as well as attention/deficit hyperactivity disorder (ADHD) has dramatically increased over the past two decades. Psychopharmacologic interventions commonly utilized in the pediatric primary care setting—selective serotonin (norepinephrine) reuptake inhibitors (SSRIs/SSNRIs), stimulants and α2 agonists—are reviewed. General pharmacologic principles are summarized along with class-related side effects and tolerability concerns (e.g., suicidality and activation in antidepressant-treated youth as well as insomnia, irritability, anorexia in stimulant-treated pediatric patients). Selected landmark trials of antidepressant medications in youth with depressive disorders (Treatment of Adolescent Depression Study [TADS] and the Treatment of SSRI-Resistant Depression Study [TADS]) and anxiety disorders (Child/Adolescent Anxiety Multimodal Study [CAMS] and Child/Adolescent Anxiety Multimodal Extended Long-term Study [CAMELS]) are described in addition to the Multimodal Treatment of ADHD Study. Finally, available data are presented that are related to prediction of treatment outcomes in youth with depressive disorders, anxiety disorders and ADHD.
Keywords: Selective Serotonin Reuptake Inhibitor (SSRI), Selective Norepinephrine Reuptake Inhibitor (SNRI), antidepressants, psychopharmacology, stimulants
INTRODUCTION
In children and adolescents, attention-deficit/hyperactivity disorder (ADHD) as well as anxiety and depressive disorders are not only common,1,2 but are associated with significant morbidity and both depressive and anxiety disorders increase the risk of suicidality in adolescents.3–5 From both a primary care and a public health perspective, effective diagnosis and treatment of these conditions is critical to prevent morbidity and to decrease the likelihood of developing secondary psychopathology. While there has been an increased acceptance of psychopharmacologic interventions among pediatricians, reliance on purely pharmacologic approaches to these conditions has raised concerns related to the underutilization of psychotherapeutic and family-based interventions.6 Despite the psychopharmacologic treatments in children and adolescents being initiated by some primary care clinicians, many remain hesitant to prescribe these medications;7,8 they attribute this discomfort to a lack of confidence,8 deficits and/or perceived deficits in their fund of knowledge.8,9
Over the last two decades, the clinical trial data supporting the use of psychopharmacologic interventions in children and adolescents has dramatically increased and, more recently these clinical trial data have been subjected to meta-analytic evaluations.10–12 However, reports of the effectiveness and tolerability of psychopharmacologic interventions in youth have been poorly disseminated outside of the psychiatric literature. Therefore, this paper reviews selected treatment trials of antidepressants and stimulants in pediatric patients, explores predictors of response to treatment selected medication side effects.
Evidence for Selective Serotonin Reuptake Inhibitors and Selective Serotonin Norepinephrine Reuptake Inhibitors in Major Depressive Disorder
Following the discovery of SSRI’s in the 1980s, the following decade saw a tsunami of studies evaluating these agents, and later the selective serotonin norepinephrine reuptake inhibitors (SSNRIs) which were introduced later during that decade. Until very recently however, the dosing of the SSRIs/SSNRIs in youth with major depressive disorder (MDD) was based on adaptation of adult dosing strategies—a feature that may have resulted in several “failed” trials of antidepressant medications and in poorer tolerability profiles of some antidepressants in a subset of the randomized, placebo-controlled trials in youth with MDD.13 Moreover, while accumulating positive trials of the SSRIs populated the literature following the initial positive trial of fluoxetine in pediatric patients with MDD14 in the mid-1990s, increasing numbers of failed trials and negative trials began to emerge.15–17 The evaluation of antidepressants in pediatric patients with MDD is complicated by increasing placebo response rates18 which have been hypothesized by some to have resulted in a number of these “failed trials”18,19 Several efforts have been made to understand placebo-response in depressed youth and it appears that this may be the result of non-specific supportive care that is provided in the context of a clinical trial, although at least one recent analyses suggests that placebo response in depressed youth may also be related to patient level factors, including socioeconomic status, age and duration of illness.19,20
At present, only two antidepressants have received FDA approval for the treatment of major depressive disorder in youth: fluoxetine and escitalopram.21 The evidence base for fluoxetine is the strongest and supported by pediatric registration trials14 and buttressed by data from the Treatment of Adolescent Depression Study (TADS)22 and the Treatment of SSRI Resistant Depression Study (TORDIA)23 and by relapse-prevention data that suggest durability of treatment effect.24 Rather than reviewing the individual studies of each antidepressant, representative, large trials will be reviewed in detail to provide a practical overview of SSRI use in children and adolescents with MDD as well as treatment-resistant MDD.
Treatment of Adolescent Depression Study (TADS)
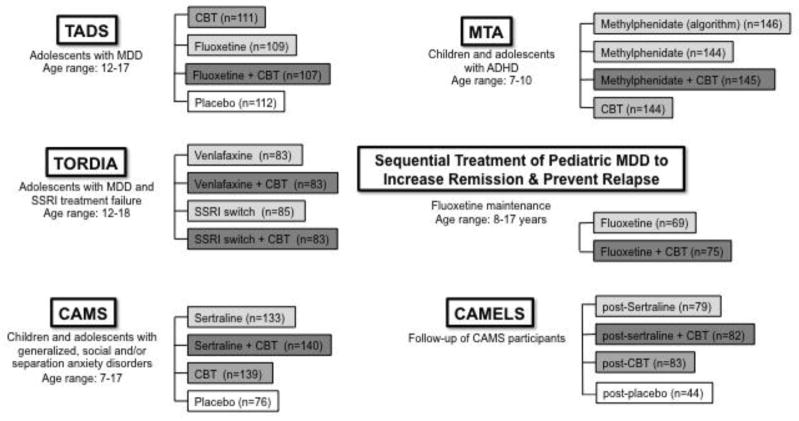
This multi-center study, which was funded by the National Institute of Mental Health, began more than 15 years ago and randomized children and adolescents with MDD to (1) fluoxetine monotherapy (10–40 mg/d), (2) CBT monotherapy, (3) CBT + fluoxetine (10–40 mg/d), or (4) placebo (Figure 1A) and evaluated the change in the Children's Depression Rating Scale-Revised25 total score as well as the Clinical Global Impressions improvement scores.26 Following 12 weeks of treatment, patients who received fluoxetine + CBT were significantly more improved compared to patients who had received either CBT or fluoxetine monotherapy. Additionally, fluoxetine monotherapy was superior to CBT monotherapy and all active treatments were superior to placebo; however it is noteworthy that more than a third of placebo-treated patients (34.8%) were classified as responders. Importantly, suicidal ideation improved across all treatments, although the greatest reductions in suicidal ideation were observed in patients who received CBT + fluoxetine.22
FIGURE 1.
Landmark studies in youth with major depressive disorder, anxiety disorders and attention/deficit hyperactivity disorder (ADHD).
Given the large sample size in TADS, Kratchovil and colleagues27 were able to examine the trajectory of improvement in depressive symptoms. These analyses modeled the time to first response and time to stable response across three of the treatments: fluoxetine + CBT, fluoxetine and placebo. Of note, fluoxetine monotherapy and CBT monotherapy could not be compared secondary to differences in contact time and visit frequency. Youth who received fluoxetine + CBT had a threefold greater probability of sustained response compared to patients who had been randomized to placebo and fluoxetine-treated youth had a twofold greater probability of response compared to placebo. Finally, the addition of CBT to fluoxetine was associated with a 1.5-fold greater probability of response compared to fluoxetine monotherapy. Taken together, these results suggest that combined treatment “accelerates response relative to CBT alone.”27
Kennard and colleagues28 evaluated remission and residual symptoms following TADS and found that while remission rate were higher in patients who had received fluoxetine + CBT (37%) relative to the other treatment groups (fluoxetine monotherapy, 23%; CBT monotherapy, 16%; placebo, 17%), residual symptoms were common. In this regard, approximately half of patients who had met the definition of response (by CGI criteria) experienced persistent depressive and specifically neurovegetative symptoms (e.g., anergia, dysomnia).28
Treatment of SSRI-Resistant Depression in Adolescents (TORDIA) Study
In many ways, TORDIA29 (Figure 1B) was the natural follow up to TADS. Having established that antidepressants are safe and effective in adolescents with MDD and that persistent depressive symptoms are common,28 TORDIA compared four treatment strategies in adolescents (N=334) aged 12–18 years of age with MDD who failed to respond to greater than two months of initial treatment with an SSRI. Youth were randomized to (1) switch to a different SSRI (paroxetine, citalopram, or fluoxetine); (2) switch to a different SSRI + CBT; (3) switch to venlafaxine; or (4) switch to venlafaxine + CBT. Like in TADS, improvement was assessed with the CGI and with the CDRS. CBT + medication switch (either to another SSRI or venlafaxine) was associated with a marked increase in response compared to simply changing medication, and no differences were detected between switching to venlafaxine relative to another SSRI. Longer term follow-up of the TORDIA patients suggests that by 72 weeks more than 60% of youth reached remission and that the initial TORDIA treatment assignment did not predict remission rate or time to remission. However, it is of interest that the patients who were switched to a second SSRI (as opposed to venlafaxine) experienced a more rapid improvement in depressive symptoms and suicidal ideation than those assigned to venlafaxine.30
Sequential Treatment of Pediatric MDD to Increase Remission & Prevent Relapse Study
Following the natural progression from TADS to TORDIA, the need to establish longer-term outcome data related to the durability and sustainability of treatment related gains became obvious. To address this void the Sequential Treatment of Pediatric MDD to Increase Remission & Prevent Relapse Study randomized 144 pediatric patients (mean age: 13.8 ± 2.6 years, 78.5% aged ≥12 years) to medication management (n=69) or medication management + CBT (n=75) and followed the patients over the course of six months. Most patients experienced remission during the first three months of treatment and no differences in time to remission were detected between the patients who received medication management + CBT compared to those who had just received medication management. However, the risk of relapse was halved in patients who received CBT + medication management compared to medication management alone (36% vs. 62%). The time to relapse was markedly longer (nearly three months) in patients who received adjunctive CBT.
Optimizing Antidepressant Use in Pediatric Patients with MDD
A recent meta-analysis of 13 pediatric trials of SSRIs in adolescents with MDD characterized the course of SSRI response and suggested that treatment gains in youth with MDD follow a logarithmic model. Improvements occur early in the course of treatment with the largest improvements occurring over the first four weeks of treatment with continued improvement in symptoms plateauing thereafter. In this study, there was no relationship between the dose of the medication and response. 31 This finding should be interpreted with caution, given a number of causal inferences. Specifically, it is likely that patients who had exhibited response to an antidepressant would be unlikely to have their antidepressant dose titrated by the treating clinician. In a secondary analysis of plasma antidepressant medication levels in TORDIA (patients with SSRI-resistant MDD)32, following six weeks of treatment with the “new” antidepressant (i.e., and SSRI other than the antidepressant with which they’d been treated previously or venlafaxine.), higher plasma citalopram concentrations were associated with higher response rates and a similar trend was observed for fluoxetine-treated patients. Additionally, increases in the dose of citalopram or fluoxetine at week six were more likely to produce a clinical response when the dose titrations resulted in a change in concentration plasma drug concentration from less than the geometric mean to greater than the geometric mean. Finally, as was recently illustrated in the TORDIA study, frequent assessment of adherence is critical to assess treatment response. In a secondary analyses of adherence among TORDIA participants, that involved assessment of variation in the dose-adjusted concentration of drug plus metabolites (level/dose ratio), approximately half of the study patients (50.8%) were non-adherent.33
Predictors of Antidepressant Treatment Response in Youth with MDD
Clinical trials investigating the efficacy of SSRIs and SSNRIs in youth with MDD illustrate important demographic and clinical factors that influence treatment response.29,34,35 Younger adolescents (<15 years of age) may respond better to pharmacotherapy compared to older adolescents. Among youth who required extended pharmacotherapy (9 months), girls were more likely than boys to experience recurrence of depression (61.1% vs 31.3%).24 Multiple trials suggest that the single most important predictor of treatment response is illness severity, with severely depressed adolescents being markedly more likely to have persistent depression despite treatment compared with less severely depressed youth.23,36,37 Suicidality, independent of depression severity, predicts poorer outcomes in youth with MDD.36,37 Concurrent anxiety disorders are associated with poor antidepressant response36 and concurrent OCD is associated with a higher likelihood of depression persistence.36 Concurrent externalizing disorders (such as ADHD) did not affect treatment response.38 Early response to treatment is a very important predictor of long-term response. Several studies report that adolescents who have higher degrees of response within 12 weeks of treatment (or as little as four weeks in one study39) are more likely to remain in remission at follow-up months to years later22,24,38,40 and also less likely to have developed substance use disorder at follow-up.40
Evidence for Selective Serotonin Reuptake Inhibitors and Selective Serotonin Norepinephrine Reuptake Inhibitors in Pediatric Anxiety Disorders
In addition to tricyclic antidepressants (which will not be reviewed in this article), multiple SSRIs and SNRIs have been evaluated in pediatric patients with anxiety disorders. At present, sertraline has the greatest evidence of efficacy41,42 with much of the currently available data related to SSRI treatment response coming from the largest of these trials, the Child/Adolescent Multimodal Study of Anxiety (see below).42 Randomized controlled trials also suggest benefit for fluoxetine,43 fluvoxamine,44 paroxetine,45 and the SNRIs, venlafaxine46,47 and duloxetine48 with the latter having recently received FDA approval for the treatment of generalized anxiety disorder (GAD) in youth 7–17 years of age.
Child/Adolescent Anxiety Multimodal Study (CAMS)
This NIH-sponsored study involved 488 patients, of whom 78% had a primary diagnosis of GAD.42 In this trial, cognitive behavioral therapy (CBT) was compared to sertraline or the combination of sertraline + CBT or sertraline monotherapy. Sertraline monotherapy was superior to placebo and not statistically different from CBT, while the combination treatment was superior to both monotherapy conditions 8 in terms of clinical global improvement scores. At 24 and 36 weeks following randomization, patients who had been randomized to psychotherapy + sertraline maintained an advantage over CBT and SRT on some symptom severity measures over the follow-up period, whereas the two monotherapies remained indistinguishable. The observed convergence of sertraline + CBT and sertraline or CBT monotherapy may be related to changes in concurrent treatment during the follow-up period or it may have related to the fluctuating course of pediatric anxiety disorders.49,50 Although outcomes were variable, most Child/Adolescent Anxiety Multimodal Study (CAMS)-treated youth experienced sustained treatment benefit.
Child/Adolescent Anxiety Multimodal Extended Long-term Study
Following completion of the acute, twelve-week CAMS treatment trial, nearly 60% of the patients (N=288) continued in Child/Adolescent Anxiety Multimodal Extended Long-term Study (CAMELS), including 82 patients who had received sertraline + CBT, 79 patients who had received sertraline monotherapy, 83 patients who had received CBT monotherapy and 44 patients who had received placebo during the acute treatment phase. Following a mean duration of six years post-initial randomization, nearly half of the sample (47%) were in remission and it was noted that responders (to acute treatment) were more likely to be in remission, highlighting the importance of initial treatment in potentially determining longer term outcome. Several predictors of remission and improved functioning were identified (see below). However, it is noteworthy that relapse was common and occurred in nearly half (48%) of acute responders. These findings highlight the fluctuating course of anxiety and underscore the importance of early treatment.
Predictors of Antidepressant Treatment Response in Youth with Anxiety Disorders
Recent analyses of SSRI and SNRI pharmacotherapy trials in pediatric anxiety disorders have yielded a wealth of information regarding demographic, environmental and clinical predictors of response and remission to treatment. Older age,51 female sex,52 minority status,51 and lower socioeconomic status53 all are associated with lower likelihood of remission following pharmacotherapy. Furthermore, greater caregiver strain54 and a family history of anxiety43 are associated with poorer response to initial treatment, while poor family functioning is associated with lower likelihood of remission.53 As in pediatric depression, baseline illness severity is strongly tied to treatment response with severe anxiety being predictive of poorer functional outcome,43 lower likelihood of initial response to treatment,54,55 and lower likelihood of remission following treatment.51 Three studies identified the presence of social anxiety disorder, at baseline, as a predictor of poorer treatment outcomes,43,51,54 although importantly, data suggest that pharmacotherapy may be necessary to yield any improvement from CBT in youth with a primary diagnosis of social anxiety disorder.54 Comorbid internalizing disorders (e.g. major depression) and comorbid externalizing disorders both predict poorer treatment response in pediatric anxiety disorders,51 although co-occuring externalizing disorders in pediatric depression do not appear to predict response 52
Evidence for Selective Serotonin Reuptake Inhibitors in Obsessive Compulsive Disorder (OCD)
OCD affects 1–2% of the general population and frequently emerges prior to age 21.56,57 Numerous SSRIs, SNRIs and TCAs have been systematically evaluated in youth with OCD; however, based on the currently available evidence, the American Academy of Child & Adolescent Psychiatry recommends cognitive behavioral therapy58 for youth with mild to moderately severe OCD; patients with more severe symptoms of OCD, the combination of an SSRI and CBT may be more effective than CBT alone.58 Regarding the efficacy of SSRIs for the treatment of OCD in youth, several meta-analyses59,60 suggest benefit although the effect sizes in these studies are smaller relative to the effect sizes of these medications for patients with non-OCD pediatric anxiety disorders.61 The choice of antidepressant may be important; findings in one meta-analysis suggest that in pediatric patients with OCD, the tricyclic antidepressant, clomipramine—which is FDA approved for the treatment of OCD in youth62—may be associated with larger effect sizes.59 Nonetheless, SSRIs are considered first-line psychopharmacologic interventions for youth with OCD and three SSRIs are approved for this indication in youth: fluoxetine, fluvoxamine and sertraline. The numerous studies of antidepressants in pediatric patients with OCD, including the Pediatric OCD Study (POTS)63 have recently been reviewed and the reader should see this review for a full discussion.64
Safety and tolerability of Selective Serotonin Reuptake Inhibitors and Selective Serotonin Norepinephrine Reuptake Inhibitors in Youth
Treatment-Emergent Adverse Effects of Antidepressants in Youth
In general, SSRIs and SSNRIs vary little in terms of their side effect profiles with regard to headaches and gastrointestinal side effects (e.g., nausea). Of note, meta-analytic evaluations of these side effects have generally failed to detect treatment-related differences in the frequencies of these events.12 This may, however, relate to the heterogeneity in reporting of these symptoms and may also relate to the relatively high rates of gastrointestinal symptoms, headaches and other somatic symptoms in youth with untreated anxiety65 and depressive disorders as the putative relationship between some antidepressants and plasma drug concentrations (e.g., venlafaxine). Class-related side effects include increases in heart rate and small increases in blood pressure associated with SSNRI treatment in youth.48 Finally, activation, which has been poorly defined in the literature but is generally recognizable by clinicians, has been associated with both SSRIs and SSNRIs. This clinical phenomenon may include irritability, mild disinhibition, increased restlessness and insomnia and in a meta-analysis of youth with anxiety disorders12 who were treated with SSRIs, this is the only treatment-emergent side effect that trended towards statistical significance (p=0.05). Activation, which occurs at higher rates in pediatric patients, compared to adults, has been increasingly recognized over the past 25 years and—very importantly— represents a distinct phenomenon from treatment-emergent mania. Activation appears to be more common in younger patients compared to adolescents, with 10.7% in children compared to 2.1% in adolescents experiencing activation in randomized, controlled trials of antidepressants.66 Nonetheless, considerable variability in observed rates of activation exists67 and this is likely related to the disorder under study, the dose titration, the medication, and other related factors. Regarding these factors, one study of the SSRI fluvoxamine, suggested that activation is associated with plasma drug concentrations during the initial phase of treatment.67
Antidepressants and Suicidality in Children and Adolescents
Concern for the risk of suicidality from antidepressants has received increased attention following the “black box” warning in 2004. However, several studies have failed to detect statistically significant differences between drug and placebo and the rates of treatment-emergent suicidality (e.g., suicidal ideation, suicidal intent, suicidal behavior, etc) appear to vary as a function of disease state as well. In youth with anxiety disorders, two meta-analyses failed to identify an increased risk of treatment-emergent suicidality12,10 However, given the rarity of treatment-emergent suicidality, this should be interpreted with caution. The actual numbers needed to harm for treatment-emergent suicidality are likely to be of value for practicing pediatricians. Bridge and colleagues,10 report that the NNH for treatment-emergent suicidality in youth with depressive disorders is 111, while the NNH for treatment-emergent suicidality in youth with anxiety disorders is 143. Although the majority of analyses have reviewed all antidepressants in general, there is growing concern that paroxetine and venlafaxine may be associated with a higher likelihood treatment emergent suicidality, perhaps related to the short half-life of these agents.21 In anxious children and adolescents treated with paroxetine, suicidal ideation was noted in four paroxetine-treated patients versus zero patients who received placebo.45 Similarly, in one randomized trial of venlafaxine, three patients treated with venlafaxine developed suicidal ideation compared to zero in the placebo group.46 Finally, in the TORDIA study,29 patients randomized to venlafaxine experienced higher rates of treatment-emergent suicidality-related adverse events, although this effect appeared to be mitigated by treatment with CBT. Due to these concerns, paroxetine and venlafaxine are generally not considered as first line interventions in youth with anxiety or depressive disorders.
Efficacy of Stimulants in Attention-Deficit/Hyperactivity Disorder
Attention-deficit/hyperactivity disorder (ADHD) is the most prevalent mental disorder in children and adolescents and is associated with impairment in academic, social and family functioning.68 Stimulant medications are considered first line psychopharmacologic interventions in this population and there are nearly two dozen stimulant medications that have received approval from the USFDA for the treatment of ADHD in children and adolescents. The age ranges associated with these FDA approvals for stimulants ranges from 3 to 17 years, with several preparations of amphetamine salts and methylphenidate approved for use in adult patients with ADHD as well.
There is no evidence that amphetamine salts or methylphenidate-based agents differ in their relative efficacy, although some patients, who do not respond to one agent, may respond to the other class. Many of the advances in stimulant medications are related to the release properties and drug delivery systems which can offer stimulant release throughout the day. Given the ease of administration that accompanies once-daily formulations and compliance difficulties associated with TID or QID dosing of immediate-release preparations, current guidelines recommend long-acting preparations as first-line stimulant pharmacotherapies in youth with ADHD ages 6 or above. In addition to the multiple individual trials of each stimulant preparation, there are two high-quality, seminal studies comparing stimulant treatment with psychosocial interventions that have clearly influenced the guidelines used to treat ADHD. The Multimodal Treatment Study of Children with ADHD (MTA)69 focused on children aged 7–10, while the Preschool ADHD Treatment Study (PATS) focused on younger children (aged 3–5.5 years).70
The Multimodal Treatment Study of Children with ADHD (MTA)
The Multimodal Treatment Study of Children With ADHD (MTA),69 randomized patients to one of four groups: medication treatment alone (with a structured algorithm-based approach), psychosocial treatment alone, algorithm-driven medication management + and psychosocial treatment or “community treatment” (Figure 1). The treatment algorithm involved monthly appointments with a physician during which the stimulant was titrated based on parent and teacher ratings. Treatment-related improvements were observed across all groups (at 14 months relative to baseline). However, algorithm-driven medication management was superior to intensive behavioral treatment alone and community treatment.69 It is noteworthy that the community treatment group had more limited physician follow-up and, in this group, the average daily stimulant dose was significantly lower than in the algorithmic medication management group. Finally, approximately a quarter of youth who were randomized to behavioral management treatment required pharmacologic treatment secondary to a lack of effectiveness of the behavioral treatment. This finding highlights the role of pharmacotherapy in the management of many pediatric patients with ADHD.
Preschool ADHD Treatment Study (PATS)
The Preschool ADHD Treatment Study (PATS) was also a large federally-funded 14 month study, but designed to examine medication efficacy for younger children. All children and their parents first participated in a pre-trial, 10-week behavioral therapy and training course. Only those children who still demonstrated significantly impairing ADHD symptoms were then randomized to receive immediate-release methylphenidate or placebo.71 Methylphenidate was significantly more effective than placebo at treating preschoolers with ADHD, however, at lower weigh-adjusted, smaller effect sizes compared with school-aged children.72
Predictors of Stimulant Treatment Response in Youth with ADHD
Demographic factors (e.g., age, gender) do not appear to consistently predict stimulant response in youth with ADHD73–75 However, as noted above, children under the age of 6 appear to have smaller effect sizes and more side effects from stimulants compared to older children. The subtype of ADHD seems to be an important predictor of treatment response. Children with ADHD and hyperactivity symptoms showing greater improvement with stimulant medications compared to children with ADHD and no hyperactivity symptoms.76 Response is also predicted by psychiatric comorbidities. In preschoolers with ADHD, having three or more comorbidities was predictive of no response to stimulant therapy.74 School-age children with comorbid anxiety and ADHD in the MTA Study, reaped greater benefit from behavioral therapy than those with ADHD alone, although both groups show similar responses to medication management.69 Co-occurring substance use disorders have been associated with poorer response to stimulant treatment, although these youth still exhibit improvement on both ADHD- and substance use-related outcomes with stimulant treatment.77
Response to stimulants in some studies appears to be dose related, although there is no evidence of a global “therapeutic” medication window, with individual patients appearing to have a unique dose-response curve.78 Guidelines recommend pediatricians should select a low starting dose, then titrate upward every 1 to 3 weeks until maximum dose is reached (as defined by the package insert), symptoms of ADHD remit, or side effects prevent further titration. Adherence to stimulant treatment is essential for response. Factors that may limit adherence including parental knowledge and beliefs,79,80 and the child’s past experiences with adverse events or ineffective medications should be explored and addressed clinically with the child and family.81
Safety and Tolerability of Stimulants in Attention-Deficit/Hyperactivity Disorder
While stimulants are generally well tolerated in youth with ADHD, side effects, including decreased appetite, sleep difficulties, rebound hyperactivity or irritability, headache, and gastrointestinal symptoms can become problematic. A meta-analysis of appetite loss associated with stimulant medications in pediatric patients with ADHD suggests that nearly half of methylphenidate-treated patients will experience appetite loss (compared to approximately 15% of placebo-treated patients); however, “serious” appetite loss occurs in 10.5% of stimulant-treated youth (compared to approximately 2% of placebo-treated youth).82 Stimulant-induced appetite decreases appear to be dose related.83 Several strategies have been proposed for the management of stimulant-induced appetite loss, including careful monitoring of appetite, weight and body mass index, administration of medication after breakfast, and the use of calorically-dense snacks (or fourth meals) later in the day or early evening.84
There has been considerable debate about the management of cardiovascular side effects of stimulant medications and, at times, conflicting recommendations have been provided. Stimulants have been associated with elevations in mean blood pressure (<5 mm Hg) and heart rate (<10 beats/min). A subset of individuals (5–10%) may have an even greater increase in heart rate or blood pressure.85 Although there are limited prospective data related to the relationship between cardiac risk factors and outcomes in stimulant-treated youth, prudent recommendations from the American Heart Association and the American Academy of Pediatrics recommend obtaining a thorough history to identify high risk youth with potential cardiac abnormalities or pre-existing cardiac disease prior to initiation of stimulant pharmacotherapy. Routine screening electrocardiography is not indicated in the absence of other cardiac risk factors.
Efficacy of Non-Stimulants in Attention-Deficit/Hyperactivity Disorder
Currently, the efficacy of three non-stimulant medications is supported by randomized controlled trials. Guanfacine extended-release, clonidine extended-release, and atomoxetine have received FDA approval for treatment of ADHD in youth ages 6–17. The α2-agonists, guanfacine and clonidine (as extended-release preparations) have also received FDA-approval for adjunctive use in patients treated with stimulants. These non-stimulants, while clearly shown to be effective for the treatment of ADHD, have much smaller effect sizes then stimulants. Most guidelines recommend that non-stimulants are “second-line” treatments for patients unable to tolerate stimulants, although should be considered first-line interventions if there is concern for abuse or diversion of stimulant medications. They also may have a unique role in the treatment of patients with a “partial response” to stimulant treatment.
Some experts have advocated that non-stimulants be considered first-line interventions in patients with other comorbidities (such as tics and anxiety disorders), although the data fail to consistently support these approaches. For example, some have advocated the use of atomoxetine in patients with anxiety disorders and co-occurring ADHD given that atomoxetine results in improvements in both symptom domains86 and given concerns that stimulants may worsen anxiety. However, data from randomized controlled trials and meta-analyses have consistently failed to demonstrate stimulant-related worsening of anxiety symptoms in patients with anxiety disorders.87 In fact, sequenced treatment trials of adolescents with anxiety disorders and co-occurring attention-deficit/hyperactivity disorder (ADHD) suggest that stimulants may actually reduce anxiety symptoms88 and a recent meta-analysis that included almost 3000 pediatric patients with ADHD found that stimulant treatment was associated with a decreased relative risk of anxiety and also observed a dose-response relationship between stimulant dose and decreases in anxiety symptoms.87
α2-agonists are effective in reducing tic symptoms. They have been recommended by some as medications that should be utilized in youth with ADHD and co-occurring tic disorders given concerns that stimulants can worsen tic severity and frequency. While the package inserts for most stimulants warn clinicians that stimulants are “contraindicated in patients with motor tics or with a family history or diagnosis of Tourette’s syndrome,” the available evidence is not entirely supportive of this association. A recent meta-analysis of 22 studies (involving nearly 2400 youth with ADHD) suggested that new onset tics or worsening of tics to be present in 5.7% of patients receiving stimulants and in 6.5% of patients receiving placebo.87
Safety and tolerability of non-stimulant medications
Atomoxetine appears to have less pronounced effects on appetite and sleep, although it produces more nausea and sedation. Atomoxetine carries a FDA boxed warning regarding the small risk of suicidal thinking due to its mechanistic similarity to noradrenergic reuptake inhibitor antidepressants. The α2-agonists are associated with sedation, dizziness, bradycardia and hypotension, and require ongoing monitoring of blood pressure and pulse. Due to concerns for rebound hypertension, α2 agonists should be gradually tapered rather then abruptly discontinued.
CONCLUSION
The evidence base for psychopharmacologic interventions in youth with depressive and anxiety disorders has dramatically increased over the past two decades. The accumulating data suggest that while antidepressant medications are effective for anxiety disorders and depressive disorders in youth, knowledge of medication-specific tolerability concerns and warnings are critical for safe and effective use of these medications in youth. Knowledge of the specific profiles of some medications discussed in this paper—paroxetine and venlafaxine in particular—suggests that primary care clinicians should exercise caution with these medications and should not use them as first line interventions for youth. Similarly, evidence supporting the use of stimulant and non-stimulant medications in youth with ADHD suggests that these agents are efficacious and generally well-tolerated, but that like antidepressants, knowledge of their side effect and safety profiles is required to utilize effectively these medications. Finally, this review has focused on psychopharmacologic interventions in youth with anxiety disorders, major depressive disorder and ADHD. However, it is critically important to consider psychosocial interventions in the treatment of mental health disorders in youth; the comparative and combined efficacy studies discussed in this paper (TADS, TORDIA, CAMS, MTA, PATS) suggest that psychotherapy may have salutary effects on both symptomatic outcomes and functioning in youth.
TABLE 1.
FDA-Approved Antidepressant Medications in Pediatric Patients
| Class | Medication | FDA Indication | Age range (years) | Target dose (mg/day) |
|---|---|---|---|---|
| SSRI | Fluoxetine | Major depressive disorder Obsessive compulsive disorder |
8–17 7–17 |
40 40 |
| Fluvoxamine | Obsessive compulsive disorder | 8–17 | 150 | |
| Sertraline | Obsessive compulsive disorder | 6–17 | 150 | |
| Escitalopram | Major depressive disorder | 12–17 | >10 | |
| SSNRI | Duloxetine | Generalized anxiety disorder | 7–17 | 60–90 |
Footnotes
DISCLOSURES/ACKNOWLEDGMENTS
Dr. Strawn has received research support from the National Institutes of Health (NIMH), Edgemont, Eli Lilly, Forest Research Institute, Neuronetics, Shire and is an employee of the University of Cincinnati. He also receives material support from Assurex/Genesight. Mr. Dobson has received research support from the American Academy of Child & Adolescent Psychiatry and Dr. Giles reports no biomedical conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Jeffrey R. Strawn, University of Cincinnati, College of Medicine, Cincinnati, Ohio 45267.
Eric Dobson, University of Cincinnati, College of Medicine, Cincinnati, Ohio 45267.
Lisa Giles, Departments of Pediatrics and Psychiatry, University of Utah School of Medicine and Department of Psychiatry and Behavioral Health, Primary Children's Hospital, Salt Lake City, Utah.
References
- 1.Merikangas KR, He J-P, Burstein M, et al. Lifetime prevalence of mental disorders in U.S. adolescents: results from the National Comorbidity Survey Replication--Adolescent Supplement (NCS-A) J Am Acad Child Adolesc Psychiatry. 2010;49:980–989. doi: 10.1016/j.jaac.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Costello EJ, Angold A, Burns BJ, et al. The Great Smoky Mountains Study of Youth. Goals, design, methods, and the prevalence of DSM-III-R disorders. Arch Gen Psychiatry. 1996;53:1129–1136. doi: 10.1001/archpsyc.1996.01830120067012. [DOI] [PubMed] [Google Scholar]
- 3.Husky MM, Olfson M, He J, Nock MK, Swanson SA, Merikangas KR. Twelve-month suicidal symptoms and use of services among adolescents: results from the National Comorbidity Survey. Psychiatr Serv. 2012;63(10):989–996. doi: 10.1176/appi.ps.201200058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Grudnikoff E, Soto EC, Frederickson A, et al. Suicidality and hospitalization as cause and outcome of pediatric psychiatric emergency room visits. Eur Child Adolesc Psychiatry. 2014 doi: 10.1007/s00787-014-0624-x. [DOI] [PubMed] [Google Scholar]
- 5.Nock MK, Green JG, Hwang I, et al. Prevalence, correlates, and treatment of lifetime suicidal behavior among adolescents: results from the National Comorbidity Survey Replication Adolescent Supplement. JAMA Psychiatry. 2013;70(3):300–310. doi: 10.1001/2013.jamapsychiatry.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Merikangas KR, He J, Rapoport J, Vitiello B, Olfson M. Medication use in US youth with mental disorders. JAMA Pediatr. 2013;167(2):141–148. doi: 10.1001/jamapediatrics.2013.431. [DOI] [PubMed] [Google Scholar]
- 7.Stein REK, Horwitz SM, Storfer-Isser A, Heneghan A, Olson L, Hoagwood KE. Do Pediatricians Think They Are Responsible for Identification and Management of Child Mental Health Problems? Results of the AAP Periodic Survey. Ambul Pediatr. 2008;8(1):11–17. doi: 10.1016/j.ambp.2007.10.006. [DOI] [PubMed] [Google Scholar]
- 8.Heneghan A, Garner AS, Storfer-Isser A, Kortepeter K, Stein REK, Horwitz SM. Pediatricians’ role in providing mental health care for children and adolescents: do pediatricians and child and adolescent psychiatrists agree? J Dev Behav Pediatr. 2008;29(4):262–269. doi: 10.1097/DBP.0b013e31817dbd97. [DOI] [PubMed] [Google Scholar]
- 9.Davis DW, Honaker SM, Jones VF, Williams PG, Stocker F, Martin E. Identification and Management of Behavioral/Mental Health Problems in Primary Care Pediatrics: Perceived Strengths, Challenges, and New Delivery Models. Clin Pediatr. 2012;51(10):978–982. doi: 10.1177/0009922812441667. [DOI] [PubMed] [Google Scholar]
- 10.Bridge JA, Iyengar S, Salary CB, et al. Clinical response and risk for reported suicidal ideation and suicide attempts in pediatric antidepressant treatment: a meta-analysis of randomized controlled trials. JAMA. 2007;297(15):1683–1696. doi: 10.1001/jama.297.15.1683. [DOI] [PubMed] [Google Scholar]
- 11.Ipser JC, Stein DJ, Hawkridge S, Hoppe L. Cochrane Review: Pharmacotherapy for anxiety disorders in children and adolescents. Evidence – Based Child Heal A Cochrane Rev J. 2010;5(2):555–628. doi: 10.1002/14651858.CD005170.pub2. [DOI] [PubMed] [Google Scholar]
- 12.Strawn JR, Welge JA, Wehry AM, Keeshin B, Rynn MA. Efficacy and tolerability of antidepressants in pediatric anxiety disorders: a systematic review and meta-analysis. Depress Anxiety. 2015;32(3):149–157. doi: 10.1002/da.22329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Findling RL, McNamara NK, Stansbrey RJ, et al. The relevance of pharmacokinetic studies in designing efficacy trials in juvenile major depression. J Child Adolesc Psychopharmacol. 2006;16(1–2):131–145. doi: 10.1089/cap.2006.16.131. [DOI] [PubMed] [Google Scholar]
- 14.Emslie GJ, Rush J, Weinberg WA, et al. A double-blind, randomized, placebo-controlled trial of fluoxetine in children and adolescents with depression. Arch Gen Psychiatry. 1997;54(11):1031–1037. doi: 10.1001/archpsyc.1997.01830230069010. [DOI] [PubMed] [Google Scholar]
- 15.DelBello MP, Hochadel TJ, Portland KB, et al. A Double-Blind, Placebo-Controlled Study of Selegiline Transdermal System in Depressed Adolescents. J Child Adolesc Psychopharmacol. doi: 10.1089/cap.2013.0138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Emslie GJ, Prakash A, Zhang Q, Pangallo BA, Bangs ME, March JS. A double-blind efficacy and safety study of duloxetine fixed doses in children and adolescents with major depressive disorder. J Child Adolesc Psychopharmacol. 2014;24:170–179. doi: 10.1089/cap.2013.0096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Emslie GJ, Findling RL, Yeung PP, Kunz NR, Li Y. Venlafaxine ER for the treatment of pediatric subjects with depression: results of two placebo-controlled trials. J Am Acad Child Adolesc Psychiatry. 2007;46(4):479–488. doi: 10.1097/chi.0b013e31802f5f03. [DOI] [PubMed] [Google Scholar]
- 18.Bridge JA, Birmaher B, Iyengar S, Barbe RP, Brent DA. Placebo response in randomized controlled trials of antidepressants for pediatric major depressive disorder. Am J Psychiatry. 2009;166:42–49. doi: 10.1176/appi.ajp.2008.08020247. [DOI] [PubMed] [Google Scholar]
- 19.Nakonezny PA, Mayes TL, Byerly MJ, Emslie GJ. Predicting placebo response in adolescents with major depressive disorder: The Adolescent Placebo Impact Composite Score (APICS) J Psychiatr Res. 2015;68:346–353. doi: 10.1016/j.jpsychires.2015.05.003. [DOI] [PubMed] [Google Scholar]
- 20.Kowatch RA, Carmody TJ, Emslie GJ, Rintelmann JW, Hughes CW, Rush AJ. Prediction of response to fluoxetine and placebo in children and adolescents with major depression: A hypothesis generating study. J Affect Disord. 1999;54(3):269–276. doi: 10.1016/s0165-0327(98)00205-5. [DOI] [PubMed] [Google Scholar]
- 21.Rahn KA, Cao YJ, Hendrix CW, Kaplin AI. The role of 5-HT1A receptors in mediating acute negative effects of antidepressants: implications in pediatric depression. Transl Psychiatry. 2015;5:e563. doi: 10.1038/tp.2015.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.March J, Silva S, Petrycki S, et al. Fluoxetine, cognitive-behavioral therapy, and their combination for adolescents with depression: Treatment for Adolescents With Depression Study (TADS) randomized controlled trial. JAMA. 2004;292(7):807–820. doi: 10.1001/jama.292.7.807. [DOI] [PubMed] [Google Scholar]
- 23.March J, Silva S, Curry J, et al. The Treatment for Adolescents With Depression Study (TADS): outcomes over 1 year of naturalistic follow-up. Am J Psychiatry. 2009;166(10):1141–1149. doi: 10.1176/appi.ajp.2009.08111620. [DOI] [PubMed] [Google Scholar]
- 24.Emslie GJ, Kennard BD, Mayes TL, et al. Fluoxetine versus placebo in preventing relapse of major depression in children and adolescents. Am J Psychiatry. 2008;165(4):459–467. doi: 10.1176/appi.ajp.2007.07091453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Poznanski EO, Grossman JA, Buchsbaum Y, Banegas M, Freeman L, Gibbons R. Preliminary studies of the reliability and validity of the children’s depression rating scale. J Am Acad Child Psychiatry. 1984;23(2):191–197. doi: 10.1097/00004583-198403000-00011. [DOI] [PubMed] [Google Scholar]
- 26.Guy W. ECDEU Assessment Manual. 1976. CGI Clinical Global Impressions; pp. 217–222. [Google Scholar]
- 27.Kratochvil C, Emslie G, Silva S, et al. Acute Time to Response in the Treatment for Adolescents with Depression Study (TADS) J Am Acad Child Adolesc Psychiatry. 2006;45(12):1412–1418. doi: 10.1097/01.chi.0000237710.73755.14. [DOI] [PubMed] [Google Scholar]
- 28.Kennard B, Silva S, Vitiello B, et al. Remission and residual symptoms after short-term treatment in the Treatment of Adolescents with Depression Study (TADS) J Am Acad Child Adolesc Psychiatry. 2006;45(12):1404–1411. doi: 10.1097/01.chi.0000242228.75516.21. [DOI] [PubMed] [Google Scholar]
- 29.Brent D, Emslie G, Clarke G, et al. Switching to another SSRI or to venlafaxine with or without cognitive behavioral therapy for adolescents with SSRI-resistant depression: the TORDIA randomized controlled trial. JAMA. 2008;299(8):901–913. doi: 10.1001/jama.299.8.901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Vitiello B, Emslie G, Clarke G, et al. Long-term outcome of adolescent depression initially resistant to selective serotonin reuptake inhibitor treatment: A follow-up study of the TORDIA sample. J Clin Psychiatry. 2011;72(3):388–396. doi: 10.4088/JCP.09m05885blu. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Varigonda AL, Jakubovski E, Taylor MJ, Freemantle N, Coughlin C, Bloch MH. Systematic Review and Meta-Analysis: Early Treatment Responses of Selective Serotonin Reuptake Inhibitors in Pediatric Major Depressive Disorder. J Am Acad Child Adolesc Psychiatry. 2015;54(7):557–564. doi: 10.1016/j.jaac.2015.05.004. [DOI] [PubMed] [Google Scholar]
- 32.DJS, JMP, GJE, et al. Antidepressant exposure as a predictor of clinical outcomes in the Treatment of Resistant Depression in Adolescents (TORDIA) study. J Clin Psychopharmacol. 2011;31(1):92–97. doi: 10.1097/JCP.0b013e318204b117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Woldu H, Porta G, Goldstein T, et al. Pharmacokinetically and clinician-determined adherence to an antidepressant regimen and clinical outcome in the TORDIA Trial. J Am Acad Child Adolesc Psychiatry. 2011;50(5):490–498. doi: 10.1016/j.jaac.2011.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Emslie GJ, Kennard BD, Mayes TL. Predictors of treatment response in adolescent depression. [References] Psychiatr Ann. 2011;(4):213–219. doi: 10.3928/00904481-20110512-05. [DOI] [PubMed] [Google Scholar]
- 35.Goodyer IM, Dubicka B, Wilkinson P, et al. A randomised controlled trial of cognitive behaviour therapy in adolescents with major depression treated by selective serotonin reuptake inhibitors. The ADAPT trial. Heal Technol Assess. 2008;12(14):iii. doi: 10.3310/hta12140. [DOI] [PubMed] [Google Scholar]
- 36.Curry J, Rohde P, Simons A, et al. Predictors and moderators of acute outcome in the Treatment for Adolescents with Depression Study (TADS) J Am Acad Child Adolesc Psychiatry. 2006;45(12):1427–1439. doi: 10.1097/01.chi.0000240838.78984.e2. [DOI] [PubMed] [Google Scholar]
- 37.Asarnow JR, Emslie G, Clarke G, et al. Treatment of selective serotonin reuptake inhibitor-resistant depression in adolescents: predictors and moderators of treatment response. J Am Acad Child Adolesc Psychiatry. 2009;48(3):330–339. doi: 10.1097/CHI.0b013e3181977476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kratochvil CJ, May DE, Silva SG, et al. Treatment response in depressed adolescents with and without co-morbid attention-deficit/hyperactivity disorder in the Treatment for Adolescents with Depression Study. J Child Adolesc Psychopharmacol. 2009;19(5):519–527. doi: 10.1089/cap.2008.0143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tao R, Emslie G, Mayes T, Nakonezny P, Kennard B, Hughes C. Early prediction of acute antidepressant treatment response and remission in pediatric major depressive disorder. J Am Acad Child Adolesc Psychiatry. 2009;48(1):71–78. doi: 10.1097/CHI.0b013e318190043e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Curry J, Silva S, Rohde P, et al. Onset of alcohol or substance use disorders following treatment for adolescent depression. J Consult Clin Psychol. 2012;80(2):299–312. doi: 10.1037/a0026929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rynn MA, Siqueland L, Rickels K. Placebo-controlled trial of sertraline in the treatment of children with generalized anxiety disorder. Am J Psychiatry. 2001;158(12):2008–2014. doi: 10.1176/appi.ajp.158.12.2008. [DOI] [PubMed] [Google Scholar]
- 42.Walkup JT, Albano AM, Piacentini J, et al. Cognitive behavioral therapy, sertraline, or a combination in childhood anxiety. N Engl J Med. 2008;359:2753–2766. doi: 10.1056/NEJMoa0804633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Birmaher B, Axelson Da, Monk K, et al. Fluoxetine for the treatment of childhood anxiety disorders. J Am Acad Child Adolesc Psychiatry. 2003;42(4):415–423. doi: 10.1097/01.CHI.0000037049.04952.9F. [DOI] [PubMed] [Google Scholar]
- 44.Pine DS, Walkup JT, Labellarte MJ, et al. Fluvoxamine for the treatment of anxiety disorders in children and adolescents. N Engl J Med. 2001;344:1279–1285. doi: 10.1056/NEJM200104263441703. [DOI] [PubMed] [Google Scholar]
- 45.Wagner KD, Berard R, Stein MB, et al. A multicenter, randomized, double-blind, placebo-controlled trial of paroxetine in children and adolescents with social anxiety disorder. Arch Gen Psychiatry. 2004;61(11):1153–1162. doi: 10.1001/archpsyc.61.11.1153. [DOI] [PubMed] [Google Scholar]
- 46.March JS, Entusah AR, Rynn M, Albano AM, Tourian KA. A Randomized controlled trial of venlafaxine ER versus placebo in pediatric social anxiety disorder. Biol Psychiatry. 2007;62(10):1149–1154. doi: 10.1016/j.biopsych.2007.02.025. [DOI] [PubMed] [Google Scholar]
- 47.Rynn MA, Riddle MA, Yeung PP, Kunz NR. Efficacy and Safety of Extended-Release Venlafaxine in the Treatment of Generalized Anxiety Disorder in Children and Adolescents: Two Placebo-Controlled Trials. Am J Psychiatry. 2007;164:290–300. doi: 10.1176/ajp.2007.164.2.290. [DOI] [PubMed] [Google Scholar]
- 48.Strawn JR, Prakash A, Zhang Q, et al. A Randomized, Placebo-Controlled Study of Duloxetine for the Treatment of Children and Adolescents With Generalized Anxiety Disorder. J Am Acad Child Adolesc Psychiatry. 2015;54(4):283–293. doi: 10.1016/j.jaac.2015.01.008. [DOI] [PubMed] [Google Scholar]
- 49.Beesdo K, Pine DS, Lieb R, Wittchen H-U. Incidence and risk patterns of anxiety and depressive disorders and categorization of generalized anxiety disorder. Arch Gen Psychiatry. 2010;67(1):47–57. doi: 10.1001/archgenpsychiatry.2009.177. [DOI] [PubMed] [Google Scholar]
- 50.Beesdo K, Knappe S, Pine DS. Anxiety and anxiety disorders in children and adolescents: developmental issues and implications for DSM-V. Psychiatr Clin North Am. 2009;32(3):483–524. doi: 10.1016/j.psc.2009.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ginsburg GS, Kendall PC, Sakolsky D, et al. Remission after acute treatment in children and adolescents with anxiety disorders: findings from the CAMS. J Consult Clin Psychol. 2011;79(6):806–813. doi: 10.1037/a0025933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ginsburg GS, Becker EM, Keeton CP, et al. Naturalistic follow-up of youths treated for pediatric anxiety disorders. JAMA Psychiatry. 2014;71(3):310–318. doi: 10.1001/jamapsychiatry.2013.4186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ginsburg GS, Becker EM, Keeton CP, et al. Naturalistic follow-up of youths treated for pediatric anxiety disorders. JAMA Psychiatry. 2014;71(3):310–318. doi: 10.1001/jamapsychiatry.2013.4186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Compton SN, Peris TS, Almirall D, et al. Predictors and moderators of treatment response in childhood anxiety disorders: results from the CAMS trial. J Consult Clin Psychol. 2014;82(2):212–224. doi: 10.1037/a0035458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Masi G, Pfanner C, Mucci M, et al. Pediatric social anxiety disorder: predictors of response to pharmacological treatment. J Child Adolesc Psychopharmacol. 2012;22(6):410–414. doi: 10.1089/cap.2012.0007. [DOI] [PubMed] [Google Scholar]
- 56.Flament MF, Whitaker A, Rapoport JL, et al. Obsessive compulsive disorder in adolescence: an epidemiological study. J Am Acad Child Adolesc Psychiatry. 1988;27(6):764–771. doi: 10.1097/00004583-198811000-00018. [DOI] [PubMed] [Google Scholar]
- 57.Apter a, Fallon TJ, King Ra, et al. Obsessive-compulsive characteristics: from symptoms to syndrome. J Am Acad Child Adolesc Psychiatry. 1996;35(7):907–912. doi: 10.1097/00004583-199607000-00016. [DOI] [PubMed] [Google Scholar]
- 58.Geller DA, March J. Practice parameter for the assessment and treatment of children and adolescents with obsessive-compulsive disorder. J Am Acad Child Adolesc Psychiatry. 2012;51(1):98–113. doi: 10.1016/j.jaac.2011.09.019. [DOI] [PubMed] [Google Scholar]
- 59.Geller DA, Biederman J, Stewart SE, et al. Which SSRI? A meta-analysis of pharmacotherapy trials in pediatric obsessive-compulsive disorder. Am J Psychiatry. 2003;160(11):1919–1928. doi: 10.1176/appi.ajp.160.11.1919. [DOI] [PubMed] [Google Scholar]
- 60.McGuire JF, Piacentini J, Lewin AB, Brennan EA, Murphy TK, Storch EA. A Meta-Analysis of Cognitive Behavior therapy and Medication for Child Obsessive-Compulsive Dsiorder: Moderators of Treatment Efficacy Response and Remission. Depress Anxiety. 2015;32(8):580–593. doi: 10.1002/da.22389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Strawn JR, Welge JA, Wehry AM, Keeshin B, Rynn MA. Efficacy and Tolerability of Antidepressants in Pediatric Anxiety Disorders: a Systematic Review and Meta-Analysis. Depress Anxiety. 2015;32(3):149–57. doi: 10.1002/da.22329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Flament MF, Rapoport JL, Berg CJ, et al. Clomipramine treatment of childhood obsessive-compulsive disorder. A double-blind controlled study. Arch Gen Psychiatry. 1985;42(10):977–983. doi: 10.1001/archpsyc.1985.01790330057007. [DOI] [PubMed] [Google Scholar]
- 63.Pediatric OCD Treatment Study (POTS) Team. Cognitive-behavior therapy, sertraline, and their combination for children and adolescents with obsessive-compulsive disorder: the Pediatric OCD Treatment Study (POTS) randomized controlled trial. JAMA. 2004;292(16):1969–1976. doi: 10.1001/jama.292.16.1969. [DOI] [PubMed] [Google Scholar]
- 64.Giles LL, Martini DR. Challenges and Promises of Pediatric Psychopharmacology. Academic Pediatrics. 2015 doi: 10.1016/j.acap.2016.03.011. [DOI] [PubMed] [Google Scholar]
- 65.Crawley SA, Caporino NE, Birmaher B, et al. Somatic complaints in anxious youth. Child Psychiatry Hum Dev. 2014;45(4):398–407. doi: 10.1007/s10578-013-0410-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Safer DJ, Zito JM. Treatment-Emergent Adverse Events from Selective Serotonin Reuptake Inhibitors by Age Group: Children versus Adolescents. J Child Adolesc Psychopharmacol. 2006;16(1–2):159–169. doi: 10.1089/cap.2006.16.159. [DOI] [PubMed] [Google Scholar]
- 67.Reinblatt SP, DosReis S, Walkup JT, Riddle MA. Activation adverse events induced by the selective serotonin reuptake inhibitor fluvoxamine in children and adolescents. J Child Adolesc Psychopharmacol. 2009;19(2):119–126. doi: 10.1089/cap.2008.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Wehmeier PM, Schacht A, Barkley Ra. Social and emotional impairment in children and adolescents with ADHD and the impact on quality of life. J Adolesc Health. 2010;46(3):209–217. doi: 10.1016/j.jadohealth.2009.09.009. [DOI] [PubMed] [Google Scholar]
- 69.MTA Cooperative Group. A 14-Month Randomized Clinical Trial of Treatment Strategies for Attention-Deficit/hyperactivity Disorder. The MTA Cooperative Group. Multimodal Treatment Study of Children with ADHD. Arch Gen Psychiatry. 1999;56(12):1073–86. doi: 10.1001/archpsyc.56.12.1073. [DOI] [PubMed] [Google Scholar]
- 70.Greenhill L, Kollins S, Abikoff H, et al. Efficacy and safety of immediate-release methylphenidate treatment for preschoolers with ADHD. J Am Acad Child Adolesc Psychiatry. 2006;45(11):1284–1293. doi: 10.1097/01.chi.0000235077.32661.61. [DOI] [PubMed] [Google Scholar]
- 71.Kollins S, Greenhill L, Swanson J, et al. Rationale, design, and methods of the Preschool ADHD Treatment Study (PATS) J Am Acad Child Adolesc Psychiatry. 2006;45(11):1275–1283. doi: 10.1097/01.chi.0000235074.86919.dc. [DOI] [PubMed] [Google Scholar]
- 72.Greenhill LL, Muniz R, Ball RR, Levine A, Pestreich L, Jiang H. Efficacy and safety of dexmethylphenidate extended-release capsules in children with attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 2006;45(7):817–823. doi: 10.1097/01.chi.0000220847.41027.5d. [DOI] [PubMed] [Google Scholar]
- 73.Johnston BA, Coghill D, Matthews K, Steele JD. Predicting methylphenidate response in attention deficit hyperactivity disorder: A preliminary study. J Psychopharmacol. 2015;29(1):24–30. doi: 10.1177/0269881114548438. [DOI] [PubMed] [Google Scholar]
- 74.Ghuman JK, Riddle MA, Vitiello B, et al. Comorbidity moderates response to methylphenidate in the Preschoolers with Attention-Deficit/Hyperactivity Disorder Treatment Study (PATS) J Child Adolesc Psychopharmacol. 2007;17(5):563–580. doi: 10.1089/cap.2007.0071. [DOI] [PubMed] [Google Scholar]
- 75.Buitelaar JK, van der Gaag RJ, Swaab-Barneveld H, Kuiper M. Prediction of clinical response to methylphenidate in children with attention-deficit hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 1995;34:1025–1032. doi: 10.1097/00004583-199508000-00012. [DOI] [PubMed] [Google Scholar]
- 76.Barkley RA, DuPaul GJ, McMurray MB. Attention deficit disorder with and without hyperactivity: clinical response to three dose levels of methylphenidate. Pediatrics. 1991;87(4):519–531. [PubMed] [Google Scholar]
- 77.Tamm L, Trello-Rishel K, Riggs P, et al. Predictors of treatment response in adolescents with comorbid substance use disorder and attention-deficit/hyperactivity disorder. J Subst Abuse Treat. 2013;44(2):224–230. doi: 10.1016/j.jsat.2012.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Newcorn JH, Stein MA, Cooper KM. Dose-response characteristics in adolescents with attention-deficit/hyperactivity disorder treated with OROS methylphenidate in a 4-week, open-label, dose-titration study. J Child Adolesc Psychopharmacol. 2010;20(3):187–196. doi: 10.1089/cap.2009.0102. [DOI] [PubMed] [Google Scholar]
- 79.Corkum P, Rimer P, Schachar R. Parental knowledge of attention-deficit hyperactivity disorder and opinions of treatment options: impact on enrollment and adherence to a 12-month treatment trial. Can J Psychiatry. 1999;44(10):1043–1048. doi: 10.1177/070674379904401011. [DOI] [PubMed] [Google Scholar]
- 80.dosReis S, Mychailyszyn MP, Evans-Lacko SE, Beltran A, Riley AW, Myers MA. The meaning of attention-deficit/hyperactivity disorder medication and parents’ initiation and continuity of treatment for their child. J Child Adolesc Psychopharmacol. 2009;19(4):377–383. doi: 10.1089/cap.2008.0118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Bussing R, Zima BT, Mason DM, Meyer JM, White K, Garvan CW. ADHD knowledge, perceptions, and information sources: perspectives from a community sample of adolescents and their parents. J Adolesc Health. 2012;51(6):593–600. doi: 10.1016/j.jadohealth.2012.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Schachter HM, Pham B, King J, Langford S, Moher D. How efficacious and safe is short-acting methylphenidate for the treatment of attention-deficit disorder in children and adolescents? A meta-analysis. CMAJ. 2001;165(11):1475–1488. [PMC free article] [PubMed] [Google Scholar]
- 83.Stein MA, Sarampote CS, Waldman ID, et al. A Dose-Response Study of OROS Methylphenidate in Children With Attention-Deficit/Hyperactivity Disorder. Pediatrics. 2003;112(5):e404–e404. doi: 10.1542/peds.112.5.e404. [DOI] [PubMed] [Google Scholar]
- 84.Cortese S, Holtmann M, Banaschewski T, et al. Practitioner Review: Current best practice in the management of adverse events during treatment with ADHD medications in children and adolescents. J Child Psychol Psychiatry Allied Discip. 2013;54(3):227–246. doi: 10.1111/jcpp.12036. [DOI] [PubMed] [Google Scholar]
- 85.Hammerness PG, Perrin JM, Shelley-Abrahamson R, Wilens TE. Cardiovascular risk of stimulant treatment in pediatric attention-deficit/hyperactivity disorder: Update and clinical recommendations. J Am Acad Child Adolesc Psychiatry. 2011;50(10):978–990. doi: 10.1016/j.jaac.2011.07.018. [DOI] [PubMed] [Google Scholar]
- 86.Geller D, Donnelly C, Lopez F, et al. Atomoxetine treatment for pediatric patients with attention-deficit/hyperactivity disorder with comorbid anxiety disorder. J Am Acad Child Adolesc Psychiatry. 2007;46(9):1119–1127. doi: 10.1097/chi.0b013e3180ca8385. [DOI] [PubMed] [Google Scholar]
- 87.Coughlin CG, Cohen SC, Mulqueen JM, Ferracioli-Oda E, Stuckelman ZD, Bloch MH. Meta-analysis: reduced risk of anxiety with psychostimulant treatment in children with attention-deficit/hyperactivity disorder. J Child Adolesc Psychopharmacol. 2015;25(8):611–617. doi: 10.1089/cap.2015.0075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Abikoff H, McGough J, Vitiello B, et al. Sequential pharmacotherapy for children with comorbid attention-deficit/hyperactivity and anxiety disorders. J Am Acad Child Adolesc Psychiatry. 2005;44(5):418–427. doi: 10.1097/01.chi.0000155320.52322.37. [DOI] [PubMed] [Google Scholar]