Abstract
Background
Positive psychological constructs have been associated with reduced suicidal ideation, and interventions to cultivate positive feelings have the potential to reduce suicide risk. This study compares the efficacy of a 6-week, telephone-based positive psychology (PP) intervention against a cognition-focused (CF) control intervention among patients recently hospitalized for depression and suicidal ideation or behavior.
Method
A total of 65 adults with a current major depressive episode reporting suicidal ideation or a recent suicide attempt were enrolled from participating in-patient psychiatric units. Prior to discharge, participants were randomized to the PP (n = 32) or CF (n = 33) intervention. In both interventions, participants received a treatment manual, performed weekly PP (e.g. gratitude letter) or CF (e.g. recalling daily events) exercises, and completed weekly one-on-one telephone sessions over 6 weeks. Between-group differences in hopelessness (primary outcome), depression, suicidality and positive psychological constructs at 6 and 12 weeks were tested using mixed-effects models accounting for intensity of post-hospitalization psychiatric treatment.
Results
Compared with PP, the CF intervention was associated with significantly greater improvements in hopelessness at 6 weeks (β = −3.15, 95% confidence interval −6.18 to −0.12, effect size = −0.84, p = 0.04), but not 12 weeks. Similarly, the CF intervention led to greater improvements in depression, suicidal ideation, optimism and gratitude at 6 and 12 weeks.
Conclusions
Contrary to our hypothesis, the CF intervention was superior to PP in improving hopelessness, other suicide risk factors and positive psychological constructs during a key post-discharge period among suicidal patients with depression. Further study of this CF intervention is warranted in populations at high suicide risk.
Keywords: Cognition, depression, optimism, positive psychology, suicide
Introduction
Each year, over 40 000 Americans die from suicide (Heron, 2013), and suicide rates have increased substantially over the past 15 years (Curtin et al. 2016). Both major depressive disorder (MDD) and recent psychiatric hospitalization significantly increase risk for suicide attempts and completed suicide (Goldacre et al. 1993; Henriksson et al. 1993; Appleby et al. 1999; Brown et al. 2000; Qin & Nordentoft, 2005; Hayashi et al. 2012; Bolton et al. 2015), and one study estimated a 100-fold increased risk for suicide shortly post-discharge relative to never-hospitalized individuals (Qin & Nordentoft, 2005). Thus, there is a critical need to develop and test post-discharge interventions that reduce suicidal behaviors among at-risk individuals.
Most interventions to reduce suicide risk target negative psychological constructs, such as depressed mood, suicidal ideation and hopelessness, which are linked to suicidal behaviors and completed suicide (Brown et al. 2005; Linehan et al. 2006; Bolton et al. 2015). For example, cognitive therapy for the prevention of suicide typically focuses on the core beliefs and thoughts that lead to suicide attempts (Brown et al. 2005), while dialectical behavior therapy focuses both on the identification of thoughts and emotions that lead to suicidal or self-injurious behavior and the development of skills to avoid engaging in those behaviors (Linehan et al. 2006). Unfortunately, such interventions have had limited impact on the prevention of suicidal behaviors (Calati & Courtet, 2016), especially in acute care settings (Inagaki et al. 2015), and current treatments may not be appropriate, feasible or available for patients in the post-discharge period.
Positive psychological constructs also may play a distinct role in reducing suicide risk. Cross-sectional studies have found that positive affect, optimism and gratitude are associated with reduced suicidal ideation or suicide attempts in depressed and non-depressed populations (Hirsch et al. 2007a, b; Yamokoski et al. 2011; Li et al. 2012), often independent of negative affect. Furthermore, positive psychology (PP) interventions, which promote psychological well-being by targeting optimism, gratitude, use of personal strengths and altruism, have been shown to reduce depressive symptoms and enhance well-being in psychiatrically healthy persons (Seligman et al. 2005, 2006; Sin & Lyubomirsky, 2009; Bolier et al. 2013), and there is preliminary evidence for the efficacy of these interventions at reducing depressive symptoms in patients with MDD (Seligman et al. 2006). Given their potential to reduce both depressive symptoms and suicide risk, there has been increasing interest in using PP treatments in psychiatrically ill populations (Jeste et al. 2015). However, there have been no randomized trials of PP interventions for patients with depression and high suicide risk.
Accordingly, we developed a 6-week, telephone-based PP intervention for depressed patients hospitalized for a suicide attempt or suicidal ideation, initiated in-hospital and continued post-discharge. In a randomized trial, we examined the efficacy of the PP intervention in reducing hopelessness (primary study outcome) and other suicide risk factors, as well as promoting positive psychological constructs, compared with an attention-matched, cognition-focused (CF) control intervention that trained participants to systematically recall life events. This CF intervention focused on recalling events from the prior week in a neutral manner. It had some similarities to interventions focused on improving specificity of memory in depression (Watkins et al. 2009), though was largely chosen given its use as a control condition in prior studies (Huffman et al. 2011).
We hypothesized that the PP intervention would result in greater improvement in hopelessness at 6 weeks (primary time point) and 12 weeks, given that this intervention targeted optimism/hope and other positive psychological constructs, and that these constructs have been prospectively associated with lower hopelessness, fewer suicidal thoughts and reduced suicidal behaviors (Hirsch & Conner, 2006; Hirsch et al. 2007a, b; O’Connor et al. 2008; Price et al. 2016). Additionally, we expected that PP would be associated with greater improvements in suicidal ideation, depression, and positive psychological constructs at 6 and 12 weeks compared with the CF intervention.
Method
The Happiness, Optimism, and Positive Emotions (HOPE) study was a single-blind, two-site randomized trial of 6-week PP and CF interventions for patients with a primary diagnosis of MDD. All participants were admitted between October 2013 and June 2015 to in-patient psychiatric units at an urban general hospital or psychiatric hospital for suicidal ideation or following a suicide attempt. Institutional Review Board approval at both sites was obtained, and the trial was registered on ClinicalTrials.gov (NCT02004145) prior to study initiation.
Participants
Eligible participants were English-speaking adults who were: (a) admitted to one of the study site in-patient psychiatric units; (b) had a primary admission diagnosis of MDD with a current major depressive episode [confirmed using the Mini International Neuropsychiatric Interview (MINI); Sheehan et al. 1998]; and (c) expressed suicidal ideation on admission or were admitted following a suicide attempt, based on review of the clinical admission interview in the medical record and confirmed by the patient’s attending physician. Patients were excluded if they had: (a) current psychosis, assessed using the MINI; (b) a cognitive disorder, assessed using a six-item screen developed for research (Callahan et al. 2002); or (c) a primary admission diagnosis of a substance use disorder.
Study procedures
Eligible participants were identified through review of unit census lists. Study staff approached potential participants with the permission of the patient and attending psychiatrist. Staff discussed the study with the patient and administered screening instruments (MINI, cognitive screen) to assess inclusion/exclusion criteria. Eligible patients provided written informed consent, and baseline study outcome measures were completed prior to discharge. Participants were then randomized (via a random number generator) to receive the PP or CF intervention, with group assignments placed in sealed envelopes opened by staff following completion of baseline assessments. During hospitalization, both before and after enrollment, participants in both conditions were free to receive any and all treatments offered by their clinical teams. These potentially included pharmacotherapy, electroconvulsive therapy (ECT), and group and individual psychotherapy.
Study interventionists delivered both PP and CF interventions; participants were paired with the same interventionist for the entire 6-week protocol. Interventionists were psychiatrists, psychologists, or licensed social workers, trained by the study principal investigator on both study conditions. Training included didactic information, observation of experienced team members, role-play, and ongoing feedback from supervising study staff throughout the study.
We chose to develop a telephone-based intervention to improve the reach of this adjunctive intervention, given that in-person visits (especially on top of existing visits with providers) may not be feasible, especially for those with intensive out-patient care, transportation limitations, functional limitations, or those from rural/outlying areas.
Following group assignment, interventionists reviewed with participants the introductory section of the PP or CF manual. Then, participants were assigned an in-hospital exercise to be completed that day. The following day, the interventionist reviewed the exercise with the participant and assigned the second exercise, to be completed over the following week at home. Post-discharge, participants independently completed one exercise each week and had 30-min weekly telephone calls with the interventionist. Calls included a review of the prior week’s exercise and assignment of the next week’s exercise via guided review of the intervention manual. During each telephone session, suicidal ideation was monitored by asking participants to rate their degree of agreement with the following statement: ‘I have been having thoughts of killing myself’. If participants endorsed any suicidal ideation, a detailed suicide evaluation was performed (Suarez et al. 2015) and assistance was provided as needed.
Baseline sociodemographic and medical data were abstracted from the electronic medical record by study staff. Blinded assessors administered psychological outcome measures at baseline and again 6 and 12 weeks post-hospitalization by telephone. At 6-and 12-week assessments, participants were also queried about suicide attempts, self-injurious behavior and rehospitalizations. To assess intervention feasibility, interventionists recorded the number of completed sessions; we defined feasibility a priori as completion of at least four of six exercises by a majority of participants assigned to that condition. Participants were compensated financially for completing follow-up telephone calls at 6 ($25) and 12 ($50) weeks.
Study interventions
PP intervention
The PP intervention utilized six PP-based exercises (see Table 1 and online Supplementary material) chosen due to their demonstrated feasibility and utility in a prior study of suicidal in-patients (Huffman et al. 2014). During each telephone session, interventionists and participants reviewed the week’s section of the treatment manual, which highlighted a specific positive construct (e.g. gratitude) and its role in their recovery. Then, participants were introduced to an associated exercise (e.g. writing a letter of gratitude) and worked with interventionists to develop a practical plan for its completion over the next week. After each telephone session, participants were instructed to complete the exercise and record in their manual the details of the exercise, along with any thoughts and feelings they experienced while performing and documenting the exercise. During each subsequent session, participants and interventionists reviewed the completed exercise, identified positive emotions associated with the exercise, and explored ways to integrate the exercise and associated skill into daily life.
Table 1.
Weekly positive psychology and cognition-focused exercises
| Week | Positive psychology condition | Cognition-focused condition |
|---|---|---|
| 1 | Gratitude for positive events (Seligman et al. 2005): Participants recalled three positive events from the past week and wrote about them | Daily activities: Participants recalled routine events that occurred on a daily basis |
| 2 | Identifying and using personal strengths (Seligman et al. 2005): Participants completed a questionnaire to choose a ‘signature strength’ that was important to them. Then, they used that strength in a new way over the next week | Events related to health: Participants recalled events related to their health (e.g. going to an appointment, taking their medications) |
| 3 | Gratitude letter (Seligman et al. 2005): Participants wrote a letter of gratitude, preferably to someone they had not thanked before. They were encouraged to send the letter to the person for maximal benefit | Activities in the mornings or evenings: Participants recalled events that occurred in the mornings and the evenings |
| 4 | Enjoyable and meaningful activities (Peterson et al. 2005): Participants performed enjoyable and meaningful activities, both alone and with others | Interactions with others: Participants recalled social encounters, whether in-person or remotely (e.g. via email or telephone) |
| 5 | Leveraging past success: Participants recalled a past success and how they were able to be successful. They then thought of how they could use this past experience to help their recovery from depression | Leisure activities: Participants recalled events that occurred during times of leisure, alone or with others |
| 6 | Acts of kindness (Lyubomirsky et al. 2005) or participant choice: Participants performed three kind acts for others. Given evidence that providing participants choice in selecting positive psychology exercises is helpful (Lyubomirsky & Layous, 2013), participants were also given the option to repeat a prior week’s exercise | Participant choice: Participants were asked to repeat a category of their choosing |
CF intervention
The CF control intervention (see Table 1 and online Supplementary material), time- and attention-matched to the PP intervention, focused on emotionally neutral memory recall and was found to be feasible and well accepted in a prior PP-based trial (Huffman et al. 2011). At the first (in-hospital) session, participants received a manual and were introduced to the CF intervention, described as an intervention to assist with memory, organization and concentration. Participants were assigned their first in-hospital exercise: to write down three events that occurred each day over the past week. Participants were encouraged to think of neutral events, to avoid assigning emotions to the events, and to be specific when describing the events (e.g. ‘I had eggs for breakfast’ rather than ‘I had breakfast’). Exercise completion and details were reviewed with interventionists the next day, and subsequent weekly exercises were assigned and reviewed by telephone. To promote participant engagement, the nature, setting or type of events to be recorded differed each week (e.g. medical events).
Intervention fidelity
Study interventionists delivered both interventions, and all sessions were audio-recorded. At weekly interventionist meetings, sessions were reviewed with the project director and interventionists to discuss clinical issues and ensure consistency of intervention delivery. The project director also reviewed randomly selected sessions and rated them on fidelity scales created for the project. The fidelity scales contained ratings related to the logistics of each session, proper delivery of interventions, and assurance that other skills/interventions (e.g. problem-solving, reducing cognitive distortions) were not being used. Sessions were assigned total numerical scores (on a scale of 0–10, with 10 being fully adherent) and interventionists received feedback as needed.
Instruments
Suicide risk factor outcomes: hopelessness (primary outcome), suicidal ideation and depressive symptoms
Beck Hopelessness Scale (BHS; range 0–20)
Hopelessness was measured with the 20-item self-report BHS (Cronbach’s α = 0.92 in this sample) (Beck et al. 1974). The well-established BHS has been used in prior studies examining risk of completed suicide (Beck et al. 1989, 1990).
Concise Health Risk Tracking scale (CHRT; range 12–60)
Suicidal ideation was assessed with the CHRT (α = 0.90) (Trivedi et al. 2011), a 12-item questionnaire previously validated in depressed patients that has participants rate their agreement with such statements as ‘I have been having thoughts of killing myself’ on a scale of 0 (strongly disagree) to 4 (strongly agree).
16-Item Quick Inventory of Depressive Symptomatology, Self-Report (QIDS-SR16; range 0–27)
Depressive symptoms were measured using the well-validated QIDS-SR16 (α = 0.73) (Rush et al. 2003). This scale has been widely used to measure depression in numerous research studies and in clinical care (Trivedi, 2009). We also used item no. 10 (concentration/decision making) to examine the impact of our interventions on cognition.
Though the CHRT is designed to directly assess suicidality, we chose hopelessness, as measured by the BHS, as our primary outcome measure. This is because the BHS has been clearly associated with suicide risk, with elevated BHS scores associated with an elevated risk of completed suicide in both in-patient and outpatient settings (Beck et al. 1989, 1990), while the CHRT’s association with completed suicide has not yet been established.
Positive psychological outcomes: optimism, gratitude and positive affect
Life Orientation Test-Revised (LOT-R; range 0–24)
Optimism was measured using the well-validated six-item LOT-R (α = 0.91) (Herzberg et al. 2006), which has been used in prior studies examining connections between optimism and suicidal ideation (Hirsch & Conner, 2006; Hirsch et al. 2007a; Huffman et al. 2016b).
Gratitude Questionnaire-6 (GQ-6; range 6–42)
Gratitude was measured using the GQ-6 (α = 0.85) (McCullough et al. 2002), a brief, validated six-item measure of dispositional gratitude. The GQ-6 has been studied in a range of populations and used in clinical research projects (McCullough et al. 2002; Ivtzan & Papantoniou, 2014; Huffman et al. 2016a).
Positive and Negative Affect Schedule (PANAS; range 10–50)
Positive affect was measured using the 10-item positive affect subscale of the PANAS (α = 0.93) (Watson et al. 1988). The PANAS has been broadly used to assess affect; this includes use in currently (Berman et al. 2012) and recently (Bagley et al. 2011) depressed samples.
Exploratory outcomes: readmissions, self-injury and suicide attempts
Self-report information about psychiatric readmissions, non-suicidal self-injurious behavior, and suicide attempts was collected at 6- and 12-week follow-up assessments.
Exploratory outcome: impact of the CF condition on cognition
To determine whether the CF condition improved cognition in those participants randomized to this condition, we examined the impact of CF on item no. 10 of the QIDS, which relates to concentration and decision-making.
Data analysis
All analyses were performed using Stata 14 (StataCorp LP, USA). Two-tailed α was set at 0.05 for all analyses. Between-group differences in baseline sociodemographic, psychiatric and self-report outcome variables were calculated using t tests for continuous variables and χ2 analyses for dichotomous variables. In the primary multivariate analyses, rather than selecting covariates based on between-group baseline differences, which can increase the risk of overfitting the model (Babyak, 2004), we selected two markers of post-discharge treatment intensity – partial hospital (PHP) day treatment program and ECT – a priori to control for these factors when assessing intervention efficacy.
To compare between-group differences on change from baseline in BHS (hopelessness), CHRT (suicidal ideation) and QIDS-SR16 (depression) scores at 6 weeks (primary time point) and 12 weeks post-hospitalization, we utilized mixed-effects regression models, with a random intercept for each patient, for multivariable between-group analyses including post-discharge PHP participation and ECT administration as covariates. These models allow inclusion of participants with missing data in an intent-to-treat analysis (Blackwell et al. 2006). Likewise, between-group differences in change from baseline LOT-R (optimism), GQ-6 (gratitude) and PANAS (positive affect) scores at 6 and 12 weeks were compared using multivariable mixed-effects models as above. The effect size of between-group differences in outcomes was also calculated, by dividing the change from baseline of each variable at each time point by the standard deviation of the residual in the regression model.
With a sample size of n = 65, 1:1 group allocation (groups of n = 32 and n = 33), using a two-tailed α of p = 0.05 via univariate analyses between groups, and assuming a between-group difference of medium effect size (Cohen’s d = 0.5), the study was powered at 81% to detect a between-group difference in the primary study outcome of change from baseline hopelessness (BHS) at 6 weeks.
To compare between-group differences on cognition, we utilized the same mixed-effects regression models noted above, controlling for PHP participation and referral to ECT post-discharge. We examined cognition using item no. 10 from the QIDS-SR16, which examines impairments in concentration and decision-making.
Finally, to explore between-group differences on rehospitalizations, non-suicidal self-injurious behavior and suicide attempts over the 12-week assessment period, Fisher’s exact tests were performed, as multivariate regression models would be overfit due to the small expected number of these events.
Results
In all, 94 patients were approached for the study, and 65 (69%) enrolled. Participants were randomized to either the PP (n = 32) or CF (n = 33) intervention [see Consolidated Standards Of Reporting Trials (CONSORT) diagram, Fig. 1]. A total of 58 individuals (89%) provided follow-up data, and all participants were included in the intent-to-treat analyses.
Fig. 1.
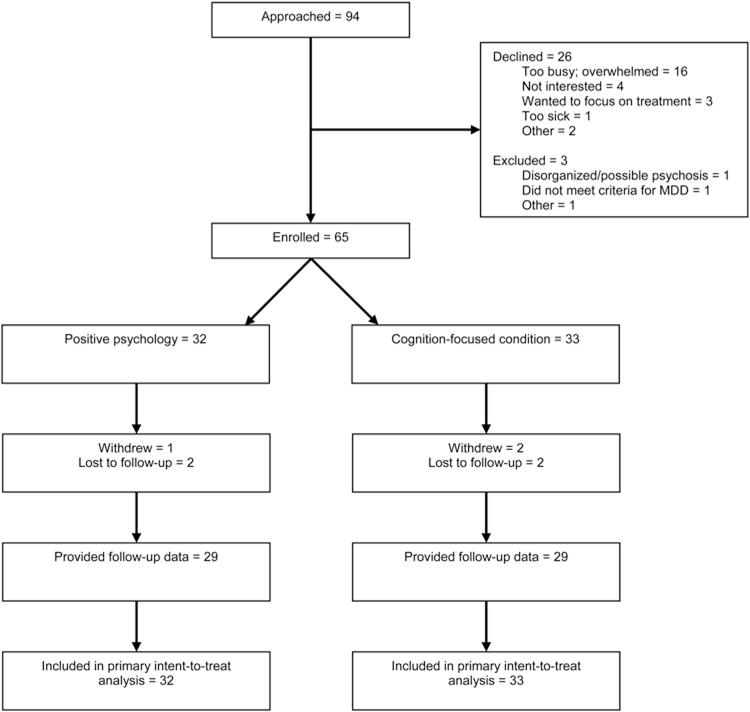
Consolidated Standards Of Reporting Trials (CONSORT) diagram of recruitment. MDD, Major depressive disorder.
Baseline sociodemographic and psychiatric data are summarized in Table 2. Participants’ ages ranged from 19 to 84 years (mean = 44.0, S.D. = 16.6 years), most (69%) were women, and 57 (87%) were white. Of the participants, 27 (42%) had a previous suicide attempt. Mean CHRT scores (mean = 28.6, S.D. = 10.5) were higher than in prior CHRT studies in out-patients (mean = 23.7–25.3) (Ostacher et al. 2015; Reilly-Harrington et al. 2016). There were no significant differences between groups on baseline sociodemographic, psychiatric or outcome measure variables. While in the hospital, similar numbers of patients in each group received ECT (31% in the PP group and 45% in the CF condition; χ2 = 1.38, p = 0.24). However, participants randomized to PP were more likely to have been referred for PHP (53.1% v. 24.2%, χ2 = 5.72, p = 0.02) and less likely to have been referred for post-discharge ECT (3.1% v. 27.3%, χ2 = 7.28, p = 0.007) than CF participants. Despite the differences in ECT between groups, ECT was not significantly associated with change in hopelessness over time (ECT × time point interaction: β = 2.03, p = 0.30 at 6 weeks, β = 2.19, p = 0.28 at 12 weeks).
Table 2.
Baseline characteristics
| PP (n = 32) | CF (n = 33) | Test statistic | p | |
|---|---|---|---|---|
| Sociodemographic variables | ||||
| Mean age, years (S.D.) | 43.2 (17.1) | 44.8 (16.4) | t = 0.39 | 0.70 |
| Male gender | 10 (31.3) | 10 (30.0) | χ2 = 0.01 | 0.93 |
| White race | 28 (84.8) | 29 (87.9) | χ2 = 0.00 | 0.96 |
| Lives alone | 10 (31.3) | 9 (27.3) | χ2 = 0.12 | 0.72 |
| Employed | 13 (40.6) | 12 (36.4) | χ2 = 0.12 | 0.72 |
| Psychiatric history | ||||
| Prior psychiatric hospitalizations | 15 (46.9) | 20 (60.6) | χ2 = 1.23 | 0.27 |
| Prior suicide attempts | 14 (43.8) | 13 (39.4) | χ2 = 0.12 | 0.72 |
| Past or current substance use disorder | 14 (43.8) | 17 (51.5) | χ2 = 0.39 | 0.53 |
| Mean length of stay, days (S.D.) | 9.3 (5.1) | 11.2 (8.0) | t = 1.13 | 0.26 |
| Discharge medications | ||||
| Antidepressant | 30 (93.8) | 31 (93.9) | χ2 = 0.00 | 0.98 |
| Anxiolytic | 11 (34.4) | 12 (36.4) | χ2 = 0.03 | 0.99 |
| Other psychiatric medication | 20 (62.5) | 18 (54.5) | χ2 = 0.42 | 0.52 |
| Intensive aftercare | ||||
| Partial hospitalization program | 17 (53.1) | 8 (24.2) | χ2 = 5.73 | 0.02 |
| Electroconvulsive therapy | 1 (3.1) | 9 (27.3) | χ2 = 7.28 | 0.007 |
| Mean baseline psychological variables (S.D.) | ||||
| Hopelessness: BHS | 10.8 (6.3) | 10.5 (5.4) | t = −0.20 | 0.84 |
| Suicidal ideation: CHRT | 27.9 (11.6) | 29.3 (9.4) | t = 0.53 | 0.59 |
| Depressive symptoms: QIDS-SR16 | 14.9 (5.9) | 15.7 (4.9) | t = 0.61 | 0.54 |
| Optimism: LOT-R | 15.1 (7.1) | 13.6 (6.0) | t = −0.92 | 0.36 |
| Gratitude: GQ-6 | 31.2 (8.3) | 28.5 (8.7) | t = −1.31 | 0.20 |
| Positive affect: PANAS | 19.9 (8.4) | 20.6 (8.9) | t = 0.33 | 0.75 |
Data are given as number of participants (percentage) unless otherwise indicated.
PP, Positive psychology; CF, cognition-focused condition; S.D., standard deviation; BHS, Beck Hopelessness Scale; CHRT, Concise Health Risk Tracking; QIDS-SR16, 16-item Quick Inventory of Depressive Symptomatology – Self-Report; LOT-R, Life Orientation Test – Revised; GQ-6, Gratitude Questionnaire-6; PANAS, Positive and Negative Affect Schedule.
Suicide risk factor outcomes
In multivariable analyses controlling for PHP and ECT (see Table 3, Fig. 2), compared with PP, CF was associated with greater reductions in hopelessness at 6 weeks; this difference was non-significant at 12 weeks. CF also was associated with significantly greater reductions in suicidal ideation and depressive symptoms at both 6 and 12 weeks.
Table 3.
Mixed-effects regression results indicating the impact of the CF intervention (compared with PP) on psychological outcomes at 6 and 12 weeksa
| Outcome | 6 weeks
|
12 weeks
|
||||
|---|---|---|---|---|---|---|
| Coefficient (95% CI) | Effect sizeb | p | Coefficient (95% CI) | Effect sizeb | p | |
| Hopelessness: BHS | −3.15 (−6.28 to −0.12) | −0.84 | 0.04 | −2.53 (−5.51 to 0.46) | −0.67 | 0.10 |
| Suicidality: CHRT | −9.88 (−15.69 to −4.08) | −1.36 | 0.001 | −7.72 (−13.46 to −1.97) | −1.06 | 0.008 |
| Depression: QIDS-SR16 | −4.58 (−8.26 to −0.91) | −1.00 | 0.02 | −5.30 (−8.92 to −1.67) | −1.15 | 0.004 |
| Optimism: LOT-R | 4.84 (1.39 to 8.30) | 1.12 | 0.006 | 4.15 (0.74 to 7.56) | 0.96 | 0.02 |
| Gratitude: GQ-6 | 8.93 (4.77 to 13.09) | 1.73 | <0.001 | 5.50 (1.40 to 9.59) | 1.06 | 0.009 |
| Positive affect: PANAS | 4.13 (−2.08 to 10.34) | 0.53 | 0.19 | 4.63 (−1.50 to 10.77) | 0.59 | 0.14 |
CF, Cognition-focused; PP, positive psychology; CI, confidence interval; BHS, Beck Hopelessness Scale; CHRT, Concise Health Risk Tracking; QIDS-SR16, 16-item Quick Inventory of Depressive Symptomatology – Self-Report; LOT-R, Life Orientation Test – Revised; GQ-6, Gratitude Questionnaire-6; PANAS, Positive and Negative Affect Schedule; ECT, electroconvulsive therapy; PHP, partial hospitalization program.
Results of mixed-effects regression models, controlling for referral to ECT and participation in PHP. Coefficients are group × time interaction values.
Effect size was calculated by dividing the change from baseline of each variable at each time point by the standard deviation of the residual in the regression model.
Fig. 2.
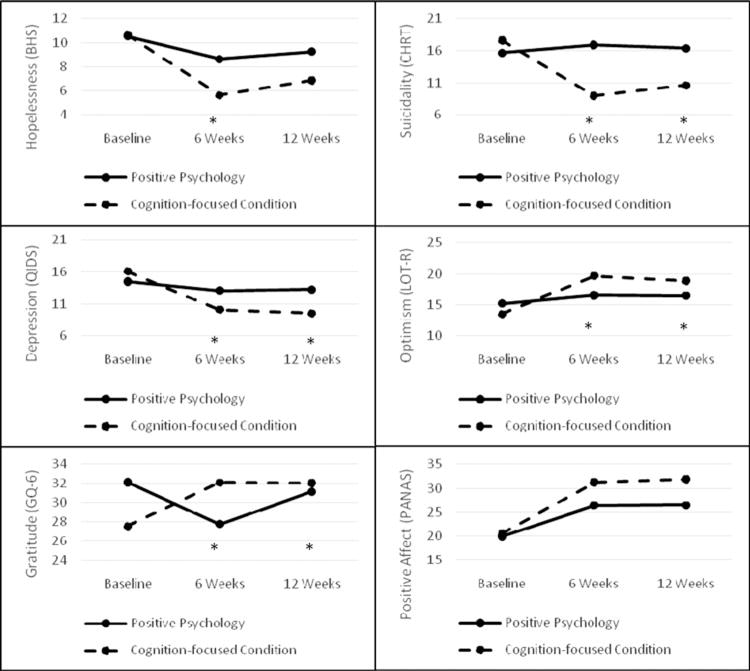
Estimated changes in suicide risk factors and positive psychological constructs (from baseline to 12 weeks). * p < 0.05. BHS, Beck Hopelessness Scale; CHRT, Concise Health Risk Tracking; QIDS, 16-item Quick Inventory of Depressive Symptomatology – Self-Report; LOT-R, Life Orientation Test – Revised; GQ-6, Gratitude Questionnaire-6; PANAS, Positive and Negative Affect Schedule.
Positive psychological outcomes
Relative to PP, the CF condition was associated with significantly greater improvements in optimism and gratitude at 6 and 12 weeks (see Table 3, Fig. 2). There were no significant between-group differences in improvement in positive affect at either time point.
Cognition
Compared with PP, the CF condition led to significantly greater improvements in cognition (QIDS-SR16 item no. 10) at 12 weeks (group × time point interaction: β = −0.90, 95% confidence interval −1.42 to −0.38, p = 0.001), but not at 6 weeks (p = 0.27).
Exploratory outcomes: rehospitalizations, self-injury and suicide attempts
Of the 52 participants who provided 12-week follow-up data regarding rehospitalizations and suicide attempts, six participants were rehospitalized (three per group), six engaged in non-suicidal self-injurious behavior (four in the PP group, two in CF) and one (in the PP group) reported a suicide attempt. The groups did not significantly differ on any of these outcomes.
Feasibility and intervention fidelity
Among PP participants, 20/32 (63%) completed at least four of the six exercises, while 27/33 (82%) in the CF group did so, with a trend towards greater feasibility of CF (χ2 = 3.03, p = 0.08). Mean fidelity ratings were 9.3/10 (S.D. = 0.9) for the PP intervention and 9.6 (S.D. = 0.8) for the CF intervention.
Discussion
Among high-risk patients with MDD and suicidality who were recently discharged following psychiatric hospitalization, the CF intervention was associated with greater reductions in hopelessness at 6 weeks and greater improvement of suicidal ideation, depression and positive psychological outcomes at 6 and 12 weeks, controlling for two markers of concurrent treatment intensity (ECT and PHP).
These findings were in contrast to our hypothesis that the PP condition would be associated with superior benefits. Our results conflict with past results demonstrating that PP interventions lead to reductions in depression and increased well-being (Sin & Lyubomirsky, 2009; Bolier et al. 2013), as well as a prior meta-analysis suggesting that the impact of PP interventions is greater in depressed individuals, compared with those without depression (Sin & Lyubomirsky, 2009). Though few PP studies had been performed in MDD patients, those using similar interventions suggested efficacy in this population (Fava et al. 1998; Seligman et al. 2006).
Both sample- and intervention-related factors may help to explain these findings. First, PP-based interventions may not be additionally beneficial to patients with ongoing moderate depression, hopelessness and suicidal ideation. In contrast to prior studies that delivered PP interventions to out-patients with MDD (Fava et al. 1998; Seligman et al. 2006), we enrolled a high-risk, in-patient sample with substantial ongoing symptoms. That more depressed or hopeless individuals may have had difficulty engaging in PP exercises is plausible. Many of the exercises used in this trial, such as writing a gratitude letter, require initiative and organization that patients in crisis may lack. Furthermore, several exercises require significant interpersonal contact, which may have been a barrier for some depressed patients struggling with low energy or interest.
Psychological factors also may have played a role, as participants may have had difficulty identifying positive aspects of themselves or their lives during a period of recent destabilization. Furthermore, when asked to focus on positive feelings (e.g. gratitude), depressed individuals may have focused instead on the discrepancy between those positive feelings and their current negative ones (Joormann et al. 2007). In addition, following hospital discharge, patients often have numerous work-, life- and treatment-related commitments, as they may be referred to new or additional mental health treatment or need to catch up on tasks missed during hospitalization. Consequently, some participants may have found it difficult to engage fully in the adjunctive PP intervention, which often required more planning and action than the CF intervention, during the immediate post-discharge period. Finally, it may be that the natural course of hopelessness and positive constructs are to worsen substantially post-discharge, given the substantial support offered in the hospital, and both interventions were superior to no treatment, with the CF condition simply being superior in all domains; this hypothesis cannot be tested without a no-treatment condition.
The CF intervention, by contrast, was more effective than anticipated. The CF intervention trained participants to recall specific personal events. Depressed patients have impaired memory for specific life events, and this reduction in autobiographical memory specificity is associated with poor depression recovery (Raes et al. 2009; Sumner et al. 2010). Interventions that target memory specificity may improve cognition and depressive symptoms. In a randomized, controlled trial, a 4-week life review intervention, in which participants recorded autobiographical events in detail, was associated with improvements in memory specificity, depression, hopelessness and life satisfaction (Serrano et al. 2004). Furthermore, a single-arm trial of a similar 4-week life review intervention increased memory specificity, reduced rumination and improved social problem-solving among depressed psychiatric in-patients(Raes et al. 2009). Finally,anintensiveintervention to improve specific, concrete memory led to greater reductions in depression and self-criticism (Watkins et al. 2009).
Memory specificity interventions could lead to decreased depression, hopelessness and other suicide risk factors through several mechanisms. Attenuating negative rumination could reduce depression (van der Velden et al. 2015), and individuals with more life satisfaction may be more hopeful about the future (Koivumaa-Honkanen et al. 2011). Furthermore, improving social problem-solving could improve empowerment and social support, reducing hopelessness (Abramson et al. 1989).
Though our CF intervention was less intensive than the memory specificity interventions described above, it may have improved memory specificity and ultimately produced downstream improvements in hopelessness, suicidal ideation and depression, as well as increases in optimism. This is supported by the finding that the CF intervention did lead to improved concentration/decision making at 12 weeks, compared with PP. One additional mechanism by which this intervention may have provided benefit is through a greater sense of accomplishment and self-efficacy. Participants in the CF group often listed events that involved successful completion of required daily tasks and/or successful social interactions, both of which may have improved self-esteem and self-efficacy. Overall, this straightforward, structured intervention also appeared to be very feasible in this cohort, as evidenced by a trend towards greater completion rates in CF than PP. Further study is needed to determine its benefit as a simple adjunctive treatment for patients with MDD and high suicide risk.
Despite having a number of strengths, it is important to note several limitations of this study. First, the study included a largely white sample recruited from academic medical centers, which may limit generalizability. Second, participants engaged in heterogeneous post-discharge treatment outside of the study interventions, and it was not possible to control for this heterogeneity in our analyses. Finally, our study’s moderate sample size and relatively short follow-up period made it difficult for us to examine the impact of the interventions on our exploratory outcomes of rehospitalizations and suicide attempts, and larger and longer studies are needed to replicate these findings and assess intervention effects on key clinical outcomes.
In sum, relative to a PP intervention, a 6-week CF intervention led to greater reductions in hopelessness and other suicide risk factors in a cohort of recently-hospitalized patients with MDD and suicidal ideation. These findings provide support for further investigation into the use of interventions focusing on memory specificity in this high-risk population.
Supplementary Material
Acknowledgments
This research project was supported by the American Foundation for Suicide Prevention (grant no. SRG-1-035-11 to J.C.H.). Time for analysis and article preparation was also funded by the National Heart, Lung and Blood Institute through grants K23HL123607 (to C.M.C.) and R01HL113272 (to J.C.H.). The National Institute of Mental Health funded time and effort through grant K23MH097786 (to R.P.A.). The content is solely the responsibility of the authors and does not represent the official views of the National Institutes of Health or other funders.
Footnotes
Previous presentation: An abstract was presented at the 62nd Annual Meeting of the Academy of Psychosomatic Medicine, New Orleans, LA, 11–14 November 2015.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S0033291716002798
Declaration of Interest
None.
References
- Abramson LY, Metalsky GI, Alloy LB. Hopelessness depression: a theory-based subtype of depression. Psychological Review. 1989;96:358–372. [Google Scholar]
- Appleby L, Shaw J, Amos T, McDonnell R, Harris C, McCann K, Kiernan K, Davies S, Bickley H, Parsons R. Suicide within 12 months of contact with mental health services: national clinical survey. British Medical Journal. 1999;318:1235–1239. doi: 10.1136/bmj.318.7193.1235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Babyak MA. What you see may not be what you get: a brief, nontechnical introduction to overfitting in regression-type models. Psychosomatic Medicine. 2004;66:411–421. doi: 10.1097/01.psy.0000127692.23278.a9. [DOI] [PubMed] [Google Scholar]
- Bagley SL, Weaver TL, Buchanan TW. Sex differences in physiological and affective responses to stress in remitted depression. Physiology and Behavior. 2011;104:180–186. doi: 10.1016/j.physbeh.2011.03.004. [DOI] [PubMed] [Google Scholar]
- Beck AT, Brown G, Berchick RJ, Stewart BL, Steer RA. Relationship between hopelessness and ultimate suicide: a replication with psychiatric outpatients. American Journal of Psychiatry. 1990;147:190–195. doi: 10.1176/ajp.147.2.190. [DOI] [PubMed] [Google Scholar]
- Beck AT, Brown G, Steer RA. Prediction of eventual suicide in psychiatric inpatients by clinical ratings of hopelessness. Journal of Consulting and Clinical Psychology. 1989;57:309–310. doi: 10.1037//0022-006x.57.2.309. [DOI] [PubMed] [Google Scholar]
- Beck AT, Weissman A, Lester D, Trexler L. The measurement of pessimism: the hopelessness scale. Journal of Consulting and Clinical Psychology. 1974;42:861–865. doi: 10.1037/h0037562. [DOI] [PubMed] [Google Scholar]
- Berman MG, Kross E, Krpan KM, Askren MK, Burson A, Deldin PJ, Kaplan S, Sherdell L, Gotlib IH, Jonides J. Interacting with nature improves cognition and affect for individuals with depression. Journal of Affective Disorders. 2012;140:300–305. doi: 10.1016/j.jad.2012.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blackwell E, de Leon CF, Miller GE. Applying mixed regression models to the analysis of repeated-measures data in psychosomatic medicine. Psychosomatic Medicine. 2006;68:870–878. doi: 10.1097/01.psy.0000239144.91689.ca. [DOI] [PubMed] [Google Scholar]
- Bolier L, Haverman M, Westerhof GJ, Riper H, Smit F, Bohlmeijer E. Positive psychology interventions: a meta-analysis of randomized controlled studies. BioMed Central Public Health. 2013;13:119. doi: 10.1186/1471-2458-13-119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bolton JM, Gunnell D, Turecki G. Suicide risk assessment and intervention in people with mental illness. British Medical Journal. 2015;351:h4978. doi: 10.1136/bmj.h4978. [DOI] [PubMed] [Google Scholar]
- Brown GK, Beck AT, Steer RA, Grisham JR. Risk factors for suicide in psychiatric outpatients: a 20-year prospective study. Journal of Consulting and Clinical Psychology. 2000;68:371–377. [PubMed] [Google Scholar]
- Brown GK, Ten Have T, Henriques GR, Xie SX, Hollander JE, Beck AT. Cognitive therapy for the prevention of suicide attempts: a randomized controlled trial. Journal of the American Medical Association. 2005;294:563–570. doi: 10.1001/jama.294.5.563. [DOI] [PubMed] [Google Scholar]
- Calati R, Courtet P. Is psychotherapy effective for reducing suicide attempt and non-suicidal self-injury rates? Meta-analysis and meta-regression of literature data. Journal of Psychiatric Research. 2016;79:8–20. doi: 10.1016/j.jpsychires.2016.04.003. [DOI] [PubMed] [Google Scholar]
- Callahan CM, Unverzagt FW, Hui SL, Perkins AJ, Hendrie HC. Six-item screener to identify cognitive impairment among potential subjects for clinical research. Medical Care. 2002;40:771–781. doi: 10.1097/00005650-200209000-00007. [DOI] [PubMed] [Google Scholar]
- Curtin SC, Warner M, Hedegaard H. Increase in Suicide in the United States, 1999–2014. National Center for Health Statistics; Hyattsville, MD: 2016. [Google Scholar]
- Fava GA, Rafanelli C, Cazzaro M, Conti S, Grandi S. Well-being therapy. A novel psychotherapeutic approach for residual symptoms of affective disorders. Psychological Medicine. 1998;28:475–480. doi: 10.1017/s0033291797006363. [DOI] [PubMed] [Google Scholar]
- Goldacre M, Seagroatt V, Hawton K. Suicide after discharge from psychiatric inpatient care. Lancet. 1993;342:283–286. doi: 10.1016/0140-6736(93)91822-4. [DOI] [PubMed] [Google Scholar]
- Hayashi N, Igarashi M, Imai A, Yoshizawa Y, Utsumi K, Ishikawa Y, Tokunaga T, Ishimoto K, Harima H, Tatebayashi Y, Kumagai N, Nozu M, Ishii H, Okazaki Y. Post-hospitalization course and predictive signs of suicidal behavior of suicidal patients admitted to a psychiatric hospital: a 2-year prospective follow-up study. BioMed Central Psychiatry. 2012;12:186. doi: 10.1186/1471-244X-12-186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henriksson MM, Aro HM, Marttunen MJ, Heikkinen ME, Isometsa ET, Kuoppasalmi KI, Lonnqvist JK. Mental disorders and comorbidity in suicide. American Journal of Psychiatry. 1993;150:935–940. doi: 10.1176/ajp.150.6.935. [DOI] [PubMed] [Google Scholar]
- Heron M. Deaths: leading causes for 2013. National Vital Statistics Reports. 2013;65:1–94. [PubMed] [Google Scholar]
- Herzberg PY, Glaesmer H, Hoyer J. Separating optimism and pessimism: a robust psychometric analysis of the revised Life Orientation Test (LOT-R) Psychological Assessment. 2006;18:433–438. doi: 10.1037/1040-3590.18.4.433. [DOI] [PubMed] [Google Scholar]
- Hirsch JK, Conner KR. Dispositional and explanatory style optimism as potential moderators of the relationship between hopelessness and suicidal ideation. Suicide and Life-Threatening Behavior. 2006;36:661–669. doi: 10.1521/suli.2006.36.6.661. [DOI] [PubMed] [Google Scholar]
- Hirsch JK, Conner KR, Duberstein PR. Optimism and suicide ideation among young adult college students. Archives of Suicide Research. 2007a;11:177–185. doi: 10.1080/13811110701249988. [DOI] [PubMed] [Google Scholar]
- Hirsch JK, Duberstein PR, Chapman B, Lyness JM. Positive affect and suicide ideation in older adult primary care patients. Psychology and Aging. 2007b;22:380–385. doi: 10.1037/0882-7974.22.2.380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huffman JC, Beale EE, Celano CM, Beach SR, Belcher AM, Moore SV, Suarez L, Motiwala SR, Gandhi PU, Gaggin HK, Januzzi JL. Effects of optimism and gratitude on physical activity, biomarkers, and readmissions after an acute coronary syndrome: the gratitude research in acute coronary events study. Circulation: Cardiovascular Quality and Outcomes. 2016a;9:55–63. doi: 10.1161/CIRCOUTCOMES.115.002184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huffman JC, Boehm JK, Beach SR, Beale EE, DuBois CM, Healy BC. Relationship of optimism and suicidal ideation in three groups of patients at varying levels of suicide risk. Journal of Psychiatric Research. 2016b;77:76–84. doi: 10.1016/j.jpsychires.2016.02.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huffman JC, DuBois CM, Healy BC, Boehm JK, Kashdan TB, Celano CM, Denninger JW, Lyubomirsky S. Feasibility and utility of positive psychology exercises for suicidal inpatients. General Hospital Psychiatry. 2014;36:88–94. doi: 10.1016/j.genhosppsych.2013.10.006. [DOI] [PubMed] [Google Scholar]
- Huffman JC, Mastromauro CA, Boehm JK, Seabrook R, Fricchione GL, Denninger JW, Lyubomirsky S. Development of a positive psychology intervention for patients with acute cardiovascular disease. Heart International. 2011;6:e14. doi: 10.4081/hi.2011.e14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inagaki M, Kawashima Y, Kawanishi C, Yonemoto N, Sugimoto T, Furuno T, Ikeshita K, Eto N, Tachikawa H, Shiraishi Y, Yamada M. Interventions to prevent repeat suicidal behavior in patients admitted to an emergency department for a suicide attempt: a meta-analysis. Journal of Affective Disorders. 2015;175:66–78. doi: 10.1016/j.jad.2014.12.048. [DOI] [PubMed] [Google Scholar]
- Ivtzan I, Papantoniou A. Yoga meets positive psychology: examining the integration of hedonic (gratitude) and eudaimonic (meaning) wellbeing in relation to the extent of yoga practice. Journal of Bodywork and Movement Therapies. 2014;18:183–189. doi: 10.1016/j.jbmt.2013.11.005. [DOI] [PubMed] [Google Scholar]
- Jeste DV, Palmer BW, Rettew DC, Boardman S. Positive psychiatry: its time has come. Journal of Clinical Psychiatry. 2015;76:675–683. doi: 10.4088/JCP.14nr09599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joormann J, Siemer M, Gotlib IH. Mood regulation in depression: differential effects of distraction and recall of happy memories on sad mood. Journal of Abnormal Psychology. 2007;116:484–490. doi: 10.1037/0021-843X.116.3.484. [DOI] [PubMed] [Google Scholar]
- Koivumaa-Honkanen H, Rissanen T, Hintikka J, Honkalampi K, Haatainen K, Tarja S, Viinamaki H. Factors associated with life satisfaction in a 6-year follow-up of depressive out-patients. Social Psychiatry and Psychiatric Epidemiology. 2011;46:595–605. doi: 10.1007/s00127-010-0225-z. [DOI] [PubMed] [Google Scholar]
- Li D, Zhang W, Li X, Li N, Ye B. Gratitude and suicidal ideation and suicide attempts among Chinese adolescents: direct, mediated, and moderated effects. Journal of Adolescence. 2012;35:55–66. doi: 10.1016/j.adolescence.2011.06.005. [DOI] [PubMed] [Google Scholar]
- Linehan MM, Comtois KA, Murray AM, Brown MZ, Gallop RJ, Heard HL, Korslund KE, Tutek DA, Reynolds SK, Lindenboim N. Two-year randomized controlled trial and follow-up of dialectical behavior therapy v. therapy by experts for suicidal behaviors and borderline personality disorder. Archives of General Psychiatry. 2006;63:757–766. doi: 10.1001/archpsyc.63.7.757. [DOI] [PubMed] [Google Scholar]
- Lyubomirsky S, King L, Diener E. The benefits of frequent positive affect: does happiness lead to success? Psychological Bulletin. 2005;131:803–855. doi: 10.1037/0033-2909.131.6.803. [DOI] [PubMed] [Google Scholar]
- Lyubomirsky S, Layous K. How do simple positive activities increase well-being? Current Directions in Psychological Science. 2013;22:57–62. [Google Scholar]
- McCullough ME, Emmons RA, Tsang JA. The grateful disposition: a conceptual and empirical topography. Journal of Personality and Social Psychology. 2002;82:112–127. doi: 10.1037//0022-3514.82.1.112. [DOI] [PubMed] [Google Scholar]
- O’Connor RC, Fraser L, Whyte M, MacHale S, Masterton G. A comparison of specific positive future expectancies and global hopelessness as predictors of suicidal ideation in a prospective study of repeat self-harmers. Journal of Affective Disorders. 2008;110:207–214. doi: 10.1016/j.jad.2008.01.008. [DOI] [PubMed] [Google Scholar]
- Ostacher MJ, Nierenberg AA, Rabideau D, Reilly-Harrington NA, Sylvia LG, Gold AK, Shesler LW, Ketter TA, Bowden CL, Calabrese JR, Friedman ES, Iosifescu DV, Thase ME, Leon AC, Trivedi MH. A clinical measure of suicidal ideation, suicidal behavior, and associated symptoms in bipolar disorder: psychometric properties of the Concise Health Risk Tracking Self-Report (CHRT-SR) Journal of Psychiatric Research. 2015;71:126–133. doi: 10.1016/j.jpsychires.2015.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peterson C, Park N, Seligman ME. Orientations to happiness and life satisfaction: the full life versus the empty life. Journal of Happiness Studies. 2005;6:25–41. [Google Scholar]
- Price MA, Butow PN, Bell ML, deFazio A, Friedlander M, Fardell JE, Protani MM, Webb PM, AOCS – Quality of Life Study Investigators on behalf of the Australian Ovarian Cancer Study Group Helplessness/hopelessness, minimization and optimism predict survival in women with invasive ovarian cancer: a role for targeted support during initial treatment decision-making? Supportive Care in Cancer. 2016;24:2627–2634. doi: 10.1007/s00520-015-3070-5. [DOI] [PubMed] [Google Scholar]
- Qin P, Nordentoft M. Suicide risk in relation to psychiatric hospitalization: evidence based on longitudinal registers. Archives of General Psychiatry. 2005;62:427–432. doi: 10.1001/archpsyc.62.4.427. [DOI] [PubMed] [Google Scholar]
- Raes F, Williams JM, Hermans D. Reducing cognitive vulnerability to depression: a preliminary investigation of MEmory Specificity Training (MEST) in inpatients with depressive symptomatology. Journal of Behavior Therapy and Experimental Psychiatry. 2009;40:24–38. doi: 10.1016/j.jbtep.2008.03.001. [DOI] [PubMed] [Google Scholar]
- Reilly-Harrington NA, Shelton RC, Kamali M, Rabideau DJ, Shesler LW, Trivedi MH, McElroy SL, Sylvia LG, Bowden CL, Ketter TA, Calabrese JR, Thase ME, Bobo WV, Deckersbach T, Tohen M, McInnis MG, Kocsis JH, Gold AK, Singh V, Finkelstein DM, Kinrys G, Nierenberg AA. A tool to predict suicidal ideation and behavior in bipolar disorder: The Concise Health Risk Tracking Self-Report. Journal of Affective Disorders. 2016;192:212–218. doi: 10.1016/j.jad.2015.12.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rush AJ, Trivedi MH, Ibrahim HM, Carmody TJ, Arnow B, Klein DN, Markowitz JC, Ninan PT, Kornstein S, Manber R, Thase ME, Kocsis JH, Keller MB. The 16-Item Quick Inventory of Depressive Symptomatology (QIDS), clinician rating (QIDS-C), and self-report (QIDS-SR): a psychometric evaluation in patients with chronic major depression. Biological Psychiatry. 2003;54:573–583. doi: 10.1016/s0006-3223(02)01866-8. [DOI] [PubMed] [Google Scholar]
- Seligman ME, Rashid T, Parks AC. Positive psychotherapy. American Psychologist. 2006;61:774–788. doi: 10.1037/0003-066X.61.8.774. [DOI] [PubMed] [Google Scholar]
- Seligman ME, Steen TA, Park N, Peterson C. Positive psychology progress: empirical validation of interventions. American Psychologist. 2005;60:410–421. doi: 10.1037/0003-066X.60.5.410. [DOI] [PubMed] [Google Scholar]
- Serrano JP, Latorre JM, Gatz M, Montanes J. Life review therapy using autobiographical retrieval practice for older adults with depressive symptomatology. Psychology and Aging. 2004;19:270–277. doi: 10.1037/0882-7974.19.2.270. [DOI] [PubMed] [Google Scholar]
- Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, Hergueta T, Baker R, Dunbar GC. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. Journal of Clinical Psychiatry. 1998;59(Suppl 20):22–33. [PubMed] [Google Scholar]
- Sin NL, Lyubomirsky S. Enhancing well-being and alleviating depressive symptoms with positive psychology interventions: a practice-friendly meta-analysis. Journal of Clinical Psychology. 2009;65:467–487. doi: 10.1002/jclp.20593. [DOI] [PubMed] [Google Scholar]
- Suarez L, Beach SR, Moore SV, Mastromauro CA, Januzzi JL, Celano CM, Chang TE, Huffman JC. Use of the Patient Health Questionnaire-9 and a detailed suicide evaluation in determining imminent suicidality in distressed patients with cardiac disease. Psychosomatics. 2015;56:181–189. doi: 10.1016/j.psym.2014.12.005. [DOI] [PubMed] [Google Scholar]
- Sumner JA, Griffith JW, Mineka S. Overgeneral autobiographical memory as a predictor of the course of depression: a meta-analysis. Behaviour Research and Therapy. 2010;48:614–625. doi: 10.1016/j.brat.2010.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trivedi MH. Tools and strategies for ongoing assessment of depression: a measurement-based approach to remission. Journal of Clinical Psychiatry. 2009;70(Suppl 6):26–31. doi: 10.4088/JCP.8133su1c.04. [DOI] [PubMed] [Google Scholar]
- Trivedi MH, Wisniewski SR, Morris DW, Fava M, Gollan JK, Warden D, Nierenberg AA, Gaynes BN, Husain MM, Luther JF, Zisook S, Rush AJ. Concise Health Risk Tracking scale: a brief self-report and clinician rating of suicidal risk. Journal of Clinical Psychiatry. 2011;72:757–764. doi: 10.4088/JCP.11m06837. [DOI] [PubMed] [Google Scholar]
- van der Velden AM, Kuyken W, Wattar U, Crane C, Pallesen KJ, Dahlgaard J, Fjorback LO, Piet J. A systematic review of mechanisms of change in mindfulness-based cognitive therapy in the treatment of recurrent major depressive disorder. Clinical Psychology Review. 2015;37:26–39. doi: 10.1016/j.cpr.2015.02.001. [DOI] [PubMed] [Google Scholar]
- Watkins ER, Baeyens CB, Read R. Concreteness training reduces dysphoria: proof-of-principle for repeated cognitive bias modification in depression. Journal of Abnormal Psychology. 2009;118:55–64. doi: 10.1037/a0013642. [DOI] [PubMed] [Google Scholar]
- Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: the PANAS scales. Journal of Personality and Social Psychology. 1988;54:1063–1070. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- Yamokoski CA, Scheel KR, Rogers JR. The role of affect in suicidal thoughts and behaviors. Suicide and Life-Threatening Behavior. 2011;41:160–170. doi: 10.1111/j.1943-278X.2011.00019.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


